Current and Emerging Inhaled Antibiotics for Chronic Pulmonary Pseudomonas aeruginosa and Staphylococcus aureus Infections in Cystic Fibrosis
Abstract
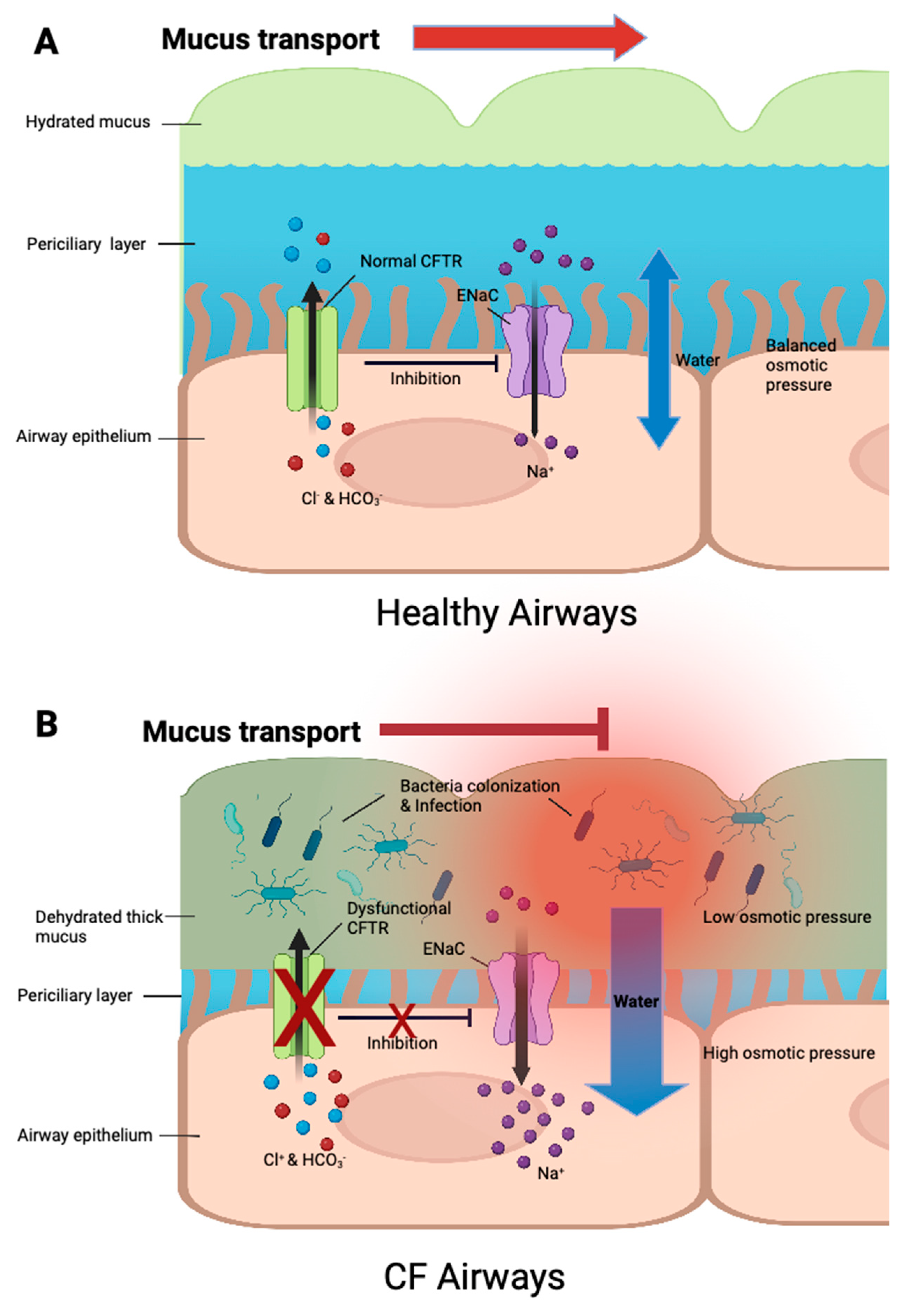
:1. Introduction
2. Major Colonized Pathogens in Cystic Fibrosis and the Adaptation to Chronic Infection
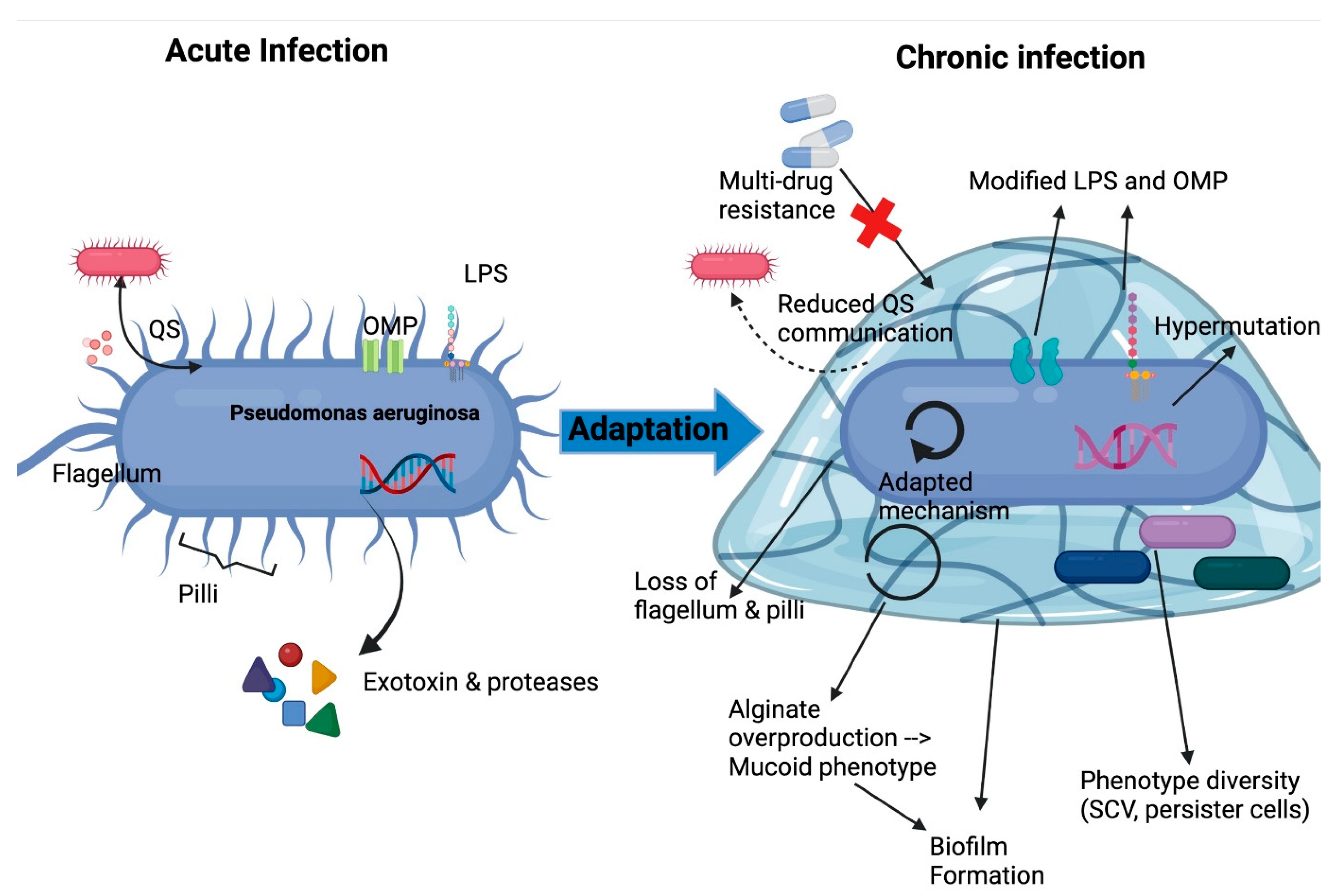
2.1. Pseudomona Aeruginosa
2.1.1. Prevalence
2.1.2. Virulence Factors
2.1.3. Adaptation and Persistence
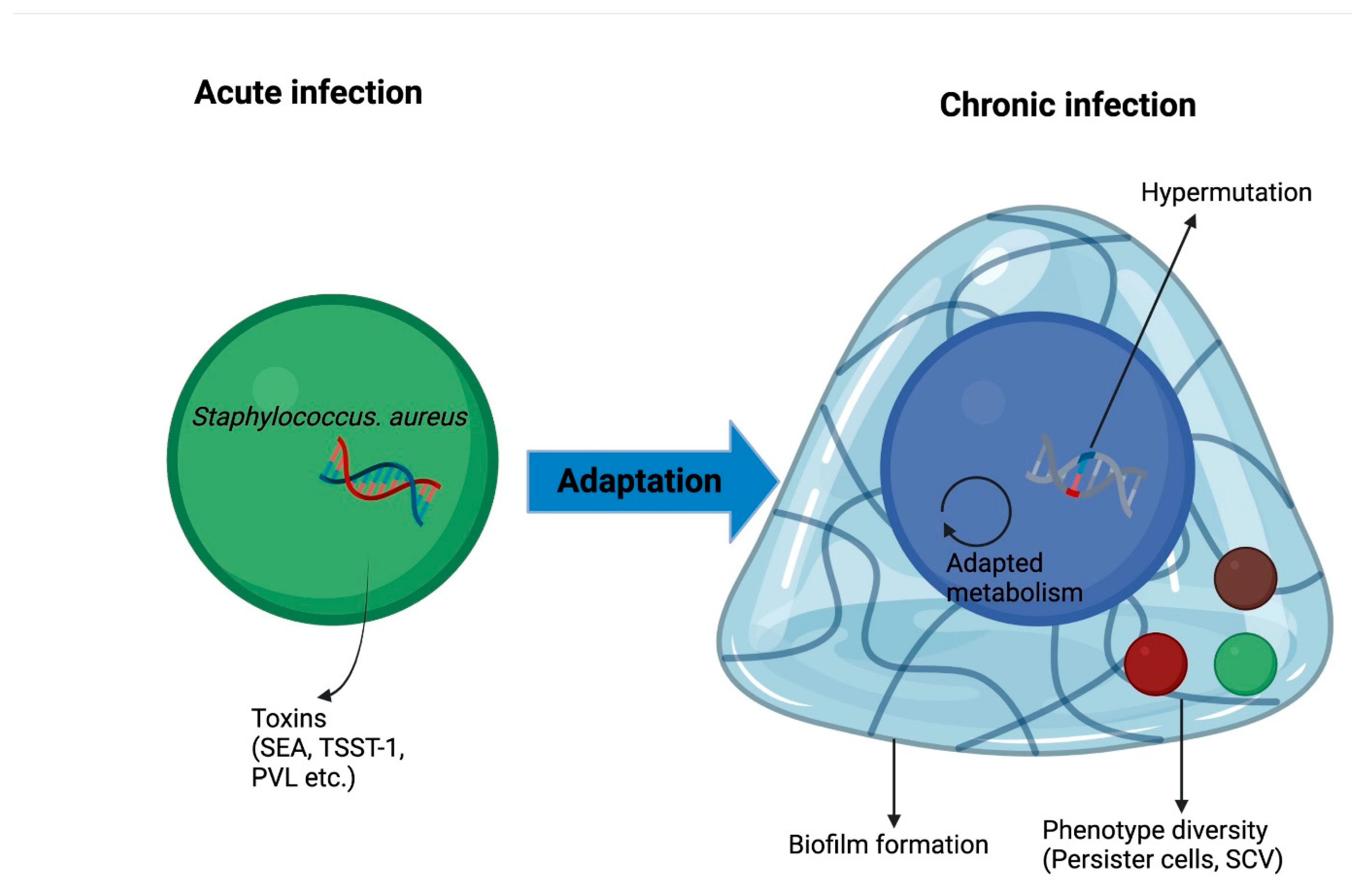
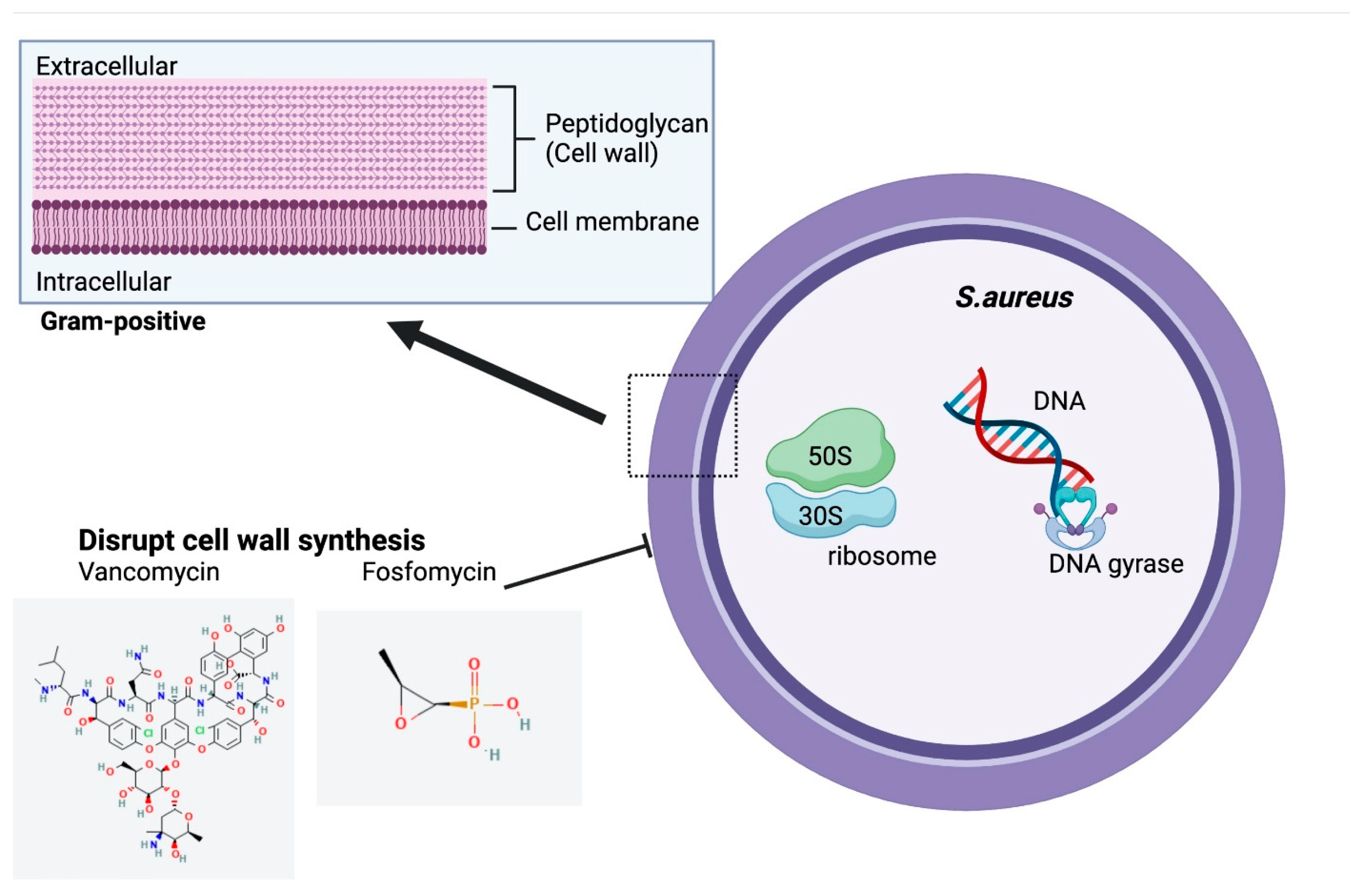
2.2. Staphylococcus aureus
2.2.1. Prevalence
2.2.2. Virulence Factors
2.2.3. Adaptation and Persistence
2.3. Other Bacteria
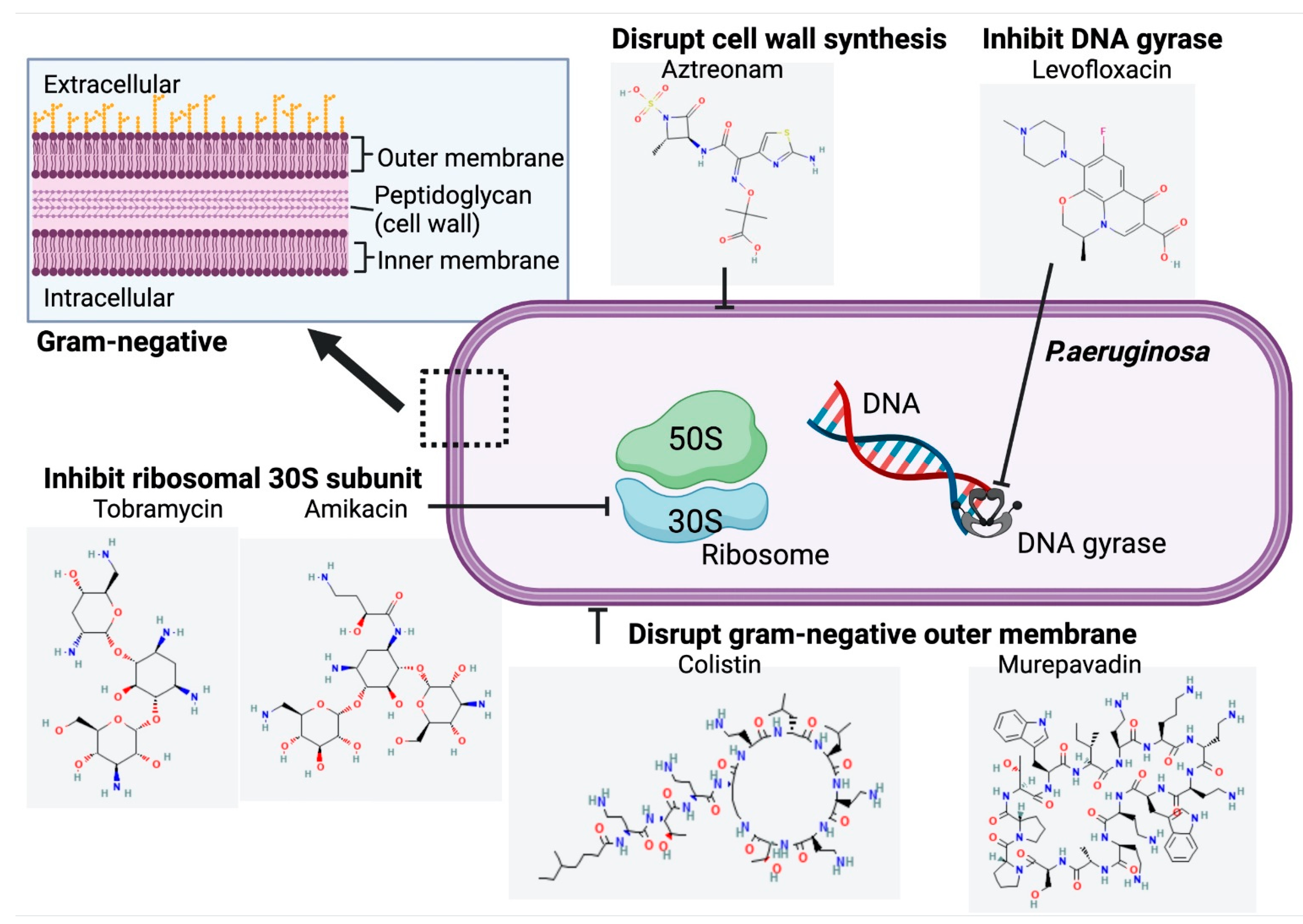
3. Inhaled Antibiotics Treating Chronic P. aeruginosa Pulmonary Infection in Patients with Cystic Fibrosis
3.1. Tobramycin
3.1.1. Mechanism of Action
3.1.2. Efficacy
3.1.3. Safety
3.1.4. Indications
3.2. Aztreonam
3.2.1. Mechanism of Action
3.2.2. Efficacy
3.2.3. Safety
3.2.4. Indications
3.3. Levofloxacin
3.3.1. Mechanism of Action
3.3.2. Efficacy
3.3.3. Safety
3.3.4. Indication
3.4. Colistin
3.4.1. Mechanism of Action
3.4.2. Efficacy
3.4.3. Safety
3.4.4. Indications
3.5. Amikacin Liposome Inhalation Suspension
3.5.1. Mechanism of Action
3.5.2. Efficacy
3.5.3. Safety
3.5.4. Indications
3.6. Murepavadin
3.6.1. Mechanism of Action
3.6.2. Efficacy
3.6.3. Safety
3.6.4. Indications
4. Inhaled Antibiotics Treating Chronic S. aureus Pulmonary Infection in CF Patients
4.1. Vancomycin
4.2. Fosfomycin
5. Selecting the Optimal Inhaled Antibiotic Therapy
Combination Therapy
6. Conclusions and Future Perspectives
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
| ALIS | amikacin liposome inhalation suspension |
| ARDS | acute respiratory distress syndrome |
| CATI | continuous alternating inhaled antibiotic therapy |
| CDPI | colistimethate sodium dry powder for inhalation |
| CF | cystic fibrosis |
