Enhancing the Antifungal Efficacy of Fluconazole with a Diterpene: Abietic Acid as a Promising Adjuvant to Combat Antifungal Resistance in Candida spp.
Abstract
:1. Introduction
2. Results
3. Discussion
- (a)
- Differences in the genetic makeup of Candida strains: Different strains have different genetic backgrounds, which can affect their response to abietic acid. It is possible that the genes involved in the response to abietic acid are differentially expressed in different Candida strains, leading to different outcomes.
- (b)
- Differences in the concentration and duration of abietic acid exposure: some strains may be more sensitive to abietic acid at lower concentrations or for shorter durations, while others require higher concentrations or longer exposure times to see an effect.
- (c)
- Differences in the mechanisms of action of abietic acid: Abietic acid may affect Candida strains through different targets and mechanisms. For example, it may disrupt the fungal cell membrane, interfere with cellular signaling pathways, or cause interference with the enzymes involved in the biochemical process of synthesis of the cell wall. Some Candida strains may be more susceptible to one mechanism of action than others, leading to different outcomes.
- (d)
- Interactions with other compounds: Abietic acid may interact with other compounds in the environment, such as antifungals of clinical relevance, other natural products, or synthetic drugs. These interactions could lead to synergistic or antagonistic effects, affecting the sensitivity of Candida strains.
4. Materials and Methods
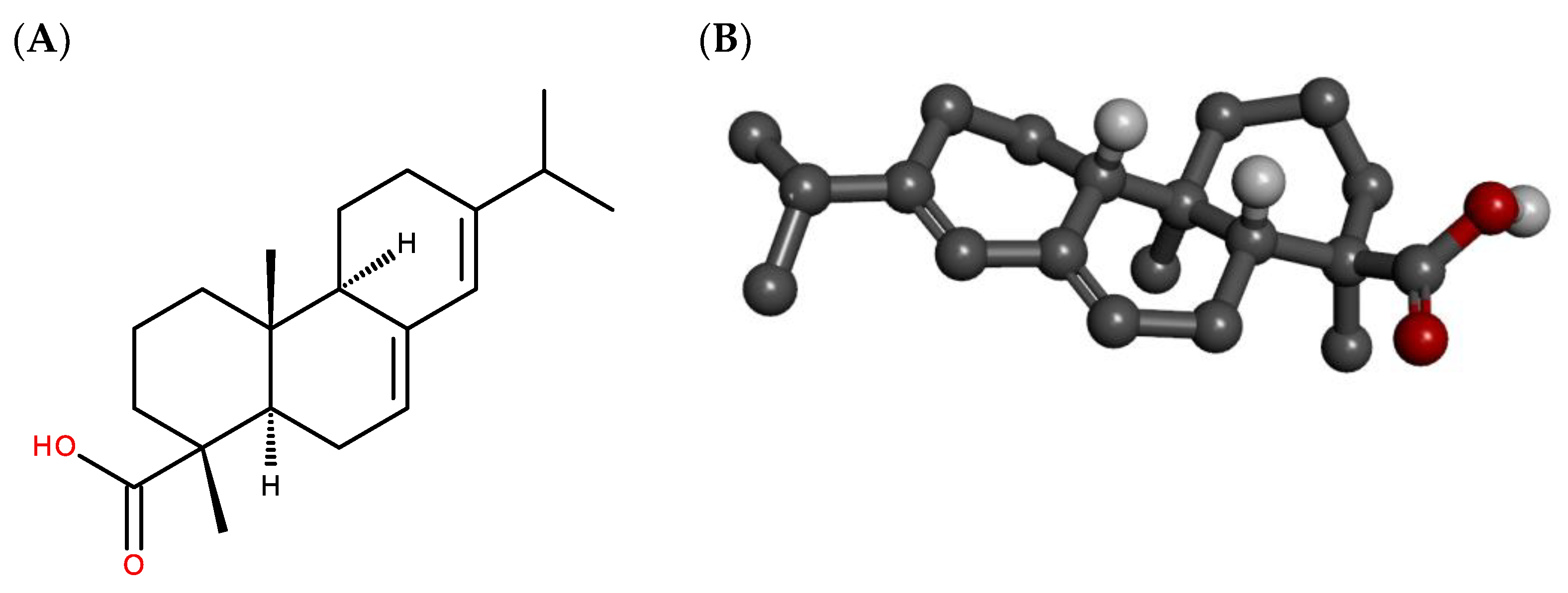
4.1. Drugs and Dilutions
4.2. Microorganisms
4.3. Culture Medium
4.4. Inoculum Preparation
4.5. Minimum Inhibitory Fungicidal Concentration (MFC)
4.6. Cell Viability Curve and Determination of the Half-Maximal Inhibitory Concentration (IC50)
4.7. Evaluation of Antifungal Activity Potentiation in Combination with Fluconazole
4.8. Evaluation of Plasma Membrane Permeabilization
4.9. Molecular Docking Analysis
4.10. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pristov, K.E.; Ghannoum, M.A. Resistance of Candida to Azoles and Echinocandins Worldwide. Clin. Microbiol. Infect. 2019, 25, 792–798. [Google Scholar] [CrossRef]
- Bezerra, C.F.; de Alencar Júnior, J.G.; de Lima Honorato, R.; dos Santos, A.T.L.; Pereira da Silva, J.C.; Gusmão da Silva, T.; Leal, A.L.A.B.; Rocha, J.E.; de Freitas, T.S.; Tavares Vieira, T.A.; et al. Antifungal Activity of Farnesol Incorporated in Liposomes and Associated with Fluconazole. Chem. Phys. Lipids 2020, 233, 104987. [Google Scholar] [CrossRef] [PubMed]
