Impact of a Pro-Active Infectious Disease Consultation on the Management of a Multidrug-Resistant Organisms Outbreak in a COVID-19 Hospital: A Three-Months Quasi-Experimental Study
Abstract
:1. Introduction
2. Methods
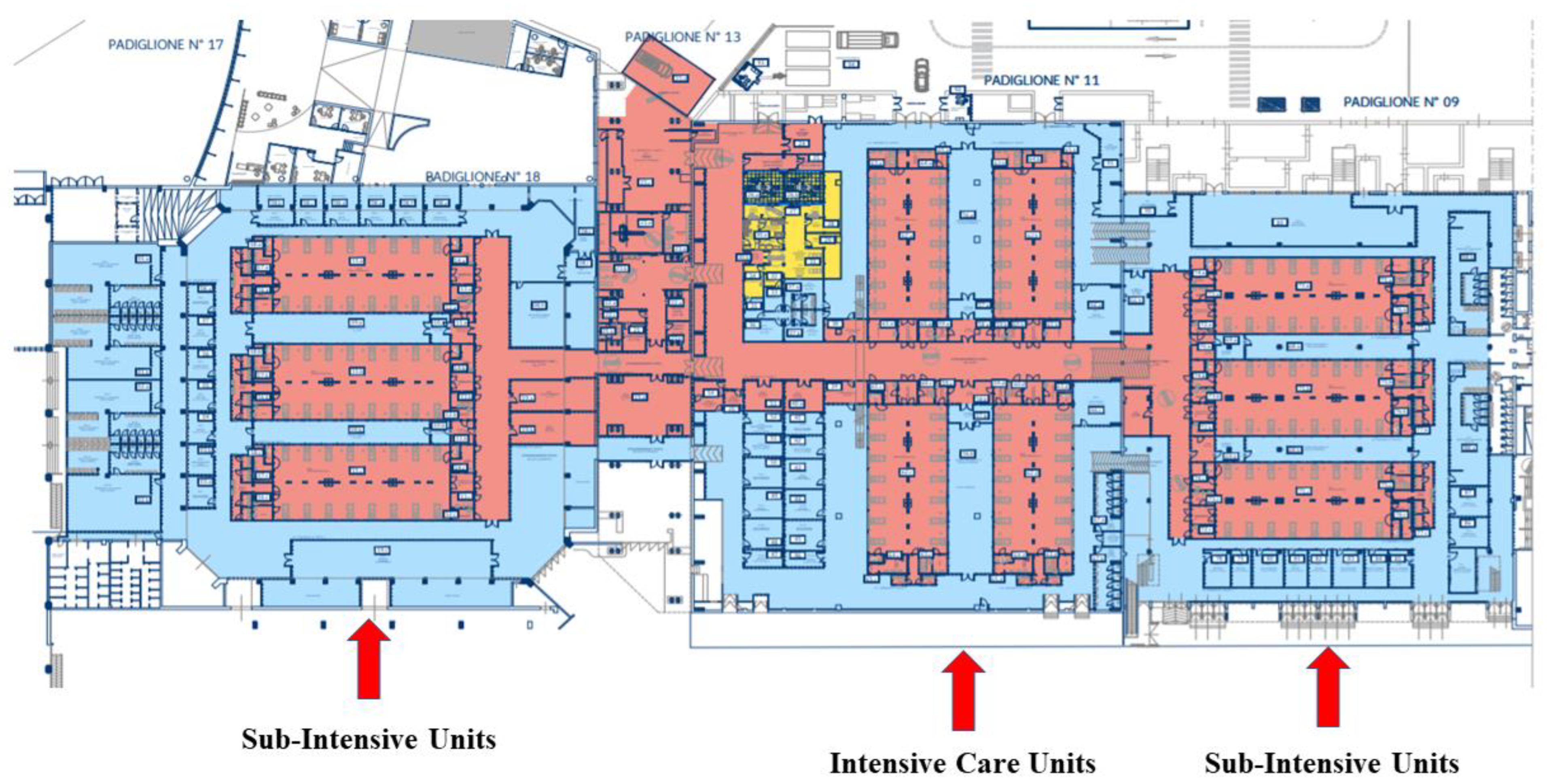
2.1. Study Setting
2.2. Study Design and Population
- -
- Bloodstream infections: presence of at least one blood culture positive for a Gram-negative bacteria, namely, S. aureus, Enterococcus spp., Streptococcus spp., or Candida spp.