| CFFPR | Cystic Fibrosis Foundation Patient Registry |
| CFTR | cystic fibrosis transmembrane conductance regulator |
| CFU | colony-forming unit |
| EMA | European Medicines Agency |
| FTI | fosfomycin and tobramycin for inhalation |
| LIS | levofloxacin inhalation solution |
| LPS | lipopolysaccharides |
| LptD | lipopolysaccharise transport protein D |
| LS | least squares |
| MAC | Mycobacterium. avium complex |
| MDR | multi-drug resistant |
| MIC | minimum inhibitory concentration |
| MIU | million international units |
| MRSA | methicilin-resistant S. aureus |
| MSSA | methicilin-sensitive S. aureus |
| NTM | Nontuberculous Mycobacteria |
| OMP | outer membrane proteins |
| P. aeruginosa | Pseudomonas aeruginosa |
| ppFEV1 | percent predicted forced expiratory volume in 1 s |
| PVL | Panton-Valentine leucocidin |
| QS | quorum sensing |
| S. aureus | Staphylococcus aureus |
| SCV | small colony variants |
| TEAE | treatment emergent adverse events |
| TIP | powder form of TIS |
| TIS | tobramycin inhalation solution |
References
- Turcios, N.L. Cystic fibrosis lung disease: An overview. Respir. Care. 2020, 65, 233–251. [Google Scholar] [CrossRef] [PubMed]
- Chen, Q.; Shen, Y.; Zheng, J. A review of cystic fibrosis: Basic and clinical aspects. Anim. Model. Exp. Med. 2021, 4, 220–232. [Google Scholar] [CrossRef] [PubMed]
- Cystic Fibrosis Foundation. Patient Registry, 2021 Annual Data Report. Available online: https://www.cff.org/sites/default/files/2021-11/Patient-Registry-Annual-Data-Report.pdf (accessed on 5 December 2022).
- Rafeeq, M.M.; Murad, H.A.S. Cystic fibrosis: Current therapeutic targets and future approaches. J. Transl. Med. 2017, 15, 84. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Merjaneh, L.; Hasan, S.; Kasim, N.; Ode, K.L. The role of modulators in cystic fibrosis related diabetes. J. Clin. Transl. Endocrinol. 2022, 27, 100286. [Google Scholar] [CrossRef]
