Dextran-Thyme Magnesium-Doped Hydroxyapatite Composite Antimicrobial Coatings
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Dextran-Thyme Coated Magnesium-Doped Hydroxyapatite (10MgHAp-Dex-thyme) Nanoparticle Suspensions
2.3. Deposition of 10MgHAp-Dex-Thyme Coatings
2.4. Physico-Chemical and Mechanical Characterization Methods
- (a)
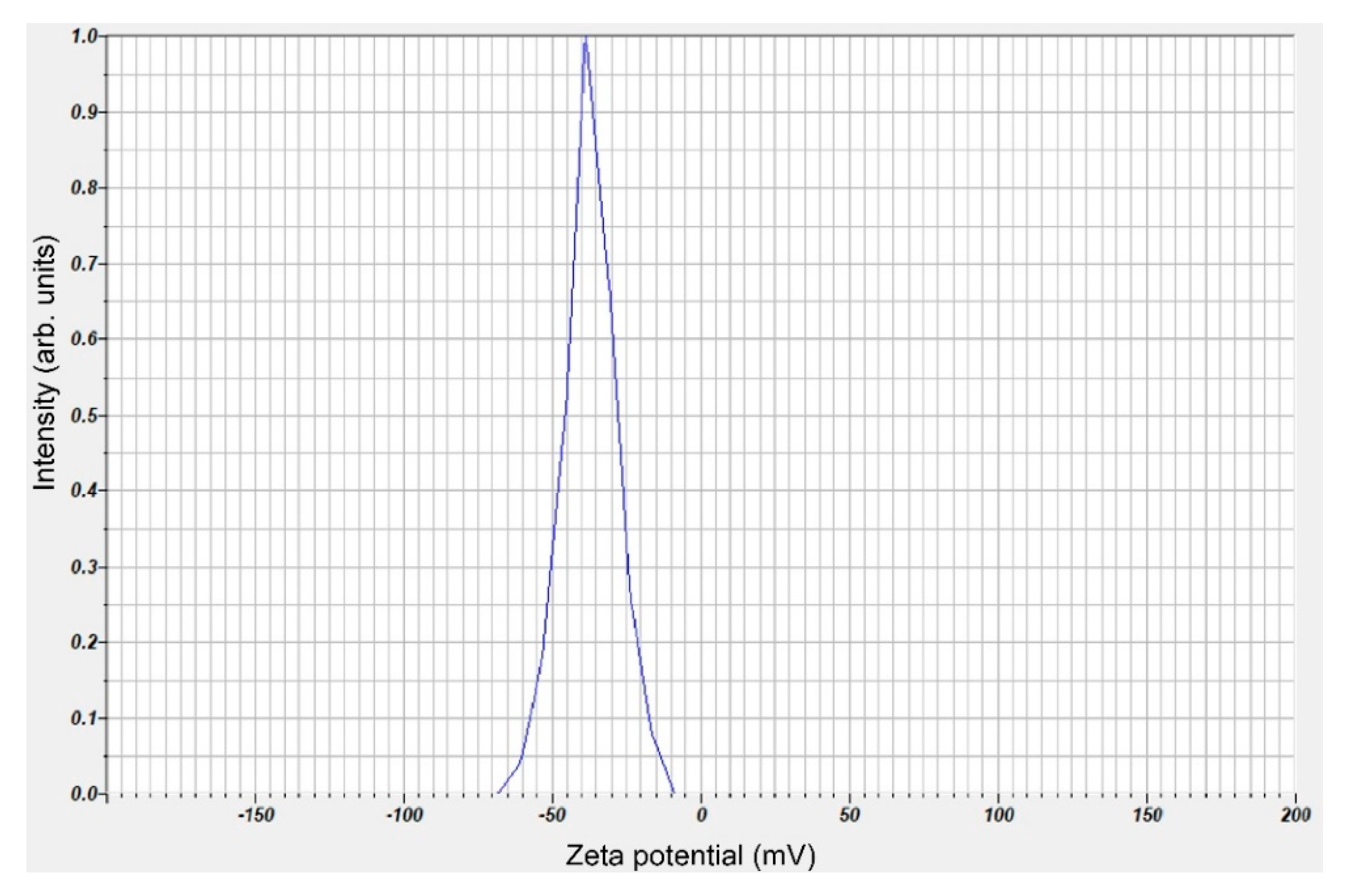
- The zeta-potential (ZP) measurements were carried out using a Horiba-Jobin Yvon SZ-100 Nanoparticle Analyzer (Horiba Ltd., Kyoto, Japan) at 25 ± 1 °C. The wavelength at which the 2 He–Ne laser beams were operated was 532 nm. The samples were measured in triplicate, and the results were averaged. The zeta-potential was performed on the diluted sample.
