Effect of Serial Passage on the Pathogenicity and Immunogenicity of Vaccinia Virus LC16m8 Strain
Abstract
Simple Summary
Abstract
1. Introduction
2. Safety of VACV Vaccine through the LC16m8 Phenotype
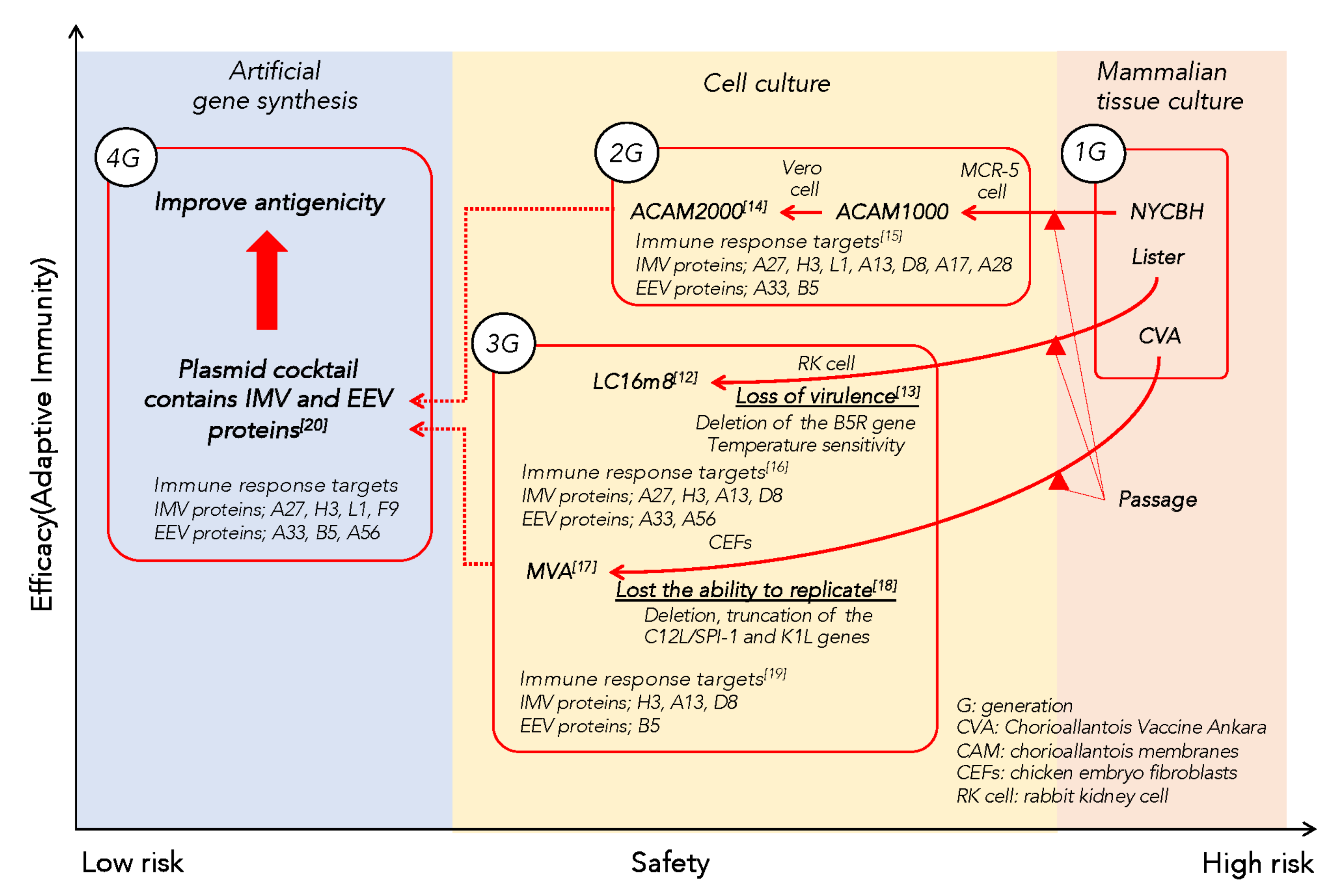
2.1. Development of the Attenuated VACV Strain LC16m8
2.2. Functions of B5 Protein and Extracellular Enveloped Virion, and Adverse Events of the Vaccine
2.3. Genotype-Phenotype Factors Related to Adverse Events after Vaccination
3. Efficacy of VACV Vaccine through a Personalized Public Health Focus
3.1. Immune Protection against VACV by Antibodies
3.2. Antibody Profile Induced by LC16m8
3.3. Genotype-Phenotype Status Related to Antibody Production in Response to VACV Vaccine
4. Future Research Directions
4.1. Vectors for Infectious and Non-Infectious Diseases
4.2. Development of Next-Generation Vaccines Based on Interindividual Differences
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wooden, S.L.; Koff, W.C. The Human Vaccines Project: Towards a comprehensive understanding of the human immune response to immunization. Hum. Vaccines Immunother. 2018, 14, 2214–2216. [Google Scholar] [CrossRef] [PubMed]
- Poland, A.G.; Ovsyannikova, I.G.; Jacobson, R.M.; Smith, I.D. Heterogeneity in Vaccine Immune Response: The Role of Immunogenetics and the Emerging Field of Vaccinomics. Clin. Pharmacol. Ther. 2007, 82, 653–664. [Google Scholar] [CrossRef]
- Minor, P.D. Live attenuated vaccines: Historical successes and current challenges. Virology 2015, 479–480, 379–392. [Google Scholar] [CrossRef] [PubMed]
- Hashizme, S.; Yoshizawa, H.; Morita, M.; Suzuki, K. Properties of Attenuated Mutant of Vaccinia Virus; LC16m8; Derived from Lister Strain. In Vaccinia Viruses as Vectors for Vaccine Antigens; Quinnan, G.V., Ed.; Elsevier Science Publishing Co. Inc.: New York, NY, USA, 1985; pp. 87–99. [Google Scholar]
- Kenner, J.; Cameron, F.; Empig, C.; Jobes, D.V.; Gurwith, M. LC16m8: An attenuated smallpox vaccine. Vaccine 2006, 24, 7009–7022. [Google Scholar] [CrossRef]
- Takahashi-Nishimaki, F.; Suzuki, K.; Morita, M.; Maruyama, T.; Miki, K.; Hashizume, S.; Sugimoto, M. Genetic Analysis of Vaccinia Virus Lister Strain and its Attenuated Mutant LC16m8: Production of Intermediate Variants by Homologous Recombination. J. Gen. Virol. 1987, 68, 2705–2710. [Google Scholar] [CrossRef] [PubMed]
- Takahashi-Nishimaki, F.; Funahashi, S.-I.; Miki, K.; Hashizume, S.; Sugimoto, M. Regulation of plaque size and host range by a vaccinia virus gene related to complement system proteins. Virology 1991, 181, 158–164. [Google Scholar] [CrossRef]
- Fenner, F.; Henderson, D.A.; Arita, I.; Jezek, Z.; Ladnyi, I.D. Smallpox and Its Eradication; World Health Organization: Geneva, Switzerland, 1988; Available online: https://apps.who.int/iris/handle/10665/39485 (accessed on 14 September 2021).
