Abstract
Bacterial foodborne infections, including meat-derived infections, are globally associated with diseases and some deaths. Antibiotics are sometimes used to treat bacterial infections. The use of antibiotics by farmers contributes to the development of resistance by foodborne pathogens. This study aimed to investigate the antibiotics used by farmers and the occurrence of antibiotic-resistant Escherichia coli in ready-to-eat (RTE) meat sources. Data was obtained from livestock farmers through the administration of semistructured questionnaires (n = 376) to obtain information on their demographics, knowledge and antibiotic usage. The procedure in the USA Food and Drug Administration (FDA)’s Bacteriological Analytical Manual was used for E. coli detection. Antibiotic resistance test was performed using the disk diffusion method. The findings revealed that most of the farmers were male (74.5%), were aged 30−39 years (28.5%), had tertiary education (30.3%) and had 6−10 years of experience in livestock husbandry. Sheep (65.7%) were the most reared livestock, and antibiotics were mostly used to treat sick animals (36.7%). Tetracycline (27.7%) was the most common antibiotic used by farmers, followed by amoxicillin/clavulanic acid (18.6%) and trimethoprim/sulfamethoxazole (11.7%). Most farmers (56.1%) said they had knowledge of antibiotic usage. The prevalence of E. coli in RTE meats was lowest in pork (6.0%) and highest in chevon (20.0%). E. coli isolates from RTE meats were highly resistant to teicoplanin (96.77%), tetracycline (93.55%), amoxicillin/clavulanic (70.97%), azithromycin (70.97%) and trimethoprim/sulfamethoxazole (58.06%) but was susceptible to chloramphenicol (93.55%), ciprofloxacin (61.29%) and ceftriaxone (58.06%). The multiple antibiotic index ranged from 0.22 to 0.78. Multidrug resistance (93.55%) was high among the E. coli isolates. The resistance pattern AmcAzmTecTeSxt (amoxicillin/clavulanic acid–azithromycin–telcoplanin–tetracycline–trimethoprim/sulfamethoxazole) was the most common. The use of antibiotics by farmers must be well regulated. Sellers of RTE meats also ought to take hygiene practices seriously to keep meat safe and healthy for public consumption.
1. Introduction
Animal food products, such as egg, meat and milk, are abundant in proteins that are essential for the maintenance, repair and growth of the body. Meat is a food rich in nutrients, containing more bioavailable proteins, vitamins and minerals than other food sources [1]. However, most meats have a high water content that corresponds to about 0.99% water activity, which is suitable for microbial growth [2]. Poultry and red meats are among the most commonly reported carriers of foodborne pathogens [3]. Hughes et al. [4] also asserted that poultry meat, red meat and eggs are recognized as major vectors for transmission of pathogens, such as E. coli.
Microorganisms of animal, environmental and human sources normally contaminate raw meat [5,6]. The initial number of microorganisms that may live, including pathogenic or sublethally injured ones, will be substantially reduced when cooking is adequate [7]. However, the prevalence of pathogenic and spoilage microorganisms in ready-to-eat (RTE) meats can be substantially increased by postcooking handling activities, exposure duration at points of sale and meat storage conditions [8]. The common pathogenic bacteria found in RTE meats are Clostridium perfringens, Salmonella enterica, Staphylococcus aureus and E. coli [9,10,11,12]. E. coli is the most common facultative anaerobic species found in the gastrointestinal tract of both animals and humans and the most common pathogen present in the family of Enterobacteriaceae [13]. Some types of E. coli are responsible for causing diseases by producing Shiga toxins, and they have been linked to several illnesses and some deaths every year [14,15].
RTE meats are popular in Ghana. They are normally sold on the streets, especially at nights, and make a significant contribution to the protein intake of Ghanaians [16]. Meats and foods sold on the streets are generally exposed to foodborne pathogens, including E. coli, and are possible sources of foodborne illnesses. Studies carried out in different parts of Ghana have indicated that RTE foods are contaminated with E. coli. For instance, E. coli was reported in RTE foods in Accra by Agbodaze et al. [17], in Tamale by Abakari et al. [18], in Sunyani by Ofosu et al. [19] and in Bolgatanga by Adzitey et al. [20].
Antibiotics are medications of natural or synthetic origin that have the ability to destroy or prevent growth of microorganisms [21]. They are popularly used for the control, prevention and treatment of infections/diseases [22]. Food animal abuse has important public health consequences as it facilitates the development of bacteria resistant to antibiotics and resistance genes that can be passed on to humans [23]. Abuse happens when farmers use antibiotics intentionally or unintentionally without the requisite knowledge. In addition, the gastrointestinal tracts of farm animals are reservoirs for microorganisms. These microorganisms potentially develop resistance to antibiotics when they are used on the animals [24]. Consequently, transmission to humans might occur when undercooked meat from such farm animals are consumed. Antibiotic resistance in humans can also originate from the environment, pets and wild animals. Microorganisms that are resistant to multiple antibiotics are sometimes widely spread in the environment, pets and wild animals. The environment, pets and wild animals serve as reservoirs and reintroduce resistant bacteria into the food chain, which reach humans via the oral–fecal route or during handling [25].
There is limited study on the knowledge of farmers regarding antibiotic usage, incidence of foodborne pathogens in RTE meats and the antibiotic resistance of foodborne pathogens from RTE meats in Ghana. Therefore, this study aimed to find the antibiotics used by farmers, their knowledge regarding antibiotic usage and prevalence of resistant E. coli from RTE meats in Bolgatanga, Ghana.
2. Results
2.1. Demographic Characteristics and Livestock Species Reared by Farmers
The demographic characteristics and livestock species reared by farmers is shown in Table 1. The majority of farmers were male (74.5%) with age ranging 30−60 years (78.2%). Most of them had either tertiary (30.3%) or nonformal (23.7%) education and had been involved in animal production for 6−10 years (31.6%) or 3−5 years (26.9%). The farmers reared sheep (n = 247), chicken (n = 246), goats (n = 243), cattle (n = 177), guinea fowls (n = 175) and pigs (n = 93).

Table 1.
The demographic characteristics of livestock farmers.
