Fostering Appropriate Antibiotic Use in a Complex Intervention: Mixed-Methods Process Evaluation Alongside the Cluster-Randomized Trial ARena
Abstract
1. Introduction
2. Results
2.1. Overview
2.2. Sociodemographic Characteristics of Survey Respondents
2.3. Sociodemographic Characteristics of Interview Participants
2.4. Implementation Program
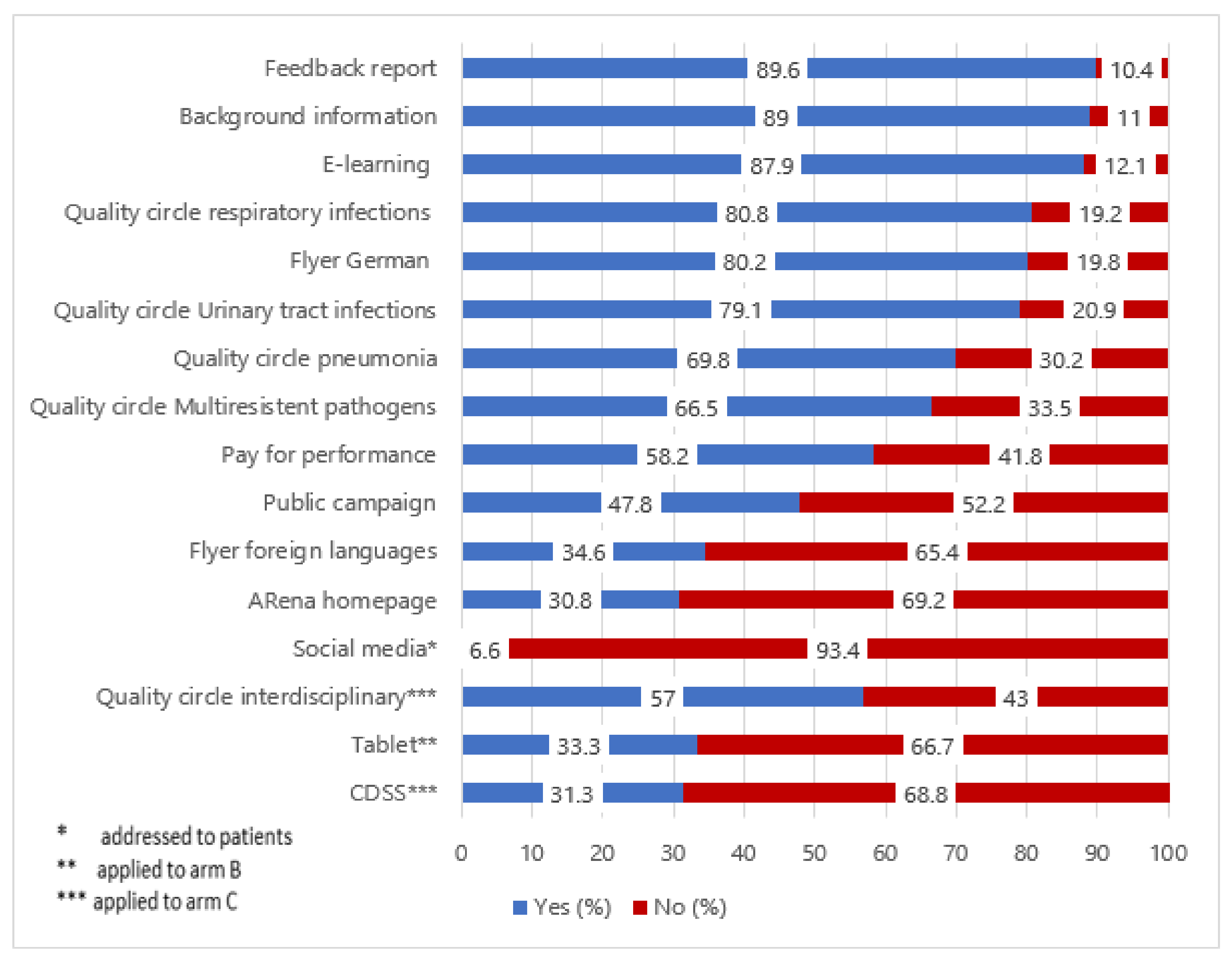
2.4.1. Uptake of Intervention Components
2.4.2. Effort for Integration
2.4.3. Perceived Reach and Impact
“So, you think more intensely about using one or the other antibiotic.”A03#74
“Patients became more sensitized as well and accepted reasons for holding back on antibiotics.”Phys07#60
2.4.4. Compatibility and Clarity
“I’ve got to give something to take home. Something coming from me, reflecting my attitudes and this [flyer] didn’t suit me […].”Phys19#32
“Of course, there has been the question which antibiotic works best in our region. So, there are differences which sometimes deviate from guideline recommendations.”Phys11#40
2.5. Organizational Factors
Social, Political and Legal Factors
“It would be good, of course, if these interventions which were quite accelerated, won’t be the last for the next ten years.”NM#03#28
“So, medical care centers with more than 80 employed physicians represent quite a market power and no primary care network can ultimately say: ‘Okay, we’re a conglomeration of established physicians, but in addition we are a power to be reckoned.”Sh05#46
2.6. Incentives and Resources
“If reimbursement changed, one question would be how to create incentives. Obviously, if reimbursement of ‘weaker’ medicine would be higher,—short consultation, writing a little prescription and off you go—that’s something basic, I suppose. So, less activism, less diagnostics, more talking, is not very well compensated, of course.”Phys08#80
2.7. Primary Care Networks
