Long-Term Clinical Behavior and Complications of Intentionally Tilted Dental Implants Compared with Straight Implants Supporting Fixed Restorations: A Systematic Review and Meta-Analysis
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol Development and PICO Question
- Population: Systemically healthy edentulous and partially edentulous patients.
- Intervention: Implant-supported restorations with tilted dental implants.
- Comparison: Implant-supported restorations with axial dental implants.
- Outcome: Long-term clinical behavior, focusing on implant success and survival rates, peri-implant marginal bone loss, and prosthodontic/biological complications around tilted implants in comparison with axial implants.
2.2. Eligibility Criteria
2.2.1. Inclusion Criteria
- Clinical human studies of implant-supported restorations comparing intentionally tilted placed dental implants (ITDI) with axial dental implants.
- Types of study: randomized controlled clinical trials, cohort studies, clinical trials, multi-center studies, pragmatic clinical trials, case-control studies.
- Clinical human studies reporting data on: implant survival rates, implant success rates, marginal bone loss, prosthodontic/biological complications of axial and tilted dental implants.
- Follow-up of at least five years.
- Total number of patients/study arm or cohort greater than 25.
- Articles published in English, Spanish, or German
- Human studies published during the last 10 years.
2.2.2. Exclusion Criteria
- Clinical studies that did not provide >5-year follow-up.
- Clinical studies that did not compare axial and tilted dental implants within the same study.
- Studies of zygomatic implants.
- Animal studies or in vitro studies.
- Review articles or case reports.
2.3. Type of Intervention and Comparisons
2.4. Data Collection
2.5. Sources an Search Strategy
2.6. Study Selection, Screening Methods, and Clinical Data Extraction
2.7. Risk of Bias in Individual Studies
2.8. Statistical Analysis
3. Results
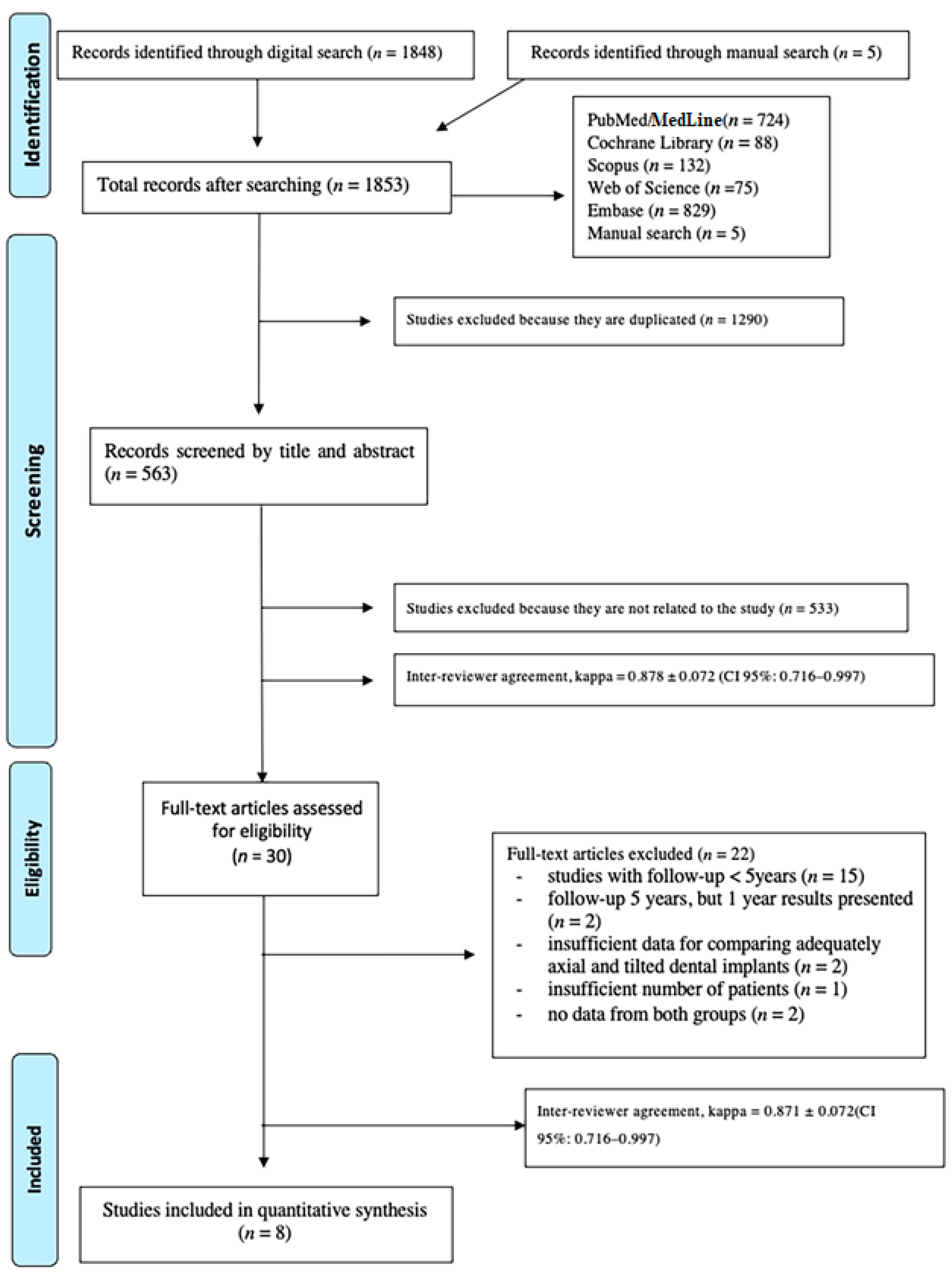
3.1. Study Selection
3.2. Study Characteristics
3.3. Study Characteristics
3.4. Synthesis of Results
3.4.1. Inter-Reviewer Agreement
3.4.2. Patient Characteristics
3.4.3. Marginal Bone Loss
3.4.4. Implant Survival Rates
3.4.5. Implant Success Rates
3.4.6. Dental Implant Angulation and Abutments
3.4.7. Properties of Dental Implants and Loading
3.4.8. Restoration Type and Location
3.4.9. Complications
4. Discussion
- Only non-randomized clinical trials were included, while the comparative studies presented a high risk of bias [40].
