Abstract
Ventilator-associated pneumonia (VAP) remains a common risk in mechanically ventilated patients. Different care bundles have been proposed to succeed VAP reduction. We aimed to identify the combined interventions that have been used to by ICUs worldwide from the implementation of “Institute for Healthcare Improvement Ventilator Bundle”, i.e., from December 2004. A search was performed on the PubMed, Scopus and Science Direct databases. Finally, 38 studies met our inclusion criteria. The most common interventions monitored in the care bundles were sedation and weaning protocols, semi-recumbent positioning, oral and hand hygiene, peptic ulcer disease and deep venus thrombosis prophylaxis, subglottic suctioning, and cuff pressure control. Head-of-bed elevation was implemented by almost all studies, followed by oral hygiene, which was the second extensively used intervention. Four studies indicated a low VAP reduction, while 22 studies found an over 36% VAP decline, and in ten of them, the decrease was over 65%. Four of these studies indicated zero or nearly zero after intervention VAP rates. The studies with the highest VAP reduction adopted the “IHI Ventilator Bundle” combined with adequate endotracheal tube cuff pressure and subglottic suctioning. Multifaced techniques can lead to VAP reduction at a great extent. Multidisciplinary measures combined with long-lasting education programs and measurement of bundle’s compliance should be the gold standard combination.
1. Introduction
Ventilator-associated pneumonia (VAP) is one of the main types of infection in critically ill mechanically ventilated patients, leading to increased mortality, morbidity, hospital stay, economic and psychological costs for patients and their families [1,2,3,4]. During the last two decades, many guidelines have been proposed to reduce the incidence of VAP. It has been scientifically proven that interventions must be combined in order to be useful [5,6,7]. Bundle is a set of individual components, combined to make a set of quality indicators for a specific system, procedure, or treatment [8]. These interventions must be all implemented together to achieve significantly better results [9].
In 1983, the CDC published the guidelines for the prevention of nosocomial pneumonia, which were specialized for VAP in 2003 [9]. In December 2004, the Institute for Healthcare Improvement (IHI), during the promotion of the “100,000 Lives Campaign”, inserted the “IHI Ventilator Bundle”, consisting of four elements: (1) elevation of the head of bed (HOB) to 30°–45°; (2) daily “sedation vacation” and assessment of readiness to extubate; (3) peptic ulcer disease (PUD) prophylaxis and (4) deep venus thrombosis (DVT) prophylaxis [9]. In 2010, IHI added a fifth intervention: (5) daily oral care with chlorhexidine. In 2016, the Intensive Care Society proposed a bundle called “Recommended bundle of Interventions for the prevention of VAP”, including elevation of head of bed, daily sedation vacation and assessment of readiness to extubate, use of subglottic secretion drainage, avoidance of scheduled ventilator circuit changes, oral hygiene without chlorhexidine and PUD prophylaxis (only for high-risk patients), without mentioning DVT prophylaxis. Next year, the European Respiratory Society, in collaboration with the European Society of Intensive Care Medicine, the European Society of Clinical Microbiology and Infectious Diseases and the American Latin Thoracic Association published the “International guidelines for the management of VAP”, introducing the use of Selective Digestive and Oropharyngeal Decontamination and proposing Oral Decontamination without chlorhexidine. Most of the ICUs worldwide adopted the “IHI Ventilator Bundle”, adapting it to their own needs. As a result, there has been a variation in the included interventions of VAP bundles among ICUs and until now there is no common bundle which can be agreed to be implemented by the communities worldwide [10].
In the last two decades, a major problem has been the increasing rates of occurrence of community-associated methicillin resistant Staphylococcus aureus (CA-MRSA) and hospital-associated MRSA (HA-MRSA). Apart from that, the communities have faced several viral outbreaks, such as SARS-1, SARS-2, and MERS. All the above severe respiratory syndromes and population aging have led to increased rates of ventilated patients [11]. As VAP is one of the most common preventable lung infections in critically ill intubated patients, it is imperative to determine the most efficient preventive measures for VAP reduction. When there is such heterogeneity in ventilator bundles, the question is which ventilator bundle may be more effective?
A great number of studies examined the effectiveness of the different combinations of interventions for VAP prevention. Several reviews have summarized the findings of those studies [11,12,13,14]. A previous systematic review [11] synthesized all the VAP bundles; however, it was published seven years ago, and several studies have been published since then. Moreover, the most recent review was published in 2022, but its main purpose was to summarize the strategies for improvement of care bundle compliance [14]. Therefore, the aim of our systematic review was to present all the multidimensional interventions used in ICUs, from the introduction of the “IHI Ventilator Bundle”, i.e., from December 2004, which is chronologically a point of intersection, as most of the ICUs started to adopt the “IHI Ventilator Bundle”, either alone or combined with other interventions in order to prevent VAP.