“You have to educate yourself together, you have to know that others do it the same way because we’ve already seen clearly […] patients from external physicians come to us and I also do see it in the on-call practice, if patients come from external physicians, there is a difference between PCN physicians and non-PCN physicians in treatment procedures.”Phys02#44
2.8. Individual Factors of Health Professionals and Patients
“The desire for an antibiotic-based treatment noticeably decreased. The public campaign and flyers seem to have helped there as well. Patients are more frequently asking for complementary methods.”Phys02#18
2.9. Capacity for Change
“Scientific investigations showed us that the provision of benchmark procedures alone gets the physician to prescribe less […] and yes, me personally, I consider this to be even more important than money.”NM03#38
3. Discussion
3.1. Comparison to Prior Research
3.2. Strengths and Limitations
4. Materials and Methods
4.1. Study Design
4.2. Study Population for Survey
4.3. Study Population for Interviews
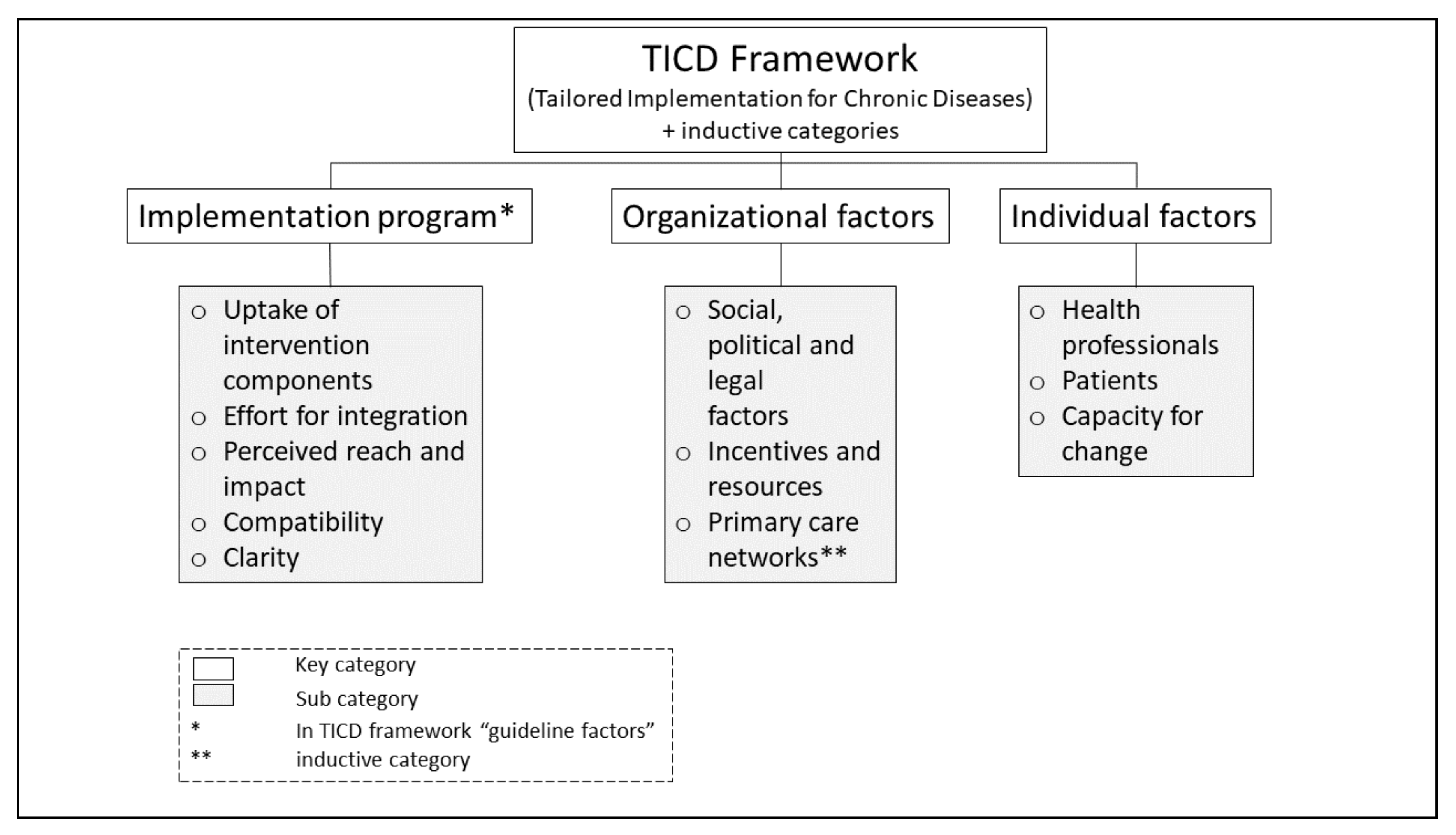
4.4. Data Collection and Analysis
4.4.1. Survey Study
4.4.2. Interview Study
4.5. Ethics Approval and Consent to Participate
4.6. Availability of Data and Materials
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
List of Abbreviations
| AOK | General local health insurance |
| AMR | Antimicrobial resistances |
| ARena | Sustainable reduction of antibiotic-induced antimicrobial resistance (German: Antibiotika-Resistenzentwicklung nachhaltig abwenden) |
| CDSS | Computerized decision support system |
| COREQ | Consolidated criteria for reporting qualitative research |
| DGPHSR-UH-HD | Department of General Practice and Health Services Research, University Hospital Heidelberg |
| G-BA | Federal Joint Committee (German: Gemeinsamer Bundesausschuss) |
| MA | Medical assistant |
| NM | Network Management |
| P4P | Pay for performance |
| PCNs | Primary care networks |
| Phys | Physician |
| QC | Quality circle |
