In Vitro Effect of Three-Antibiotic Combinations plus Potential Antibiofilm Agents against Biofilm-Producing Mycobacterium avium and Mycobacterium intracellulare Clinical Isolates
Abstract
:1. Introduction
2. Results
3. Discussion
4. Materials and Methods
4.1. Mycobacterium avium–Intracellulare Complex Isolates
4.2. Antibiotics and Potential Antibiofilm Agents (PAAs)
4.3. Antimicrobial Susceptibility Testing in Planktonic Forms
Control Testing of the Antibiotic Solvents DMSO and Ethanol in 8 MAC Isolates
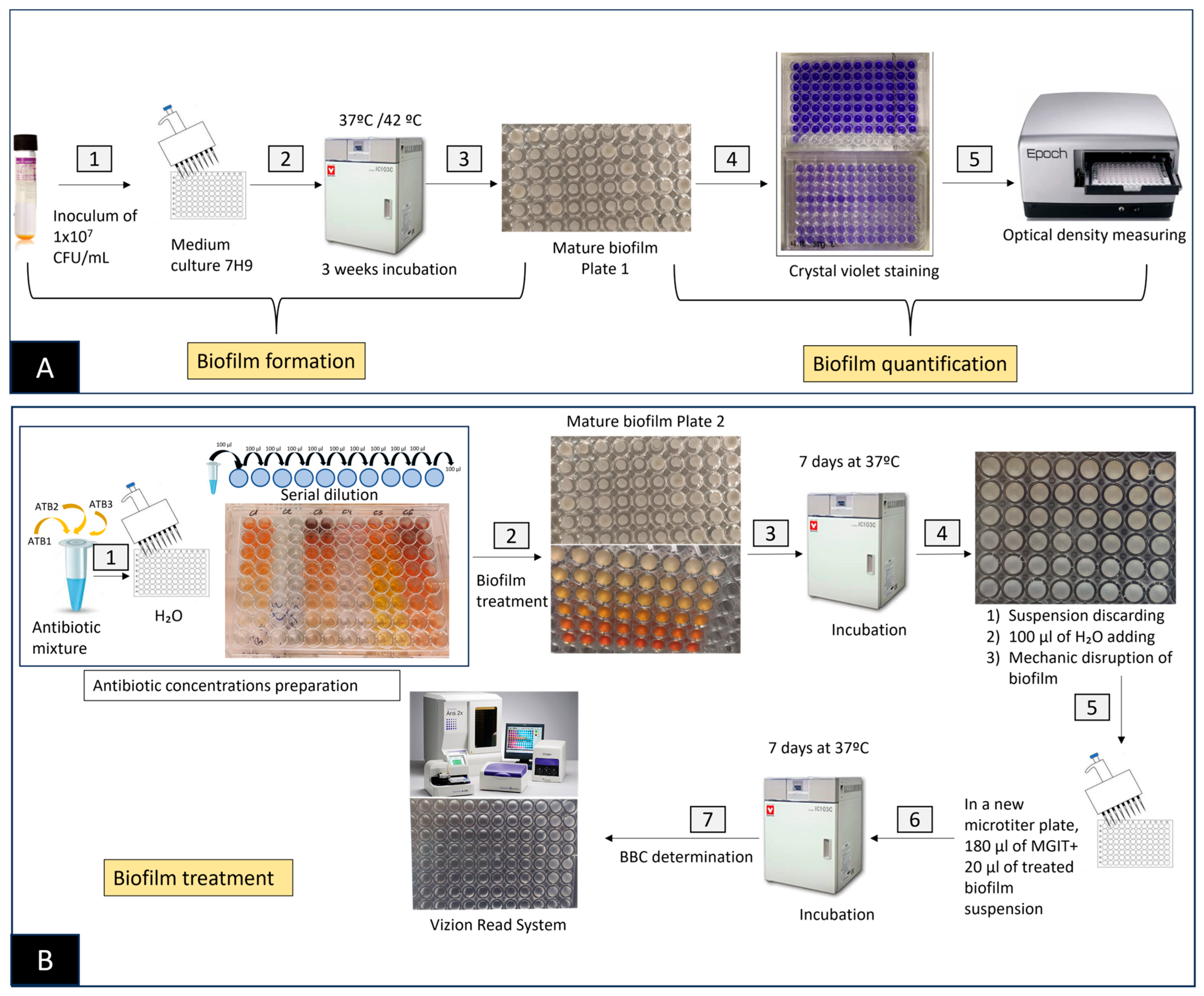
4.4. Biofilm Formation in Clinical Isolates
4.5. Biofilm Treatment Study
4.5.1. Antibiotic Alone plus PAAs in Biofilm
4.5.2. Determination of Biofilm Bactericidal Concentration
4.5.3. Determination of the Fractional Inhibitory Concentration Index
In Planktonic Forms
In Biofilm-Forming Forms
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ASA | Acetyl salicylic acid |
| BED | Bedaquiline |
| BBC | Biofilm bactericidal concentration |
| BF | Biofilm forming |
| BTS | British thoracic society |
| CFU | Colony-forming unit |
| CIC | Combination inhibitory concentration |
| CLA | Clarithromycin |
| CLO | Clofazimine |
| CV | Crystal violet |
| DDS | Diallyl disulfide |
| DMSO | Dimethyl sulfoxide |
| EMB | Ethambutol |
| FIC | Fractional inhibitory concentration |
| FICI | Fractional inhibitory concentration index |
| I | Intermediate |
| IBU | Ibuprofen |
| MAC | Mycobacterium avium complex |
| MBC | Minimum bactericidal concentration |
| MIC | Minimum inhibitory concentration |
| MOX | Moxifloxacin |
| NAC | N-acetyl-L-cysteine |
| NTM | Non-tuberculous mycobacteria |
| OD | Optical density |
| PAA | Potential antibiofilm agent |
| PBS | Phosphate-buffered saline |
| QS | Quorum sensing |
| R | Resistant |
| RB | Rifabutin |
| RIF | Rifampicin |
| SD | Standard deviation |
| S | Susceptible |
| TB | Tuberculosis |
References
- World Health Organization. Global Tuberculosis Report 2022; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Ratnatunga, C.N.; Lutzky, V.P.; Kupz, A.; Doolan, D.L.; Reid, D.W.; Field, M.; Bell, S.C.; Thomson, R.M.; Miles, J.J. The rise of non-tuberculosis mycobacterial lung disease. Front. Immunol. 2020, 11, 303. [Google Scholar] [CrossRef]
- Prevots, D.R.; Shaw, P.A.; Strickland, D.; Jackson, L.A.; Raebel, M.A.; Blosky, M.A.; Montes De Oca, R.; Shea, Y.R.; Seitz, A.E.; Holland, S.M.; et al. Nontuberculous mycobacterial lung disease prevalence at four integrated health care delivery systems. Am. J. Respir. Crit. Care Med. 2010, 182, 970–976. [Google Scholar] [CrossRef]
- Adjemian, J.; Daniel-Wayman, S.; Ricotta, E.; Prevots, D.R. Epidemiology of Nontuberculous Mycobacteriosis. Semin. Respir. Crit. Care Med. 2018, 39, 325–335. [Google Scholar] [CrossRef]
