Misconceptions and Knowledge Gaps on Antibiotic Use and Resistance in Four Healthcare Settings and Five European Countries—A Modified Delphi Study
Abstract
:1. Introduction
2. Results
2.1. Literature Search
2.2. Panel of Experts
2.3. Delphi Process
2.4. Antimicrobial Resistance
2.5. General Use of Antibiotics
2.6. The Use of Antibiotics for Respiratory Tract Infections
2.7. The Use of Antibiotics for Urinary Tract Infections
3. Discussion
3.1. Main Findings
3.2. Strengths and Limitations of the Study
3.3. Comparison with Existing Literature
3.4. Implications for Practice
4. Materials and Methods
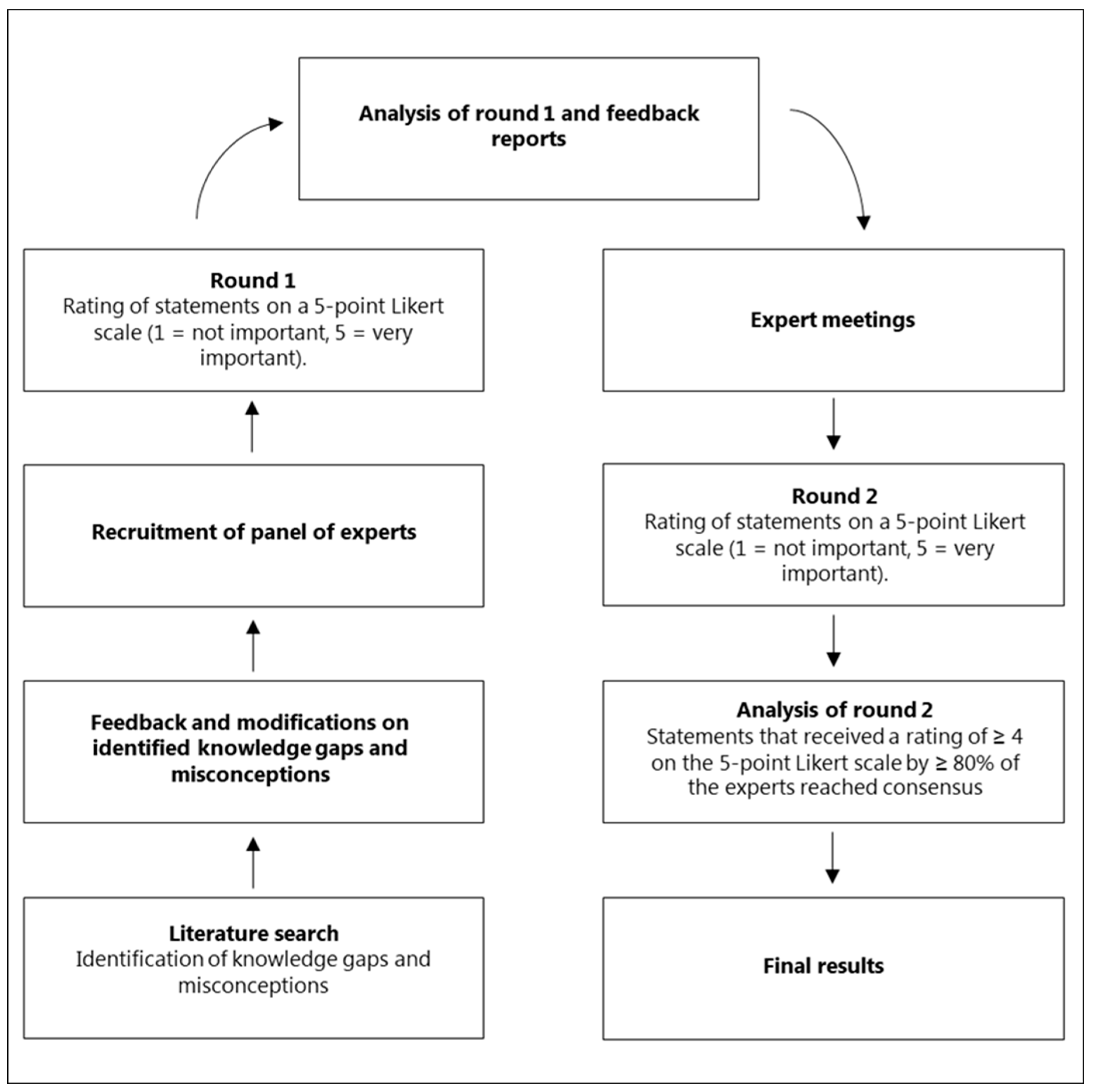
4.1. Design
4.2. Recruitment and Coordination of Panel of Experts
4.3. Identification of Misconceptions and Knowledge Gaps
4.4. Data Collection
4.4.1. Round 1
4.4.2. Feedback and Expert Meetings
4.4.3. Round 2
4.5. Definition of Consensus and End of Delphi Process
4.6. Data Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
List of Abbreviations
| AMR | Antimicrobial resistance |
| HCP(s) | Healthcare professional(s) |
| EU | European Union |
| HAPPY PATIENT | Health Alliance for Prudent Prescribing and Yield of Antibiotics in a Patient-Centred Perspective |
| OoHS | Out-of-hours services |
| UTI | Urinary tract infection |
References
- World Health Organisation. Antimicrobial Resistance. Available online: https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance (accessed on 7 August 2023).
