Consumer Preferences and Attitudes towards Antibiotic Use in Food Animals
Abstract
:1. Introduction
2. Literature Review
3. Results
3.1. Responses
3.2. Descriptive Analysis
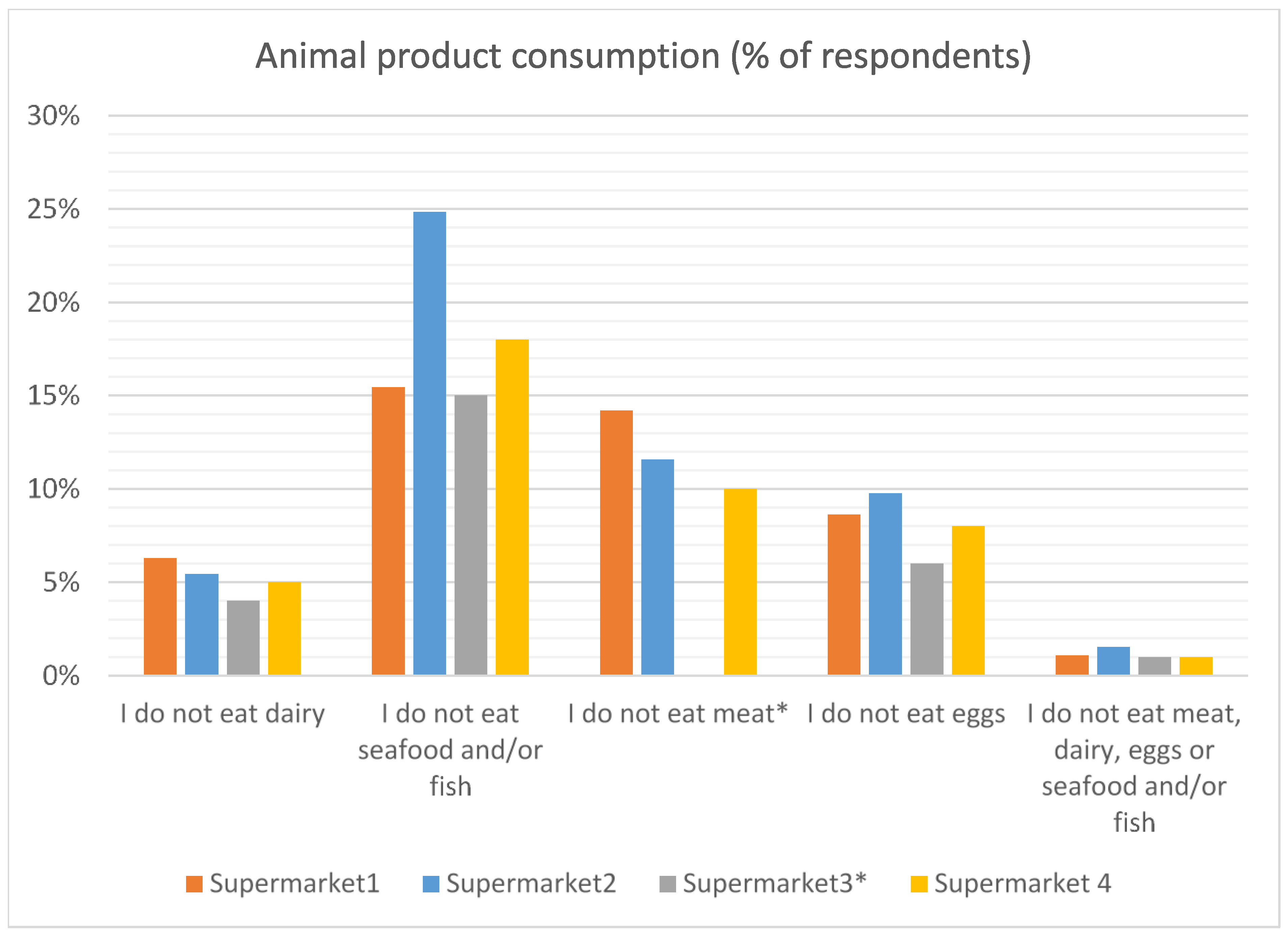
3.2.1. Animal Product Consumption
3.2.2. Attitudes towards Animal Use

3.2.3. Perceived Risk of Animal Treatments




3.2.4. Attitudes to Vaccination

3.2.5. Personal Experience of Antibiotic Use

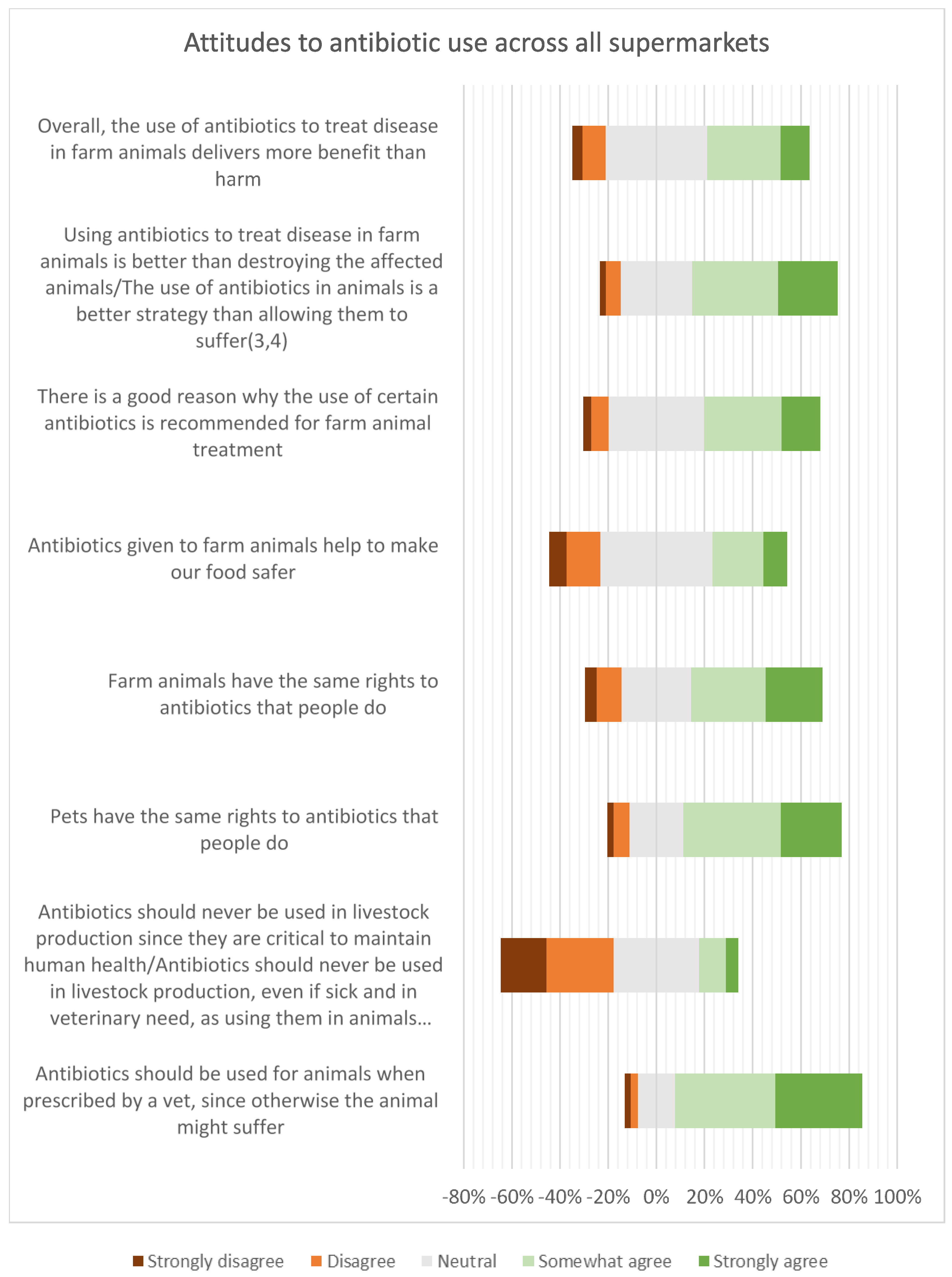
3.2.6. Attitudes to Antibiotic Use in Animals

3.2.7. Awareness of Antibiotic Resistance

3.2.8. Knowledge of Antibiotic Use and Resistance

3.3. Inferential Analysis
3.3.1. Demographics
3.3.2. Consumer Attitudes towards Antibiotic Use in Livestock
3.3.3. Consumer Preferences for Products Labelled Antibiotic-Free
4. Discussion
“It would be a brave politician who, after having made the electorate and their children jump through inconvenient and expensive hoops before being prescribed an antibiotic, would not expect livestock and companion animals to jump even higher”([40], p. 169).