- Cowman, S.; van Ingen, J.; Griffith, D.E.; Loebinger, M.R. Non-tuberculous mycobacterial pulmonary disease. Eur. Respir. J. 2019, 54, 1900250. [Google Scholar] [CrossRef]
- Daley, C.L. Mycobacterium avium complex disease. Microbiol. Spectr. 2017, 5, 663–701. [Google Scholar] [CrossRef]
- Falkinham, J.O. Environmental sources of nontuberculous mycobacteria. Clin. Chest Med. 2015, 36, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Henkle, E.; Winthrop, K.L. Non-tuberculous mycobacteria infections in immunosuppressed hosts. Clin. Chest Med. 2015, 36, 91–99. [Google Scholar] [CrossRef]
- Daley, C.L.; Iaccarino, J.M.; Lange, C.; Cambau, E.; Wallace, R.J., Jr.; Andrejak, C.; Böttger, E.C.; Brozek, J.; Griffith, D.E.; Guglielmetti, L.; et al. Treatment of Nontuberculous Mycobacterial Pulmonary Disease: An Official ATS/ERS/ESCMID/IDSA Clin. Practice Guideline. Clin. Infect. Dis. 2020, 71, e1–e36. [Google Scholar] [CrossRef]
- Diel, R.; Lipman, M.; Hoefsloot, W. High mortality in patients with Mycobacterium avium complex lung disease: A systematic review. BMC Infect. Dis. 2018, 18, 206. [Google Scholar] [CrossRef]
- Brown-Elliott, B.A.; Nash, K.A.; Wallace, R.J., Jr. Antimicrobial susceptibility testing, drug resistance mechanisms, and therapy of infections with nontuberculous mycobacteria. Clin. Med. Rev. 2012, 25, 545–582. [Google Scholar] [CrossRef]
- Parker, H.; Lorenc, R.; Ruelas Castillo, J.; Karakousis, P.C. Mechanisms of antibiotics tolerance in Mycobacterium avium complex: Lessons from related mycobacteria. Front. Microbiol. 2020, 11, 573983. [Google Scholar] [CrossRef]
- Griffith, D.E. Nontuberculous mycobacterial lung disease. Curr. Opin. Infect. Dis. 2010, 23, 185–190. [Google Scholar] [CrossRef]
- Griffith, D.E.; Aksamit, T.; Brown-Elliott, B.A.; Catanzaro, A.; Daley, C.; Gordin, F.; Holland, S.M.; Horsburh, R.; Huitt, G.; Iademarco, M.F.; et al. ATS Mycobacterial Diseases Subcommittee; American thoracic Society: Infectious Disease Society of America. An official ATS/IDSA statement: Diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am. J. Respir. Crit. Care Med. 2007, 175, 367–416. [Google Scholar] [CrossRef]
- Van Ingen, J.; Boeree, M.J.; van Soolingen, D.; Mouton, J.W. Resistance mechanism and drug susceptibility of nontuberculous mycobacteria. Drug Resist. Updates 2012, 15, 149–161. [Google Scholar] [CrossRef] [PubMed]
- Haworth, C.S.; Banks, J.; Capstick, T.; Fisher, A.J.; Gorsuch, T.; Laurenson, I.F.; Leitch, A.; Loebinger, M.R.; Milburn, H.J.; Nightingale, M.; et al. British Thoracic Society guidelines for the management of nontuberculous mycobacterial pulmonary disease (NTM-PD). Thorax 2017, 72 (Suppl. S2), ii1–ii64. [Google Scholar] [CrossRef] [PubMed]
- Muñoz-Egea, M.C.; Akir, A.; Esteban, J. Mycobacterium biofilms. Biofilm 2023, 5, 100107. [Google Scholar] [CrossRef]
