Addressing Consumer Misconceptions on Antibiotic Use and Resistance in the Context of Sore Throat: Learnings from Social Media Listening
Abstract
1. Introduction
2. Results
2.1. Consumer Profiles and Associated Misconceptions around Antibiotic Use in Sore Throat
2.2. Impact of COVID-19 on the Sore Throat AMR Conversation
2.3. Impact of COVID-19 on Patient Response to Early Sore Throat Symptoms
3. Discussion
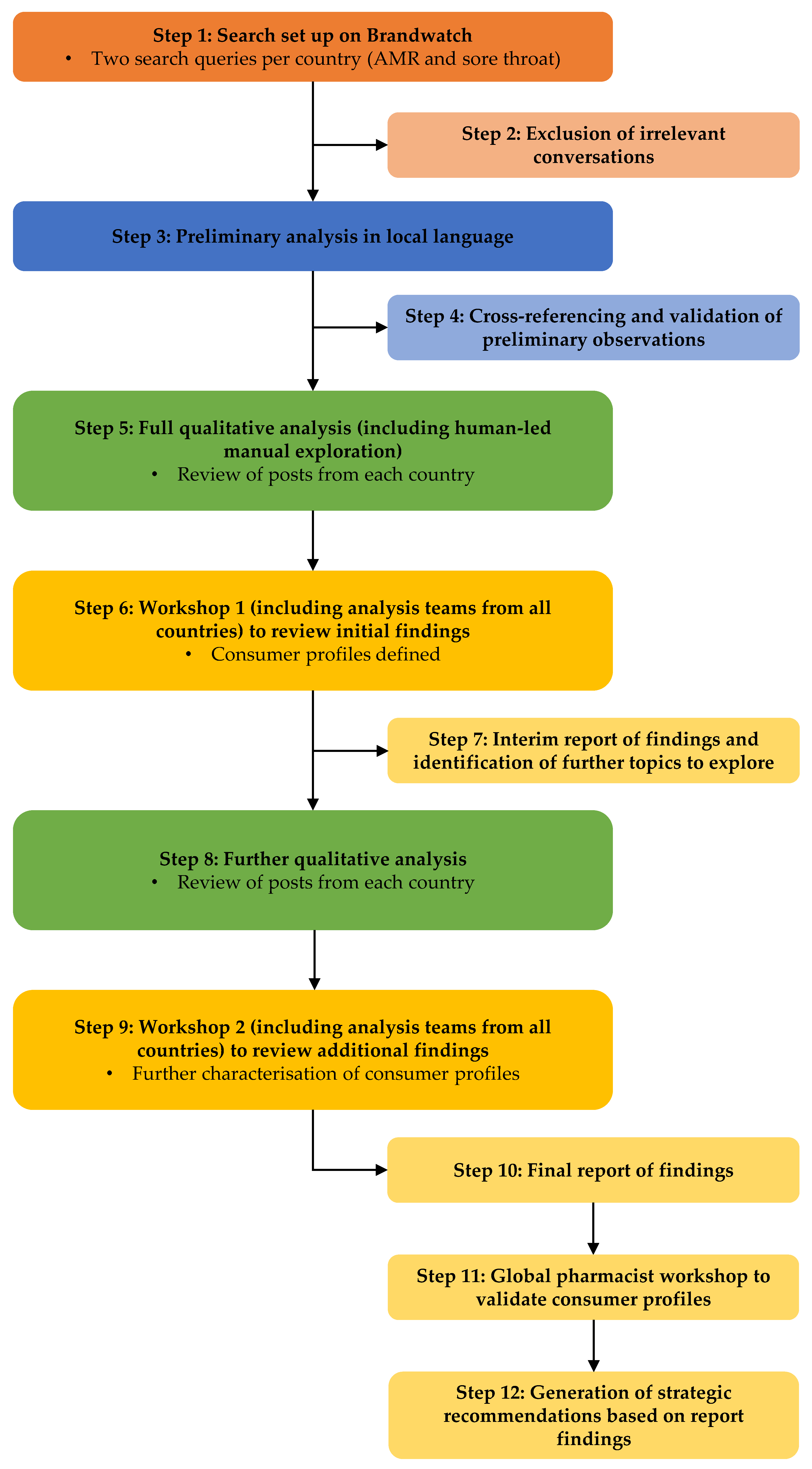
4. Materials and Methods
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Prestinaci, F.; Pezzotti, P.; Pantosti, A. Antimicrobial resistance: A global multifaceted phenomenon. Pathog. Glob. Health 2015, 109, 309–318. [Google Scholar] [CrossRef]
- World Health Organization. Antimicrobial Resistance: Key Facts. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance (accessed on 4 October 2022).
