Application of Physiologically Based Pharmacokinetic Model to Delineate the Impact of Aging and Renal Impairment on Ceftazidime Clearance
Abstract
:1. Introduction
2. Results
3. Discussion
4. Materials and Methods
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
- The following virtual trial settings were used to replicate studies investigating ceftazidime PK in young adult and elderly subjects after i.v. administration.
| Trial (Ref.) | Trial Code: Virtual Trial Settings |
| Trial A [26] | Trial A1: Healthy-Pop (18–39 years): a bolus of 2 g to 200 individuals (40% female) Trial A2: Healthy-Pop (40–59 years): a bolus of 2 g to 200 individuals (50% female) Trial A3: Healthy-Pop (60–79 years): a bolus of 2 g to 200 individuals (23% female) Trial A4: Healthy-Pop (80–95 years): a bolus of 2 g to 200 individuals (44% female) |
| Trial B [27] | Trial B1: Healthy-Pop (23–31 years): a bolus of 2 g to 200 individuals (0% female) Trial B2: Healthy-Pop (63–76 years): a bolus of 2 g to 200 individuals (0% female) |
| Trial C [25] | Trial C1: Healthy-Pop (24–32 years): a bolus of 2 g to 200 individuals (0.5% female) Trial C2: Healthy-Pop (65–83 years): a bolus of 2 g to 200 individuals (0.15% female) |
| Trial D [30] | Trial D1: Healthy-Pop (19–29 years): a bolus of 1 g to 200 individuals (50% female) Trial D2: Healthy-Pop (57–73 years): a bolus of 1 g to 200 individuals (0% female) |
| Trial E [28] | Trial E: Healthy-Pop (67–75 years): a 30-min infusion of 2 g to 200 individuals (50% female) |
| Trial F [29] | Trial F: Healthy-Pop (69–91 years): a 30-min infusion dose of 2 g to 200 individuals (0% female). |
| Trial G [31] | Trial G: Healthy-Pop (68–82 years): a bolus of 1 g to 200 individuals (0.33% female) |
- 2.
- The following trial designs were used for predicting ceftazidime PK in individuals with varying degrees of renal impairment after i.v. administration.
| Trial (Ref.) | Trial Code: Virtual Trial Settings |
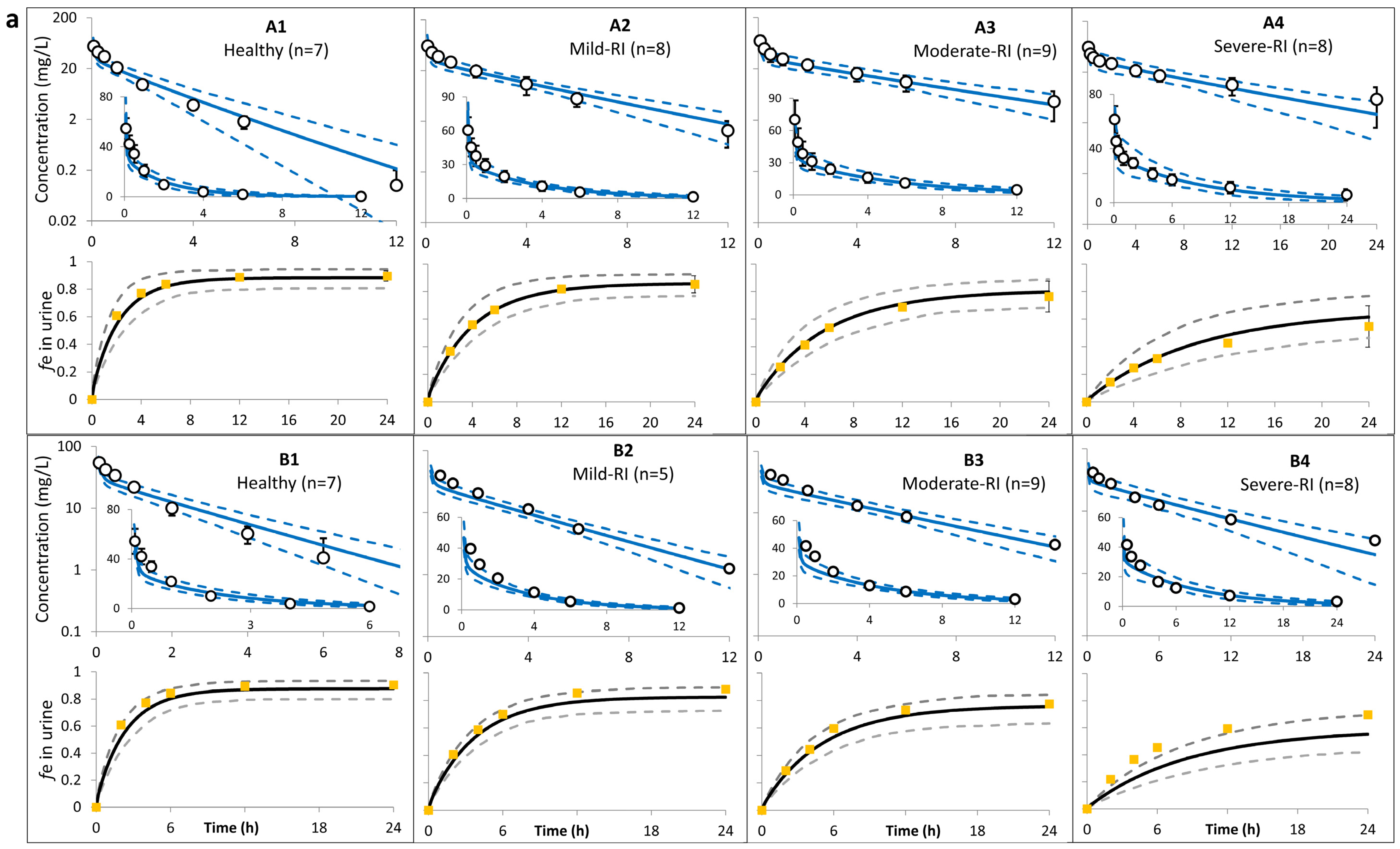
| Trial A (Ohkawa [32]) | Trial A1: Healthy-Pop: a bolus of 0.5 g to 200 individuals (43% female) aged 20–65 years, with CLcr of 105–133 mL/min/1.73 m2. Trial A2: Mild-RI-Pop: a bolus of 0.5 g to 200 individuals (43% female) aged 20–87 years, with CLcr of 63–89 mL/min/1.73 m2. Trial A3: Moderate-RI-Pop: a bolus of 0.5 g to 200 individuals (43% female) aged 20–87 years, with CLcr of 30–57 mL/min/1.73 m2. Trial A4: Severe-RI-Pop: a bolus of 0.5 g to 200 individuals (43% female) aged 20–87 years, with CLcr of 8–29 mL/min/1.73 m2. |
| Trial B (Saito [33]) | Trial B1: Healthy-Pop: a bolus of 1 g to 200 individuals (0% female) aged 20–50 years, with CLcr of >90 mL/min. Trial B2: Mild-RI-Pop: a bolus of 1 g to 200 individuals (0% female) aged 20–50 years, with CLcr of 60–89 mL/min. Trial B3: Moderate-RI-Pop: a bolus of 1 g to 200 individuals (0% female) aged 20–50 years, with CLcr of 30–59 mL/min. Trial B4: Severe-RI-Pop: a bolus of 1 g to 200 individuals (0% female) aged 20–50 years, with CLcr of 10–29 mL/min. |
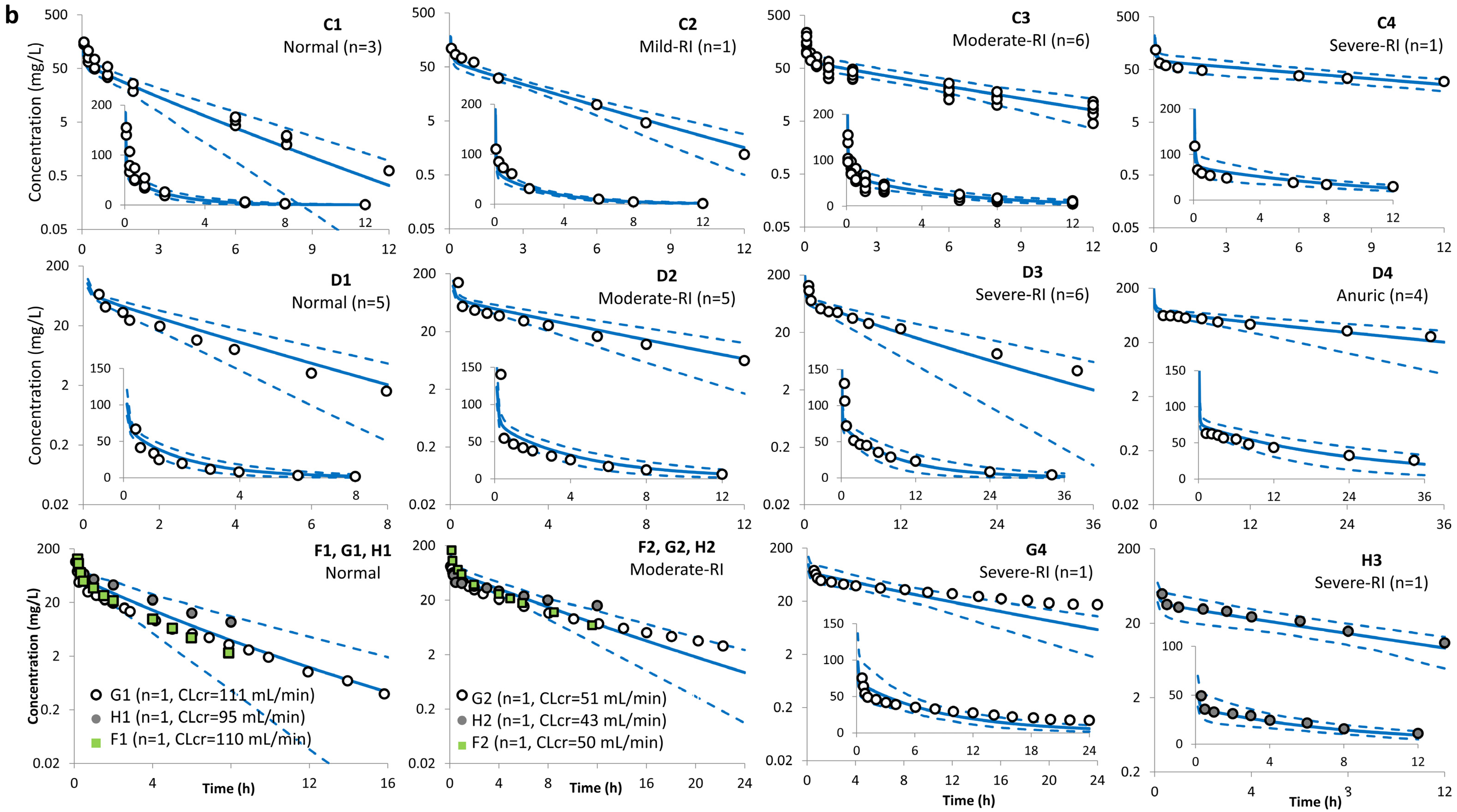