5. Materials and Methods
5.1. Questionnaire Design
5.2. Data Collection
5.3. Data Analysis
5.4. Descriptive Analysis
5.5. Inferential Analysis
5.5.1. Predictor Variables
5.5.2. Outcome Variables
5.5.3. Analysis
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Walsh, F. Antibiotics Resistance ‘As Big As Terrorism’—Medical Chief. BBC News [Online]. 11 March 2013. Available online: https://www.bbc.co.uk/news/health-21737844 (accessed on 5 September 2023).
- ESPAUR Report 2021 to 2022 English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR) Report 2021 to 2022, London: UK Health Security Agency; November 2022. Available online: https://www.gov.uk/government/news/new-antibiotic-resistant-infections-rise-to-178-per-day-in-england (accessed on 5 September 2023).
- Fischer, M.M.; Bild, M. Hospital use of antibiotics as the main driver of infections with antibiotic-resistant bacteria—A reanalysis of recent data from the European Union. bioRxiv 2019, 553537. [Google Scholar] [CrossRef]
- Chang, Q.; Wang, W.; Regev-Yochay, G.; Lispitch, M.; Hanage, W. Antibiotics in agriculture and the risk to human health: How worried should we be? Evol. Appl. 2015, 8, 240–247. [Google Scholar] [CrossRef] [PubMed]
- Magouras, I.; Carmo, L.P.; Stärk, K.D.C.; Schüpbach-Regula, G. Antimicrobial Usage and -Resistance in Livestock: Where Should We Focus? Front. Vet. Sci. 2017, 4, 148. [Google Scholar] [CrossRef] [PubMed]
- Bennani, H.; Mateys, A.; Mays, N.; Eastmure, E.; Stãrk, K.D.C.; Häsler, B. Review of antimicrobial use and antimicrobial resistance in the food chain. Antibiotics 2020, 9, 49. [Google Scholar] [CrossRef]
- Review of Antimicrobial Resistance. Tackling Drug-Resistant Infections Globally: Final Report. In The Review on Antimicrobial Resistance; H.M. Government and the Wellcome Trust: London, UK, 2016. [Google Scholar]
- UK-VARSS Veterinary Antibiotic Resistance and Sales Surveillance Report (UK-VARSS 2021). New Haw, Addlestone: Veterinary Medicine Directorate. 2021. Available online: www.gov.uk (accessed on 19 August 2023).
- Hudson, J.A.; Frewer, L.J.; Jones, G.; Brereton, P.; Whittingham, M.J.; Stewart, G. The Agri-food chain and antimicrobial resistance: A review. Trends Food Sci. Technol. 2017, 69, 131–147. [Google Scholar] [CrossRef]
- Lechner, I.; Freivogel, C.; Stärk, K.D.C.; Visschers, V.H.M. Exposure Pathways to Antimicrobial Resistance at the Human-Animal Interface—A Qualitative Comparison of Swiss Expert and Consumer Opinions. Front. Public Health 2020, 8, 345. [Google Scholar] [CrossRef]
- Hocknell, S.; Hughes, A.; Roe, E.; Keevil, B.; Wrigley, N.; Lowe, M. Corporate Food Retailers, Meat Supply Chains, and the Responsibilities of Tackling Antimicrobial Resistance. Stakeholder Report. 2018. Available online: https://eprints.ncl.ac.uk/file_store/production/253101/D0EA9E6C-A2E1-4596-89BF-AC4B6A7E556E.pdf (accessed on 20 February 2021).