- Reygaert, W.C. An overview of the antimicrobial resistance mechanisms of bacteria. AIMS Microbiol. 2018, 4, 482–501. [Google Scholar] [CrossRef] [PubMed]
- Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. Lancet 2022, 399, 629–655. [Google Scholar] [CrossRef]
- Ventola, C.L. The antibiotic resistance crisis: Part 1: Causes and threats. P&T 2015, 40, 277–283. [Google Scholar]
- European Commission. Special Eurobarometer 522 Report Antimicrobial Resistance. 2022. Available online: https://www.eunews.it/wp-content/uploads/2022/11/Antimicrobial_Resistance_ebs_522_report_en.pdf (accessed on 8 December 2022).
- Centers for Disease Control and Prevention. Be Antibiotics Aware: Smart Use, Best Care. 2021. Available online: https://www.cdc.gov/patientsafety/features/be-antibiotics-aware.html (accessed on 24 January 2023).
- Mustafa, Z.; Ghaffari, M. Diagnostic methods, clinical guidelines, and antibiotic treatment for group A Streptococcal pharyngitis: A narrative review. Front. Cell Infect. Microbiol. 2020, 10, 563627. [Google Scholar] [CrossRef] [PubMed]
- Pouwels, K.B.; Dolk, F.C.K.; Smith, D.R.; Robotham, J.V.; Smieszek, T. Actual versus ‘ideal’ antibiotic prescribing for common conditions in English primary care. J. Antimicrob. Chemother. 2018, 73, 19–26. [Google Scholar] [CrossRef]
- World Health Organization. Antibiotic Resistance: Multi-Country Public Awareness Survey. 2015. Available online: https://apps.who.int/iris/bitstream/handle/10665/194460/9789241509817_eng.pdf (accessed on 9 November 2022).
- Cals, J.W.; Boumans, D.; Lardinois, R.J.; Gonzales, R.; Hopstaken, R.M.; Butler, C.C.; Dinant, G.J. Public beliefs on antibiotics and respiratory tract infections: An internet-based questionnaire study. Br. J. Gen. Pract. 2007, 57, 942–947. [Google Scholar] [CrossRef]
- Widayati, A.; Suryawati, S.; de Crespigny, C.; Hiller, J.E. Knowledge and beliefs about antibiotics among people in Yogyakarta City Indonesia: A cross sectional population-based survey. Antimicrob. Resist. Infect. Control 2012, 1, 38. [Google Scholar] [CrossRef]
- Gaarslev, C.; Yee, M.; Chan, G.; Fletcher-Lartey, S.; Khan, R. A mixed methods study to understand patient expectations for antibiotics for an upper respiratory tract infection. Antimicrob. Resist. Infect. Control 2016, 5, 39. [Google Scholar] [CrossRef]
- Davis, M.E.; Liu, T.L.; Taylor, Y.J.; Davidson, L.; Schmid, M.; Yates, T.; Scotton, J.; Spencer, M.D. Exploring patient awareness and perceptions of the appropriate use of antibiotics: A mixed-methods study. Antibiotics 2017, 6, 23. [Google Scholar] [CrossRef]
- Altiner, A.; Duerden, M.; Kozlov, R.; López-Pintor, E.; Sessa, A.; Shephard, A.; van der Velden, A.W. Understanding attitudes and perceptions of consumers in relation to antibiotic use for respiratory illnesses and symptoms in Europe. In Proceedings of the 33rd European Congress of Clinical Microbiology & Infectious Diseases (P2298), Copenhagen, Denmark, 15–18 April 2023. [Google Scholar]
- Bakhit, M.; Del Mar, C.; Gibson, E.; Hoffmann, T. Exploring patients’ understanding of antibiotic resistance and how this may influence attitudes towards antibiotic use for acute respiratory infections: A qualitative study in Australian general practice. BMJ Open 2019, 9, e026735. [Google Scholar] [CrossRef]
- Statista. Number of Social Media Users Worldwide from 2018 to 2027 (In Billions). 2023. Available online: https://www.statista.com/statistics/278414/number-of-worldwide-social-network-users/ (accessed on 10 November 2022).