- Hall-Stoodley, L.; Stoodley, P. Evolving concepts in biofilm infections. Cell Microbiol. 2009, 11, 1034–1043. [Google Scholar] [CrossRef] [PubMed]
- Zamora, N.; Esteban, J.; Kinnari, T.J.; Zafra, C. In vitro evaluation of the adhesion to polypropylene sutures of non-pigmented, rapidly growing mycobacteria. Clin. Microbiol. Infect. 2007, 13, 902. [Google Scholar] [CrossRef]
- Sharma, D.; Misba, L.; Khan, A.U. Antibiotics versus biofilm: An emerging battleground in microbial communities. Antimicrob. Resist. Infect. Control 2019, 8, 76. [Google Scholar] [CrossRef] [PubMed]
- Dai, L.; Wu, T.Q.; Xiong, Y.S.; Ni, H.B.; Ding, Y.; Zhang, W.C.; Chu, S.P.; Ju, S.Q.; Yu, J. Ibuprofen-mediated potential inhibition of biofilm development and quorum sensing in Pseudomonas aeruginosa. Life Sci. 2019, 237, 116947. [Google Scholar] [CrossRef]
- Vilaplana, C.; Marzo, E.; Tapia, G.; Diaz, J.; Garcia, V.; Cardona, P.-J. Ibuprofen therapy resulted in significantly decreased tissue bacillary loads and increased survival in a new murine experimental model of active tuberculosis. J. Infect. Dis. 2013, 208, 199–202. [Google Scholar] [CrossRef]
- Li, W.-R.; Ma, Y.K.; Xie, X.B.; Shi, Q.S.; Wen, X.; Sun, T.L.; Peng, H. Diallyl disulfite from garlic oil inhibits Pseudomonas aeruginosa quorum sensing systems and corresponding virulence factors. Front. Microbiol. 2019, 9, 3222. [Google Scholar] [CrossRef] [PubMed]
- Stepanovic, S.; Vukovic, D.; Jesic, M.; Ranin, L. Influence of acetylsalicylic acid (Aspirin) on biofilm production by Candida Species. J. Chemother. 2004, 16, 134–138. [Google Scholar] [CrossRef]
- Elbestawy, M.K.M.; El-Sherbiny, G.M.; Moghannem, S.A. Antibacterial, Antibiofilm and anti-inflammatory activities of eugenol clove essential oil against resistant Helicobacter pylori. Molecules 2023, 28, 2448. [Google Scholar] [CrossRef] [PubMed]
- Neagu, R.; Popovici, V.; Ionescu, L.E.; Ordeanu, V.; Popescu, D.M.; Ozon, E.A.; Gîrd, C.E. Antibacterial and antibiofilm effects of different samples of five commercially available essential oils. Antibiotics 2023, 12, 1191. [Google Scholar] [CrossRef]
- Rayan, M.; Abu Lafi, S.; Falah, M.; Kacergius, T.; Kirkliauskiene, A.; Gabe, V.; Rayan, A. alkyl gallates as potential antibiofilm agents: A Review. Molecules 2023, 28, 1751. [Google Scholar] [CrossRef] [PubMed]
- Purkait, S.; Bhattacharya, A.; Bag, A.; Chattopadhyay, R.R. Evaluation of antibiofilm efficacy of essential oil components β-caryophyllene, cinnamaldehyde and eugenol alone and in combination against biofilm formation and preformed biofilms of Listeria monocytogenes and Salmonella typhimurium. Lett. Appl. Microbiol. 2020, 71, 195–202. [Google Scholar] [CrossRef]