- (b)
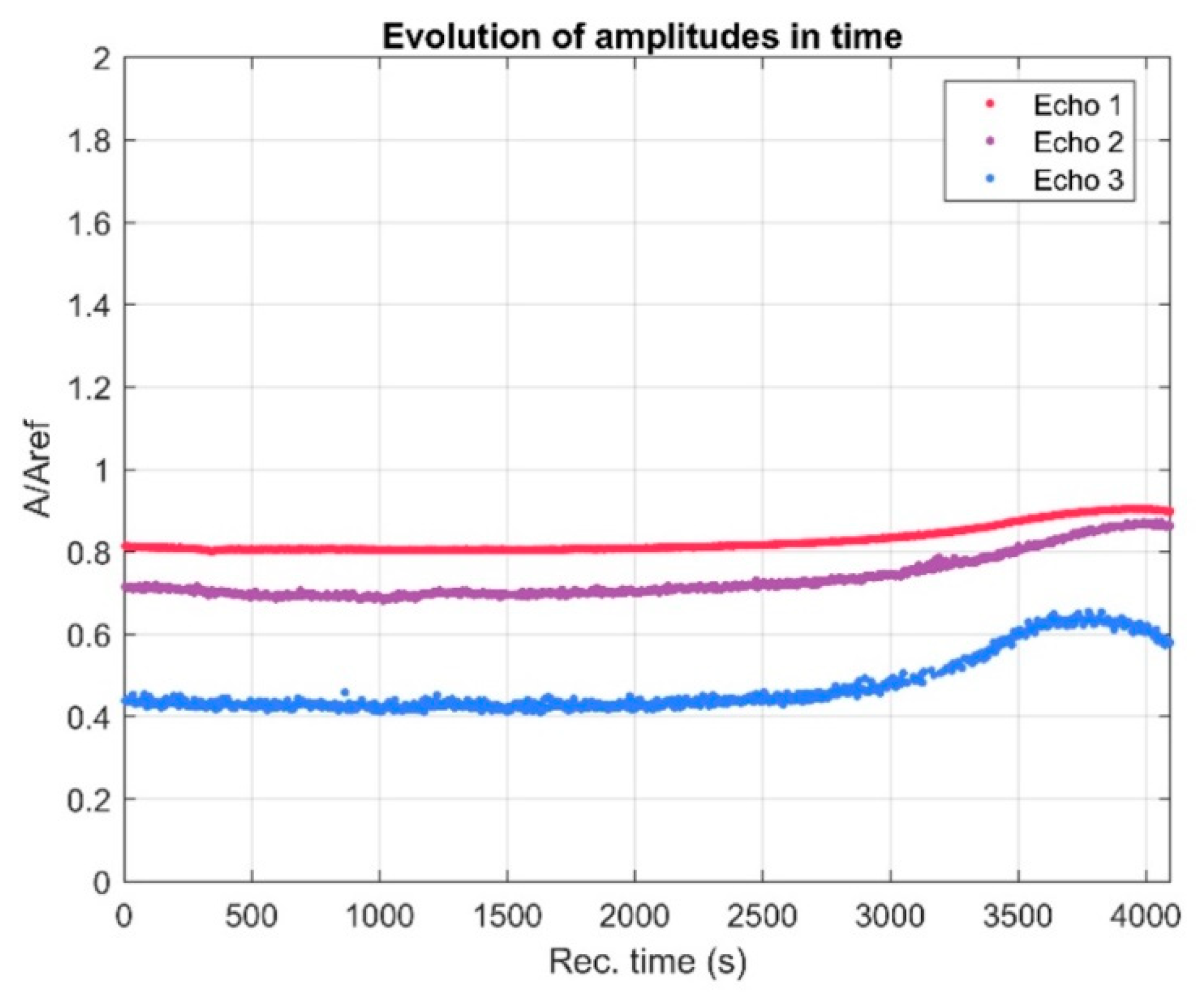
- The ultrasound measurements were performed on concentrated solutions obtained from the preparation process. The ultrasound pulses were sent by the analyzed suspension [38]. Digital signals from the oscilloscope were recorded at a very precise interval of 5 s. For good signal processing, a comparison with the properties of double-distilled water (the most stable suspension) was performed. Double-distilled water was considered as reference fluid, analyzed under the same experimental conditions.
- (c)
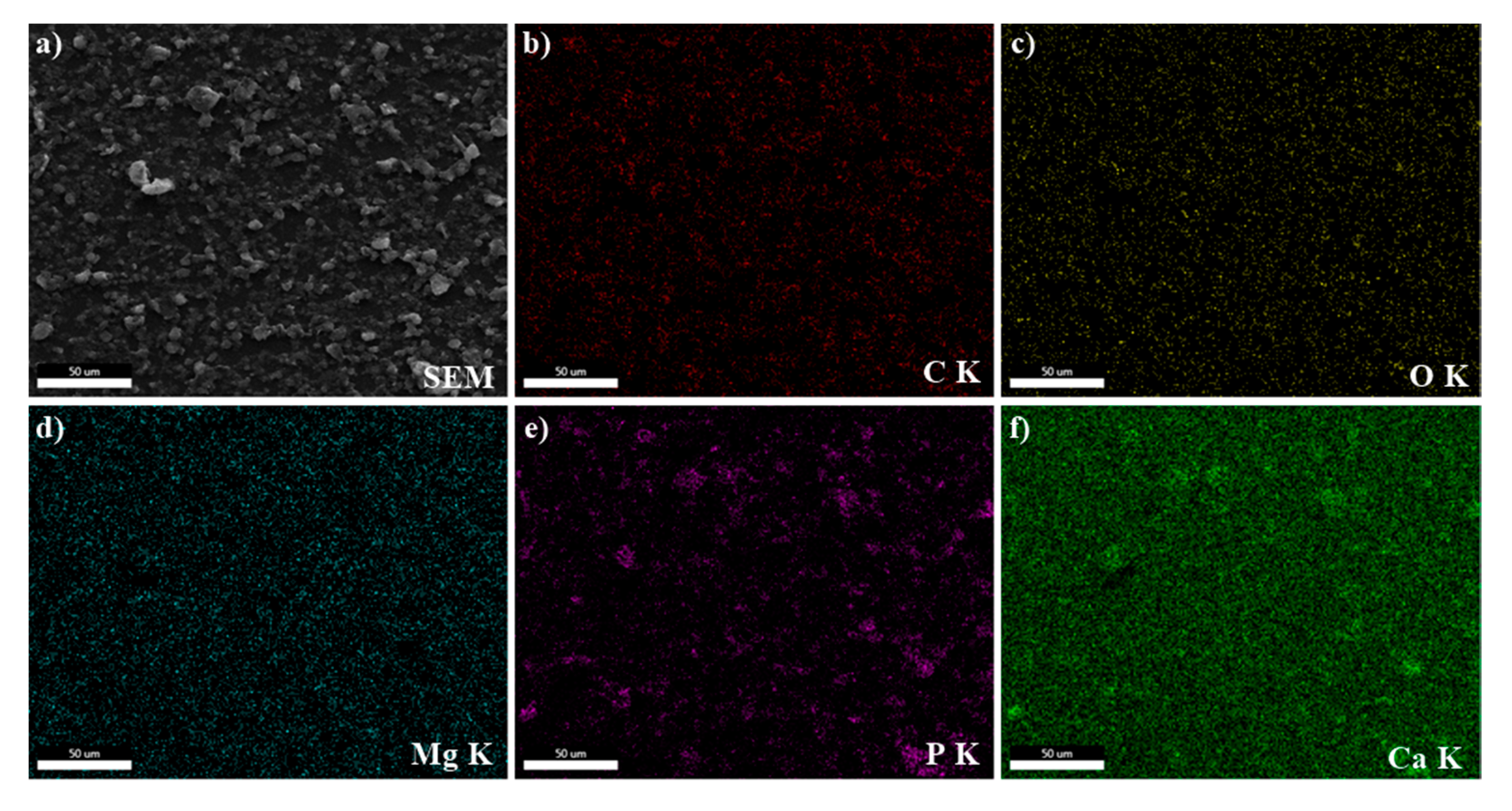
- The morphology of the 10MgHAp-Dex-thyme suspension particles and derived-coatings was explored by scanning electron microscopy (SEM) using a Hitachi S4500 equipment (Hitachi, Tokyo, Japan).