- Boucher, R.C. Muco-obstructive lung diseases. Reply. N. Engl. J. Med. 2019, 381, e20. [Google Scholar] [CrossRef]
- Harwood, K.H.; McQuade, R.M.; Jarnicki, A.; Schneider-Futschik, E.K. Anti-inflammatory influences of cystic fibrosis transmembrane conductance regulator drugs on lung inflammation in cystic fibrosis. Int. J. Mol. Sci. 2021, 22, 7606. [Google Scholar] [CrossRef]
- Schneider, E.K.; Azad, M.A.; Han, M.L.; Tony Zhou, Q.; Wang, J.; Huang, J.X.; Cooper, M.A.; Doi, Y.; Baker, M.A.; Bergen, P.J.; et al. An “unlikely” pair: The antimicrobial synergy of polymyxin b in combination with the cystic fibrosis transmembrane conductance regulator drugs kalydeco and orkambi. ACS Infect. Dis. 2016, 2, 478–488. [Google Scholar] [CrossRef] [Green Version]
- Anderson, S.; Atkins, P.; Backman, P.; Cipolla, D.; Clark, A.; Daviskas, E.; Disse, B.; Entcheva-Dimitrov, P.; Fuller, R.; Gonda, I.; et al. Inhaled medicines: Past, present, and future. Pharmacol. Rev. 2022, 74, 48–118. [Google Scholar] [CrossRef]
- Kidd, T.J.; Ramsay, K.A.; Vidmar, S.; Carlin, J.B.; Bell, S.C.; Wainwright, C.E.; Grimwood, K.; Investigators, A.S. Pseudomonas aeruginosa genotypes acquired by children with cystic fibrosis by age 5-years. J. Cyst. Fibros. 2015, 14, 361–369. [Google Scholar] [CrossRef] [Green Version]
- Lund-Palau, H.; Turnbull, A.R.; Bush, A.; Bardin, E.; Cameron, L.; Soren, O.; Wierre-Gore, N.; Alton, E.W.; Bundy, J.G.; Connett, G.; et al. Pseudomonas aeruginosa infection in cystic fibrosis: Pathophysiological mechanisms and therapeutic approaches. Expert Rev. Respir. Med. 2016, 10, 685–697. [Google Scholar] [CrossRef]
- Brian, P.; O’Sullivan, S.D.F. Cystic fibrosis. Lancet 2009, 373, 1891–1904. [Google Scholar] [CrossRef]
- Cystic Fibrosis Foundation. Cystic Fibrosis Foundation Patient Registry. 2017. Available online: https://www.cff.org/community-posts/2018-06/highlights-2017-cf-foundation-patient-registry (accessed on 16 November 2022).