- Gatewood, J.; Monks, S.L.; Singletary, C.R.; Vidrascu, E.; Moore, J.B. Social media in public health: Strategies to distill, package, and disseminate public health research. J. Public Health Manag. Pract. 2020, 26, 489–492. [Google Scholar] [CrossRef]
- Chen, J.; Wang, Y. Social media use for health purposes: Systematic review. J. Med. Internet Res. 2021, 23, e17917. [Google Scholar] [CrossRef]
- Kubheka, B.Z.; Carter, V.; Mwaura, J. Social media health promotion in South Africa: Opportunities and challenges. Afr. J. Prim. Health Care Fam. Med. 2020, 12, e1–e7. [Google Scholar] [CrossRef]
- Brandwatch. The Complete Social Listening Guide. 2022. Available online: https://www.brandwatch.com/blog/social-listening-guide/ (accessed on 8 December 2022).
- Stivers, T.; Timmermans, S. Arriving at no: Patient pressure to prescribe antibiotics and physicians’ responses. Soc. Sci. Med. 2021, 290, 114007. [Google Scholar] [CrossRef]
- Bagnulo, A.; Muñoz Sastre, M.T.; Kpanake, L.; Sorum, P.C.; Mullet, E. Why patients want to take or refuse to take antibiotics: An inventory of motives. BMC Public Health 2019, 19, 441. [Google Scholar] [CrossRef]
- Jha, A.; Lin, L.; Savoia, E. The use of social media by state health departments in the US: Analyzing health communication through Facebook. J. Community Health 2016, 41, 174–179. [Google Scholar] [CrossRef]
- Ranschaert, E.R.; Van Ooijen, P.M.; McGinty, G.B.; Parizel, P.M. Radiologists’ usage of social media: Results of the RANSOM survey. J. Digit. Imaging 2016, 29, 443–449. [Google Scholar] [CrossRef] [PubMed]
- Smailhodzic, E.; Hooijsma, W.; Boonstra, A.; Langley, D.J. Social media use in healthcare: A systematic review of effects on patients and on their relationship with healthcare professionals. BMC Health Serv. Res. 2016, 16, 442. [Google Scholar] [CrossRef]
- Twitter. Counting Characters. 2023. Available online: https://developer.twitter.com/en/docs/counting-characters (accessed on 10 January 2023).