- Abdel Bar, F.M.; Alossaimi, M.A.; Elekhnawy, E.; Alzeer, M.A.A.; Abo Kamer, A.; Moglad, E.; ElNaggar, M.H. Anti-quorum sensing and anti-biofilm activity of Pelargonium hortorum root extract against Pseudomonas aeruginosa: Combinatorial effect of catechin and gallic acid. Molecules 2022, 27, 7841. [Google Scholar] [CrossRef]
- Ratti, A.; Fassi, E.M.A.; Forlani, F.; Mori, M.; Villa, F.; Cappitelli, F.; Sgrignani, J.; Roda, G.; Cavalli, A.; Villa, S.; et al. Mechanistic insights into the antibiofilm mode of action of ellagic acid. Pharmaceutics 2023, 15, 1757. [Google Scholar] [CrossRef]
- Woods, G.L.; Brown-Elliott, B.A.; Conville, P.S.; Desmond, E.P.; Hall, G.S.; Lin, G.; Pfyffer, G.E.; Ridderhof, J.C.; Siddiqi, S.H.; Wallace, R.J.; et al. Susceptibility Testing of Mycobacteria, Nocardiae, and Other Aerobic Actinomycetes; Report No.: M24-3nd ed-M62-1st ed. Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2018. [Google Scholar]
- Brown-Elliott, B.A.; Philley, J.V.; Griffith, D.E.; Thakkar, F.; Wallace, R.J., Jr. In Vitro susceptibility testing of bedaquiline against Mycobacterium avium complex. Antimicrob. Agents Chemother. 2017, 61, e01798-16. [Google Scholar] [CrossRef] [PubMed]
- Fröberg, G.; Maurer, F.P.; Chryssanthou, E.; Fernström, L.; Benmansour, H.; Boarbi, S.; Mengshoel, A.T.; Keller, P.M.; Viveiros, M.; Machado, D.; et al. Towards clinical breakpoints for non-tuberculous mycobacteria—Determination of epidemiological cut off values for the Mycobacterium avium complex and Mycobacterium abscessus using broth microdilution. Clin. Microbiol. Infect. 2023, 29, 758–764. [Google Scholar] [CrossRef] [PubMed]
- Portell-Buj, E.; González-Criollo, C.; López-Gavín, A.; Fernández-Pittol, M.; Busquets, M.A.; Estelrich, J.; Garrigó, M.; Rubio, M.; Tudó, G.; González-Martin, J. Activity of antibiotics and potential antibiofilm agents against biofilm-producing Mycobacterium avium-intracellulare complex causing chronic pulmonary infections. Antibiotics 2022, 11, 589. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Pittol, M.; Batista-Arnau, S.; Román, A.; San Nicolás, L.; Oliver, L.; González-Moreno, O.; Martínez, J.A.; Amaro-Rodríguez, R.; Soler, N.; Gené, A.; et al. Differences in drug-susceptibility patterns between Mycobacterium avium, Mycobacterium intracellulare, and Mycobacterium chimaera clinical isolates: Prospective 8.5-year analysis by three laboratories. Antibiotics 2023, 12, 64. [Google Scholar] [CrossRef] [PubMed]
- Hu, J.; Zhu, H.; Feng, Y.; Yu, M.; Xu, Y.; Zhao, Y.; Zheng, B.; Lin, J.; Miao, W.; Zhou, R.; et al. Emulsions containing composite (clove, oregano, and cinnamon) essential oils: Phase inversion preparation, physicochemical properties and antibacterial mechanism. Food Chem. 2023, 421, 136201. [Google Scholar] [CrossRef]