- Doidge, C.; Hudson, C.; Lovatt, F.; Kalevr, J. To prescribe or not to prescribe? A factorial survey to explore veterinarians’ decision making when prescribing antimicrobials to sheep and beef farmers in the UK. PLoS ONE 2019, 14, e0213855. [Google Scholar] [CrossRef]
- Fischer, K.; Sjöström, K.; Stienström, A.; Emanuelson, U. Dairy farmers’ perspectives on antibiotic use: A qualitative study. J. Dairy Sci. 2019, 102, 2724–2737. [Google Scholar] [CrossRef]
- Adam, K. Balancing conflicting demands: Factors influencing vets’ choice of antimicrobial agent. Vet. Rec. 2019, 184, 795–797. [Google Scholar] [CrossRef]
- Schneider, S.; Salm, F.; Vincze, S.; Moeser, A.; Petruschke, I.; Schmücker, K.; Ludwig, N.; Hanke, R.; Schröder, C.; Gropmann, A.; et al. Perceptions and attitudes regarding antibiotic resistance in Germany: A cross-sectoral survey amongst physicians, veterinarians, farmers and the general public. J. Antimicrob. Chemother. 2018, 73, 1984–1988. [Google Scholar] [CrossRef]
- Begemann, S.; Watkins, F.; van Hoyweghen, I.; Vivancos, R.; Christley, R.; Perkins, E. The Governance of UK Dairy Antibiotic Use: Industry-Led Policy in Action. Front. Vet. Sci. 2020, 7, 557. [Google Scholar] [CrossRef] [PubMed]
- Alban, L.; Dahl, J.; Andreasen, M.; Petersen, J.V.; Sandberg, M. Possible impact of the “yellow card” antimicrobial scheme on meat inspection lesions in Danish finisher pigs. Prev. Vet. Med. 2013, 108, 334–341. [Google Scholar] [CrossRef] [PubMed]
- Eriksen, E.O.; Smed, S.; Klit, K.J.; Olsen, J.E. Factors influencing Danish veterinarians’ choice of antimicrobials prescribed for intestinal diseases in weaner pigs. Vet. Rec. 2019, 184, 798. [Google Scholar] [CrossRef] [PubMed]
- Carmo, L.P.; Nielsen, L.R.; Alban, L.; da Costa, P.M.; Schüpbach-Regula, G.; Magoulras, I. Veterinary Expert Opinion on Potential Drivers and Opportunities for Changing Antimicrobial Usage Practices in Livestock in Denmark, Portugal, and Switzerland. Front. Vet. Sci. 2018, 5, 29. [Google Scholar] [CrossRef] [PubMed]
- Hinchliffe, S.; Butcher, A.; Rahman, M.M. The AMR problem: Demanding economies, biological margins, and co-producing alternative strategies. Palgrave Commun. 2018, 4, 142. [Google Scholar] [CrossRef]
- McCullough, A.R.; Parekh, S.; Rathbone, J.; Del Mar, C.B.; Hoffman, T.C. A systematic review of the public’s knowledge and beliefs about antibiotic resistance. J. Antimicrob. Chemother. 2016, 71, 27–33. [Google Scholar] [CrossRef]
- Regan, A.; Sweeney, S.; McKernan, C.; Benson, T.; Dean, M. Consumer perception and understanding of the risks of antibiotic use and antimicrobial resistance in farming. Agric. Hum. Values 2022, 40, 989–1001. [Google Scholar] [CrossRef]
- Cornejo, J.; Cabezón, C.; San Martín, B.; Lapierre, L. Assessment of Consumer Perceptions on the Use of Antimicrobials in Production Animals in Chlle. J. Food Prot. 2018, 81, 1331–1338. [Google Scholar] [CrossRef]
- Ding, Q.; Gao, J.; Ding, X.; Huang, D.; Zhao, Y.; Yang, M. Consumers’ knowledge, attitude, and behaviour towards antimicrobial resistance and antimicrobial use in food production in China. Front. Public Health 2022, 10, 1015950. [Google Scholar] [CrossRef]
- Wemette, M.; Greiner Safi, A.; Wolverton, A.K.; Beuvais, W.; Shapiro, M.; Moroni, P.; Welcome, F.L.; Ivanek, R. Public perceptions of antibiotic use on dairy farms in the United States. J. Dairy Sci. 2021, 104, 2807–2821. [Google Scholar] [CrossRef]