- Ciurea, C.N.; Kosovski, I.B.; Mare, A.D.; Toma, F.; Pintea-Simon, I.A.; Man, A. Candida and Candidiasis—Opportunism Versus Pathogenicity: A Review of the Virulence Traits. Microorganisms 2020, 8, 857. [Google Scholar] [CrossRef] [PubMed]
- Pappas, P.G.; Lionakis, M.S.; Arendrup, M.C.; Ostrosky-Zeichner, L.; Kullberg, B.J. Invasive Candidiasis. Nat. Rev. Dis. Primers 2018, 4, 18026. [Google Scholar] [CrossRef]
- Ricotta, E.E.; Lai, Y.L.; Babiker, A.; Strich, J.R.; Kadri, S.S.; Lionakis, M.S.; Prevots, D.R.; Adjemian, J. Invasive Candidiasis Species Distribution and Trends, United States, 2009–2017. J. Infect. Dis. 2021, 223, 1295–1302. [Google Scholar] [CrossRef]
- Sun, F.-J.; Li, M.; Gu, L.; Wang, M.-L.; Yang, M.-H. Recent Progress on Anti-Candida Natural Products. Chin. J. Nat. Med. 2021, 19, 561–579. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.; Puumala, E.; Robbins, N.; Cowen, L.E. Antifungal Drug Resistance: Molecular Mechanisms in Candida albicans and Beyond. Chem. Rev. 2021, 121, 3390–3411. [Google Scholar] [CrossRef]
- Chen, P.-Y.; Chuang, Y.; Wu, U.; Sun, H.; Wang, J.; Sheng, W.; Chen, Y.; Chang, S. Mechanisms of Azole Resistance and Trailing in Candida tropicalis Bloodstream Isolates. J. Fungi 2021, 7, 612. [Google Scholar] [CrossRef]
- O’Brien, C.E.; Oliveira-Pacheco, J.; Cinnéide, E.; Haase, M.A.B.; Hittinger, C.T.; Rogers, T.R.; Zaragoza, O.; Bond, U.; Butler, G. Population Genomics of the Pathogenic Yeast Candida tropicalis Identifies Hybrid Isolates in Environmental Samples. PLoS Pathog. 2021, 17, e1009138. [Google Scholar] [CrossRef]
- Jamiu, A.T.; Albertyn, J.; Sebolai, O.M.; Pohl, C.H. Update on Candida krusei, a Potential Multidrug-Resistant Pathogen. Med. Mycol. 2021, 59, 14–30. [Google Scholar] [CrossRef]
- Gómez-Gaviria, M.; Mora-Montes, H.M. Current Aspects in the Biology, Pathogeny, and Treatment of Candida krusei, a Neglected Fungal Pathogen. Infect. Drug Resist. 2020, 13, 1673–1689. [Google Scholar] [CrossRef]
- Bohner, F.; Papp, C.; Gácser, A. The Effect of Antifungal Resistance Development on the Virulence of Candida Species. FEMS Yeast Res. 2022, 22, foac019. [Google Scholar] [CrossRef]
- Ben-Ami, R.; Kontoyiannis, D.P. Resistance to Antifungal Drugs. Infect. Dis. Clin. N. Am. 2021, 35, 279–311. [Google Scholar] [CrossRef]
- Caesar, L.K.; Cech, N.B. Synergy and Antagonism in Natural Product Extracts: When 1 + 1 Does Not Equal 2. Nat. Prod. Rep. 2019, 36, 869–888. [Google Scholar] [CrossRef] [PubMed]
- Pemmaraju, S.C.; Pruthi, P.A.; Prasad, R.; Pruthi, V. Candida albicans Biofilm Inhibition by Synergistic Action of Terpenes and Fluconazole. Indian J. Exp. Biol. 2013, 51, 1032–1037. [Google Scholar] [PubMed]