- Dotto, C.; Lombarte-Serrat, A.; Cattelan, N.; Barbagelata, M.S.; Yantorno, O.M.; Sordelli, D.O.; Ehling-Schulz, M.; Grunert, T.; Buzzola, F.R. The active component of aspirin, salicylic acid, promotes Staphylococcus aureus biofilm formation in a PIA-dependent manner. Front. Microbiol. 2017, 8, 4. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Wang, D.; Yu, C.; Li, T.; Liu, J.; Sun, S. Potential antifungal targets against a Candida biofilm based on an enzyme in the arachidonic acid cascade-A Review. Front. Microbiol. 2016, 7, 1925. [Google Scholar] [CrossRef]
- Davis, D.G.; Parsek, M.R.; Pearson, J.P.; Iglewski, B.H.; Costerton, J.W.; Greenberg, E.P. The involvement of cell-to-cell signals in the development of bacterial biofilm. Science 1998, 208, 295–298. [Google Scholar] [CrossRef]
- Feng, W.; Yang, J.; Ma, Y.; Xi, Z.; Ren, Q.; Wang, S.; Ning, H. Aspirin and verapamil increase the sensitivity of Candida albicans to caspofungin under planktonic and biofilm conditions. J. Glob. Antimicrob. Resist. 2021, 24, 32–39. [Google Scholar] [CrossRef]
- Di Bella, S.; Luzzati, R.; Principe, L.; Zerbato, V.; Meroni, E.; Giuffre, M.; Croce, L.S.; Merlo, M.; Perotto, M.; Dolso, E.; et al. Aspirin and infection: A narrative review. Biomedicines 2022, 10, 263. [Google Scholar] [CrossRef]
- Alem, M.A.; Douglas, L.J. Effects of aspirin and other nonsteroidal anti-inflammatory drugs on biofilms and planktonic cells of Candida albicans. Antimicrob. Agents Chemother. 2004, 48, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Liao, Y.; Cong, L.; Lu, X.; Yang, R. In vitro interactions between non-steroidal anti-inflammatory drugs and antifungal agents against planktonic and biofilm forms of Trichosporon asahii. PLoS ONE 2016, 11, e0157047. [Google Scholar] [CrossRef] [PubMed]
- Snoussi, M.; Noumi, E.; Hajlaoui, H.; Bouslama, L.; Hamdi, A.; Saeed, M.; Alreshidi, M.; Adnan, M.; Al-Rashidi, A.; Aouadi, K.; et al. Phytochemical profiling of Allium subhirsutum L. aqueous extract with antioxidant, antimicrobial, antibiofilm, and anti-quorum sensing properties: In vitro and in silico studies. Plants 2022, 11, 495. [Google Scholar] [CrossRef]
- Bjarnsholt, T.; Jensen, P.; Rasmussen, T.B.; Christophersen, L.; Calum, H.; Hentzer, M.; Hougen, H.P.; Rygaard, J.; Moser, C.; Eberl, L.; et al. Garlic blocks quorum sensing and promotes rapid clearing of pulmonary Pseudomonas aeruginosa infections. Microbiology 2005, 151, 3873–3880. [Google Scholar] [CrossRef]
- Bhatwalkar, S.B.; Mondal, R.; Krishna, S.B.N.; Adam, J.K.; Govender, P.; Anupam, R. Antibacterial Properties of Organosulfur Compounds of Garlic (Allium sativum). Front. Microbiol. 2021, 12, 613077. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, I.M.; Borges, A.; Borges, F.; Simões, M. Repurposing ibuprofen to control Staphylococcus aureus biofilms. Eur. J. Med. Chem. 2019, 15, 197–205. [Google Scholar] [CrossRef] [PubMed]