| Sh | Stakeholder |
| TAP | Tailored Antimicrobial Resistance Program |
| TICDs | Tailored Implementation for Chronic Diseases |
| WHO | World Health Organization |
References
- World Health Organization. Fact Sheets. Antimicrobial Resistance. Internet: WHO. Available online: https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance (accessed on 31 July 2020).
- Centers for Disease Control and Prevention. Antibiotic Resistance Threats in the United States, 2019. Atlanta. GA: Centers for Disease Control and Prevention. Available online: https://www.cdc.gov/drugresis-tance/pdf/threatsreport/2019-ar-threats-report-508.pdf (accessed on 25 November 2020).
- European Centre for Disease Prevention and Control. Surveillance of Antimicrobial Resistance in Europe 2018. Stockholm 2019. Available online: https://www.ecdc.europa.eu/sites/default/files/documents/surveillance-antimicrobial-resistance-Europe-2018.pdf (accessed on 26 November 2020).
- Cassini, A.; Högberg, L.D.; Plachouras, D.; Quattrocchi, A.; Hoxha, A.; Simonsen, G.S.; Colomb-Cotinat, M.; Kretzschmar, M.E.; Devleesschauwer, B.; Cecchini, M.; et al. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: A population-level modelling analysis. Lancet Infect. Dis. 2019, 19, 56–66. [Google Scholar] [CrossRef]
- German Federal Ministry of Health. Bundesministerium Für Gesundheit. In DART 2020–Antibiotika-Resistenzen Bekämpfen Zum Wohl Von Mensch Und Tier; Bundesministerium Für Gesundheit: Berlin, Germany; Available online: https://www.bundesgesundheitsministerium.de/fileadmin/Dateien/3_Downloads/D/DART_2020/BMG_DART_2020_Bericht_dt.pdf (accessed on 3 November 2020).
- Federal Ministry of Health, Federal Ministry of Food and Agriculture, Federal Ministry of Education and Research. DART 2020 2nd Interim Report 2017. Available online: https://www.bundesgesundheitsministerium.de/fileadmin/Dateien/3_Downloads/D/DART_2020/DART2020_Interim_Report_2017.pdf (accessed on 3 November 2020).