- -
- Pneumonia: onset of new lung infiltrate associated with a worsening of respiratory function, fever and/or other systemic sign/symptoms, and a culture from the respiratory tract positive for a Gram-negative bacteria, namely, S. aureus or Aspergillus spp.
- -
- Urinary tract infections: fever and/or other systemic sign/symptoms (especially low urinary tract symptoms) without any other attributable cause excluding new positive urine culture for Gram-negative MDROs.
2.3. Intervention
- (1)
- Evaluation of the extent of the problem
- Molecular rectal swab for the detection of carbapenemase genes in all patients hospitalized in PME within 72 h from the start of the intervention. In detail, the presence of the bla genes in the carbapenemases, including KPC and NDM, was determined on isolates from rectal swab by polymerase chain reaction (PCR) using the GeneXpert® System (Cepheid). Whole genome sequencing and electrophoresis were not performed.
- Tracheal aspirate for culture test in all intubated patients.
- For patients with at least 3 episodes of diarrhea, the Clostridioides difficile test was provided in addition with stool culture.
- (2)
- Assessment of the nosocomial infection control procedures
- Contact isolation procedures (hand washing, use of protective personal equipment, and spatial isolation) and environmental cleaning practices.
- Prevention protocols of nosocomial infections, including ventilation-associated pneumonia, catheter-associated bloodstream infections, catheter-associated urinary tract infections, and general principles of antimicrobial stewardship, with a focus on the appropriateness of prescriptions and adequate duration of therapies.
- A specific discussion on the importance of appropriate treatment strategies of MDROs, including carbapenem-resistant A. baumannii (CRAB), carbapenem-resistant Klebsiella pneumoniae (CR-Kp), and carbapenem-resistant P. aeruginosa (CR-Pa), was had.
- (3)
- Targeted diagnostic–therapeutic interventions
- The screening of all patients for carbapenemase genes on a rectal swab at the admission, once a week during the hospital stay, and at discharge (if not performed in the previous 72 h). In contrast, rectal swabbing was not used for an already-known MDR-pathogen-colonized patient; they were considered colonized and managed with contact isolation procedures until the end of hospitalization.
- The following of empirical antibiotic therapy protocols for different sites of infection (pneumonia, central-line-associated BSI, and urinary tract) based on current international guidelines; protocol deviations were recorded.
- Identification of a reference person for the implementation of prevention protocols for each unit.
- The reporting of the number of colonizations and infections weekly.
- (4)
- Pro-active bedside evaluation of the patients
- -
- Antibiotics initiated without a clear suspicion/diagnosis of bacterial infection.
- -
- Antibiotics with documented inefficacy against the causative pathogen(s) for the index infection.
- -
- Antibiotics active against a wider spectrum of pathogen(s) than the one(s) isolated in the site of infection.
- -
- Antibiotics prescribed against an infection which occurred in a site where they poorly penetrate.
- -
- Antibiotics prescribed for a longer duration than what is needed to cure the infection.
- -
- Antibiotics prescribed in combination with other molecules with redundant spectra of activity.