- Bhattacharya, S.; Sae-Tia, S.; Fries, B.C. Candidiasis and Mechanisms of Antifungal Resistance. Antibiotics 2020, 9, 312. [Google Scholar] [CrossRef] [PubMed]
- Heard, S.C.; Wu, G.; Winter, J.M. Antifungal Natural Products. Curr. Opin. Biotechnol. 2021, 69, 232–241. [Google Scholar] [CrossRef] [PubMed]
- Park, J.Y.; Lee, Y.K.; Lee, D.-S.; Yoo, J.-E.; Shin, M.-S.; Yamabe, N.; Kim, S.-N.; Lee, S.; Kim, K.H.; Lee, H.-J.; et al. Abietic Acid Isolated from Pine Resin (Resina Pini) Enhances Angiogenesis in HUVECs and Accelerates Cutaneous Wound Healing in Mice. J. Ethnopharmacol. 2017, 203, 279–287. [Google Scholar] [CrossRef]
- Termentzi, A.; Fokialakis, N.; Leandros Skaltsounis, A. Natural Resins and Bioactive Natural Products Thereof as Potential Anitimicrobial Agents. Curr. Pharm. Des. 2011, 17, 1267–1290. [Google Scholar] [CrossRef]
- Bathe, U.; Tissier, A. Cytochrome P450 Enzymes: A Driving Force of Plant Diterpene Diversity. Phytochemistry 2019, 161, 149–162. [Google Scholar] [CrossRef]
- Simoneit, B.R.T.; Cox, R.E.; Oros, D.R.; Otto, A. Terpenoid Compositions of Resins from Callitris Species (Cupressaceae). Molecules 2018, 23, 3384. [Google Scholar] [CrossRef] [PubMed]
- Olmo, F.; Guardia, J.J.; Marin, C.; Messouri, I.; Rosales, M.J.; Urbanová, K.; Chayboun, I.; Chahboun, R.; Alvarez-Manzaneda, E.J.; Sánchez-Moreno, M. Prospects of an Alternative Treatment against Trypanosoma Cruzi Based on Abietic Acid Derivatives Show Promising Results in Balb/c Mouse Model. Eur. J. Med. Chem. 2015, 89, 863–890. [Google Scholar] [CrossRef] [PubMed]
- Ito, Y.; Ito, T.; Yamashiro, K.; Mineshiba, F.; Hirai, K.; Omori, K.; Yamamoto, T.; Takashiba, S. Antimicrobial and Antibiofilm Effects of Abietic Acid on Cariogenic Streptococcus mutans. Odontology 2020, 108, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Ulusu, N.N.; Ercil, D.; Sakar, M.K.; Tezcan, E.F. Abietic Acid Inhibits Lipoxygenase Activity. Phytother. Res. 2002, 16, 88–90. [Google Scholar] [CrossRef]
- Rosam, K.; Monk, B.C.; Lackner, M. Sterol 14α-Demethylase Ligand-Binding Pocket-Mediated Acquired and Intrinsic Azole Resistance in Fungal Pathogens. J. Fungi 2020, 7, 1. [Google Scholar] [CrossRef]
- Iman, M.; Davood, A. Homology Modeling of Lanosterol 14α-Demethylase of Candida albicans and Insights into Azole Binding. Med. Chem. Res. 2014, 23, 2890–2899. [Google Scholar] [CrossRef]
- Sagatova, A.A.; Keniya, M.V.; Wilson, R.K.; Sabherwal, M.; Tyndall, J.D.A.; Monk, B.C. Triazole Resistance Mediated by Mutations of a Conserved Active Site Tyrosine in Fungal Lanosterol 14α-Demethylase. Sci. Rep. 2016, 6, 26213. [Google Scholar] [CrossRef]
