‘Brave Enough’: A Qualitative Study of Veterinary Decisions to Withhold or Delay Antimicrobial Treatment in Pets
Abstract
1. Introduction
2. Materials and Methods
2.1. Pre-Interview Survey
2.2. Interviews
3. Results and Discussion
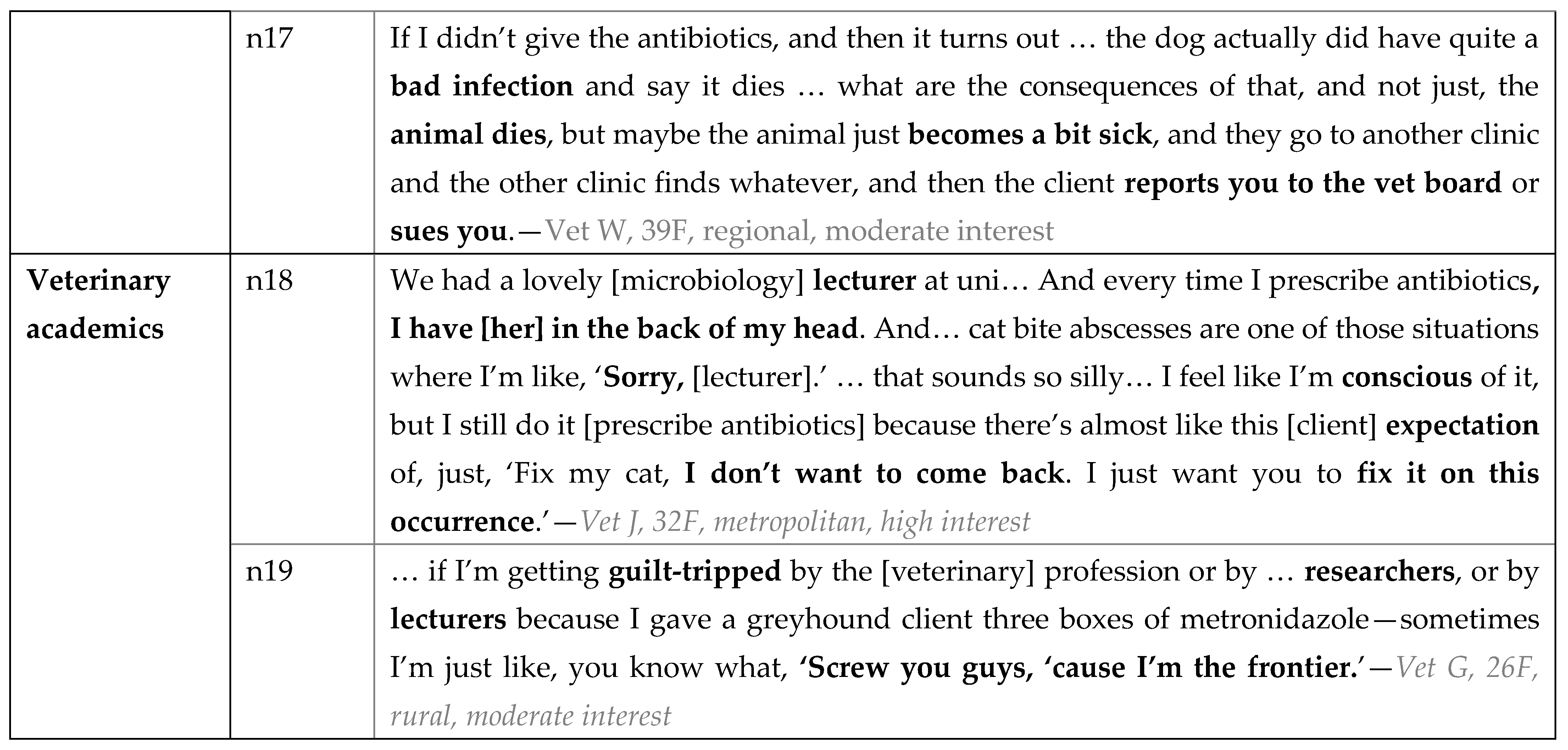
3.1. Pre-Interview Survey (Participant Characteristics)
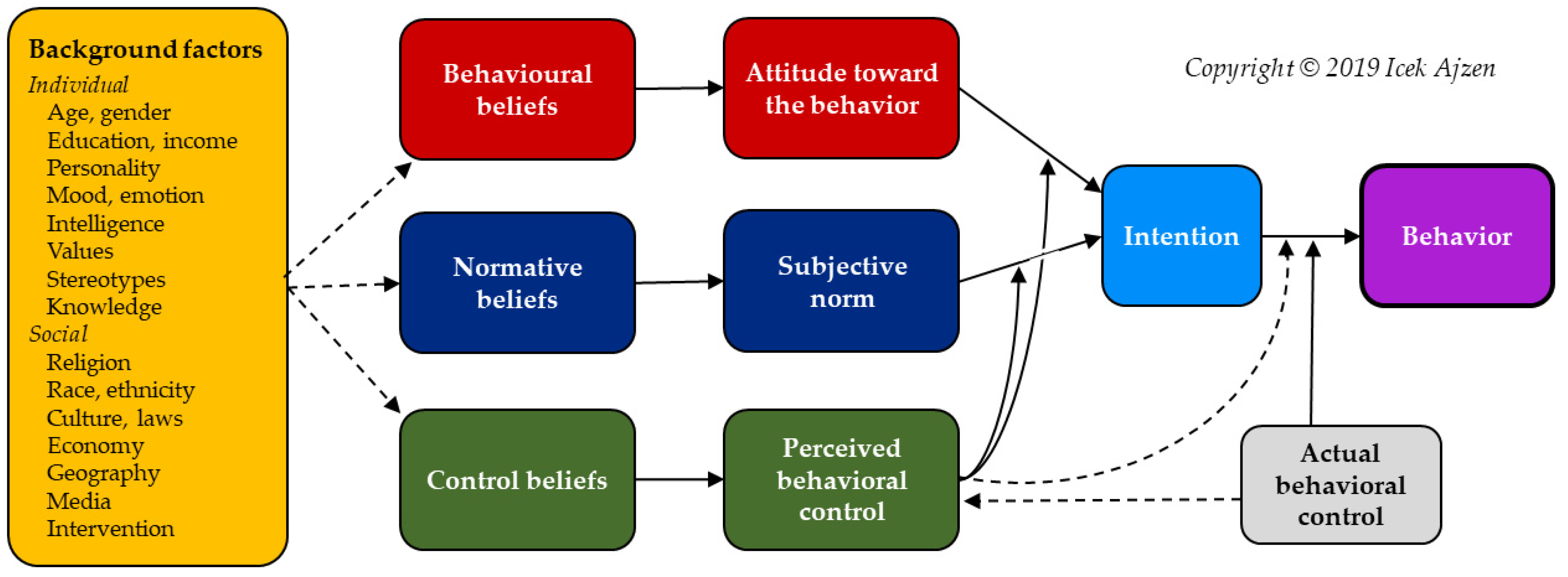
3.2. Interviews
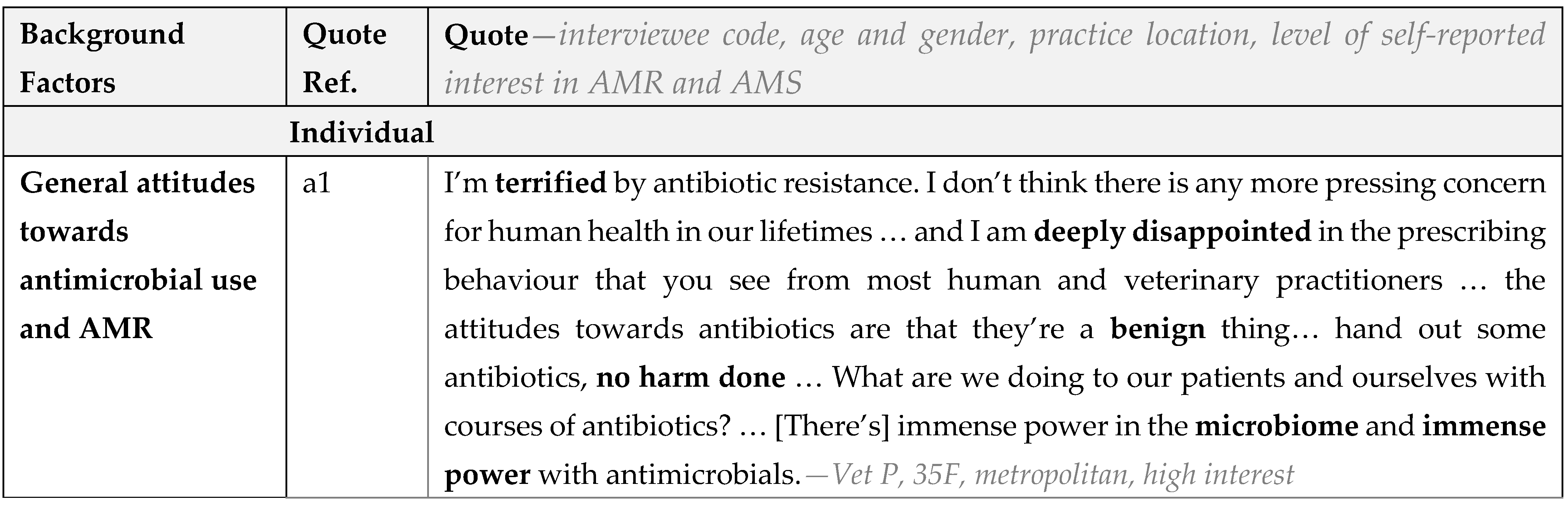
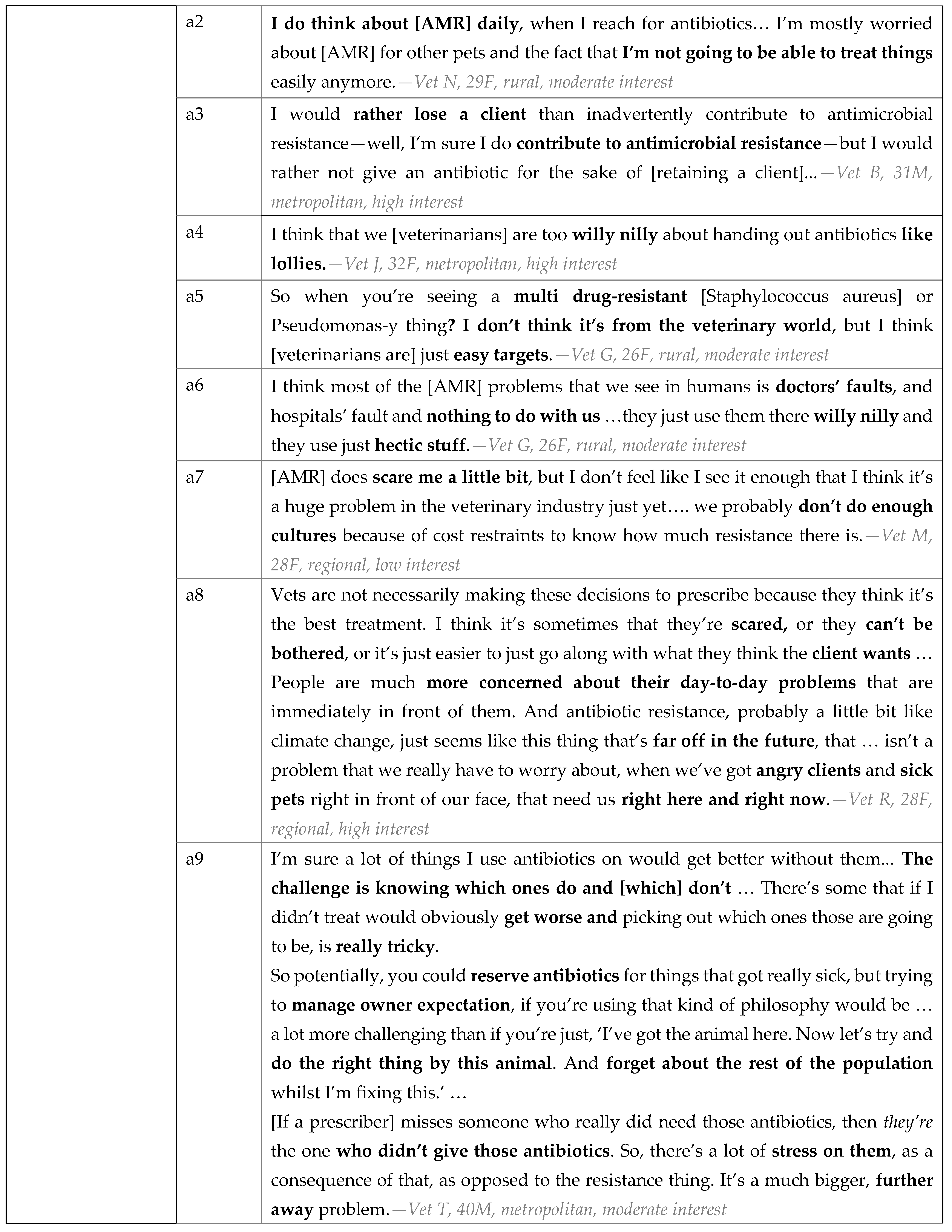
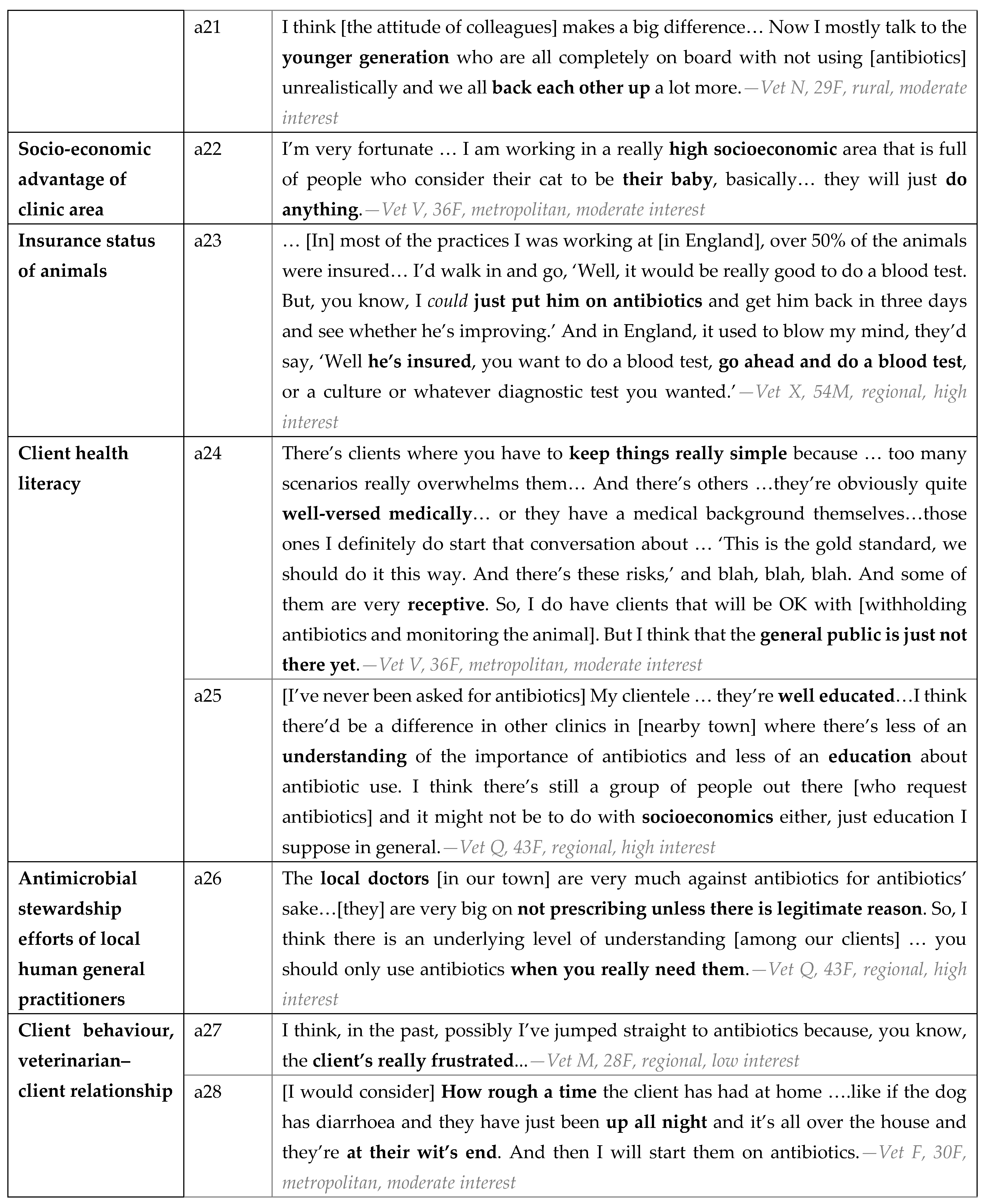
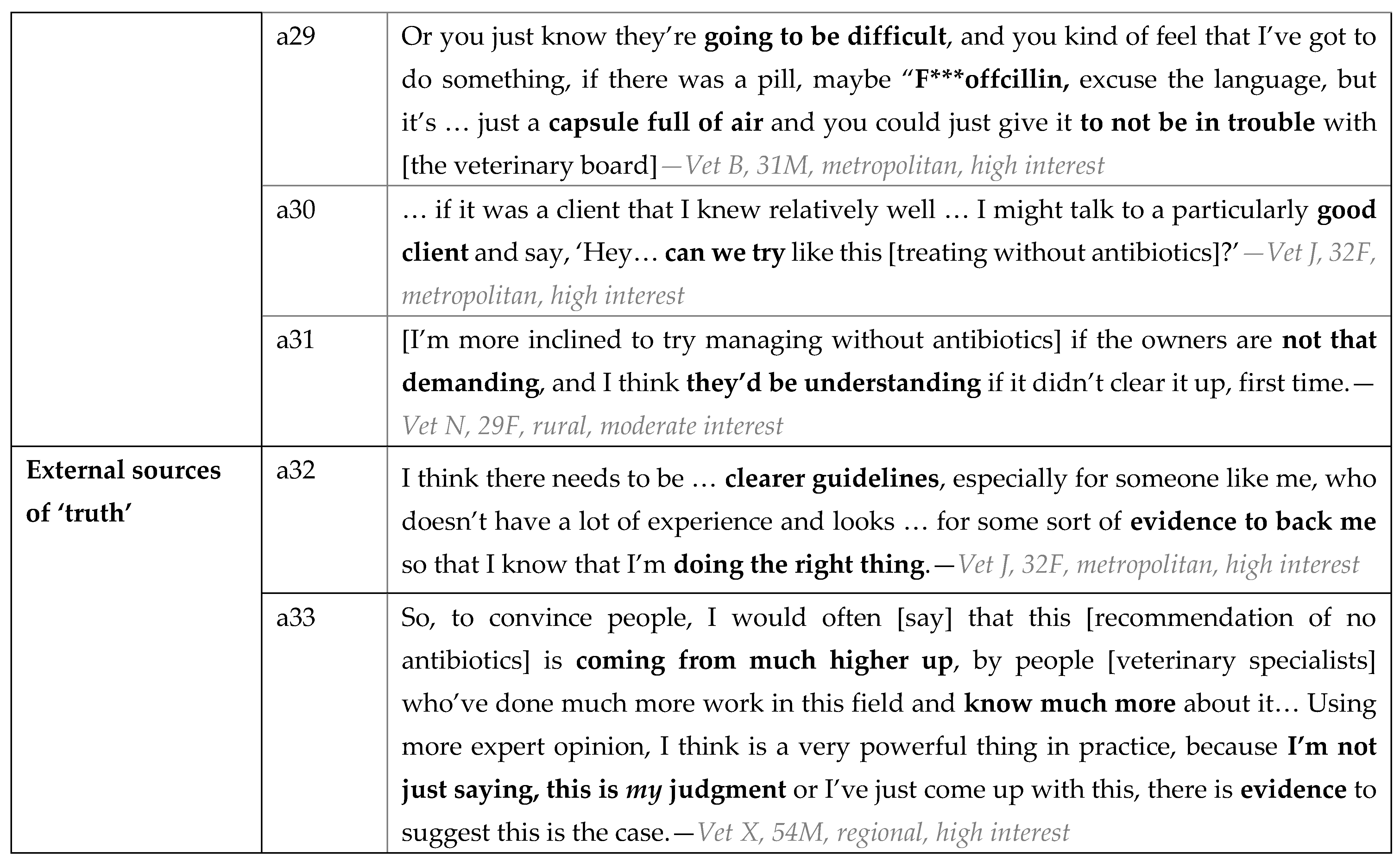
3.2.1. Background Factors
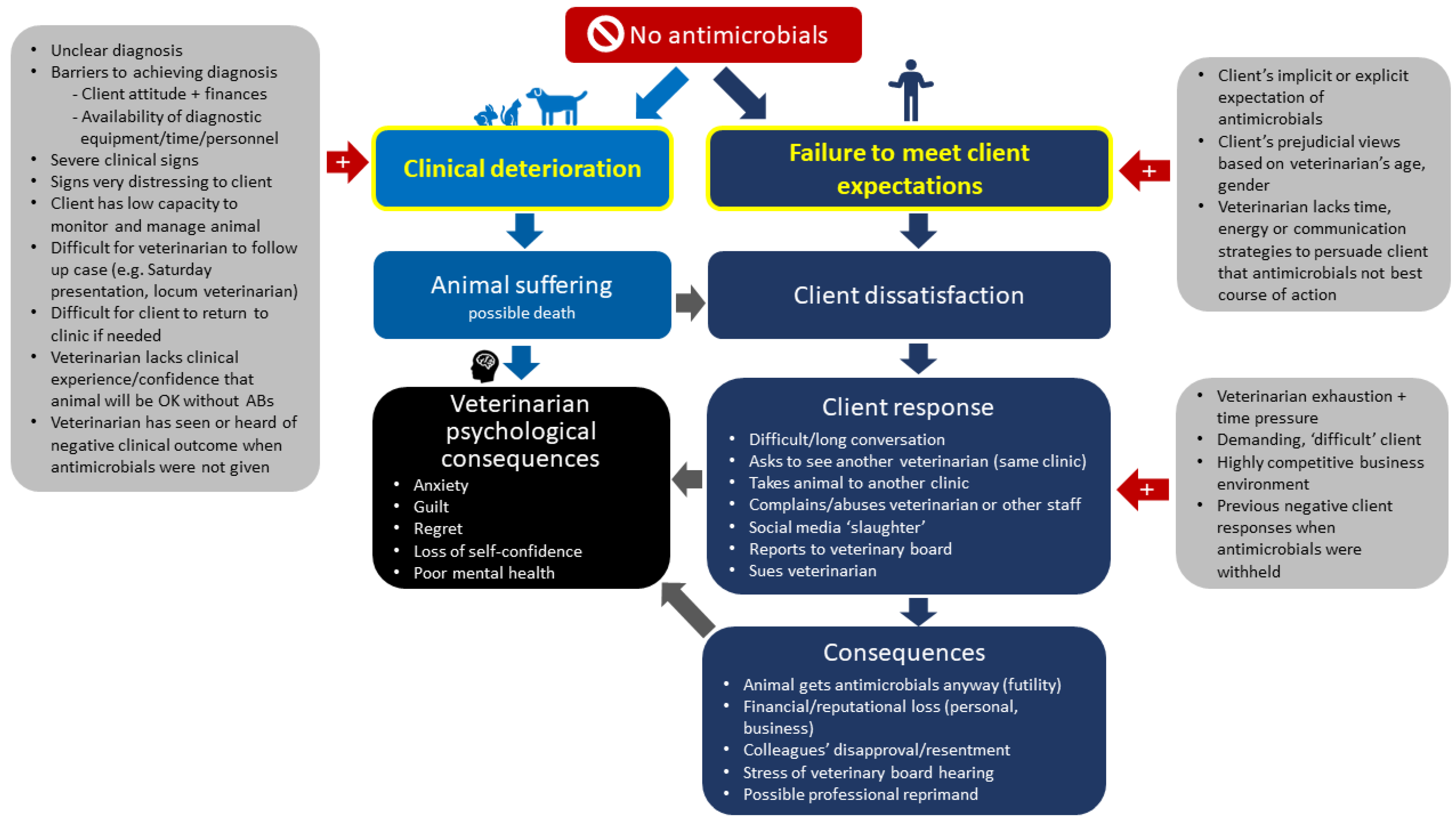
3.2.2. Behavioural Beliefs
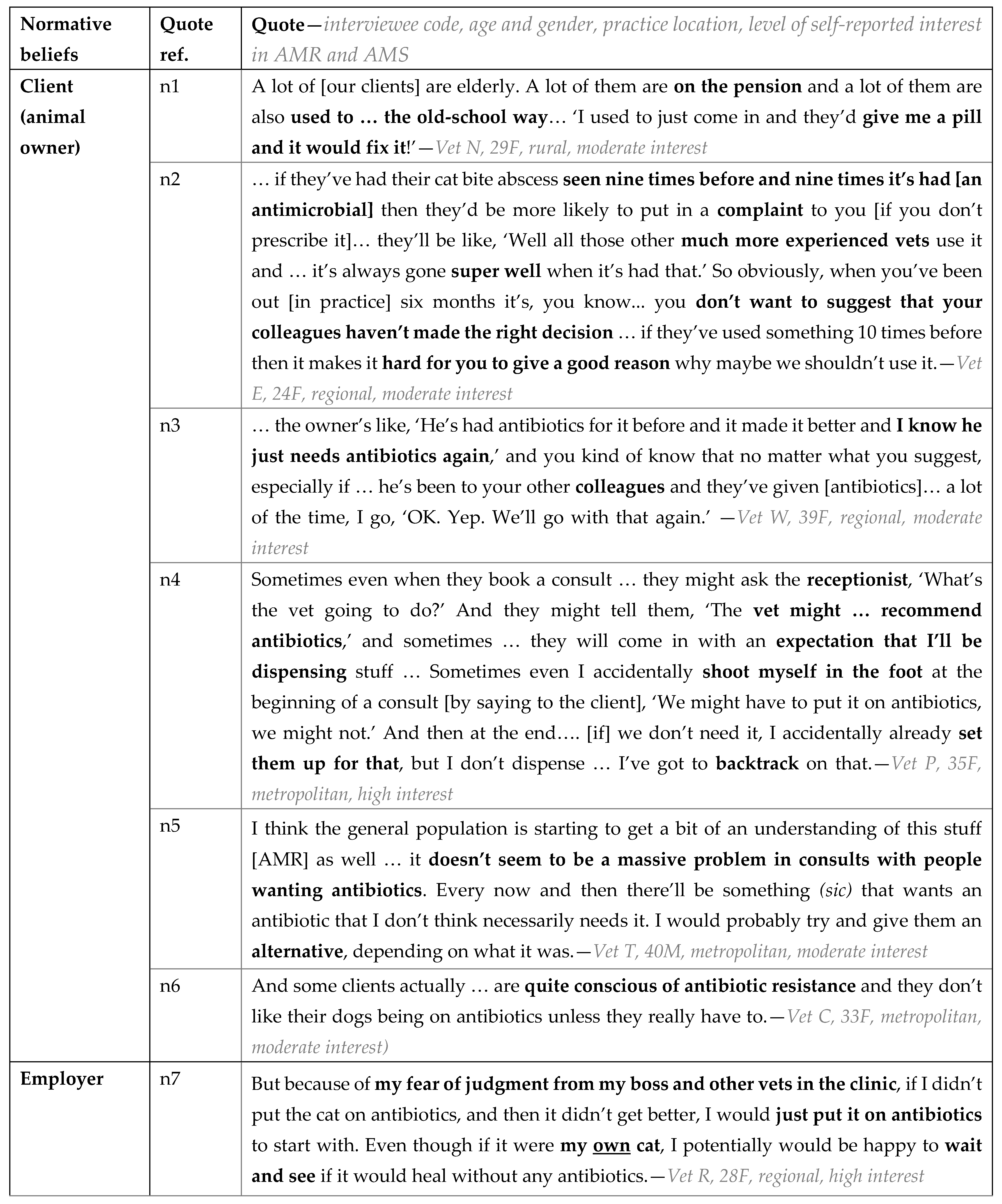
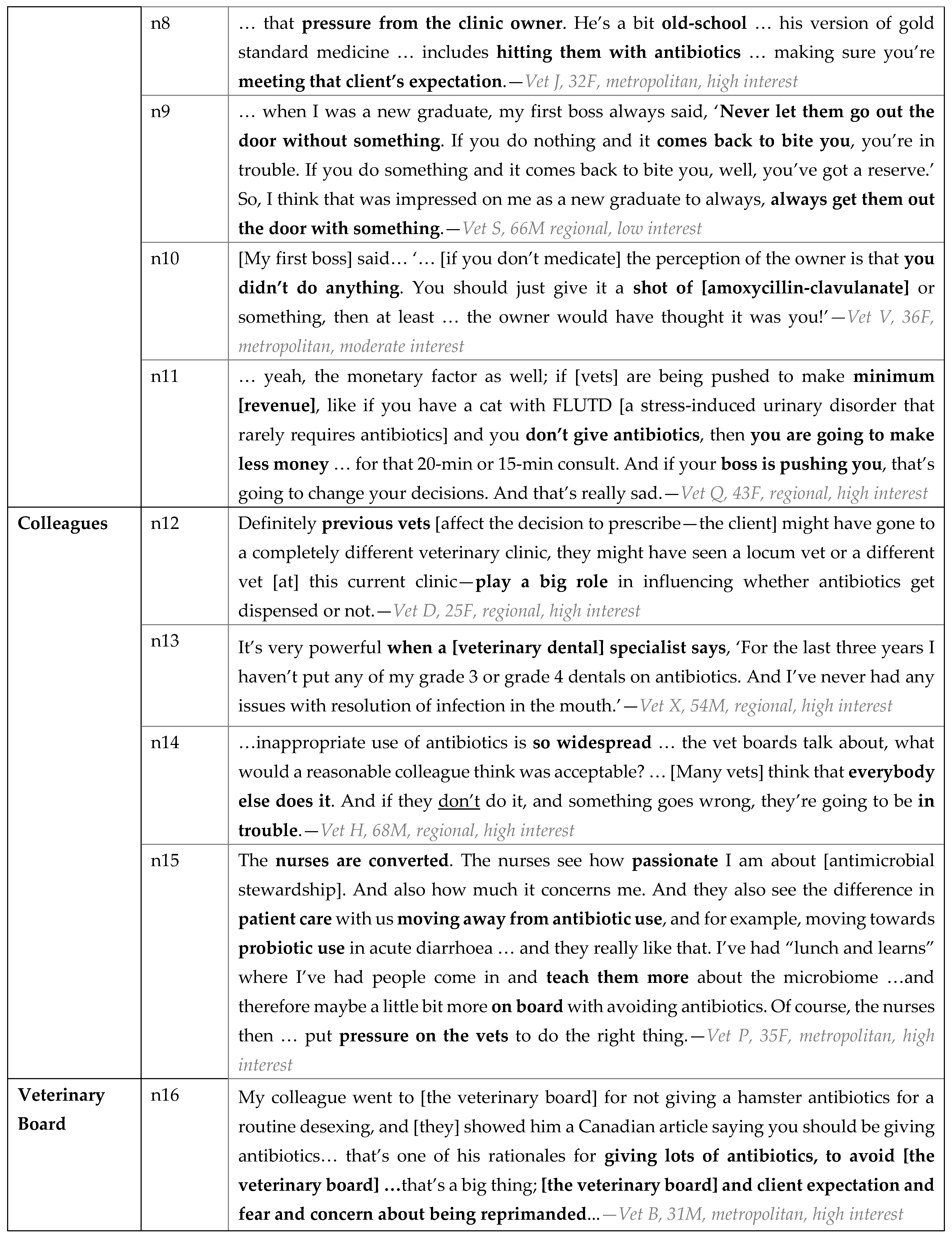
3.2.3. Normative Beliefs
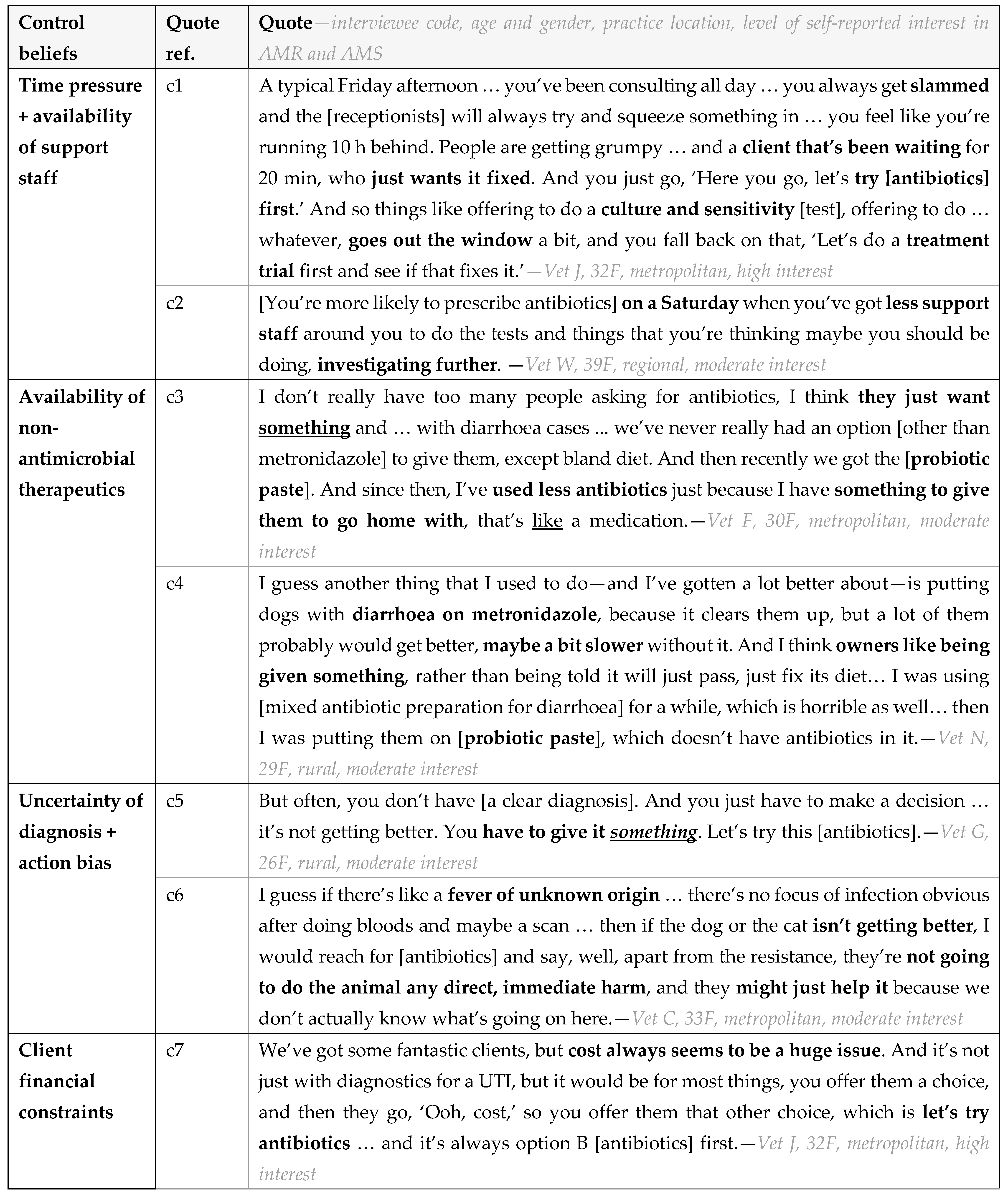
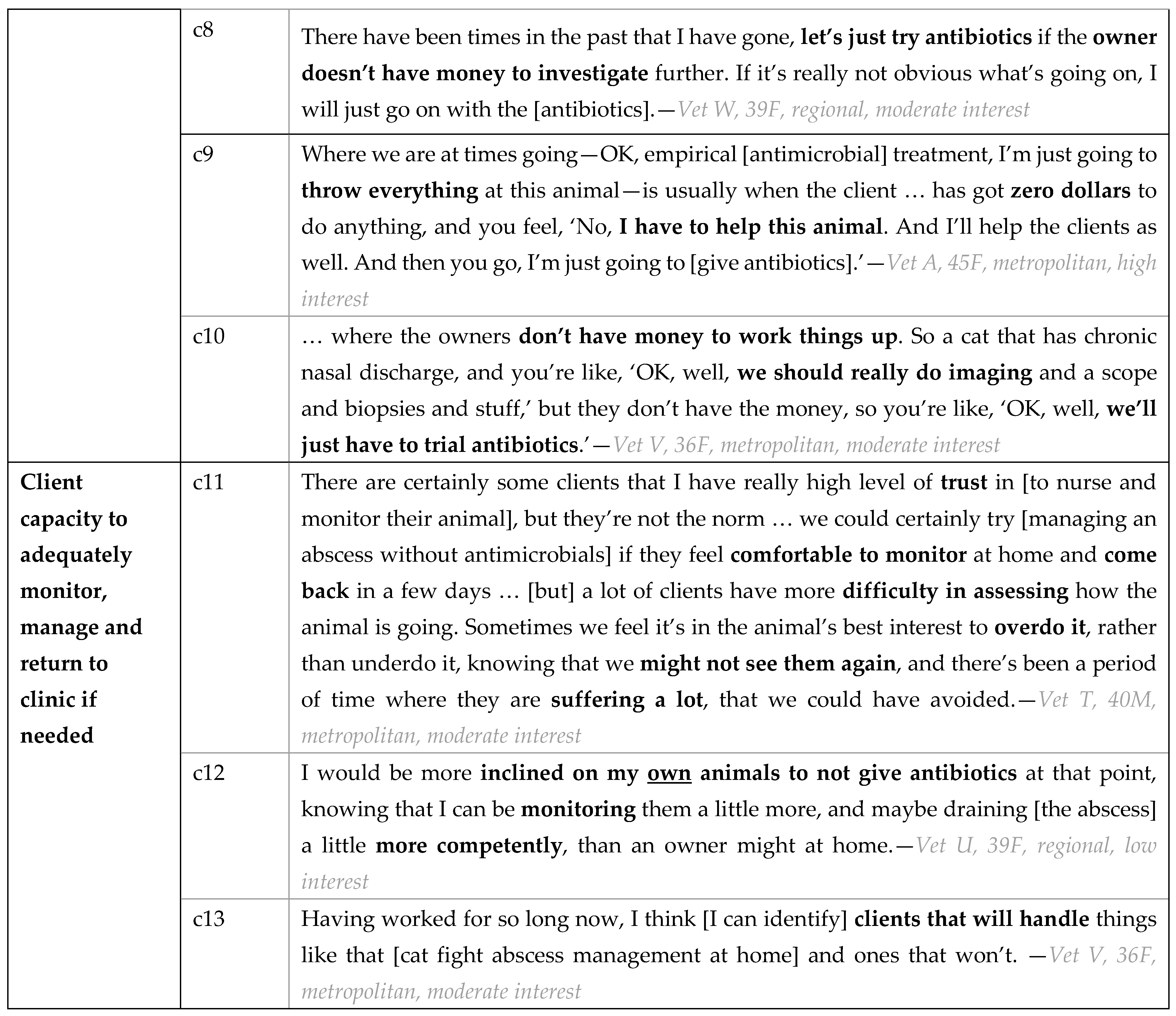
3.2.4. Control Beliefs
3.3. Suggestions for Curbing Unnecessary Antimicrobial Use in Companion Animals
3.4. Further Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Estimated Contribution to AMR | Stratified by Participant Interest Level in AMR/AMS | |||
|---|---|---|---|---|
| All (n = 22) | Low | Moderate | High | |
| Human hospitals | 33% | 30% | 27% | 39% |
| Human community care | 25% | 23% | 24% | 27% |
| Companion animals (inc. horses) | 15% | 20% | 14% | 14% |
| Production animals | 22% | 22% | 27% | 17% |
| Other farming | 6% | 4% | 8% | 4% |
Appendix B
Interview Guide
Appendix C
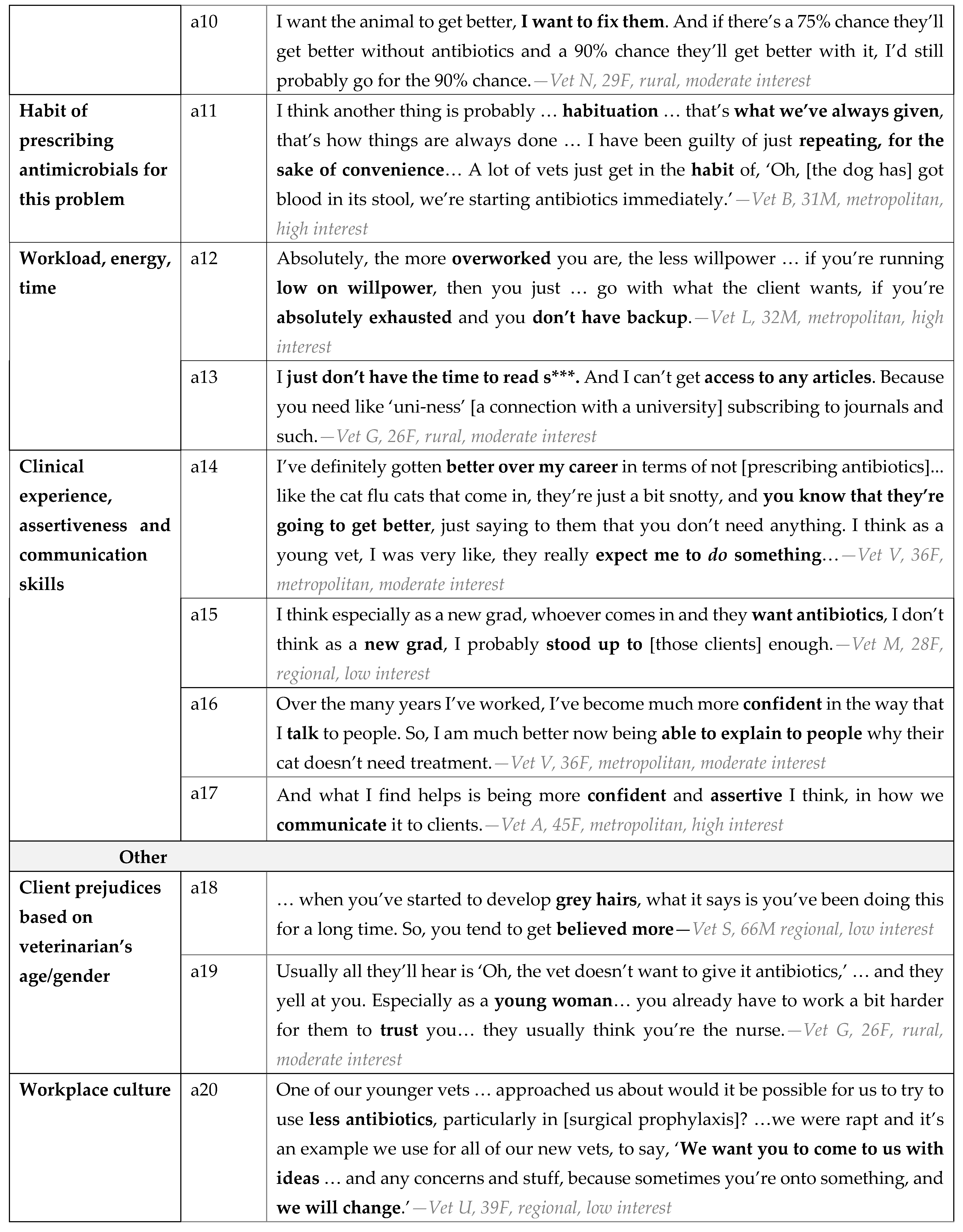