2.4. Endpoints
2.5. Data Collection
2.6. Statistical Analyses
3. Results
3.1. General Characteristics of the Study Population
3.2. Infections and Antimicrobial Therapies
3.3. Description of Pro-Active IDs Consultation
3.4. Comparison of Outcomes between Pre- and Post-Phase
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ripa, M.; Galli, L.; Poli, A.; Oltolini, C.; Spagnuolo, V.; Mastrangelo, A.; Muccini, C.; Monti, G.; De Luca, G.; Landoni, G.; et al. Secondary infections in patients hospitalized with COVID-19: Incidence and predictive factors. Clin. Microbiol. Infect. 2021, 27, 451–457. [Google Scholar] [CrossRef] [PubMed]
- Segala, F.V.; Bavaro, D.F.; Di Gennaro, F.; Salvati, F.; Marotta, C.; Saracino, A.; Murri, R.; Fantoni, M. Impact of SARS-CoV-2 Epidemic on Antimicrobial Resistance: A Literature Review. Viruses 2021, 13, 2110. [Google Scholar] [CrossRef] [PubMed]
- Weiner-Lastinger, L.M.; Pattabiraman, V.; Konnor, R.Y.; Patel, P.R.; Wong, E.; Xu, S.Y.; Smith, B.; Edwards, J.R.; Dudeck, M.A. The impact of coronavirus disease 2019 (COVID-19) on healthcare-associated infections in 2020: A summary of data reported to the National Healthcare Safety Network. Infect. Control Hosp. Epidemiol. 2021, 43, 12–25. [Google Scholar] [CrossRef] [PubMed]
- Karruli, A.; Boccia, F.; Gagliardi, M.; Patauner, F.; Ursi, M.P.; Sommese, P.; De Rosa, R.; Murino, P.; Ruocco, G.; Corcione, A.; et al. Multidrug-Resistant Infections and Outcome of Critically Ill Patients with Coronavirus Disease 2019: A Single Center Experience. Microb. Drug Resist. 2021, 27, 1167–1175. [Google Scholar] [CrossRef]
- Ippolito, M.; Simone, B.; Filisina, C.; Catalanotto, F.R.; Catalisano, G.; Marino, C.; Misseri, G.; Giarratano, A.; Cortegiani, A. Bloodstream Infections in Hospitalized Patients with COVID-19: A Systematic Review and Meta-Analysis. Microorganisms 2021, 9, 2016. [Google Scholar] [CrossRef]
- Khatri, A.; Malhotra, P.; Izard, S.; Kim, A.; Oppenheim, M.; Gautam-Goyal, P.; Chen, T.; Doan, T.-L.; Berlinrut, I.; Niknam, N.; et al. Hospital-Acquired Bloodstream Infections in Patients Hospitalized with Severe Acute Respiratory Syndrome Coronavirus 2 Infection (Coronavirus Disease 2019): Association with Immunosuppressive Therapies. Open Forum Infect. Dis. 2021, 8, ofab339. [Google Scholar] [CrossRef]
- Pontefract, B.A.; Ho, H.T.; Crain, A.; Kharel, M.K.; Nybo, S.E. Drugs for Gram-Negative Bugs from 2010–2019: A Decade in Review. Open Forum Infect. Dis. 2020, 7, ofaa276. [Google Scholar] [CrossRef] [PubMed]
- Bavaro, D.; Belati, A.; Diella, L.; Stufano, M.; Romanelli, F.; Scalone, L.; Stolfa, S.; Ronga, L.; Maurmo, L.; Dell’Aera, M.; et al. Cefiderocol-Based Combination Therapy for “Difficult-to-Treat” Gram-Negative Severe Infections: Real-Life Case Series and Future Perspectives. Antibiotics 2021, 10, 652. [Google Scholar] [CrossRef]
- Belati, A.; Bavaro, D.F.; Diella, L.; De Gennaro, N.; Di Gennaro, F.; Saracino, A. Meropenem/Vaborbactam Plus Aztreonam as a Possible Treatment Strategy for Bloodstream Infections Caused by Ceftazidime/Avibactam-Resistant Klebsiella pneumoniae: A Retrospective Case Series and Literature Review. Antibiotics 2022, 11, 373. [Google Scholar] [CrossRef]