- Abu Sin, M.; Nahrgang, S.; Ziegelmann, A.; Clarici, A.; Matz, S.; Tenhagen, B.-A.; Eckmanns, T. Globale und nationale Strategien gegen Antibiotikaresistenzen. Bundesgesundheitsblatt-Gesundh-Gesundh. 2018, 61, 507–514. [Google Scholar] [CrossRef] [PubMed]
- Kamradt, M.; Kaufmann-Kolle, P.; Andres, E.; Brand, T.; Klingenberg, A.; Glassen, K.; Poß-Doering, R.; Uhlmann, L.; Hees, K.; Weber, D.; et al. Sustainable reduction of antibiotic-induced antimicrobial resistance (ARena) in German ambulatory care: Study protocol of a cluster randomised trial. Implement. Sci. 2018, 1313, 23. [Google Scholar] [CrossRef]
- Moore, G.F.; Audrey, S.; Barker, M.; Bond, L.; Bonell, C.; Hardeman, W.; Moore, L.; O’Cathain, A.; Tinati, T.; Wight, D.; et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ Br. Med. J. 2015, 350, h1258. [Google Scholar] [CrossRef] [PubMed]
- Freund, T.; Everett, C.; Griffiths, P.; Hudon, C.; Naccarella, L.; Laurant, M. Skill mix, roles and remuneration in the primary care workforce: Who are the healthcare professionals in the primary care teams across the world? Int. J. Nurs. Stud. 2015, 52, 727–743. [Google Scholar] [CrossRef]
- Michie, S.; Richardson, M.; Johnston, M.; Abraham, C.; Francis, J.; Hardeman, W.; Eccles, M.P.; Cane, J.; Wood, C. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Ann. Behav. Med. 2013, 46, 81–95. [Google Scholar] [CrossRef]
- Shively, N.R.; Buehrle, D.J.; Wagener, M.M.; Clancy, C.J.; Decker, B.K. Improved Antibiotic Prescribing within a Veterans Affairs Primary Care System through a Multifaceted Intervention Centered on Peer Comparison of Overall Antibiotic Prescribing Rates. Antimicrob Agents Chemother. 2019, 64. [Google Scholar] [CrossRef]
- Roque, F.; Herdeiro, M.T.; Soares, S.; Teixeira Rodrigues, A.; Breitenfeld, L.; Figueiras, A. Educational interventions to improve prescription and dispensing of antibiotics: A systematic review. BMC Public Health 2014, 14, 1276. [Google Scholar] [CrossRef]
- McNulty, C.; Hawking, M.; Lecky, D.; Jones, L.; Owens, R.; Charlett, A.; Butle, C.; Moore, P.; Francis, N. Effects of primary care antimicrobial stewardship outreach on antibiotic use by general practice staff: Pragmatic randomized controlled trial of the TARGET antibiotics workshop. J. Antimicrob. Chemother. 2018, 73, 1423–1432. [Google Scholar] [CrossRef]
- Gerber, J.S.; Prasad, P.A.; Fiks, A.G.; Localio, A.R.; Grundmeier, R.W.; Bell, L.M.; Wasserman, R.; Keren, R.; Zaoutis, T.E. Effect of an outpatient antimicrobial stewardship intervention on broad-spectrum antibiotic prescribing by primary care pediatricians: A randomized trial. JAMA 2013, 309, 2345–2352. [Google Scholar] [CrossRef]
- Vinnard, C.; Linkin, D.R.; Localio, A.R.; Leonard, C.E.; Teal, V.L.; Fishman, N.O.; Hennessy, S. Effectiveness of interventions in reducing antibiotic use for upper respiratory infections in ambulatory care practices. Popul. Health Manag. 2013, 16, 22–27. [Google Scholar] [CrossRef] [PubMed]
- Gerber, J.S.; Prasad, P.A.; Fiks, A.G.; Localio, A.R.; Bell, L.M.; Keren, R.; Zaoutis, T.E. Durability of benefits of an outpatient antimicrobial stewardship intervention after discontinuation of audit and feedback. JAMA 2014, 312, 2569–2570. [Google Scholar] [CrossRef] [PubMed]
- Holstiege, J.; Mathes, T.; Pieper, D. Effects of computer-aided clinical decision support systems in improving antibiotic prescribing by primary care providers: A systematic review. J. Am. Med. Inform. Assoc. 2015, 22, 236–242. [Google Scholar] [CrossRef] [PubMed]
- Meeker, D.; Linder, J.A.; Fox, C.R.; Friedberg, M.W.; Persell, S.D.; Goldstein, N.J.; Knight, T.K.; Hay, J.W.; Doctor, J.N. Effect of Behavioral Interventions on Inappropriate Antibiotic Prescribing Among Primary Care Practices: A Randomized Clinical Trial. JAMA 2016, 315, 562–570. [Google Scholar] [CrossRef] [PubMed]
- Linder, J.A.; Meeker, D.; Fox, C.R.; Friedberg, M.W.; Persell, S.D.; Goldstein, N.J.; Doctor, J.N. Effects of Behavioral Interventions on Inappropriate Antibiotic Prescribing in Primary Care 12 Months After Stopping Interventions. JAMA. 2017, 318, 1391–1392. [Google Scholar] [CrossRef] [PubMed]
- Persell, S.D.; Doctor, J.N.; Friedberg, M.W.; Meeker, D.; Friesema, E.; Cooper, A.; Haryani, A.; Gregory, D.L.; Fox, C.R.; Goldstein, N.J. Behavioral interventions to reduce inappropriate antibiotic prescribing: A randomized pilot trial. BMC Infect. Dis. 2016, 16, 373. [Google Scholar] [CrossRef] [PubMed]
- Jeffs, L.; McIsaac, W.; Zahradnik, M.; Senthinathan, A.; Dresser, L.; McIntyre, M.; Tannenbaum, D.; Bell, C.; Morris, A. Barriers and facilitators to the uptake of an antimicrobial stewardship program in primary care: A qualitative study. PLoS ONE 2020, 15, e0223822. [Google Scholar] [CrossRef]
- King, L.M.; Fleming-Dutra, K.E.; Hicks, L.A. Advances in optimizing the prescription of antibiotics in outpatient settings. BMJ 2018, 363, k3047. [Google Scholar] [CrossRef]
- Ivers, N.; Jamtvedt, G.; Flottorp, S.; Young, J.M.; Odgaard-Jensen, J.; French, S.D.; O’Brien, M.A.; Johansen, M.; Grimshaw, J.; Oxman, A.D. Audit and feedback: Effects on professional practice and healthcare outcomes. Cochrane Database Syst. Rev. 2012, 6, CD000259. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention Control. Antimicrobial resistance surveillance in Europe. Annual report of the European Antimicrobial Resistance Surveillance Network (EARS-Net) 2015. Stockholm: ECDC; 2017. Available online: https://www.ecdc.europa.eu/en/publications-data/antimicrobial-resistance-surveillance-europe-2015#no-link (accessed on 26 November 2020).