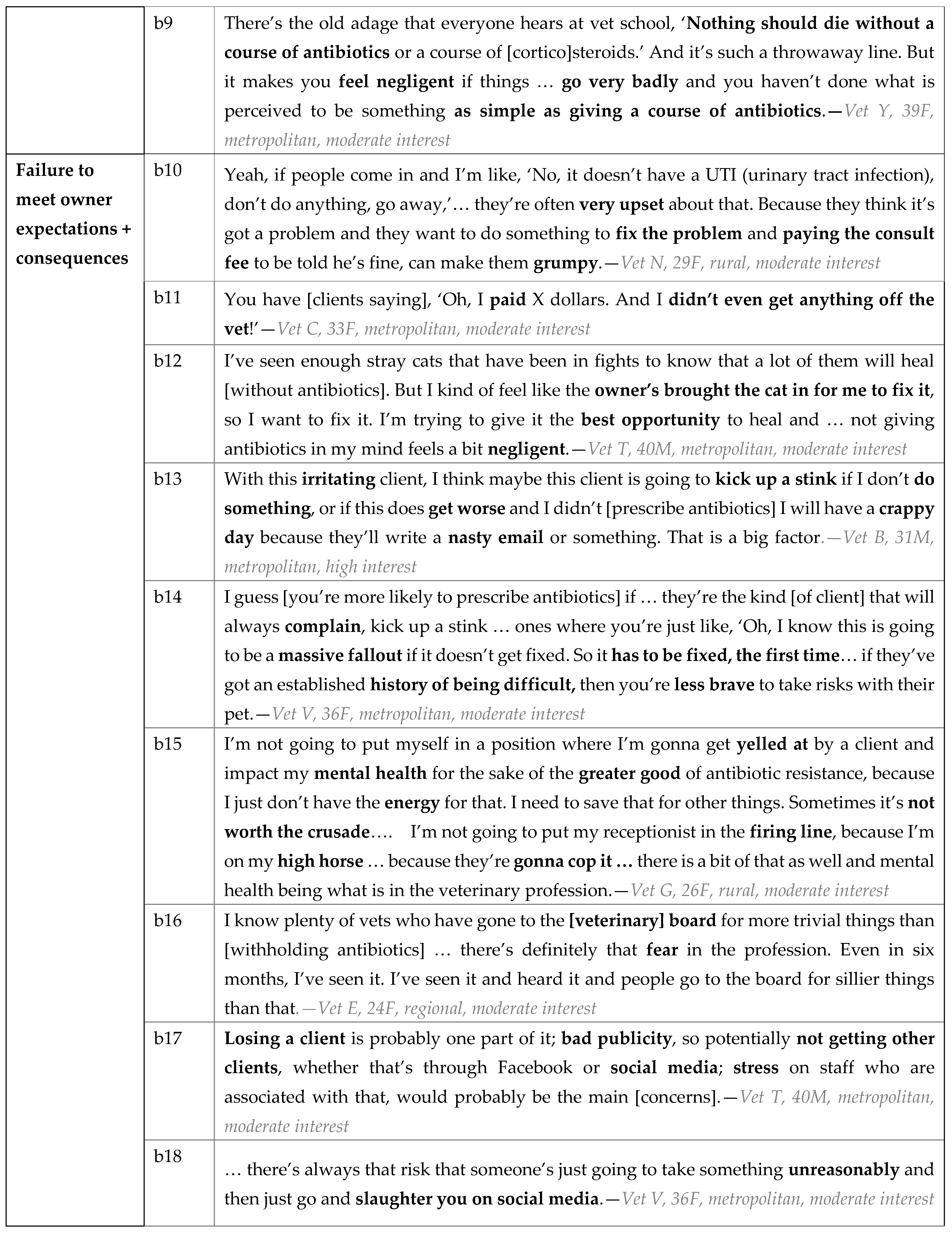
Codebook
| Background Factors | |
| Client factors | Including whether they have pet insurance, health literacy, attitudes, behaviour in consultation |
| Veterinarian’s clinical experience and confidence | Include communication skills |
| Veterinarian’s attitudes to antimicrobial use and AMR | How concerned do they feel? |
| Habits | |
| Veterinarians’ workload, energy, time | |
| Workplace factors | Including culture, policies and procedures, location |
| Other | |
| Behavioural beliefs | |
| Fear of clinical deterioration | Include downstream consequences |
| Fear of failing to meet client expectations | Include downstream consequences |
| Perceived impact of withholding antimicrobials | Will it make a difference? |
| Time and workflow issues | What are the alternatives to giving antimicrobials in this situation? What is the work impact of that? |
| Normative beliefs | |
| Employer and colleagues | Expectations regarding antimicrobial use, contribution to practice profit, etc. |
| Pet owner | E.g., pre-existing expectations of receiving antimicrobials, awareness of AMR |
| Veterinary Board | Potential for complaints and professional reprimand |
| Other | Undergraduate lecturers, etc. |
| Control beliefs | |
| Availability of non-antibiotic treatment options | e.g., probiotics |
| Client factors | Including capacity to undertake non-antimicrobial therapy, or to competently ‘watch and wait’ |