- (d)
- The qualitative (elemental distribution maps) and quantitative composition of samples were analyzed by energy-dispersive X-ray spectroscopy (EDS) with an EDAX (Ametek EDAX Inc., Mahwah, NJ, USA). The EDS quantitative analyses were performed on four randomly SEM selected (~250 × 250 µm2) surface regions. The EDS data were calibrated using a NIST 2910b hydroxyapatite standard reference material. The data were presented as mean ± standard deviation (SD).
- (e)
- The crystalline structure of the bioceramic powder and coating was investigated by X-ray diffraction (XRD). The powder was analyzed in symmetric geometry (θ–θ) using a Bruker D8 Advance diffractometer with CuKα (λ = 1.5418 Å) radiation (Bruker, Karlsruhe, Germany), equipped with a high-efficiency LynxEye™ 1D linear detector, while the film was measured in grazing incidence (GIXRD) geometry, with a Rigaku SmartLab 3 kW equipment (Rigaku, Tokyo, Japan), using CuKα radiation (λ = 1.5418 Å) and an incidence angle of 0.5°. The patterns were acquired in the 2θ range 9–60°, with a step size of 0.02°, and a dwell time of 5 s (for the powder) and 8.5 s (for the film).
- (f)
- The chemical structure and the presence of functional groups were assessed in the case of both synthesized biocomposite powder and coating by Fourier transform infra-red (FTIR) spectroscopy in attenuated total reflectance (ATR) mode, using a Perkin Elmer Spectrum BX II spectrometer (Perkin Elmer, Waltham, MA, USA) equipped with a Pike-MIRacle ATR head with diamond-ZnSe crystal plate, having a diameter of 1.8 mm (Pike Technologies, Madison, WI, USA). The spectra were acquired in the 500–4000 cm−1 spectral range, at a resolution of 4 cm−1, and represented the average of 32 individual scans.
- (g)
- The adhesion/cohesion strength of the 10MgHAp-Dex-thyme coating was tested by the pull-off method, complying with the ASTM D4541-17 “Standard test method for pull-off strength of coatings using portable adhesion testers” standard. A DFD® Instruments PAT MICRO AT101 dedicated machine (DFD® Instruments, Kristiansand, Norway) was employed. The testing procedure has been described in detail in [42]. The coating was cleanly detached from the surface. The adhesion strength was computed from the recorded failure value divided by the quantified detached surface area of the coatings. The average adherence value and SDs were calculated.
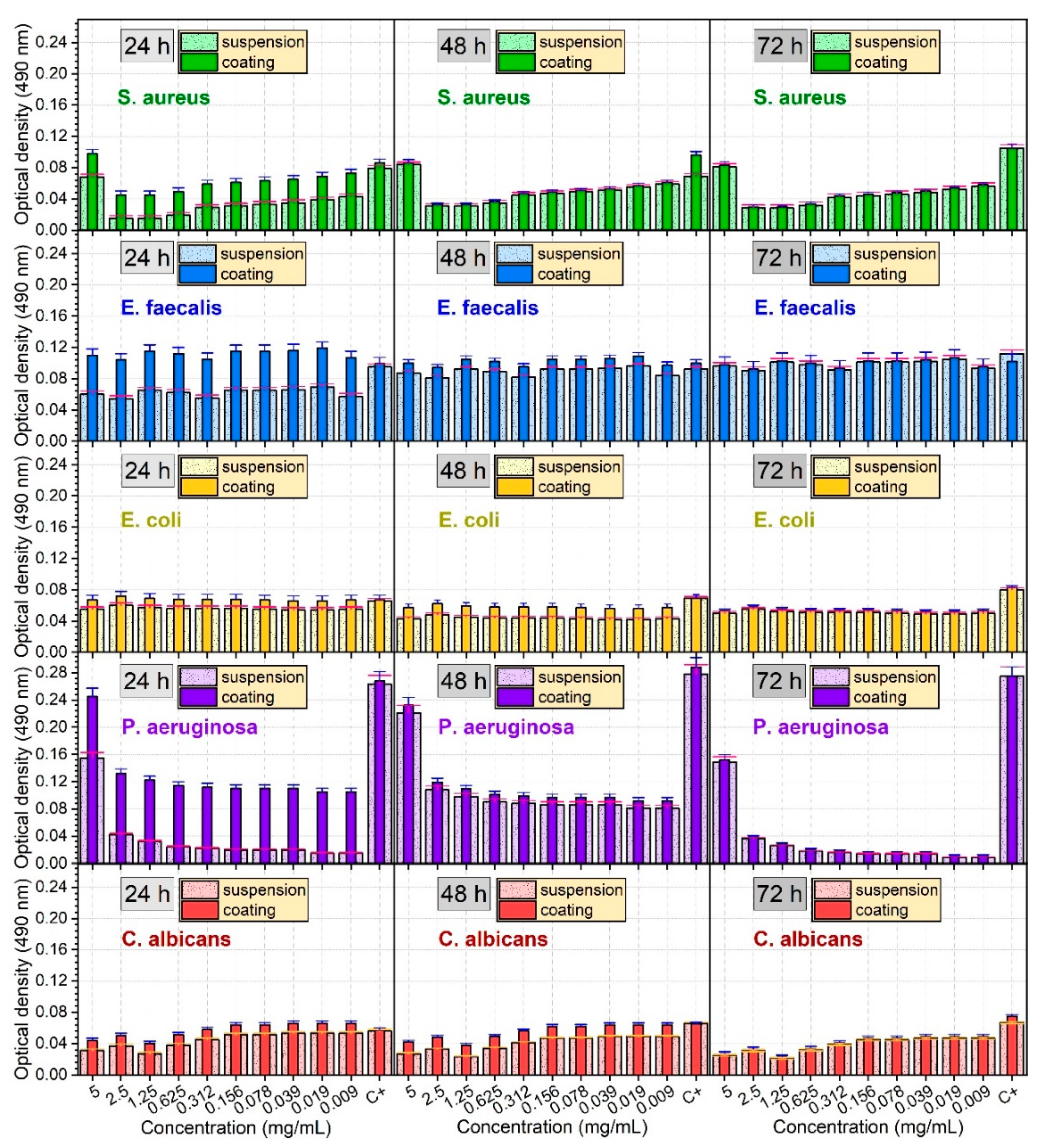
2.5. In Vitro Antimicrobial activity
3. Results and Discussion
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Tite, T.; Popa, A.-C.; Balescu, L.M.; Bogdan, I.M.; Pasuk, I.; Ferreira, J.M.F.; Stan, G.E. Cationic substitutions in hydroxyapatite: Current status of the derived biofunctional effects and their in vitro interrogation methods. Materials 2018, 11, 2081. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Graziani, G.; Boi, M.; Bianchi, M. A review on ionic substitutions in hydroxyapatite thin films: Towards complete biomimetism. Coatings 2018, 8, 269. [Google Scholar] [CrossRef] [Green Version]
- Duta, L.; Popescu, A.C. Current status on pulsed laser deposition of coatings from animal-origin calcium phosphate sources. Coatings 2019, 9, 335. [Google Scholar] [CrossRef] [Green Version]
- Stan, G.E.; Popescu, A.C.; Mihailescu, I.N.; Marcov, D.A.; Mustata, R.C.; Sima, L.E.; Petrescu, S.M.; Ianculescu, A.; Trusca, R.; Morosanu, C.O. On the bioactivity of adherent bioglass thin films synthesized by magnetron sputtering techniques. Thin Solid Films 2010, 518, 5955–5964. [Google Scholar] [CrossRef]
- Campana, V.; Milano, G.; Pagano, E.; Barba, M.; Cicione, C.; Salonna, G.; Lattanzi, W.; Logroscino, G. Bone substitutes in orthopaedic surgery: From basic science to clinical practice. J. Mater. Sci. Mater. Med. 2014, 25, 2445–2461. [Google Scholar] [CrossRef] [PubMed]
- LeGeros, R.Z. Hydroxyapatite and Related Materials; CRC Press: Boca Raton, FL, USA, 1994. [Google Scholar]
- LeGeros, R.Z. Calcium Phosphates in Oral Biology and Medicine; Karger: Basel, Switzerland, 1991. [Google Scholar]