- Elmahi OK, O.; Uakkas, S.; Olalekan, B.Y.; Damilola, I.A.; Adedeji, O.J.; Hasan, M.M.; Costa, A.C.S.; Ahmad, S.; Essar, M.Y.; Thomson, D.J. Antimicrobial resistance and one health in the post COVID-19 era: What should health students learn? Antimicrob. Resist. Infect. Control 2022, 11, 58. [Google Scholar] [CrossRef]
- Zucco, R.; Lavano, F.; Anfosso, R.; Bianco, A.; Pileggi, C.; Pavia, M. Internet and social media use for antibiotic-related information seeking: Findings from a survey among adult population in Italy. Int. J. Med. Inform. 2018, 111, 131–139. [Google Scholar] [CrossRef] [PubMed]
- Del Vicario, M.; Bessi, A.; Zollo, F.; Petroni, F.; Scala, A.; Caldarelli, G.; Stanley, H.E.; Quattrociocchi, W. The spreading of misinformation online. Proc. Natl. Acad. Sci. USA 2016, 113, 554–559. [Google Scholar] [CrossRef] [PubMed]
- Wolford, R.W.G.; Syed, A.B.; Schaefer, S.T.J. Pharyngitis. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Essack, S.; Bell, J.; Burgoyne, D.; Tongrod, W.; Duerden, M.; Sessa, A.; Altiner, A.; Shephard, A. Point-of-Care Testing for Pharyngitis in the Pharmacy. Antibiotics 2020, 9, 743. [Google Scholar] [CrossRef]
- Demoré, B.; Tebano, G.; Gravoulet, J.; Wilcke, C.; Ruspini, E.; Birgé, J.; Boivin, J.-M.; Hénard, S.; Dieterling, A.; Munerol, L.; et al. Rapid antigen test use for the management of group A streptococcal pharyngitis in community pharmacies. Eur. J. Clin. Microbiol. Infect. Dis. 2018, 37, 1637–1645. [Google Scholar] [CrossRef]
- Papastergiou, J.; Trieu, C.R.; Saltmarche, D.; Diamantouros, A. Community pharmacist-directed point-of-care group A Streptococcus testing: Evaluation of a Canadian program. J. Am. Pharm. Assoc. 2018, 58, 450–456. [Google Scholar] [CrossRef]
- Ogawa, T.; Terao, Y.; Sakata, H.; Okuni, H.; Ninomiya, K.; Ikebe, K.; Maeda, Y.; Kawabata, S. Epidemiological characterization of Streptococcus pyogenes isolated from patients with multiple onsets of pharyngitis. FEMS Microbiol. Lett. 2011, 318, 143–151. [Google Scholar] [CrossRef]
- Giovanetti, E.; Prenna, M.; Repetto, A.; Biavasco, F.; Romagnoli, M.; Ripa, S.; Varaldo, P.E. Susceptibility of Streptococcus pyogenes from throat cultures to macrolide antibiotics and influence of collection criteria. Clin. Microbiol. Infect. 1997, 3, 58–62. [Google Scholar] [CrossRef]
- Bayot, M.L.; Bragg, B.N. Antimicrobial Susceptibility Testing. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Jorgensen, J.H.; Ferraro, M.J. Antimicrobial susceptibility testing: A review of general principles and contemporary practices. Clin. Infect. Dis. 2009, 49, 1749–1755. [Google Scholar] [CrossRef]
- van Belkum, A.; Bachmann, T.T.; Lüdke, G.; Lisby, J.G.; Kahlmeter, G.; Mohess, A.; Becker, K.; Hays, J.P.; Woodford, N.; Mitsakakis, K.; et al. Developmental roadmap for antimicrobial susceptibility testing systems. Nat. Rev. Microbiol. 2019, 17, 51–62. [Google Scholar] [CrossRef]
| Country | Number of AMR Conversations | Number of Sore Throat Conversations |
|---|---|---|
| Germany | 125,000 | 447,000 |
| Italy | 196,000 | 339,000 |
| Spain and Mexico | 168,000 | 494,000 |
| Romania | 5000 | 20,000 |
| Russia | 102,000 | 816,000 |
| Brazil | 93,000 | 1,400,000 |
| Thailand | 73,000 | Data unavailable |
| Consumer Profiles | ||||
|---|---|---|---|---|
 | ||||
| Opposed to Antibiotics | In Favor of Antibiotics | |||
| Antibiotic-Preserving Peer Educators | Antibiotic-Cautious Consumers | Medication-Resistant Antibiotic Opponents | Believers in the Strength of Antibiotics | Determined Pro-Antibiotic Consumers |