- Sepúlveda, R.A.; Ortega, M.; Donoso, N.; Jara, A. Intoxicación por ácido acetilsalicílico, fisiopatología y manejo. Rev. Med. Chile 2018, 146, 1309–1316. [Google Scholar] [CrossRef] [PubMed]
- Flannagan, R.J.; Meredith, T.J. The use of N-acetylcysterine in clinical toxicology. Am. J. Med. 1991, 91, S131–S139. [Google Scholar] [CrossRef]
- Geith, S.; Renner, B.; Rabe, C.; Stenzel, J.; Eyer, F. Ibuprofen plasma concentration profile in deliberate ibuprofen overdose with circulatory depression treated with therapeutic plasma exchange: A case report. BMC Pharmacol. Toxicol. 2017, 18, 81. [Google Scholar] [CrossRef] [PubMed]
- Dahiya, A.; Prakash, A.; Agrawala, P.K.; Dutta, A. Investigation on oral toxicity of diallyl sulfide a principle organosulfur compound derived from allium sativum garlic in mice. Def. Life Sci. J. 2022, 7, 3–10. [Google Scholar] [CrossRef]
- Macia, M.D.; Rojo-Molinero, E.; Oliver, A. Antimicrobial susceptibility testing in biofilm-growing bacteria. Clin. Microbiol. Infect. 2014, 20, 981–990. [Google Scholar] [CrossRef] [PubMed]
- López-Gavín, A.; Tudó, G.; Vergara, A.; Hurtado, J.C.; Gonzalez-Martín, J. In vitro activity against Mycobacterium tuberculosis of levofloxacin, moxifloxacin and UB-8902 in combination with clofazimine and pretomanid. Int. J. Antimicrob. Agents 2015, 46, 582–585. [Google Scholar] [CrossRef] [PubMed]
| Planktonic Form | Biofilm Form | |||||
|---|---|---|---|---|---|---|
| Antibiotic | M. avium | M. intracellulare | M. avium | M. intracellulare | ||
| MIC50 | MBC50 | MIC50 | MBC50 | BBC50 | BBC50 | |
| CLA | 4 | 16 | 2 | 32 | 256 | 256 |
| MOX | 4 | 32 | 2 | 4 | 512 | 512 |
| BED | 0.5 | 4 | 0.5 | 4 | 128 | 64 |
| CLO | 4 | 4 | 16 | 32 | 512 | 256 |
| RB | 0.25 | 4 | 0.25 | 0.5 | 32 | 512 |
| RIF | 0.25 | 4 | 0.5 | 1 | 256 | 512 |
| EMB | 8 | 8 | 2 | 32 | 2048 | 2048 |
| Planktonic Forms | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Combination | Mycobacterium avium | Mycobacterium intracellulare | ||||||||||
| MIC50 | MIC50 FICI Range | % Isolates Showing Synergistic Activity | MBC50 | MBC50 FICI Range | % Isolates Showing Synergistic Activity | MIC50 | MIC50 FICI Range | % Isolates Showing Synergistic Activity | MBC50 | MBC50 FICI Range | % Isolates Showing Synergistic Activity | |
| CLA + BED + CLO | 0.25 | 0.75–2.5 | 25 | 0.25 | 0.30–4.5 | 50 | 0.5 | 0.31–0.64 | 100 | 1 | 0.19–0.63 | 100 |
| CLA + BED + EMB | 0.25 | 0.33–1.28 | 25 | 0.25 | 0.17–0.88 | 100 | 0.5 | 0.30–0.50 | 100 | 1 | 0.19–0.41 | 100 |
| CLA + CLO + EMB | 0.25 | 0.28–1.09 | 50 | 0.5 | 0.13–1.75 | 50 | 2 | 0.17–2.13 | 50 | 4 | 0.38–0.75 | 100 |
| CLA + RB + EMB | 0.06 | 0.05–1.09 | 50 | 0.06 | 0.03–0.08 | 100 | 0.125 | 0.38–1.5 | 50 | 0.25 | 0.27–0.54 | 100 |