- Busch, G.; Kassas, B.; Palma, M.A.; Risius, A. Perceptions of antibiotic use in livestock farming in Germany, Italy and the United States. Livest. Sci. 2020, 241, 104251. [Google Scholar] [CrossRef]
- Goddard, E.; Hartmann, M.; Klink-Lehmann, J. Public Acceptance of Antibiotic Use in Livestock Production Canada and Germany. Proc. Food Syst. Dyn. 2017, 424–437. [Google Scholar] [CrossRef]
- Bradford, H.; McKernan, C.; Elliott, C.; Dean, M. Consumers’ perceptions and willingness to purchase pork labelled ‘raised without antibiotics. Appetite 2022, 171, 105900. [Google Scholar] [CrossRef] [PubMed]
- Barret, J.R.; Innes, G.K.; Johnson, K.A.; Lhermie, G.; Ivanek, R.; Safi, A.G.; Lansing, D. Consumer perceptions of antimicrobial use in animal husbandry: A scoping review. PLoS ONE 2021, 16, e0261010. [Google Scholar] [CrossRef]
- Meerza, S.I.A.; Gulab, S.; Brooks, K.R.; Gustafson, C.R.; Yiannaka, A.U.S. Consumer Attitudes towards Antibiotic Use in Livestock Production. Sustainability 2022, 14, 7035. [Google Scholar] [CrossRef]
- Kirchelle, C. Pharming animals: A global history of antibiotics in food production (1935–2017). Palgrave Commun. 2018, 4, 96. [Google Scholar] [CrossRef]
- Woods, A. Decentring antibiotics: UK responses to the diseases of intensive pig production (ca. 1925-65). Palgrave Commun. 2018, 5, 41. [Google Scholar] [CrossRef]
- Regulation (EU) 2019/6 of the European Parliament and of the Council of 11 December 2018 on Veterinary Medicinal Products and Repealing Directive 2001/82/EEC. Available online: https://eur-lex.europa.eu/legal-content/EN/AUTO/?uri=celex:32019R0006 (accessed on 29 September 2023).
- Cervantes, H.M. Antibiotic-free poultry production: Is it sustainable? J. Appl. Poult. Res. 2015, 24, 91–97. [Google Scholar] [CrossRef]
- Hughes, A.; Roe, E.; Hocknell, S. Food supply chains and the antimicrobial resistance challenge: On the framing, accomplishments and limitations of corporate responsibility. Environ. Plan. A Econ. Space 2021, 53, 1373–1390. [Google Scholar] [CrossRef]
- Jia, S.; McWhorter, A.R.; Andrews, D.M.; Underwood, G.J.; Chousalkar, K.K. Challenges in vaccinating layer hens against Salmonella TyphimuriumI. Vaccines 2020, 8, 696. [Google Scholar] [CrossRef]
- Redding, L.E.; Parsons, B.; Bender, J.S. Educational interventions to address misconceptions about antibiotic residues in milk can alter consumer perception and may affect purchasing habits. J. Dairy Sci. 2021, 104, 11474–11485. [Google Scholar] [CrossRef]
- Schell, R.C.; Bulut, E.; Padda, H.; Safi, A.G.; Moroni, P.; Ivanek, R. Responsible antibiotic use labeling and consumers’ willingness to buy and pay for fluid milk. J. Dairy Sci. 2022, 106, 150. [Google Scholar] [CrossRef] [PubMed]
- Ancilotti, M.; Nilsson, E.; Nordvall, A.-C.; Oljans, E. The Status Quo problem and the Role of Consumers against Antimicrobial Resistance. Front. Sustain. Food Syst. 2022, 6, 834022. [Google Scholar] [CrossRef]
- Scannell, J.W.; Bruce, A. Antibiotics: Expect to use less, more responsibly. Vet. Rec. 2015, 177, 168–170. [Google Scholar] [CrossRef] [PubMed]
- Roselius, T. Consumer Rankings of Risk Reduction Methods. J. Mark. 1971, 35, 56. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2019; Available online: https://www.R-project.org/ (accessed on 29 September 2023).
