Impact of Menopausal Status and Recurrent UTIs on Symptoms, Severity, and Daily Life: Findings from an Online Survey of Women Reporting a Recent UTI
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants and Setting
2.3. Exposures and Outcomes
2.4. Analysis
3. Results
3.1. Menopausal Status and Self-Reported Symptoms
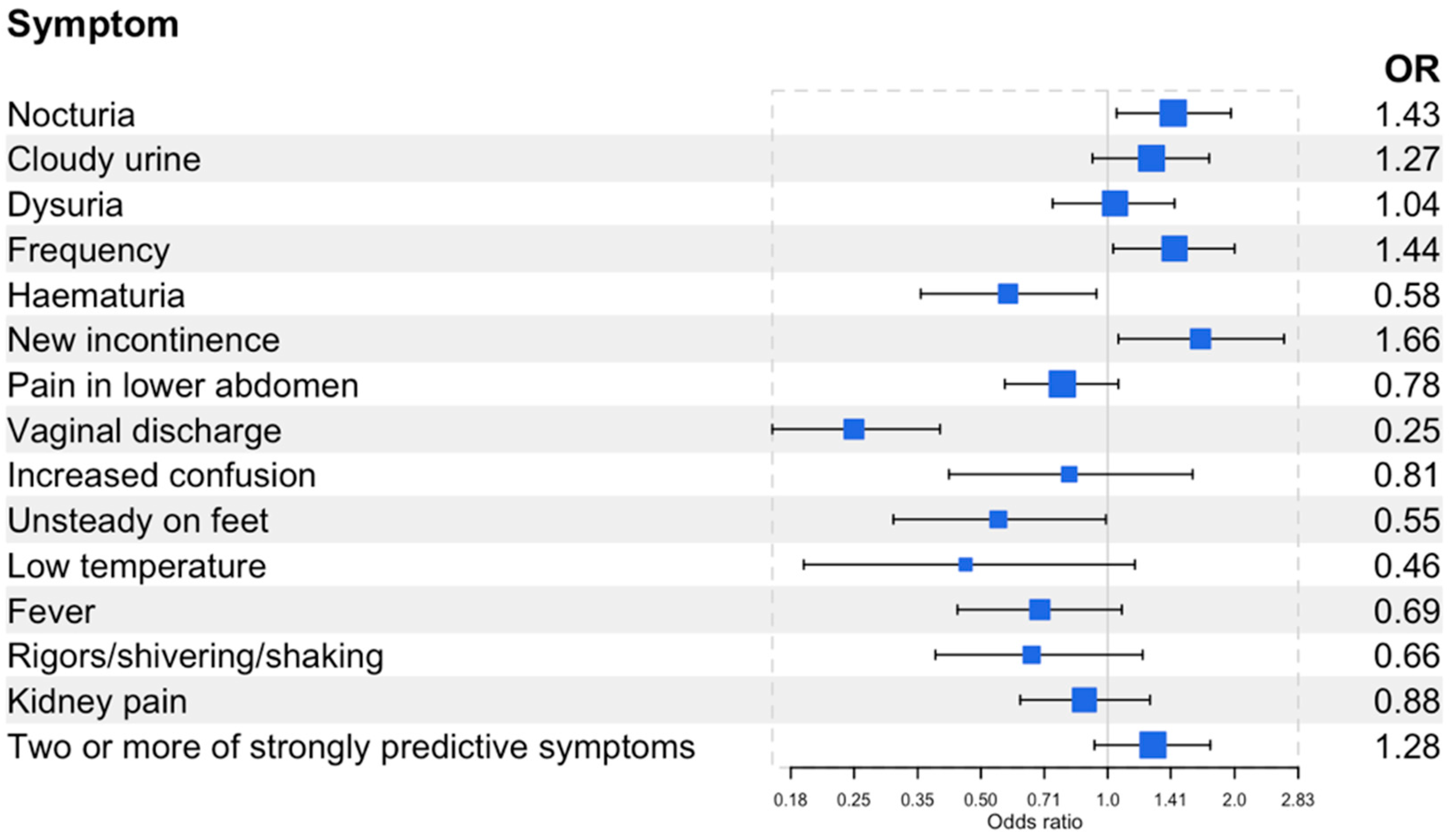
3.2. Recurrent UTIs and Self-Reported Symptoms
4. Discussion
4.1. Comparison with Existing Literature
4.2. Strengths and Limitations
4.3. Implications for Clinical Practice and Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Beerepoot, M.A.J.; Geerlings, S.E.; van Haarst, E.P.; Mensing Van Charante, N.; ter Riet, G. Nonantibiotic prophylaxis for recurrent urinary tract infections: A systematic review and meta-analysis of randomized controlled trials. J. Urol. 2013, 190, 1981–1989. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Butler, C.C.; Hawking, M.K.D.; Quigley, A.; McNulty, C.A.M. Incidence, severity, help seeking, and management of uncomplicated urinary tract infection: A population-based survey. Br. J. Gen. Pract. 2015, 65, e702–e707. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Medina-Bombardó, D.; Jover-Palmer, A. Does clinical examination aid in the diagnosis of urinary tract infections in women? A systematic review and meta-analysis. BMC Fam. Pract. 2011, 12, 111. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Butler, C.C.; Hillier, S.; Roberts, Z.; Dunstan, F.; Howard, A.; Palmer, S. Antibiotic-resistant infections in primary care are symptomatic for longer and increase workload: Outcomes for patients with E. coli UTIs. Br. J. Gen. Pract. 2006, 56, 686–692. [Google Scholar] [PubMed]
- Alam, M.F.; Cohen, D.; Butler, C.; Dunstan, F.; Roberts, Z.; Hillier, S.; Palmer, S. The additional costs of antibiotics and re-consultations for antibiotic-resistant Escherichia coli urinary tract infections managed in general practice. Int. J. Antimicrob. Agents 2009, 33, 255–257. [Google Scholar] [CrossRef]
- Holm, A.; Siersma, V.; Cordoba, G.C. Diagnosis of urinary tract infection based on symptoms: How are likelihood ratios affected by age? a diagnostic accuracy study. BMJ Open 2021, 11, e039871. [Google Scholar] [CrossRef]
- Public Health England. Diagnosis of Urinary Tract Infections: Quick Reference Tool for Primary Care for Consultation and Local Adaptation. 2020. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/927195/UTI_diagnostic_flowchart_NICE-October_2020-FINAL.pdf (accessed on 27 September 2022).