- Singh, G. In Silico Prediction and Pharmacokinetic Studies on Glucosinolates as a Potential Drug and Key Inhibitor Molecule for Lanosterol-14α- Demethylase: A Fungal Membrane Biosynthesis Enzyme. Curr. Drug. Discov. Technol. 2022, 19, 23–32. [Google Scholar] [CrossRef]
- Keniya, M.V.; Sabherwal, M.; Wilson, R.K.; Woods, M.A.; Sagatova, A.A.; Tyndall, J.D.A.; Monk, B.C. Crystal Structures of Full-Length Lanosterol 14α-Demethylases of Prominent Fungal Pathogens Candida albicans and Candida glabrata Provide Tools for Antifungal Discovery. Antimicrob. Agents Chemother. 2018, 62, 10-1128. [Google Scholar] [CrossRef]
- Himejima, M.; Hobson, K.R.; Otsuka, T.; Wood, D.L.; Kubo, I. Antimicrobial Terpenes from Oleoresin of Ponderosa Pine Tree Pinus ponderosa: A Defense Mechanism against Microbial Invasion. J. Chem. Ecol. 1992, 18, 1809–1818. [Google Scholar] [CrossRef]
- Neto, Í.; Faustino, C.M.C.; Rijo, P.; Neto, Í.; Faustino, C.; Rijo, P. Antimicrobial abietane diterpenoids against resistant bacteria and biofilms. In The Battle against Microbial Pathogens: Basic Science, Technological Advances and Educational Programs; Méndez-Vilas, A., Ed.; Formatex Research Center S.L.: Badajoz, Spain, 2015; pp. 15–26. [Google Scholar]
- Gil, F.; Laiolo, J.; Bayona-Pacheco, B.; Cannon, R.D.; Ferreira-Pereira, A.; Carpinella, M.C. Extracts from Argentinian Native Plants Reverse Fluconazole Resistance in Candida Species by Inhibiting the Efflux Transporters Mdr1 and Cdr1. BMC Complement. Med. Ther. 2022, 22, 264. [Google Scholar] [CrossRef] [PubMed]
- Mónico, A.; Nim, S.; Duarte, N.; Rawal, M.K.; Prasad, R.; Di Pietro, A.; Ferreira, M.J.U. Lathyrol and Epoxylathyrol Derivatives: Modulation of Cdr1p and Mdr1p Drug-Efflux Transporters of Candida albicans in Saccharomyces cerevisiae Model. Bioorg. Med. Chem. 2017, 25, 3278–3284. [Google Scholar] [CrossRef] [PubMed]
- Fuentefria, A.M.; Pippi, B.; Dalla Lana, D.F.; Donato, K.K.; de Andrade, S.F. Antifungals Discovery: An Insight into New Strategies to Combat Antifungal Resistance. Lett. Appl. Microbiol. 2018, 66, 2–13. [Google Scholar] [CrossRef]
- Hurt, W.J.; Harrison, T.S.; Molloy, S.F.; Bicanic, T.A. Combination Therapy for HIV-Associated Cryptococcal Meningitis—A Success Story. J. Fungi 2021, 7, 1098. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.; Lee, D.G. A Novel Mechanism of Fluconazole: Fungicidal Activity through Dose-Dependent Apoptotic Responses in Candida albicans. Microbiology 2018, 164, 194–204. [Google Scholar] [CrossRef] [PubMed]
- Lima, V.N.; Oliveira-Tintino, C.D.M.; Santos, E.S.; Morais, L.P.; Tintino, S.R.; Freitas, T.S.; Geraldo, Y.S.; Pereira, R.L.S.; Cruz, R.P.; Menezes, I.R.A.; et al. Antimicrobial and Enhancement of the Antibiotic Activity by Phenolic Compounds: Gallic Acid, Caffeic Acid and Pyrogallol. Microb. Pathog. 2016, 99, 56–61. [Google Scholar] [CrossRef] [PubMed]