2. Materials and Methods
2.1. Data Sources and Strategies
A systematic literature review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines [15]. A comprehensive search was performed on the PubMed, Scopus, and Science Direct databases. We used the following strategy: “ventilator-associated pneumonia” AND “care bundles” AND ”intensive care units” AND ”prevention”. Databases were searched from January 2005 to 23 October 2022. The selected period was intended because in December 2004, the IHI introduced the “IHI Ventilator Bundle”. This systematic review has been registered on PROSPERO registry (ID: CRD42022384828).
2.2. Selection and Eligibility Criteria
Three independent authors were responsible for removing the duplicates, screening the title and abstract, and analyzing the full content of the studies in accordance with the inclusion criteria. Two independent authors selected the included studies and another independent author resolved possible disagreements. To be included in our systematic review, studies had to (a) be published in the English language; (b) be pre–post observational studies; (c) include adult critically ill patients, intubated at least 48 h, admitted to all kinds of adult ICUs; (d) evaluate the implementation of care bundles in VAP prevention by thoroughly presenting all the combined interventions and calculating the pre and post intervention VAP rate; (e) compare with the individual intervention’s implementation for VAP prevention; and (f) be published after the implementation of “IHI Ventilator Bundle”. Additionally, we excluded protocols, conference papers, abstracts, posters, and letters to editors and editorials.
2.3. Data Extraction and Risk of Bias Assessment
For each study, the main characteristics were extracted: authors, country, data collection period, study setting, sample size, age of patients, measures, implementation of an educational program, and main findings. The appraisal of quality of the included studies was performed by using the Risk of Bias in Non-randomized Studies of Interventions (ROBINS-I) [16]. The checklist consisted of seven domains of bias: confounding, participants’ selection, interventions’ classification, deviation from intended interventions, missing data, outcomes’ measurement, and reporting biases. After completing the checklist, all studies were classified as low risk, moderate risk, serious risk, critical risk, or “no information”.
3. Results
3.1. Identification and Selection of Studies
The study selection process is demonstrated in Figure 1. After an initial database search, a total of 3984 studies were identified. After title, abstract, and full content screening, 38 studies were finally included in the review.
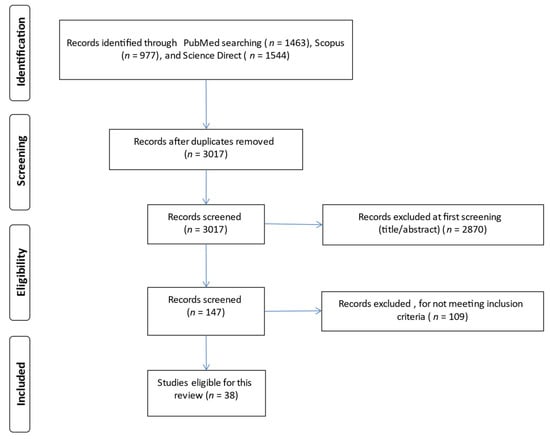
Figure 1.
Flow diagram according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis.
3.2. Characteristics of the Studies Included in This Review
Finally, 38 studies were included in our review. The main characteristics of the studies are presented in Table 1. Fifteen studies took place in Asia, ten in Europe, six in South America, five in North America, one in Australia, and one in Africa. The data collection period ranged from October 2003 [17] to February 2021 [18]. Two studies [5,19] were conducted in Saudi Arabia, at the period of MERS outburst and one study [18] was carried out in Egypt during the coronavirus pandemic. The total sample size ranged from 43 intubated patients [20] to 171,237 intubated patients [21]. All the studies, due to the inclusion criteria, had a pre- and post-intervention observational study design. The studied populations were critically ill ventilated patients admitted to general, medical, surgical, neurosurgical, trauma, and cardiovascular ICUs. Most of the included studies were performed in general ICUs and fifteen of them were multicenter.

Table 1.
Main characteristics of the reviewed studies (n = 38).
3.3. Risk of Bias Assessment
The risk of bias assessment of the reviewed studies is demonstrated in Supplementary Table S1. The risk of bias was low in seven studies [2,5,22,23,24,25,26], serious and critical in 11 studies [3,6,7,17,19,27,28,29,30,31] and moderate in the remaining studies. The most common bias in the pre-post observational studies was the bias due to deviations from intended interventions.
3.4. Ventilator-Associated Care Bundles—Patients’ Outcomes
All of the studies used multifaceted strategies to prevent VAP, as it was one of the inclusion criteria. The number of the included ventilator bundle elements varied from four to thirteen and is shown in Table 2. Head-of-Bed elevation, with a range of 30° to 45°, was implemented by all the reviewed studies, except one [32]. The second most widely used intervention was oral hygiene using chlorhexidine 0.12%. Only one study [3] used sodium bicarbonate and another one [33] sponges and mouthwashes, albeit without a particular change in VAP reduction. Six studies did not adopt the measure of oral care [3,17,18,29,30,32]. Nine studies adopted the IHI Ventilator Bundle [5,6,19,20,23,33,34,35,36]. In two studies, one additional preventive measure was selective oropharyngeal decontamination by using colistin, tobramycin, and nystatin, three times daily, with remarkable VAP reduction rates [25,37].