- Isaacs, S.N.; Wolffe, E.J.; Payne, L.G.; Moss, B. Characterization of a vaccinia virus-encoded 42-kilodalton class I membrane glycoprotein component of the extracellular virus envelope. J. Virol. 1992, 66, 7217–7224. [Google Scholar] [CrossRef]
- Engelstad, M.; Howard, S.; Smith, G.L. A constitutively expressed vaccinia gene encodes a 42-kDa glycoprotein related to complement control factors that forms part of the extracellular virus envelope. Virology 1992, 188, 801–810. [Google Scholar] [CrossRef]
- Morikawa, S.; Sakiyama, T.; Hasegawa, H.; Saijo, M.; Maeda, A.; Kurane, I.; Maeno, G.; Kimura, J.; Hirama, C.; Yoshida, T.; et al. An Attenuated LC16m8 Smallpox Vaccine: Analysis of Full-Genome Sequence and Induction of Immune Protection. J. Virol. 2005, 79, 11873–11891. [Google Scholar] [CrossRef]
- Eto, A.; Saito, T.; Yokote, H.; Kurane, I.; Kanatani, Y. Recent advances in the study of live attenuated cell-cultured smallpox vaccine LC16m8. Vaccine 2015, 33, 6106–6111. [Google Scholar] [CrossRef]
- Kidokoro, M.; Tashiro, M.; Shida, H. Genetically stable and fully effective smallpox vaccine strain constructed from highly attenuated vaccinia LC16m8. Proc. Natl. Acad. Sci. USA 2005, 102, 4152–4157. [Google Scholar] [CrossRef]
- Nalca, A.; Zumbrun, E. ACAM2000™: The new smallpox vaccine for United States Strategic National Stockpile. Drug Des. Dev. Ther. 2010, 4, 71–79. [Google Scholar] [CrossRef]
- Townsend, M.B.; Keckler, M.S.; Patel, N.; Davies, D.H.; Felgner, P.; Damon, I.K.; Karem, K.L.; King, D.F.L.; Siddiqui, A.A.; Buffa, V.; et al. Humoral Immunity to Smallpox Vaccines and Monkeypox Virus Challenge: Proteomic Assessment and Clinical Correlations. J. Virol. 2013, 87, 900–911. [Google Scholar] [CrossRef]
- Eto, A.; Fujita, M.; Nishiyama, Y.; Saito, T.; Molina, U.M.; Morikawa, S.; Saijo, M.; Shinmura, Y.; Kanatani, Y. Profiling of the antibody response to attenuated LC16m8 smallpox vaccine using protein array analysis. Vaccine 2019, 37, 6588–6593. [Google Scholar] [CrossRef]
- Volz, A.; Sutter, G. Modified Vaccinia Virus Ankara: History, value in basic research and current perspectives for vaccine development. Adv. Virus Res. 2016, 97, 187–243. [Google Scholar] [CrossRef] [PubMed]
- Liu, R.; Mendez-Rios, J.D.; Peng, C.; Xiao, W.; Weisberg, A.S.; Wyatt, L.S.; Moss, B. SPI-1 is a missing host-range factor required for replication of the attenuated modified vaccinia Ankara (MVA) vaccine vector in human cells. PLoS Pathog. 2019, 15, e1007710. [Google Scholar] [CrossRef]
- Davies, D.H.; Wyatt, L.S.; Newman, F.K.; Earl, P.L.; Chun, S.; Hernandez, J.E.; Molina, D.M.; Hirst, S.; Moss, B.; Frey, S.E.; et al. Antibody Profiling by Proteome Microarray Reveals the Immunogenicity of the Attenuated Smallpox Vaccine Modified Vaccinia Virus Ankara Is Comparable to That of Dryvax. J. Virol. 2008, 82, 652–663. [Google Scholar] [CrossRef] [PubMed]
