Unraveling the Microbial Symphony: Impact of Antibiotics and Probiotics on Infant Gut Ecology and Antibiotic Resistance in the First Six Months of Life
Abstract
:1. Introduction
2. Results
2.1. Sociodemographic Information of Mothers and Infants
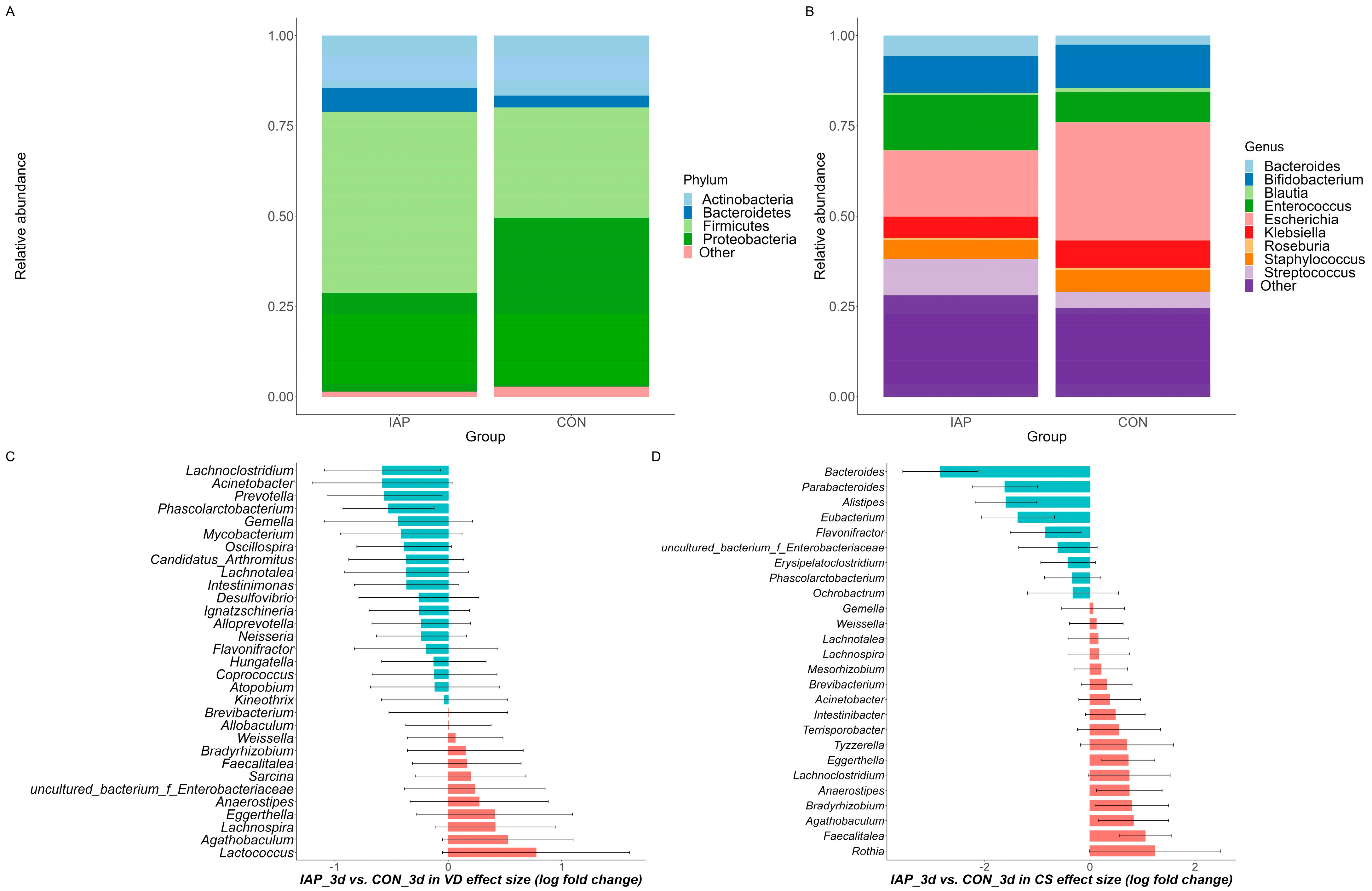
2.2. Overview of Microbial Communities in Infants
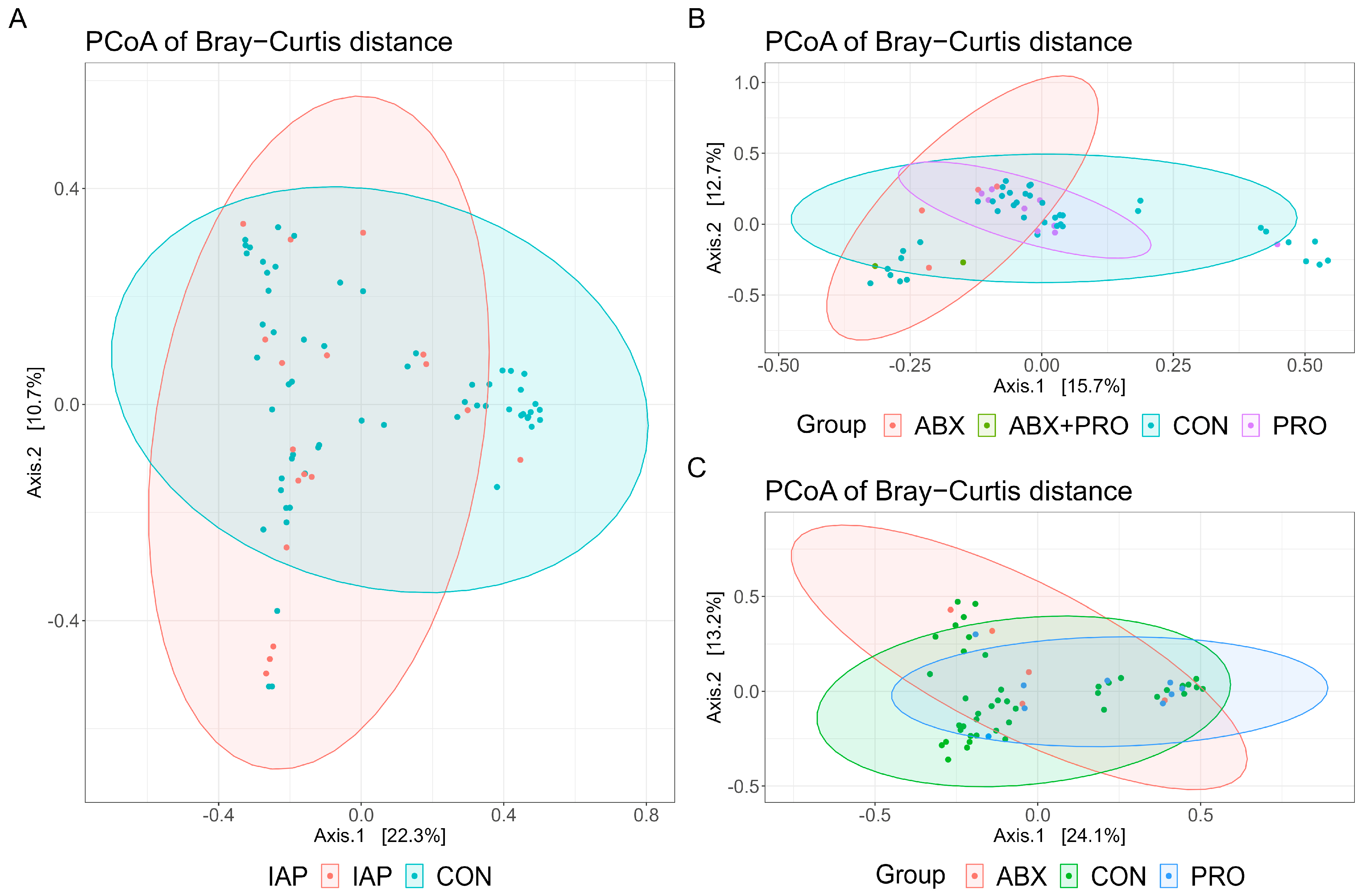
2.3. Impact of Antibiotics and Probiotics on Diversity of Gut Microbiota in Infants
2.4. Core Genus Differences Resulting from Usage of Antibiotics and Probiotics
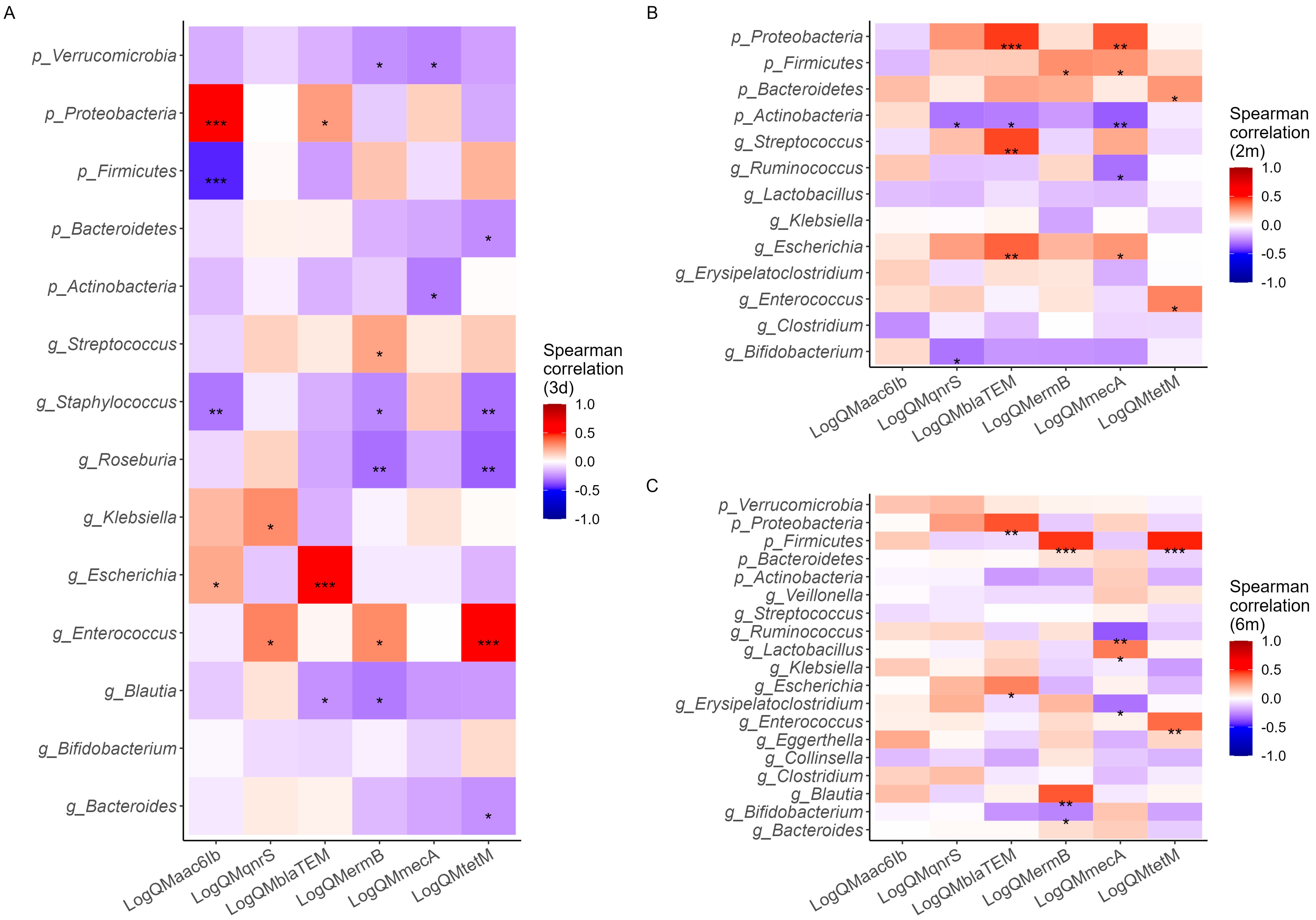
2.5. Effects of Antibiotic and Probiotic Use on Antibiotic Resistance Genes
2.6. Correlation of Antibiotic Resistance Gens with Gut Microbiota Communities
3. Discussion
4. Materials and Methods
4.1. Study Design and Participant Enrollment
4.2. Collection of Sociodemographic Information
4.3. Collection of Fecal Samples
4.4. DNA Extraction and High-Throughput 16s rRNA Gene Amplicon Sequencing
4.5. Detection of Antibiotic-Resistant Genes Using qPCR
4.6. Bioinformatic and Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kundu, P.; Blacher, E.; Elinav, E.; Pettersson, S. Our Gut Microbiome: The Evolving Inner Self. Cell 2017, 171, 1481–1493. [Google Scholar] [CrossRef] [PubMed]
- Lim, E.S.; Wang, D.; Holtz, L.R. The Bacterial Microbiome and Virome Milestones of Infant Development. Trends Microbiol. 2016, 24, 801–810. [Google Scholar] [CrossRef] [PubMed]
- Derrien, M.; Alvarez, A.-S.; Vos, W.M. de The Gut Microbiota in the First Decade of Life. Trends Microbiol. 2019, 27, 997–1010. [Google Scholar] [CrossRef] [PubMed]
- Selma-Royo, M.; Tarrazó, M.; García-Mantrana, I.; Gómez-Gallego, C.; Salminen, S.; Collado, M.C. Shaping Microbiota During the First 1000 Days of Life. Adv. Exp. Med. Biol. 2019, 1125, 3–24. [Google Scholar] [PubMed]
- Milani, C.; Duranti, S.; Bottacini, F.; Casey, E.; Turroni, F.; Mahony, J.; Belzer, C.; Delgado Palacio, S.; Arboleya Montes, S.; Mancabelli, L.; et al. The First Microbial Colonizers of the Human Gut: Composition, Activities, and Health Implications of the Infant Gut Microbiota. Microbiol. Mol. Biol. Rev. 2017, 81, e00036-17. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Wang, Y.; Wang, J.; Lowe, A.J.; Grzeskowiak, L.E.; Hu, Y.J. Early-Life Antibiotic Exposure and Childhood Asthma Trajectories: A National Population-Based Birth Cohort. Antibiotics 2023, 12, 314. [Google Scholar] [CrossRef] [PubMed]
- Korpela, K.; Salonen, A.; Vepsäläinen, O.; Suomalainen, M.; Kolmeder, C.; Varjosalo, M.; Miettinen, S.; Kukkonen, K.; Savilahti, E.; Kuitunen, M.; et al. Probiotic Supplementation Restores Normal Microbiota Composition and Function in Antibiotic-Treated and in Caesarean-Born Infants. Microbiome 2018, 6, 182. [Google Scholar] [CrossRef] [PubMed]
- Azad, M.; Konya, T.; Persaud, R.; Guttman, D.; Chari, R.; Field, C.; Sears, M.; Mandhane, P.; Turvey, S.; Subbarao, P.; et al. Impact of Maternal Intrapartum Antibiotics, Method of Birth and Breastfeeding on Gut Microbiota during the First Year of Life: A Prospective Cohort Study. BJOG Int. J. Obstet. Gynaecol. 2016, 123, 983–993. [Google Scholar] [CrossRef] [PubMed]