| Diagnostic uncertainty and action bias | Feeling that you need to ‘do something’ even if you don’t know what you’re treating |
| Time pressure | Include availability of para-veterinary staff |
| Veterinarians’ suggestions for improving antimicrobial use | |
| Veterinarian education and training | Webinars on antimicrobial use, communication skills |
| Para-veterinary staff education and training | Avoid setting client expectations of antimicrobials, enable non-antimicrobial treatment options |
| Client education | Improved understanding of AMR |
| Workplace culture | |
| Informational resources | Prescribing guidelines, webinars, other |
| Audit and sanctions |
References
- McManus, M.C. Mechanisms of bacterial resistance to antimicrobial agents. Am. J. Health Syst. Pharm. 1997, 54, 1420–1433; quiz 1444–1426. [Google Scholar] [CrossRef] [PubMed]
- Lipsitch, M.; Samore, M.H. Antimicrobial use and antimicrobial resistance: A population perspective. Emerg. Infect. Dis. 2002, 8, 347–354. [Google Scholar] [CrossRef] [PubMed]
- Gibson, J.S.; Morton, J.M.; Cobbold, R.N.; Sidjabat, H.E.; Filippich, L.J.; Trott, D.J. Multidrug-resistant E. coli and enterobacter extraintestinal infection in 37 dogs. J. Vet. Intern. Med. 2008, 22, 844–850. [Google Scholar] [CrossRef] [PubMed]
- van Cleef, B.A.; van Benthem, B.H.; Verkade, E.J.; van Rijen, M.; Kluytmans-van den Bergh, M.F.; Schouls, L.M.; Duim, B.; Wagenaar, J.A.; Graveland, H.; Bos, M.E.; et al. Dynamics of methicillin-resistant Staphylococcus aureus and methicillin-susceptible Staphylococcus aureus carriage in pig farmers: A prospective cohort study. Clin. Microbiol. Infect. 2014, 20, O764–O771. [Google Scholar] [CrossRef]