- Hirao, L.A.; Draghia-Akli, R.; Prigge, J.T.; Yang, M.; Satishchandran, A.; Wu, L.; Hammarlund, E.; Khan, A.S.; Babas, T.; Rhodes, L.; et al. Multivalent Smallpox DNA Vaccine Delivered by Intradermal Electroporation Drives Protective Immunity in Nonhuman Primates Against Lethal Monkeypox Challenge. J. Infect. Dis. 2011, 203, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Payne, L.G. Significance of Extracellular Enveloped Virus in the in vitro and in vivo Dissemination of Vaccinia. J. Gen. Virol. 1980, 50, 89–100. [Google Scholar] [CrossRef]
- Smith, G.L.; Vanderplasschen, A.; Law, M. The formation and function of extracellular enveloped vaccinia virus. J. Gen. Virol. 2002, 83, 2915–2931. [Google Scholar] [CrossRef]
- Roberts, K.L.; Smith, G.L. Vaccinia virus morphogenesis and dissemination. Trends Microbiol. 2008, 16, 472–479. [Google Scholar] [CrossRef] [PubMed]
- Doceul, V.; Hollinshead, M.; van der Linden, L.; Smith, G.L. Repulsion of Superinfecting Virions: A Mechanism for Rapid Virus Spread. Science 2010, 327, 873–876. [Google Scholar] [CrossRef] [PubMed]
- Garcel, A.; Fauquette, W.; Dehouck, M.-P.; Crance, J.-M.; Favier, A.-L. Vaccinia virus-induced smallpox postvaccinal encephalitis in case of blood–brain barrier damage. Vaccine 2012, 30, 1397–1405. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Rubin, A.S.; Taffs, E.R.; Merchlinsky, M.; Ye, Z.; Carbone, K.M. Mouse neurotoxicity test for vaccinia-based smallpox vaccines. Vaccine 2004, 22, 1486–1493. [Google Scholar] [CrossRef]
- Kitamura, T. Effort to improve smallpox vaccine. Rinsho to Uirusu. Clin. Virus. 1996, 24, 41–47. [Google Scholar]
- Sirven, P.; Castelli, F.A.; Probst, A.; Szely, N.; Maillere, B. In vitro human CD4+ T cell response to the vaccinia protective antigens B5R and A33R. Mol. Immunol. 2009, 46, 1481–1487. [Google Scholar] [CrossRef]
- Tang, J.; Murtadha, M.; Schnell, M.; Eisenlohr, L.C.; Hooper, J.; Flomenberg, P. Human T-Cell Responses to Vaccinia Virus Envelope Proteins. J. Virol. 2006, 80, 10010–10020. [Google Scholar] [CrossRef]
- Aldaz-Carroll, L.; Whitbeck, J.C.; de Leon, M.P.; Lou, H.; Hirao, L.; Isaacs, S.N.; Moss, B.; Eisenberg, R.J.; Cohen, G.H. Epitope-Mapping Studies Define Two Major Neutralization Sites on the Vaccinia Virus Extracellular Enveloped Virus Glycoprotein B5R. J. Virol. 2005, 79, 6260–6271. [Google Scholar] [CrossRef]
- Immune Epitope Database and Analysis Resource. IEDB Website. Available online: https://www.iedb.org (accessed on 14 September 2021).
- Vita, R.; Mahajan, S.; Overton, A.J.; Dhanda, S.K.; Martini, S.; Cantrell, J.R.; Wheeler, D.K.; Sette, A.; Peters, B. The Immune Epitope Database (IEDB): 2018 update. Nucl. Acids Res. 2018, 47, D339–D343. [Google Scholar] [CrossRef]
- Yokote, H.; Shinmura, Y.; Kanehara, T.; Maruno, S.; Kuranaga, M.; Matsui, H.; Hashizume, S. Vaccinia virus strain LC16m8 defective in the B5R gene keeps strong protection comparable to its parental strain Lister in immunodeficient mice. Vaccine 2015, 33, 6112–6119. [Google Scholar] [CrossRef]