- Teodoro, G.R.; Brighenti, F.L.; Delbem, A.C.B.; Delbem, Á.C.B.; Khouri, S.; Gontijo, A.V.L.; Pascoal, A.C.; Salvador, M.J.; Koga-Ito, C.Y. Antifungal Activity of Extracts and Isolated Compounds from Buchenavia tomentosa on Candida albicans and Non-albicans. Future Microbiol. 2015, 10, 917–927. [Google Scholar] [CrossRef]
- Urzúa, A.; Rezende, M.C.; Mascayano, C.; Vásquez, L. A Structure-Activity Study of Antibacterial Diterpenoids. Molecules 2008, 13, 882–891. [Google Scholar] [CrossRef]
- Canturk, Z. Evaluation of Synergistic Anticandidal and Apoptotic Effects of Ferulic Acid and Caspofungin against Candida albicans. J. Food Drug Anal. 2018, 26, 439–443. [Google Scholar] [CrossRef]
- Guo, N.; Ling, G.; Liang, X.; Jin, J.; Fan, J.; Qiu, J.; Song, Y.; Huang, N.; Wu, X.; Wang, X.; et al. In Vitro Synergy of Pseudolaric Acid B and Fluconazole against Clinical Isolates of Candida albicans. Mycoses 2011, 54, e400–e406. [Google Scholar] [CrossRef]
- dos Santos, A.T.L.; Carneiro, J.N.P.; da Cruz, R.P.; Sales, D.L.; Andrade-Pinheiro, J.C.; de Freitas, M.A.; Kerntopf, M.R.; Delmondes, G.d.A.; Ribeiro, P.R.V.; de Brito, E.S.; et al. UPLC-MS-ESI-QTOF Analysis and Antifungal Activity of Aqueous Extracts of Spondias tuberosa. Molecules 2023, 28, 305. [Google Scholar] [CrossRef] [PubMed]
- Sardi, J.d.C.O.; Gullo, F.P.; Freires, I.A.; Pitangui, N.d.S.; Segalla, M.P.; Fusco-Almeida, A.M.; Rosalen, P.L.; Regasini, L.O.; Mendes-Giannini, M.J.S. Synthesis, Antifungal Activity of Caffeic Acid Derivative Esters, and Their Synergism with Fluconazole and Nystatin against Candida spp. Diagn. Microbiol. Infect. Dis. 2016, 86, 387–391. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Lu, C.; Zhao, X.; Wang, D.; Liu, Y.; Sun, S. Antifungal Activity and Potential Mechanism of Asiatic Acid Alone and in Combination with Fluconazole against Candida albicans. Biomed. Pharmacother. 2021, 139, 111568. [Google Scholar] [CrossRef] [PubMed]
- dos Santos, J.F.S.; Rocha, J.E.; Bezerra, C.F.; do Nascimento Silva, M.K.; de Matos, Y.M.L.S.; de Freitas, T.S.; dos Santos, A.T.L.; da Cruz, R.P.; Machado, A.J.T.; Rodrigues, T.H.S.; et al. Chemical Composition, Antifungal Activity and Potential Anti-Virulence Evaluation of the Eugenia uniflora Essential Oil against Candida spp. Food Chem. 2018, 261, 233–239. [Google Scholar] [CrossRef]