Table 2.
Preventive VAP measures monitored in revised studies.
Patients’ outcomes are shown in Table 3. Thirty-six of the included studies indicated a reduction in VAP incidence. VAP reduction rates ranged from 13% [2] to 100% [23,36]. Only four studies showed low VAP reduction [2,38,39,40]. The majority of the studies showed a reduction of 36–64% and twelve of them a reduction over 65% [5,6,19,20,23,24,25,27,29,30,36,41]. None of the studies that found low rates of VAP reduction, used the “IHI Ventilator Bundle” and more specifically, all of them did not adopt the PUD and DVT prophylaxis, with three of them adopting the rest measures of the “IHI Ventilator Bundle” (daily sedation vacation, daily assessment of readiness for extubation, head-of-bed elevation and oral care with chlorhexidine). Fourteen studies [2,5,17,18,19,20,21,22,25,35,38,40,42,43] included subglottic suctioning in their bundles, with four of them [5,19,20,25] to achieve more than 65% VAP reduction.

Table 3.
Patient outcomes in each study.
In nine studies [7,17,19,21,23,24,26,30,42], statistical significance was not mentioned, and in four studies [2,32,38,43], the results were not statistically significant, while 24 studies reported a statistically significant reduction. One single center study [43] showed that there were no significant differences in after-intervention VAP and early onset VAP rates but only in late onset VAP rates. In our systematic review, p-values of less than 0.05 were considered significant.
The studies with the highest rate of reduction [5,19,25] implemented the “IHI Ventilator Bundle” combined with adequate ETT cuff pressure at 20–30 cm H2O and subglottic suctioning. Moreover, the study of Gallagher et al. (2012) [36] indicated zero after intervention VAP rate, giving great importance not only to the adoption of “IHI Ventilator Bundle” but also to hand washing and condensate removal. Another study with zero after intervention VAP rate was the study of Chen et al. (2014) [23], where “IHI Ventilator Bundle” with adequate ETT cuff pressure were used as preventive measures.
3.5. Educational Program
We identified thirty-three studies that adopted an education program, as demonstrated in Supplementary Table S2. Education program included self-learning packets, presentations, discussions, knowledge questionnaires, posters, checklists, videos, reminder signs in patients’ rooms, nursing and medical champions, stimulation scenarios and feedback meetings. Thirty-two studies measured the compliance to ventilator bundles and/or education program, and in all of them there was a significant increase in VAP bundle adherence after the education program.
4. Discussion
Our systematic review demonstrated the variety of interventions included in ventilator care bundles and their implementation in VAP decrease in adult ICUs. Thirty-eight studies met our inclusion criteria and we found that the combined measures can prevent VAP toa greater extent. Moreover, our review showed that the number of intervention strategies varied widely in the included studies. Most of the studies examined whether ventilator bundle’s compliance could be increased through health workers’ training.
VAP is one of the main healthcare-associated infections in intubated critically ill patients. VAP is associated with an exceeded duration of mechanical ventilation. The most common microorganisms responsible for VAP are pseudomonas aeruginosa, escherichiacoli, klebsiella pneumoniae and the Acinetobacter species from Gram-negative microorganisms and staphylococcus aureus from Gram-positive microorganisms. VAP diagnostic criteria differ among ICUs but usually require factors such as fever, leukocytosis, progressive infiltrate on chest X-ray, positive cultures from respiratory secretions and reduction in gas exchange [1,9].
During the last decades, there has been a great scientific concern about finding the best strategies to prevent VAP and ventilator-associated events [1]. Worldwide, scientists’ aim to decrease VAP incidence in order: first, to improve ventilated patients’ outcomes, and thereafter to decrease mortality, hospital length of stay and healthcare expenditures. VAP diagnostic criteria, methods of respiratory sampling, interventions in VAP bundles and study designs varies, at a great extent, among the ICUs worldwide [24]. Nevertheless, VAP care bundles combined with a focused education program, which could lead to increased compliance, have proved their efficacy in VAP reduction [6].
A multimodal approach for VAP prevention includes functional, mechanical, and pharmacological measures [21]. The most important intervention for preventing VAP, is avoiding intubation, by using noninvasive positive pressure ventilation whenever possible [1]. By the review of the existing studies, the most frequent proposed interventions, when the patient should be intubated, were sedation and weaning protocols, semi-recumbent positioning, oral and hand hygiene, PUD and DVT prophylaxis, subglottic suctioning, and cuff pressure control. However, interventions as, avoidance of nasogastric tubes, nasotracheal intubation, accidental extubation and gastric overdistension, aseptic suctioning technique and adherence to recommended frequency of equipment change were monitored in the minority of the included studies. Two studies used as an additional preventive measure Selective Oropharyngeal Decontamination (SOD) [25,37]. The care bundle without SOD was associated with a decrease of 42% in VAP rates, while with the implementation of SOD there was a further decrease of 70% in VAP rates [25].