- Murray, C.J.; Ikuta, K.S.; Sharara, F.; Swetschinski, L.; Robles Aguilar, G.; Gray, A.; Han, C.; Bisignano, C.; Rao, P.; Wool, E.; et al. Global Burden of Bacterial Antimicrobial Resistance in 2019: A Systematic Analysis. Lancet 2022, 399, 629–655. [Google Scholar] [CrossRef] [PubMed]
- Ventola, C.L. The Antibiotic Resistance Crisis: Part 1: Causes and Threats. Pharm. Ther. 2015, 40, 277. [Google Scholar]
- Llor, C.; Bjerrum, L. Antimicrobial Resistance: Risk Associated with Antibiotic Overuse and Initiatives to Reduce the Problem. Ther. Adv. Drug Saf. 2014, 5, 229. [Google Scholar] [CrossRef]
- Tangcharoensathien, V.; Chanvatik, S.; Kosiyaporn, H.; Kirivan, S.; Kaewkhankhaeng, W.; Thunyahan, A.; Lekagul, A. Population Knowledge and Awareness of Antibiotic Use and Antimicrobial Resistance: Results from National Household Survey 2019 and Changes from 2017. BMC Public Health 2021, 21, 2188. [Google Scholar] [CrossRef] [PubMed]
- Cals, J.W.L.; Boumans, D.; Lardinois, R.J.M.; Gonzales, R.; Hopstaken, R.M.; Butler, C.C.; Dinant, G.J. Public Beliefs on Antibiotics and Respiratory Tract Infections: An Internet-Based Questionnaire Study. Br. J. Gen. Pract. 2007, 57, 942–947. [Google Scholar] [CrossRef]
- Napolitano, F.; Izzo, M.T.; Di Giuseppe, G.; Angelillo, I.F. Public Knowledge, Attitudes, and Experience Regarding the Use of Antibiotics in Italy. PLoS ONE 2013, 8, e84177. [Google Scholar] [CrossRef] [PubMed]
- Björkman, I.; Berg, J.; Viberg, N.; Stålsby Lundborg, C. Awareness of Antibiotic Resistance and Antibiotic Prescribing in UTI Treatment: A Qualitative Study among Primary Care Physicians in Sweden. Scand. J. Prim. Health Care 2013, 31, 50–55. [Google Scholar] [CrossRef]
- Dempsey, P.P.; Businger, A.C.; Whaley, L.E.; Gagne, J.J.; Linder, J.A. Primary Care Clinicians’ Perceptions about Antibiotic Prescribing for Acute Bronchitis: A Qualitative Study. BMC Fam. Pract. 2014, 15, 194. [Google Scholar] [CrossRef]
- Charani, E.; Cooke, J.; Holmes, A. Antibiotic Stewardship Programmes—What’s Missing? J. Antimicrob. Chemother. 2010, 65, 2275–2277. [Google Scholar] [CrossRef]
- MacDougall, C.; Polk, R.E. Antimicrobial Stewardship Programs in Health Care Systems. Clin. Microbiol. Rev. 2005, 18, 638–656. [Google Scholar] [CrossRef]
- Wathne, J.S.; Kleppe, L.K.S.; Harthug, S.; Blix, H.S.; Nilsen, R.M.; Charani, E. The Effect of Antibiotic Stewardship Interventions with Stakeholder Involvement in Hospital Settings: A Multicentre, Cluster Randomized Controlled Intervention Study. Antimicrob. Resist. Infect. Control 2018, 7, 109. [Google Scholar] [CrossRef] [PubMed]
- Van Buul, L.W.; Sikkens, J.J.; Van Agtmael, M.A.; Kramer, M.H.H.; Van der Steen, J.T.; Hertogh, C.M.P.M. Participatory Action Research in Antimicrobial Stewardship: A Novel Approach to Improving Antimicrobial Prescribing in Hospitals and Long-Term Care Facilities. J. Antimicrob. Chemother. 2014, 69, 1734–1741. [Google Scholar] [CrossRef] [PubMed]
- Jairoun, A.; Hassan, N.; Ali, A.; Jairoun, O.; Shahwan, M.; Hassali, M. University Students’ Knowledge, Attitudes, and Practice Regarding Antibiotic Use and Associated Factors: A Cross-Sectional Study in the United Arab Emirates. Int. J. Gen. Med. 2019, 12, 235. [Google Scholar] [CrossRef] [PubMed]
- Sakr, S.; Ghaddar, A.; Hamam, B.; Sheet, I. Antibiotic Use and Resistance: An Unprecedented Assessment of University Students’ Knowledge, Attitude and Practices (KAP) in Lebanon. BMC Public Health 2020, 20, 535. [Google Scholar] [CrossRef]
- Karasneh, R.A.; Al-Azzam, S.I.; Ababneh, M.; Al-Azzeh, O.; Al-Batayneh, O.B.; Muflih, S.M.; Khasawneh, M.; Khassawneh, A.R.M.; Khader, Y.S.; Conway, B.R.; et al. Prescribers’ Knowledge, Attitudes and Behaviors on Antibiotics, Antibiotic Use and Antibiotic Resistance in Jordan. Antibiotics 2021, 10, 858. [Google Scholar] [CrossRef] [PubMed]