- Ebrahimi, M.; Botelho, M.G.; Dorozhkin, S.V. Biphasic calcium phosphates bioceramics (HA/TCP): Concept, physicochemical properties and the impact of standardization of study protocols in biomaterials research. Mater. Sci. Eng. C 2018, 71, 1293–1312. [Google Scholar] [CrossRef]
- Zhou, H.; Lee, J. Nanoscale hydroxyapatite particles for bone tissue engineering. Acta Biomater. 2011, 7, 2769–2781. [Google Scholar] [CrossRef]
- Carrodeguas, R.G.; De Aza, S. α-Tricalcium phosphate: Synthesis, properties and biomedical applications. Acta Biomater. 2011, 7, 3536–3546. [Google Scholar] [CrossRef]
- Prakasam, M.; Locs, J.; Salma-Ancane, K.; Loca, D.; Largeteau, A.; Berzina-Cimdina, L. Fabrication, properties and applications of dense hydroxyapatite: A review. J. Funct. Biomater. 2015, 6, 1099–1140. [Google Scholar] [CrossRef] [Green Version]
- Joo, L.; Ong, D.; Chanm, C.N. Hydroxyapatite and their use as coatings in dental implants: A review. Crit. Rev. Biomed. Eng. 1999, 28, 667–707. [Google Scholar] [CrossRef]
- Marques, C.F.; Olhero, S.; Abrantes, J.C.C.; Marote, A.; Ferreira, S.; Vieira, S.I.; Ferreira, J.M.F. Biocompatibility and antimicrobial activity of biphasic calcium phosphate powders doped with metal ions for regenerative medicine. Ceram. Int. 2017, 43, 15719–15728. [Google Scholar] [CrossRef]
- Chung, R.-J.; Hsieh, M.-F.; Huang, C.-W.; Perng, L.-H.; Wen, H.-W.; Chin, T.-S. Antimicrobial effects and human gingival biocompatibility of hydroxyapatite sol-gel coatings. J. Biomed. Mater. Res. B 2006, 76, 169–178. [Google Scholar] [CrossRef] [PubMed]
- Johnson, C.T.; Garcia, A.J. Scaffold-based anti-infection strategies in bone repair. Ann. Biomed. Eng. 2015, 43, 515–528. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holloway, J.L. One step solution for fighting bacteria and growing bone. Sci. Transl. Med. 2019, 11, eaaw5326. [Google Scholar] [CrossRef]
- Yuan, K.; Chen, K.C.; Chan, Y.J.; Tsai, C.C.; Chen, H.H.; Shih, C.C. Dental implant failure associated with bacterial infection and long-term bisphosphonate usage: A case report. Implant Dent. 2012, 21, 3–7. [Google Scholar] [CrossRef]
- Popa, A.C.; Fernandes, H.R.; Necsulescu, M.; Luculescu, C.; Cioangher, M.; Dumitru, V.; Stuart, B.W.; Grant, D.M.; Ferreira, J.M.F.; Stan, G.E. Antibacterial efficiency of alkali-free bio-glasses incorporating ZnO and/or SrO as therapeutic agents. Ceram. Int. 2019, 45, 4368–4380. [Google Scholar] [CrossRef]
- Aslam, B.; Wang, W.; Arshad, M.I.; Khurshid, M.; Muzammil, S.; Rasool, M.H.; Nisar, M.A.; Alvi, R.F.; Aslam, M.A.; Qamar, M.U.; et al. Antibiotic resistance: A rundown of a global crisis. Infect. Drug Resist. 2018, 11, 1645–1658. [Google Scholar] [CrossRef] [Green Version]
- Badea, M.L.; Iconaru, S.L.; Groza, A.; Chifiriuc, M.C.; Beuran, M.; Predoi, D. Peppermint essential oil-doped hydroxyapatite nanoparticles with antimicrobial properties. Molecules 2019, 24, 2169. [Google Scholar] [CrossRef] [Green Version]
- Burt, S. Essential oils: Their antibacterial properties and potential applications in foods—A review. Int. J. Food. Microbiol. 2004, 94, 223–253. [Google Scholar] [CrossRef]
- Predoi, D.; Iconaru, S.L.; Buton, N.; Badea, M.L.; Marutescu, L. Antimicrobial activity of new materials based on lavender and basil essential oils and hydroxyapatite. Nanomaterials 2018, 8, 291. [Google Scholar] [CrossRef] [Green Version]
- de Carvalho, R.J.; de Souza, G.T.; Honorio, V.G.; de Sousa, J.S.; da Conceiçao, M.L.; Maganani, M.; de Souza, E.L. Comparative inhibitory effects of Thymus vulgaris L. essential oil against Staphylococcus aureus, Listeria monocytogenes and mesophilic starter co-culture in cheese-mimicking models. Food Microbiol. 2015, 52, 59–65. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bagamboula, C.F.; Uyttendaele, M.; Debevere, J. Antimicrobial effect of spices and herbs on Shigella sonnei and Shigella flexneri. J. Food Prot. 2003, 66, 668–673. [Google Scholar] [CrossRef] [PubMed]
- Food and Drug Administration. Part 182—Substances Generally Recognized a Safe. Subpart A—General Provisions. Sec. 182.10 Species and Other Natural Seasoning and Flavorings. Available online: https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/cfrsearch.cfm?fr=182.10 (accessed on 27 November 2019).