- Montoya-Williams, D.; Lemas, D.J.; Spiryda, L.; Patel, K.; Carney, O.O.; Neu, J.; Carson, T.L. The Neonatal Microbiome and Its Partial Role in Mediating the Association between Birth by Cesarean Section and Adverse Pediatric Outcomes. Neonatology 2018, 114, 103–111. [Google Scholar] [CrossRef] [PubMed]
- Stearns, J.C.; Simioni, J.; Gunn, E.; McDonald, H.; Holloway, A.C.; Thabane, L.; Mousseau, A.; Schertzer, J.D.; Ratcliffe, E.M.; Rossi, L.; et al. Intrapartum Antibiotics for GBS Prophylaxis Alter Colonization Patterns in the Early Infant Gut Microbiome of Low Risk Infants. Sci. Rep. 2017, 7, 16527. [Google Scholar] [CrossRef] [PubMed]
- Nogacka, A.; Salazar, N.; Suárez, M.; Milani, C.; Arboleya, S.; Solís, G.; Fernández, N.; Alaez, L.; Hernández-Barranco, A.M.; de Los Reyes-Gavilán, C.G.; et al. Impact of Intrapartum Antimicrobial Prophylaxis upon the Intestinal Microbiota and the Prevalence of Antibiotic Resistance Genes in Vaginally Delivered Full-Term Neonates. Microbiome 2017, 5, 93. [Google Scholar] [CrossRef] [PubMed]
- Wushouer, H.; Du, K.; Yu, J.; Zhang, W.; Hu, L.; Ko, W.; Fu, M.; Zheng, B.; Shi, L.; Guan, X. Outpatient Antibiotic Prescribing Patterns in Children among Primary Healthcare Institutions in China: A Nationwide Retrospective Study, 2017–2019. Antibiotics 2024, 13, 70. [Google Scholar] [CrossRef] [PubMed]
- Aversa, Z.; Atkinson, E.J.; Schafer, M.J.; Theiler, R.N.; Rocca, W.A.; Blaser, M.J.; LeBrasseur, N.K. Association of Infant Antibiotic Exposure With Childhood Health Outcomes. Mayo Clin. Proc. 2021, 96, 66–77. [Google Scholar] [CrossRef] [PubMed]
- Aires, J. First 1000 Days of Life: Consequences of Antibiotics on Gut Microbiota. Front. Microbiol. 2021, 12, 681427. [Google Scholar] [CrossRef] [PubMed]
- Cotten, C.M. Adverse Consequences of Neonatal Antibiotic Exposure. Curr. Opin. Pediatr. 2016, 28, 141–149. [Google Scholar] [CrossRef] [PubMed]
- Rueda-Robles, A.; Rodríguez-Lara, A.; Meyers, M.S.; Sáez-Lara, M.J.; Álvarez-Mercado, A.I. Effect of Probiotics on Host-Microbiota in Bacterial Infections. Pathogens 2022, 11, 986. [Google Scholar] [CrossRef] [PubMed]
- Esaiassen, E.; Hjerde, E.; Cavanagh, J.P.; Pedersen, T.; Andresen, J.H.; Rettedal, S.I.; Støen, R.; Nakstad, B.; Willassen, N.P.; Klingenberg, C. Effects of Probiotic Supplementation on the Gut Microbiota and Antibiotic Resistome Development in Preterm Infants. Front. Pediatr. 2018, 6, 347. [Google Scholar] [CrossRef] [PubMed]
- Ghoshal, U.C.; Gwee, K.-A.; Holtmann, G.; Li, Y.; Park, S.J.; Simadibrata, M.; Sugano, K.; Cohen, H.; Quigley, E.M.M. Physician Perceptions on the Use of Antibiotics and Probiotics in Adults: An International Survey in the Asia-Pacific Area. Front. Cell Infect. Microbiol. 2021, 11, 722700. [Google Scholar] [CrossRef] [PubMed]
- Barratt, M.J.; Nuzhat, S.; Ahsan, K.; Frese, S.A.; Arzamasov, A.A.; Sarker, S.A.; Islam, M.M.; Palit, P.; Islam, M.R.; Hibberd, M.C.; et al. Bifidobacterium Infantis Treatment Promotes Weight Gain in Bangladeshi Infants with Severe Acute Malnutrition. Sci. Transl. Med. 2022, 14, eabk1107. [Google Scholar] [CrossRef] [PubMed]
- Alcon-Giner, C.; Dalby, M.J.; Caim, S.; Ketskemety, J.; Shaw, A.; Sim, K.; Lawson, M.A.E.; Kiu, R.; Leclaire, C.; Chalklen, L.; et al. Microbiota Supplementation with Bifidobacterium and Lactobacillus Modifies the Preterm Infant Gut Microbiota and Metabolome: An Observational Study. Cell Rep. Med. 2020, 1, 100077. [Google Scholar] [CrossRef] [PubMed]