- Jurado-Martin, I.; Sainz-Mejias, M.; McClean, S. Pseudomonas aeruginosa: An audacious pathogen with an adaptable arsenal of virulence factors. Int. J. Mol. Sci. 2021, 22, 3128. [Google Scholar] [CrossRef]
- Han, M.L.; Shen, H.H.; Hansford, K.A.; Schneider, E.K.; Sivanesan, S.; Roberts, K.D.; Thompson, P.E.; Le Brun, A.P.; Zhu, Y.; Sani, M.A.; et al. Investigating the interaction of octapeptin a3 with model bacterial membranes. ACS Infect. Dis. 2017, 3, 606–619. [Google Scholar] [CrossRef] [Green Version]
- Rosales-Reyes, R.; Vargas-Roldan, S.Y.; Lezana-Fernandez, J.L.; Santos-Preciado, J.I. Pseudomonas aeruginosa: Genetic adaptation, a strategy for its persistence in cystic fibrosis. Arch. Med. Res. 2021, 52, 357–361. [Google Scholar] [CrossRef]
- Deretic, V.; Schurr, M.J.; Yu, H. Pseudomonas aeruginosa, mucoidy and the chronic infection phenotype in cystic fibrosis. Trends Microbiol. 1995, 3, 351–356. [Google Scholar] [CrossRef]
- Pritt, B.; O’Brien, L.; Winn, W. Mucoid pseudomonas in cystic fibrosis. Am. J. Clin. Pathol. 2007, 128, 32–34. [Google Scholar] [CrossRef] [Green Version]
- Hogardt, M.; Heesemann, J. Microevolution of pseudomonas aeruginosa to a chronic pathogen of the cystic fibrosis lung. Curr. Top. Microbiol. Immunol. 2013, 358, 91–118. [Google Scholar] [CrossRef]
- Hengzhuang, W.; Wu, H.; Ciofu, O.; Song, Z.; Hoiby, N. In vivo pharmacokinetics/pharmacodynamics of colistin and imipenem in pseudomonas aeruginosa biofilm infection. Antimicrob. Agents Chemother. 2012, 56, 2683–2690. [Google Scholar] [CrossRef] [Green Version]
- Lory, S.; Merighi, M.; Hyodo, M. Multiple activities of c-di-gmp in pseudomonas aeruginosa. Nucleic Acids Symp Ser. 2009, 53, 51–52. [Google Scholar] [CrossRef] [Green Version]
- Smith, E.E.; Buckley, D.G.; Wu, Z.; Saenphimmachak, C.; Hoffman, L.R.; D’Argenio, D.A.; Miller, S.I.; Ramsey, B.W.; Speert, D.P.; Moskowitz, S.M.; et al. Genetic adaptation by pseudomonas aeruginosa to the airways of cystic fibrosis patients. Proc. Natl. Acad. Sci. USA 2006, 103, 8487–8492. [Google Scholar] [CrossRef] [Green Version]
- Akil, N.; Muhlebach, M.S. Biology and management of methicillin resistant staphylococcus aureus in cystic fibrosis. Pediatr. Pulmonol. 2018, 53, S64–S74. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hussein, M.; Karas, J.A.; Schneider-Futschik, E.K.; Chen, F.; Swarbrick, J.; Paulin, O.K.A.; Hoyer, D.; Baker, M.; Zhu, Y.; Li, J.; et al. The killing mechanism of teixobactin against methicillin-resistant staphylococcus aureus: An untargeted metabolomics study. mSystems 2020, 5, e00077-20. [Google Scholar] [CrossRef] [PubMed]
- Blanchard, A.C.; Waters, V.J. Microbiology of cystic fibrosis airway disease. Semin. Respir. Crit. Care Med. 2019, 40, 727–736. [Google Scholar] [CrossRef] [PubMed]
- Cheung, G.Y.C.; Bae, J.S.; Otto, M. Pathogenicity and virulence of staphylococcus aureus. Virulence 2021, 12, 547–569. [Google Scholar] [CrossRef] [PubMed]
- To, K.; Cao, R.; Yegiazaryan, A.; Owens, J.; Venketaraman, V. General overview of nontuberculous mycobacteria opportunistic pathogens: Mycobacterium avium and mycobacterium abscessus. J. Clin. Med. 2020, 9, 2541. [Google Scholar] [CrossRef]
- Cogen, J.D.; Onchiri, F.; Emerson, J.; Gibson, R.L.; Hoffman, L.R.; Nichols, D.P.; Rosenfeld, M. Chronic azithromycin use in cystic fibrosis and risk of treatment-emergent respiratory pathogens. Ann. Am. Thorac Soc. 2018, 15, 702–709. [Google Scholar] [CrossRef]
- Elborn, J.S.; Flume, P.A.; Van Devanter, D.R.; Procaccianti, C. Management of chronic pseudomonas aeruginosa infection with inhaled levofloxacin in people with cystic fibrosis. Future Microbiol. 2021, 16, 1087–1104. [Google Scholar] [CrossRef]
- Waters, V.J.; Kidd, T.J.; Canton, R.; Ekkelenkamp, M.B.; Johansen, H.K.; LiPuma, J.J.; Bell, S.C.; Elborn, J.S.; Flume, P.A.; VanDevanter, D.R.; et al. Reconciling antimicrobial susceptibility testing and clinical response in antimicrobial treatment of chronic cystic fibrosis lung infections. Clin. Infect. Dis. 2019, 69, 1812–1816. [Google Scholar] [CrossRef] [Green Version]
- National Center for Biotechnology Information. Pubchem Compound Summary for Cid 36294, tobramycin. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Tobramycin (accessed on 12 January 2023).
- National Center for Biotechnology Information. Pubchem Compound Summary for Cid 5742832, azactam. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Azactam (accessed on 12 January 2023).
- National Center for Biotechnology Information. Pubchem Compound Summary for Cid 149096, levofloxacin. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Levofloxacin (accessed on 12 January 2023).
- National Center for Biotechnology Information. Pubchem Compound Summary for Cid 5311054, colistin. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Colistin (accessed on 12 January 2023).
- National Center for Biotechnology Information. Pubchem Compound Summary for Cid 37768, amikacin. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Amikacin (accessed on 12 January 2023).
- National Center for Biotechnology Information. Pubchem Compound Summary for Cid 91824766, murepavadin. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Murepavadin. (accessed on 12 January 2023).