| Antibiotic-preserving peer educators feel it is their duty to educate friends, family and acquaintances about the importance of following antibiotic prescriptions correctly, and of mitigating antibiotic resistance | Antibiotic-cautious consumers believe antibiotics are unnecessary for sore throat, driven by either explicit awareness of AMR or an implicit reluctance to take ‘hard’ medicine | Medication-resistant antibiotic opponents are opposed to antibiotics because of a reluctance towards taking medication, a preference for natural/holistic treatment, and even outright conspiracy in some instances | Believers in the strength of antibiotics are characterized by the opinion that antibiotics are a ‘strong’ medication, and they fundamentally do not make the viral/bacterial distinction | Determined pro-antibiotic consumers are convinced that their sore throat warrants antibiotic treatment and that, as a ‘strong medicine’, it will enable them to recover more quickly |
| Key Beliefs 1 | ||||
| “I need to educate my peers around how to use antibiotics appropriately” | “I don’t want antibiotics because they are unnecessary/this is contributing to AMR” | “I would always prefer natural/holistic treatments to antibiotics” | “I want antibiotics because they are a strong medication and I want to get better quickly” | “I should be prescribed antibiotics, but my doctor won’t give them to me” |
| “You should only take antibiotics if you have white plaques/a fever for more than three days/if your child also has ear pain or cough” | “I am annoyed because my doctor has prescribed me antibiotics unnecessarily” | “I don’t want to ‘catch’ AMR/I don’t want to make the bacteria in my system stronger” | ”Because my sore throat is getting worse, I am going to seek out and take antibiotics” | “I need antibiotics and have therefore got them directly from a pharmacy” |
| “Antibiotics should be prescribed by doctors and prescriptions should be followed thoroughly” | “Taking antibiotics for sore throat is dangerous and stupid” | “I don’t want antibiotics because they are harmful to my/my child’s immune system/they can cause side effects” | “I am dissatisfied about why antibiotics aren’t working for my sore throat, I thought they were a powerful medication” | “Of course, luckily enough we live in Romania where you can get antibiotics without a prescription” |
| Prevalence of Consumer Profiles | ||||
| ▲DE, ES, BR, TH, IT; ▼RU, RO | ▲DE, RU | ▲RU | Prevalent in all markets | ▲ES, RU, RO, TH, BR, MX; ▼DE, IT |
| Rank | Consumer Belief |
|---|---|
| 1 | People experiencing sore throat often alluded to the belief that antibiotics are strong medications, which are effective at treating all types of sore throat
|
| 2 | Some people experiencing sore throat express the belief that antibiotics will be able to help them recover from sore throat more quickly when compared with pharmacologic symptomatic relief or home remedies
|
| 3 | Some people experiencing sore throat discussed their fear that if they take too many antibiotics, or do not take them properly, they will ‘catch AMR’ or will personally become resistant to antibiotics |
| 4 | People experiencing sore throat also mention the belief that if they take too many antibiotics, or don’t take them properly, they will make the bacteria in their system stronger or create a ‘superbug’ in their body which will only affect them, rather than having an impact on the community |
| Misconception | Belief/Behavior Shift Required | Strategies to Address | |
|---|---|---|---|