- Little, P.; Rumsby, K.; Jones, R.; Warner, G.; Moore, M.; Lowes, J.A.; Smith, H.; Hawke, C.; Leydon, G.; Mullee, M. Validating the prediction of lower urinary tract infection in primary care: Sensitivity and specificity of urinary dipsticks and clinical scores in women. Br. J. Gen. Pract. 2010, 60, 495–500. [Google Scholar] [CrossRef] [Green Version]
- Smieszek, T.; Pouwels, K.; Dolk, C.; Smith, D.; Hopkins, S.; Sharland, M.; Hay, A.; Moore, M.; Robotham, J.V. Potential for reducing inappropriate antibiotic prescribing in English primary care. J. Antimicrob. Chemother. 2018, 73, ii36–ii43. [Google Scholar] [CrossRef] [Green Version]
- Pouwels, K.B.; Dolk, F.C.K.; Smith, D.R.M.; Robotham, J.V.; Smieszek, T. Actual versus “ideal” antibiotic prescribing for common conditions in English primary care. J. Antimicrob. Chemother. 2018, 73, ii19–ii26. [Google Scholar] [CrossRef]
- Chatterjee, A.; Modarai, M.; Naylor, N.R.; Boyd, S.E.; Atun, R.; Barlow, J.; Holmes, A.H.; Johnson, A.; Robotham, J.V. Quantifying drivers of antibiotic resistance in humans: A systematic review. Lancet Infect. Dis. 2018, 18, e368–e378. [Google Scholar] [CrossRef] [Green Version]
- Arinzon, Z.; Shabat, S.; Peisakh, A.; Berner, Y. Clinical presentation of urinary tract infection (UTI) differs with aging in women. Arch. Gerontol. Geriatr. 2012, 55, 145–147. [Google Scholar] [CrossRef] [PubMed]
- Laupland, K.B.; Ross, T.; Pitout, J.D.D.; Church, D.L.; Gregson, D.B. Community-onset urinary tract infections: A population-based assessment. Infection 2007, 35, 150–153. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, H.; Farewell, D.; Jones, H.M.; Francis, N.A.; Paranjothy, S.; Butler, C.C. Incidence and antibiotic prescribing for clinically diagnosed urinary tract infection in older adults in UK primary care, 2004–2014. PLoS ONE 2018, 13, e0190521. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gandhi, J.; Chen, A.; Dagur, G.; Suh, Y.; Smith, N.; Cali, B.; Khan, S.A. Genitourinary syndrome of menopause: An overview of clinical manifestations, pathophysiology, etiology, evaluation, and management. Am. J. Obstet. Gynecol. 2016, 215, 704–711. [Google Scholar] [CrossRef] [Green Version]
- Kagan, R.; Kellogg-Spadt, S.; Parish, S.J. Practical Treatment Considerations in the Management of Genitourinary Syndrome of Menopause. Drugs Aging 2019, 36, 897–908. [Google Scholar] [CrossRef] [Green Version]
- Phillips, N.A.; Bachmann, G.A. The genitourinary syndrome of menopause. Menopause 2021, 28, 579–588. [Google Scholar] [CrossRef]