A semi-recumbent position was established with the introduction of “IHI Ventilator Bundle”, though it was proposed much earlier in studies conducted from 1992 to 1999 to test its contribution in aspiration prevention [9]. The implementation of this measure by almost all studies shows the acceptance and the recognition of its importance in VAP treatment. In our systematic review, most of the studies involved oral hygiene in their bundles. Oral care remains an important tool for dental plaque removal and the promotion of a normal microbial community inside the oral cavity, thus preventing the growth of microorganisms in the trachea and the creation of VAP [44,45,46,47]. Fourteen studies aimed to figure out the benefits of subglottic secretion drainage as the secretions concentrated between the vocal cords and the ETT may cause VAP because of the potential growth of pathogens. These studies showed that subglottic suctioning seem to be a useful preventive measure.
A notable result of our study is that ten studies did not control the daily readiness for extubating, when the presence of the endotracheal tube is one of the major predisposing factors for VAP development, as pathogens enter the trachea either by micro aspiration around the ETT cuff or by the biofilm formed in the inner side of the ETT. Moreover, only nine of the included studies followed the “IHI VAP preventive Bundle”. All of them, achieved a VAP reduction at least 36%, five of them showed a reduction of over 65% and two of them managed a zero after intervention VAP rate. These results may indicate the important contribution of the IHI VAP preventive Bundle, alone or in combination with other measures, in VAP reduction. It is noteworthy that the revised studies, carried out the last six years, did not use the “IHI Ventilator Bundle” but adopted some of its interventions.
Another thing that was remarkable was that in many studies, hand hygiene was not mentioned to be monitored as an element in the VAP care bundles. We assume that measures such as hand hygiene and aseptic suctioning technique are of the most basic techniques and that they were taken for granted, along with all the other interventions for VAP prevention in the included studies. Another interesting conclusion in some studies [19,23,28,36] was the after intervention zero-VAP rate, which could be due to many factors, such as country health care policy makers, diversity in VAP diagnostic criteria and methods of BAL sampling [48].
Over the past two decades, humanity has faced several viral outbreaks, causing severe respiratory syndromes, such as SARS-1, SARS-2 and MERS, which may have increased the percentage of intubated patients at a local level. According to the inclusion criteria, all the included studies were conducted after December 2004. Taking into consideration the data collection periods of the revised studies, in two studies [5,19] carried out the period of MERS outbreak in Saudi Arabia, the viral load of the study population and the patient outcomes might have been influenced. Furthermore, only one of the included studies [18] has been performed since the beginning of the coronavirus pandemic. In all three studies, the authors did not mention the possibility of any influence in patients’ outcomes. The data collection periods of the remaining studies did not coincide with the above viral outbreaks’ periods.
The study of Alvarez-Lerma et al. (2018) [21] was the largest study, including 181 ICUs and 171,237 patients, demonstrating the effectiveness of implementing a VAP prevention bundle at a national level. The study of Kao et al. (2019) [39] indicated that compliance rates of VAP bundle care and VAP reduction rates differ between the different types of ICUs (medical, surgical, cardiovascular). Three studies [41,49,50] adopted the INICC multidimensional approach, including the following practices: (1) bundle for VAP prevention (2) education (3) outcome surveillance (4) process surveillance (5) feedback on VAP rates and (6) performance feedback of infection control practices.
Finally, most of the included studies, apart from the implementation of care bundles, adopted at the same time a multifaced educational program. Presentations, posters, videos, discussions, stimulating scenarios and feedback meetings were some of the ways that ICU staff was trained. Our systematic review underlined the wide range in VAP reduction. This wide fluctuation may have been affected, to some extent, by either the country’s healthcare system or the extent variety of educational programs and different degree of personnel’s adherence, but at the same time the studies’ results highlighted that multidisciplinary health professionals’ education and frequent monitoring of adherence can lead to better patients’ outcomes.
5. Limitations
There are several limitations in this systematic review. At first, as we searched for relevant studies only in English language, other potential studies written in different languages were not included in our review. Also, we included three databases in our research, and thus additional studies could be found in other databases. In addition, application of vigorous inclusion and exclusion criteria may preclude some studies to be included in our review. Moreover, among the reviewed studies, there was a heterogeneity, to a greater extent, of the study settings. In particular, differences in study quality are indicative of great differences in studies design, since seven studies had a high level of quality, 20 had a moderate level, and 11 a low level. However, we should notice that heterogeneity among studies was not a limitation of our review but an unavoidable effect of the studies design. Therefore, we should consider our results with caution since it is difficult to establish solid conclusions.