- Ljungquist, O.; Kampmann, C.; Resman, F.; Riesbeck, K.; Tham, J. Probiotics for Intestinal Decolonization of ESBL-Producing Enterobacteriaceae: A Randomized, Placebo-Controlled Clinical Trial. Clin. Microbiol. Infect. 2020, 26, 456–462. [Google Scholar] [CrossRef] [PubMed]
- Tóth, A.G.; Judge, M.F.; Nagy, S.Á.; Papp, M.; Solymosi, N. A Survey on Antimicrobial Resistance Genes of Frequently Used Probiotic Bacteria, 1901 to 2022. Eurosurveillance 2023, 28, 2200272. [Google Scholar] [CrossRef] [PubMed]
- Vangay, P.; Ward, T.; Gerber, J.S.; Knights, D. Antibiotics, Pediatric Dysbiosis, and Disease. Cell Host Microbe 2015, 17, 553–564. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.-Y.; Chiang Chiau, J.-S.; Chang, J.-H.; Hsu, C.-H.; Lin, C.-Y.; Ko, M.H.-J.; Lee, H.-C. Characteristics of Gut Microbiota in Small for Gestational Age Infants with Very Low Birth Weight. Nutrients 2022, 14, 5158. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Lu, Y.; Teng, K.-L.; Chen, M.-L.; Zheng, H.-J.; Zhu, Y.-Q.; Zhong, J. Complete Genome Sequence of Lactococcus Lactis Subsp. Lactis CV56, a Probiotic Strain Isolated from the Vaginas of Healthy Women. J. Bacteriol. 2011, 193, 2886–2887. [Google Scholar] [CrossRef] [PubMed]
- Murphy, R.; Morgan, X.C.; Wang, X.Y.; Wickens, K.; Purdie, G.; Fitzharris, P.; Otal, A.; Lawley, B.; Stanley, T.; Barthow, C.; et al. Eczema-Protective Probiotic Alters Infant Gut Microbiome Functional Capacity but Not Composition: Sub-Sample Analysis from a RCT. Benef. Microbes 2019, 10, 5–17. [Google Scholar] [CrossRef] [PubMed]
- Zaidi, A.Z.; Moore, S.E.; Okala, S.G. Impact of Maternal Nutritional Supplementation during Pregnancy and Lactation on the Infant Gut or Breastmilk Microbiota: A Systematic Review. Nutrients 2021, 13, 1137. [Google Scholar] [CrossRef] [PubMed]
- Saturio, S.; Suárez, M.; Mancabelli, L.; Fernández, N.; Mantecón, L.; de los Reyes-Gavilán, C.G.; Ventura, M.; Gueimonde, M.; Arboleya, S.; Solís, G. Effect of Intrapartum Antibiotics Prophylaxis on the Bifidobacterial Establishment within the Neonatal Gut. Microorganisms 2021, 9, 1867. [Google Scholar] [CrossRef] [PubMed]
- Stinson, L.F.; Payne, M.S.; Keelan, J.A. A Critical Review of the Bacterial Baptism Hypothesis and the Impact of Cesarean Delivery on the Infant Microbiome. Front. Med. 2018, 5, 135. [Google Scholar] [CrossRef] [PubMed]
- Mazzola, G.; Murphy, K.; Ross, R.P.; Di Gioia, D.; Biavati, B.; Corvaglia, L.T.; Faldella, G.; Stanton, C. Early Gut Microbiota Perturbations Following Intrapartum Antibiotic Prophylaxis to Prevent Group B Streptococcal Disease. PLoS ONE 2016, 11, e0157527. [Google Scholar] [CrossRef] [PubMed]
- Dierikx, T.; Berkhout, D.; Eck, A.; Tims, S.; van Limbergen, J.; Visser, D.; de Boer, M.; de Boer, N.; Touw, D.; Benninga, M.; et al. Influence of Timing of Maternal Antibiotic Administration during Caesarean Section on Infant Microbial Colonisation: A Randomised Controlled Trial. Gut 2022, 71, 1803–1811. [Google Scholar] [CrossRef] [PubMed]
- Ren, J.; Li, H.; Zeng, G.; Pang, B.; Wang, Q.; Wei, J. Gut Microbiome-Mediated Mechanisms in Aging-Related Diseases: Are Probiotics Ready for Prime Time? Front. Pharmacol. 2023, 14, 1178596. [Google Scholar] [CrossRef] [PubMed]