- European Centre for Disease Prevention Control. Surveillance of antimicrobial consumption in Europe 2013‒2014. Stockholm: European Centre for Disease Prevention and Control, 2018. Available online: https://www.ecdc.europa.eu/en/publications-data/surveillance-antimicrobial-consumption-europe-2013-2014 (accessed on 26 November 2020).
- Holstiege, J.; Schulz, M.; Akmatov, M.; Steffen, A.; Bätzing, J. Outpatient Use of Systemic Antibiotics in Germany from 2010 to 2018—A Population-Based Study; Central Research Institute for Ambulatory Health Care in Germany (Zi): Berlin, Germany, 2019. [Google Scholar]
- Holstiege, J.; Schulz, M.; Akmatov, M.; Kern, W.; Steffen, A.; Bätzing, J. The decline in outpatient antibiotic use—An analysis of nationwide prescription data from 2010 to 2018. Dtsch. Ärzteblatt 2020, 117, 679–686. [Google Scholar] [CrossRef]
- Poss-Doering, R.; Weber, D.; Kamradt, M.; Andres, E.; Kaufmann-Kolle, P.; Wensing, M.; Szecsenyi, J. Baseline assessment of antibiotics prescribing for acute, non-complicated infections in primary care in Germany in the cluster randomized trial ARena. Antimicrob. Resist. Infect. Control. 2020. [Google Scholar] [CrossRef]
- Poss-Doering, R.; Kamradt, M.; Glassen, K.; Andres, E.; Kaufmann-Kolle, P.; Wensing, M. Promoting rational antibiotic prescribing for non-complicated infections: Understanding social influence in primary care networks in Germany. BMC Fam. Pract. 2020, 21, 51. [Google Scholar] [CrossRef] [PubMed]
- Huttner, B.; Goossens, H.; Verheij, T.; Harbarth, S. Characteristics and outcomes of public campaigns aimed at improving the use of antibiotics in outpatients in high-income countries. Lancet Infect. Dis. 2010, 10, 17–31. [Google Scholar] [CrossRef]
- Zucco, R.; Lavano, F.; Anfosso, R.; Bianco, A.; Pileggi, C.; Pavia, M. Internet and social media use for antibiotic-related information seeking: Findings from a survey among adult population in Italy. Int. J. Med. Inform. 2018, 111, 131–139. [Google Scholar] [CrossRef] [PubMed]
- Poss-Doering, R.; Kamradt, M.; Stuermlinger, A.; Glassen, K.; Kaufmann-Kolle, P.; Broermann, M.; Wensing, M. The complex phenomenon of dysrational antibiotics prescribing decisions in German primary healthcare: A qualitative interview study using dual process theory. Antimicrob. Resist. Infect. Control. 2020, 9, 6–11. [Google Scholar] [CrossRef] [PubMed]
- Salm, F.; On behalf of the RAI-Study Group; Schneider, S.; Schmücker, K.; Petruschke, I.; Kramer, T.S.; Hanke, R.; Schröder, C.; Heintze, C.; Schwantes, U.; et al. Antibiotic prescribing behavior among general practitioners–a questionnaire-based study in Germany. BMC Infect. Dis. 2018, 18, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Gordon, N.P.; Hornbrook, M.C. Older adults’ readiness to engage with eHealth patient education and self-care resources: A cross-sectional survey. BMC Health Serv. Res. 2018, 18, 220. [Google Scholar] [CrossRef]
- Poss-Doering, R.; Kuehn, L.; Kamradt, M.; Glassen, K.; Wensing, M. Applying Digital Information Delivery to Convert Habits of Antibiotic Use in Primary Care in Germany: Mixed-Methods Study. J. Med. Internet. Res. 2020, 22, e18200. [Google Scholar] [CrossRef]
- Schreiweis, B.; Pobiruchin, M.; Strotbaum, V.; Suleder, J.; Wiesner, M.; Bergh, B. Barriers and Facilitators to the Implementation of eHealth Services: Systematic Literature Analysis. J. Med. Internet. Res. 2019, 21, e14197. [Google Scholar] [CrossRef]
- Henshall, C.; Cipriani, A.; Ruvolo, D.; Macdonald, O.; Wolters, L.; Koychev, I. Implementing a digital clinical decision support tool for side effects of antipsychotics: A focus group study. Evid. Based Ment. Health 2019, 22, 56–60. [Google Scholar] [CrossRef]