- Falcone, M.; Daikos, G.L.; Tiseo, G.; Bassoulis, D.; Giordano, C.; Galfo, V.; Leonildi, A.; Tagliaferri, E.; Barnini, S.; Sani, S.; et al. Efficacy of Ceftazidime-avibactam Plus Aztreonam in Patients with Bloodstream Infections Caused by Metallo-β-lactamase-Producing Enterobacterales. Clin. Infect. Dis. 2021, 72, 1871–1878. [Google Scholar] [CrossRef]
- Burnham, J.P.; Olsen, M.A.; Stwalley, D.; Kwon, J.H.; Babcock, H.M.; Kollef, M.H. Infectious Diseases Consultation Reduces 30-Day and 1-Year All-Cause Mortality for Multidrug-Resistant Organism Infections. Open Forum Infect. Dis. 2018, 5, ofy026. [Google Scholar] [CrossRef] [Green Version]
- Ramanathan, S.; Albarillo, F.S.; A Fitzpatrick, M.; Suda, K.J.; Poggensee, L.; Vivo, A.; Evans, M.E.; Jones, M.; Safdar, N.; Pfeiffer, C.; et al. Infectious Disease Consults of Pseudomonas aeruginosa Bloodstream Infection and Impact on Health Outcomes. Open Forum Infect. Dis. 2022, 9, ofac456. [Google Scholar] [CrossRef]
- Kim, I.; Kim, W.-Y.; Jeoung, E.S.; Lee, K. Current Status and Survival Impact of Infectious Disease Consultation for Multidrug-Resistant Bacteremia in Ventilated Patients: A Single-Center Experience in Korea. Acute Crit. Care 2018, 33, 73–82. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marschall, J.; Mermel, L.A.; Fakih, M.; Hadaway, L.; Kallen, A.; O’Grady, N.P.; Pettis, A.M.; Rupp, M.E.; Sandora, T.; Maragakis, L.L.; et al. Strategies to prevent central line–associated bloodstream infections in acute care hospitals: 2014 update. Infect. Control Hosp. Epidemiol. 2014, 35, 753–771. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gould, C.V.; Umscheid, C.A.; Agarwal, R.K.; Kuntz, G.; Pegues, D.A.; Healthcare Infection Control Practices Advisory Committee (HICPAC). Guideline for prevention of catheter-associated urinary tract infections 2009. Infect. Control Hosp. Epidemiol. 2010, 31, 319–326. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- American Thoracic Society; Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am. J. Respir. Crit. Care Med. 2005, 171, 388–416. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barlam, T.F.; Cosgrove, S.E.; Abbo, L.M.; MacDougall, C.; Schuetz, A.N.; Septimus, E.J.; Srinivasan, A.; Dellit, T.H.; Falck-Ytter, Y.T.; Fishman, N.O.; et al. Implementing an Antibiotic Stewardship Program: Guidelines by the INFECTIOUS Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin. Infect. Dis. 2016, 62, e51–e77. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Austin, P.C.; Stuart, E.A. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat. Med. 2015, 34, 3661–3679. [Google Scholar] [CrossRef] [Green Version]
- Chesdachai, S.; Kline, S.; Helmin, D.; Rajasingham, R. The Effect of Infectious Diseases Consultation on Mortality in Hospitalized Patients with Methicillin-Resistant Staphylococcus aureus, Candida, and Pseudomonas Bloodstream Infections. Open Forum Infect. Dis. 2020, 7, ofaa010. [Google Scholar] [CrossRef] [PubMed]