- Kennedy, J.S.; Gurwith, M.; Dekker, C.L.; Frey, S.E.; Edwards, K.M.; Kenner, J.; Lock, M.; Empig, C.; Morikawa, S.; Saijo, M.; et al. Safety and Immunogenicity of LC16m8, an Attenuated Smallpox Vaccine in Vaccinia-Naive Adults. J. Infect. Dis. 2011, 204, 1395–1402. [Google Scholar] [CrossRef]
- Nishiyama, Y.; Fujii, T.; Kanatani, Y.; Shinmura, Y.; Yokote, H.; Hashizume, S. Freeze-dried live attenuated smallpox vaccine prepared in cell culture “LC16-KAKETSUKEN”: Post-marketing surveillance study on safety and efficacy compliant with Good Clinical Practice. Vaccine 2015, 33, 6120–6127. [Google Scholar] [CrossRef]
- Rock, M.T.; Yoder, S.M.; Talbot, T.R.; Edwards, K.M.; Crowe, J.E. Adverse Events after Smallpox Immunizations Are Associated with Alterations in Systemic Cytokine Levels. J. Infect. Dis. 2004, 189, 1401–1410. [Google Scholar] [CrossRef]
- Tian, T.; Jin, M.Q.; Dubin, K.; King, S.L.; Hoetzenecker, W.; Murphy, G.F.; Chen, C.A.; Kupper, T.S.; Fuhlbrigge, R.C. IL-1R Type 1–Deficient Mice Demonstrate an Impaired Host Immune Response against Cutaneous Vaccinia Virus Infection. J. Immunol. 2017, 198, 4341–4351. [Google Scholar] [CrossRef]
- Ovsyannikova, I.G.; Haralambieva, I.H.; Kennedy, R.B.; Pankratz, V.S.; Vierkant, R.A.; Jacobson, R.M.; Poland, G.A. Impact of cytokine and cytokine receptor gene polymorphisms on cellular immunity after smallpox vaccination. Gene 2012, 510, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, R.B.; Ovsyannikova, I.G.; Pankratz, V.S.; Haralambieva, I.H.; Vierkant, R.; Poland, G.A. Genome-wide analysis of polymorphisms associated with cytokine responses in smallpox vaccine recipients. Qual. Life Res. 2012, 131, 1403–1421. [Google Scholar] [CrossRef] [PubMed]
- Stanley, J.S.L.; Frey, S.E.; Taillon-Miller, P.; Guo, J.; Miller, R.D.; Koboldt, D.C.; Elashoff, M.; Christensen, R.; Saccone, N.L.; Belshe, R.B. The Immunogenetics of Smallpox Vaccination. J. Infect. Dis. 2007, 196, 212–219. [Google Scholar] [CrossRef] [PubMed]
- Reif, D.M.; McKinney, B.A.; Motsinger, A.A.; Chanock, S.J.; Edwards, K.M.; Rock, M.T.; Moore, J.H.; Crowe, J.J.E. Genetic Basis for Adverse Events after Smallpox Vaccination. J. Infect. Dis. 2008, 198, 16–22. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Reif, D.M.; Motsinger-Reif, A.A.; McKinney, B.A.; Rock, M.T.; Crowe, J.E.; Moore, J.H. Integrated analysis of genetic and proteomic data identifies biomarkers associated with adverse events following smallpox vaccination. Genes Immun. 2008, 10, 112–119. [Google Scholar] [CrossRef]
- Moss, B. Smallpox vaccines: Targets of protective immunity. Immunol. Rev. 2010, 239, 8–26. [Google Scholar] [CrossRef] [PubMed]
- Jones-Trower, A.; Garcia, A.; Meseda, C.A.; He, Y.; Weiss, C.; Kumar, A.; Weir, J.P.; Merchlinsky, M. Identification and preliminary characterization of vaccinia virus (Dryvax) antigens recognized by vaccinia immune globulin. Virology 2005, 343, 128–140. [Google Scholar] [CrossRef]