| Trial C (Ackerman [34]) | Trial C1: Healthy-Pop: a bolus of 1 g to 200 individuals (40% female) aged 26–27 years, with CLcr of 97–113 mL/min. Trial C2: Mild-RI-Pop: a bolus of 1 g to 200 individuals (40% female) aged 27 years with, CLcr of 75 mL/min. Trial C3: Moderate-RI-Pop: a bolus of 1 g to 200 individuals (40% female) aged 33–74 years with, CLcr of 34–45 mL/min. Trial C4: Severe-RI-Pop: a bolus of 1 g to 200 individuals (40% female) aged 78 years with, CLcr of 6 mL/min using lowest limit CLcr of 15 mL/min). |
| Trial D (Leroy [35]) | Trial D1: Healthy-Pop: a bolus of 15 mg/kg to 200 individuals (32% female) aged 22–31 years, with CLcr of 110–141 mL/min. Trial D2: Moderate-RI-Pop: a bolus of 15 mg/kg to 200 individuals (32% female) aged 26–74 years, with CLcr of 39–73 mL/min. Trial D3: Severe-RI-Pop: a bolus of 15 mg/kg to 200 individuals (32% female) aged 26–74 years, with CLcr of 14–27 mL/min. Trial D4: Severe-RI-Pop: a bolus of 15 mg/kg to 200 individuals (32% female) aged 26–74 years, with CLR reset to zero. |
| Trial E (Norrby [37]) | Trial E1: Healthy-Pop: a 20-min infusion of 1 g to 200 individuals (33% female) aged 57–77 years, with CLEDTA 92–146 mL/min/1.73 m2. Trial E2: Mild-RI-Pop: a 20-min infusion of 1 g to 200 individuals (60% female) aged 69–84 years, with CLEDTA 60–76 mL/min/1.73 m2. Trial E3: Moderate-RI-Pop: a 20-min infusion of 1 g to 200 individuals (33% female) aged 57–77 years, with CLEDTA 47–54 mL/min/1.73 m2. |
| Trial F (Welage [40]) | Trial F1: Healthy-Pop: a bolus of 1 g to 200 individuals (0% female) aged 30–36 years, with CLcr of 110–122 mL/min. Trial F2: Moderate-RI-Pop: a bolus of 1 g to 200 individuals (20% female) aged 49–69 years, with CLcr of 34–53 mL/min. Trial F3: Severe-RI-Pop: a bolus of 1 g to 200 individuals (0%female) aged 27–91 years, with CLcr of 21–29.5 mL/min. |
| Trial G (van Dalen [38]) | Trial G1: Healthy-Pop: a bolus of 1 g to 200 individuals (30% female) aged 34–65 years, with CLcr of 93–134 mL/min. Trial G2: Mild-RI-Pop: a bolus of 1 g to 200 individuals (30% female) aged 34–88 years, with CLcr of 72–86 mL/min. Trial G3: Moderate-RI-Pop: an i.v. bolus of 1 g to 200 individuals (30% female) aged 34–88 years, with CLcr of 30–59 mL/min. Trial G4: Severe-RI-Pop: an i.v. bolus of 1 g to 200 individuals (30% female) aged 34–88 years, with CLcr of 9–20 mL/min. |
| Trial H (Walstad [39]) | Trial H1: Mild-RI-Pop: a bolus of 1 g to 200 individuals (57% female) aged 28–89 years, with CLcr ≥50 mL/min. Trial H2: Moderate-RI-Pop: a bolus of 1 g to 200 individuals (57% female) aged 28–89 years, with CLcr 31–50 mL/min. Trial H3: Severe-RI-Pop: a bolus of 0.5 g to 200 individuals (57% female) aged 28–89 years, with CLcr 16–30 mL/min. |
| Trial I (Lin [36]) | Trial I1: Mild-RI-Pop: two 30-min infusions of 2 g each to 200 individuals (33% female) aged 21–74 years, with CLcr of 51–94 mL/min. Trial I2: Severe-RI-Pop: two 30-min infusions of 2 g each to 200 individuals (38% female) aged 58–75 years, with CLcr of 10–35 mL/min. |
References
- United Nations. Population Divisions. World Population Ageing 2017—Highlights. United Nations, Department of Economic and Social Affairs. 2017. Available online: https://www.un.org/en/development/desa/population/publications/pdf/ageing/WPA2017_Highlights.pdf (accessed on 24 January 2024).