| CLA + RIF + EMB * | 0.125 | 0.14–1.10 | 50 | 0.5 | 0.22–0.34 | 100 | 0.5 | 0.51–1.5 | 25 | 1 | 1.09–2.3 | 50 |
| MOX + BED + CLO | 0.125 | 0.39–1.25 | 50 | 0.125 | 0.20–2.13 | 50 | 0.25 | 0.16–0.64 | 100 | 1 | 0.38–0.53 | 100 |
| MOX + BED + EMB | 0.5 | 0.37–2.56 | 25 | 0.5 | 0.05–0.20 | 100 | 0.25 | 0.15–0.75 | 100 | 1 | 0.19–0.63 | 100 |
| MOX + CLO + EMB | 0.25 | 0.03–1.09 | 50 | 0.5 | 0.07–0.41 | 100 | 2 | 0.39–2.13 | 50 | 4 | 0.38–1.63 | 50 |
| MOX + RB + EMB | 0.06 | 0.26–1.28 | 25 | 0.06 | 0.02–0.08 | 100 | 0.125 | 0.25–1.25 | 50 | 0.25 | 0.27–4.75 | 50 |
| MOX + RIF + EMB * | 0.25 | 0.28–2.03 | 25 | 0.5 | 0.2–0.2 | 100 | 0.5 | 0.57–3 | 25 | 1 | 1.06–2.75 | 0 |
| Antibiotic Combination | M. avium | M. intracellulare | ||||
|---|---|---|---|---|---|---|
| BBC50 (µg/mL) | FICI50 Range | % Isolates Showing Synergistic Activity 1 | BBC50 (µg/mL) | FICI50 Range | % Isolates Showing Synergistic Activity 1 | |
| CLA + BED + CLO | 64 | 0.54–>4 | 25 | 64 | 0.31–1.75 | 50 |
| CLA + BED + EMB | 32 | 0.63–>4 | 25 | 64 | 0.22–1.38 | 50 |
| CLA + CLO + EMB | 256 | 0.52–>4 | 50 | 64 | 0.13–0.88 | 50 |
| CLA + RB + EMB | 16 | 1–>4 | 0 | 32 | 0.20–0.44 | 100 |
| CLA + RF + EMB * | 128 | 0.25–>4 | 25 | 64 | 0.20–0.53 | 100 |
| MOX + BED + CLO | 32 | 0.22–>4 | 25 | 64 | 0.31–1.63 | 75 |
| MOX + BED + EMB | 32 | 0.17–>4 | 50 | 64 | 0.22–3.23 | 50 |
| MOX + CLO + EMB | 128 | 0.43–>4 | 75 | 64 | 0.13–0.44 | 75 |
| MOX + RB + EMB | 64 | 1–>4 | 0 | 256 | 0.39–2.25 | 50 |
| MOX + RF + EMB * | 32 | 0.17–>4 | 25 | 64 | 0.25–3 | 75 |
| Antibiotic Combination | M. avium | |||||||
|---|---|---|---|---|---|---|---|---|
| NAC | IBU | ASA | DDS | |||||
| BBC50 | FICI50 Range | BBC50 | FICI50 Range | BBC50 | FICI50 Range | BBC50 | FICI50 Range | |
| CLA + BED + CLO | 2 | 0.007–0.16 * | 4 | 0.08–0.16 * | 2 | 0.08–0.13 * | 4 | 0.03–0.13 * |
| CLA + BED + EMB | 1 | 0.005–0.13 * | 1 | 0.005–0.07 * | 2 | 0.01–0.27 * | 1 | 0.005–0.27 * |
| CLA + CLO + EMB | 16 | 0.05–0.20 * | 32 | 0.08–0.20 * | 8 | 0.03–0.20 * | 8 | 0.05–0.41 * |
| CLA + RB + EMB | 4 | 0.03–0.26 * | 2 | 0.03–0.16 * | 2 | 0.03–0.13 * | 2 | 0.04–0.34 * |
| CLA + RIF + EMB ** | 32 | 0.03–0.53 * | 8 | 0.03–0.22 * | 8 | 0.07–0.22 * | 8 | 0.03–0.17 * |
| MOX + BED + CLO | 4 | 0.08–0.14 * | 2 | 0.034–0.11 * | 4 | 0.034–0.11 * | 4 | 0.034–0.08 * |
| MOX + BED + EMB | 4 | 0.04–0.34 * | 4 | 0.04–0.69 * | 4 | 0.04–0.06 * | 4 | 0.04–0.34 * |
| MOX + CLO + EMB | 16 | 0.05–0.11 * | 8 | 0.03–0.14 * | 8 | 0.03–0.14 * | 8 | 0.03–0.22 * |
| MOX + RB + EMB | 1 | 0.06–0.55 * | 2 | 0.06–0.14 * | 2 | 0.07–0.55 * | 4 | 0.04–0.55 * |
| MOX + RIF + EMB ** | 16 | 0.06–0.22 * | 8 | 0.04–0.44 * | 8 | 0.03–0.44 * | 8 | 0.03–0.44 * |
| Antibiotic Combination | M. intracellulare | |||||||
|---|---|---|---|---|---|---|---|---|