- Ballester-Costa, C.; Sendra, E.; Fernandez-Lopez, J.; Perez-Alvarez, J.A.; Viuda-Martos, M. Chemical composition and in vitro antibacterial properties of essential oils of four Thymus species from organic growth. Ind. Crop. Prod. 2013, 50, 304–311. [Google Scholar] [CrossRef]
- Kohiyama, C.Y.; Ribeiro, M.M.Y.; Mossini, S.A.G.; Bando, E.; Bomfim, N.S.; Nerilo, S.B.; Rocha, G.H.O.; Grespan, R.; Mikcha, J.M.G.; Machinski, M., Jr. Antifungal properties and inhibitory effects upon aflatoxin production of Thymus vulgaris L. by Aspergillus flavus Link. Food Chem. 2015, 173, 1006–1010. [Google Scholar] [CrossRef] [Green Version]
- Alioui, H.; Bouras, O.; Bollinger, J.C. Toward an efficient antibacterial agent: Zn- and Mg-doped hydroxyapatite nanopowders. J. Environ. Sci. Health Part A-Toxic/Hazard. Subst. Environ. Eng. 2018, 54, 315–327. [Google Scholar] [CrossRef] [PubMed]
- Coelho, C.C.; Araujo, R.; Quadros, P.A.; Sousa, S.R.; Monteiro, F.J. Antibacterial bone substitute of hydroxyapatite and magnesium oxide to prevent dental and orthopaedic infections. Mater. Sci. Eng. C 2019, 97, 529–538. [Google Scholar] [CrossRef]
- Predoi, D.; Iconaru, S.L.; Predoi, M.V.; Stan, G.E.; Buton, N. Synthesis, characterization, and antimicrobial activity of magnesium-doped hydroxyapatite suspensions. Nanomaterials 2019, 9, 1295. [Google Scholar] [CrossRef] [Green Version]
- Zhang, H.; Zhao, C.; Wen, J.; Li, X.; Fu, L. Synthesis and structural characteristics of magnesium and zinc doped hydroxyapatite whiskers. Ceram. Silik. 2017, 61, 244–249. [Google Scholar] [CrossRef] [Green Version]
- Landi, E.; Logroscino, G.; Proietti, L.; Tampieri, A.; Sandri, M.; Sprio, S. Biomimetic Mg-substituted hydroxyapatite: From synthesis to in vivo behaviour. J. Mater. Sci. Mater. Med. 2008, 19, 239–247. [Google Scholar] [CrossRef]
- Singh, J.; Singh, H.; Batra, U. Magnesium doped hydroxyapatite: Synthesis, characterization and bioactivity evaluation. In Biomaterials Science: Processing, Properties, and Applications V: Ceramic Transactions; Narayan, R., Bose, S., Bandyopadhyay, A., Eds.; Wiley: Hoboken, NJ, USA, 2015; Chapter 15; Volume 254, pp. 161–174. [Google Scholar]
- Bernardini, D.; Nasulewic, A.; Mazur, A.; Maier, J.A. Magnesium and microvascular endothelial cells: A role in inflammation and angiogenesis. Front. Biosci. 2005, 10, 1177–1182. [Google Scholar] [CrossRef] [Green Version]
- Xu, T.; He, X.; Chen, Z.; He, L.; Lu, M.; Ge, J.; Weng, J.; Mu, Y.; Duan, K. Effect of magnesium particle fraction on osteoinduction of hydroxyapatite sphere-based scaffolds. J. Mater. Chem. B 2019, 7, 5648–5660. [Google Scholar] [CrossRef] [PubMed]
- Bigi, A.; Falini, G.; Foresti, E.; Gazzano, M.; Ripamonti, A.; Roveri, N. Magnesium influence on hydroxyapatite crystallization. J. Inorg. Biochem. 1993, 49, 69–78. [Google Scholar] [CrossRef]
- Ciobanu, C.S.; Iconaru, S.L.; Massuyeau, F.; Constantin, L.V.; Costescu, A.; Predoi, D. Synthesis, structure, and luminescent properties of europium-doped hydroxyapatite nanocrystalline powders. J. Nanomater. 2012, 2012, 942801. [Google Scholar] [CrossRef] [Green Version]
- Predoi, D.; Iconaru, S.L.; Predoi, M.V. Dextran-coated zinc-doped hydroxyapatite for biomedical applications. Polymers 2019, 11, 886. [Google Scholar] [CrossRef] [Green Version]
- Predoi, D.; Iconaru, S.L.; Predoi, M.V.; Motelica-Heino, M.; Guegan, R.; Buton, N. Evaluation of antibacterial activity of zinc-doped hydroxyapatite colloids and dispersion stability using ultrasounds. Nanomaterials 2019, 9, 515. [Google Scholar] [CrossRef] [Green Version]
- Ciobanu, C.S.; Iconaru, S.L.; Popa, C.L.; Motelica-Heino, M.; Predoi, D. Evaluation of samarium doped hydroxyapatite, ceramics for medical application: Antimicrobial activity. J. Nanomater. 2015, 2015, 849216. [Google Scholar] [CrossRef] [Green Version]
- Rodriguez, L.; Matoušek, J. Preparation of TiO2 sol-gel layers on glass. Ceram. Silik. 2003, 47, 28–31. [Google Scholar]