- Avorn, J. Medication use and the elderly: Current status and opportunities. Health Aff. 1995, 14, 276–286. [Google Scholar] [CrossRef] [PubMed]
- Lassiter, J.; Bennett, W.M.; Olyaei, A.J. Drug dosing in elderly patients with chronic kidney disease. Clin. Geriatr. Med. 2013, 29, 657–705. [Google Scholar] [CrossRef]
- Tian, F.; Chen, Z.; Zeng, Y.; Feng, Q.; Chen, X. Prevalence of Use of Potentially Inappropriate Medications Among Older Adults Worldwide: A Systematic Review and Meta-Analysis. JAMA Netw. Open 2023, 6, e2326910. [Google Scholar] [CrossRef]
- Maher, R.L.; Hanlon, J.; Hajjar, E.R. Clinical consequences of polypharmacy in elderly. Expert. Opin. Drug Saf. 2014, 13, 57–65. [Google Scholar] [CrossRef]
- Florisson, S.; Aagesen, E.K.; Bertelsen, A.S.; Nielsen, L.P.; Rosholm, J.U. Are older adults insufficiently included in clinical trials?-An umbrella review. Basic. Clin. Pharmacol. Toxicol. 2021, 128, 213–223. [Google Scholar] [CrossRef]
- The International Conference on Harmonization (ICH). Studies in Support of Special Populations: Geriatrics E7. 1994. Available online: https://database.ich.org/sites/default/files/E7_Guideline.pdf (accessed on 23 January 2024).
- Food and Drug Administration (FDA). Guidance for Industry. E7 Studies in Support of Special Populations: Geriatrics Questions and Answers. 2012. Available online: https://www.fda.gov/files/drugs/published/E7-Studies-in-Support-of-Special-Populations--Geriatrics--Questions-and-Answers.pdf (accessed on 5 March 2024).
- Hilmer, S.N.; Gnjidic, D.; Abernethy, D.R. Pharmacoepidemiology in the postmarketing assessment of the safety and efficacy of drugs in older adults. J. Gerontol. A Biol. Sci. Med. Sci. 2012, 67, 181–188. [Google Scholar] [CrossRef]
- Coetzee, E.; Absalom, A.R. Pharmacokinetic and Pharmacodynamic Changes in the Elderly: Impact on Anesthetics. Anesth. Clin. 2023, 41, 549–565. [Google Scholar] [CrossRef]
- Jamei, M.; Dickinson, G.L.; Rostami-Hodjegan, A. A framework for assessing inter-individual variability in pharmacokinetics using virtual human populations and integrating general knowledge of physical chemistry, biology, anatomy, physiology and genetics: A tale of ‘bottom-up’ vs ‘top-down’ recognition of covariates. Drug Metab. Pharmacokinet. 2009, 24, 53–75. [Google Scholar] [CrossRef]
- Turnheim, K. Pharmacokinetic dosage guidelines for elderly subjects. Expert Opin Drug Metab. Toxicol. 2005, 1, 33–48. [Google Scholar] [CrossRef]
- Mangoni, A.A. Cardiovascular drug therapy in elderly patients: Specific age-related pharmacokinetic, pharmacodynamic and therapeutic considerations. Drugs Aging 2005, 22, 913–941. [Google Scholar] [CrossRef]
- Sobamowo, H.; Prabhakar, S.S. The Kidney in Aging: Physiological Changes and Pathological Implications. Prog. Mol. Biol. Transl. Sci. 2017, 146, 303–340. [Google Scholar] [CrossRef]
- Davies, D.F.; Shock, N.W. Age changes in glomerular filtration rate, effective renal plasma flow, and tubular excretory capacity in adult males. J. Clin. Invest. 1950, 29, 496–507. [Google Scholar] [CrossRef]
- DeSanto, N.G.; Anastasio, P.; Coppola, S.; Barba, G.; Jadanza, A.; Capasso, G. Age-related changes in renal reserve and renal tubular function in healthy humans. Child. Nephrol. Urol. 1991, 11, 33–40. [Google Scholar] [PubMed]
- European Medicines Agency (EMA). Guideline on the Evaluation of the Pharmacokinetics of Medicinal Products in Patients with Decreased Renal Function. 2015. Available online: https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-evaluation-pharmacokinetics-medicinal-products-patients-decreased-renal-function_en.pdf (accessed on 15 February 2024).
- US Food and Drug Administration (FDA). Pharmacokinetics in Patients with Impaired Renal Function—Study Design, Data Analysis, and Impact on Dosing. Guidance for Industry. March 2024. Available online: https://www.fda.gov/media/78573/download (accessed on 5 March 2024).
- Chetty, M.; Johnson, T.N.; Polak, S.; Salem, F.; Doki, K.; Rostami-Hodjegan, A. Physiologically based pharmacokinetic modelling to guide drug delivery in older people. Adv. Drug Deliv. Rev. 2018, 135, 85–96. [Google Scholar] [CrossRef]
- Polasek, T.M.; Patel, F.; Jensen, B.P.; Sorich, M.J.; Wiese, M.D.; Doogue, M.P. Predicted metabolic drug clearance with increasing adult age. Br. J. Clin. Pharmacol. 2013, 75, 1019–1028. [Google Scholar] [CrossRef] [PubMed]
- De Sousa Mendes, M.; Chetty, M. Are Standard Doses of Renally-Excreted Antiretrovirals in Older Patients Appropriate: A PBPK Study Comparing Exposures in the Elderly Population With Those in Renal Impairment. Drugs R D 2019, 19, 339–350. [Google Scholar] [CrossRef] [PubMed]