6. Conclusions
From our systematic review, it emerged that there is a considerable variation between the VAP care bundles and education programs in ICUs worldwide. This variation leads to discrepancies and does not allow comparability, to a greater extent, between the studies to find the gold standard VAP care bundle. The IHI VAP preventive Bundle seems to be a very useful tool in VAP reduction, combined with adequate ETT cuff pressure and subglottic suctioning, without forgetting the hand hygiene and aseptic suctioning technique. ICUs should adopt basic practices that prevent or decrease VAP rates, and as a result, mortality, duration of mechanical ventilation, length of stay, and healthcare costs. Moreover, the strategies should be multifaceted and supported by a long-term education program by ensuring compliance in the care bundle. These multidisciplinary strategies and education programs should be common in all ICUs. At least in the same country, national or cross-sectional randomized controlled studies need to be carried out in order to be able to compare the measures’ efficacy and find the best combination of preventive interventions.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/antibiotics12020227/s1, Supplementary Table S1: Risk of Bias in Non-randomized Studies of Interventions (ROBINS-I); Supplementary Table S2: Impact of multidisciplinary educational program in the reviewed studies.
Author Contributions
Conceptualization, M.M., T.K., P.G., A.K. and P.M.; methodology, M.M., T.K., P.G. and P.M.; validation, M.M., T.K. and P.G.; investigation, M.M., T.K., P.G., A.K. and P.M.; resources: P.M.; data curation, M.M., T.K. and P.G.; writing-original draft preparation: M.M., T.K., P.G., A.K. and P.M.; writing-review and editing: M.M., T.K., P.G. and P.M.; supervision: P.M.; funding acquisition: P.M. All authors have read and agreed to the published version of the manuscript.
Funding
Special Account for Research Grants of the National and Kapodistrian University of Athens.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors have no conflicts of interest to declare.
References
- Klompas, M.; Branson, R.; Eichenwald, E.C.; Greene, L.R.; Howell, M.D.; Lee, G.; Magill, S.; Maragakis, L.L.; Priebe, G.P.; Speck, K.; et al. Strategies to prevent ventilator-associated pneumonia in acute care hospitals: 2014 Update. Infect. Control. Hosp. Epidemiol. 2014, 35, 133–154. [Google Scholar] [CrossRef] [PubMed]
- Sousa, A.S.; Ferriso, C.; Paira, J.A. Application of a ventilator associated pneumonia prevention guideline and outcomes: A quasi-experimental study. Intensive Crit. Care Nurs. 2019, 51, 50–56. [Google Scholar] [CrossRef]
- Parisi, M.; Gerovasili, V.; Dimopoulos, D.; Kampisiouli, E.; Goga, C.; Perivolioti, E.; Argyropoulou, A.; Routsi, C.; Tsiodras, S.; Nanas, S. Use of Ventilator Bundle and Staff Education to Decrease Ventilator Associated Pneumonia in Intensive Care Patients. Crit. Care Nurse 2016, 36, e1–e7. [Google Scholar] [CrossRef] [PubMed]
- Pileggi, C.; Mascaro, V.; Bianco, A.; Nobile, C.G.; Pavia, M. Ventilator Bundle and Its Effects on Mortality Among ICU Patients: A Meta-Analysis. Crit. Care Med. 2018, 46, 1167–1174. [Google Scholar] [CrossRef] [PubMed]
- Khan, R.; Al-Dorzi, H.M.; Al-Attas, K.; Ahmed, F.W.; Marini, A.M.; Mundekkadan, S.; Balkhy, H.H.; Tarnous, J.; Arabi, Y.M. The impact of implementing multifaceted interventions on the prevention of ventilator-associated pneumonia. Am. J. Infect. Control. 2016, 44, 320–326. [Google Scholar] [CrossRef] [PubMed]
- Lim, K.P.; Kuo, S.W.; Ko, W.J.; Sheng, W.H.; Chang, Y.Y.; Hong, M.C.; Sun, C.C.; Chen, Y.C.; Chang, S.C. Efficacy of ventilator-associated pneumonia care bundle for prevention of ventilator-associated pneumonia in the surgical intensive care units of a medical center. J. Microbiol. Immunol. Infect. 2015, 48, 316–321. [Google Scholar] [CrossRef]
- Moore, K.R. Critical Care Nursing Interventions and Incidence of Ventilator Associated Pneumonia in the Trauma Population 2012, Nursing Theses and Capstone Projects.135. Available online: https://digitalcommons.gardner-webb.edu/cgi/viewcontent.cgi?article=1134&context=nursing_etd (accessed on 1 September 2022).