- Monteleone, P.; Mascagni, G.; Giannini, A.; Genazzani, A.R.; Simoncini, T. Symptoms of menopause—Global prevalence, physiology and implications. Nat. Rev. Endocrinol. 2018, 14, 199–215. [Google Scholar] [CrossRef]
- Ninan, S.; Walton, C.; Barlow, G. Investigation of suspected urinary tract infection in older people. BMJ 2014, 349, g4070. [Google Scholar] [CrossRef]
- Mody, L.; Juthani-Mehta, M. Urinary tract infections in older women: A clinical review. JAMA 2014, 311, 844–854. [Google Scholar] [CrossRef] [Green Version]
- Foxman, B. Recurring urinary tract infection: Incidence and risk factors. Am. J. Public Health 1990, 80, 331–333. [Google Scholar] [CrossRef] [Green Version]
- Ikähelmo, R.; Siitonen, A.; Heiskanen, T.; Kärkkäinen, U.; Kuosmanen, P.; Lipponen, P.; Mäkelä, P.H. Recurrence of Urinary Tract Infection in a Primary Care Setting: Analysis of a I-Year Follow-up of 179 Women. Clin. Infect. Dis. 1996, 22, 91–99. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Care Excellence (NICE). Urinary Tract Infection (Lower)—Women. 2022. Available online: https://cks.nice.org.uk/topics/urinary-tract-infection-lower-women/ (accessed on 6 October 2022).
- Lecky, D.M.; Howdle, J.; Butler, C.C.; McNulty, C.A. Optimising management of UTIs in primary care: A qualitative study of patient and GP perspectives to inform the development of an evidence-based, shared decision-making resource. Br. J. Gen. Pract. 2020, 70, e330–e338. [Google Scholar] [CrossRef] [PubMed]
- Flower, A.; Bishop, F.L.; Lewith, G. How women manage recurrent urinary tract infections: An analysis of postings on a popular web forum. BMC Fam. Pract. 2014, 15, 162. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Flower, A.; Winters, D.; Bishop, F.L.; Lewith, G. The challenges of treating women with recurrent urinary tract infections in primary care: A qualitative study of GPs’ experiences of conventional management and their attitudes towards possible herbal options. Prim. Health Care Res. Dev. 2015, 16, 597–606. [Google Scholar] [CrossRef] [PubMed]
- Eriksson, I.; Olofsson, B.; Gustafson, Y.; Fagerström, L. Older women’s experiences of suffering from urinary tract infections. J. Clin. Nurs. 2014, 23, 1385–1394. [Google Scholar] [CrossRef] [PubMed]
- Duffy, B.; Mori, K.S.; Terhanian, O.G.; Bremer, J. Comparing data from online and face-to-face surveys. Int. J. Mark. Res. 2005, 47, 615–639. [Google Scholar] [CrossRef] [Green Version]
- IPSOS. Survey Methods At Ipsos. 2006. Available online: https://www.ipsos.com/en-uk/survey-methods-ipsos-mori (accessed on 26 October 2022).