| Misconceptions about antibiotic strength | “Antibiotics will help me to get better more quickly” “Antibiotics are strong medications which are more effective at treating my sore throat [regardless of whether it is viral or bacterial]” | Antibiotics are only effective for bacterial infections; their primary role is not to alleviate symptoms, but to kill bacteria Antibiotics are ineffective for viral infections—and therefore for most sore throat conditions [that are viral] Effective OTC products are available to manage the painful symptoms quickly, without the need for antibiotics | 1. ASK questions to understand where the patient is in their AMR journey and identify misconceptions they may have
|
| Misconceptions about antimicrobial resistance | “I’ve never used antibiotics so I can’t have resistant infections” “If I take too many antibiotics or don’t take them properly, I will ‘catch AMR’ or I will personally become resistant to antibiotics” | AMR is a public health issue and not only a personal issue Inappropriate use of antibiotics can lead to bacteria becoming resistant to antibiotics | 1.ASK questions to understand where the patient is in their AMR journey and identify misconceptions they may have
|
| Standalone Terms | Terminology Associated with Sore Throat | Anchored Terms of Descriptions of Sore Throat | Anchored Terms for Treatment | Anchored Terms: Conditions where Sore Throat Is a Symptom |
|---|---|---|---|---|
| “sore throat” OR sorethroat | “streptococcal infection” | anchor term: throat NEAR/3 | anchor term: throat NEAR/5 | anchor term: throat NEAR/5 |
| “soar throat” OR soarthroat | streptococcus | scratchy | Halls | “acid reflux” |
| “strep throat” | pharyngitis | dry | Riccola | COVID-19 |
| “throat pain” | laryngitis | irritated | Strepsils | COVID |
| “swollen glands” | tonsillitis OR tonsilitis | allergies | lozenge | Coronavirus |
| “throat relief” | “lost voice” | ibuprofen | flu * | |
| (lost OR lose OR losing) NEAR/1 voice | hoarseness | paracetamol | influenza | |
| “Centor score” OR “Centor test” OR “Centor criteria” | swell * OR swollen | nurofen | virus | |
| “FEVERPain” OR (FEVER NEAR/1 Pain) | hurt * | penicillin | “viral infection” | |
| “McIsaac score” OR “McIsaac test” | pain * | amoxicillin | “coronavirus symptoms” | |
| “strep test” OR “strep A test” | sore OR soar | Amoxil | “COVID symptoms” | |
| “throat swab” | itchy | cephalexin | “COVID-19 symptoms” | |
| throat NEAR/3 (“CRP test” OR “CRP level” OR “C-reactive protein”) | inflam * | Keflex | #COVID_19 | |
| discomfort | cefadroxil | #COVID-19 | ||
| uncomfortable | clindamycin | #COVID | ||
| “fxxxxd up” OR “is fxxxxd” | azithromycin | allergies | ||
| “killing me” | clarithromycin | allergy | ||
| “bothering me” | cephalosporin | mononucleosis | ||
| “can’t eat” OR “cannot eat” OR “difficulty eating” | tertracycline | mono | ||
| “can’t drink” OR “cannot drink” OR “difficulty drinking” | macrolide | mumps | ||
| fluoroquinolone | “gastroesophageal reflex disease” | |||
| glycopeptide | GERD | |||
| Mebucaina | streptococcal pharyngitis | |||
| tyrothricin OR Mybacin OR Anginovag | croup OR laryngotracheitis OR laryngotracheobronchitis | |||
| gramicidin OR grammicidin | sinusitis OR “sinus infection” | |||
| lemocin | rhinitis OR rhinosinusitis | |||
| dorithricin | “common cold” OR “a cold” | |||
| antibiotic * OR “anti B” OR “anti-B” OR “anti-B’s” OR “anti Bs” | infection OR infected | |||
| carbapenem | ||||
| methicillin | ||||
| vancomycin |
| Condition Terms | “Superbug“ Infection Terminology | Antiviral/Antifungal Resistance Terminology | Anchored Terms | Exclusions |
|---|---|---|---|---|