- Resar, R.; Pronovost, P.; Haraden, C.; Simmond, T.; Rainey, T.; Nolan, T. Using a Bundle Approach to Improve Ventilator Care Processes and Reduce Ventilator Associated Pneumonia. J. Qual. Patient Saf. 2005, 31, 243–248. [Google Scholar] [CrossRef]
- Munro, N.; Ruggiero, M. Ventilator-Associated Pneumonia Bundle. Reconstruction for Best Care. AACN Adv. Crit. Care 2014, 25, 163–175. [Google Scholar] [CrossRef]
- Kandeel, N.; Tantawy, N. Current Nursing Practice for Prevention of Ventilator Associated Pneumonia in ICUs. Life Sci. J. 2012, 9, 966–975. [Google Scholar]
- Chahoud, J.; Semaan, A.; Almoosa, K. Ventilator-associated events prevention, learning lessons from the past: A systematic review. Heart Lung 2015, 44, 251–259. [Google Scholar] [CrossRef]
- Alecrim, R.X.; Taminato, M.; Belasco, A.; Longo, M.C.; Lusahara, D.M.; Fram, D. Strategies for preventing ventilator-associated pneumonia: An integrative review. Rev. Bras. Enferm. 2019, 72, 521–530. [Google Scholar] [CrossRef] [PubMed]
- Kallet, R.H. Ventilator Bundles in Transition: From Prevention of Ventilator Associated Pneumonia to Prevention of Ventilator-Associated Events. Respir. Care 2019, 8, 994–1006. [Google Scholar] [CrossRef] [PubMed]
- Thapa, D.; Liu, T.; Chair, S.Y. Multifaceted interventions are likely to be more effective to increase adherence to the ventilator care bundle: A systematic review of strategies to improve care bundle compliance. Intensive Crit. Care Nurs. 2022, 74, 103310. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. The PRISMA Group Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons: Hoboken, NJ, USA, 2019. [Google Scholar]
- Berenholtz, S.M.; Pham, J.C.; Thompson, D.A.; Needham, D.M.; Lubomski, L.H.; Hyzy, R.C.; Welsh, R.; Cosgrove, S.E.; Sexton, J.B.; Colantuoni, E.; et al. Collaborative Cohort Study of an Intervention to Reduce Ventilator-Associated Pneumonia in the Intensive Care Unit. Infect. Control. Hosp. Epidemiol. 2011, 32, 305–314. [Google Scholar] [CrossRef] [PubMed]
- Shaban, A.M.; El-Mokadem, N.M.; Abdallah, S.E. Effectiveness of Implementing Ventilator Associated Pneumonia Prevention Bundle among Mechanically Ventilated Patients. Int. J. Nov. Res. Healthc. Nurs. 2021, 8, 329–342. [Google Scholar]
- Marini, A.L.; Khan, R.; Mundekkadan, S. Multifaceted bundle interventions shown effective in reducing VAP rates in our multidisciplinary ICUs. BMJ Qual. Improv. Rep. 2016, 5, u205566-w2278. [Google Scholar] [CrossRef]
- Ismail, R.; Zahran, E. The effect of nurses training on ventilator-associated pneumonia (VAP) prevention bundle on VAP incidence rate at a critical care unit. J. Nurs. Educ. Pract. 2015, 5, 42–48. [Google Scholar] [CrossRef]
- AÁlvarez-Lerma, F.; Palomar-Martínez, M.; Sánchez-García, M.; Martínez-Alonso, M.; Álvarez-Rodríguez, J.; Lorente, L.; Arias-Rivera, S.; García, R.; Gordo, F.; Añón, J.M.; et al. Prevention of Ventilator-Associated Pneumonia: The Multimodal Approach of the Spanish ICU “Pneumonia Zero” Program. Crit. Care Med. 2018, 46, 181–188. [Google Scholar] [CrossRef]
- Cengiz, H.O.; Kanan, N. The effectiveness of training given to nurses for reducing ventilator-associated pneumonia in intensive care patients. Dev. Health Sci. 2019, 2, 36–45. [Google Scholar]
- Chen, J.K.; Chen, T.H.; Liu, H.E.; Kao, C.C.; Chen, C.F.; Ou, T.Y.; Tseng, P.C.; Kuo, K.N.; Lee, W.S. Bundle Care for Preventing Ventilator-associated Pneumonia at a Medical Center: A Preliminary Report. J. Exp. Clin. Med. 2014, 6, 157–160. [Google Scholar] [CrossRef]
- Eom, J.S.; Lee, M.S.; Chun, H.K.; Choi, H.J.; Jung, S.Y.; Kim, Y.S.; Yoon, S.J.; Kwak, Y.G.; Oh, G.B.; Jeon, M.H.; et al. The impact of a ventilator bundle on preventing ventilator-associated pneumonia: A multicenter study. Am. J. Infect. Control. 2014, 42, 34–37. [Google Scholar] [CrossRef] [PubMed]