- Schlender, J.F.; Meyer, M.; Thelen, K.; Krauss, M.; Willmann, S.; Eissing, T.; Jaehde, U. Development of a Whole-Body Physiologically Based Pharmacokinetic Approach to Assess the Pharmacokinetics of Drugs in Elderly Individuals. Clin. Pharmacokinet. 2016, 55, 1573–1589. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Tong, X.; Sharma, P.; Xu, H.; Al-Huniti, N.; Zhou, D. Physiologically based pharmacokinetic modelling to predict exposure differences in healthy volunteers and subjects with renal impairment: Ceftazidime case study. Basic. Clin. Pharmacol. Toxicol. 2019, 125, 100–107. [Google Scholar] [CrossRef] [PubMed]
- Abduljalil, K.; Gardner, I.; Jamei, M. An Application of a Physiologically Based Pharmacokinetic Approach to Predict Ceftazidime Pharmacokinetics in a Pregnant Population. Pharmaceutics 2024, 16, 474. [Google Scholar] [CrossRef] [PubMed]
- Naber, K.G.; Kees, F.; Grobecker, H. Ceftazidime: Pharmacokinetics in young volunteers versus elderly patients and therapeutic efficacy with complicated urinary tract infections. J. Antimicrob. Chemother. 1983, 12 (Suppl. SA), 41–45. [Google Scholar] [CrossRef] [PubMed]
- Ljungberg, B.; Nilsson-Ehle, I. Influence of age on the pharmacokinetics of ceftazidime in acutely ill, adult patients. Eur. J. Clin. Pharmacol. 1988, 34, 173–178. [Google Scholar] [CrossRef] [PubMed]
- Ljungberg, B.; Nilsson-Ehle, I. Advancing age and acute infection influence the kinetics of ceftazidime. Scand. J. Infect. Dis. 1989, 21, 327–332. [Google Scholar] [CrossRef] [PubMed]
- Deeter, R.G.; Weinstein, M.P.; Swanson, K.A.; Gross, J.S.; Bailey, L.C. Crossover assessment of serum bactericidal activity and pharmacokinetics of five broad-spectrum cephalosporins in the elderly. Antimicrob. Agents Chemother. 1990, 34, 1007–1013. [Google Scholar] [CrossRef] [PubMed]
- Higbee, M.D.; Swenson, E.; Gooch, W.M., 3rd. Pharmacokinetics of ceftazidime in elderly patients. Clin. Pharm. 1989, 8, 59–62. [Google Scholar]
- LeBel, M.; Barbeau, G.; Vallee, F.; Bergeron, M.G. Pharmacokinetics of ceftazidime in elderly volunteers. Antimicrob. Agents Chemother. 1985, 28, 713–715. [Google Scholar] [CrossRef]
- Shimada, K.; Inamatsu, T.; Urayama, K.; Ikuma, K. Ceftazidime pharmacokinetics and clinical experiences in the aged patients. Chemotherapy 1983, 31, 251–257. [Google Scholar]
- Ohkawa, M.; Nakashima, T.; Shoda, R.; Ikeda, A.; Orito, M.; Sawaki, M.; Sugata, T.; Shimamura, M.; Hirano, S.; Okumura, K. Pharmacokinetics of ceftazidime in patients with renal insufficiency and in those undergoing hemodialysis. Chemotherapy 1985, 31, 410–416. [Google Scholar] [CrossRef]
- Saito, A. Studies on absorption, distribution, metabolism and excretion of ceftazidime in Japan. J. Antimicrob. Chemother. 1983, 12 (Suppl. SA), 255–262. [Google Scholar] [CrossRef]
- Ackerman, B.H.; Ross, J.; Tofte, R.W.; Rotschafer, J.C. Effect of decreased renal function on the pharmacokinetics of ceftazidime. Antimicrob. Agents Chemother. 1984, 25, 785–786. [Google Scholar] [CrossRef]
- Leroy, A.; Leguy, F.; Borsa, F.; Spencer, G.R.; Fillastre, J.P.; Humbert, G. Pharmacokinetics of ceftazidime in normal and uremic subjects. Antimicrob. Agents Chemother. 1984, 25, 638–642. [Google Scholar] [CrossRef]
- Lin, M.S.; Wang, L.S.; Huang, J.D. Single- and multiple-dose pharmacokinetics of ceftazidime in infected patients with varying degrees of renal function. J. Clin. Pharmacol. 1989, 29, 331–337. [Google Scholar] [CrossRef] [PubMed]
- Norrby, S.R.; Burman, L.A.; Linderholm, H.; Trollfors, B. Ceftazidime: Pharmacokinetics in patients and effects on the renal function. J. Antimicrob. Chemother. 1982, 10, 199–206. [Google Scholar] [CrossRef] [PubMed]
- van Dalen, R.; Vree, T.B.; Baars, A.M.; Termond, E. Dosage adjustment for ceftazidime in patients with impaired renal function. Eur. J. Clin. Pharmacol. 1986, 30, 597–605. [Google Scholar] [CrossRef]
- Walstad, R.A.; Dahl, K.; Hellum, K.B.; Thurmann-Nielsen, E. The pharmacokinetics of ceftazidime in patients with impaired renal function and concurrent frusemide therapy. Eur. J. Clin. Pharmacol. 1988, 35, 273–279. [Google Scholar] [CrossRef] [PubMed]
- Welage, L.S.; Schultz, R.W.; Schentag, J.J. Pharmacokinetics of ceftazidime in patients with renal insufficiency. Antimicrob. Agents Chemother. 1984, 25, 201–204. [Google Scholar] [CrossRef]
- GlaxoSmithKline. FORTAZ®: Ceftazidime for Injection. 2007. Available online: http://www.accessdata.fda.gov/drugsatfda_docs/label/2007/050578s053,050634s020lbl.pdf (accessed on 5 March 2024).