- El-Sokkary, R.; Kishk, R.; El-Din, S.M.; Nemr, N.; Mahrous, N.; Alfishawy, M.; Morsi, S.; Abdalla, W.; Ahmed, M.; Tash, R. Antibiotic Use and Resistance Among Prescribers: Current Status of Knowledge, Attitude, and Practice in Egypt. Infect. Drug Resist. 2021, 14, 1209–1218. [Google Scholar] [CrossRef]
- Al-Taani, G.M.; Al-Azzam, S.; Karasneh, R.A.; Sadeq, A.S.; Mazrouei, N.A.; Bond, S.E.; Conway, B.R.; Aldeyab, M.A. Pharmacists’ Knowledge, Attitudes, Behaviors and Information Sources on Antibiotic Use and Resistance in Jordan. Antibiotics 2022, 11, 175. [Google Scholar] [CrossRef]
- Bjerrum, A.; García-Sangenís, A.; Modena, D.; Córdoba, G.; Bjerrum, L.; Chalkidou, A.; Lykkegaard, J.; Hansen, M.P.; Søndergaard, J.; Nexøe, J.; et al. Health Alliance for Prudent Prescribing and Yield of Antibiotics in a Patient-Centred Perspective (HAPPY PATIENT): A before-and-after Intervention and Implementation Study Protocol. BMC Prim. Care 2022, 23, 102. [Google Scholar] [CrossRef]
- Rusic, D.; Bukić, J.; Seselja Perisin, A.; Leskur, D.; Modun, D.; Petric, A.; Vilovic, M.; Bozic, J. Are We Making the Most of Community Pharmacies? Implementation of Antimicrobial Stewardship Measures in Community Pharmacies: A Narrative Review. Antibiotics 2021, 10, 63. [Google Scholar] [CrossRef]
- van der Velden, A.; Duerden, M.G.; Bell, J.; Oxford, J.S.; Altiner, A.; Kozlov, R.; Sessa, A.; Pignatari, A.C.; Essack, S.Y. Prescriber and Patient Responsibilities in Treatment of Acute Respiratory Tract Infections—Essential for Conservation of Antibiotics. Antibiotics 2013, 2, 316. [Google Scholar] [CrossRef]
- Panagakou, S.G.; Spyridis, N.; Papaevangelou, V.; Theodoridou, K.M.; Goutziana, G.P.; Theodoridou, M.N.; Syrogiannopoulos, G.A.; Hadjichristodoulou, C.S. Antibiotic Use for Upper Respiratory Tract Infections in Children: A Cross-Sectional Survey of Knowledge, Attitudes, and Practices (KAP) of Parents in Greece. BMC Pediatr. 2011, 11, 60. [Google Scholar] [CrossRef] [PubMed]
- Woods, C.J.; Morrice, Z.; Francis, N.A.; Little, P.; Verheij, T.; Leydon, G.M. Parent and Clinician Views of Managing Children with Symptoms of a Lower Respiratory Tract Infection and Their Influence upon Decisions to Take Part in a Placebo-Controlled Randomised Control Trial. Antibiotics 2021, 10, 356. [Google Scholar] [CrossRef] [PubMed]
- Cordoba, G.; Siersma, V.; Lopez-Valcarcel, B.; Bjerrum, L.; Llor, C.; Aabenhus, R.; Makela, M. Prescribing Style and Variation in Antibiotic Prescriptions for Sore Throat: Cross-Sectional Study across Six Countries. BMC Fam. Pract. 2015, 16, 7. [Google Scholar] [CrossRef] [PubMed]
- Chaaban, T.; Ahouah, M.; Lombrail, P.; Le Febvre, H.; Mourad, A.; Morvillers, J.M.; Rothan-Tondeur, M. Decisional Issues in Antibiotic Prescribing in French Nursing Homes: An Ethnographic Study. J. Public Health Res. 2019, 8, 90–95. [Google Scholar] [CrossRef]
- Willems, C.S.J.; Van den Broek D’Obrenan, J.; Numans, M.E.; Verheij, T.J.M.; Van der Velden, A.W. Cystitis: Antibiotic Prescribing, Consultation, Attitudes and Opinions. Fam. Pract. 2014, 31, 149–155. [Google Scholar] [CrossRef]
- Plate, A.; Kronenberg, A.; Risch, M.; Mueller, Y.; Di Gangi, S.; Rosemann, T.; Senn, O. Treatment of Urinary Tract Infections in Swiss Primary Care: Quality and Determinants of Antibiotic Prescribing. BMC Fam. Pract. 2020, 21, 125. [Google Scholar] [CrossRef]
- Lakhani, J.D.; Lakhani, S.J.; Meera, S.; Sanket, P.; Sandeep, J. Appropriate Use of Antimicrobial Agents in Urinary Tract Infections: Perception of Physicians and Resident Doctors. J. Integr. Health Sci. 2019, 7, 19. [Google Scholar] [CrossRef]