2.2. Usage of Antibiotics by Livestock Farmers
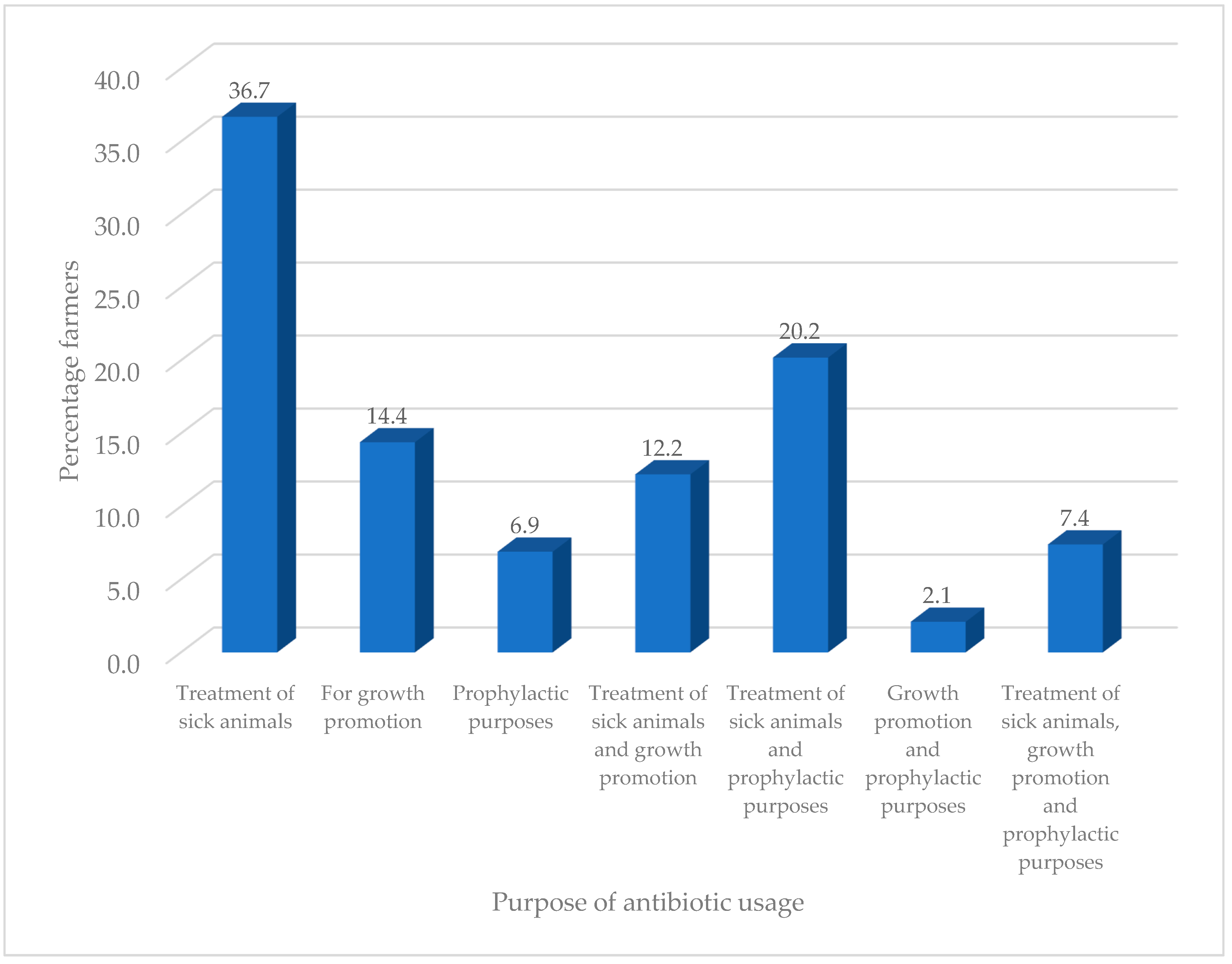
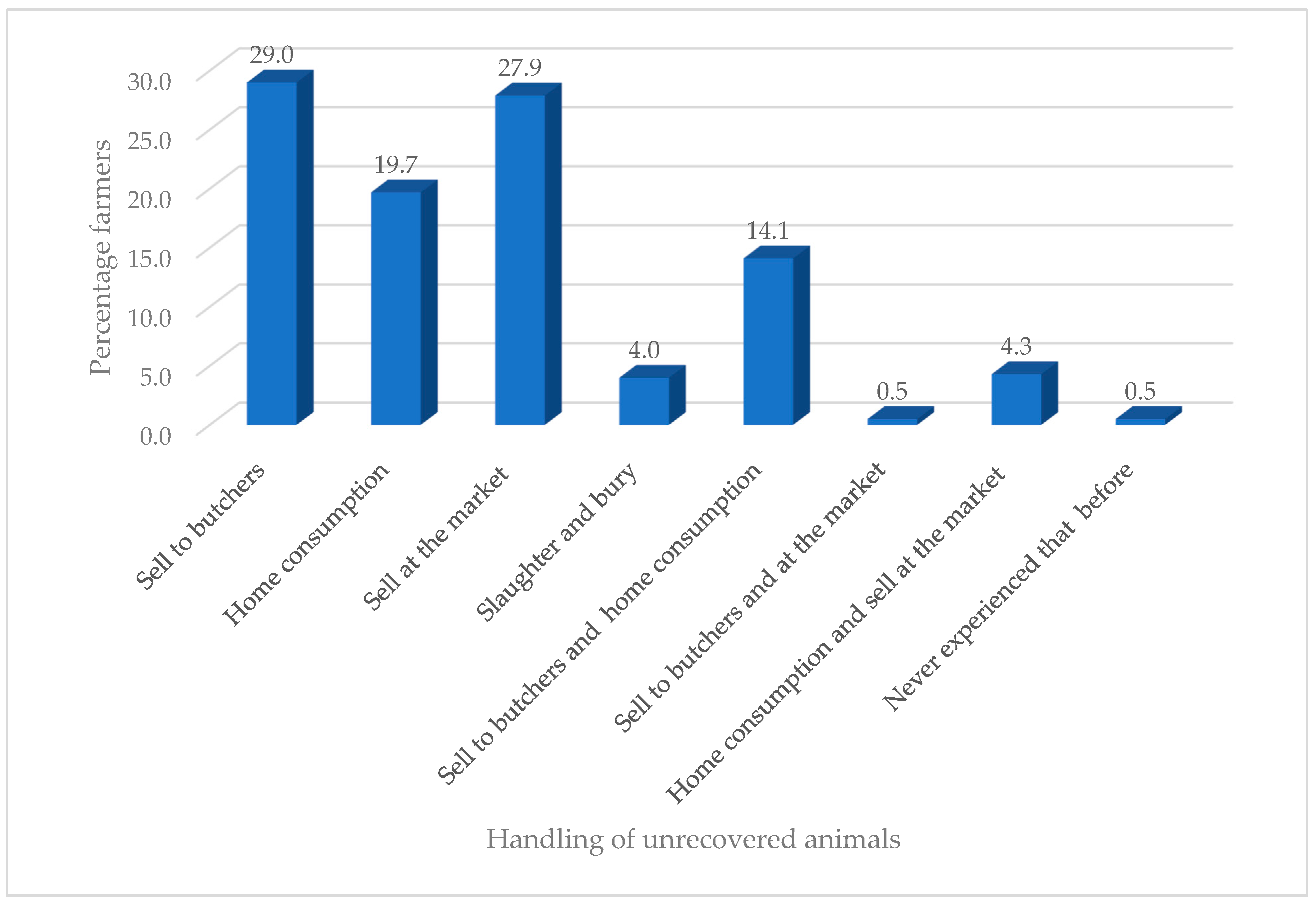
The majority of farmers (92.8%) had experienced infections on their farm and mostly consulted veterinary officers (77.7%) for advice (Table 2). The farmers mostly used tetracycline (27.7%) to treat their animal, while the least used antibiotics were penicillin (4.3%) and erythromycin (4.3%). Recommendations for antibiotic usage mostly came from colleague farmers (35.1%) and veterinarians (31.6%) and the least from veterinarians and drug sellers (2.1%). The majority of farmers said they had knowledge of antibiotic usage (56.1%), and they got this from colleague farmers (32.7%) and veterinary officers (21.8%). The educational level of farmers had no influence on their knowledge of antibiotic usage (χ2 = 5.651a, df = 10, p = 0.844) but had influence (χ2 = 32.158a, df = 5, p = 0.000) on the type of antibiotics used. The years of experience in livestock production had no influence on their knowledge of antibiotic usage (χ2 = 8.460a, df = 8, p = 0.390) and on the type