- Conil, J.M.; Georges, B.; Lavit, M.; Laguerre, J.; Samii, K.; Houin, G.; Saivin, S. A population pharmacokinetic approach to ceftazidime use in burn patients: Influence of glomerular filtration, gender and mechanical ventilation. Br. J. Clin. Pharmacol. 2007, 64, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Rodgers, T.; Rowland, M. Physiologically based pharmacokinetic modelling 2: Predicting the tissue distribution of acids, very weak bases, neutrals and zwitterions. J. Pharm. Sci. 2006, 95, 1238–1257. [Google Scholar] [CrossRef]
- Harding, S.M.; Harper, P.B. The pharmacokinetic behaviour of ceftazidime in man and the relationship between serum levels and the in vitro susceptibility of clinical isolates. Infection 1983, 11 (Suppl. S1), S49–S53. [Google Scholar] [CrossRef] [PubMed]
- Rowland Yeo, K.; Aarabi, M.; Jamei, M.; Rostami-Hodjegan, A. Modeling and predicting drug pharmacokinetics in patients with renal impairment. Expert Rev. Clin. Pharmacol. 2011, 4, 261–274. [Google Scholar] [CrossRef]
- Rostoker, G.; Andrivet, P.; Pham, I.; Griuncelli, M.; Adnot, S. A modified Cockcroft-Gault formula taking into account the body surface area gives a more accurate estimation of the glomerular filtration rate. J. Nephrol. 2007, 20, 576–585. [Google Scholar]
- National Kidney, F. K/DOQI clinical practice guidelines for chronic kidney disease: Evaluation, classification, and stratification. Am. J. Kidney Dis. 2002, 39, S1–S266. [Google Scholar]

| Study (Dose) | Age (Years) | Sample Size | Sex | Weight (kg) | CLcr (mL/min) | SerCr (µmol/L) | Additional Notes |
|---|---|---|---|---|---|---|---|
| |||||||
| Ljungberg et al. [26] (2 g i.v. bolus) | 18–39 | 7 | 5M/2F | NA | 112 ± 19 | 74.3 ± 17.7 | GFR determined by 15Cr-EDTA; unit of mL/min/1.73 m2 |
| 40–59 | 8 | 4M/4F | NA | 105 ± 26 | 71.6 ±17.7 | ||
| 60–79 | 13 | 10M/3F | NA | 79 ± 18 | 90.2 ± 19.5 | ||
| 84 ± 3.6 | 9 | 5M/4F | NA | 56 ± 16 | 92.0 ± 19.5 | ||
| Ljungberg et al. [27] (2 g i.v. bolus) | 23–31 | 9 | M | NA | 101 ± 6.5 | 84.9 ± 10.6 | GFR determined by 15Cr-EDTA; unit of mL/min/1.73 m2 |
| 63–76 | 10 | M | NA | 77 ± 9.8 | 90.2 ± 11.5 | ||
| Naber et al. [25] (2 g i.v. bolus) | 24–32 | 6 | 3M/3F | 54–81 | NA | 35.4–79.6 | |
| 63–83 | 13 | 11M/2F | 55–96 | 61.9–132.6 | |||
| LeBel et al. [30] (2 g i.v. bolus) | 19–29 | 12 | 6M/6F | 44–78.5 | 76.6–124 | 70.74–88.42 | CLcr calculated using Cockcroft–Gault equation; unit of mL/min. Individual demographics available |
| 57–73 | 5 | M | 50–84 | 56.9–89.8 | 70.74–97.26 | ||
| Deeter et al. [28] (2 g infused over 30 min) | 70.7 ± 3.5 | 6 | 3M/3F | 75 ± 16 | 55.9 ± 13.5 | 88.4 ± 26.5 | CLcr calculated using Cockcroft–Gault equation; unit of mL/min/1.73 m2 |
| Higbee et al. [29] (2 g infused over 30 min) | 69–90 | 10 | M | 43.6–81.4 | 24–80 | <221.05 | Individual demographic available; CLcr calculated using Cockcroft–Gault equation; unit of mL/min |
| Shimada et al. [31] (1 g i.v. bolus) | 68–82 | 3 | 2M/1F | 35–55 | 30–70 | 61.9–88.4 | |
| |||||||
| Ohkawa et al. [32] (0.5 g bolus) | 20–87 | 7 | 29 M/10 F | 38–79 | 105.2–133 | NA | CLcr determined from endogenous creatinine clearance corrected for a normalized body surface area (per 1.73 m2) |
| 8 | 63.1–89.1 | ||||||
| 9 | 30–56.8 | ||||||
| 8 | 8.3–29.2 | ||||||
| Saito et al. [33] (0.5 g bolus) | NA | 7 | M | NA | >90 | NA | Determination of CLcr not described |
| 5 | 60–90 | ||||||
| 9 | 30–60 | ||||||
| 8 | 10–30 | ||||||
| 10 | <10 | ||||||
| Ackerman et al. [34] (1 g bolus) | 26–92 | 11 | 7M/4F | NA | 6–113 | NA | Individual conc and PK data available, but not for sex and weight. Determination of CLcr not described |
| Leroy et al. [35] (15 mg/kg bolus) | 22–31 | 5 | NA | 64–78 | 110–141 | NA | CLcr determined from measurement of endogenous creatinine over time |
| 26–74 | 5 | NA NA NA NA | 41–83 | 39–72.5 | NA | ||
| 6 | 13.8–27 | ||||||
| 4 | 2.0–12 | ||||||
| 4 | Anuric | ||||||
| Norrby et al. [37] (1 g; 20-min inf) | 57–88 | 14 | 8M/6F | NA | 47–146 | 54.8–122 | No conc profiles. GFR determined (51Cr-EDTA Clearance); individual data for PK, CLEDTA, demographics reported |
| Welage et al. [40] (1 g bolus) | 30–91 | 14 | 12M/2F | 57–95 | 4.5–122.3 | 88.4–751.6 | Individual data for PK, measured CLcr (urine collection), demographics. Conc profiles from 3 individuals only |
| Van Dalen et al. [38] (1 g bolus) | 34–88 | 20 | 14M/9F | NA | 0–133.8 | NA | Individual PK data and CLcr (urine collection) available, but not demographics. Conc profiles from 3 individuals only |
| Walstad et al. [39] (1 g, but 0.5 g for severe RI patients) | 28–89 (26 of them > 75 years) | 9 | 16M/21F | NA | >50 | NA | CLcr estimated using Cockcroft and Gault’s method |
| 10 | 50–31 | ||||||
| 10 | 30–16 | ||||||
| 8 | 5.0–15 | ||||||
| Lin et al. [36] (2 g b.i.d. bolus) | 21–74 | 6 | 4M/2F | 50–65 | 51–94 | NA | CLcr estimated using Bjornsson’s method using serum creatinine, age, and weight |
| 58–75 | 8 | 5M/3F | 42–74 | 10–35 | |||