- Duane, S.; Domegan, C.; Callan, A.; Galvin, S.; Cormican, M.; Bennett, K.; Murphy, A.W.; Vellinga, A. Using Qualitative Insights to Change Practice: Exploring the Culture of Antibiotic Prescribing and Consumption for Urinary Tract Infections. BMJ Open 2016, 6, e008894. [Google Scholar] [CrossRef]
- Leydon, G.M.; Turner, S.; Smith, H.; Little, P. Women’s Views about Management and Cause of Urinary Tract Infection: Qualitative Interview Study. BMJ 2010, 340, 407. [Google Scholar] [CrossRef]
- Leydon, G.M.; Turner, S.; Smith, H.; Little, P. The Journey from Self-Care to GP Care: A Qualitative Interview Study of Women Presenting with Symptoms of Urinary Tract Infection. Br. J. Gen. Pract. 2009, 59, e219. [Google Scholar] [CrossRef]
- Minejima, E.; Lee, E.; Quach, S.; Santos, N.; Lou, M.; Wong-Beringer, A. Understanding Patient Perceptions and Attitudes toward Urinary Tract Infections and Treatment in a Medically Underserved Population. J. Am. Coll. Clin. Pharm. 2019, 2, 616–622. [Google Scholar] [CrossRef]
- Roope, L.S.J.; Tonkin-Crine, S.; Butler, C.C.; Crook, D.; Peto, T.; Peters, M.; Walker, A.S.; Wordsworth, S. Reducing Demand for Antibiotic Prescriptions: Evidence from an Online Survey of the General Public on the Interaction between Preferences, Beliefs and Information, United Kingdom, 2015. Euro Surveill. 2018, 23, 1700424. [Google Scholar] [CrossRef] [PubMed]
- Robert, A.; Nguyen, Y.; Bajolet, O.; Vuillemin, B.; Defoin, B.; Vernet-Garnier, V.; Drame, M.; Bani-Sadr, F. Knowledge of Antibiotics and Antibiotic Resistance in Patients Followed by Family Physicians. Med. Mal. Infect. 2017, 47, 142–151. [Google Scholar] [CrossRef]
- McNulty, C.A.M.; Nichols, T.; Boyle, P.J.; Woodhead, M.; Davey, P. The English Antibiotic Awareness Campaigns: Did They Change the Public’s Knowledge of and Attitudes to Antibiotic Use? J. Antimicrob. Chemother. 2010, 65, 1526–1533. [Google Scholar] [CrossRef]
- Mcnulty, C.A.M.; Collin, S.M.; Cooper, E.; Lecky, D.M.; Butler, C.C. Public Understanding and Use of Antibiotics in England: Findings from a Household Survey in 2017. BMJ Open 2019, 9, e030845. [Google Scholar] [CrossRef] [PubMed]
- Van Hecke, O.; Butler, C.C.; Wang, K.; Tonkin-Crine, S. Parents’ Perceptions of Antibiotic Use and Antibiotic Resistance (PAUSE): A Qualitative Interview Study. J. Antimicrob. Chemother. 2019, 74, 1741–1747. [Google Scholar] [CrossRef]
- Hawke, K.L.; McGuire, T.M.; Ranmuthugala, G.; Van Driel, M.L. What Do Consumers Want to Know about Antibiotics? Analysis of a Medicines Call Centre Database. Fam. Pract. 2016, 33, 75–81. [Google Scholar] [CrossRef]
- Pavydė, E.; Veikutis, V.; Mačiulienė, A.; Mačiulis, V.; Petrikonis, K.; Stankevičius, E. Public Knowledge, Beliefs and Behavior on Antibiotic Use and Self-Medication in Lithuania. Int. J. Environ. Res. Public Health 2015, 12, 7002–7016. [Google Scholar] [CrossRef]
- McCullough, A.R.; Parekh, S.; Rathbone, J.; Del Mar, C.B.; Hoffmann, T.C. A Systematic Review of the Public’s Knowledge and Beliefs about Antibiotic Resistance. J. Antimicrob. Chemother. 2016, 71, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Godycki-Cwirko, M.; Cals, J.W.L.; Francis, N.; Verheij, T.; Butler, C.C.; Goossens, H.; Zakowska, I.; Panasiuk, L. Public Beliefs on Antibiotics and Symptoms of Respiratory Tract Infections among Rural and Urban Population in Poland: A Questionnaire Study. PLoS ONE 2014, 9, e109248. [Google Scholar] [CrossRef]
- Roope, L.S.J.; Tonkin-Crine, S.; Herd, N.; Michie, S.; Pouwels, K.B.; Castro-Sanchez, E.; Sallis, A.; Hopkins, S.; Robotham, J.V.; Crook, D.W.; et al. Reducing Expectations for Antibiotics in Primary Care: A Randomised Experiment to Test the Response to Fear-Based Messages about Antimicrobial Resistance. BMC Med. 2020, 18, 110. [Google Scholar] [CrossRef] [PubMed]