- Neugebauer, M.; Ebert, M.; Vogelmann, R. Lack of information and provision of information at the workplace as potential reasons for inappropriate antibiotic therapy in Germany. Z. Evid. Fortbild. Qual. Gesundhwes 2019, 144–145, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Tonkin-Crine, S.; Tan, P.S.; Van Hecke, O.; Wang, K.; Roberts, N.W.; McCullough, A.; Hansen, M.P.; Butler, C.C.; Del Mar, C.B. Clinician-targeted interventions to influence antibiotic prescribing behaviour for acute respiratory infections in primary care: An overview of systematic reviews. Cochrane Database Syst. Rev. 2017, 9, CD012252. [Google Scholar] [CrossRef] [PubMed]
- Wensing, M.; Paech, B.; Roth, C.; Schwill, S. Learning, understanding and the use of information technology: A survey study among primary care physician trainees. BMC Health Serv. Res. 2019, 19, 728. [Google Scholar] [CrossRef] [PubMed]
- Jan, C.-F.; Lee, M.-C.; Chiu, C.-M.; Huang, C.-K.; Hwang, S.-J.; Chang, C.-J.; Chiu, T.-Y. Awareness of, attitude toward, and willingness to participate in pay for performance programs among family physicians: A cross-sectional study. BMC Fam. Pract. 2020, 21, 1–9. [Google Scholar] [CrossRef]
- Bundesministerium Für Gesundheit. DART 2020–Deutsche Antibiotika-Resistenzstrategie; Bundesministerium Für Gesundheit: Berlin, Germany, 2011; Available online: https://www.bundesgesundheitsministerium.de/fileadmin/Dateien/5_Publikationen/Gesundheit/Berichte/Bericht_DART_Deutsche_Antibiotika-Resistenzstrategie.pdf (accessed on 15 July 2020).
- Kaplan, N.M.; Khader, Y.S.; Alfaqih, M.A.; Saadeh, R.; Al Sawalha, L. Implementation of the WHO Approved “Tailoring Antimicrobial Resistance Programs (TAP)” Reduces Patients’ Request for Antibiotics. Antibiotics 2020, 9, 507. [Google Scholar] [CrossRef] [PubMed]
- Gabriel, J. Praxisnetze Im Wandel–Chancen Und Stärken Eines Versorgungsmodells. In Management Von Gesundheitsregionen III: Gesundheitsnetzwerke Zur Optimierung Der Krankenversorgung Durch Kooperation Und Vernetzung; Pfannstiel, M.A., Focke, A., Mehlich, H., Eds.; Springer Fachmedien Wiesbaden: Wiesbaden, Jermany, 2017; pp. 13–24. [Google Scholar]
- Tannenbaum, S.S.; Soulos, P.R.; Herrin, J.; Pollack, C.; Xu, X.; Christakis, N.A.; Forman, H.P.; Yu, J.B.; Killelea, B.K.; Wang, S.-Y.; et al. Surgeon peer network characteristics and adoption of new imaging techniques in breast cancer: A study of perioperative MRI. Cancer Med. 2018, 7, 5901–5909. [Google Scholar] [CrossRef]
- Muller, E.; Peres, R. The effect of social networks structure on innovation performance: A review and directions for research. Int. J. Res. Mark. 2019, 36, 3–19. [Google Scholar] [CrossRef]
- Christakis, N.A.; Fowler, J.H. Social contagion theory: Examining dynamic social networks and human behavior. Stat. Med. 2013, 32, 556–577. [Google Scholar] [CrossRef]
- On behalf of the ESAC Project Group; Adriaenssens, N.; Coenen, S.; Versporten, A.; Muller, A.; Minalu, G.; Faes, C.; Vankerckhoven, V.; Aerts, M.; Hens, N.; et al. European Surveillance of Antimicrobial Consumption (ESAC): Outpatient antibiotic use in Europe (1997–2009). J. Antimicrob. Chemother. 2011, 66, vi3–vi12. [Google Scholar] [CrossRef]
- Keating, N.L. Peer Influence and Opportunities for Physician Behavior Change. J. Natl. Cancer Inst. 2017, 109, djx009. [Google Scholar] [CrossRef]
- Pollack, C.E.; Soulos, P.R.; Herrin, J.; Xu, X.; Christakis, N.A.; Forman, H.P.; Yu, J.B.; Killelea, B.K.; Wang, S.-Y.; Gross, C.P. The Impact of Social Contagion on Physician Adoption of Advanced Imaging Tests in Breast Cancer. J. Natl. Cancer Inst. 2017, 109. [Google Scholar] [CrossRef]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care. 2007, 19, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Klingenberg, A.B.T.; Andres, E.; Kaufmann-Kolle, P.; Wambach, V.; Szecsenyi, J. Was wissen Patienten über Antibiotika, und wie häufig erwarten sie deren Verordnung? ZFA 2019. [CrossRef]