| Study Design * | AUC (h·mg/L) | Half-Life (h) | Clearance (L/h) | fe_12h (%) ** | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | Population Age (N) | (Trial Code) | Obs | Pred | Ratio | Obs | Pred | Ratio | Obs | Pred | Ratio | Obs | Pred | Ratio |
| Ljungberg et al. [26] 2 g i.v. bolus | 18–39 y (7) | A1 | 248 ± 61 | 278 ± 53 | 1.12 | 2.0 | 1.5 ± 0.3 | 0.74 | 8.06 | 7.48 ± 1.5 | 0.93 | 84 ± 7 | 88 ± 4 | 1.05 |
| 40–59 y (8) | A2 | 287 ± 121 | 323 ± 54 | 1.13 | 2.0 | 1.7 ± 0.4 | 0.84 | 6.97 | 6.38 ± 1.21 | 0.92 | 85 ± 7.5 | 88 ± 5 | 1.04 | |
| Ratio (40–59 y/18–39 y) | 1.16 | 1.16 | 1.00 | 0.99 | 1.12 | 1.13 | 0.86 | 0.85 | 0.99 | 1.01 | 1.00 | 0.99 | ||
| 60–79 y (13) | A3 | 392 ± 115 | 481 ± 118 | 1.23 | 2.73 | 2.64 ± 0.65 | 0.97 | 5.1 | 4.4 ± 1.1 | 0.86 | 74 ± 14 | 83 ± 6 | 1.12 | |
| Ratio (60–79 y/18–39 y) | 1.58 | 1.73 | 1.09 | 1.35 | 1.77 | 1.31 | 0.63 | 0.59 | 0.93 | 0.88 | 0.94 | 1.07 | ||
| >80 y (9) | A4 | 536 ± 142 | 626 ± 164 | 1.17 | 3.54 | 3.08 ± 0.8 | 0.87 | 5.73 | 3.4 ± 0.85 | 0.59 | 67 ± 16 | 82 ± 7 | 1.22 | |
| Ratio (>80 y/18–39 y) | 2.16 | 2.25 | 1.04 | 1.75 | 2.07 | 1.18 | 0.71 | 0.45 | 0.64 | 0.80 | 0.93 | 1.17 | ||
| Ljungberg et al. [27] 2 g i.v. bolus | 23–31 y (9) | B1 | 277 ± 29 | 291 ± 49 | 1.05 | 1.94 | 1.67 ± 0.27 | 0.86 | 7.22 ± 0.8 | 7.05 ± 1.2 | 0.98 | 87 ± 10 | 87 ± 4.4 | 1.00 |
| 63–76 y (10) | B2 | 418 ± 52 | 503 ± 119 | 1.20 | 2.63 | 2.84 ± 0.63 | 1.08 | 4.78 | 4.19 ± 0.9 | 0.88 | 72 ± 8.6 | 82 ± 6.3 | 1.14 | |
| Ratio (63–76 y/23–31) | 1.51 | 1.73 | 1.15 | 1.36 | 1.70 | 1.25 | 0.66 | 0.59 | 0.90 | 0.82 | 0.94 | 1.15 | ||
| Naber et al. [25] 2 g i.v. bolus | 24–32 y (6) | C1 | 271 | 270 ± 55 | 1.0 | 1.75 ± 0.14 | 1.4 ± 0.33 | 0.80 | 7.38 ± 0.7 | 7.71 ± 1.6 | 1.0 | 87 ± 8.4 | 89 ± 4.0 | 1.0 |
| 65–83 y (13) | C2 | 422 | 515 ± 128 | 1.2 | 2.9 ± 0.5 | 2.85 ± 0.69 | 0.98 | 4.74 ± 1.0 | 4.1 ± 0.95 | 0.86 | 57 ± 18 | 82 ± 6.9 | 1.43 | |
| Ratio (65–83 y/24–32 y) | 1.56 | 1.91 | 1.2 | 1.66 | 2.04 | 1.23 | 0.64 | 0.53 | 0.83 | 0.66 | 0.92 | 0.14 | ||
| Le Bel et al. [30] 1 g i.v. bolus | 19–29 y (12) | D1 | 134 ± 13 | 133 ± 27 | 0.99 | 1.9 ± 0.3 | 1.41 ± 0.35 | 0.74 | 7.50 ± 0.7 | 7.86 ± 1.6 | 1.05 | 77 ± 8.6 | 89 ± 4.3 | 1.16 |
| 57–73 y (5) | D2 | 224 ± 79 | 224 ± 54 | 1.00 | 1.9 ± 0.7 | 2.54 ± 0.58 | 1.34 | 4.99 ± 2.0 | 4.71 ± 1.1 | 0.94 | 76 ± 13 | 86 ± 5 | 1.14 | |
| Ratio (19–29 y/19–29 y) | 1.67 | 1.68 | 1.0 | 1 | 1.8 | 1.8 | 0.67 | 0.60 | 0.90 | 0.98 | 0.97 | 0.98 | ||
| Deeter et al. [28] 2 g infusion | 70.7 ± 3.5 y (6) | E | 409 ± 62 | 483 ± 107 | 1.18 | 3.7 ± 2.0 | 2.47 ± 0.59 | 0.67 | 4.89 ± 0.80 | 4.34 ± 0.92 | 0.89 | NA | 84 ± 6.2 | NA |
| Higbee et al. [29] 2 g infusion | 69–91 y (10) | G | 463 ± 209 | 541 ± 137 | 1.17 | 3.9 ± 1.3 | 3.0 ± 0.65 | 0.77 | 4.9 ± 1.4 | 3.93 ± 0.96 | 0.80 | 71 ± 3 | 70 ± 9 | 0.98 |
| Shimada et al. [31] 1 g i.v. (bolus) | 68–82 y (3) | F | 287 ± 93 | 260 ± 69 | 0.91 | 3.7 ± 1.1 | 2.76 ± 0.10 | 0.74 | NA | 4.08 ± 0.97 | NA | 71 ± 3 | 70 ± 9 | 0.99 |
| Model Predictions 2 g (bolus) | 25–35 y (200) | H1 | 282 ± 55 | 1.5 ± 0.4 | 7.4 ± 1.6 | 88 ± 4 | ||||||||
| 45–55 y (200) | H2 | 328 ± 49 | 1.8 ± 0.4 | 6.2 ± 1.1 | 88 ± 4 | |||||||||
| Ratio (45–55/25–35 y) | 1.16 | 1.18 | 0.85 | 1.0 | ||||||||||
| 65–75 y (200) | H3 | 499 ± 134 | 2.5 ± 0.6 | 4.3 ± 1.1 | 84 ± 6 | |||||||||
| Ratio (65–75 y/25–35 y) | 1.77 | 1.69 | 0.58 | 0.95 | ||||||||||
| 85–95 y (200) | H4 | 722 ± 205 | 3.5 ± 1.0 | 3.0 ± 0.8 | 80 ± 8 | |||||||||
| Ratio (85–95 y/25–35 y) | 2.56 | 2.36 | 0.40 | 0.91 | ||||||||||
| Ref. | Population *; Age (n: CLcr (mL/min) | Trial Code | AUC (h · mg/L) | Half-Life (h) | Clearance (L/h) | fe_24h (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Obs | Pred | Ratio | Obs | Pred | Ratio | Obs | Pred | Ratio | Obs | Pred | Ratio | |||
| Ohkawa et al. [32] (0.5 i.v. g bolus) | 20–65 y (7 Normal: 105.2–133 a) | A1 | 72.9 ± 14 | 71.3 ± 14 | 0.98 | 1.55 ± 0.3 | 1.52 ± 0.4 | 0.98 | 8.2 ± 1.5 | 7.3 ± 1.4 | 0.89 | 90 ± 4 | 89 ± 4 | 0.99 |
| 20–87 y (8 Mild RI: 63.1–89.1) | A2 | 133 ± 14 | 134 ± 15 | 1.0 | 2.9 ± 0.6 | 2.9 ± 0.6 | 1.0 | 4.6 ± 1.2 | 3.8 ± 0.4 | 0.82 | 85 ± 6 | 86 ± 5 | 1.0 | |
| Ratio (Mild/Normal) | 1.83 | 1.88 | 1.0 | 1.84 | 1.93 | 1.1 | 0.56 | 0.52 | 0.92 | 0.95 | 0.97 | 1.0 | ||
| 20–87 y (9 Moderate RI: 30–57) | A3 | 192 ± 32 | 192 ± 32 | 1.0 | 3.9 ± 0.9 | 4.1 ± 0.9 | 1.0 | 2.9 ± 1.0 | 2.7 ± 0.4 | 0.92 | 76 ± 11 | 80 ± 6 | 1.04 | |
| Ratio (Moderate/Normal) | 2.64 | 2.69 | 1.0 | 2.54 | 2.67 | 1.1 | 0.36 | 0.37 | 1.0 | 0.85 | 0.90 | 1.1 | ||
| 20–87 y (8 Severe RI: 8.3–29.2) | A4 | 338 ± 65 | 344 ± 66 | 1.0 | 6.7 ± 1.8 | 6.9 ± 1.9 | 1.0 | 1.5 ± 0.6 | 1.5 ± 0.3 | 1.0 | 55 ± 15 | 62 ± 10 | 1.1 | |