- Rieg, S.; Küpper, M.F. Infectious diseases consultations can make the difference: A brief review and a plea for more infectious diseases specialists in Germany. Infection 2016, 44, 159–166. [Google Scholar] [CrossRef]
- Jiménez-Aguilar, P.; López-Cortés, L.E.; Rodríguez-Baño, J. Impact of infectious diseases consultation on the outcome of patients with bacteremia. Ther. Adv. Infect. Dis. 2019, 6, 2049936119893576. [Google Scholar] [PubMed] [Green Version]
- Hasegawa, S.; Kakiuchi, S.; Tholany, J.; Kobayashi, T.; Marra, A.R.; Schweizer, M.L.; Samuelson, R.J.; Suzuki, H. Impact of infectious diseases consultation among patients with infections caused by gram-negative rod bacteria: A systematic literature review and meta-analysis. Infect. Dis. 2022, 54, 618–621. [Google Scholar] [CrossRef] [PubMed]
- Tang, G.; Huang, L.; Zong, Z. Impact of Infectious Disease Consultation on Clinical Management and Outcome of Patients with Bloodstream Infection: A Retrospective Cohort Study. Sci. Rep. 2017, 7, 12898. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spec, A.; Olsen, M.A.; Raval, K.; Powderly, W.G. Impact of Infectious Diseases Consultation on Mortality of Cryptococcal Infection in Patients without HIV. Clin. Infect. Dis. 2017, 64, 558–564. [Google Scholar] [CrossRef]
- Bavaro, D.F.; Pizzutilo, P.; Catino, A.; Signorile, F.; Pesola, F.; Di Gennaro, F.; Cassiano, S.; Marech, I.; Lamorgese, V.; Angarano, G.; et al. Incidence of Infections and Predictors of Mortality during Checkpoint Inhibitor Immunotherapy in Patients with Advanced Lung Cancer: A Retrospective Cohort Study. Open Forum Infect. Dis. 2021, 8, ofab187. [Google Scholar] [CrossRef]
- Viale, P.; Tedeschi, S.; Scudeller, L.; Attard, L.; Badia, L.; Bartoletti, M.; Cascavilla, A.; Cristini, F.; Dentale, N.; Fasulo, G.; et al. Infectious Diseases Team for the Early Management of Severe Sepsis and Septic Shock in the Emergency Department. Clin. Infect. Dis. 2017, 65, 1253–1259. [Google Scholar] [CrossRef]
- Erickson, R.M.; Tritle, B.J.; Spivak, E.S.; Timbrook, T.T. Impact of an Antimicrobial Stewardship Bundle for Uncomplicated Gram-Negative Bacteremia. Open Forum Infect. Dis. 2019, 6, ofz490. [Google Scholar] [CrossRef] [Green Version]
- Bavaro, D.F.; Diella, L.; Belati, A.; De Gennaro, N.; Fiordelisi, D.; Papagni, R.; Guido, G.; De Vita, E.; Frallonardo, L.; Camporeale, M.; et al. Impact of a Multistep Bundles Intervention in the Management and Outcome of Gram-Negative Bloodstream Infections: A Single-Center “Proof-of-Concept” Study. Open Forum Infect. Dis. 2022, 9, ofac488. [Google Scholar] [CrossRef]
- Rawson, T.M.; Moore, L.; Castro-Sanchez, E.; Charani, E.; Davies, F.; Satta, G.; Ellington, M.J.; Holmes, A.H. COVID-19 and the potential long-term impact on antimicrobial resistance. J. Antimicrob. Chemother. 2020, 75, 1681–1684. [Google Scholar] [CrossRef]
- Di Gennaro, F.; Marotta, C.; Amicone, M.; Bavaro, D.; Bernaudo, F.; Frisicale, E.; Kurotschka, P.K.; Mazzari, A.; Veronese, N.; Murri, R.; et al. Italian young doctors’ knowledge, attitudes and practices on antibiotic use and resistance: A national cross-sectional survey. J. Glob. Antimicrob. Resist. 2020, 23, 167–173. [Google Scholar] [CrossRef]