- Bosch, T.; Verkade, E.; van Luit, M.; Landman, F.; Kluytmans, J.; Schouls, L.M. Transmission and persistence of livestock-associated methicillin-resistant Staphylococcus aureus among veterinarians and their household members. Appl. Environ. Microbiol. 2015, 81, 124–129. [Google Scholar] [CrossRef]
- Agga, G.E.; Cook, K.L.; Netthisinghe, A.M.P.; Gilfillen, R.A.; Woosley, P.B.; Sistani, K.R. Persistence of antibiotic resistance genes in beef cattle backgrounding environment over two years after cessation of operation. PLoS ONE 2019, 14, e0212510. [Google Scholar] [CrossRef]
- Pouwels, K.B.; Hopkins, S.; Llewelyn, M.J.; Walker, A.S.; McNulty, C.A.; Robotham, J.V. Duration of antibiotic treatment for common infections in English primary care: Cross sectional analysis and comparison with guidelines. BMJ 2019, 364, l440. [Google Scholar] [CrossRef]
- Weese, J.S.; Cruz, A. Retrospective study of perioperative antimicrobial use practices in horses undergoing elective arthroscopic surgery at a veterinary teaching hospital. Can. Vet. J. 2009, 50, 185–188. [Google Scholar]
- Hardefeldt, L.Y.; Browning, G.F.; Thursky, K.A.; Gilkerson, J.R.; Billman-Jacobe, H.; Stevenson, M.A.; Bailey, K.E. Cross-sectional study of antimicrobials used for surgical prophylaxis by bovine veterinary practitioners in Australia. Vet. Rec. 2017, 181, 426. [Google Scholar] [CrossRef]