| Variable | Supermarket 2 Respondents | UK Population * | |
|---|---|---|---|
| Gender 1 | Male | 41.3% | 49% |
| Female | 58.7% | 51% | |
| Age 2 | 18–34 | 31% | - |
| 20–34 | - | 26% | |
| 35–44 | 16.5% | 16% | |
| 45–54 | 17.5% | 18% | |
| 55 or over | 33.8% | 40% | |
| Prefer not to say | 1.2% | - | |
| Region 3 | East Midlands | 8.5% | 7.2% |
| East of England | 6.0% | 9.3% | |
| London | 13.5% | 13.4% | |
| North East | 6.0% | 4.0% | |
| North West | 11.5% | 11.0% | |
| Scotland | 6.0% | 8.2% | |
| South East | 15.5% | 13.7% | |
| South West | 11.1% | 8.4% | |
| Wales | 3.8% | 4.7% | |
| West Midlands | 9.7% | 8.9% | |
| Yorkshire and the Humber | 7.5% | 8.2% | |
| Prefer not to say | 0.9% | - | |
| Rural/urban 4 | Rural | 27.9% | 16.5% |
| Urban | 66.3% | 82.9% | |
| Prefer not to say | 5.8% | - | |
| Pet ownership 5 | 42.7% | 40% | |
| Variable | p-Value | Odds Ratio (95% Confidence Interval) |
|---|---|---|
| Female gender | 0.259 | 1.174 (0.889–1.552) |
| Age | Baseline < 35 | |
| Age 35–44: 0.057 | 1.500 (0.989–2.280) | |
| Age 45–54: 0.959 | 0.989 (0.654–1.493) | |
| Age 55+: 0.060 | 0.717 (0.506–1.013) | |
| Prefer not to say: 0.061 | 4.590 (1.082–31.240) | |
| Urban location | 0.079 | 0.772 (0.578–1.031) |
| Keeping pets/livestock * | 0.016 * | 0.710 (0.537–0.937) |
| Animal food consumed (1) * | 0.038 * | 0.846 (0.722–0.990) |
| Attitudes to vaccination (2) * | <0.001 * | 0.348 (0.276–0.4351) |
| Attitudes to animal use (3) * | 0.033 * | 0.969 (0.941–0.997) |
| Importance of animal welfare | 0.312 | 0.952 (0.866–1.047) |
| Knowledge of antibiotic resistance (5) * | <0.001 * | 0.757 (0.699–0.818) |
| Agreement with “I am very concerned about the issue of antibiotic resistance but not sure what I can do” | 0.577 | 1.043 (0.899–1.212) |
| Are you afraid that antibiotic resistance might affect you one day?—yes | 0.161 | 1.285 (0.907–1.828) |
| Importance of AMR | 0.889 | 0.992 (0.888–1.108) |
| Antibiotic use in last 12 months * | <0.001 * | 0.557 (0.407–0.760) |
| Experience of AMR in family | 0.681 | 1.076 (0.759–1.520) |
| Perceived risk of antibiotics * | <0.001 * | 1.390 (1.238–1.565) |
| Awareness of AMR | 0.134 | 0.865 (0.715–1.046) |
| Importance of sustainability | 0.354 | 1.056 (0.9411.186) |
| Variable | p-Value | Odds Ratio (95% Confidence Interval) |
|---|---|---|
| Keeping pets/livestock | 0.049 | 0.73 (0.53–1.00) |
| Attitudes to vaccination | <0.001 | 0.43 (0.34–0.55) |
| Knowledge of antibiotic use and resistance | 0.002 | 0.87 (0.79–0.95) |
| Antibiotic use in last 12 months | <0.001 | 0.56 (0.40–0.78) |
| Perceived risk of antibiotics | <0.001 | 1.25 (1.10–1.44) |
| Variable | p-Value | Odds Ratio (95% Confidence Interval) |
|---|---|---|
| Female gender * | 0.036 * | 1.342 (1.020–1.766) |
| Age * | Baseline < 35 | |
| Age 35–44: 0.356 | 0.822 (0.542–1.249) | |
| Age 45–54: 0.531 | 0.878 (0.585–1.321) | |
| Age 55+: 0.004 * | 0.610 (0.435–0.854) | |
| Prefer not to say: 0.125 | 5.238 (0.907–98.860) | |
| Urban location | 0.056 | 1.321 (0.993–1.755) |