- Concerning the restoration materials used in the different studies, the types of restoration placed were diverse and the complications were also diverse and irregularly distributed. Future research should also take the antagonist arch into consideration, as this factor in combination with the occlusion may influence the type and number of mechanical complications.
- Eight of the studies reported the degree of angulation of their tilted implants (20°, 30°, 40°, 45°, and 50°), but only three studies reported the measurement methods used to ensure these angulations (guide, splint, or intraoral x-ray). It would be useful to establish an effective method of accurately confirming that the implant angulation achieved is as intended. Future studies should compare the influence that the degree of implant angulation has on implant survival or success rates, MBL, and biomechanical complications.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Adell, R.; Eriksson, B.; Lekholm, U.; I Brånemark, P.; Jemt, T. Long-term follow-up study of osseointegrated implants in the treatment of totally edentulous jaws. Int. J. Oral Maxillofac. Implant. 1990, 5, 347–359. [Google Scholar]
- Lambrecht, J.T.; Filippi, A.; Künzel, A.R.; Schiel, H.J. Long-term evaluation of submerged and nonsubmerged ITI solid-screw titanium implants: A 10-year life table analysis of 468 implants. Int. J. Oral Maxillofac. Implant. 2003, 18, 826–834. [Google Scholar] [CrossRef]
- Cochran, D.L.; Nummikoski, P.V.; Schoolfield, J.D.; Jones, A.A.; Oates, T.W. A Prospective Multicenter 5-Year Radiographic Evaluation of Crestal Bone Levels Over Time in 596 Dental Implants Placed in 192 Patients. J. Periodontol. 2009, 80, 725–733. [Google Scholar] [CrossRef] [PubMed]
- Ravald, N.; Dahlgren, S.; Teiwik, A.; Gröndahl, K. Long-term evaluation of Astra Tech and Brånemark implants in patients treated with full-arch bridges. Results after 12-15 years. Clin. Oral Implant. Res. 2012, 24, 1144–1151. [Google Scholar] [CrossRef]
- Barone, A.; Varanini, P.; Orlando, B.; Tonelli, P.; Covani, U. Deep-Frozen Allogeneic Onlay Bone Grafts for Reconstruction of Atrophic Maxillary Alveolar Ridges: A Preliminary Study. J. Oral Maxillofac. Surg. 2009, 67, 1300–1306. [Google Scholar] [CrossRef]
- Nissan, J.; Ghelfan, O.; Mardinger, O.; Calderon, S.; Chaushu, G. Efficacy of Cancellous Block Allograft Augmentation Prior to Implant Placement in the Posterior Atrophic Mandible. Clin. Implant. Dent. Relat. Res. 2009, 13, 279–285. [Google Scholar] [CrossRef] [PubMed]
- Koca, O.L.; Eskitascioglu, G.; Usumez, A. Three-dimensional finite-element analysis of functional stresses in different bone locations produced by implants placed in the maxillary posterior region of the sinus floor. J. Prosthet. Dent. 2005, 93, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Brånemark, P.; Gröndahl, K.; Öhrnell, L.; Nilsson, P.; Petruson, B.; Svensson, B.; Engstrand, P.; Nannmark, U. Zygoma fixture in the management of advanced atrophy of the maxilla: Technique and long-term results. Scand. J. Plast. Reconstr. Surg. Hand Surg. 2004, 38, 70–85. [Google Scholar] [CrossRef]
- A Fugazzotto, P. Shorter implants in clinical practice: Rationale and treatment results. Int. J. Oral Maxillofac. Implant. 2008, 23, 487–496. [Google Scholar]
- Krekmanov, L.; Kahn, M.; Rangert, B.; Lindström, H. Tilting of posterior mandibular and maxillary implants for improved prosthesis support. Int. J. Oral Maxillofac. Implant. 2000, 15, 405–414. [Google Scholar]
- Fortin, Y.; Sullivan, R.M. Terminal Posterior Tilted Implants Planned as a Sinus Graft Alternative for Fixed Full-Arch Implant-Supported Maxillary Restoration: A Case Series with 10- to 19-Year Results on 44 Consecutive Patients Presenting for Routine Maintenance. Clin. Implant. Dent. Relat. Res. 2016, 19, 56–68. [Google Scholar] [CrossRef] [Green Version]