- National Institute for Health and Care Excellence (NICE). Menopause: Diagnosis and Management—NICE Guideline [NG23]. 2015. Available online: https://www.nice.org.uk/guidance/ng23/ifp/chapter/menopause (accessed on 6 October 2022).
- Giesen, L.G.; Cousins, G.; Dimitrov, B.D.; van de Laar, F.A.; Fahey, T. Predicting acute uncomplicated urinary tract infection in women: A systematic review of the diagnostic accuracy of symptoms and signs. BMC Fam Pract. 2010, 11, 78. [Google Scholar] [CrossRef] [Green Version]
- Bent, S.; Nallamothu, B.K.; Simel, D.L.; Fihn, S.D.; Saint, S. Does This Woman Have an Acute Uncomplicated Urinary Tract Infection? JAMA 2002, 287, 2701–2710. [Google Scholar] [CrossRef]
- Jolleys, J.V. The reported prevalence of urinary symptoms in women in one rural general practice. Br. J. Gen. Pract. 1990, 40, 335–357. [Google Scholar]
- Gavazzi, G.; Krause, K.H. Ageing and infection. Lancet Infect. Dis. 2002, 2, 659–666. [Google Scholar] [CrossRef]
- Norman, D.C. Fever in the Elderly. Clin. Infect. Dis. 2000, 31, 148–151. [Google Scholar] [CrossRef]
- van Duin, D. Diagnostic challenges and opportunities in older adults with infectious diseases. Clin. Infect. Dis. 2012, 54, 973–978. [Google Scholar] [CrossRef] [Green Version]
- Gbinigie, O.A.; Ordóñez-Mena, J.M.; Fanshawe, T.R.; Plüddemann, A.; Heneghan, C. Diagnostic value of symptoms and signs for identifying urinary tract infection in older adult outpatients: Systematic review and meta-analysis. J. Infect. 2018, 77, 379–390. [Google Scholar] [CrossRef] [Green Version]



| Demographics | e-Survey Study Population (%) n = 1096 | |
|---|---|---|
| Age (years) | 16–24 | 130 (12%) |
| 25–34 | 254 (23%) | |
| 35–44 | 183 (17%) | |
| 45–54 | 205 (19%) | |
| 55–64 | 133 (12%) | |
| 65–74 | 119 (11%) | |
| Over 75 | 72 (7%) | |
| Ethnicity | White | 988 (90%) |
| Ethnic minorities | 101 (9%) | |
| Social grade | AB | 284 (26%) |
| C1 | 360 (33%) | |
| C2 | 159 (15%) | |
| DE | 293 (27%) | |
| Region | North England | 327 (30%) |
| Midlands | 327 (30%) | |
| South England | 287 (26%) | |
| London | 155 (14%) | |
| Marital status | Married/living as married | 690 (63%) |
| Single | 253 (23%) | |
| Widowed/divorced/separated | 153 (14%) | |
| Education | GCSE/O-level/NVQ12 | 279 (25%) |
| A-level or equivalent | 276 (25%) | |
| Degree/Masters/PhD | 401 (37%) | |
| No formal qualifications | 140 (13%) | |
| Employment status | Employed (full-time/part-time or self-employed) | 636 (58%) |
| Unemployed | 460 (42%) | |
| Children in the household (17 years of age or under) | No children | 708 (65%) |
| 1 child | 204 (19%) | |
| 2 children | 130 (12%) | |
| 3 or more children | 54 (5%) | |