- Krause, K.M.; Serio, A.W.; Kane, T.R.; Connolly, L.E. Aminoglycosides: An overview. Cold Spring Harb Perspect. Med. 2016, 6, a027029. [Google Scholar] [CrossRef] [Green Version]
- Nasr, S.Z.; Sakmar, E.; Christodoulou, E.; Eckhardt, B.P.; Streetman, D.S.; Strouse, P.J. The use of high resolution computerized tomography (hrct) of the chest in evaluating the effect of tobramycin solution for inhalation in cystic fibrosis lung disease. Pediatr. Pulmonol. 2010, 45, 440–449. [Google Scholar] [CrossRef]
- Ramsey, B.W.; Pepe, M.S.; Quan, J.M.; Otto, K.L.; Montgomery, A.B.; Williams-Warren, J.; Vasiljev, K.M.; Borowitz, D.; Bowman, C.M.; Marshall, B.C.; et al. Intermittent administration of inhaled tobramycin in patients with cystic fibrosis. Cystic fibrosis inhaled tobramycin study group. N. Engl. J. Med. 1999, 340, 23–30. [Google Scholar] [CrossRef] [Green Version]
- Chuchalin, A.; Csiszer, E.; Gyurkovics, K.; Bartnicka, M.T.; Sands, D.; Kapranov, N.; Varoli, G.; Monici Preti, P.A.; Mazurek, H. A formulation of aerosolized tobramycin (bramitob) in the treatment of patients with cystic fibrosis and pseudomonas aeruginosa infection: A double-blind, placebo-controlled, multicenter study. Paediatr. Drugs. 2007, 9 (Suppl. 1), 21–31. [Google Scholar] [CrossRef]
- Lenoir, G.; Antypkin, Y.G.; Miano, A.; Moretti, P.; Zanda, M.; Varoli, G.; Monici Preti, P.A.; Aryayev, N.L. Efficacy, safety, and local pharmacokinetics of highly concentrated nebulized tobramycin in patients with cystic fibrosis colonized with pseudomonas aeruginosa. Paediatr. Drugs. 2007, 9 (Suppl. 1), 11–20. [Google Scholar] [CrossRef]
- Konstan, M.W.; Flume, P.A.; Kappler, M.; Chiron, R.; Higgins, M.; Brockhaus, F.; Zhang, J.; Angyalosi, G.; He, E.; Geller, D.E. Safety, efficacy and convenience of tobramycin inhalation powder in cystic fibrosis patients: The eager trial. J. Cyst. Fibros. 2011, 10, 54–61. [Google Scholar] [CrossRef] [Green Version]
- Konstan, M.W.; Geller, D.E.; Minic, P.; Brockhaus, F.; Zhang, J.; Angyalosi, G. Tobramycin inhalation powder for p. Aeruginosa infection in cystic fibrosis: The evolve trial. Pediatr. Pulmonol. 2011, 46, 230–238. [Google Scholar] [CrossRef] [Green Version]
- Quittner, A.L.; Buu, A. Effects of tobramycin solution for inhalation on global ratings of quality of life in patients with cystic fibrosis and pseudomonas aeruginosa infection. Pediatr. Pulmonol. 2002, 33, 269–276. [Google Scholar] [CrossRef]
- McCoy, K.S.; Quittner, A.L.; Oermann, C.M.; Gibson, R.L.; Retsch-Bogart, G.Z.; Montgomery, A.B. Inhaled aztreonam lysine for chronic airway pseudomonas aeruginosa in cystic fibrosis. Am. J. Respir. Crit. Care Med. 2008, 178, 921–928. [Google Scholar] [CrossRef] [Green Version]
- Retsch-Bogart, G.Z.; Quittner, A.L.; Gibson, R.L.; Oermann, C.M.; McCoy, K.S.; Montgomery, A.B.; Cooper, P.J. Efficacy and safety of inhaled aztreonam lysine for airway pseudomonas in cystic fibrosis. Chest 2009, 135, 1223–1232. [Google Scholar] [CrossRef] [Green Version]
- Wainwright, C.E.; Quittner, A.L.; Geller, D.E.; Nakamura, C.; Wooldridge, J.L.; Gibson, R.L.; Lewis, S.; Montgomery, A.B. Aztreonam for inhalation solution (azli) in patients with cystic fibrosis, mild lung impairment, and p. Aeruginosa. J. Cyst. Fibros. 2011, 10, 234–242. [Google Scholar] [CrossRef] [Green Version]
- Assael, B.M.; Pressler, T.; Bilton, D.; Fayon, M.; Fischer, R.; Chiron, R.; LaRosa, M.; Knoop, C.; McElvaney, N.; Lewis, S.A.; et al. Inhaled aztreonam lysine vs. Inhaled tobramycin in cystic fibrosis: A comparative efficacy trial. J. Cyst. Fibros. 2013, 12, 130–140. [Google Scholar] [CrossRef] [Green Version]
- Geller, D.E.; Flume, P.A.; Staab, D.; Fischer, R.; Loutit, J.S.; Conrad, D.J.; Mpex 204 Study, G. Levofloxacin inhalation solution (mp-376) in patients with cystic fibrosis with pseudomonas aeruginosa. Am. J. Respir. Crit. Care Med. 2011, 183, 1510–1516. [Google Scholar] [CrossRef] [PubMed]
- Stuart Elborn, J.; Geller, D.E.; Conrad, D.; Aaron, S.D.; Smyth, A.R.; Fischer, R.; Kerem, E.; Bell, S.C.; Loutit, J.S.; Dudley, M.N.; et al. A phase 3, open-label, randomized trial to evaluate the safety and efficacy of levofloxacin inhalation solution (apt-1026) versus tobramycin inhalation solution in stable cystic fibrosis patients. J. Cyst. Fibros. 2015, 14, 507–514. [Google Scholar] [CrossRef] [PubMed]
- Flume, P.A.; Clancy, J.P.; Retsch-Bogart, G.Z.; Tullis, D.E.; Bresnik, M.; Derchak, P.A.; Lewis, S.A.; Ramsey, B.W. Continuous alternating inhaled antibiotics for chronic pseudomonal infection in cystic fibrosis. J. Cyst. Fibros. 2016, 15, 809–815. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jensen, T.; Pedersen, S.S.; Garne, S.; Heilmann, C.; Hoiby, N.; Koch, C. Colistin inhalation therapy in cystic fibrosis patients with chronic pseudomonas aeruginosa lung infection. J. Antimicrob. Chemother. 1987, 19, 831–838. [Google Scholar] [CrossRef]
- Hodson, M.E.; Gallagher, C.G.; Govan, J.R. A randomised clinical trial of nebulised tobramycin or colistin in cystic fibrosis. Eur. Respir. J. 2002, 20, 658–664. [Google Scholar] [CrossRef] [Green Version]
- Schuster, A.; Haliburn, C.; Doring, G.; Goldman, M.H.; Freedom Study Group. Safety, efficacy and convenience of colistimethate sodium dry powder for inhalation (colobreathe dpi) in patients with cystic fibrosis: A randomised study. Thorax 2013, 68, 344–350. [Google Scholar] [CrossRef] [Green Version]
- Clancy, J.P.; Dupont, L.; Konstan, M.W.; Billings, J.; Fustik, S.; Goss, C.H.; Lymp, J.; Minic, P.; Quittner, A.L.; Rubenstein, R.C.; et al. Phase ii studies of nebulised arikace in cf patients with pseudomonas aeruginosa infection. Thorax 2013, 68, 818–825. [Google Scholar] [CrossRef] [Green Version]
- Bilton, D.; Pressler, T.; Fajac, I.; Clancy, J.P.; Sands, D.; Minic, P.; Cipolli, M.; Galeva, I.; Sole, A.; Quittner, A.L.; et al. Amikacin liposome inhalation suspension for chronic pseudomonas aeruginosa infection in cystic fibrosis. J. Cyst. Fibros. 2020, 19, 284–291. [Google Scholar] [CrossRef]
- Spexis. Inhaled Murepavadin. Available online: https://spexisbio.com/pol7080/. (accessed on 6 December 2022).
- U.S. Food and Drug Aministration. Tobi (Tobramycin Inhalation Solution), for Oral Inhalation Use. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/050753s022lbl.pdf (accessed on 20 December 2022).
- U.S. Food and Drug Administration. Bethkis (Tobramycin Inhalation Solution). Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2012/201820s000lbl.pdf. (accessed on 20 December 2022).
- U.S. Food and Drug Administration. Tobi Podhaler (Tobramycin Inhalation Powder), for Oral Inhalation Use. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/201688s006lbl.pdf (accessed on 20 December 2022).
- Ehsan, Z.; Clancy, J.P. Management of pseudomonas aeruginosa infection in cystic fibrosis patients using inhaled antibiotics with a focus on nebulized liposomal amikacin. Future Microbiol. 2015, 10, 1901–1912. [Google Scholar] [CrossRef] [Green Version]
- Bush, K.; Bradford, P.A. Beta-lactams and beta-lactamase inhibitors: An overview. Cold Spring Harb Perspect Med. 2016, 6, a025247. [Google Scholar] [CrossRef]
- McCoy, K.S. Compounded colistimethate as possible cause of fatal acute respiratory distress syndrome. N. Engl. J. Med. 2007, 357, 2310–2311. [Google Scholar] [CrossRef]
- U.S. Food and Drug Administration. Cayston (Aztreonam for Inhalation Solution). Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2012/050814s007lbl.pdf (accessed on 20 December 2022).