- Gilchuk, I.; Gilchuk, P.; Sapparapu, G.; Lampley, R.; Singh, V.; Kose, N.; Blum, D.L.; Hughes, L.J.; Satheshkumar, P.S.; Townsend, M.B.; et al. Cross-Neutralizing and Protective Human Antibody Specificities to Poxvirus Infections. Cell 2016, 167, 684–694.e9. [Google Scholar] [CrossRef]
- Galmiche, M.C.; Goenaga, J.; Wittek, R.; Rindisbacher, L. Neutralizing and Protective Antibodies Directed against Vaccinia Virus Envelope Antigens. Virology 1999, 254, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Davies, D.H.; Liang, X.; Hernandez, J.E.; Randall, A.; Hirst, S.; Mu, Y.; Romero, K.M.; Nguyen, T.T.; Kalantari-Dehaghi, M.; Crotty, S.; et al. Profiling the humoral immune response to infection by using proteome microarrays: High-throughput vaccine and diagnostic antigen discovery. Proc. Natl. Acad. Sci. USA 2005, 102, 547–552. [Google Scholar] [CrossRef] [PubMed]
- Davies, D.H.; Molina, D.M.; Wrammert, J.; Miller, J.; Hirst, S.; Mu, Y.; Pablo, J.; Unal, B.; Nakajima-Sasaki, R.; Liang, X.; et al. Proteome-wide analysis of the serological response to vaccinia and smallpox. Proteomics 2007, 7, 1678–1686. [Google Scholar] [CrossRef]
- Davies, D.H.; McCausland, M.M.; Valdez, C.; Huynh, D.; Hernandez, J.E.; Mu, Y.; Hirst, S.; Villarreal, L.; Felgner, P.L.; Crotty, S. Vaccinia Virus H3L Envelope Protein Is a Major Target of Neutralizing Antibodies in Humans and Elicits Protection against Lethal Challenge in Mice. J. Virol. 2005, 79, 11724–11733. [Google Scholar] [CrossRef] [PubMed]
- Benhnia, M.R.-E.; McCausland, M.M.; Su, H.-P.; Singh, K.; Hoffmann, J.; Davies, D.H.; Felgner, P.L.; Head, S.; Sette, A.; Garboczi, D.N.; et al. Redundancy and Plasticity of Neutralizing Antibody Responses Are Cornerstone Attributes of the Human Immune Response to the Smallpox Vaccine. J. Virol. 2008, 82, 3751–3768. [Google Scholar] [CrossRef] [PubMed]
- Schmid, K.; Keasey, S.L.; Pittman, P.; Emerson, G.L.; Meegan, J.; Tikhonov, A.P.; Chen, G.; Schweitzer, B.; Ulrich, R.G. Analysis of the human immune response to vaccinia by use of a novel protein microarray suggests that antibodies recognize less than 10% of the total viral proteome. Proteom.-Clin. Appl. 2008, 2, 1528–1538. [Google Scholar] [CrossRef]
- Duke-Cohan, J.S.; Wollenick, K.; Witten, E.A.; Seaman, M.S.; Baden, L.R.; Dolin, R.; Reinherz, E.L. The heterogeneity of human antibody responses to vaccinia virus revealed through use of focused protein arrays. Vaccine 2009, 27, 1154–1165. [Google Scholar] [CrossRef]
- Keasey, S.; Pugh, C.; Tikhonov, A.; Chen, G.; Schweitzer, B.; Nalca, A.; Ulrich, R.G. Proteomic Basis of the Antibody Response to Monkeypox Virus Infection Examined in Cynomolgus Macaques and a Comparison to Human Smallpox Vaccination. PLoS ONE 2010, 5, e15547. [Google Scholar] [CrossRef]