- Popa, A.C.; Stan, G.E.; Husanu, M.A.; Pasuk, I.; Popescu, I.D.; Popescu, A.C.; Mihailescu, I.N. Multi-layer haemocompatible diamond-like carbon coatings obtained by combined radio frequency plasma enhanced chemical vapor deposition and magnetron sputtering. J. Mater. Sci.: Mater. Med. 2013, 24, 2695–2707. [Google Scholar] [CrossRef]
- Patel, V.R.; Agrawal, Y.K. Nanosuspension: An approach to enhance solubility of drugs. J. Adv. Pharm. Technol. Res. 2011, 2, 81–87. [Google Scholar] [CrossRef]
- Rietveld, H. A profile refinement method for nuclear and magnetic structures. J. Appl. Crystallogr. 1969, 2, 65–71. [Google Scholar] [CrossRef]
- Markovic, M.; Fowler, B.O.; Tung, M.S. Preparation and comprehensive characterization of a calcium hydroxyapatite reference material. J. Res. Natl. Inst. Stand. Technol. 2004, 109, 553–568. [Google Scholar] [CrossRef] [PubMed]
- Mocanu, A.C.; Miculescu, M.; Machedon-Pisu, T.; Maidaniuc, A.; Ciocoiu, R.C.; Ionita, M.; Pasuk, I.; Stan, G.E.; Miculescu, F. Internal and external surface features of newly developed porous ceramics with random interconnected 3D channels by a fibrous sacrificial porogen method. Appl. Surf. Sci. 2019, 489, 226–238. [Google Scholar] [CrossRef]
- Duta, L.; Mihailescu, N.; Popescu, A.C.; Luculescu, C.R.; Mihailescu, I.N.; Cetin, G.; Gunduz, O.; Oktar, F.N.; Popa, A.C.; Kuncser, A.; et al. Comparative physical, chemical and biological assessment of simple and titanium-doped ovine dentine-derived hydroxyapatite coatings fabricated by pulsed laser deposition. Appl. Surf. Sci. 2017, 413, 129–139. [Google Scholar] [CrossRef]
- Stan, G.E.; Marcov, D.A.; Pasuk, I.; Miculescu, F.; Pina, S.; Tulyaganov, D.U.; Ferreira, J.M.F. Bioactive glass thin films depositd by magnetron sputtering technique: The role of working pressure. Appl. Surf. Sci. 2010, 256, 7102–7110. [Google Scholar] [CrossRef]
- Can, H.K.; Kavlak, S.; Khosroshahi, S.P.; Guner, A. Preparation, characterization and dynamical properties of dextran-coated iron oxide nanoparticles (DIONPs). Artif. Cell. Nanomed. Biotechnol. 2018, 46, 421–431. [Google Scholar] [CrossRef] [Green Version]
- Vettori, M.H.P.B.; Franchetti, S.M.M.; Contiero, J. Structural characterization of a new dextran with a low degree of branching produced by Leuconostoc mesenteroides FT045B dextransucrase. Carbohydr. Polym. 2012, 88, 1440–1444. [Google Scholar] [CrossRef] [Green Version]
- Siddiqui, N.N.; Aman, A.; Silipo, A.; Qader, S.A.U.; Molinaro, A. Structural analysis and characterization of dextran produced by wild and mutant strains of Leuconostoc mesenteroides. Carbohydr. Polym. 2014, 99, 331–338. [Google Scholar] [CrossRef]
- Mitic, Z.; Nikolic, G.M.; Cakic, M.; Mitic, S.; Nikolic, G.S.; Najman, S. Spectroscopic characterization of cobalt (II) complexes with reduced low-molar dextran derivatives. Acta Fac. Med. Naiss. 2018, 35, 37–48. [Google Scholar] [CrossRef]
- Glisic, S.; Nikolic, G.; Cakic, M.; Trutic, N. Spectroscopic study of copper(II) complexes with carboxymethyl dextran and dextran sulfate. Russ. J. Phys. Chem. A 2015, 89, 1254–1262. [Google Scholar] [CrossRef]
- Topala, C.M.; Tataru, L.D. ATR-FTIR of thyme and rosemary oils extracted by supercritical carbon dioxide. Rev. Chem. 2016, 67, 842–846. [Google Scholar]
- Solan Valderrama, A.C.; Rojas De, G.C. Traceability of active compounds of essential oils in antimicrobial food packaging using a chemometric method by ATR-FTIR. Am. J. Anal. Chem. 2017, 8, 726–741. [Google Scholar] [CrossRef] [Green Version]
- Schultz, H.; Quilitzsch, R.; Kruger, H. Rapid evaluation and quantitative analysis of thyme, oregano and chamomile essential oils by ATR-IR and NIR spectroscopy. J. Mol. Struct. 2003, 661–662, 299–306. [Google Scholar] [CrossRef]
- Stan, G.E.; Marcov, D.A.; Popa, A.C.; Husanu, M.A. Polymer-like and diamond-like carbon coatings prepared by RF-PECVD for biomedical application. Dig. J. Nanomater. Biostruct. 2010, 5, 705–718. [Google Scholar]
- Ibrahim, A.I.O.; Moodley, D.S.; Petrik, L.; Patel, N. Use of antibacterial nanoparticles in Endodontics. S. Afr. Dent. J. 2017, 72, 105–112. [Google Scholar]