- Fu, X.; Lyu, L.; Wang, Y.; Zhang, Y.; Guo, X.; Chen, Q.; Liu, C. Safety Assessment and Probiotic Characteristics of Enterococcus Lactis JDM1. Microb. Pathog. 2022, 163, 105380. [Google Scholar] [CrossRef] [PubMed]
- Arrieta, M.-C.; Stiemsma, L.T.; Amenyogbe, N.; Brown, E.M.; Finlay, B. The Intestinal Microbiome in Early Life: Health and Disease. Front. Immunol. 2014, 5, 427. [Google Scholar] [CrossRef] [PubMed]
- Nance, C.L.; Deniskin, R.; Diaz, V.C.; Paul, M.; Anvari, S.; Anagnostou, A. The Role of the Microbiome in Food Allergy: A Review. Children 2020, 7, 50. [Google Scholar] [CrossRef] [PubMed]
- Loo, E.X.L.; Zain, A.; Yap, G.C.; Purbojati, R.W.; Drautz-Moses, D.I.; Koh, Y.Q.; Chong, Y.S.; Tan, K.H.; Gluckman, P.D.; Yap, F.; et al. Longitudinal Assessment of Antibiotic Resistance Gene Profiles in Gut Microbiomes of Infants at Risk of Eczema. BMC Infect. Dis. 2020, 20, 312. [Google Scholar] [CrossRef] [PubMed]
- Ouwehand, A.C.; Forssten, S.; Hibberd, A.A.; Lyra, A.; Stahl, B. Probiotic Approach to Prevent Antibiotic Resistance. Ann. Med. 2016, 48, 246–255. [Google Scholar] [CrossRef] [PubMed]
- Pieniz, S.; Andreazza, R.; Anghinoni, T.; Camargo, F.; Brandelli, A. Probiotic Potential, Antimicrobial and Antioxidant Activities of Enterococcus Durans Strain LAB18s. Food Control 2014, 37, 251–256. [Google Scholar] [CrossRef]
- Neut, C.; Mahieux, S.; Dubreuil, L.J. Antibiotic Susceptibility of Probiotic Strains: Is It Reasonable to Combine Probiotics with Antibiotics? Médecine Mal. Infect. 2017, 47, 477–483. [Google Scholar] [CrossRef] [PubMed]
- Hollenbeck, B.L.; Rice, L.B. Intrinsic and Acquired Resistance Mechanisms in Enterococcus. Virulence 2012, 3, 421–433. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Yang, Y.; Ma, L.; Ju, F.; Guo, F.; Tiedje, J.M.; Zhang, T. Metagenomic and Network Analysis Reveal Wide Distribution and Co-Occurrence of Environmental Antibiotic Resistance Genes. ISME J. 2015, 9, 2490–2502. [Google Scholar] [CrossRef]
- Wu, G.; Zhang, C.; Wang, J.; Zhang, F.; Wang, R.; Shen, J.; Wang, L.; Pang, X.; Zhang, X.; Zhao, L.; et al. Diminution of the Gut Resistome after a Gut Microbiota-Targeted Dietary Intervention in Obese Children. Sci. Rep. 2016, 6, 24030. [Google Scholar] [CrossRef] [PubMed]
- Qi, Q.; Wang, L.; Gebremedhin, M.A.; Li, S.; Wang, X.; Shen, J.; Zhu, Y.; Andegiorgish, A.K.; Cheng, Y.; Shi, L.; et al. The Impact of Early-Life Antibiotics and Probiotics on Gut Microbial Ecology and Infant Health Outcomes: A Pregnancy and Birth Cohort in Northwest China (PBCC) Study Protocol. BMC Pediatr. 2022, 22, 738. [Google Scholar] [CrossRef] [PubMed]
- Pinto-Lopes, R.; Sousa-Pinto, B.; Azevedo, L. Single Dose versus Multiple Dose of Antibiotic Prophylaxis in Caesarean Section: A Systematic Review and Meta-Analysis. BJOG Int. J. Obstet. Gynaecol. 2017, 124, 595–605. [Google Scholar] [CrossRef] [PubMed]
- Russell, N.J.; Seale, A.C.; O’Sullivan, C.; Le Doare, K.; Heath, P.T.; Lawn, J.E.; Bartlett, L.; Cutland, C.; Gravett, M.; Ip, M.; et al. Risk of Early-Onset Neonatal Group B Streptococcal Disease with Maternal Colonization Worldwide: Systematic Review and Meta-Analyses. Clin. Infect. Dis. 2017, 65, S152–S159. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Antibiotic Categorization. Available online: https://aware.essentialmeds.org/list (accessed on 4 June 2024).