- Tunitskaya, V.L.; Khomutov, A.R.; Kochetkov, S.N.; Kotovskaya, S.K.; Charushin, V.N. Inhibition of DNA gyrase by levofloxacin and related fluorine-containing heterocyclic compounds. Acta Nat. 2011, 3, 94–99. [Google Scholar] [CrossRef]
- King, P.; Lomovskaya, O.; Griffith, D.C.; Burns, J.L.; Dudley, M.N. In vitro pharmacodynamics of levofloxacin and other aerosolized antibiotics under multiple conditions relevant to chronic pulmonary infection in cystic fibrosis. Antimicrob. Agents Chemother. 2010, 54, 143–148. [Google Scholar] [CrossRef] [Green Version]
- Flume, P.A.; VanDevanter, D.R.; Morgan, E.E.; Dudley, M.N.; Loutit, J.S.; Bell, S.C.; Kerem, E.; Fischer, R.; Smyth, A.R.; Aaron, S.D.; et al. A phase 3, multi-center, multinational, randomized, double-blind, placebo-controlled study to evaluate the efficacy and safety of levofloxacin inhalation solution (apt-1026) in stable cystic fibrosis patients. J. Cyst. Fibros. 2016, 15, 495–502. [Google Scholar] [CrossRef] [Green Version]
- Zemanick, E.T.; Taylor-Cousar, J.L.; Davies, J.; Gibson, R.L.; Mall, M.A.; McKone, E.F.; McNally, P.; Ramsey, B.W.; Rayment, J.H.; Rowe, S.M.; et al. A phase 3 open-label study of elexacaftor/tezacaftor/ivacaftor in children 6 through 11 years of age with cystic fibrosis and at least one f508del allele. Am. J. Respir. Crit. Care Med. 2021, 203, 1522–1532. [Google Scholar] [CrossRef]
- Elborn, J.S.; Flume, P.A.; Cohen, F.; Loutit, J.; VanDevanter, D.R. Safety and efficacy of prolonged levofloxacin inhalation solution (apt-1026) treatment for cystic fibrosis and chronic pseudomonas aeruginosa airway infection. J. Cyst. Fibros. 2016, 15, 634–640. [Google Scholar] [CrossRef]
- European Medicines Agency. Quinsair—Levofloxacin. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/quinsair (accessed on 20 December 2022).
- Canadian Agency for Drugs and Technologies in Health. Cdr Clinical Reveiw Report for Quinsair. Available online: https://www.cadth.ca/sites/default/files/cdr/clinical/SR0493_Quinsair_CL_Report.pdf (accessed on 20 December 2022).
- Electronic Medicines Compendium. Quinsair 240 mg Neubuliser Solution. Available online: https://www.medicines.org.uk/emc/product/7202/smpc#gref (accessed on 20 December 2022).
- U.S. Food and Drug Administration. Fluoroquinolones Drug Safety Communication—Safety Announcement. Available online: https://www.fda.gov/media/119532/download (accessed on 23 December 2022).
- Falagas, M.E.; Kasiakou, S.K. Colistin: The revival of polymyxins for the management of multidrug-resistant gram-negative bacterial infections. Clin. Infect. Dis. 2005, 40, 1333–1341. [Google Scholar] [CrossRef] [Green Version]
- Hussein, M.; Schneider-Futschik, E.K.; Paulin, O.K.A.; Allobawi, R.; Crawford, S.; Zhou, Q.T.; Hanif, A.; Baker, M.; Zhu, Y.; Li, J.; et al. Effective strategy targeting polymyxin-resistant gram-negative pathogens: Polymyxin b in combination with the selective serotonin reuptake inhibitor sertraline. ACS Infect. Dis. 2020, 6, 1436–1450. [Google Scholar] [CrossRef]
- Allobawi, R.; Ghelani, D.P.; Schneider-Futschik, E.K. Metabolomic description of ivacaftor elevating polymyxin b mediated antibacterial activity in cystic fibrosis pseudomonas aeruginosa. ACS Pharmacol. Transl. Sci. 2020, 3, 433–443. [Google Scholar] [CrossRef]
- Koerner-Rettberg, C.; Ballmann, M. Colistimethate sodium for the treatment of chronic pulmonary infection in cystic fibrosis: An evidence-based review of its place in therapy. Core Evid. 2014, 9, 99–112. [Google Scholar] [CrossRef] [Green Version]
- Adeboyeku, D.; Scott, S.; Hodson, M.E. Open follow-up study of tobramycin nebuliser solution and colistin in patients with cystic fibrosis. J. Cyst. Fibros. 2006, 5, 261–263. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Valenza, G.; Radike, K.; Schoen, C.; Horn, S.; Oesterlein, A.; Frosch, M.; Abele-Horn, M.; Hebestreit, H. Resistance to tobramycin and colistin in isolates of pseudomonas aeruginosa from chronically colonized patients with cystic fibrosis under antimicrobial treatment. Scand. J. Infect. Dis. 2010, 42, 885–889. [Google Scholar] [CrossRef] [PubMed]
- Pitt, T.L.; Sparrow, M.; Warner, M.; Stefanidou, M. Survey of resistance of pseudomonas aeruginosa from uk patients with cystic fibrosis to six commonly prescribed antimicrobial agents. Thorax 2003, 58, 794–796. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Littlewood, J.M.; Koch, C.; Lambert, P.A.; Hoiby, N.; Elborn, J.S.; Conway, S.P.; Dinwiddie, R.; Duncan-Skingle, F. A ten year review of colomycin. Respir. Med. 2000, 94, 632–640. [Google Scholar] [CrossRef] [Green Version]
- Burns, J.L.; Van Dalfsen, J.M.; Shawar, R.M.; Otto, K.L.; Garber, R.L.; Quan, J.M.; Montgomery, A.B.; Albers, G.M.; Ramsey, B.W.; Smith, A.L. Effect of chronic intermittent administration of inhaled tobramycin on respiratory microbial flora in patients with cystic fibrosis. J. Infect. Dis. 1999, 179, 1190–1196. [Google Scholar] [CrossRef] [Green Version]
- Giwercman, B.; Lambert, P.A.; Rosdahl, V.T.; Shand, G.H.; Hoiby, N. Rapid emergence of resistance in pseudomonas aeruginosa in cystic fibrosis patients due to in-vivo selection of stable partially derepressed beta-lactamase producing strains. J. Antimicrob. Chemother. 1990, 26, 247–259. [Google Scholar] [CrossRef]
- Cohen, J.; McConnell, J.S. Release of endotoxin from bacteria exposed to ciprofloxacin and its prevention with polymyxin b. Eur. J. Clin. Microbiol. 1986, 5, 13–17. [Google Scholar] [CrossRef]
- Alothman, G.A.; Ho, B.; Alsaadi, M.M.; Ho, S.L.; O’Drowsky, L.; Louca, E.; Coates, A.L. Bronchial constriction and inhaled colistin in cystic fibrosis. Chest 2005, 127, 522–529. [Google Scholar] [CrossRef]
- Maddison, J.; Dodd, M.; Webb, A.K. Nebulized colistin causes chest tightness in adults with cystic fibrosis. Respir. Med. 1994, 88, 145–147. [Google Scholar] [CrossRef] [Green Version]
- Kaplan, S.; Lee, A.; Caine, N.; Charman, S.C.; Bilton, D. Long-term safety study of colistimethate sodium (colobreathe(r)): Findings from the uk cystic fibrosis registry. J. Cyst. Fibros. 2021, 20, 324–329. [Google Scholar] [CrossRef]
- Electronic Medicines Compendium. Colomycin 1 Million International Units (iu) Powder for Solution for Injection, Infusion and Inhalation. Available online: https://www.medicines.org.uk/emc/product/1094/smpc#gref (accessed on 20 December 2022).
- National Institute of Allergy and Infectious Diseases. Aerosolized and Intravenous Colistin in Healthy Adults. Available online: https://clinicaltrials.gov/ct2/show/NCT01863719 (accessed on 12 January 2023).