- Hermanson, G.; Chun, S.; Felgner, J.; Tan, X.; Pablo, J.; Nakajima-Sasaki, R.; Molina, D.M.; Felgner, P.L.; Liang, X.; Davies, D.H. Measurement of antibody responses to Modified Vaccinia virus Ankara (MVA) and Dryvax® using proteome microarrays and development of recombinant protein ELISAs. Vaccine 2012, 30, 614–625. [Google Scholar] [CrossRef]
- Tan, X.; Chun, S.; Pablo, J.; Felgner, P.; Liang, X.; Davies, D.H. Failure of the Smallpox Vaccine To Develop a Skin Lesion in Vaccinia Virus-Naïve Individuals Is Related to Differences in Antibody Profiles before Vaccination, Not After. Clin. Vaccine Immunol. 2012, 19, 418–428. [Google Scholar] [CrossRef]
- Pugh, C.; Keasey, S.; Korman, L.; Pittman, P.; Ulrich, R.G. Human Antibody Responses to the Polyclonal Dryvax Vaccine for Smallpox Prevention Can Be Distinguished from Responses to the Monoclonal Replacement Vaccine ACAM2000. Clin. Vaccine Immunol. 2014, 21, 877–885. [Google Scholar] [CrossRef]
- Saito, T.; Fujii, T.; Kanatani, Y.; Saijo, M.; Morikawa, S.; Yokote, H.; Takeuchi, T.; Kuwabara, N. Clinical and Immunological Response to Attenuated Tissue-Cultured Smallpox Vaccine LC16m8. JAMA 2009, 301, 1025–1033. [Google Scholar] [CrossRef]
- Johnson, B.; Kanatani, Y.; Fujii, T.; Saito, T.; Yokote, H.; Smith, G.L. Serological responses in humans to the smallpox vaccine LC16m8. J. Gen. Virol. 2011, 92, 2405–2410. [Google Scholar] [CrossRef] [PubMed]
- Ovsyannikova, I.G.; Pankratz, V.S.; Salk, H.M.; Kennedy, R.B.; Poland, G.A. HLA alleles associated with the adaptive immune response to smallpox vaccine: A replication study. Qual. Life Res. 2014, 133, 1083–1092. [Google Scholar] [CrossRef]
- Haralambieva, I.H.; Ovsyannikova, I.G.; Dhiman, N.; Kennedy, R.B.; O’Byrne, M.; Pankratz, V.S.; Jacobson, R.M.; Poland, G.A. Common SNPs/Haplotypes in IL18R1 and IL18 Genes Are Associated With Variations in Humoral Immunity to Smallpox Vaccination in Caucasians and African Americans. J. Infect. Dis. 2011, 204, 433–441. [Google Scholar] [CrossRef]
- Ovsyannikova, I.G.; Kennedy, R.B.; O’Byrne, M.; Jacobson, R.M.; Pankratz, V.S.; Poland, G.A. Genome-wide association study of antibody response to smallpox vaccine. Vaccine 2012, 30, 4182–4189. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, R.B.; Ovsyannikova, I.G.; Pankratz, V.S.; Vierkant, R.; Jacobson, R.; Ryan, M.A.; Poland, G.A. Gender effects on humoral immune responses to smallpox vaccine. Vaccine 2009, 27, 3319–3323. [Google Scholar] [CrossRef]
- Moss, B. Reflections on the early development of poxvirus vectors. Vaccine 2013, 31, 4220–4222. [Google Scholar] [CrossRef] [PubMed]
- Mackett, M.; Smith, G.L.; Moss, B. Vaccinia virus: A selectable eukaryotic cloning and expression vector. Proc. Natl. Acad. Sci. USA 1982, 79, 7415–7419. [Google Scholar] [CrossRef]
- Panicali, D.; Paoletti, E. Construction of poxviruses as cloning vectors: Insertion of the thymidine kinase gene from herpes simplex virus into the DNA of infectious vaccinia virus. Proc. Natl. Acad. Sci. USA 1982, 79, 4927–4931. [Google Scholar] [CrossRef]