- Liu, H.; Hou, C.; Li, N.; Zhang, X.; Zhang, G.; Yang, F.; Zeng, X.; Liu, Z.; Qiao, S. Microbial and Metabolic Alterations in Gut Microbiota of Sows during Pregnancy and Lactation. FASEB J. 2019, 33, 4490–4501. [Google Scholar] [CrossRef] [PubMed]
- Bolger, A.M.; Lohse, M.; Usadel, B. Trimmomatic: A Flexible Trimmer for Illumina Sequence Data. Bioinformatics 2014, 30, 2114–2120. [Google Scholar] [CrossRef] [PubMed]
- Martin, M. Cutadapt Removes Adapter Sequences from High-Throughput Sequencing Reads. EMBnet J. 2011, 17, 10–12. [Google Scholar] [CrossRef]
- Callahan, B.J.; McMurdie, P.J.; Rosen, M.J.; Han, A.W.; Johnson, A.J.A.; Holmes, S.P. DADA2: High-Resolution Sample Inference from Illumina Amplicon Data. Nat. Methods 2016, 13, 581–583. [Google Scholar] [CrossRef] [PubMed]
- Bolyen, E.; Rideout, J.R.; Dillon, M.R.; Bokulich, N.A.; Abnet, C.C.; Al-Ghalith, G.A.; Alexander, H.; Alm, E.J.; Arumugam, M.; Asnicar, F.; et al. Reproducible, Interactive, Scalable and Extensible Microbiome Data Science Using QIIME 2. Nat. Biotechnol. 2019, 37, 852–857. [Google Scholar] [CrossRef]
- Quast, C.; Pruesse, E.; Yilmaz, P.; Gerken, J.; Schweer, T.; Yarza, P.; Peplies, J.; Glöckner, F.O. The SILVA Ribosomal RNA Gene Database Project: Improved Data Processing and Web-Based Tools. Nucleic Acids Res. 2013, 41, D590–D596. [Google Scholar] [CrossRef] [PubMed]
- Gosalbes, M.J.; Vallès, Y.; Jiménez-Hernández, N.; Balle, C.; Riva, P.; Miravet-Verde, S.; de Vries, L.E.; Llop, S.; Agersø, Y.; Sørensen, S.J.; et al. High Frequencies of Antibiotic Resistance Genes in Infants’ Meconium and Early Fecal Samples. J. Dev. Orig. Health Dis. 2016, 7, 35–44. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Wang, H.H. Impact of Microbiota Transplant on Resistome of Gut Microbiota in Gnotobiotic Piglets and Human Subjects. Front. Microbiol. 2020, 11, 932. [Google Scholar] [CrossRef] [PubMed]
- McMurdie, P.J.; Holmes, S. Phyloseq: An R Package for Reproducible Interactive Analysis and Graphics of Microbiome Census Data. PLoS ONE 2013, 8, e61217. [Google Scholar] [CrossRef] [PubMed]
- McMurdie, P.J.; Holmes, S. Waste Not, Want Not: Why Rarefying Microbiome Data Is Inadmissible. PLoS Comput. Biol. 2014, 10, e1003531. [Google Scholar] [CrossRef] [PubMed]
- Lahti, L.; Shetty, S. Introduction to the Microbiome R Package. Available online: https://microbiome.github.io/tutorials/ (accessed on 4 June 2024).
- Lin, H.; Peddada, S.D. Analysis of Compositions of Microbiomes with Bias Correction. Nat. Commun. 2020, 11, 3514. [Google Scholar] [CrossRef] [PubMed]
- Oksanen, J.; Blanchet, F.G.; Friendly, M.; Kindt, R.; Legendre, P.; McGlinn, D.; Minchin, P.R. Vegan: Community Ecology Package. R Package Version 2.5-6. Available online: https://github.com/vegandevs/vegan (accessed on 4 June 2024).
- Wickham, H. Mastering the Grammar. In ggplot2: Elegant Graphics for Data Analysis; Springer: New York, NY, USA, 2016; pp. 27–40. [Google Scholar]
| Variable | First 3d | 2 m | 6 m | |
|---|---|---|---|---|
| n = 189 | 77 | 55 | 57 | |
| Mother | ||||
| Age (Year) | Mean ± SD | 27.4 ± 3.6 | 26.8 ± 3.6 | 27.6 ± 3.3 |
| <25 | 21 (27.3) | 20 (36.4) | 12 (21.1) | |
| ≥25 | 56 (72.7) | 35 (63.6) | 45 (78.9) | |
| Education (Year) a | Mean ± SD | 10.6 ± 2.7 | 10.7 ± 2.7 | 10.7 ± 3.1 |
| <9 | 42 (55.3) | 30 (55.6) | 32 (57.1) | |
| ≥9 | 34 (44.7) | 24 (44.4) | 24 (42.9) | |
| Occupation b | ||||
| Farmer | 59 (77.6) | 41 (75.9) | 44 (78.6) | |
| Non-farmer | 17 (22.4) | 13 (24.1) | 12 (21.4) | |
| Height (m) | Mean ± SD | 1.6 ± 0.05 | 1.6 ± 0.05 | 1.6 ± 0.05 |
| Weight (kg) | Mean ± SD | 56.0 ± 7.7 | 55.1 ± 7.5 | 54.4 ± 8.0 |
| Pre-pregnancy BMI (kg/m2) | Mean ± SD | 21.8 ± 3.2 | 21.4 ± 2.9 | 21.4 ± 3.2 |
| Delivery mode | ||||
| VD | 54 (70.1) | 42 (76.4) | 41 (71.9) | |
| CS | 23 (29.9) | 13 (23.6) | 16 (28.1) | |
| Infant | ||||
| Gender | ||||
| Male | 36 (46.7) | 22 (40.0) | 26 (45.6) | |
| Female | 41 (53.3) | 33 (60.0) | 31 (54.4) | |
| Gestational age (Week) | Median (P25, P75) | 39.2 (39.0, 40.1) | 39.2 (39.0, 40.1) | 39.2 (39.0, 40.1) |
| Birth weight (g) | Mean ± SD | 3230.5 ± 386.8 | 3183.6 ± 411.5 | 3186.0 ± 377.3 |
| Birth length (cm) c | Mean ± SD | 51.6 ± 1.8 | 51.6 ± 2.0 | 51.3 ± 1.7 |
| IAP | ||||
| Yes | 18 (23.4) | |||