- Monzavi, A.; Eshraghi, S.; Hashemian, R.; Momen-Heravi, F. In vitro and ex vivo antimicrobial efficacy of nano-MgO in the elimination of endodontic pathogens. Clin. Oral Investig. 2015, 19, 349–356. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Li, D.-Q.; Lin, Y.-J.; Wei, M.; Evans, D.G.; Duan, X. Controllable preparation of nano-MgO and investigation of its bactericidal properties. J. Inorg. Biochem. 2005, 99, 986–993. [Google Scholar] [CrossRef]
- Hammer, K.A.; Carson, C.F.; Riley, T.V. Antimicrobial activity of essential oils and other plant extracts. J. Appl. Microbiol. 1999, 86, 985–990. [Google Scholar] [CrossRef] [Green Version]
- Msaada, K.; Salem, N.; Bachrouch, O.; Bousselmi, S.; Tammar, S.; Alfaify, A.; Al Sane, K.; Ben Ammar, W.; Azeiz, S.; Brahim, A.H.; et al. Chemical composition and antioxidant and antimicrobial activities of wormwood (Artemisia absinthium L.) essential oils and phenolics. J. Chem. 2015, 2017, 804658. [Google Scholar] [CrossRef] [Green Version]
- Boskovic, M.; Zdravkovic, N.; Ivanovic, J.; Janjic, J.; Djordjevic, J.; Starcevic, M.; Baltic, M.Z. Antimicrobial activity of thyme (Tymus vulgaris) and oregano (Origanum vulgare) essential oils against some food-borne microorganisms. Procedia Food Sci. 2015, 5, 18–21. [Google Scholar] [CrossRef] [Green Version]
- Poelstra, K.A.; Barekzi, N.A.; Rediske, A.M.; Felts, A.G.; Slunt, J.B.; Grainger, D.W. Prophylactic treatment of gram-positive and gram-negative abdominal implant infections using locally delivered polyclonal antibodies. J. Biomed. Mater. Res. 2002, 60, 206–215. [Google Scholar] [CrossRef]
- Seebach, E.; Kubatzky, K.F. Chronic implant-related bone infections—Can immune modulation be a therapeutic strategy? Front. Immunol. 2019, 10, 1724. [Google Scholar] [CrossRef] [Green Version]
- Zimmerli, W.; Sendi, P. Orthopaedic biofilm infections. APMIS 2017, 125, 353–364. [Google Scholar] [CrossRef] [Green Version]
- Zimmerli, W.; Trampuz, A.; Ochsner, P.E. Prosthetic-joint infections. N. Engl. J. Med. 2004, 351, 1645–1654. [Google Scholar] [CrossRef] [Green Version]
- Pan, C.; Zhou, Z.; Yu, X. Coatings as the useful drug delivery system for the prevention of implant-related infections. J. Orthop. Surg. Res. 2018, 13, 220. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Akiyama, T.; Miyamoto, H.; Yonekura, Y.; Tsukamoto, M.; Ando, Y.; Noda, I.; Sonohata, M.; Mawatari, M. Silver oxide containing hydroxyapatite coating has in vivo antibacterial activity in the rat tibia. J. Orthop. Surg. Res. 2013, 31, 1195–1200. [Google Scholar] [CrossRef] [PubMed]
- Ueno, M.; Miyamoto, H.; Tsukamoto, M.; Eto, S.; Noda, I.; Shobuike, T.; Kobatake, T.; Sonohata, M.; Mawatari, M. Silver-containing hydroxyapatite coating reduces biofilm formation by methicillin-resistant Staphylococcus aureus in vitro and in vivo. Biomed. Res. Int. 2016, 2016, 8070597. [Google Scholar] [CrossRef] [Green Version]
- Lian, X.; Mao, K.; Liu, X.; Wang, X.; Cui, F. In vivo osteogenesis of vancomycin loaded nanohydroxyapatite/collagen/calcium sulfate composite for treating infectious bone defect induced by chronic osteomyelitis. J. Nanomater. 2015, 2015, 261492. [Google Scholar] [CrossRef] [Green Version]
- Townsend, L.; Williams, R.L.; Anuforom, O.; Berwick, M.R.; Halstead, F.; Hughes, E.; Stamboulis, A.; Oppenheim, B.; Gough, J.; Grover, L.; et al. Antimicrobial peptide coatings for hydroxyapatite: Electrostatic and covalent attachment of antimicrobial peptides to surfaces. J. R. Soc. Interface 2017, 14, 20160657. [Google Scholar] [CrossRef] [Green Version]







| SAMPLE TYPE | a-lattice Constant (Å) | c-lattice Constant (Å) | Average Crystallite Size (Å) |
|---|---|---|---|
| 10MgHAp powder | 9.549 ± 0.06 | 6.796 ± 0.03 | ~36 |
| 10MgHAp-Dex-thyme powder | 9.551 ± 0.05 | 6.848 ± 0.03 | ~32 |
| 10MgHAp-Dex-thyme coating | n/a | n/a | n/a |
| SAMPLE TYPE | IR BAND ASSIGNMENT | ||||
|---|---|---|---|---|---|
| 10MgHAp Powder | Dextran Powder | Thyme Oil | 10MgHAp-Dex-thyme Powder | 10MgHAp-Dex-thyme Coating | |
| 558 | – | – | 558 | 558 | asymmetric bending (ν4) vibrations of (PO4)3− groups in HA [30,45,46,47,48] |
| 559 | – | – | 599 | 600 | asymmetric bending (ν4) vibrations of (PO4)3− groups in HA [30,45,46,47,48] |