- Walsh, S.R.; Dolin, R. Vaccinia viruses: Vaccines against smallpox and vectors against infectious diseases and tumors. Expert Rev. Vaccines 2011, 10, 1221–1240. [Google Scholar] [CrossRef] [PubMed]
- Verardi, P.H.; Titong, A.; Hagen, C.J. A vaccinia virus renaissance: New vaccine and immunotherapeutic uses after smallpox eradication. Hum. Vaccines Immunother. 2012, 8, 961–970. [Google Scholar] [CrossRef] [PubMed]
- Sugimoto, M.; Yamanouchi, K. Characteristics of an attenuated vaccinia virus strain, LC16m0, and its recombinant virus vaccines. Vaccine 1994, 12, 675–681. [Google Scholar] [CrossRef]
- Kidokoro, M.; Shida, H. Vaccinia Virus LC16m8∆ as a Vaccine Vector for Clinical Applications. Vaccines 2014, 2, 755–771. [Google Scholar] [CrossRef]
- Yoshikawa, T. Third-generation smallpox vaccine strain-based recombinant vaccines for viral hemorrhagic fevers. Vaccine 2021, 39, 6174–6181. [Google Scholar] [CrossRef]
- Artenstein, A.W.; Johnson, C.; Marbury, T.C.; Morrison, D.; Blum, P.S.; Kemp, T.; Nichols, R.; Balser, J.P.; Currie, M.; Monath, T.P. A novel, cell culture-derived smallpox vaccine in vaccinia-naïve adults. Vaccine 2005, 23, 3301–3309. [Google Scholar] [CrossRef]
- CDC. Contraindication for Primary Vaccines and Revaccinees. Available online: https://www.cdc.gov/smallpox/clinicians/vaccination-contraindications1.html (accessed on 14 September 2021).
- World Health Organization. Meeting of the Strategic Advisory Group of Experts on Immunization, November 2013—Conclusions and Recommendations. In Weekly Epidemiological Record = Relevé Épidémiologique Hebdomadaire; WHO: Geneva, Switzerland, 2014; Volume 89, pp. 1–20. [Google Scholar]
- Pittman, P.R.; Hahn, M.; Lee, H.S.; Koca, C.; Samy, N.; Schmidt, D.; Hornung, J.; Weidenthaler, H.; Heery, C.R.; Meyer, T.P.; et al. Phase 3 Efficacy Trial of Modified Vaccinia Ankara as a Vaccine against Smallpox. N. Engl. J. Med. 2019, 381, 1897–1908. [Google Scholar] [CrossRef]
- Overton, E.T.; Lawrence, S.J.; Wagner, E.; Nopora, K.; Rösch, S.; Young, P.; Schmidt, D.; Kreusel, C.; De Carli, S.; Meyer, T.P.; et al. Immunogenicity and safety of three consecutive production lots of the non replicating smallpox vaccine MVA: A randomised, double blind, placebo controlled phase III trial. PLoS ONE 2018, 13, e0195897. [Google Scholar] [CrossRef]
- Georgana, I.; Sumner, R.P.; Towers, G.J.; de Motes, C.M. Virulent Poxviruses Inhibit DNA Sensing by Preventing STING Activation. J. Virol. 2018, 92, e02145-17. [Google Scholar] [CrossRef] [PubMed]
| T–Cell Epitopes of Vaccinia Virus B5 Protein | First–Last Amino Acid | Epitope Sequence | HLA Class | Ref. | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Class I | Class II | ||||||||||||||||
| A 2 | B 35 | B 44 | B 55 | DR1 | DR3 | DR4 | DR7 | DR 11 | DR 13 | DR 15 | DR B3 | DR B4 | DR B5 | ||||
| T–cell epitopes that reside in B5 protein of LC16m8 | 1–15 | MKTISVVTLLCVLPA | * | * | * | * | * | * | * | * | * | [28] | |||||