- Morais, S.M.; Calixto-Júnior, J.T.; Ribeiro, L.M.; Sousa, H.A.; Silva, A.A.S.; Figueiredo, F.G.; Matias, E.F.F.; Boligon, A.A.; Athayde, M.L.; Morais-Braga, M.F.B.; et al. Phenolic Composition and Antioxidant, Anticholinesterase and Antibiotic-Modulating Antifungal Activities of Guazuma ulmifolia Lam. (Malvaceae) Ethanol Extract. S. Afr. J. Bot. 2017, 110, 251–257. [Google Scholar] [CrossRef]
- Rodrigues, F.C.; dos Santos, A.T.L.; Machado, A.J.T.; Bezerra, C.F.; de Freitas, T.S.; Coutinho, H.D.M.; Morais-Braga, M.F.B.; Bezerra, J.W.A.; Duarte, A.E.; Kamdem, J.P.; et al. Chemical Composition and Anti-Candida Potencial of the Extracts of Tarenaya spinosa (Jacq.) Raf. (Cleomaceae). Comp. Immunol. Microbiol. Infect. Dis. 2019, 64, 14–19. [Google Scholar] [CrossRef]
- CLSI. Performance Standards for Antifungal Susceptibility Testing of Yeasts, 2nd ed.; CLSI supplement M60; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2020; ISBN 9781684400829. [Google Scholar]
- Humam, S.H.; Dheeb, B.I.; Hamad, T.A. Studying the Candida Resistance and Sensitivity for Some Antifungals. J. Biotechnol. Res. Cent. 2019, 13, 26–34. [Google Scholar]
- Monk, B.C.; Sagatova, A.A.; Hosseini, P.; Ruma, Y.N.; Wilson, R.K.; Keniya, M.V. Fungal Lanosterol 14α-Demethylase: A Target for next-Generation Antifungal Design. Biochim. Biophys. Acta Proteins Proteom. 2020, 1868, 140206. [Google Scholar] [CrossRef]
- Sagatova, A.A.; Keniya, M.V.; Wilson, R.K.; Monk, B.C.; Tyndall, J.D.A. Structural Insights into Binding of the Antifungal Drug Fluconazole to Saccharomyces cerevisiae Lanosterol 14α-Demethylase. Antimicrob. Agents Chemother. 2015, 59, 4982–4989. [Google Scholar] [CrossRef]
- Sanati, H.; Belanger, P.; Fratti, R.; Ghannoum, M. A New Triazole, Voriconazole (UK-109,496), Blocks Sterol Biosynthesis in Candida albicans and Candida krusei. Antimicrob. Agents Chemother. 1997, 41, 2492–2496. [Google Scholar] [CrossRef]
- Gerphagnon, M.; Latour, D.; Colombet, J.; Sime-Ngando, T. A Double Staining Method Using SYTOX Green and Calcofluor White for Studying Fungal Parasites of Phytoplankton. Appl. Environ. Microbiol. 2013, 79, 3943–3951. [Google Scholar] [CrossRef] [PubMed]
- Roth, B.L.; Poot, M.; Yue, S.T.; Millard, P.J. Bacterial Viability and Antibiotic Susceptibility Testing with SYTOX Green Nucleic Acid Stain. Appl. Environ. Microbiol. 1997, 63, 2421–2431. [Google Scholar] [CrossRef] [PubMed]
- Thevissen, K.; Terras, F.R.G.; Broekaert, W.F. Permeabilization of Fungal Membranes by Plant Defensins Inhibits Fungal Growth. Appl. Environ. Microbiol. 1999, 65, 5451–5458. [Google Scholar] [CrossRef] [PubMed]
- Lebaron, P.; Catala, P.; Parthuisot, N. Effectiveness of SYTOX Green Stain for Bacterial Viability Assessment. Appl. Environ. Microbiol. 1998, 64, 2697–2700. [Google Scholar] [CrossRef]