- Vaughn, V.M.; Flanders, S.A.; Snyder, A.; Conlon, A.; Rogers, M.A.M.; Malani, A.N.; McLaughlin, E.; Bloemers, S.; Srinivasan, A.; Nagel, J.; et al. Excess antibiotic treatment duration and adverse events in patients hospitalized with pneumonia: A multihospital cohort study. Ann. Intern. Med. 2019, 171, 153–163. [Google Scholar] [CrossRef]
- Touboul-Lundgren, P.; Jensen, S.; Drai, J.; Lindbaek, M. Identification of cultural determinants of antibiotic use cited in primary care in Europe: A mixed research synthesis study of integrated design “Culture is all around us”. BMC Public Health 2015, 15, 908. [Google Scholar] [CrossRef] [PubMed]
- Currie, K.; King, C.; Nuttall, T.; Smith, M.; Flowers, P. Expert consensus regarding drivers of antimicrobial stewardship in companion animal veterinary practice: A Delphi study. Vet. Rec. 2018, 182, 691. [Google Scholar] [CrossRef]
- Servia-Dopazo, M.; Taracido-Trunk, M.; Figueiras, A. Non-Clinical Factors Determining the Prescription of Antibiotics by Veterinarians: A Systematic Review. Antibiotics 2021, 10, 133. [Google Scholar] [CrossRef] [PubMed]
- Degeling, C.; Rock, M. Qualitative research for One Health: From methodological principles to impactful applications. Front. Vet. Sci. 2020, 7, 70. [Google Scholar] [CrossRef] [PubMed]