| Overall (n. 134) | Pre-Phase (n. 89) | Post-Phase (n. 45) | p Value | |
|---|---|---|---|---|
| Age (y), median (q1–q3) | 66 (58–73) | 66 (57–73) | 66 (61–73) | 0.787 |
| Male sex, n. (%) | 92 (69) | 60 (67) | 32 (71) | 0.663 |
| Charlson Comorbidity Index, median (q1–q3) | 5 (3–7) | 5 (3–7) | 5 (4–7) | 0.915 |
| Severe COVID-19 (requiring intubation), n. (%) | 60 (44) | 35 (39) | 25 (56) | 0.074 |
| Ward of evaluation, n. (%) | ||||
| Non-Intensive Care Units | 40 (30) | 25 (28) | 15 (33) | 0.531 |
| Intensive Care Units | 94 (70) | 64 (72) | 30 (67) | |
| Infectious condition at the time of enrollment, n (%) | ||||
| No secondary infections/colonizations | 56 (42) | 52 (59) | 4 (9) | <0.001 |
| Colonized by MDROs | 24 (18) | 10 (11) | 14 (31) | <0.001 |
| With a secondary Infection (+/− Colonization) | 53 (40) | 26 (30) | 27 (60) | <0.001 |
| Type of MDROs Colonization(s) | (n. 67) | (n. 33) | (n.34) | |
| Carbapenem-resistant A.baumannii | 46 (69) | 26 (79) | 20 (59) | 0.078 |
| KPC-Kp | 33 (49) | 13 (39) | 20 (59) | 0.112 |
| NDM-Kp | 3 (5) | 1 (3) | 2 (6) | 0.573 |
| Overall (n. 53) | Pre-Phase (n. 26) | Post-Phase (n. 27) | p Value | |
|---|---|---|---|---|
| Source of Secondary Infection, n (%) | ||||
| Lung | 10 (19) | 7 (27) | 3 (11) | 0.225 |
| Bloodstream | 36 (68) | 17 (65) | 19 (70) | |
| Urinary Tract | 7 (13) | 2 (8) | 5 (19) | |
| Monomicrobial infection, n (%) | 38 (72) | 23 (88) | 15 (56) | 0.007 |
| Polymicrobial/multiple infections, n (%) | 9 (18) | 3 (12) | 12 (44) | |
| Etiological agent(s), n (%) | ||||
| Carbapenem-resistant A. baumannii | 22 (47) | 14 (54) | 8 (38) | 0.282 |
| KPC-Kp | 8 (17) | 1 (4) | 7 (33) | 0.007 |
| Other GNB | 9 (19) | 5 (19) | 4 (19) | 0.987 |
| Enterococcus spp. | 9 (19) | 5 (19) | 4 (19) | 0.987 |
| CVC-related CoNS | 2 (4) | 2 (8) | 0 | 0.194 |
| Fungi * | 5 (10) | 0 | 5 (19) | 0.020 |
| Other Gram positive ** | 2 (4) | 2 (8) | 0 | 0.194 |
| Empirical antibiotic regimens prescribed before IDs consultation, n (%) | n. 60 | n.24 | n.36 | |
| Carbapenems | 48 (79) | 21 (87) | 27 (73) | 0.176 |
| Beta lactams | 11 (18) | 3 (12) | 8 (22) | 0.365 |
| Glycopeptides | 8 (13) | 2 (8) | 6 (16) | 0.373 |
| Lipopeptides | 12 (20) | 6 (25) | 6 (16) | 0.399 |
| Colistin | 28 (46) | 17 (71) | 11 (30) | 0.002 |
| Fosfomycin | 7 (11) | 3 (12) | 4 (11) | 0.840 |
| Linezolid | 10 (16) | 2 (8) | 8 (22) | 0.171 |
| Antifungal Agents | 10 (17) | 3 (12) | 7 (19) | 0.508 |
| Other Agents | 5 (8) | 1 (4) | 4 (11) | 0.379 |
| Pro-Active IDs Team Interventions, n (%) * | |
|---|---|
| Antimicrobial Stewardship | |
| Initiation/improvement of antibiotic therapy | 15 (33) |
| De-escalation to narrow spectrum | 11 (24) |
| De-escalation to less toxic drugs | 9 (20) |
| Discontinuation of antibiotics | 29 (64) |
| Diagnostic Stewardship | |
| Request of Microbiologic Tests | 37 (82) |
| Request of Instrumental Tests | 7 (16) |
| Univariate Analysis | Multivariate Analysis | |||||
|---|---|---|---|---|---|---|
| HR | 95%CI | p Value | aHR | 95%CI | p Value | |
| Age, per 1 year increase | 1.07 | 1.03–1.11 | <0.001 | 1.08 | 1.03–1.13 | <0.001 |