- Richmond, J.; Mangrum, R.; Wang, G.; Maurer, M.; Sofaer, S.; Yang, M.; Carman, K.L. An Informed Public’s Views on Reducing Antibiotic Overuse. Health Serv. Res. 2019, 54, 1283. [Google Scholar] [CrossRef] [PubMed]
- Keeney, S.; Hasson, F.; Mckenna, H. The Delphi Technique in Nursing and Health Research. In The Delphi Technique in Nursing and Health Research; John Wiley & Sons: Hoboken, NJ, USA, 2010. [Google Scholar] [CrossRef]
- Powell, C. The Delphi Technique: Myths and Realities. J. Adv. Nurs. 2003, 41, 376–382. [Google Scholar] [CrossRef]
- Trevelyan, E.G.; Robinson, N. Delphi Methodology in Health Research: How to Do It? Eur. J. Integr. Med. 2015, 7, 423–428. [Google Scholar] [CrossRef]
- Belton, I.; MacDonald, A.; Wright, G.; Hamlin, I. Improving the Practical Application of the Delphi Method in Group-Based Judgment: A Six-Step Prescription for a Well-Founded and Defensible Process. Technol. Forecast. Soc. Chang. 2019, 147, 72–82. [Google Scholar] [CrossRef]
- Skulmoski, G.J.; Skulmoski, G.J.; Hartman, F.T.; Krahn, J. The Delphi Method for Graduate Research. J. Inf. Technol. Educ. Res. 2007, 6, 1–21. [Google Scholar] [CrossRef]
- McMillan, S.S.; King, M.; Tully, M.P. How to Use the Nominal Group and Delphi Techniques. Int. J. Clin. Pharm. 2016, 38, 655–662. [Google Scholar] [CrossRef]
- Boulkedid, R.; Abdoul, H.; Loustau, M.; Sibony, O.; Alberti, C. Using and Reporting the Delphi Method for Selecting Healthcare Quality Indicators: A Systematic Review. PLoS ONE 2011, 6, e20476. [Google Scholar] [CrossRef]
- Lange, T.; Kopkow, C.; Lützner, J.; Günther, K.P.; Gravius, S.; Scharf, H.P.; Stöve, J.; Wagner, R.; Schmitt, J. Comparison of Different Rating Scales for the Use in Delphi Studies: Different Scales Lead to Different Consensus and Show Different Test-Retest Reliability. BMC Med. Res. Methodol. 2020, 20, 28. [Google Scholar] [CrossRef] [PubMed]
- Toma, C.L.; Picioreanu, I. The Delphi Technique: Methodological Considerations and the Need for Reporting Guidelines in Medical Journals. Int. J. Public Health Res. 2016, 4, 47–59. [Google Scholar]
- Md Rezal, R.S.; Hassali, M.A.; Alrasheedy, A.A.; Saleem, F.; Md Yusof, F.A.; Godman, B. Physicians’ Knowledge, Perceptions and Behaviour towards Antibiotic Prescribing: A Systematic Review of the Literature. Expert Rev. Anti Infect. Ther. 2015, 13, 665–680. [Google Scholar] [CrossRef] [PubMed]
- Harris, A.; Chandramohan, S.; Awali, R.A.; Grewal, M.; Tillotson, G.; Chopra, T. Physicians’ Attitude and Knowledge Regarding Antibiotic Use and Resistance in Ambulatory Settings. Am. J. Infect. Control 2019, 47, 864–868. [Google Scholar] [CrossRef] [PubMed]
- Teixeira Rodrigues, A.; Roque, F.; Falcão, A.; Figueiras, A.; Herdeiro, M.T. Understanding Physician Antibiotic Prescribing Behaviour: A Systematic Review of Qualitative Studies. Int. J. Antimicrob. Agents 2013, 41, 203–212. [Google Scholar] [CrossRef]
- Gourgoulis, G.M.; Katerelos, P.; Maragos, A.; Gargalianos, P.; Lazanas, M.; Maltezou, H.C. Antibiotic Prescription and Knowledge about Antibiotic Costs of Physicians in Primary Health Care Centers in Greece. Am. J. Infect. Control 2013, 41, 1296–1297. [Google Scholar] [CrossRef] [PubMed]
- Zalmanovici Trestioreanu, A.; Lador, A.; Sauerbrun-Cutler, M.T.; Leibovici, L. Antibiotics for Asymptomatic Bacteriuria. Cochrane Database Syst. Rev. 2015, 4, CD009534. [Google Scholar] [CrossRef]
- Royal College of General Practice Course: TARGET Antibiotics Toolkit Hub. Available online: https://elearning.rcgp.org.uk/course/view.php?id=553 (accessed on 7 August 2023).