- Mateus, A.L.; Brodbelt, D.C.; Barber, N.; Stark, K.D. Qualitative study of factors associated with antimicrobial usage in seven small animal veterinary practices in the UK. Prev. Vet. Med. 2014, 117, 68–78. [Google Scholar] [CrossRef] [PubMed]
- King, C.; Smith, M.; Currie, K.; Dickson, A.; Smith, F.; Davis, M.; Flowers, P. Exploring the behavioural drivers of veterinary surgeon antibiotic prescribing: A qualitative study of companion animal veterinary surgeons in the UK. BMC Vet. Res. 2018, 14, 332. [Google Scholar] [CrossRef]
- Smith, M.; King, C.; Davis, M.; Dickson, A.; Park, J.; Smith, F.; Currie, K.; Flowers, P. Pet owner and vet interactions: Exploring the drivers of AMR. Antimicrob. Resist. Infect. Control. 2018, 7, 46. [Google Scholar] [CrossRef]
- Tompson, A.C.; Chandler, C.I.R.; Mateus, A.L.P.; O’Neill, D.G.; Chang, Y.M.; Brodbelt, D.C. What drives antimicrobial prescribing for companion animals? A mixed-methods study of UK veterinary clinics. Prev. Vet. Med. 2020, 183, 105117. [Google Scholar] [CrossRef]
- Hopman, N.E.M.; Hulscher, M.E.J.L.; Graveland, H.; Speksnijder, D.C.; Wagenaar, J.A.; Broens, E.M. Factors influencing antimicrobial prescribing by Dutch companion animal veterinarians: A qualitative study. Prev. Vet. Med. 2018, 158, 106–113. [Google Scholar] [CrossRef]
- Business Wire. UK Pet Insurance Market 2019: Consumer Research Report. Available online: https://www.businesswire.com/news/home/20190910005520/en/United-Kingdom-Pet-Insurance-Market-2019-Consumer-Research-Report---ResearchAndMarkets.com (accessed on 25 May 2022).