- Cystic Fibrosis Foundation. Drug Development Pipeline—Inhaled Colistin (Colifin). Available online: https://apps.cff.org/Trials/Pipeline/details/10196/Inhaled-Colistin-ColiFin (accessed on 1 December 2022).
- Shirley, M. Amikacin liposome inhalation suspension: A review in mycobacterium avium complex lung disease. Drugs 2019, 79, 555–562. [Google Scholar] [CrossRef] [Green Version]
- Okusanya, O.O.; Bhavnani, S.M.; Hammel, J.P.; Forrest, A.; Bulik, C.C.; Ambrose, P.G.; Gupta, R. Evaluation of the pharmacokinetics and pharmacodynamics of liposomal amikacin for inhalation in cystic fibrosis patients with chronic pseudomonal infections using data from two phase 2 clinical studies. Antimicrob. Agents Chemother. 2014, 58, 5005–5015. [Google Scholar] [CrossRef] [Green Version]
- Bilton, D.; Fajac, I.; Pressler, T.; Clancy, J.P.; Sands, D.; Minic, P.; Cipolli, M.; Galeva, I.; Sole, A.; Quittner, A.L.; et al. Long-term amikacin liposome inhalation suspension in cystic fibrosis patients with chronic p. Aeruginosa infection. J. Cyst. Fibros. 2021, 20, 1010–1017. [Google Scholar] [CrossRef]
- U.S. Food and Drug Administration. Arikayce (Amikacin Liposome Inhalation Suspension), for Oral Inhalation Use. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/207356s004lbl.pdf (accessed on 20 December 2022).
- Electronic Medicines Compendium. Arikayce liposomal 590mg nebulise dispersion. Available online: https://www.medicines.org.uk/emc/product/12067/smpc#gref (accessed on 20 December 2022).
- Chiron, R.; Hoefsloot, W.; Van Ingen, J.; Marchandin, H.; Kremer, L.; Morisse-Pradier, H.; Charriot, J.; Mallet, J.P.; Herrmann, J.L.; Caimmi, D.; et al. Amikacin liposomal inhalation suspension in the treatment of mycobacterium abscessus lung infection: A french observational experience. Open Forum Infect. Dis. 2022, 9, ofac465. [Google Scholar] [CrossRef]
- Martin-Loeches, I.; Dale, G.E.; Torres, A. Murepavadin: A new antibiotic class in the pipeline. Expert Rev. Anti Infect. Ther. 2018, 16, 259–268. [Google Scholar] [CrossRef]
- Diez-Aguilar, M.; Hernandez-Garcia, M.; Morosini, M.I.; Fluit, A.; Tunney, M.M.; Huertas, N.; Del Campo, R.; Obrecht, D.; Bernardini, F.; Ekkelenkamp, M.; et al. Murepavadin antimicrobial activity against and resistance development in cystic fibrosis pseudomonas aeruginosa isolates. J. Antimicrob. Chemother. 2021, 76, 984–992. [Google Scholar] [CrossRef]
- Bernardini, F.; Dale, G.E.; Wach, A.; Obrecht, D. Pharmacokinetics and pharmacodynamics of murepavadin (pol7080) in neutropenic lung infection models when evaluated by aerosol administration. J. Cyst. Fibros. 2019, 18. [Google Scholar] [CrossRef]
- Ekkelenkamp, M.B.; Canton, R.; Diez-Aguilar, M.; Tunney, M.M.; Gilpin, D.F.; Bernardini, F.; Dale, G.E.; Elborn, J.S.; Bayjanov, J.R.; Fluit, A. Susceptibility of pseudomonas aeruginosa recovered from cystic fibrosis patients to murepavadin and 13 comparator antibiotics. Antimicrob. Agents Chemother. 2020, 64, e01541-19. [Google Scholar] [CrossRef]
- Diez-Aguilar, M.; Ekkelenkamp, M.; Morosini, M.I.; Huertas, N.; Del Campo, R.; Zamora, J.; Fluit, A.C.; Tunney, M.M.; Obrecht, D.; Bernardini, F.; et al. Anti-biofilm activity of murepavadin against cystic fibrosis pseudomonas aeruginosa isolates. J. Antimicrob. Chemother. 2021, 76, 2578–2585. [Google Scholar] [CrossRef]
- Esposito, S.; Pennoni, G.; Mencarini, V.; Palladino, N.; Peccini, L.; Principi, N. Antimicrobial treatment of staphylococcus aureus in patients with cystic fibrosis. Front. Pharmacol. 2019, 10, 849. [Google Scholar] [CrossRef] [Green Version]
- Bruniera, F.R.; Ferreira, F.M.; Saviolli, L.R.; Bacci, M.R.; Feder, D.; da Luz Gonçalves Pedreira, M.; Sorgini Peterlini, M.A.; Azzalis, L.A.; Campos Junqueira, V.B.; Fonseca, F.L. The use of vancomycin with its therapeutic and adverse effects: A review. Eur. Rev. Med. Pharmacol. Sci. 2015, 19, 694–700. [Google Scholar] [PubMed]
- National Center for Biotechnology Information. Pubchem Compound Summary for Cid 446987, fosfomycin. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Fosfomycin (accessed on 13 January 2023).
- National Center for Biotechnology Information. Pubchem Compound Summary for Cid 14969, vancomycin. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Vancomycin (accessed on 13 January 2023).
- Solis, A.; Brown, D.; Hughes, J.; Van Saene, H.K.; Heaf, D.P. Methicillin-resistant staphylococcus aureus in children with cystic fibrosis: An eradication protocol. Pediatr. Pulmonol. 2003, 36, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Kappler, M.; Nagel, F.; Feilcke, M.; Kroner, C.; Pawlita, I.; Naehrig, S.; Ripper, J.; Hengst, M.; von Both, U.; Forstner, M.; et al. Eradication of methicillin resistant staphylococcus aureus detected for the first time in cystic fibrosis: A single center observational study. Pediatr. Pulmonol. 2016, 51, 1010–1019. [Google Scholar] [CrossRef] [PubMed]
- Kiefer, A.; Bogdan, C.; Melichar, V.O. Successful eradication of newly acquired mrsa in six of seven patients with cystic fibrosis applying a short-term local and systemic antibiotic scheme. BMC Pulm. Med. 2018, 18, 20. [Google Scholar] [CrossRef] [Green Version]
- Maiz, L.; Canton, R.; Mir, N.; Baquero, F.; Escobar, H. Aerosolized vancomycin for the treatment of methicillin-resistant staphylococcus aureus infection in cystic fibrosis. Pediatr. Pulmonol. 1998, 26, 287–289. [Google Scholar] [CrossRef]
- Dezube, R.; Jennings, M.T.; Rykiel, M.; Diener-West, M.; Boyle, M.P.; Chmiel, J.F.; Dasenbrook, E.C. Eradication of persistent methicillin-resistant staphylococcus aureus infection in cystic fibrosis. J. Cyst. Fibros. 2019, 18, 357–363. [Google Scholar] [CrossRef]
- Silver, L.L. Fosfomycin: Mechanism and resistance. Cold Spring Harb Perspect Med. 2017, 7, a025262. [Google Scholar] [CrossRef] [Green Version]
- Trapnell, B.C.; McColley, S.A.; Kissner, D.G.; Rolfe, M.W.; Rosen, J.M.; McKevitt, M.; Moorehead, L.; Montgomery, A.B.; Geller, D.E.; Phase, F.T.I.S.G. Fosfomycin/tobramycin for inhalation in patients with cystic fibrosis with pseudomonas airway infection. Am. J. Respir. Crit. Care Med. 2012, 185, 171–178. [Google Scholar] [CrossRef] [Green Version]
- Waters VJ, R.F. Is there a role for antimicrobial stewardship in cystic fibrosis? Ann. Am. Thorac Soc. 2014, 11, 1116–1119. [Google Scholar] [CrossRef]