- Public Health England Antibiotic Awareness: Posters and Leaflets. Available online: https://www.gov.uk/government/publications/european-antibiotic-awareness-day-and-antibiotic-guardian-posters-and-leaflets (accessed on 7 August 2023).
- Centers for Disease Control and Prevention Print Materials—Antibiotic Use. Available online: https://www.cdc.gov/antibiotic-use/print-materials.html (accessed on 7 August 2023).
- European Centre for Disease Prevention and Control Communication Toolkit to Promote Prudent Antibiotic Use Aimed at Primary Care Prescribers. Available online: https://antibiotic.ecdc.europa.eu/en/toolkit-primary-care-prescribers (accessed on 7 August 2023).
| Participating Countries | General Practice | Out-of-Hours Services | Nursing Homes | Pharmacies | Total |
|---|---|---|---|---|---|
| France | 2 | 2 | 1 | 2 | 7 |
| Greece | 2 | 1 | 0 | 1 | 4 |
| Lithuania | 3 | 3 | 2 | 3 | 11 |
| Poland | 3 | 3 | 3 | 3 | 12 |
| Spain | 3 | 3 | 2 | 3 | 11 |
| Total | 13 | 12 | 8 | 12 | 45 |
| General Practice | Out-of-Hours Services | Nursing Homes | Community Pharmacies | |||||
|---|---|---|---|---|---|---|---|---|
| Round 1 (N = 17) | Round 2 (N = 13) | Round 1 (N = 16) | Round 2 (N = 12) | Round 1 (N = 15) | Round 2 (N = 8) | Round 1 (N = 18) | Round 2 (N = 12) | |
| Theme 1: Antimicrobial resistance (8) * | 8 | 6 | 8 | 4 | 6 | 6 | 7 | 7 |
| Theme 2: Antibiotic use (9) * | 7 | 4 | 8 | 6 | 5 | 5 | 8 | 9 |
| Theme 3: Respiratory tract infections (15) * | 13 | 12 | 8 | 12 | 6 | 5 | 11 | 12 |
| Theme 4: Urinary tract infections (12) * | 11 | 12 | 2 | 8 | 1 | 8 | 5 | 8 |
| Total (44) *: | 39 | 34 | 26 | 30 | 18 | 24 | 31 | 36 |
| No | Statements Divided by Theme | Mean (Consensus Level in %) | Mean (Consensus Level in %) | Mean (Consensus Level in %) | Mean (Consensus Level in %) | 4-Setting Consensus |
|---|---|---|---|---|---|---|
| Theme 1: Statements related to antimicrobial resistance in general | General practice | Out-of-hours services | Nursing homes | Community pharmacies | All settings | |
| 1 | Bacteria resistant to antibiotics are only present in hospitals * | 4.46 (100.0) | 3.92 (66.6) | 4.38 (75.0) | 4.46 (91.7) | |
| 2 | Antimicrobial resistance is not a problem in my country * | 4.46 (84.6) | 4.46 (91.7) | 4.46 (87.5) | 4.46 (91.7) | × |
| 3 | I cannot contribute to the increase of antimicrobial resistance * | 4.38 (92.4) | 4.25 (75.0) | 4.38 (87.5) | 4.38 (91.7) | |
| 4 | Others, not me, are responsible for controlling the problem of antimicrobial resistance † | 4.23 (92.3) | 4.00 (75.0) | 4.23 (87.5) | 4.23 (91.7) | |
| 5 | Antimicrobial Resistance is not a problem where I work † | 4.15 (92.3) | 4.15 (83.3) | 4.15 (100.0) | 4.15 (83.3) | × |
| 6 | Antimicrobial resistance is not an important problem because better antibiotics are continuously being discovered † | 4.08 (84.7) | 4.08 (91.7) | 4.08 (100.0) | 4.08 (91.7) | × |
| 7 | Not all antibiotics are at risk of becoming ineffective against infections by resistant bacteria * | 4.00 (77.0) | 4.00 (83.3) | 4.00 (62.5) | 4.00 (91.6) | × |
| 8 | If I am not exposed to antibiotics (e.g., directly by consuming antibiotics, or indirectly via the environment), then I cannot carry or transmit antibiotic-resistant bacteria * | 4.00 (77.0) | 4.00 (75.0) | 3.85 (87.5) | 3.67 (66.7) | |
| Theme 2: Statements about the use of antibiotics in general | General practice | Out-of-hours services | Nursing homes | Community pharmacies | All settings | |
| 9 | It is fine to use leftover antibiotics (or sharing antibiotics with family and friends) without consulting a healthcare professional, when experiencing similar symptoms to previous acute infections * | 4.92 (100.0) | 4.92 (91.6) | 4.13 (75.0) | 4.92 (100.0) | |
| 10 | The single presence of fever suggests high probability of bacterial infection and need of antibiotics * | 4.46 (92.3) | 4.17 (75.0) | 4.46 (87.5) | 4.46 (100.0) | |
| 11 | The benefits of prescribing antibiotics when unsure of the bacterial or viral origin of the symptoms outweigh the harms of exposure to antibiotics † | 4.46 (84.6) | 4.46 (100.0) | 4.46 (100.0) | 4.46 (100.0) | × |
| 12 | Antibiotics are effective against all type of infections * | 4.38 (84.6) | 4.38 (100.0) | 4.38 (100.0) | 4.38 (100.0) | × |