- Engel, P.; Mihm, U. Six Things You Need to Know about Pet Insurance. Available online: https://www.choice.com.au/money/insurance/pet/articles/six-things-you-need-to-know-about-pet-insurance (accessed on 21 June 2022).
- Hardefeldt, L.Y.; Gilkerson, J.R.; Billman-Jacobe, H.; Stevenson, M.A.; Thursky, K.; Bailey, K.E.; Browning, G.F. Barriers to and enablers of implementing antimicrobial stewardship programs in veterinary practices. J. Vet. Intern. Med. 2018, 32, 1092–1099. [Google Scholar] [CrossRef]
- Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Warreman, E.B.; Lambregts, M.M.C.; Wouters, R.H.P.; Visser, L.G.; Staats, H.; van Dijk, E.; de Boer, M.G.J. Determinants of in-hospital antibiotic prescription behaviour: A systematic review and formation of a comprehensive framework. Clin. Microbiol. Infect. 2019, 25, 538–545. [Google Scholar] [CrossRef]
- Walker, A.E.; Grimshaw, J.M.; Armstrong, E.M. Salient beliefs and intentions to prescribe antibiotics for patients with a sore throat. Br. J. Health Psychol. 2001, 6, 347–360. [Google Scholar] [CrossRef] [PubMed]
- Sable, M.R.; Schwartz, L.R.; Kelly, P.J.; Lisbon, E.; Hall, M.A. Using the theory of reasoned action to explain physician intention to prescribe emergency contraception. Perspect. Sex. Reprod. Health 2006, 38, 20–27. [Google Scholar] [CrossRef] [PubMed]
- Rashidian, A.; Russell, I. General practitioners’ intentions and prescribing for asthma: Using the theory of planned behavior to explain guideline implementation. Int. J. Prev. Med. 2012, 3, 17–28. [Google Scholar] [PubMed]
- Talkhan, H.; Stewart, D.; McIntosh, T.; Ziglam, H.; Abdulrouf, P.V.; Al-Hail, M.; Diab, M.; Cunningham, S. The use of theory in the development and evaluation of behaviour change interventions to improve antimicrobial prescribing: A systematic review. J. Antimicrob. Chemother. 2020, 75, 2394–2410. [Google Scholar] [CrossRef]
- Alradini, F.; Bepari, A.; AlNasser, B.H.; AlGheshem, E.F.; AlGhamdi, W.K. Perceptions of primary health care physicians about the prescription of antibiotics in Saudi Arabia: Based on the model of Theory of planned behaviour. Saudi Pharm. J. 2021, 29, 1416–1425. [Google Scholar] [CrossRef]
- Ajzen, I. The theory of planned behaviour: Reactions and reflections. Psychol. Health 2011, 26, 1113–1127. [Google Scholar] [CrossRef]
- Zhuo, A.; Labbate, M.; Norris, J.M.; Gilbert, G.L.; Ward, M.P.; Bajorek, B.V.; Degeling, C.; Rowbotham, S.J.; Dawson, A.; Nguyen, K.A.; et al. Opportunities and challenges to improving antibiotic prescribing practices through a One Health approach: Results of a comparative survey of doctors, dentists and veterinarians in Australia. BMJ Open 2018, 8, e020439. [Google Scholar] [CrossRef]
- Jernberg, C.; Lofmark, S.; Edlund, C.; Jansson, J.K. Long-term ecological impacts of antibiotic administration on the human intestinal microbiota. ISME J. 2007, 1, 56–66. [Google Scholar] [CrossRef]
- Crespo-Piazuelo, D.; Lawlor, P.G. Livestock-associated methicillin-resistant Staphylococcus aureus (LA-MRSA) prevalence in humans in close contact with animals and measures to reduce on-farm colonisation. Ir. Vet. J. 2021, 74, 21. [Google Scholar] [CrossRef] [PubMed]
- Scarborough, R.; Hardefeldt, L.; Browning, G.; Bailey, K. Pet Owners and Antibiotics: Knowledge, Opinions, Expectations, and Communication Preferences. Antibiotics 2021, 10, 1326. [Google Scholar] [CrossRef] [PubMed]
- Unterer, S.; Strohmeyer, K.; Kruse, B.D.; Sauter-Louis, C.; Hartmann, K. Treatment of aseptic dogs with hemorrhagic gastroenteritis with amoxicillin/clavulanic acid: A prospective blinded study. J. Vet. Intern. Med. 2011, 25, 973–979. [Google Scholar] [CrossRef] [PubMed]
- Australian Infectious Diseases Advisory Panel (AIDAP). Antibiotic Prescribing: Detailed Guidelines. Available online: https://animalmedicinesaustralia.org.au/wp-content/uploads/2019/11/AIDAP-Australian-Infectious-Diseases-Advisory-Panel-and-Antibiotic-Prescribing-Detailed-Guidelines-.pdf (accessed on 25 May 2022).
- British Small Animal Veterinary Association. PROTECT ME: BSAVA/SAMSoc Guide to Responsible Use of Antibacterials. Available online: https://www.bsavalibrary.com/content/chapter/10.22233/9781910443644.chap6_1 (accessed on 3 May 2022).
- Findlay, J. As Pet Ownership Skyrockets during Pandemic, a National Vet Shortage Puts Pressure on Clinics and Pets at Risk. Available online: https://www.abc.net.au/news/2020-12-26/vet-shortage-puts-pressure-on-clinics,-puts-pets-at-risk/13009562 (accessed on 25 May 2022).
- Rafferty, S. Shortage of Vets Nationally in ‘Demanding and Exhausting’ Job. Available online: https://www.abc.net.au/news/2021-05-10/vet-shortage-causing-exhaustion-prompts-cry-for-government-help/100121134 (accessed on 25 May 2022).
- Linder, J.A.; Doctor, J.N.; Friedberg, M.W.; Reyes Nieva, H.; Birks, C.; Meeker, D.; Fox, C.R. Time of day and the decision to prescribe antibiotics. JAMA Intern. Med. 2014, 174, 2029–2031. [Google Scholar] [CrossRef] [PubMed]
- The University of Melbourne. Australian Veterinary Prescribing Guidelines, Dogs and Cats (Version 2). Available online: https://vetantibiotics.fvas.unimelb.edu.au/about/resources (accessed on 25 May 2022).
- Bhattacharya, A.; Hopkins, S.; Sallis, A.; Budd, E.L.; Ashiru-Oredope, D. A process evaluation of the UK-wide Antibiotic Guardian campaign: Developing engagement on antimicrobial resistance. J. Public Health 2017, 39, e40–e47. [Google Scholar] [CrossRef]
- The University of Melbourne. Australian Veterinary Prescribing Guidelines, Dogs and Cats (Version 1). Available online: https://vetantibiotics.fvas.unimelb.edu.au (accessed on 19 June 2019).