| Male sex | 1.15 | 0.53–2.51 | 0.709 | 1.20 | 0.51–2.81 | 0.663 |
| Severe COVID-19 (requiring intubation) | 1.20 | 0.59–2.43 | 0.604 | 1.50 | 0.61–3.65 | 0.371 |
| Ward of evaluation | ||||||
| Non-Intensive Care Units | 1 | \ | ||||
| Intensive Care Units | 0.64 | 0.31–1.32 | 0.235 | \ | ||
| Colonization by Carbapenem-resistant A.baumannii | 0.63 | 0.28–1.41 | 0.263 | \ | ||
| Colonization by KPC-Kp | 1.04 | 0.46–2.34 | 0.907 | \ | ||
| Source of Infection | ||||||
| Colonization only | 1 | 1 | ||||
| Bloodstream | 1.33 | 0.61–2.92 | 0.465 | 1.45 | 0.49–4.28 | 0.492 |
| Others (lung, urinary tract) | 1.08 | 0.36–3.23 | 0.880 | 0.81 | 0.19–3.43 | 0.781 |
| Type of Infection | ||||||
| Monomicrobial infection | 1 | \ | ||||
| Polymicrobial/multiple infections | 1.53 | 0.41–5.66 | 0.522 | \ | ||
| Etiological agent(s), n (%) | ||||||
| Carbapenem-resistant A.baumannii | 1.96 | 0.88–4.40 | 0.099 | 1.65 | 0.48–5.65 | 0.424 |
| KPC-Kp | 0.51 | 0.07–3.76 | 0.512 | 0.49 | 0.05–4.33 | 0.526 |
| Other GNB | 0.87 | 0.20–3.66 | 0.855 | \ | ||
| Enterococcus spp. | 0.41 | 0.05–3.03 | 0.385 | \ | ||
| CVC-related CoNS | 2.18 | 0.29–16.04 | 0.442 | \ | ||
| Fungi | 2.52 | 0.60–10.61 | 0.206 | \ | ||
| Attendance in the post-phase | 0.34 | 0.13–0.89 | 0.029 | 0.31 | 0.10–0.92 | 0.035 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bavaro, D.F.; De Gennaro, N.; Belati, A.; Diella, L.; Papagni, R.; Frallonardo, L.; Camporeale, M.; Guido, G.; Pellegrino, C.; Marrone, M.; et al. Impact of a Pro-Active Infectious Disease Consultation on the Management of a Multidrug-Resistant Organisms Outbreak in a COVID-19 Hospital: A Three-Months Quasi-Experimental Study. Antibiotics 2023, 12, 712. https://doi.org/10.3390/antibiotics12040712
Bavaro DF, De Gennaro N, Belati A, Diella L, Papagni R, Frallonardo L, Camporeale M, Guido G, Pellegrino C, Marrone M, et al. Impact of a Pro-Active Infectious Disease Consultation on the Management of a Multidrug-Resistant Organisms Outbreak in a COVID-19 Hospital: A Three-Months Quasi-Experimental Study. Antibiotics. 2023; 12(4):712. https://doi.org/10.3390/antibiotics12040712
Chicago/Turabian StyleBavaro, Davide Fiore, Nicolò De Gennaro, Alessandra Belati, Lucia Diella, Roberta Papagni, Luisa Frallonardo, Michele Camporeale, Giacomo Guido, Carmen Pellegrino, Maricla Marrone, and et al. 2023. "Impact of a Pro-Active Infectious Disease Consultation on the Management of a Multidrug-Resistant Organisms Outbreak in a COVID-19 Hospital: A Three-Months Quasi-Experimental Study" Antibiotics 12, no. 4: 712. https://doi.org/10.3390/antibiotics12040712
APA StyleBavaro, D. F., De Gennaro, N., Belati, A., Diella, L., Papagni, R., Frallonardo, L., Camporeale, M., Guido, G., Pellegrino, C., Marrone, M., Dell’Erba, A., Gesualdo, L., Brienza, N., Grasso, S., Columbo, G., Moschetta, A., Carpagnano, G. E., Daleno, A., Minicucci, A. M., ... Saracino, A. (2023). Impact of a Pro-Active Infectious Disease Consultation on the Management of a Multidrug-Resistant Organisms Outbreak in a COVID-19 Hospital: A Three-Months Quasi-Experimental Study. Antibiotics, 12(4), 712. https://doi.org/10.3390/antibiotics12040712