| No | 59 (76.6) | |||
| Only antibiotics (ABX) | 4 (7.3) | 5 (8.8) | ||
| Only probiotics (PRO) | 9 (16.4) | 9 (15.8) | ||
| Both antibiotics and probiotics (ABX + PRO) | 2 (3.6) | 0 | ||
| Neither antibiotics nor probiotics (CON) | 40 (72.7) | 43 (75.4) | ||
| α Diversity Indices | IAP (n = 18) | CON (n = 59) | p Value |
|---|---|---|---|
| Chao1 | |||
| General | 35.5 (23.0, 80.0) | 60.0 (30.0, 86.0) | 0.233 |
| VD | 52.0 (26.0, 89.0) | 58.0 (30.0, 85.0) | 0.871 |
| CS | 25.0 (23.0, 57.0) | 67.5 (40.0, 95.0) | 0.186 |
| Shannon | |||
| General | 1.8 (0.9, 2.3) | 1.7 (0.8, 3.0) | 0.895 |
| VD | 2.2 (1.1, 2.3) | 1.5 (0.7, 2.5) | 0.494 |
| CS | 1.8 (0.5, 2.2) | 2.0 (1.2, 3.3) | 0.208 |
| Simpson | |||
| General | 0.8 (0.4, 0.8) | 0.7 (0.3, 0.9) | 0.914 |
| VD | 0.8 (0.6, 0.8) | 0.6 (0.3, 0.8) | 0.523 |
| CS | 0.7 (0.2, 0.8) | 0.8 (0.5, 0.9) | 0.186 |
| α Diversity Indices | ABX | PRO | ABX + PRO | CON | p Value a |
|---|---|---|---|---|---|
| 2m (n = 55) | 4 | 9 | 2 | 40 | |
| Chao1 | |||||
| General | 85.5 (57.5, 90.0) | 55.0 (34.0, 87.0) | 43.5 (40.0, 47.0) | 42.5 (34.0, 73.5) | 0.405 |
| VD | 83.0 (32.0, 88.0) | 47.0 (34.0, 87.0) | 43.5 (40.0, 47.0) | 43.0 (34.0, 73.0) | 0.793 |
| CS | 92.0 (92.0, 92.0) | 84.0 (28.0, 89.0) | - | 39.0 (34.0, 77.0) | 0.242 |
| Shannon | |||||
| General | 2.2 (2.1, 2.2) | 2.4 (1.7, 2.5) | 2.0 (1.8, 2.2) | 1.9 (1.5, 2.3) | 0.484 |
| VD | 2.1 (2.1, 2.2) | 2.5 (2.2, 2.6) | 2.0 (1.8, 2.2) | 1.9 (1.5, 2.3) | 0.309 |
| CS | 2.2 (2.2, 2.2) | 1.7 (1.2, 2.4) | - | 1.6 (1.2, 2.3) | 0.724 |
| Simpson | |||||
| General | 0.8 (0.8, 0.8) | 0.9 (0.7, 0.9) | 0.8 (0.7, 0.8) | 0.8 (0.6, 0.8) | 0.426 |
| VD | 0.8 (0.8, 0.8) | 0.9 (0.9, 0.9) | 0.8 (0.7, 0.8) | 0.8 (0.7, 0.8) | 0.239 |
| CS | 0.8 (0.8, 0.8) | 0.7 (0.6, 0.9) | - | 0.6 (0.4, 0.8) | 0.724 |
| 6m (n = 57) | 5 | 9 | 0 | 43 | |
| Chao1 | |||||
| General | 85.0 (65.0, 90.0) | 59.0 (40.0, 74.0) | - | 81.0 (44.0, 93.0) | 0.345 |
| VD | 75.0 (50.5, 87.5) | 74.0 (62.0, 91.0) | - | 79.0 (44.0, 91.0) | 0.807 |
| CS | 91.0 (91.0, 91.0) | 34.5 (26.0, 42.5) | - | 82.0 (79.0, 101.0) | 0.049 |
| Shannon | |||||
| General | 1.7 (1.6, 2.0) | 1.8 (1.7, 2.3) | - | 2.0 (1.7, 2.4) | 0.428 |
| VD | 1.7 (1.1, 1.9) | 1.8 (1.7, 2.7) | - | 2.0 (1.7, 2.4) | 0.286 |
| CS | 2.1 (2.1, 2.1) | 1.8 (1.3, 2.1) | - | 2.0 (1.7, 2.2) | 0.726 |
| Simpson | |||||
| General | 0.6 (0.6, 0.7) | 0.7 (0.7, 0.8) | - | 0.8 (0.7, 0.8) | 0.261 |
| VD | 0.6 (0.4, 0.7) | 0.7 (0.7, 0.9) | - | 0.8 (0.7, 0.8) | 0.130 |
| CS | 0.8 (0.8, 0.8) | 0.8 (0.5, 0.8) | - | 0.7 (0.6, 0.8) | 0.820 |
| Core Genus | General (n = 77) | IAP (n = 18) | CON (n = 59) | p Value a |
|---|---|---|---|---|
| ASV1: Escherichia. Escherichia_coli | ||||
| General | 50.1 (13.2, 91.3) | 26.6 (2.1, 88.8) | 52.5 (23, 92) | 0.102 |
| VD | 66.8 (26.5, 96.7) | 56.7 (13.3, 91.3) | 69.3 (31.4, 97.1) | 0.372 |
| CS | 22.5 (0.4, 50.1) | 15.3 (2.1, 33.6) | 32.9 (0.4, 50.1) | 0.659 |
| ASV2: Bifidobacterium. Bifidobacterium_pseudocatenulatum | ||||
| General | 1.6 (0.2, 13.9) | 0.2 (0, 3.7) | 4.2 (0.6, 17.3) | 0.009 |
| VD | 2.3 (0.4, 11) | 0.3 (0, 4.5) | 3.6 (0.6, 11) | 0.147 |
| CS | 1 (0, 14.8) | 0 (0, 3.6) | 10.6 (0.3, 18.3) | 0.035 |
| ASV3: Bifidobacterium. Bifidobacterium_longum | ||||
| General | 1.5 (0.1, 13.5) | 0.5 (0, 17.3) | 2.2 (0.1, 13.5) | 0.709 |
| VD | 1.5 (0.2, 13.4) | 0.5 (0.2, 18.2) | 2.1 (0.3, 12.4) | 0.991 |
| CS | 1.5 (0.1, 17.2) | 0.5 (0, 9.5) | 5.9 (0.1, 17.2) | 0.571 |
| ASV6: Enterococcus. Enterococcus_faecium | ||||
| General | 1.2 (0.1, 6.1) | 2.3 (0.5, 8.2) | 0.7 (0, 6.1) | 0.152 |
| VD | 0.3 (0, 3.6) | 1.2 (0.5, 5.5) | 0.3 (0, 2.8) | 0.104 |
| CS | 6.9 (1.2, 88.7) | 3.4 (0.8, 8.2) | 13.3 (3.8, 88.7) | 0.314 |
| ASV7: Streptococcus. Streptococcus_salivarius | ||||
| General | 1 (0, 5.1) | 1.3 (0.1, 6.5) | 0.4 (0, 4.9) | 0.229 |
| VD | 0.4 (0, 2.9) | 1.2 (0.1, 5.9) | 0.4 (0, 2.2) | 0.384 |
| CS | 3.2 (0.1, 8.7) | 1.4 (0.2, 6.5) | 4 (0, 8.7) | 0.801 |
| ASV30: Staphylococcus. Staphylococcus_epidermidis | ||||
| General | 0.3 (0, 1.7) | 0.5 (0, 4.6) | 0.2 (0, 1.7) | 0.596 |
| VD | 0.1 (0, 1.7) | 0.3 (0.1, 1.4) | 0.1 (0, 1.7) | 0.935 |
| CS | 0.7 (0, 29.5) | 1.6 (0, 34.3) | 0.5 (0.1, 1.7) | 0.488 |
| Core Genus | General (n = 55) | ABX (n = 4) | PRO (n = 9) | CON (n = 40) | p Value b |