of antibiotics used (χ2 = 5.701a, df = 4, p = 0.223). Many farmers (67.6%) were involved in treating their animals but observed safety dosage instructions (72.1%) and withdrawal periods (65.7%). Antibiotics were used purposely for treatment of sick animals (36.7%), and only few used it for prophylactic and growth purposes (2.1%) (Figure 1). The majority of farmers sold their unrecovered animals after treatment to butchers (29.0%), whilst those who had never experienced that situation (0.5%) were the least common (Figure 2).

Table 2.
The knowledge and usage of antibiotics by livestock farmers.
Figure 1.
Purpose of antibiotic usage by farmers.
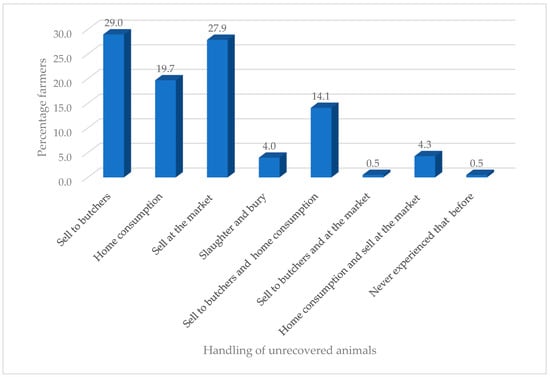
Figure 2.
Handling of unrecovered animals.
2.3. Prevalence of E. coli in Ready-to-Eat Meats
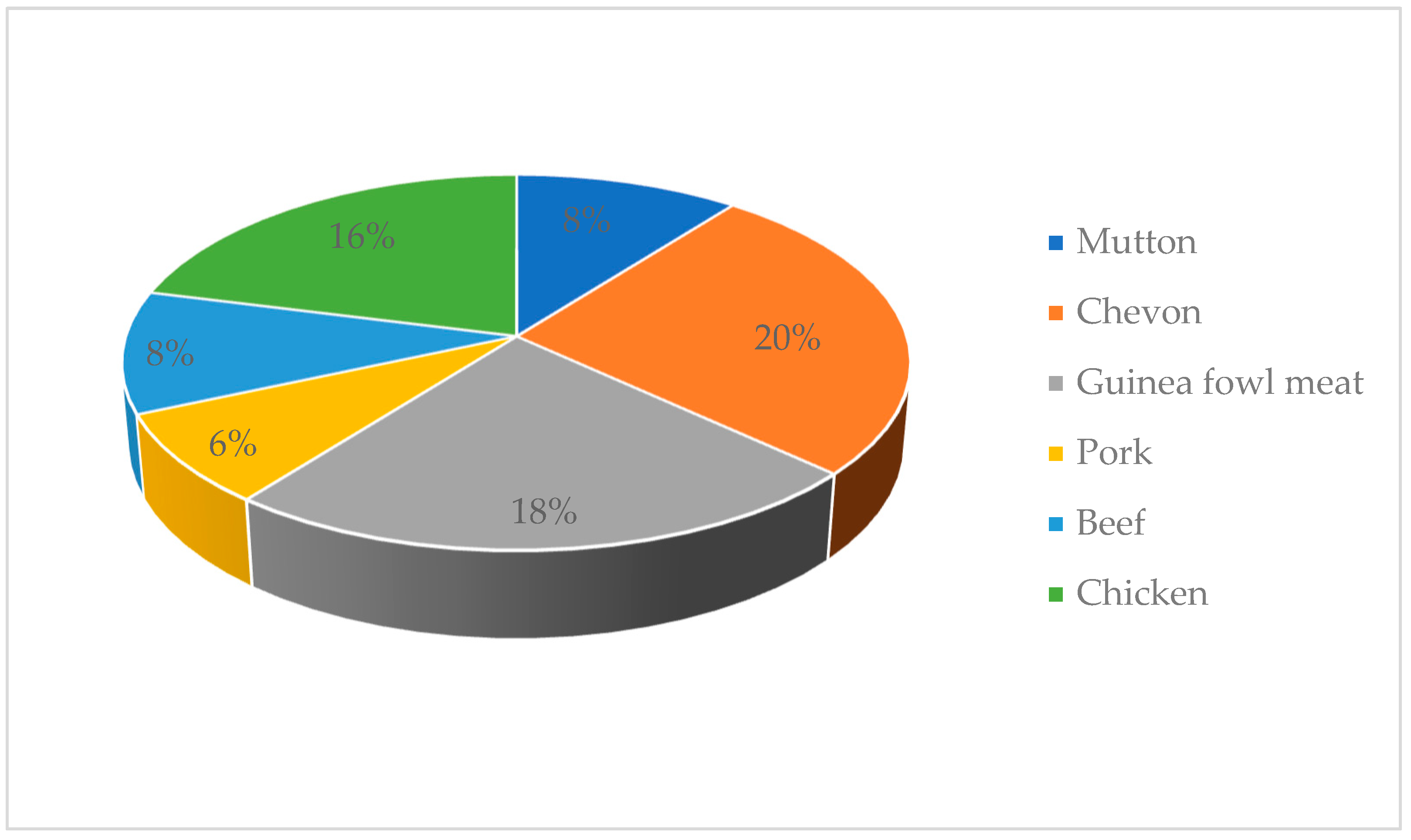
The prevalence of E. coli in RTE meats is presented in Figure 3. Ten samples of RTE chevon (20%), nine samples of guinea fowl (18%), eight samples of chicken (16%), four samples of beef (8%), four samples of mutton (8%) and three samples of pork (6%) were contaminated by E. coli.