| Ratio (Severe/Normal) | 4.64 | 4.82 | 1.0 | 4.34 | 4.51 | 1.0 | 0.18 | 0.21 | 1.1 | 0.61 | 0.70 | 1.1 | ||
| Saito [33] (0.5 g i.v. bolus) | 20–50 y (7 Normal: >=90) | B1 | NA | 73 ± 13 | NA | 1.7 | 1.7 ± 0.3 | 1.00 | NA | 7.0 ± 1.2 | NA | 90 | 89 ± 4 | 0.99 |
| 20–50 y (5 Mild RI: 60–90) | B2 | NA | 111 ± 11 | NA | 2.3 | 2.7 ± 0.4 | 1.16 | NA | 4.6 ± 0.5 | NA | 88 | 83 ± 5 | 0.94 | |
| Ratio (Mild/Normal) | NA | 1.51 | NA | 1.4 | 1.57 | 1.16 | NA | 0.65 | NA | 0.98 | 0.94 | 0.96 | ||
| 20–50 y (9 Moderate RI: 30–60) | B3 | NA | 154 ± 18 | NA | 3.4 | 3.6 ± 0.6 | 1.06 | NA | 3.3 ± 0.4 | NA | 78 | 76 ± 7 | 0.98 | |
| Ratio (Moderate/Normal) | NA | 2.10 | NA | 2.0 | 2.11 | 1.1 | NA | 0.47 | NA | 0.86 | 0.87 | 1.0 | ||
| 20–50 y (8 Severe RI: 10–30) | B4 | NA | 267 ± 49 | NA | 6.1 | 6.2 ± 1.4 | 1.02 | NA | 1.9 ± 0.4 | NA | 70 | 55 ± 9 | 0.79 | |
| Ratio (Severe/Normal) | NA | 3.64 | NA | 3.6 | 3.65 | 1.0 | NA | 0.28 | NA | 0.77 | 0.63 | 0.82 | ||
| Ackerman et al. [34] (1 g i.v. bolus) | 26–27 y (3 Normal: >=90) | C1 | 133 ± 28 | 138 ± 27 | 1.0 | 1.3 ± 0.1 | 1.5 ± 0.3 | 1.14 | 7.8 ± 1.5 | 7.5 ± 1.4 | 0.96 | NA | 88 ± 4 | NA |
| 33–74 y (5 Moderate RI: 34–45) | C3 | 336 ± 64 | 353 ± 56 | 1.16 | 4.7 ± 2 | 3.8 ± 0.8 | 0.87 | 3.1 ± 0.6 | 2.9 ± 0.4 | 0.94 | NA | 72 ± 7 | NA | |
| Ratio (Moderate/Normal) | 2.52 | 2.56 | 1.12 | 3.55 | 2.52 | 0.71 | 0.40 | 0.39 | 0.98 | NA | 0.82 | NA | ||
| Leroy et al. [35] (15 mg/kg i.v. bolus) * | 22–31 y (5 Normal: 110–141) | D1 | 127 ± 15 | 159 ± 36 | 1.25 | 1.6 ± 0.1 | 1.5 ± 0.3 | 0.97 | 7.8 ± 0.8 | 7.5 ± 1.4 | 0.96 | 84 ± 4 | 88 ± 4 | 1.05 |
| 26–74 y (5 Moderate RI: 39–73) | D2 | 314 ± 38 | 376 ± 90 | 1.20 | 3.7 ± 0.8 | 3.5 ± 0.8 | 0.92 | 3.3 ± 0.5 | 3.2 ± 0.4 | 0.97 | 56 ± 7 | 72 ± 7 | 1.28 | |
| Ratio (Moderate/Normal) | 2.47 | 2.36 | 0.96 | 2.38 | 2.27 | 0.95 | 0.42 | 0.43 | 1.01 | 0.67 | 0.82 | 1.21 | ||
| 26–74 y (6 Severe RI: 14–27) | D3 | 773 ± 119 | 708 ± 205 | 0.92 | 9.3 ± 1.1 | 6.5 ± 1.7 | 0.71 | 1.3 ± 0.1 | 1.6 ± 0.3 | 1.25 | 45 ± 13 | 63 ± 8 | 1.42 | |
| Ratio (Severe/Normal) | 6.09 | 4.45 | 0.73 | 5.89 | 4.30 | 0.73 | 0.17 | 0.22 | 1.30 | 0.53 | 0.72 | 1.34 | ||
| 26–74 y (4 Anuric: 0) | D4 | 2313 ± 414 | 2166 ± 849 | 0.94 | 25 ± 4.1 | 19.8 ± 7.3 | 0.78 | 0.4 ± 0.0 | 0.6 ± 0.2 | 1.42 | 0.0 | 0.0 | NA | |
| Ratio (Anuric/Normal) | 18.2 | 13.6 | 0.75 | 16.1 | 13.0 | 0.81 | 0.05 | 0.08 | 1.48 | NA | 0.00 | NA | ||
| Norrby et al. [37] (1 g; 20-min i.v. infusion) | 57–77 y (6 Normal: 92–146) | E1 | 118 ± 38 | 218 ± 54 | 1.84 | 1.5 ± 0.4 | 2.4 ± 0.5 | 1.57 | 9.4 ± 3.3 | 4.9 ± 1.2 | 0.52 | NA | 87 ± 5 | NA |
| 69–84 y (5 Mild RI: 60–76) | E2 | 175 ± 36 | 264 ± 30 | 1.51 | 2.4 ± 0.4 | 2.7 ± 0.5 | 1.13 | 6.0 ± 1.4 | 3.9 ± 0.5 | 0.64 | NA | 87 ± 5 | NA | |
| Ratio (Mild/Normal) | 1.48 | 1.21 | 0.82 | 1.60 | 1.15 | 0.72 | 0.64 | 0.79 | 1.24 | NA | 1 | NA | ||
| 62–78 y (3 Moderate RI: 47–54) | E3 | 228 ± 24 | 368 ± 64 | 1.61 | 3.4 ± 0.3 | 3.9 ± 0.9 | 1.14 | 4.4 ± 0.5 | 2.8 ± 0.5 | 0.64 | NA | 79 ± 7 | NA | |
| Ratio (Moderate/Normal) | 1.93 | 1.69 | 0.88 | 2.27 | 1.66 | 0.73 | 0.47 | 0.57 | 1.23 | NA | 0.91 | NA | ||
| Welage et al. [40] (1 g i.v. bolus) | 30–36 y (2 Normal: 110–122) | F1 | 152 ± 37 | 150 ± 27 | 0.99 | 1.7 ± 0.2 | 1.7 ± 0.3 | 0.99 | 7.0 ± 1.7 | 6.9 ± 1.2 | 0.98 | 78 ± 23 | 87 ± 4 | 1.12 |
| 49–69 y (5 Moderate RI: 30–60) | F2 | 336 ± 39 | 317 ± 45 | 0.94 | 3.6 ± 0.5 | 3.4 ± 0.7 | 0.93 | 3.0 ± 0.3 | 3.2 ± 0.4 | 1.06 | 80 ± 15 | 72 ± 6 | 0.90 | |
| Ratio (Moderate/Normal) | 2.21 | 2.11 | 0.96 | 2.12 | 1.99 | 0.94 | 0.43 | 0.47 | 1.09 | 1.03 | 0.83 | 0.81 | ||
| 27–91 y (4 Severe RI: 21–29.5) | F3 | 582 ± 86 | 548 ± 89 | 0.94 | 6.3 ± 2.4 | 5.6 ± 1.5 | 0.89 | 1.8 ± 0.3 | 1.9 ± 0.3 | 1.06 | 74 ± 11 | 50 ± 8 | 0.68 | |
| Ratio (Severe/Normal) | 3.83 | 3.65 | 0.95 | 3.71 | 3.31 | 0.89 | 0.25 | 0.27 | 1.09 | 0.95 | 0.57 | 0.61 | ||
| Van Dalen et al. [38] (1 g i.v. bolus) | 34–88 y (4 Normal: 93–134) | G1 | 136 ± 36 | 160 ± 26 | 1.18 | 2.5 ± 0.9 | 1.7 ± 0.4 | 0.70 | 7.8 ± 1.7 | 6.4 ± 1.1 | 0.83 | 80 ± 2 | 89 ± 4 | 1.11 |
| 34–88 y (3 Mild RI: 72–86) | G2 | 190 ± 6 | 268 ± 31 | 1.41 | 3.7 ± 1.1 | 2.9 ± 0.6 | 0.78 | 5.3 ± 0.2 | 3.8 ± 0.5 | 0.72 | 88 ± 5 | 86 ± 5 | 0.98 | |
| Ratio (Mild/Normal) | 1.40 | 1.68 | 1.20 | 1.49 | 1.67 | 1.12 | 0.67 | 0.59 | 0.87 | 1.10 | 0.97 | 0.88 | ||
| 34–88 y (4 Moderate RI: 30–59) | G3 | 393 ± 187 | 386 ± 66 | 0.98 | 6.9 ± 3.1 | 4.0 ± 0.9 | 0.58 | 3.0 ± 1.0 | 2.7 ± 0.4 | 0.89 | 69 ± 10 | 81 ± 6 | 1.17 | |
| Ratio (Moderate/Normal) | 2.89 | 2.41 | 0.83 | 2.76 | 2.32 | 0.84 | 0.38 | 0.41 | 1.08 | 0.86 | 0.91 | 1.06 | ||
| 34–88 y (2 Severe RI: 9–20) | G4 | 1140 ± 314 | 681 ± 131 | 0.60 | 15.1 ± 1.0 | 6.9 ± 1.9 | 0.46 | 0.9 ± 0.2 | 1.5 ± 0.3 | 1.63 | 41 ± 12 | 62 ± 9 | 1.51 | |