| NAC | IBU | ASA | DDS | |||||
| BBC50 | FICI50 Range | BBC50 | FICI50 Range | BBC50 | FICI50 Range | BBC50 | FICI50 Range | |
| CLA + BED + CLO | 0.5 | 0.006–0.02 * | <0.25 | 0.001–0.01 * | <0.25 | 0.001–0.01 * | 0.5 | 0.006–0.01 * |
| CLA + BED + EMB | 0.5 | 0.007–0.27 * | <0.25 | 0.0009–0.01 * | 0.5 | 0.003–0.017 * | 0.5 | 0.007–0.017 * |
| CLA + CLO + EMB | 2 | 0.007–0.2 * | 2 | 0.007–0.02 * | 8 | 0.008–0.06 * | 16 | 0.008–0.39 * |
| CLA + RB + EMB | 2 | 0.007–0.027 * | 1 | 0.002–0.22 * | 1 | 0.006–0.22 * | 2 | 0.007–0.01 * |
| CLA + RIF + EMB ** | 16 | 0.05–0.13 * | 8 | 0.01–0.13 * | 8 | 0.01–0.13 * | 16 | 0.03–0.13 * |
| MOX + BED + CLO | 0.5 | 0.005–0.06 * | <0.25 | 0.001–0.02 * | <0.25 | 0.001–0.13 * | <0.25 | 0.001–0.13 * |
| MOX + BED + EMB | <0.25 | 0.0009–0.07* | <0.25 | 0.009–0.006 * | <0.25 | 0.0009–0.01 * | 0.5 | 0.002–0.07 * |
| MOX + CLO + EMB | 8 | 0.04–0.33 * | 2 | 0.008–0.16 * | 4 | 0.008–0.33 * | 8 | 0.02–0.33 * |
| MOX + RB + EMB | 4 | 0.008–0.05 * | 1 | 0.009–0.01* | 4 | 0.008–0.03 * | 2 | 0.008–0.04 * |
| MOX + RIF + EMB ** | 16 | 0.09–0.13 * | 16 | 0.01–0.1 + | 16 | 0.03–0.1 * | 16 | 0.05–0.19 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Batista, S.; Fernandez-Pittol, M.; Nicolás, L.S.; Martínez, D.; Rubio, M.; Garrigo, M.; Vila, J.; Tudó, G.; González-Martin, J. In Vitro Effect of Three-Antibiotic Combinations plus Potential Antibiofilm Agents against Biofilm-Producing Mycobacterium avium and Mycobacterium intracellulare Clinical Isolates. Antibiotics 2023, 12, 1409. https://doi.org/10.3390/antibiotics12091409
Batista S, Fernandez-Pittol M, Nicolás LS, Martínez D, Rubio M, Garrigo M, Vila J, Tudó G, González-Martin J. In Vitro Effect of Three-Antibiotic Combinations plus Potential Antibiofilm Agents against Biofilm-Producing Mycobacterium avium and Mycobacterium intracellulare Clinical Isolates. Antibiotics. 2023; 12(9):1409. https://doi.org/10.3390/antibiotics12091409
Chicago/Turabian StyleBatista, Sara, Mariana Fernandez-Pittol, Lorena San Nicolás, Diego Martínez, Marc Rubio, Montserrat Garrigo, Jordi Vila, Griselda Tudó, and Julian González-Martin. 2023. "In Vitro Effect of Three-Antibiotic Combinations plus Potential Antibiofilm Agents against Biofilm-Producing Mycobacterium avium and Mycobacterium intracellulare Clinical Isolates" Antibiotics 12, no. 9: 1409. https://doi.org/10.3390/antibiotics12091409
APA StyleBatista, S., Fernandez-Pittol, M., Nicolás, L. S., Martínez, D., Rubio, M., Garrigo, M., Vila, J., Tudó, G., & González-Martin, J. (2023). In Vitro Effect of Three-Antibiotic Combinations plus Potential Antibiofilm Agents against Biofilm-Producing Mycobacterium avium and Mycobacterium intracellulare Clinical Isolates. Antibiotics, 12(9), 1409. https://doi.org/10.3390/antibiotics12091409