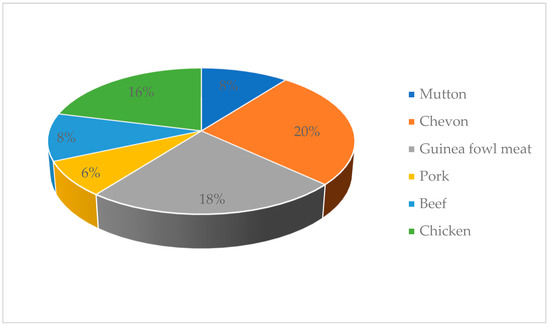
Figure 3.
Prevalence of E. coli in ready-to-eat meats.
2.4. Antibiotic Resistance of E. coli from RTE Meats
The E. coli isolates showed high resistance to teicoplanin (96.77%), tetracycline (93.55%), amoxicillin/clavulanic acid (70.97%) and azithromycin (70.97%) (Table 3). Relatively high intermediate resistance was observed for gentamicin (38.71%), sulfamethoxazole/trimethoprim (25%), ceftriaxone (22.58%), azithromycin (16.13%) and ciprofloxacin (16.13%). The E. coli isolates were highly susceptible to chloramphenicol (93.55%).

Table 3.
Percentage antibiotic resistance of E. coli from ready-to-eat meat samples.
2.5. Multidrug Resistance of Individual E. coli Isolates
The antibiotic resistance pattern of the RTE meats can be found in Table 4. The multiple antibiotic (MAR) index ranged from 0.22 to 0.78. The 31 E. coli exhibited 24 different resistance profiles. In addition, 6.45%, 16.13%, 22.58%, 32.26%, 12.90% and 9.68% were resistant to two, three, four, five, six and seven antibiotics, respectively.

Table 4.
Antibiotic resistance profile and multiple antibiotic resistance (MAR) index of E. coli.
3. Discussions
Resistance of bacteria to antibiotics is essentially linked to their usage either as prophylactic treatment of diseases or as growth promoters [22,23]. This phenomenon is a worldwide issue and threatens public health [23]. Farmers are among the primary users of antibiotics, which ends up in animals, the environment and eventually humans as a result of consumption [26,27]. To ascertain this, we studied livestock farmers’ knowledge and usage of antibiotics and the sensitivity of E. coli from RTE meat sources to antibiotics. In our study, males and the youth dominated the livestock rearing business, which could be attributed to the fact that males in Northern Ghana mostly keep animals as their main source of work and for payment of dowry and most often own animals kept by women as the head of the family. Similar findings have been reported by Akansale et al. [28] and Ozturk et al. [29]. The farmers who kept ruminants and fowls made up the majority due to the usefulness of these animals for religious purposes and the ready market availability. Those who reared pigs were few in number due to religious restrictions, particularly Islam, which forbids Muslims from keeping and consuming swine. Education and experience played a key role in the acquisition, acceptance and application of knowledge. A higher proportion of farmers had tertiary education compared to nonformal education and had appreciable years of experience in livestock rearing. This reflected and contributed to their knowledge and usage of antibiotics as the majority consulted veterinarians when they experienced infections on their farm. In addition, the majority said they had knowledge of antibiotic usage and observed withdrawal periods and safety measures and dosage instructions when administering antibiotics. There was no relationship between the level of education and knowledge of antibiotic usage, although this did exist with the type of antibiotics used. There was no relationship between the years of experience and knowledge of antibiotic usage and the type of antibiotics used. Farmers acquired information on antibiotics and their usage from experienced people (veterinary officers, extension officers and colleague farmers) and organizations (nongovernmental organizations (NGOs)). They mainly used the following antibiotics to treat animals: gentamicin, tetracycline, amoxicillin/clavulanic acid, trimethoprim/sulfamethoxazole, ciprofloxacin, erythromycin, chloramphenicol and penicillin. This finding is similar to the work of Adesokan et al. [26], who reported that beta-lactams/aminoglycosides (20.4%), fluoroquinolones (26.5%) and tetracycline (33.6%) formed the majority of antibiotics used by farmers in livestock production in Nigeria. Katakweba et al. [27] also identified tetracycline (61%), sulfadimidine (23%), penicillin–streptomycin (2%) and gentamycin (1%) as the most used and commonly reported antibiotics among livestock keepers in Tanzania. In this study, farmers received recommendations to use a particular antibiotic from relevant people, such as veterinarians, colleague farmers and veterinary drug sellers. This study also found that antibiotics were used mainly for prophylaxis, treatment of sick animals and as growth promoters. These findings agree with that of Ferdous et al. [30], who found that antibiotics were used by farmers for prophylactic purposes (14.17%), therapeutic purposes (34.16%) or for both therapeutic and prophylactic purposes (40.83%). Oluwasile et al. [31] revealed that four (6.9%) poultry farmers used antibiotics as growth promoters. It is bad practice for farmers to sell or consume animals that do not recover from their sickness following antibiotic treatments. These animals may end up at the abattoir and processed into meats, which will enter the food chain. The meats produced from these animals are potential sources of antibiotic-resistant bacteria, which can easily be consumed by humans, thus increasing the antibiotic resistance burden.