- Gale, N.K.; Heath, G.; Cameron, E.; Rashid, S.; Redwood, S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med. Res. Methodol. 2013, 13, 117. [Google Scholar] [CrossRef] [PubMed]
- Flottorp, S.A.; Oxman, A.D.; Krause, J.; Musila, N.R.; Wensing, M.; Godycki-Cwirko, M.; Baker, R.; Eccles, M.P. A checklist for identifying determinants of practice: A systematic review and synthesis of frameworks and taxonomies of factors that prevent or enable improvements in healthcare professional practice. Implement. Sci. 2013, 8, 35. [Google Scholar] [CrossRef]
| Survey Respondents (T0) | N | Physicians | Medical Assistants | Total |
|---|---|---|---|---|
| Sex (f/m) n (%) | 304 | 76/148 (34.0/66.0) | 80/0 (100/0) | 156/148 (51.3/48.7) |
| Age in years (range) (mean) | 299 | 35–73 (54.4) | 19–61 (38.7) | 19–73 (46.5) |
| Years of working experience (range) (mean) | 306 | 5–48 (25.4) | 1–40 (19.2) | 1–48 (22.3) |
| Working in general practice (%) | 309 | 75.3 | 76 | 75.6 |
| medical practitioner in private practice years (range) (mean) | 220 | 1–41 (17.7) | N/A | 220 (17.7) |
| Network member years (range) (mean) | 207 | 0–28 (10) | N/A | 10 |
| Participating in network events times/year (range) | 217 | 7.3 (0–50) | N/A | 7.3 (0–50) |
| Survey Respondents (T2) | ||||
| Sex (f/m) n (%) | 240 | 59/125 (32/68) | 56/0 (100/0) | 115/125 (48/52) |
| Age in years (range) (mean) | 35–73 (54.2) | 19–61 (39.5) | 19–73 (46.9) | |
| Experience in years (SD) (mean) | 7.9 (26.4) | 12.9 (19.3) | 24.8 (9.8) |
| Interview Participants (in 2018) | N | Physicians | Medical Assistants | Stakeholder | Total |
|---|---|---|---|---|---|
| Gender f/m (%) | 45 | 9/18 (33/66) | 11/0 (100/0) | 3/4 (43/57) | 23/22 (59/41) |
| Age in years range (mean) | 45 | 43–66 (55.2) | 20–60 (38.5) | 31–63 (46.3) | 31.3–63 (46.6) |
| Years of experience in current position range (mean) | 45 | 10–38 (26) | 2–40 (19) | 1–10 (5.8) | 1–40 (17) |
| Working in general practice (%) | 38 | 66.6 | 81.8 | N/A | 74.2 |
| Employed part-time n (%) | 4 | 1 (2.7) | 3 (27.3) | N/A | 4 (8.88) |
| PCN * member in years range (mean) | 27 | 2–23 (10) | N/A | N/A | 10 |
| Additional qualifications n | 7 | N/A | 7 | N/A | 7 |
| Interview participants (additional; in 2020) | |||||
| Sex f/m (%) | 6 | 2/1 (66/33) | N/A | 1/2 (33/66) | 3/3 (50/50) |
| Age years range (mean) | 6 | 58–66 (60.7) | N/A | 44–55 (49.7) | 44–66 (55.1) |
| PCN * management function years range (mean) | 3 | N/A | N/A | 8–22 (13) | 8–22 (13) |
| PCN * member in years range (mean) | 2 | 9–22 (15.5) | N/A | N/A | 9–22 (15.5) |
| Integrating Study Components into Practice Routines Was Associated with Great Effort | Agree * n (%) |
|---|---|
| Flyer German | 4 (6.9) |
| Flyer foreign languages | 6 (10.3) |
| Website | 14 (24.1) |
| Public campaign | 17 (29.3) |
| Social media content | 20 (34.5) |
| Tablet device | 29 (50.0) |
| Transferring Newly Gained Knowledge Was Associated with Great Effort | Agree * n (%) |
| Content of online training | 9 (15.5) |
| Content of background information | 11 (19.0) |
| Content of quality circles | 13 (22.4) |
| Content of feedback reports | 13 (22.4) |
| The Intervention Component Provided New Impulses | Agree *(%) | ||
|---|---|---|---|
| Intervention Arm | A | B | C |
| Online training | 48.5 | 59.7 | 40.8 |
| Quality circles | 72.1 | 83.6 | 79.6 |
| Feedback report | 58.8 | 65.7 | 55.1 |
| Background information | 73.5 | 68.7 | 73.5 |