- Castellani, C.; Duff, A.J.A.; Bell, S.C.; Heijerman, H.G.M.; Munck, A.; Ratjen, F.; Sermet-Gaudelus, I.; Southern, K.W.; Barben, J.; Flume, P.A.; et al. Ecfs best practice guidelines: The 2018 revision. J. Cyst. Fibros. 2018, 17, 153–178. [Google Scholar] [CrossRef] [Green Version]
- Gilligan, P.H. Microbiology of airway disease in patients with cystic fibrosis. Clin. Microbiol Rev. 1991, 4, 35–51. [Google Scholar] [CrossRef]
- Taccetti, G.; Francalanci, M.; Pizzamiglio, G.; Messore, B.; Carnovale, V.; Cimino, G.; Cipolli, M. Cystic fibrosis: Recent insights into inhaled antibiotic treatment and future perspectives. Antibiotics 2021, 10, 338. [Google Scholar] [CrossRef]
- Van de Kerkhove, C.; Goeminne, P.C.; Kicinski, M.; Nawrot, T.S.; Lorent, N.; Van Bleyenbergh, P.; De Boeck, K.; Dupont, L.J. Continuous alternating inhaled antibiotic therapy in cf: A single center retrospective analysis. J. Cyst. Fibros. 2016, 15, 802–808. [Google Scholar] [CrossRef] [Green Version]
- Dasenbrook, E.C.; Konstan, M.; Van Devanter, D.R. Association between the introduction of a new cystic fibrosis inhaled antibiotic class and change in prevalence of patients receiving multiple inhaled antibiotic classes. J. Cyst. Fibros. 2015, 14, 370–375. [Google Scholar] [CrossRef] [Green Version]
- Tangden, T. Combination antibiotic therapy for multidrug-resistant gram-negative bacteria. Ups. J. Med. Sci. 2014, 119, 149–153. [Google Scholar] [CrossRef]
| Pharmaceutical Form | Dose | Dose Frequency | Inhalation Time | FDA Status | |
|---|---|---|---|---|---|
| Tobramycin | Clear slightly yellow nebulizer solution | 300 mg/5 mL | Twice daily | ~15 min | FDA approved |
| Clear yellowish nebulizer solution | 300 mg/4 mL | Twice daily | ~15 min | FDA approved | |
| Dry powder in capsule | 4 × 28 mg (4 capsules) = 112 mg | Twice daily | ~5 min | FDA approved | |
| Clear, slightly yellow solution | 170 mg/1.7 mL | Twice daily | ~4 min | Approved in Europe | |
| Aztreonam | White powder diluted in diluent for nebulizer solution | 75 mg/mL | Three times daily | ~2–3 min | FDA approved |
| Levofloxacin | Clear pale yellow nebulizer solution | 240 mg/3 mL | Twice daily | ~5 min | Phase III |
| Colistin | Sterile white dry power | 1–2 MIU (80–160 mg) | Two to three times daily | ~1 min | Phase III |
| Amikacin liposome inhalation suspension | Milky white nebulizer dispersion | 590 mg/8.4 mL | Once daily | NA | Phase III |
| Murepavadin | NA | NA | NA | NA | Phase I |
| Reference | Year | Type | Treatment | Duration (Days) | |
|---|---|---|---|---|---|
| Tobramycin | Ramsey et al. [39] | 1999 | Double-blinded | TIS 300 mg/5 mL BID, n = 258; Placebo, n = 262 | 168 = (28 on + 28 follow-up) × 3 |
| Chuchalin et al. [40] | 2007 | Double-blinded, multicenter | TIS 300 mg/4 mL BID, n = 161; Placebo, n = 86 | 168 = (28 on + 28 follow-up) × 3 | |
| Lenoir et al. [41] | 2007 | Double-blinded | TIS 300 mg/4 mL BID, n = 29; Placebo, n = 30 | 56 = 28 on + 28 follow-up | |
| Nasr et al. [38] | 2010 | Double-blinded, multicenter | TIS 300 mg/5 mL BID, n = 16; Placebo, n = 16 | 168 = (28 on + 28 follow-up) × 3 | |
| Konstan et al. (EVOLVE study) [43] | 2011 | Double-blinded, multicenter | TIP 112 mg BID n = 46; Placebo, n = 49 | 168 = (28 on + 28 follow-up) × 3 | |
| Konstan et al. (EAGER study) [42] | 2011 | Open-labelled, Multicenter | TIP 112 mg BID, n = 308; TIS 300 mg/5 mL BID, n = 209 | 168 = (28 on + 28 follow-up) × 3 | |
| Quittner et al. [44] | 2012 | Double-blinded | TIP 112 mg BID, n = 32; Placebo, n = 30 | 56 = 28 on + 28 follow-up | |
| Aztrenom | McCoy et al. [45] | 2008 | Double-blinded, multicenter | AZLI 75 mg BID, n = 69; AZLI 75 mg TID, n = 66; Placebo, n = 76 | 28 + 36 follow-up |
| Retsch-Bogart et al. [46] | 2009 | Double-blinded, multicenter | AZLI 75 mg TID, n = 80; Placebo, n = 84 | 28 | |
| Wainwright et al. [47] | 2011 | Double-blinded, multicenter | AZLI 75 mg, TID, n = 76; Placebo, n = 81 | 28 + 14 follow-up | |
| Assael et al. [48] | 2013 | Open-labelled, multicenter | AZLI 75 mg TID, n = 136; TIS 300 mg BID, n = 132 | 168 = (28 on + 28 follow-up) × 3 | |
| Levofloxacin | Geller et al. [49] | 2014 | Phase II, double-blinded | LIS 120 mg/1.2 mL QD, n = 38; LIS 240 mg/2.4 mL QD, n = 37; LIS 240 mg/2.4 mL BID, n = 39; Placebo, n = 37 | 56 = 28 on + 28 follow-up |
| Stuart Elborn et al. [50] | 2015 | Phase III, open-labelled | LIS 240 mg/2.4 mL BID, n = 189; TIS 300 mg/5 mL BID, n = 93 | 168 = (28 on + 28 follow-up) × 3 | |
| Flume et al. [51] | 2016 | Phase III, double-blinded | LIS 240 mg/2.4 mL BID, n = 220; Placebo, n = 110 | 56 = 28 on + 28 follow-up | |
| Colistin | Jensen et al. [52] | 1987 | Double-blinded | COL 1 MIU/3 mL BID, n = 20; Placebo, n = 20 | 90 |
| Hodsen et al. [53] | 2001 | Multicenter | COL 1 MIU/3 mL BID, n = 62; TIS 300 mg/5 mL BID, n = 52 | 28 | |
| Schuster et al. [54] | 2013 | Phase III, open-labelled, multicentfoer | COL-P 1.6625 MIU BID, n = 187; TIS 300 mg/5 mL BID, n = 193 | 168 = (28 on + 28 follow-up) × 3 | |
| Amikacin Liposome Inhalation Suspension | Clancy et al. [55] | 2013 | Phase II | ALIS 70 mg OD, n = 7; ALIS 140 mg OD, n = 5; ALIS 280 mg OD, n = 21; ALIS 560 mg OD, n = 36; Placebo, n = 36 | 168 = (28 on + 28 follow-up) × 3 |
| Bilton et al. [56] | 2020 | Phase III | ALIS 590 mg/8.5 mL OD, n = 152; TIS 300 mg/5 mL BID, n = 150 | 168 = (28 on + 28 follow-up) × 3 | |
| Murepavadin | Spexis [57] | 2021 | Phase I | NA | NA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, D.; Schneider-Futschik, E.K. Current and Emerging Inhaled Antibiotics for Chronic Pulmonary Pseudomonas aeruginosa and Staphylococcus aureus Infections in Cystic Fibrosis. Antibiotics 2023, 12, 484. https://doi.org/10.3390/antibiotics12030484
Li D, Schneider-Futschik EK. Current and Emerging Inhaled Antibiotics for Chronic Pulmonary Pseudomonas aeruginosa and Staphylococcus aureus Infections in Cystic Fibrosis. Antibiotics. 2023; 12(3):484. https://doi.org/10.3390/antibiotics12030484
Chicago/Turabian StyleLi, Danni, and Elena K. Schneider-Futschik. 2023. "Current and Emerging Inhaled Antibiotics for Chronic Pulmonary Pseudomonas aeruginosa and Staphylococcus aureus Infections in Cystic Fibrosis" Antibiotics 12, no. 3: 484. https://doi.org/10.3390/antibiotics12030484
APA StyleLi, D., & Schneider-Futschik, E. K. (2023). Current and Emerging Inhaled Antibiotics for Chronic Pulmonary Pseudomonas aeruginosa and Staphylococcus aureus Infections in Cystic Fibrosis. Antibiotics, 12(3), 484. https://doi.org/10.3390/antibiotics12030484