- Cavassin, F.B.; Baú-Carneiro, J.L.; Vilas-Boas, R.R.; Queiroz-Telles, F. Sixty Years of Amphotericin B: An Overview of the Main Antifungal Agent Used to Treat Invasive Fungal Infections. Infect. Dis. Ther. 2021, 10, 115–147. [Google Scholar] [CrossRef]
- Escribano, P.; Guinea, J. Fluconazole-Resistant Candida parapsilosis: A New Emerging Threat in the Fungi Arena. Front. Fungal Biol. 2022, 3, 1010782. [Google Scholar] [CrossRef]
- Mukhopadhyay, K.; Prasad, T.; Saini, P.; Pucadyil, T.J.; Chattopadhyay, A.; Prasad, R. Membrane Sphingolipid-Ergosterol Interactions Are Important Determinants of Multidrug Resistance in Candida albicans. Antimicrob. Agents Chemother. 2004, 48, 1778–1787. [Google Scholar] [CrossRef]
- Fonseca, V.J.A.; Braga, A.L.; de Almeida, R.S.; da Silva, T.G.; da Silva, J.C.P.; de Lima, L.F.; dos Santos, M.H.C.; dos Santos Silva, R.R.; Teixeira, C.S.; Coutinho, H.D.M.; et al. Lectins ConA and ConM Extracted from Canavalia ensiformis (L.) DC and Canavalia rosea (Sw.) DC Inhibit Planktonic Candida albicans and Candida tropicalis. Arch. Microbiol. 2022, 204, 346. [Google Scholar] [CrossRef]
- Ernst, E.J.; Klepser, M.E.; Ernst, M.E.; Messer, S.A.; Pfaller, M.A. In Vitro Pharmacodynamic Characteristics of Flucytosine Determined by Time-Kill Methods. Diagn. Microbiol. Infect. Dis. 1999, 36, 101–105. [Google Scholar] [CrossRef]
- Arikan, S. Current Status of Antifungal Susceptibility Testing Methods. Med. Mycol. 2007, 45, 569–587. [Google Scholar] [CrossRef]
- Morais-Braga, M.F.B.; Sales, D.L.; Carneiro, J.N.P.; Machado, A.J.T.; dos Santos, A.T.L.; de Freitas, M.A.; Martins, G.M.d.A.B.; Leite, N.F.; de Matos, Y.M.L.S.; Tintino, S.R.; et al. Psidium guajava L. and Psidium brownianum Mart Ex DC.: Chemical Composition and Anti-Candida Effect in Association with Fluconazole. Microb. Pathog. 2016, 95, 200–207. [Google Scholar] [CrossRef] [PubMed]
- Javadpour, M.M.; Juban, M.M.; Lo, W.-C.J.; Bishop, S.M.; Alberty, J.B.; Cowell, S.M.; Becker, C.L.; McLaughlin, M.L. De Novo Antimicrobial Peptides with Low Mammalian Cell Toxicity. J. Med. Chem. 1996, 39, 3107–3113. [Google Scholar] [CrossRef]
- Coutinho, H.D.M.; Costa, J.G.M.; Lima, E.O.; Falcão-Silva, V.S.; Siqueira, J.P. Enhancement of the Antibiotic Activity against a Multiresistant Escherichia coli by Mentha arvensis L. and Chlorpromazine. Chemotherapy 2008, 54, 328–330. [Google Scholar] [CrossRef] [PubMed]
- Morais-Braga, M.F.B.; Carneiro, J.N.P.; Machado, A.J.T.; dos Santos, A.T.L.; Sales, D.L.; Lima, L.F.; Figueredo, F.G.; Coutinho, H.D.M. Psidium guajava L., from Ethnobiology to Scientific Evaluation: Elucidating Bioactivity against Pathogenic Microorganisms. J. Ethnopharmacol. 2016, 194, 1140–1152. [Google Scholar] [CrossRef] [PubMed]