| “antimicrobial resistance” | “superbug” | anchor terms: (antiviral OR “anti-viral” OR antifungal OR “anti-fungal” OR Gocovri OR Symadine OR Symmetrel OR amantadine OR Flumavine OR rimantadine OR Tamiflu OR oseltamivir OR Relenza OR zanamivir) NEAR/3 | anchor terms: (antibiotic * OR “anti B” OR “anti-B” OR “anti-B’s” OR “anti Bs” OR penicillin OR amoxicillin OR Amoxil OR cephalexin OR Keflex OR cefadroxil OR clindamycin OR azithromycin OR clarithromycin OR cephalosporin * OR tertracycline * OR macrolide * OR fluoroquinolone * OR glycopeptide * OR tyrothricin OR Mybacin OR Anginovag OR gramicidin OR grammicidin OR lemocin OR dorithricin OR carbapenem OR methicillin OR vancomycin) NEAR/3 | “fossil fuel” |
| “antibiotic resistance” | “methicillin-resistant Staphylococcus aureus” | overuse * OR overprescribe * OR overprescription | “do not respond” OR “does not respond” | agriculture |
| “antibiotic addiction” | MRSA | “stop working” OR “stops working” OR “stopped working” | response | farming |
| “antibiotic resistant pathogens” | “Carbapenem-resistant Enterobacteriaceae” | “doesn’t work” OR “does not work” | resilient | animals |
| “multidrug-resistant bacterium” | CRE | resilience | climate | |
| AMR | “ESBL-producing Enterobacteriaceae” | “biothreat pathogens” | food | |
| “drug resistant” | “ESBL bacteria” | “health threat” | “food safety” | |
| “drug resistance” | “Vancomycin-resistant Enterococcus” | #onehealth | “food science” | |
| “when antibiotics fail” | VRE | #AntibioticStewardship | livestock | |
| “antibiotics overuse” | “Multidrug-resistant Pseudomonas aeruginosa” | abuse | “animal health” | |
| “World Antimicrobial Awareness Week” | MDR | resistance | “animal welfare” | |
| #WAAW | “Multidrug-resistant Acinetobacter” | virus | environment | |
| #AMR | “H30-Rx” | viral | environmental | |
| #AntimicrobialResistance | E. coli H30-Rx | coronavirus | “AMR Industry Alliance” | |
| superbug | flu | “American Medical Response” | ||
| #superbug | “the cold” | “Aston Martin Racing” | ||
| #AntibioticResistantInfections | “a cold” | “AMR Consultancy” | ||
| #EAAD | #ECDC | “European Alliance Against Depression” | ||
| “European Centre for Disease Prevention and Control” | pig * OR cow * OR cattle * | |||
| overuse * OR overprescribe * OR overprescription | ||||
| “stop working” OR “stops working” OR “stopped working” | ||||
| “doesn’t work” OR “does not work” |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Essack, S.; Bell, J.; Burgoyne, D.; Eljaaly, K.; Tongrod, W.; Markham, T.; Shephard, A.; López-Pintor, E. Addressing Consumer Misconceptions on Antibiotic Use and Resistance in the Context of Sore Throat: Learnings from Social Media Listening. Antibiotics 2023, 12, 957. https://doi.org/10.3390/antibiotics12060957
Essack S, Bell J, Burgoyne D, Eljaaly K, Tongrod W, Markham T, Shephard A, López-Pintor E. Addressing Consumer Misconceptions on Antibiotic Use and Resistance in the Context of Sore Throat: Learnings from Social Media Listening. Antibiotics. 2023; 12(6):957. https://doi.org/10.3390/antibiotics12060957
Chicago/Turabian StyleEssack, Sabiha, John Bell, Douglas Burgoyne, Khalid Eljaaly, Wirat Tongrod, Thomas Markham, Adrian Shephard, and Elsa López-Pintor. 2023. "Addressing Consumer Misconceptions on Antibiotic Use and Resistance in the Context of Sore Throat: Learnings from Social Media Listening" Antibiotics 12, no. 6: 957. https://doi.org/10.3390/antibiotics12060957
APA StyleEssack, S., Bell, J., Burgoyne, D., Eljaaly, K., Tongrod, W., Markham, T., Shephard, A., & López-Pintor, E. (2023). Addressing Consumer Misconceptions on Antibiotic Use and Resistance in the Context of Sore Throat: Learnings from Social Media Listening. Antibiotics, 12(6), 957. https://doi.org/10.3390/antibiotics12060957