| 13 | Broad spectrum antibiotics, such as quinolones and 3rd–5th generation cephalosporines, are the best treatment options because they cover a wide range of bacteria † | 3.85 (69.3) | 3.85 (91.6) | 3.85 (87.5) | 3.85 (83.3) | |
| 14 | Ending the consultation without an antibiotic prescription, when the patient is asking for it, indicates lack of empathy from the doctor * | 3.85 (77.0) | 3.85 (91.7) | 4.13 (75.0) | 3.85 (91.7) | |
| 15 | Ending the consultation without an antibiotic prescription indicates that the doctor is not taking my symptoms seriously enough * | 3.77 (69.3) | 4.25 (91.7) | 3.77 (100.0) | 3.77 (91.7) | |
| 16 | Ciprofloxacin, doxycycline, levofloxacin, ofloxacin, tetracycline, trimethoprim do not cause sensitivity to sunlight † | 3.23 (53.9) | 3.67 (66.7) | 4.00 (75.0) | 3.23 (83.4) | |
| 17 | A good doctor is the one that prescribes the newest type of antibiotics † | 3.15 (53.9) | 3.83 (75.0) | 4.13 (75.0) | 3.15 (91.6) | |
| Theme 3: Statements about the use of antibiotics for respiratory tract infections | General practice | Out-of-hours services | Nursing homes | Community pharmacies | All settings | |
| 18 | More than 2 weeks coughing suggests a high probability of bacterial infection and need of antibiotics † | 4.69 (92.3) | 4.69 (100.0) | 4.00 (75.0) | 4.69 (100.0) | |
| 19 | As soon as I feel symptoms like sore throat, running nose, fever I should seek medical care to get antibiotics * | 4.62 (92.3) | 4.62 (83.3) | 4.62 (100.0) | 4.62 (91.6) | × |
| 20 | All children with middle ear inflammation and ear pain require antibiotic therapy † | 4.54 (92.3) | 4.54 (91.7) | 3.50 (50.0) | 4.54 (100.0) | |
| 21 | The single presence of tonsillar exudate in patients with sore throat suggests a high probability of bacterial infection and need of antibiotics † | 4.46 (92.3) | 4.46 (91.6) | 4.00 (75.0) | 4.46 (83.3) | |
| 22 | In patients with sore throat and other symptoms such as tonsillar exudates, fever, tender anterior cervical adenopathy, antibiotics have a great impact in the course of symptoms by shortening the length of symptoms by more than two days † | 4.46 (100.0) | 4.46 (91.7) | 4.46 (100.0) | 4.46 (83.4) | × |
| 23 | Based on the characteristics of the cough the health care professional can differentiate the viral or bacterial origin of the cough. For example, a chesty cough (wet, productive, or phlegmy) means that it is caused by a bacterium † | 4.38 (92.3) | 4.38 (91.7) | 3.38 (62.5) | 4.38 (83.4) | |
| 24 | A patient with the combination of two or more of the following symptoms: (a) nasal congestion, (b) nasal discharge, (c) pain in the face/teeth, (d) reduced sense of smell, (e) fever; requires antibiotic therapy independently of the number of days with symptoms † | 4.31 (92.3) | 4.31 (83.3) | 3.63 (62.5) | 4.31 (100.0) | |
| 25 | Cough with purulent sputum (or change of color of the sputum) suggests a high probability of bacterial infection and need of antibiotics † | 4.31 (84.6) | 4.31 (91.6) | 4.31 (100.0) | 4.31 (100.0) | × |
| 26 | The single presence of tender anterior cervical adenopathy in patients with sore throat suggests a high probability of bacterial infection and need of antibiotics † | 4.23 (84.7) | 4.00 (75.0) | 4.23 (87.5) | 4.17 (75.0) | |
| 27 | Purulent nasal discharge suggests a high probability of bacterial infection and need of antibiotics † | 4.23 (84.6) | 4.23 (91.7) | 4.23 (87.5) | 4.23 (100.0) | × |
| 28 | The majority of patients with a sore throat require antibiotic treatment † | 4.15 (84.7) | 4.15 (83.4) | 3.63 (62.5) | 4.15 (91.7) | |
| 29 | A bacterial infection is the most common cause of the single or combined presentation of the following symptoms: (a) nasal congestion, (b) nasal discharge, (c) pain in the face/teeth, (d) reduced sense of smell, (e) fever † | 3.92 (84.6) | 4.17 (75.0) | 3.88 (75.0) | 4.50 (83.4) | |
| 30 | The presence of cough without other symptom suggests a high probability of bacterial infection and need of antibiotics † | 4.08 (77.0) | 4.08 (83.3) | 3.75 (62.5) | 4.08 (91.7) | |
| 31 | Macrolides are the best first option for treating a bacterial lower respiratory tract infection in order to cover typical and atypical pathogens † | 3.85 (69.3) | 3.85 (91.6) | 4.13 (75.0) | 3.83 (66.7) | |