- Cantón, E.; Espinel-Ingroff, A.; Pemán, J. Trends in Antifungal Susceptibility Testing Using CLSI Reference and Commercial Methods. Expert Rev. Anti Infect. Ther. 2009, 7, 107–119. [Google Scholar] [CrossRef]
- Andrade, J.C.; Dos Santos, A.T.L.; Da Silva, A.R.P.; Freitas, M.A.; Afzal, M.I.; Gonçalo, M.I.P.; Fonseca, V.J.A.; Costa, M.d.S.; Carneiro, J.N.P.; Sousa, E.O.; et al. Phytochemical Characterization of the Ziziphus joazeiro Mart. Metabolites by UPLC-QTOF and Antifungal Activity Evaluation. Cell Mol. Biol. 2020, 66, 127–132. [Google Scholar] [CrossRef]
- Mello, E.O.; Ribeiro, S.F.F.; Carvalho, A.O.; Santos, I.S.; Da Cunha, M.; Santa-Catarina, C.; Gomes, V.M. Antifungal Activity of PvD1 Defensin Involves Plasma Membrane Permeabilization, Inhibition of Medium Acidification, and Induction of ROS in Fungi Cells. Curr. Microbiol. 2011, 62, 1209–1217. [Google Scholar] [CrossRef]




| Substance (IC50 μg/mL) | C. albicans | C. krusei | C. tropicalis |
|---|---|---|---|
| Abietic acid | 1621 * | 1748 * | 2189 * |
| Fluconazole | 1449.85 * | 90.14 | 263.2 |
| Abietic acid + Fluconazole | 37.15 | 147.91 | 12.58 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Lima Silva, M.G.; de Lima, L.F.; Alencar Fonseca, V.J.; Santos da Silva, L.Y.; Calixto Donelardy, A.C.; de Almeida, R.S.; de Morais Oliveira-Tintino, C.D.; Pereira Bezerra Martins, A.O.B.; Ribeiro-Filho, J.; Bezerra Morais-Braga, M.F.; et al. Enhancing the Antifungal Efficacy of Fluconazole with a Diterpene: Abietic Acid as a Promising Adjuvant to Combat Antifungal Resistance in Candida spp. Antibiotics 2023, 12, 1565. https://doi.org/10.3390/antibiotics12111565
de Lima Silva MG, de Lima LF, Alencar Fonseca VJ, Santos da Silva LY, Calixto Donelardy AC, de Almeida RS, de Morais Oliveira-Tintino CD, Pereira Bezerra Martins AOB, Ribeiro-Filho J, Bezerra Morais-Braga MF, et al. Enhancing the Antifungal Efficacy of Fluconazole with a Diterpene: Abietic Acid as a Promising Adjuvant to Combat Antifungal Resistance in Candida spp. Antibiotics. 2023; 12(11):1565. https://doi.org/10.3390/antibiotics12111565
Chicago/Turabian Stylede Lima Silva, Maria Gabriely, Luciene Ferreira de Lima, Victor Juno Alencar Fonseca, Lucas Yure Santos da Silva, Ana Cecília Calixto Donelardy, Ray Silva de Almeida, Cícera Datiane de Morais Oliveira-Tintino, Anita Oliveira Brito Pereira Bezerra Martins, Jaime Ribeiro-Filho, Maria Flaviana Bezerra Morais-Braga, and et al. 2023. "Enhancing the Antifungal Efficacy of Fluconazole with a Diterpene: Abietic Acid as a Promising Adjuvant to Combat Antifungal Resistance in Candida spp." Antibiotics 12, no. 11: 1565. https://doi.org/10.3390/antibiotics12111565