- Landelle, C.; NocquetBooyer, V.; Abbas, M.; Genevois, E.; Abidi, N.; Naimo, S.; Raulais, R.; Bouchoud, L.; Boroli, F.; Terrisse, H.; et al. Impact of a multifaceted prevention program on ventilator-associated pneumonia including selective oropharyngeal decontamination. Intensive Care Med. 2018, 44, 1777–1786. [Google Scholar] [CrossRef] [PubMed]
- Mogyorodi, B.; Dunai, E.; Gal, J.; Ivanyi, Z. Ventilator—Associated pneumonia and the importance of education of ICU nurses on prevention—Preliminary results. Interv. Med. Appl. Sci. 2016, 8, 147–151. [Google Scholar] [CrossRef] [PubMed]
- Fortaleza, C.M.C.B.; Filho, S.P.F.; Silva, M.O.; Queiroz, S.M.; Cavalcante, R.S. Sustained reduction of healthcare-associated infections after the introduction of a bundle for prevention of ventilator-associated pneumonia in medical-surgical intensive care units. Braz. J. Infect. Dis. 2020, 24, 373–379. [Google Scholar] [CrossRef]
- Zeng, W.P.; Su, H.; Chen, C.W.; Cheng, S.M.; Chang, L.F.; Tzeng, W.C.; Tzeng, B.H. Care Bundle for Ventilator-Associated Pneumonia in a Medical Intensive Care Unit in Northern Taiwan. J. Med. Sci. 2015, 35, 68–73. [Google Scholar]
- Al-Tawfiq, J.A.; Abed, M.S. Decreasing ventilator-associated pneumonia in adult intensive care units using the Institute for Healthcare Improvement bundle. Am. J. Infect. Control. 2010, 38, 552–556. [Google Scholar] [CrossRef]
- Bird, D.; Zambuto, A.; O’Donnell, C.; Silva, J.; Korn, C.; Burke, R.; Burke, P.; Agarwal, S. Adherence to Ventilator-Associated Pneumonia Bundle and Incidence of Ventilator-Associated Pneumonia in the Surgical Intensive Care Unit. Achieves Surg. 2010, 145, 465–470. [Google Scholar] [CrossRef]
- Branco, A.; Louvencone, E.M.; Monteiro, A.B.; Fonseca, J.P.; Blatt, C.R.; Caregnato, R.C. Education to prevent ventilator-associated pneumonia in intensive care unit. Rev. Bras. De Enferm. 2020, 73, e20190477. [Google Scholar] [CrossRef]
- Ban, K.O. The effectiveness of an evidence-based nursing program to reduce ventilator-associated pneumonia in a Korean ICU. Intensive Crit. Care Nurs. 2011, 27, 226–232. [Google Scholar] [CrossRef]
- Viana, W.N.; Bragazzi, C.; Couto de Castro, J.E.; Alves, M.B.; Rocco, J.R. Ventilator-associated pneumonia prevention by education and two combined bedside strategies. Int. J. Qual. Health Care 2013, 25, 308–313. [Google Scholar] [CrossRef] [PubMed]
- Alcan, A.O.; Korkmaz, F.D.; Uyar, M. Prevention of ventilator—Associated pneumonia: Use of the care bundle approach. Am. J. Infect. Control. 2016, 44, e173–e176. [Google Scholar] [CrossRef] [PubMed]
- Dosher, W.B.; Loomis, E.C.; Richardson, S.L.; Crowell, J.A.; Waltman, R.D.; Miller, L.D.; Nazim, M.; Khasawneh, F.A. The effect of a Nurse—Led Multidisciplinary Team on Ventilator—Associated Pneumonia Rates. Crit. Care Res. Pract. 2014, 2014, 682621. [Google Scholar] [CrossRef]
- Gallagher, J.A. Implementation of VentilatorAssociated Pneumonia Clinical Guideline (Bundle). J. Nurse Pract. 2012, 8, 377–382. [Google Scholar] [CrossRef]
- Righi, E.; Aggazzotti, G.; Ferrari, E.; Giovanardi, C.; Busani, S.; Rinaldi, L.; Girardis, M. Trends in ventilator-associated pneumonia: Impact of a ventilator care bundle in an Italian tertiary care hospital intensive care unit. Am. J. Infect. Control. 2014, 42, 1312–1316. [Google Scholar] [CrossRef]
- Gatell, M.R.; Roig, M.S.; Vian, O.H.; Santin, E.C.; Duaso, C.T.; Moreno, I.F.; Daunis, J.V. Assessment of a training programme for the prevention of ventilator-associated pneumonia. Br. Assoc. Crit. Care Nurses 2012, 17, 285–292. [Google Scholar] [CrossRef]