| Severity Score N (%) | Adjusted OR (95% CI) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |||
| Menopausal status | Pre-menopause | 5 (1%) | 11 (2%) | 17 (3%) | 40 (7%) | 45 (8%) | 80 (14%) | 132 (23%) | 113 (20%) | 71 (13%) | 35 (6%) | 19 (3%) | Reference |
| Menopause | 2 (1%) | 3 (1%) | 8 (2%) | 21 (6%) | 15 (4%) | 52 (16%) | 59 (18%) | 79 (24%) | 59 (18%) | 20 (6%) | 14 (4%) | 1.39 (1.04, 1.86) | |
| Post-menopause | 4 (2%) | 1 (0.5%) | 6 (3%) | 12 (6%) | 20 (11%) | 25 (13%) | 22 (12%) | 48 (25%) | 31 (16%) | 11 (5%) | 11 (6%) | 1.20 (0.78, 1.85) | |
| UTIs in the previous year | 1–2 UTIs | 7 (1%) | 14 (1%) | 29 (3%) | 71 (8%) | 70 (8%) | 134 (14%) | 186 (20%) | 207 (22%) | 134 (14%) | 45 (5%) | 31 (3%) | Reference |
| 3 or more UTIs | 4 (2%) | 1 (0.5%) | 2 (1%) | 3 (2%) | 10 (6%) | 23 (14%) | 27 (17%) | 33 (20%) | 28 (17%) | 20 (12%) | 13 (8%) | 1.93 (1.37, 2.73) | |
| Impact on Daily Life N (%) | Adjusted OR (95% CI) | |||||
|---|---|---|---|---|---|---|
| None | Not Much | Fair Amount | Great Deal | |||
| Menopausal status | Pre-menopause | 19 (3%) | 125 (22%) | 307 (54%) | 117 (21%) | Reference |
| Menopause | 7 (2%) | 72 (22%) | 184 (55%) | 69 (21%) | 1.09 (0.80, 1.47) | |
| Post-menopause | 11 (6%) | 64 (33%) | 86 (45%) | 33 (17%) | 0.62 (0.39, 0.98) | |
| UTIs in the previous year | 1–2 UTIs | 31 (3%) | 234 (25%) | 491 (53%) | 173 (19%) | Reference |
| 3 or more UTIs | 5 (3%) | 27 (16%) | 86 (53%) | 46 (28%) | 1.68 (1.19, 2.37) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sanyaolu, L.N.; Cooper, E.; Read, B.; Ahmed, H.; Lecky, D.M. Impact of Menopausal Status and Recurrent UTIs on Symptoms, Severity, and Daily Life: Findings from an Online Survey of Women Reporting a Recent UTI. Antibiotics 2023, 12, 1150. https://doi.org/10.3390/antibiotics12071150
Sanyaolu LN, Cooper E, Read B, Ahmed H, Lecky DM. Impact of Menopausal Status and Recurrent UTIs on Symptoms, Severity, and Daily Life: Findings from an Online Survey of Women Reporting a Recent UTI. Antibiotics. 2023; 12(7):1150. https://doi.org/10.3390/antibiotics12071150
Chicago/Turabian StyleSanyaolu, Leigh N., Emily Cooper, Brieze Read, Haroon Ahmed, and Donna M. Lecky. 2023. "Impact of Menopausal Status and Recurrent UTIs on Symptoms, Severity, and Daily Life: Findings from an Online Survey of Women Reporting a Recent UTI" Antibiotics 12, no. 7: 1150. https://doi.org/10.3390/antibiotics12071150
APA StyleSanyaolu, L. N., Cooper, E., Read, B., Ahmed, H., & Lecky, D. M. (2023). Impact of Menopausal Status and Recurrent UTIs on Symptoms, Severity, and Daily Life: Findings from an Online Survey of Women Reporting a Recent UTI. Antibiotics, 12(7), 1150. https://doi.org/10.3390/antibiotics12071150