The RTE meats in this study were sources of E. coli, with the prevalence being highest in chevon and lowest in pork. The presence of E. coli in RTE meats is due to poor pre- and postcooking handling practices, resulting in direct or indirect fecal and/or environmental contamination. Pathogenic E. coli is known to cause kidney failure, low blood platelets and hemolytic anemia [32]. In Italy, Nobili et al. [33] isolated E. coli from RTE hamburger and beef carpaccio, and these E. coli strains were positive for vtx1 genes. Outbreaks of Shiga toxin-producing E. coli (STEC) associated with the consumption of RTE cooked and processed meat products in Australia [34] and deli meats in the USA [35] have been reported. This study is also comparable to the findings of Hassanin et al. [36], who reported that E. coli were present in RTE meats such as hawawshi (46.7%), kofta (40%) and shawerma (33.3%) in a study conducted in Egypt. Ahmadi et al. [37] examined RTE meats and meat products in India and reported that meat curry (12.12%) and nonveg momo (4.0%) were positive for E. coli. In Bangladesh, Rahman et al. [38] reported that RTE chicken (49.02%) and beef (70.00%) samples were contaminated by E. coli. E. coli was detected in 32.0% of RTE meats from Latvia [39]. Contrary to the present work, Syne et al. [10] did not find E. coli in RTE meats sampled in Trinidad but did detect E. coli in some precooked RTE samples. In Europe, low contamination rates (2.21%) of STEC were reported in meat products and meat preparations from mixed sources [40].
The RTE E. coli isolates exhibited >50% resistance to teicoplanin, amoxicillin/clavulanic acid, tetracycline, azithromycin and sulfamethoxazole/trimethoprim. Lower (19–23%) resistance was observed for ceftriaxone, ciprofloxacin and gentamicin. Among the antibiotics used by livestock farmers in this study to treat their animals were tetracycline, ciprofloxacin, amoxicillin/clavulanic acid and gentamicin. Tetracycline and amoxicillin/clavulanic acid were used by most farmers, and high resistance to these antibiotics were exhibited by RTE E. coli isolates. Both tetracycline and amoxicillin/clavulanic acid are broad-spectrum antibiotics. Tetracycline destroys bacteria by inhibiting protein synthesis, while amoxicillin/clavulanic acid does the same by inhibiting biosynthesis of the peptidoglycan layer in the cell wall [41,42]. A relatively higher proportion of E. coli species showed intermediate resistances to gentamicin, sulfamethoxazole/trimethoprim, ceftriaxone, ciprofloxacin and azithromycin. Intermediate resistance suggests potential future resistance, and such isolates are cumbersome to handle or must be destroyed when they are responsible for causing infections [43,44,45]. Harakeh et al. [46] reported that E. coli of RTE meats origin were 100% resistant to trimethoprim/sulfamethoxazole and teicoplanin and 88.9% resistant to erythromycin, clindamycin, vancomycin and oxacillin. This study also found high resistance to teicoplanin but lower resistance to trimethoprim/sulfamethoxazole. Susceptibility to gentamicin was very low in this study compared to that of Harakeh et al. [46], which was 100%. Rahman et al. [38] reported that E. coli from RTE meats were resistant to amoxicillin (76.00%), sulfonamide–trimethoprim, (84.00%) and oxytetracycline (92%), while E. coli of RTE from beef showed resistance to oxytetracycline (92%) but susceptibility to gentamicin (100%) and ciprofloxacin (100%). This study found lower susceptibility to gentamicin and ciprofloxacin. Multidrug resistance (resistance to three or more antibiotics) was observed among most of the RTE meat E. coli isolates. Most of the isolates also exhibited different resistance profiles and were either resistant to two (6.45%), three (16.13%), four (22.58%), five (32.26%), six (12.90%) or seven (9.68%) antibiotics. Similar findings were made by Harakeh et al. [46] and Rahman et al. [38]. Multidrug resistance has been linked to the use of antibiotics in livestock production for prophylactics, treatment of animals and as growth promoters [10,47], which is in agreement with the findings of this study.
4. Materials and Methods
4.1. Study Area
The study was carried out in Bolgatanga, Ghana. Bolgatanga is the Upper East regional capital and situated between latitudes 10°30’ and 10°50’ North and longitudes 0°30’ and 1°00’ West [48]. Bolgatanga is urban and has a population of 66,685 [48].
4.2. Study Population, Sample Size and Sampling Method
The study population was ruminant and nonruminant farmers who were willing to take part in the study. The sample size was 376 livestock farmers, and they were selected using snow ball sampling technique. According to this, each farmer we contacted referred us to and recruited other farmers willing to take part in the survey. The sample size was obtained by querying the population of livestock farmers in the sample size calculator [49], and a sample size of 376 was obtained at a confidence level of 95%.
4.3. Structure of Questionnaire
The study used semistructured questionnaires, which included both open- and close-ended questions to collect information from livestock farmers (the questionnaire used has been provided as Supplementary Materials). The participants’ personal details, the antibiotics used for treatments to improve animal health and farmers’ general knowledge of antibiotics were assessed.
4.4. Sampling of Ready-to-Eat Meats
Sampling was conducted from January to October, 2019. Five samples each of mutton, chevon, beef, pork, chicken and guinea fowl were collected each month. In total, 300 RTE meat samples comprising 50 mutton, 50 chevon, 50 beef, 50 pork, 50 chicken and 50 guinea fowl meats were collected randomly from street vendors to investigate the existence of E. coli. Sterile surface swab template (10 cm2) was placed on the surface of each RTE meat and swabbed with a sterile swab stick. The swabbed samples of RTE meat were transported under 4 °C to the laboratory for microbial analysis.