| 630 | – | – | 630 | 630 | libration vibrations of (OH)− structural groups in HA [30,45,46,47,48] |
| – | 761 | – | 763 | 760 | vibrations of α-(1,3) linkages of glycoside units [49,50,51,52,53] |
| – | – | 812 | 818 | – | out-of-plane wagging vibrations of C–H in thymol units [54,55,56] |
| – | 845 | – | – | – | vibrations of α-(1,3) linkages of glycoside units [49,50,51,52] |
| 873 | – | – | 873 | 872 | symmetric stretching (ν2) vibrations of (CO3)2− groups [45,46] |
| – | 916 | – | – | 918 | vibrations of α-(1,3) linkages of glycoside units [49,50,51,52] |
| 950 | – | – | 950 | 951 | symmetric stretching (ν1) vibrations of (PO4)3− groups in HA [30,45,46] |
| – | 1002 | – | – | – | vibrations of α-(1,6) linkages of glycoside units [49,50,51,52] |
| 1013 | – | – | 1013 | 1004 | asymmetric stretching (ν3) vibrations of (PO4)3− groups in HA [30,45,46,47,48] |
| – | 1077 | – | – | 1075 | stretching (ν) vibrations of C–O–C covalent bonds and glycosidic bridges [49,50,51,52] |
| 1097 | – | – | 1097 | 1099 | asymmetric stretching (ν3) of (PO4)3− groups in HA [30,45,46,47,48] |
| – | 1104 | – | – | – | stretching (ν) vibrations of C–O–C covalent bonds and glycosidic bridges [49,50,51,52] |
| – | 1150 | – | 1167 | 1150 | stretching (ν) vibrations of C–O–C covalent bonds and glycosidic bridges [49,50,51,52] |
| – | 1208 | – | 1206 | 1209 | stretching (ν) vibrations of C–O–C covalent bonds and glycosidic bridges [49,50,51,52] |
| – | – | 1252 | 1244 | 1243 | stretching (ν) vibrations of C–O [54,55,56] |
| – | 1277 | – | 1280 | 1275 | bending (δ) vibrations of C–OH [53] |
| – | 1346 | – | 1350 | 1348 | bending (δ) vibration of C–H [52] |
| – | – | 1421 | – | – | stretching (ν) vibrations of C–C [54,55,56] |
| 1424 | – | – | – | 1418 | asymmetric stretching (ν3) vibrations of (CO3)2− groups [30,45,46] |
| – | 1426 | – | 1424 | – | bending (δ) vibrations of O–H [52] |
| – | – | 1459 | – | – | bending (δ) vibrations of C–H [52] |
| 1478 | – | – | 1478 | 1456 | asymmetric stretching (ν3) of (CO3)2− groups [30,45,46] |
| – | – | 1522 | – | – | wagging vibrations of C–H in CH3 units [53,54,55,56] |
| – | – | 1590 | – | – | aromatic vibration domain and bending vibrations of C–H [53,54,55,56] |
| – | – | 1630 | – | – | stretching (ν) vibrations of C–H and bending (δ) vibrations of adsorbed H2O molecules [53,54,55,56] |
| 1640 | – | – | 1640 | 1636 | bending (δ) vibrations of adsorbed H2O molecules [30,45,48] |
| – | 1644 | – | – | – | bending (δ) vibrations of bound water molecules [50] |
| – | 2888 | – | – | 2889 | symmetric stretching (ν) vibrations of C–H bonds [50,52,57] |
| – | 2926 | – | 2934 | 2920 | asymmetric stretching (ν) vibrations of C–H bonds [50,52,57] |
| – | – | 2959 | 2973 | 2979 | asymmetric stretching (ν) vibrations of C–H bonds [50,52,54,55,56,57] |
| 2700–3700 | 2700–3700 | 2700–3700 | 2700–3700 | 2700–3700 | stretching (ν) vibrations of adsorbed H2O molecules on the surface of HAp, (OH)− of polysaccharide [30,45,46,47,48] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iconaru, S.L.; Predoi, M.V.; Motelica-Heino, M.; Predoi, D.; Buton, N.; Megier, C.; Stan, G.E. Dextran-Thyme Magnesium-Doped Hydroxyapatite Composite Antimicrobial Coatings. Coatings 2020, 10, 57. https://doi.org/10.3390/coatings10010057
Iconaru SL, Predoi MV, Motelica-Heino M, Predoi D, Buton N, Megier C, Stan GE. Dextran-Thyme Magnesium-Doped Hydroxyapatite Composite Antimicrobial Coatings. Coatings. 2020; 10(1):57. https://doi.org/10.3390/coatings10010057
Chicago/Turabian StyleIconaru, Simona Liliana, Mihai Valentin Predoi, Mikael Motelica-Heino, Daniela Predoi, Nicolas Buton, Christelle Megier, and George E. Stan. 2020. "Dextran-Thyme Magnesium-Doped Hydroxyapatite Composite Antimicrobial Coatings" Coatings 10, no. 1: 57. https://doi.org/10.3390/coatings10010057
APA StyleIconaru, S. L., Predoi, M. V., Motelica-Heino, M., Predoi, D., Buton, N., Megier, C., & Stan, G. E. (2020). Dextran-Thyme Magnesium-Doped Hydroxyapatite Composite Antimicrobial Coatings. Coatings, 10(1), 57. https://doi.org/10.3390/coatings10010057