| Keeping pets/livestock | 0.493 | 1.100 (0.838–1.445) |
| Animal food consumed (1) | 0.589 | 0.958 (0.819–1.118) |
| Attitudes to vaccination (2) | 0.572 | 0.987 (0.942–1.033) |
| Attitudes to animal use (3) | 0.102 | 0.975 (0.942–1.005) |
| Importance of animal welfare | 0.724 | 1.017 (0.927–1.115) |
| Attitudes to antibiotic use in livestock | 0.191 | 1.022 (0.989-1.005) |
| Knowledge of antibiotic resistance (5) * | 0.002 * | 1.116 (1.040–1.199) |
| Agreement with “I am very concerned about the issue of antibiotic resistance but not sure what I can do” * | <0.001 * | 0.728 (0.632–0.836) |
| Are you afraid that antibiotic resistance might affect you one day?—yes * | 0.012 * | 0.652 (0.466–0.909) |
| Importance of AMR | 0.889 | 0.992 (0.888–1.108) |
| Antibiotic use in last 12 months | 0.360 | 1.148 (0.855–1.544) |
| Experience of AMR in family * | 0.036 * | 0.703 (0.505 –0.978) |
| Perceived risk of antibiotics * | <0.001 * | 0.729 (0.648–0.819) |
| Awareness of AMR * | 0.018 * | 0. 798 (0.662–0.961) |
| Importance of sustainability | 0.986 | 1.001 (0.893–1.121) |
| Variable | p-Value | Odds Ratio (95% Confidence Interval) |
|---|---|---|
| Being female | 0.004 | 1.61 (1.16-2.22) |
| Having had a family member affected by antibiotic failure | 0.019 | 0.67 (0.47–0.93) |
| Knowledge of antibiotic use and resistance | 0.007 | 1.12 (1.03–1.21) |
| Being concerned about AMR, but not knowing what to do about it | 0.002 | 0.78 (0.67–0.91) |
| Perceived risk of antibiotic use in livestock | <0.001 | 0.78 (0.68–0.90) |
| Gender |
|---|
| Age |
| Urban/rural location |
| Keeping pets and/or livestock |
| Animal products consumed (1) |
| Attitudes to vaccination (2) |
| Attitudes to animal use (3) |
| Importance of animal welfare |
| Attitudes to antibiotic use in livestock (4) |
| Knowledge of antibiotic resistance (5) |
| Agreement with “I am very concerned about the issue of antibiotic resistance but not sure what I can do” |
| Fear of being affected personally by AMR |
| Importance of AMR |
| Antibiotic use in last 12 months |
| Experience of antibiotic treatment failure in self or family member |
| Perceived risk of antibiotics |
| Awareness of antibiotic resistance |
| Importance of sustainability |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Adam, K.E.; Bruce, A. Consumer Preferences and Attitudes towards Antibiotic Use in Food Animals. Antibiotics 2023, 12, 1545. https://doi.org/10.3390/antibiotics12101545
Adam KE, Bruce A. Consumer Preferences and Attitudes towards Antibiotic Use in Food Animals. Antibiotics. 2023; 12(10):1545. https://doi.org/10.3390/antibiotics12101545
Chicago/Turabian StyleAdam, Katherine E., and Ann Bruce. 2023. "Consumer Preferences and Attitudes towards Antibiotic Use in Food Animals" Antibiotics 12, no. 10: 1545. https://doi.org/10.3390/antibiotics12101545
APA StyleAdam, K. E., & Bruce, A. (2023). Consumer Preferences and Attitudes towards Antibiotic Use in Food Animals. Antibiotics, 12(10), 1545. https://doi.org/10.3390/antibiotics12101545