- Kao, C.C.; Chiang, H.T.; Chen, C.Y.; Hung, C.T.; Chen, Y.C.; Su, L.H.; Shi, Z.Y.; Liu, J.W.; Liu, C.P.; Chuang, Y.C.; et al. National bundle care program implementation to reduce ventilator-associated pneumonia in intensive care units in Taiwan. J. Microbiol. Immunol. Infect. 2019, 52, 592–597. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Yang, Y.; Zhang, K.; Hai, Y.; Li, H.; Xing, H.; Xu, B.; Bai, H.; Zhao, H.; Bao, H.; et al. Evaluation of the effects of applying the ventricular care bundle (VCB) method for reducing ventilator-associated pneumonia (VAP) in the intensive care unit of a general Chinese tertiary hospital. Ann. Palliat. Med. 2020, 9, 2853–2861. [Google Scholar] [CrossRef]
- Guanche-Garcell, H.; Morales-Perez, C.; Rosenthal, V.D. Effectiveness of a multidimensional approach for the prevention of ventilator-associated pneumonia in an adult intensive care unit in Cuba: Findings of the International Nosocomial Infection Control Consortium (INICC). J. Infect. Public Health 2013, 6, 98–107. [Google Scholar] [CrossRef]
- Micik, S.; Besic, N.; Johnson, N.; Han, M.; Harnlyn, S.; Ball, H. Reducing risk for ventilator associated pneumonia through nursing sensitive interventions. Intensive Crit. Care Nurs. 2013, 29, 261–265. [Google Scholar] [CrossRef]
- Burja, S.; Belec, T.; Bizjak, N.; Mori, J.; Markota, A.; Sinkovic, A. Efficacy of a bundle approach in preventing the incidence of ventilator associated pneumonia (VAP). Bosn. J. Basic Med. Sci. 2018, 18, 105–109. [Google Scholar] [CrossRef] [PubMed]
- Bouadma, L.; Mourvillier, B.; Deiler, V.; Le Corre, B.; Lolom, I.; Regnier, B.; Wolff, M.; Lucet, J.C. A multifaceted program to prevent ventilator—Associated pneumonia: Impact on compliance with preventive measures. Crit. Care Med. 2010, 38, 789–796. [Google Scholar] [CrossRef]
- Michelangelo, H.; Angriman, F.; Pizarro, R.; Bauque, S.; Kecskes, C.; Staneloni, I.; Garcia, D.; Espinola, F.; Mazer, G.; Ferrari, C. Implementation of an experiential learning strategy to reduce the risk of ventilator-associated pneumonia in critically ill adult patients. J. Intensive Care Soc. 2020, 21, 320–326. [Google Scholar] [CrossRef]
- Morris, A.C.; Hay, A.W.; Swann, D.G.; Everingham, K.; McCulloch, C.; McNulty, J.; Brooks, O.; Laurenson, I.F.; Cook, B.; Walsh, T.S. Reducing ventilator-associated pneumonia in intensive care: Impact of implementing a care bundle. Crit. Care Med. 2011, 39, 2218–2224. [Google Scholar] [CrossRef] [PubMed]
- Ochoa-Hein, E.; Choi, S.J.; Gomez-Santillan, J.A.; Oyervides-Alvarado, J.A.; Galindo-Fraga, A.; Rivero-Sigarroa, E.; Hernandez-Gilsoul, T.; Dominguez-Cherit, J.G. Near-zero ventilator-associated pneumonia rates after implementation of a multimodal preventive strategy in a Mexican hospital. Am. J. Infect. Control 2020, 48, 446–447. [Google Scholar] [CrossRef]
- Colombo, S.M.; Palomeque, A.C.; Bassi, G. The zero-VAP sophistry and controversies surrounding prevention of ventilator-associated pneumonia. Intensive Care Med. 2020, 46, 368–371. [Google Scholar] [CrossRef] [PubMed]
- Leblebicioglu, H.; Yalcin, A.N.; Rosenthal, V.D.; Koksal, I.; Sirmatel, F.; Unal, S.; Turgut, H.; Ozdemir, D.; Ersoz, G.; Uzun, C. Effectiveness of a multidimensional approach for prevention of ventilator-associated pneumonia in 11 adult intensive care units from 10 cities of Turkey: Findings of the International Nosocomial Infection Control Consortium (INICC). Infection 2013, 41, 447–456. [Google Scholar] [CrossRef] [PubMed]
- Mehta, Y.; Jaggi, N.; Rosenthal, V.D.; Rodrigues, C.; Todi, S.K.; Saini, N.; Udwadia, F.E.; Karlekar, A.; Kothari, V.; Myatra, S.N.; et al. Effectiveness of a multidimensional approach for prevention of ventilator-associated pneumonia in 21 adult intensive-care units from 10 cities in India: Findings of the International Nosocomial Infection Control Consortium (INICC). Epidemiol. Infect. 2013, 141, 2483–2491. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).