| Patient flyer German | 35.3 | 53.7 | 53.1 |
| Patient flyer foreign | 13.2 | 19.4 | 22.4 |
| Website | 14.7 | 14.9 | 20.4 |
| Social media | 5.9 | 4.5 | 6.1 |
| Public campaign | 26.5 | 26.9 | 36.7 |
| Pay for performance | 32.4 | 37.3 | 30.6 |
| Tablet device | N/A | 9.0 | N/A |
| Interdisciplinary quality circles | N/A | N/A | 53.1 |
| Decision support tool | N/A | N/A | 16.3 |
| Participating in the Network | Agree T0/T1 (%) | Neutral T0/T1 (%) | Disagree T0/T1 (%) |
|---|---|---|---|
| provides motivation for guideline-oriented patient care | 70.5/60.0 | 18.5/19.0 | 11/22.0 |
| furthers shared-decision making | 60.8/59.0 | 19.8/24.0 | 19.4/18.0 |
| supports management of patient expectations | 61.2/51.0 | 21.6/30.0 | 17.2/19.0 |
| supports implementation of new routines | 74.0/59.0 | 16.3/18.0 | 9.7/24.0 |
| impacts antibiotic prescribing decisions | 43.3/36.0 | 22.1/22.0 | 34.5/43.0 |
| In My Primary Care Network | Agree T0/T1 (%) | Neutral T0/T1 (%) | Disagree T0/T1 (%) |
| antibiotics therapy is discussed | 89.5/86.0 | 8.8/10.0 | 1.7/4.0 |
| peer exchange on guideline-oriented antibiotics therapy is facilitated | 79.9/79.0 | 14.5/11.0 | 5.6/10.0 |
| exchange about antibiotic prescribing routines for non-complicated infections is contingent | 71.5/73.0 | 18.4/16.0 | 10.1/11.0 |
| there are conventions about the use of antibiotics for non-complicated infections | 65.8/72.0 | 21.5/16.0 | 12.7/12.0 |
| training on guideline-oriented antibiotics therapy is offered | 89.0/75.0 | 6.6/18.0 | 4.4/7.0 |
| I have taken part in training on guideline-oriented antibiotics therapy | 89.0/87.0 | 6.6/9.0 | 4.4/4.0 |
| Source | Physicians | Medical Assistants | Stakeholders | Description |
|---|---|---|---|---|
| Interviews (n) | 27 | 11 | 7 | Over telephone |
| Socio-demographic questionnaire (n) | 27 | 11 | 7 | Paper based |
| Thematic in-depth interviews (n) | 3 | N/A | 3 | over telephone |
| Survey T0 (n) | 229 | 80 | N/A | Paper based |
| Survey T1 (n) | 200 | 73 | N/A | Paper based |
| Survey T2 (n) | 184 | 58 | N/A | Paper based |
| Online survey (n) | N/A | N/A | 10 | Online |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Poss-Doering, R.; Kühn, L.; Kamradt, M.; Stürmlinger, A.; Glassen, K.; Andres, E.; Kaufmann-Kolle, P.; Wambach, V.; Bader, L.; Szecsenyi, J.; et al. Fostering Appropriate Antibiotic Use in a Complex Intervention: Mixed-Methods Process Evaluation Alongside the Cluster-Randomized Trial ARena. Antibiotics 2020, 9, 878. https://doi.org/10.3390/antibiotics9120878
Poss-Doering R, Kühn L, Kamradt M, Stürmlinger A, Glassen K, Andres E, Kaufmann-Kolle P, Wambach V, Bader L, Szecsenyi J, et al. Fostering Appropriate Antibiotic Use in a Complex Intervention: Mixed-Methods Process Evaluation Alongside the Cluster-Randomized Trial ARena. Antibiotics. 2020; 9(12):878. https://doi.org/10.3390/antibiotics9120878
Chicago/Turabian StylePoss-Doering, Regina, Lukas Kühn, Martina Kamradt, Anna Stürmlinger, Katharina Glassen, Edith Andres, Petra Kaufmann-Kolle, Veit Wambach, Lutz Bader, Joachim Szecsenyi, and et al. 2020. "Fostering Appropriate Antibiotic Use in a Complex Intervention: Mixed-Methods Process Evaluation Alongside the Cluster-Randomized Trial ARena" Antibiotics 9, no. 12: 878. https://doi.org/10.3390/antibiotics9120878
APA StylePoss-Doering, R., Kühn, L., Kamradt, M., Stürmlinger, A., Glassen, K., Andres, E., Kaufmann-Kolle, P., Wambach, V., Bader, L., Szecsenyi, J., & Wensing, M. (2020). Fostering Appropriate Antibiotic Use in a Complex Intervention: Mixed-Methods Process Evaluation Alongside the Cluster-Randomized Trial ARena. Antibiotics, 9(12), 878. https://doi.org/10.3390/antibiotics9120878