4.5. Isolation and Confirmation of E. coli
This was done using a slightly modified method of Feng et al. [50] and Adzitey et al. [12]. Swabs were broken into universal bottles containing 9 mL of buffered peptone water and incubated for 24 h at 37 °C. A loopful of culture from the buffered peptone water was streaked onto Levines’s eosin methylene blue (LEMB) agar and then incubated for 24 h at 37 °C. Presumptive E. coli isolates on the LEMB agar were streaked onto tryptic soy agar and incubated for 24 h at 37 °C for purification. Three to five presumptive E. coli isolates from each plate were confirmed by Gram staining, growth in brilliant green bile with Durham tubes, growth in nitrate agar and latex agglutination test for E. coli. All media used were purchased from Oxoid Limited, Basingstoke, UK.
4.6. Antimicrobial Susceptibility Test
This was done using the disk diffusion method by Bauer et al. [51]. A total of nine antibiotics—amoxicillin/clavulanic acid 30 µg (Amc), azithromycin 15 µg (Azm), ceftriaxone 30 µg (Cro), chloramphenicol 30 µg (C), ciprofloxacin 5 µg (Cip), gentamycin 10 µg (Cn), teicoplanin 30 µg (Tec), tetracycline 30 µg (Te) and sulfamethoxazole/trimethoprim (Sxt)—were used. Purified cultures of E. coli were grown for 16−18 h in trypticase soy broth (TSB) at 37 °C, after which the cultures were adjusted to 0.5 McFarland solution and spread on the surface of Mueller–Hinton agar using sterile cotton swabs. Four or five antibiotic disks were placed on the surface of the Mueller–Hinton agar plates at a distance to avoid overlapping of inhibition zones. The plates were incubated overnight at 37 °C. Inhibition zones were measured, and the results were interpreted as sensitive, intermediate resistant or resistant according to Clinical and Laboratory Standards Institute guidelines [52]. All media and antibiotic disks used were purchased from Oxoid Limited, Basingstoke, UK.
4.7. Analysis of Data
Results from the questionnaires were analyzed using SPSS (Statistical Package for Social Sciences) version 20. Chi square test (χ2) was used to show the relationships between some of the parameters, and significant differences were considered when p ≤ 0.05.
5. Conclusions
The antibiotics used by farmers have a link with the resistance pattern of bacteria isolated from the animals they use them on, which may end up in meat and meat products. The RTE meats in this study were sources of resistant E. coli isolates. Therefore, RTE meats in Ghana is a potential public health hazard and could be a route for transmission of antibiotic-resistant E. coli. This study recommends training farmers on antibiotics and their usage and training RTE meat processors on hygienic meat handling.
Supplementary Materials
The questionnaire used for the study is available online at https://www.mdpi.com/2079-6382/9/12/869/s1.
Author Contributions
Conceptualization, F.A. and N.H.; methodology, A.A., F.A. and N.H.; software, A.A., F.A. and N.H.; validation, F.A., A.A. and N.H.; formal analysis, F.A. and A.A.; investigation, F.A. and A.A.; resources, F.A., A.A. and N.H.; data curation, F.A. and A.A.; writing—original draft preparation, F.A. and A.A.; writing—review and editing, F.A., A.A. and N.H.; supervision, F.A. and N.H.; funding acquisition, F.A., A.A. and N.H. All authors have read and agreed to the published version of the manuscript.
Funding
Grant for publication fee was provided by Universiti Malaysia Sabah, Jalan UMS, 88400, Kota Kinabalu, Sabah, Malaysia.
Acknowledgments
The authors are grateful to the University for Development Studies for allowing them to use the Spanish Laboratory, Nyankpala Campus for microbiological analysis and the livestock farmers who willingly took part in the survey.
Conflicts of Interest
The authors declare no conflict of interest.
References
- McAfee, A.J.; McSorley, E.M.; Cuskelly, G.J.; Moss, B.W.; Wallace, J.M.; Bonham, M.P.; Fearon, A.M. Red meat consumption: An overview of the risks and benefits. Meat Sci. 2010, 84, 1–13. [Google Scholar] [CrossRef]
- Rao, V.A.; Thulasi, G.; Ruban, S.W. Meat quality characteristics of non-descript buffalo as affected by age and sex. World Appl. Sci. J. 2009, 6, 1058–1065. [Google Scholar]
- Akbar, A.; Anal, A.K. Food safety concerns and food-borne pathogens, Salmonella, Escherichia coli and Campylobacter. FUUAST J. Biol. 2011, 1, 5–17. [Google Scholar]
- Hughes, C.; Gillespie, I.A.; O‘Brien, S.J. The breakdowns in food safety group. foodborne transmission of infectious intestinal disease in England and Wales, 1992–2003. Food Control 2007, 18, 766–772. [Google Scholar] [CrossRef]
- Akanele, A.E.; Chukwu, U.S.M.O.; Ahudie, B.C.M. Microbiological contamination of food: the mechanisms, impacts and prevention. Int. J. Sci. Tech. Res. 2016, 5, 65–79. [Google Scholar]
- Adzitey, F. Incidence and antimicrobial susceptibility of Escherichia coli isolated from beef (meat muscle, liver and kidney) samples in Wa Abattoir, Ghana. Cogent Food Agric. 2020, 6, 2–10. [Google Scholar] [CrossRef]
- Yousef, A.E.; Balasubramaniam, V.M. Physical methods of food preservation. In Food Microbiology: Fundamentals and Frontiers, 4th ed.; Doyle, M.P., Buchanan, R.L., Eds.; ASM Press: Washington, DC, USA, 2012. [Google Scholar]
- Henriques, A.R.; Fraqueza, M.J. Listeria monocytogenes and ready-to-eat meat-based food products: Incidence and control. In Listeria Monocytogenes: Incidence, Growth Behavior and Control, 1st ed.; Nova Science Publishers: New York, NY, USA, 2015; pp. 71–103. [Google Scholar]
- Mor-Mur, M.; Yuste, J. Emerging bacterial pathogens in meat and poultry: An overview. Food Biop. Tech. 2010, 3, 24. [Google Scholar] [CrossRef]
- Syne, S.-M.; Ramsubhag, A.; Adesiyun, A.A. Microbiological hazard analysis of ready-to-eat meats processed at a food plant in Trinidad, West Indies. Infect. Ecol. Epid. 2013, 3, 1. [Google Scholar] [CrossRef]
- Adzitey, F.; Ekli, R.; Abu, A. Prevalence and antibiotic susceptibility of Staphylococcus aureus isolated from raw and grilled beef in Nyankpala community in the Northern Region of Ghana. Cogent Food Agric. 2019, 5, 1671115. [Google Scholar] [CrossRef]
- Adzitey, F.; Ekli, R.; Aduah, M. Incidence and antibiotic susceptibility of Staphylococcus aureus isolated from ready-to-eat meats in the environs of Bolgatanga Municipality of Ghana. Cogent Environ. Sci. 2020, 6, 1791463. [Google Scholar] [CrossRef]
- Pitout, J. Extraintestinal pathogenic Escherichia coli: A combination of virulence with antibiotic resistance. Front. Microbial. 2012, 3, 9. [Google Scholar] [CrossRef] [PubMed]
- Painter, J.A.; Hoekstra, R.M.; Ayers, T.; Tauxe, R.V.; Braden, C.R.; Angulo, F.J.; Griffin, P.M. Attribution of foodborne illnesses, hospitalizations, and deaths to food commodities by using outbreak data, United States, 1998–2008. Emerg. Infect. Dis. 2013, 19, 407. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. E. coli. 2018. Available online: https://www.who.int/news-room/fact-sheets/detail/e-coli (accessed on 9 September 2020).