| 4–18 | ISVVTLLCVLPAVVY | * | * | * | * | * | [28] | ||||||||||
| 5–19 | SVVTLLCVLPAVVYS | * | [29] | ||||||||||||||
| 79–93 | SDYISELYNKPLYEV | * | [28] | ||||||||||||||
| T–cell epitopes of B5 protein that are lost from a truncated form of LC16m8 | 105–119 | TKYFRCEEKNGNTSW | * | [29] | |||||||||||||
| 166–180 | ASYISCTANSWNVIP | * | * | * | * | * | * | * | [28] | ||||||||
| 174–188 | NSWNVIPSCQQKCDI | * | * | [28] | |||||||||||||
| 193–207 | NGLISGSTFSIGGVI | * | [29] | ||||||||||||||
| 204–218 | GGVIHLSCKSGFILT | * | * | * | * | * | * | * | * | * | [28] | ||||||
| 225–239 | CIDGKWNPILPTCVR | * | [29] | ||||||||||||||
| 269–283 | QEIESLEATYHIIIV | * | * | * | [28] | ||||||||||||
| Vaccinia Virus Vaccines | Effectiveness | Safety | Vaccine Characteristics | Host Factors | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Cellular Immunity | Humoral Immunity | |||||||||
| Take Rate | Sero- Conversion | Adverse Events | B5R | Temperature Sensitivity | Plaque Formation | HLA | Genetic Polymorphism | Comorbidities | Ref. | |
| Lister | High | High | Temporary abnormal electro- encephalogram | Yes | No | Large | Not found | Not found | Usual contraindications to vaccination | [4,7,27,71], |
| NYCBH | High | High | Myo-/ pericarditis | Yes | No | Large | Neutralizing antibody titers | Neutralizing antibody titers, IFNγ secretion, cytokine production, adverse events (fever) | Usual contraindications to vaccination | [14,38,39,40,41,59,60,61,62,70,71] |
| ACAM2000 | High | High | Myo-/ pericarditis | Yes | No | Large | Neutralizing antibody titers | Not found | Usual contraindications to vaccination | [14,59,70,71] |
| MVA | ND | High | No cardiac events | Yes | No | No | Not found | Not found | Less restriction for immunodeficiencies, immunosuppressive therapies or atopic dermatitis | [17,72,74,75] |
| LC16m8 | High | High | No cardiac events | No | Yes | Small | ND | ND | Less restriction for atopic dermatitis if skin lesions are dry and stable | [4,7,27,57] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Eto, A.; Yamamoto, N.; Kanatani, Y. Effect of Serial Passage on the Pathogenicity and Immunogenicity of Vaccinia Virus LC16m8 Strain. Biology 2021, 10, 1158. https://doi.org/10.3390/biology10111158
Eto A, Yamamoto N, Kanatani Y. Effect of Serial Passage on the Pathogenicity and Immunogenicity of Vaccinia Virus LC16m8 Strain. Biology. 2021; 10(11):1158. https://doi.org/10.3390/biology10111158
Chicago/Turabian StyleEto, Akiko, Norio Yamamoto, and Yasuhiro Kanatani. 2021. "Effect of Serial Passage on the Pathogenicity and Immunogenicity of Vaccinia Virus LC16m8 Strain" Biology 10, no. 11: 1158. https://doi.org/10.3390/biology10111158
APA StyleEto, A., Yamamoto, N., & Kanatani, Y. (2021). Effect of Serial Passage on the Pathogenicity and Immunogenicity of Vaccinia Virus LC16m8 Strain. Biology, 10(11), 1158. https://doi.org/10.3390/biology10111158