|---|---|---|---|---|---|
| ASV1: Escherichia. Escherichia_coli | |||||
| General | 8.8 (1.7, 26.2) | 7.6 (4.5, 23) | 7.1 (5.7, 13.4) | 11.7 (2.4, 35.7) | 0.168 |
| VD | 10 (2.7, 34.1) | 7.3 (1.7, 38) | 6.7 (5.7, 13.4) | 13.7 (5.5, 41) | 0.123 |
| CS | 7.1 (1.6, 15) | 8 (8, 8) | 7.1 (1.6, 15) | 2.2 (1.1, 17.2) | 0.943 |
| ASV2: Bifidobacterium. Bifidobacterium_pseudocatenulatum | |||||
| General | 1.8 (0.2, 11.2) | 13 (7.7, 32.1) | 17.1 (1.1, 33.1) | 1.4 (0.2, 6.5) | 0.064 |
| VD | 1.8 (0.4, 10.6) | 10.6 (4.8, 48.6) | 25.1 (1.2, 41.3) | 1.4 (0.4, 6.7) | 0.057 |
| CS | 1.1 (0.2, 15.5) | 15.5 (15.5, 15.5) | 1.1 (0, 33.1) | 0.6 (0.2, 5.7) | 0.709 |
| ASV3: Bifidobacterium. Bifidobacterium_longum | |||||
| General | 8.7 (1.7, 27) | 31.9 (15.9, 38) | 9.4 (1.4, 19) | 7.4 (1.5, 27) | 0.429 |
| VD | 11.8 (3.8, 28.3) | 29.9 (1.9, 33.8) | 14.2 (1.9, 24.6) | 10.8 (3.8, 29.8) | 0.855 |
| CS | 2.2 (1, 13.3) | 42.2 (42.2, 42.2) | 1.4 (1.1, 13.3) | 2.2 (0, 8.7) | 0.268 |
| ASV4: Bifidobacterium. Bifidobacterium_longum | |||||
| General | 2.2 (1, 10.5) | 0.7 (0.3, 0.9) | 1.7 (1.2, 1.9) | 3.3 (1.3, 22.4) | 0.072 |
| VD | 1.9 (0.8, 8.8) | 0.6 (0, 1) | 1.3 (0, 1.9) | 2.6 (1.1, 20.8) | 0.121 |
| CS | 4.1 (1.8, 70.5) | 0.8 (0.8, 0.8) | 1.8 (1.7, 73.1) | 4.3 (3.1, 70.5) | 0.314 |
| ASV5: Bifidobacterium. Bifidobacterium_breve | |||||
| General | 1.7 (0.5, 13.2) | 18.2 (6.3, 53.1) | 1.7 (0.1, 2.5) | 1.4 (0.5, 12.4) | 0.120 |
| VD | 2.3 (0.3, 13.6) | 12 (0.6, 81.8) | 0.9 (0, 1.9) | 2.7 (0.3, 13.6) | 0.150 |
| CS | 1.4 (0.9, 2.5) | 24.4 (24.4, 24.4) | 2.5 (1.3, 2.5) | 1.1 (0.9, 1.6) | 0.273 |
| ASV6: Enterococcus. Enterococcus_faecium | |||||
| General | 0.8 (0.2, 2.8) | 4.6 (1.9, 9.2) | 4.8 (1.1, 14.3) | 0.5 (0.1, 1.5) | 0.008 |
| VD | 0.8 (0.2, 2.1) | 2.8 (1.1, 11.9) | 3.5 (1.1, 9.7) | 0.5 (0.1, 1.3) | 0.019 |
| CS | 1.3 (0.5, 14.3) | 6.5 (6.5, 6.5) | 14.3 (0.7, 18.9) | 0.5 (0.2, 4.7) | 0.380 |
| ASV7: Streptococcus. Streptococcus_salivarius | |||||
| General | 3.1 (1.1, 9) | 0.9 (0.4, 1.7) | 2.7 (1.3, 6.8) | 3.7 (1.2, 13.6) | 0.117 |
| VD | 3.1 (1.3, 9) | 1.4 (0.3, 2.1) | 4.7 (1.3, 8.5) | 3.5 (1.3, 13.1) | 0.228 |
| CS | 1.6 (0.6, 8.9) | 0.4 (0.4, 0.4) | 1.6 (0.3, 3.1) | 3.9 (0.6, 22.7) | 0.392 |
| ASV13: Bifidobacterium. Bifidobacterium_bifidum | |||||
| General | 1.9 (0.4, 6.7) | 1.4 (0.5, 3.8) | 1.9 (0.8, 14.4) | 2.2 (0.4, 6.4) | 0.737 |
| VD | 2 (0.5, 6.9) | 0.9 (0, 5.6) | 2.8 (1.8, 14.4) | 2.1 (0.4, 6.9) | 0.652 |
| CS | 1.9 (0.4, 3) | 1.9 (1.9, 1.9) | 0.8 (0.2, 14.8) | 2.3 (0.4, 3) | 0.999 |
| ASV18: Ruminococcus. Ruminococcus_gnavus | |||||
| General | 0.3 (0.1, 1.3) | 0.2 (0.1, 0.6) | 0.2 (0.1, 0.9) | 0.3 (0.1, 1.7) | 0.834 |
| VD | 0.5 (0.1, 1.6) | 0.1 (0.1, 0.9) | 0.4 (0, 0.9) | 0.5 (0.1, 2.3) | 0.658 |
| CS | 0.1 (0.1, 0.3) | 0.3 (0.3, 0.3) | 0.1 (0.1, 88.1) | 0.1 (0, 0.3) | 0.590 |
| ASV34: Erysipelatoclostridium. Erysipelatoclostridium_ramosum | |||||
| General | 0.1 (0, 0.5) | 0.1 (0, 0.1) | 0.1 (0.1, 0.3) | 0.1 (0, 0.6) | 0.781 |
| VD | 0.1 (0, 0.6) | 0.1 (0, 0.1) | 0.3 (0.1, 1.8) | 0.1 (0, 0.6) | 0.456 |
| CS | 0 (0, 0) | 0.1 (0.1, 0.1) | 0.1 (0, 0.1) | 0 (0, 0.2) | 0.693 |
| Core Genus | General (n = 57) | ABX (n = 5) | PRO (n = 9) | CON (n = 43) | p Value a |
|---|---|---|---|---|---|
| ASV1: Escherichia. Escherichia_coli | |||||
| General | 9.6 (2.4, 23.8) | 15.8 (1.5, 23.8) | 12.6 (4.3, 26.9) | 8.2 (2.4, 21.8) | 0.911 |
| VD | 6.3 (2, 21.8) | 12.6 (0.9, 45.2) | 17.4 (12.3, 26.9) | 5.1 (2, 17.2) | 0.336 |
| CS | 13.9 (6.2, 28.6) | 15.8 (15.8, 15.8) | 7.2 (1.2, 20.5) | 15.2 (8, 30) | 0.474 |
| ASV2: Bifidobacterium. Bifidobacterium_pseudocatenulatum | |||||
| General | 1.3 (0.7, 10.8) | 1.1 (0.7, 1.2) | 0.7 (0, 1) | 2.4 (0.8, 22.4) | 0.004 |
| VD | 2.4 (1, 19.6) | 1.2 (0.5, 1.8) | 1 (1, 1) | 5.5 (1.1, 26.9) | 0.048 |
| CS | 0.8 (0.3, 1.5) | 0.7 (0.7, 0.7) | 0 (0, 0.3) | 1.3 (0.7, 1.8) | 0.041 |
| ASV3: Bifidobacterium. Bifidobacterium_longum | |||||
| General | 6.7 (1.4, 19.3) | 1.8 (1.6, 6.7) | 1.2 (0.8, 7.1) | 8.8 (1.7, 19.5) | 0.125 |
| VD | 6.9 (1.6, 19.5) | 1.7 (1.1, 4.2) | 1 (0.8, 7.1) | 9.6 (2.2, 22.5) | 0.114 |
| CS | 2.1 (1.1, 15) | 7.7 (7.7, 7.7) | 1.4 (0.6, 19.5) | 2.5 (1, 19.3) | 0.717 |
| ASV4: Bifidobacterium. Bifidobacterium_longum | |||||