- Rane, S. Street vended food in developing world: Hazard analyses. Indian J. Microbiol. 2011, 51, 100–106. [Google Scholar] [CrossRef] [PubMed]
- Agbodaze, D.; Nmai, P.N.; Robertson, F.; Yeboah-Manu, D.; Owusu-Darko, K.; Addo, K. Microbiological quality of khebab consumed in the Accra metropolis. Ghana Med. J. 2015, 39, 46–49. [Google Scholar] [CrossRef] [PubMed]
- Abakari, G.; Cobbina, S.J.; Yeleliere, E. Microbial quality of ready-to-eat vegetable salads vended in the central business district of Tamale, Ghana. Int. J. Food Cont. 2018, 5, 3. [Google Scholar] [CrossRef]
- Ofosu, A.H.; Dzigbede, B.A.; Agidi, J.E.L.; Adjei, J.; Koranteng, A. A study into microbial quality of ready to eat foods sold in the Sunyani Municipality of Ghana. Glob. J. Biol. Agric. Health Sci. 2014, 3, 84–91. [Google Scholar]
- Adzitey, F.; Teye, G.A.; Anachinaba, I.A. Microbial quality of fresh and smoked guinea fowl meat sold in the Bolgatanga Municipality, Ghana. Asian J. Poult. Sci. 2015, 9, 165–171. [Google Scholar] [CrossRef][Green Version]
- Pelaez, F. The historical delivery of antibiotics from microbial natural products—Can history repeat? Biochem. Pharm. 2006, 71, 981–990. [Google Scholar] [CrossRef]
- Ventola, C.L. The antibiotic resistance crisis: Part 1: Causes and threats. Pharm. Therap. 2015, 40, 277. [Google Scholar]
- Smith, D.L.; Harris, A.D.; Johnson, J.A.; Silbergeld, E.K.; Morris, J.G. Animal antibiotic use has an early but important impact on the emergence of antibiotic resistance in human commensal bacteria. Proc. Nat. Acad. Sci. USA 2002, 99, 6434–6439. [Google Scholar] [CrossRef]
- Huijbers, P.M.C. Transmission of Antibiotic Resistance from Animals to Humans: Broilers as a Reservoir of ESBL-Producing Bacteria. Ph.D. Thesis, Wageningen University, Wageningen, The Netherlands, 2016. Available online: https://research.wur.nl/en/publications/transmission-of-antibiotic-resistance-from-animals-to-humans-broi (accessed on 5 November 2020).
- Muloi, D.; Ward, M.J.; Pedersen, A.B.; Fèvre, E.M.; Woolhouse, M.E.J.; van Bunnik, B.A.D. Are food animals responsible for transfer of antimicrobial-resistant Escherichia coli or their resistance determinants to human populations? A systematic review. Foodborne Path. Dis. 2018, 15, 467–474. [Google Scholar] [CrossRef] [PubMed]
- Adesokan, H.K.; Akanbi, I.O.; Akanbi, I.M.; Obaweda, R.A. Pattern of antimicrobial usage in livestock animals in south-western Nigeria: The need for alternative plans. Onderstepoort J. Vet. Res. 2015, 82, 1–6. [Google Scholar] [CrossRef]
- Katakweba, A.A.S.; Mtambo, M.M.A.; Olsen, J.E.; Muhairwa, A.P. Awareness of human health risks associated with the use of antibiotics among livestock keepers and factors that contribute to selection of antibiotic resistance bacteria within livestock in Tanzania. Livest. Res. Rur. Dev. 2012, 24, 170. [Google Scholar]
- Akansale, R.; Adzitey, F.; Teye, G. Knowledge of farmers in antibiotic usage and investigation of antibiotic residues in meats in the Sunyani Municipality of Ghana. J. Food Safe. Hyg. 2019, 5, 155–164. [Google Scholar]
- Ozturk, Y.; Celik, S.; Sahin, E.; Acik, M.N.; Cetinkaya, B. Assessment of farmers’ knowledge, attitudes and practices on antibiotics and antimicrobial resistance. Animals 2019, 9, 653. [Google Scholar] [CrossRef] [PubMed]
- Ferdous, J.; Sachi, S.; Noman, Z.A.; Hussani, S.M.A.K.; Sarker, Y.A.; Sikder, M.H. Assessing farmers’ perspective on antibiotic usage and management practices in small-scale layer farms of Mymensingh district, Bangladesh. Vet. World. 2019, 2, 1441. [Google Scholar] [CrossRef]
- Oluwasile, B.B.; Agbaje, M.; Ojo, O.E.; Dipeolu, M.A. Antibiotic usage pattern in selected poultry farms in Ogun state. Sokoto J. Vet. Sci. 2014, 12, 45–50. [Google Scholar] [CrossRef]
- World Health Organization and WHO Advisory Group on Integrated Surveillance of Antimicrobial Resistance. Critically Important Antimicrobials for human Medicine: Ranking of Antimicrobial Agents for Risk Management of Antimicrobial Resistance Due to non-Human Use, 5th rev. World Health Organization. 2017. Available online: https://apps.who.int/iris/handle/10665/255027 (accessed on 9 September 2020).