| 32 | A sinus X-ray can help doctors to discriminate the bacterial or viral origin of the rhinosinusitis symptoms † | 3.31 (53.9) | 3.33 (58.3) | 3.50 (50.0) | 3.33 (41.6) | |
| Theme 4: Statements about the use of antibiotics for urinary tract infections | General practice | Out-of-hours services | Nursing homes | Community pharmacies | All settings | |
| 33 | The single presence of painful discharge of urine suggests a high probability of bacterial infection and need of antibiotics † | 4.69 (100.0) | 4.69 (83.3) | 4.69 (87.5) | 4.69 (91.6) | × |
| 34 | The single presence of frequent urination suggests a high probability of bacterial infection and need of antibiotics † | 4.54 (100.0) | 4.54 (91.7) | 4.00 (75.0) | 4.54 (100.0) | |
| 35 | The single presence of burning sensation during urination suggests a high probability of bacterial infection and need of antibiotics † | 4.54 (100.0) | 4.54 (91.7) | 3.88 (75.0) | 4.54 (100.0) | |
| 36 | The single presence of blood in urine suggests a high probability of bacterial infection and need of antibiotics † | 4.46 (92.3) | 4.46 (83.3) | 4.46 (87.5) | 4.46 (100.0) | × |
| 37 | When a patient comes with acute UTI 1 symptoms it is okay to prescribe antibiotics, despite of the negative result of a dipstick test [nitrites (−), leucocytes (−)]. A negative dipstick test is not a good predictor of absence of UTI 1 † | 4.46 (100.0) | 4.46 (100.0) | 4.46 (87.5) | 3.17 (25.0) | |
| 38 | Leucocytes positive and nitrite negative result in a dipstick test indicates with high certainty bacterial infection and need of antibiotics † | 4.31 (92.3) | 4.00 (75.0) | 4.31 (87.5) | 3.58 (41.7) | |
| 39 | The single presence of smelly urine suggests a high probability of bacterial infection and need of antibiotics † | 4.31 (84.7) | 3.92 (75.0) | 4.00 (75.0) | 4.31 (83.4) | |
| 40 | The single presence of cloudy urine suggests a high probability of bacterial infection and need of antibiotics † | 4.31 (84.7) | 3.75 (66.7) | 4.31 (87.5) | 4.31 (83.4) | |
| 41 | A positive dipstick in the elderly without urinary tract symptoms is a strong indicator for urinary tract infection and requires antibiotics † | 4.31 (92.3) | 4.31 (83.4) | 4.31 (100.0) | 3.67 (50.0) | |
| 42 | The single presence of persistent urge to urinate suggests a high probability of bacterial infection and need of antibiotics † | 4.23 (84.7) | 4.23 (83.3) | 3.75 (75.0) | 4.23 (100.0) | |
| 43 | In an uncomplicated UTI 1, antibiotic treatment should be started as soon as possible to prevent the dissemination of the infection to the kidneys and bloodstream, independently of the risk of complication † | 4.23 (84.7) | 4.23 (83.3) | 4.23 (87.5) | 4.23 (91.7) | × |
| 44 | Cognitive changes (e.g., agitation, confusion) in the elderly suggest a high probability of bacterial infection and the need of antibiotics, even without the presence of urinary tract symptoms † | 4.00 (84.7) | 4.08 (75.0) | 4.00 (87.5) | 3.75 (58.3) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chalkidou, A.; Lambert, M.; Cordoba, G.; Taxis, K.; Hansen, M.P.; Bjerrum, L. Misconceptions and Knowledge Gaps on Antibiotic Use and Resistance in Four Healthcare Settings and Five European Countries—A Modified Delphi Study. Antibiotics 2023, 12, 1435. https://doi.org/10.3390/antibiotics12091435
Chalkidou A, Lambert M, Cordoba G, Taxis K, Hansen MP, Bjerrum L. Misconceptions and Knowledge Gaps on Antibiotic Use and Resistance in Four Healthcare Settings and Five European Countries—A Modified Delphi Study. Antibiotics. 2023; 12(9):1435. https://doi.org/10.3390/antibiotics12091435
Chicago/Turabian StyleChalkidou, Athina, Maarten Lambert, Gloria Cordoba, Katja Taxis, Malene Plejdrup Hansen, and Lars Bjerrum. 2023. "Misconceptions and Knowledge Gaps on Antibiotic Use and Resistance in Four Healthcare Settings and Five European Countries—A Modified Delphi Study" Antibiotics 12, no. 9: 1435. https://doi.org/10.3390/antibiotics12091435
APA StyleChalkidou, A., Lambert, M., Cordoba, G., Taxis, K., Hansen, M. P., & Bjerrum, L. (2023). Misconceptions and Knowledge Gaps on Antibiotic Use and Resistance in Four Healthcare Settings and Five European Countries—A Modified Delphi Study. Antibiotics, 12(9), 1435. https://doi.org/10.3390/antibiotics12091435