| General | 3 (0.9, 52.8) | 0.6 (0.2, 13) | 52.8 (1.6, 60) | 2.7 (1, 48) | 0.393 |
| VD | 1.8 (0.4, 28.8) | 0.4 (0.1, 31) | 58.3 (4.2, 60) | 1.8 (0.4, 13.9) | 0.197 |
| CS | 31.6 (2.1, 60.7) | 13 (13, 13) | 27.2 (0.8, 69.9) | 48 (2.7, 68.1) | 0.870 |
| ASV5: Bifidobacterium. Bifidobacterium_breve | |||||
| General | 1.7 (0.7, 14.1) | 1.5 (1.1, 52.6) | 0.5 (0.2, 0.9) | 2.1 (0.9, 14.8) | 0.106 |
| VD | 1.8 (0.8, 19.4) | 1.3 (0.8, 39.9) | 0.5 (0.4, 0.9) | 4.3 (0.9, 31.1) | 0.276 |
| CS | 1.6 (0.6, 11.4) | 52.6 (52.6, 52.6) | 0.4 (0.1, 26.9) | 1.6 (1.2, 10) | 0.221 |
| ASV6: Enterococcus. Enterococcus_faecium | |||||
| General | 1 (0.2, 2.9) | 0.4 (0.4, 24.4) | 1 (0.2, 1.8) | 1.1 (0.2, 2.9) | 0.938 |
| VD | 0.6 (0.2, 2.5) | 12.4 (0.2, 59.7) | 0.4 (0.1, 1.8) | 0.7 (0.2, 2.4) | 0.701 |
| CS | 1.1 (0.3, 3.5) | 0.4 (0.4, 0.4) | 1 (0.6, 27.3) | 1.9 (0.2, 3.6) | 0.750 |
| ASV7: Streptococcus. Streptococcus_salivarius | |||||
| General | 1 (0.3, 3.2) | 0.5 (0.4, 2.3) | 3.1 (0.7, 4.5) | 0.9 (0.3, 2.2) | 0.655 |
| VD | 0.6 (0.3, 2.2) | 0.5 (0.3, 4) | 3.1 (0.3, 5.3) | 0.9 (0.3, 2) | 0.804 |
| CS | 1.5 (0.4, 4.3) | 2.3 (2.3, 2.3) | 2.5 (0.8, 4.3) | 0.9 (0.3, 8.4) | 0.762 |
| ASV9: Blautia. Blautia_obeum | |||||
| General | 0.3 (0.1, 0.9) | 0.3 (0.2, 0.3) | 0.2 (0, 0.3) | 0.6 (0.2, 1.6) | 0.013 |
| VD | 0.6 (0.2, 1.4) | 0.3 (0.1, 0.6) | 0.3 (0.2, 0.3) | 0.7 (0.2, 2.6) | 0.161 |
| CS | 0.2 (0, 0.4) | 0.2 (0.2, 0.2) | 0 (0, 0) | 0.3 (0.1, 0.5) | 0.047 |
| ASV12: Collinsella. Collinsella_aerofaciens | |||||
| General | 0.1 (0.1, 0.2) | 0.1 (0.1, 0.1) | 0.2 (0, 0.2) | 0.2 (0.1, 0.3) | 0.684 |
| VD | 0.2 (0, 0.9) | 0.1 (0, 0.5) | 0.2 (0.2, 0.2) | 0.2 (0.1, 1.4) | 0.644 |
| CS | 0.07 (0, 0.1) | 0.1 (0.1, 0.1) | 0 (0, 0.1) | 0.1 (0.1, 0.1) | 0.275 |
| ASV13: Bifidobacterium. Bifidobacterium_bifidum | |||||
| General | 2 (0.2, 4.5) | 0.2 (0.1, 1.8) | 0.6 (0.2, 2) | 2.4 (0.3, 5.9) | 0.217 |
| VD | 1.8 (0.2, 4.2) | 0.2 (0, 1) | 0.3 (0.2, 0.8) | 2.2 (0.3, 5.8) | 0.082 |
| CS | 2.5 (0.5, 6.1) | 6.4 (6.4, 6.4) | 1.3 (0.3, 6.3) | 2.6 (0.4, 6.1) | 0.447 |
| ASV18: Ruminococcus. Ruminococcus_gnavus | |||||
| General | 0.3 (0.1, 1.6) | 0.2 (0.1, 0.2) | 0.1 (0, 0.9) | 0.5 (0.2, 2) | 0.256 |
| VD | 0.3 (0.1, 2) | 0.2 (0.1, 3.8) | 0.3 (0.1, 0.9) | 0.5 (0.1, 2.1) | 0.876 |
| CS | 0.3 (0.1, 1.2) | 0.2 (0.2, 0.2) | 0 (0, 0.6) | 0.5 (0.2, 1.6) | 0.178 |
| ASV19: Akkermansia. Akkermansia_muciniphila | |||||
| General | 0.2 (0, 0.5) | 0.2 (0.1, 0.2) | 0.1 (0, 0.2) | 0.2 (0, 0.5) | 0.682 |
| VD | 0.2 (0, 0.5) | 0.2 (0, 0.3) | 0.2 (0.1, 0.2) | 0.2 (0, 0.6) | 0.869 |
| CS | 0.2 (0, 6.4) | 0.2 (0.2, 0.2) | 0 (0, 16) | 0.2 (0.1, 0.4) | 0.531 |
| ASV34: Erysipelatoclostridium. Erysipelatoclostridium_ramosum | |||||
| General | 0.1 (0, 0.8) | 0.1 (0, 0.1) | 0 (0, 0.1) | 0.2 (0.1, 1.1) | 0.026 |
| VD | 0.2 (0, 1.1) | 0.1 (0, 3.4) | 0 (0, 0.1) | 0.2 (0.1, 1.3) | 0.276 |
| CS | 0 (0, 0.3) | 0.1 (0.1, 0.1) | 0 (0, 0) | 0.1 (0.1, 0.8) | 0.117 |
| ASV39: Streptococcus. Streptococcus_oralis | |||||
| General | 0.1 (0, 0.1) | 0.1 (0.1, 0.1) | 0.1 (0, 0.2) | 0.1 (0, 0.1) | 0.596 |
| VD | 0 (0, 0.1) | 0.1 (0, 0.1) | 0.1 (0.1, 0.1) | 0.1 (0, 0.1) | 0.696 |
| CS | 0 (0, 0.1) | 0.2 (0.2, 0.2) | 0.1 (0, 3.8) | 0 (0, 0.1) | 0.376 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Qi, Q.; Wang, L.; Zhu, Y.; Li, S.; Gebremedhin, M.A.; Wang, B.; Zhu, Z.; Zeng, L. Unraveling the Microbial Symphony: Impact of Antibiotics and Probiotics on Infant Gut Ecology and Antibiotic Resistance in the First Six Months of Life. Antibiotics 2024, 13, 602. https://doi.org/10.3390/antibiotics13070602
Qi Q, Wang L, Zhu Y, Li S, Gebremedhin MA, Wang B, Zhu Z, Zeng L. Unraveling the Microbial Symphony: Impact of Antibiotics and Probiotics on Infant Gut Ecology and Antibiotic Resistance in the First Six Months of Life. Antibiotics. 2024; 13(7):602. https://doi.org/10.3390/antibiotics13070602
Chicago/Turabian StyleQi, Qi, Liang Wang, Yingze Zhu, Shaoru Li, Mitslal Abrha Gebremedhin, Baozhu Wang, Zhonghai Zhu, and Lingxia Zeng. 2024. "Unraveling the Microbial Symphony: Impact of Antibiotics and Probiotics on Infant Gut Ecology and Antibiotic Resistance in the First Six Months of Life" Antibiotics 13, no. 7: 602. https://doi.org/10.3390/antibiotics13070602