- Nobili, G.; Franconieri, I.; La Bella, G.; Basanisi, M.G.; La Salandra, G. Prevalence of verocytotoxigenic Escherichia coli strains isolated from raw beef in southern Italy. Int. J. Food Microbiol. 2017, 257, 201–205. [Google Scholar] [CrossRef]
- Rajpura, A.; Lamden, K.; Forster, S.; Clarke, S.; Cheesbrough, J.; Gornall, S.; Waterworth, S. Large outbreak of infection with Escherichia coli O157 PT21/28 in Eccleston, Lancashire, due to cross contamination at a butcher’s counter. Com. Dis. Pub. Health 2003, 6, 279–284. [Google Scholar]
- CDC (2015) Foodborne outbreak online database (FOOD). Centers for Disease Control and Prevention, Atlanta. Available online: http://wwwn.cdc.gov/foodborneoutbreaks/ (accessed on 3 February 2016).
- Hassanin, F.S.; Reham, A.A.; Shawky, N.A.; Gomaa, W.M. Incidence of Escherichia coli and Salmonella in ready to eat foods. Benha Vet. Med. J. 2014, 27, 84–91. [Google Scholar]
- Ahmadi, S.A.; Panda, A.K.; Kumar, Y.; Brahmne, H.G. Prevalence of Escherichia coli and Salmonella spp. in ready-to-eat meat and meat products in Himachal Pradesh. J. Com. Dis. 2012, 44, 71–77. [Google Scholar]
- Rahman, M.A.; Rahman, A.K.; Islam, M.A.; Alam, M.M. Antimicrobial resistance of Escherichia coli isolated from milk, beef and chicken meat in Bangladesh Bangl. J. Vet. Med. 2017, 2. [Google Scholar]
- Ciekure, E.; Siksna, I.; Valcina, O.; Viksna, L.; Krumina, A. Microbiological quality of ready-to-eat products and potential risks for consumers in Latvia. Nat. Exact Appl. Sci. 2016, 70, 245–251. [Google Scholar]
- EFSA and ECDC (European Food Safety Authority and European Centre for Disease Prevention and Control). The European Union summary report on trends and sources of zoonoses, zoonotic agents and food-borne outbreaks in 2017. EFSA J. 2018, 16, 262. [Google Scholar]
- Chopra, I.; Roberts, M. Tetracycline antibiotics: Mode of action, applications, molecular biology, and epidemiology of bacterial resistance. Microbiol. Mol. Bio. Rev. 2001, 65, 232–260. [Google Scholar] [CrossRef]
- Hannoodee, E.J.; Wittler, M.M. Amoxicillin Clavulanate. 2020. Available online: https://www.ncbi.nlm.nih.gov/books/NBK538164/ (accessed on 9 September 2020).
- Weinstein, R.A.; Fridkin, S.K. Vancomycin-intermediate and-resistant Staphylococcus aureus: What the infectious disease specialist needs to know. Clin. Infect. Dis. 2001, 32, 108–115. [Google Scholar] [CrossRef]
- Adzitey, F.; Rusul, G.; Huda, N.; Cogan, T.; Corry, J. Prevalence, antibiotic resistance and RAPD typing of Campylobacter species isolated from ducks, duck rearing and processing environments in Penang, Malaysia. Int. J. Food Microbiol. 2012, 154, 197–205. [Google Scholar] [CrossRef]
- Fair, R.J.; Tor, Y. Antibiotics and bacterial resistance in the 21st century. Perspect. Med. Chem. 2014, 6, 25–64. [Google Scholar] [CrossRef]
- Harakeh, S.; Yassine, H.; Gharios, M.; Barbour, E.; Hajjar, S.; El-Fadel, M.; Toufeili, I.; Tannous, R. Isolation, molecular characterization and antibiotic resistance patterns of Salmonella and Escherichia coli isolates from meat-based fast food in Lebanon. Sci. Total Environ. 2005, 341, 33–44. [Google Scholar] [CrossRef]
- Heredia, N.; García, S. Animals as sources of food-borne pathogens: A review. Anim. Nutr. 2018, 4, 250–255. [Google Scholar] [CrossRef]
- Ghana Statistical Service. Population and Housing Census. 2012. Available online: https://www.statsghana.gov.gh/gssmain/storage/img/marqueeupdater/Census2010_Summary_report_of_final_results.pdf (accessed on 9 September 2020).
- Anonymous. Sample Size Calculator. 2020. Available online: https://www.calculator.net/sample-size-calculator.html?type=1&cl=95&ci=5&pp=50&ps=66685&x=39&y=22 (accessed on 23 August 2019).
- Feng, P.; Weagant, S.D.; Jinneman, K. Bacteriological Analytical Manuel Chapter 4A: Diarrheagenic Escherichia coli. Available online: https://www.fda.gov/food/laboratory-methods-food/bam-chapter-4a-diarrheagenic-escherichia-coli (accessed on 23 April 2019).
- Bauer, A.W.; Kirby, W.M.M.; Sherris, J.C.; Turk, M. Antibiotic susceptibility testing by a standardized single disc method. American J. Clin. Pathol. 1966, 45, 493–496. [Google Scholar] [CrossRef]
- Clinical and Laboratory Standard Institute. Document M31-A3. In Performance Standards for Antimicrobial Disk and Dilution Susceptibility Tests for Bacteria Isolated from Animals, Approved Standard, 3rd ed.; Wayne: Pennsylvania, PA, USA, 2017. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).