- Pandolfo, A.M.; Horne, R.; Jani, Y.; Reader, T.W.; Bidad, N.; Brealey, D.; Enne, V.I.; Livermore, D.M.; Gant, V.; Brett, S.J.; et al. Understanding decisions about antibiotic prescribing in ICU: An application of the Necessity Concerns Framework. BMJ Qual. Saf. 2022, 31, 199–210. [Google Scholar] [CrossRef]
- Fletcher-Lartey, S.; Yee, M.; Gaarslev, C.; Khan, R. Why do general practitioners prescribe antibiotics for upper respiratory tract infections to meet patient expectations: A mixed methods study. BMJ Open 2016, 6, e012244. [Google Scholar] [CrossRef]
- Broom, A.; Kirby, E.; Gibson, A.F.; Post, J.J.; Broom, J. Myth, manners, and medical ritual: Defensive medicine and the fetish of antibiotics. Qual. Health Res. 2017, 27, 1994–2005. [Google Scholar] [CrossRef]
- Charani, E.; Castro-Sanchez, E.; Sevdalis, N.; Kyratsis, Y.; Drumright, L.; Shah, N.; Holmes, A. Understanding the determinants of antimicrobial prescribing within hospitals: The role of “prescribing etiquette”. Clin. Infect. Dis. 2013, 57, 188–196. [Google Scholar] [CrossRef]
- Singleton, D.A.; Rayner, A.; Brant, B.; Smyth, S.; Noble, P.M.; Radford, A.D.; Pinchbeck, G.L. A randomised controlled trial to reduce highest priority critically important antimicrobial prescription in companion animals. Nat. Commun. 2021, 12, 1593. [Google Scholar] [CrossRef]
- Hardefeldt, L.Y.; Hur, B.; Richards, S.; Scarborough, R.; Browning, G.F.; Billman-Jacobe, H.; Gilkerson, J.R.; Ierardo, J.; Awad, M.; Chay, R.; et al. Antimicrobial stewardship in companion animal practice: An implementation trial in 135 general practice veterinary clinics. JAC Antimicrob. Resist. 2022, 4, dlac015. [Google Scholar] [CrossRef] [PubMed]
- Huibers, L.; Vestergaard, C.H.; Keizer, E.; Bech, B.H.; Bro, F.; Christensen, M.B. Variation of GP antibiotic prescribing tendency for contacts with out-of-hours primary care in Denmark—A cross-sectional register-based study. Scand. J. Prim. Health Care 2022, 40, 227–236. [Google Scholar] [CrossRef]
- Nixon, S.L.; Rose, L.; Muller, A.T. Efficacy of an orally administered anti-diarrheal probiotic paste (Pro-Kolin Advanced) in dogs with acute diarrhea: A randomized, placebo-controlled, double-blinded clinical study. J. Vet. Intern. Med. 2019, 33, 1286–1294. [Google Scholar] [CrossRef]
- Strumann, C.; Steinhaeuser, J.; Emcke, T.; Sonnichsen, A.; Goetz, K. Communication training and the prescribing pattern of antibiotic prescription in primary health care. PLoS ONE 2020, 15, e0233345. [Google Scholar] [CrossRef] [PubMed]
- Bradley, D.T.; Allen, S.E.; Quinn, H.; Bradley, B.; Dolan, M. Social norm feedback reduces primary care antibiotic prescribing in a regression discontinuity study. J. Antimicrob. Chemother. 2019, 74, 2797–2802. [Google Scholar] [CrossRef] [PubMed]
- Hallsworth, M.; Chadborn, T.; Sallis, A.; Sanders, M.; Berry, D.; Greaves, F.; Clements, L.; Davies, S.C. Provision of social norm feedback to high prescribers of antibiotics in general practice: A pragmatic national randomised controlled trial. Lancet 2016, 387, 1743–1752. [Google Scholar] [CrossRef] [PubMed]


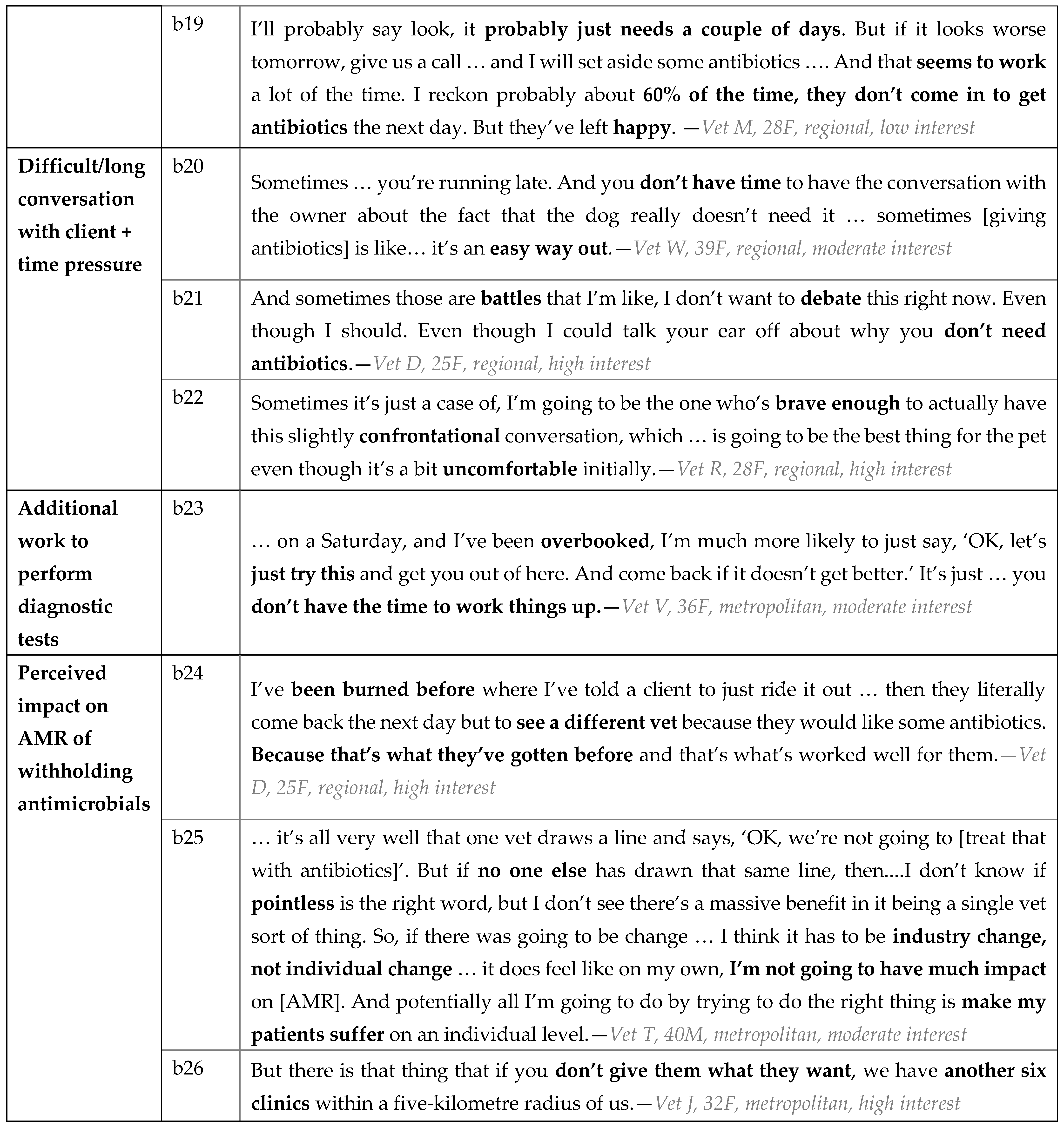
| Characteristic | Category | n | % |
|---|---|---|---|
| Gender | Female | 16 | 73% |
| Male | 6 | 27% | |
| Age | 20–29 | 6 | 27% |
| 30–39 | 10 | 45% | |
| 40–49 | 3 | 14% | |
| 50–59 | 1 | 5% | |
| 60–69 | 2 | 9% | |
| Postgraduate veterinary qualifications | Yes | 5 | 23% |
| No | 17 | 77% | |
| Role | Principal Veterinarian | 9 | 41% |
| Associate/Senior Associate | 10 | 45% | |
| Locum or other | 2 | 9% | |
| Practice location | Metropolitan | 10 | 45% |
| Regional | 9 | 41% | |
| Rural | 3 | 14% | |
| Practice type | Primary/emergency care only | 19 | 86% |
| Specialist/referral | 1 | 5% | |
| Combination of above | 2 | 9% | |
| Animals serviced | Small animals only | 19 | 86% |
| Mixed practice | 3 | 14% | |
| Size of practice (veterinary full-time equivalent staff) | 2 to 3 veterinary FTEs | 6 | 27% |
| 4 to 5 veterinary FTEs | 11 | 50% | |
| more than 5 veterinary FTEs | 5 | 23% | |
| State where practice is located | Victoria | 10 | 45% |
| New South Wales | 6 | 27% | |
| Queensland | 2 | 9% | |
| South Australia | 2 | 9% | |
| Tasmania | 1 | 5% | |
| Western Australia | 1 | 5% | |
| Self-reported interest in AMR and AMS | Low | 3 | 14% |
| Moderate | 9 | 41% | |
| High | 10 | 45% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scarborough, R.O.; Sri, A.E.; Browning, G.F.; Hardefeldt, L.Y.; Bailey, K.E. ‘Brave Enough’: A Qualitative Study of Veterinary Decisions to Withhold or Delay Antimicrobial Treatment in Pets. Antibiotics 2023, 12, 540. https://doi.org/10.3390/antibiotics12030540
Scarborough RO, Sri AE, Browning GF, Hardefeldt LY, Bailey KE. ‘Brave Enough’: A Qualitative Study of Veterinary Decisions to Withhold or Delay Antimicrobial Treatment in Pets. Antibiotics. 2023; 12(3):540. https://doi.org/10.3390/antibiotics12030540
Chicago/Turabian StyleScarborough, Ri O., Anna E. Sri, Glenn F. Browning, Laura Y. Hardefeldt, and Kirsten E. Bailey. 2023. "‘Brave Enough’: A Qualitative Study of Veterinary Decisions to Withhold or Delay Antimicrobial Treatment in Pets" Antibiotics 12, no. 3: 540. https://doi.org/10.3390/antibiotics12030540
APA StyleScarborough, R. O., Sri, A. E., Browning, G. F., Hardefeldt, L. Y., & Bailey, K. E. (2023). ‘Brave Enough’: A Qualitative Study of Veterinary Decisions to Withhold or Delay Antimicrobial Treatment in Pets. Antibiotics, 12(3), 540. https://doi.org/10.3390/antibiotics12030540