| Ratio (Severe/Normal) | 8.38 | 4.26 | 0.51 | 6.04 | 3.97 | 0.66 | 0.12 | 0.24 | 1.97 | 0.51 | 0.70 | 1.36 | ||
| Walstad et al. [39] (1 g i.v.) | 28–89 y (9 Mild RI: ≥50) | H1 | 232 ± 34 | 261 ± 32 | 1.13 | 2.8 ± 0.5 | 2.7 ± 0.6 | 0.95 | 4.4 ± 0.7 | 3.9 ± 0.5 | 0.89 | 94 ± 8 | 87 ± 4 | 0.93 |
| 28–89 y (10 Moderate RI: 31–50) | H2 | 359 ± 62 | 382 ± 68 | 1.06 | 5.0 ± 1.2 | 3.8 ± 0.9 | 0.75 | 2.9 ± 0.5 | 2.7 ± 0.5 | 0.95 | 80 ± 12 | 81 ± 6 | 1.01 | |
| 28–89 y (10 Severe RI: 16–30) | H3 | 279 ± 54 | 337 ± 65 | 1.21 | 8.6 ± 1.7 | 6.5 ± 1.8 | 0.75 | 1.9 ± 0.4 | 1.5 ± 0.3 | 0.83 | 58 ± 5 | 64 ± 9 | 1.10 | |
| Lin et al. [36] (2 g i.v. b.i.d. bolus) | 21–74 y (6 Mild RI: 51–94) | I1 | 410 ± 13 | 504 ± 54 | 1.23 | 3.3 ± 1.1 | 2.9 ± 0.6 | 0.86 | 5.7 | 4.0 ± 0.5 | 0.70 | NA | NA | |
| 58–75 y (8 Severe RI: 10–35) | I2 | 990 ± 265 | 1114 ± 213 | 1.13 | 7.6 ± 1.6 | 6.2 ± 1.7 | 0.82 | 2.0 | 1.9 ± 0.4 | 0.97 | NA | NA | ||
| Model prediction (1 g i.v. bolus) | 65–80 y (200 Normal) | 254 ± 63 | 2.9 ± 0.7 | 4.2 ± 1.0 | 86 ± 6 | |||||||||
| 65–80 y (200 Mild RI) | 268 ± 29 | 3.1 ± 0.5 | 3.8 ± 0.4 | 85 ± 5 | ||||||||||
| Ratio (Mild/Normal) | 1.06 | 1.08 | 0.91 | 0.99 | ||||||||||
| 65–80 y (200 Moderate RI) | 376 ± 64 | 4.2 ± 0.8 | 2.7 ± 0.4 | 79 ± 6 | ||||||||||
| Ratio (Moderate/Normal) | 1.48 | 1.46 | 0.66 | 0.92 | ||||||||||
| 65–80 y (200 Severe RI) | 665 ± 126 | 7.2 ± 1.7 | 1.6 ± 0.3 | 60 ± 8 | ||||||||||
| Ratio (Severe/Normal) | 2.62 | 2.50 | 0.38 | 0.70 | ||||||||||
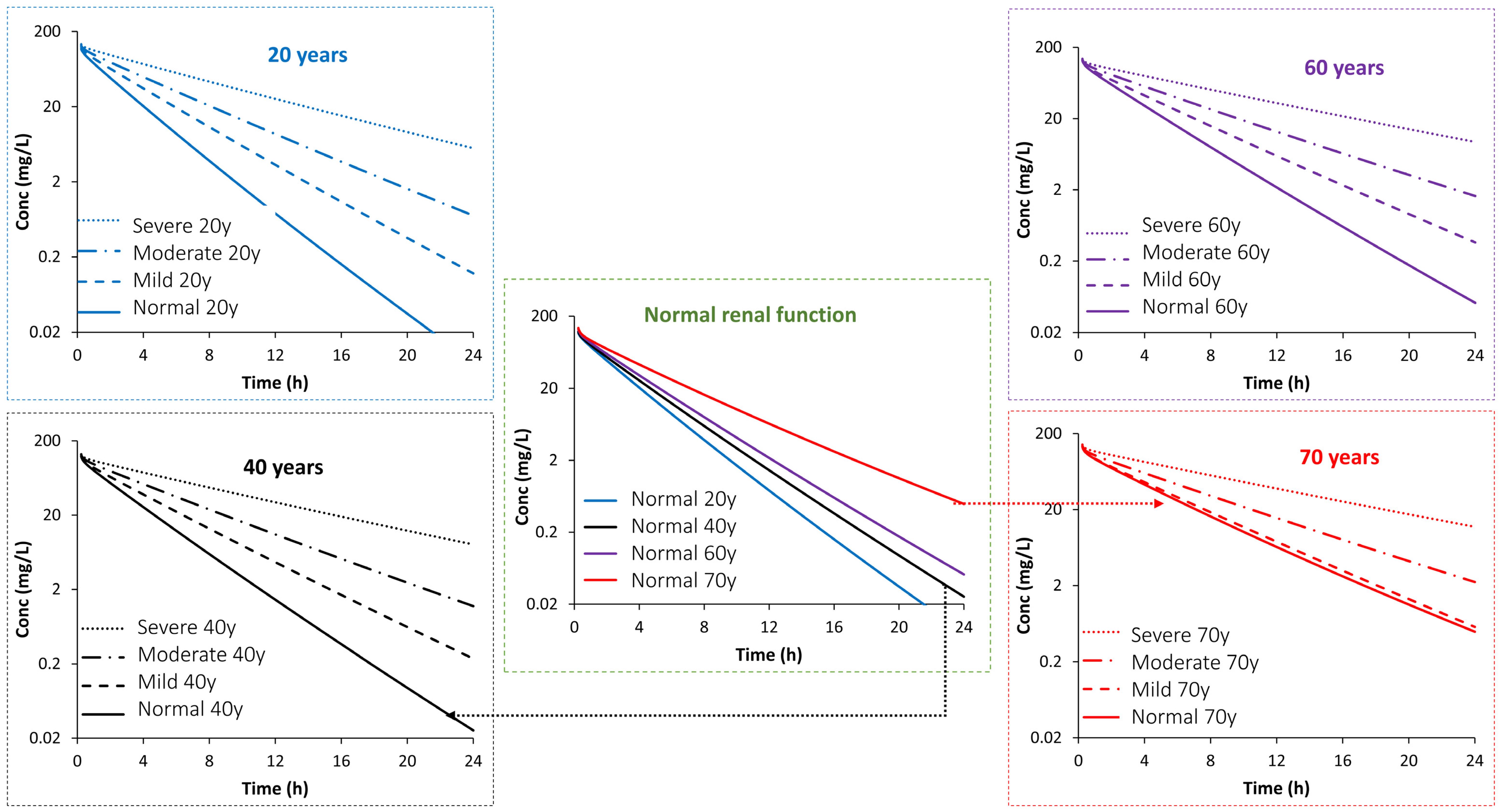
| PK Parameter | Age (Years) | Impact of Age or/and Disease Stage (Fold Change from Predicted Mean PK Value in a Population Aged 20 Years with Normal Function) | Impact of Disease Stage (Fold Change from Predicted Mean PK Value in an Age-Matched Population with Normal Function) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Normal | Mild RI | Moderate RI | Severe RI | Normal | Mild RI | Moderate RI | Severe RI | ||
| Half-Life | 20 | 1.00 | 1.42 | 1.93 | 3.22 | 1.0 | 1.42 | 1.93 | 3.22 |
| 30 | 1.08 | 1.52 | 2.07 | 3.57 | 1.0 | 1.41 | 1.92 | 3.31 | |
| 40 | 1.18 | 1.59 | 2.16 | 3.75 | 1.0 | 1.36 | 1.84 | 3.19 | |
| 50 | 1.30 | 1.67 | 2.26 | 3.96 | 1.0 | 1.29 | 1.74 | 3.06 | |
| 60 | 1.44 | 1.72 | 2.32 | 3.96 | 1.0 | 1.19 | 1.61 | 2.75 | |
| 70 | 1.73 | 1.87 | 2.50 | 4.32 | 1.0 | 1.08 | 1.44 | 2.49 | |
| AUCINF | 20 | 1.00 | 1.47 | 2.03 | 3.50 | 1.0 | 1.47 | 2.03 | 3.50 |
| 30 | 1.07 | 1.52 | 2.12 | 3.71 | 1.0 | 1.42 | 1.98 | 3.47 | |
| 40 | 1.17 | 1.58 | 2.19 | 3.84 | 1.0 | 1.34 | 1.87 | 3.27 | |
| 50 | 1.31 | 1.64 | 2.31 | 4.04 | 1.0 | 1.26 | 1.77 | 3.10 | |
| 60 | 1.50 | 1.74 | 2.41 | 4.18 | 1.0 | 1.16 | 1.60 | 2.79 | |
| 70 | 1.83 | 1.90 | 2.62 | 4.67 | 1.0 | 1.04 | 1.43 | 2.55 | |
| Clearance | 20 | 1.00 | 0.67 | 0.48 | 0.29 | 1.0 | 0.67 | 0.48 | 0.29 |
| 30 | 0.93 | 0.64 | 0.46 | 0.27 | 1.0 | 0.69 | 0.50 | 0.29 | |
| 40 | 0.85 | 0.62 | 0.45 | 0.26 | 1.0 | 0.73 | 0.53 | 0.31 | |
| 50 | 0.76 | 0.60 | 0.43 | 0.25 | 1.0 | 0.78 | 0.56 | 0.33 | |
| 60 | 0.67 | 0.56 | 0.41 | 0.24 | 1.0 | 0.85 | 0.62 | 0.36 | |
| 70 | 0.56 | 0.52 | 0.38 | 0.22 | 1.0 | 0.93 | 0.68 | 0.39 | |
| Parameter | Value | Reference |
|---|---|---|
| Physicochemical properties and binding | ||
| Molecular Weight (g/mol) | 546.580 | Zhou et al., 2019 [23] |
| Log P | −3.750 | |
| Compound Type | Diprotic Acid | |
| pKa 1 | 2.430 | |
| pKa 2 | 2.890 | |
| BP | 0.550 | Default |
| Plasma fu (Binding Protein) | 0.9 (Human Serum Albumin) | Predicted and used as input |
| Distribution | ||
| Distribution Model | Full PBPK Model | |
| Vss (L/kg) | 0.20 | (Predicted using Method 2 after [43]) |
| Kp Scalar | 1.0 | |
| Elimination | ||
| Elimination option | Enzyme Kinetics | |
| CLR (L/h) | 6.0 | Zhou et al., 2019 [23] |
| Biliary CLint (µL/min/million hepatocyte) | 0.085 (30% CV) | Adjusted to recover Harding et al., 1983 [44] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abduljalil, K.; Gardner, I.; Jamei, M. Application of Physiologically Based Pharmacokinetic Model to Delineate the Impact of Aging and Renal Impairment on Ceftazidime Clearance. Antibiotics 2024, 13, 862. https://doi.org/10.3390/antibiotics13090862
Abduljalil K, Gardner I, Jamei M. Application of Physiologically Based Pharmacokinetic Model to Delineate the Impact of Aging and Renal Impairment on Ceftazidime Clearance. Antibiotics. 2024; 13(9):862. https://doi.org/10.3390/antibiotics13090862
Chicago/Turabian StyleAbduljalil, Khaled, Iain Gardner, and Masoud Jamei. 2024. "Application of Physiologically Based Pharmacokinetic Model to Delineate the Impact of Aging and Renal Impairment on Ceftazidime Clearance" Antibiotics 13, no. 9: 862. https://doi.org/10.3390/antibiotics13090862