- Dds, R.C.; Dds, M.T. Simplified Treatment of the Atrophic Posterior Maxilla via Immediate/Early Function and Tilted Implants: A Prospective 1-Year Clinical Study. Clin. Implant. Dent. Relat. Res. 2005, 7, s1–s12. [Google Scholar] [CrossRef]
- Monje, A.; Chan, H.-L.; Suarez, F.; Galindo-Moreno, P.; Wang, H.-L. Marginal bone loss around tilted implants in comparison to straight implants: A meta-analysis. Int. J. Oral Maxillofac. Implant. 2012, 27, 1576–1583. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; for the PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef] [Green Version]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Misch, C.E.; Perel, M.L.; Wang, H.-L.; Sammartino, G.; Galindo-Moreno, P.; Trisi, P.; Steigmann, M.; Rebaudi, A.; Palti, A.; Pikos, M.A.; et al. Implant Success, Survival, and Failure: The International Congress of Oral Implantologists (ICOI) Pisa Consensus Conference. Implant. Dent. 2008, 17, 5–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [Green Version]
- Wells, G.A.; Shea, B.; O’Connel, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa scale (NOS) for Assessing the Quality of Nonrandomized Studies in Meta-Analyses. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 28 February 2021).
- Liesegang, T.J. Evidence-based medicine: Principles for applying the users’ guides to patient care. Guyatt GH,∗ Haynes RB, Jaeschke RZ, Cook DJ, Green L, Naylor CD, Wilson MC, Richardson WS for the Evidence-Based Medicine Working Group. JAMA 2000;284:1290–1296. Am. J. Ophthalmol. 2001, 131, 153. [Google Scholar] [CrossRef]
- Mantel, N.; Haenszel, W. Statistical Aspects of the Analysis of Data From Retrospective Studies of Disease. J. Natl. Cancer Inst. 1959, 22, 719–748. [Google Scholar] [CrossRef] [Green Version]
- Francetti, L.; Romeo, D.; Corbella, S.; Taschieri, S.; Bsc, M.D.F. Bone Level Changes Around Axial and Tilted Implants in Full-Arch Fixed Immediate Restorations. Interim Results of a Prospective Study. Clin. Implant. Dent. Relat. Res. 2012, 14, 646–654. [Google Scholar] [CrossRef]
- Agnini, A.; Agnini, A.M.; Romeo, D.; Chiesi, M.; Pariente, L.; Stappert, C.F.J. Clinical Investigation on Axial versus Tilted Implants for Immediate Fixed Rehabilitation of Edentulous Arches: Preliminary Results of a Single Cohort Study. Clin. Implant. Dent. Relat. Res. 2012, 16, 527–539. [Google Scholar] [CrossRef] [PubMed]
- Gherlone, E.F.; Sannino, G.; Rapanelli, A.; Crespi, R.; Gastaldi, G.; Capparé, P. Prefabricated Bar System for Immediate Loading in Edentulous Patients: A 5-Year Follow-Up Prospective Longitudinal Study. BioMed Res. Int. 2018, 2018, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ayna, M.; Gulses, A.; Açil, Y. Comprehensive Comparison of the 5-Year Results of All-on-4 Mandibular Implant Systems With Acrylic and Ceramic Suprastructures. J. Oral Implant. 2015, 41, 675–683. [Google Scholar] [CrossRef] [PubMed]
- Toljanic, J.; Ekstrand, K.; Baer, R.; Thor, A. Immediate Loading of Tilted and Axial Posterior Implants in the Edentulous Maxillary Arch: A Retrospective Comparison of 5-Year Outcomes. Int. J. Oral Maxillofac. Implant. 2018, 33, 433–438. [Google Scholar] [CrossRef] [Green Version]
- Barnea, E.; Tal, H.; Nissan, J.; Tarrasch, R.; Peleg, M.; Kolerman, R. The Use of Tilted Implant for Posterior Atrophic Maxilla. Clin. Implant. Dent. Relat. Res. 2015, 18, 788–800. [Google Scholar] [CrossRef]
- Hopp, M.; Nobre, M.D.A.; Maló, P. Comparison of marginal bone loss and implant success between axial and tilted implants in maxillary All-on-4 treatment concept rehabilitations after 5 years of follow-up. Clin. Implant. Dent. Relat. Res. 2017, 19, 849–859. [Google Scholar] [CrossRef]
- Queridinha, B.M.; Almeida, R.F.; Felino, A.; Nobre, M.D.A.; Maló, P. Partial Rehabilitation with Distally Tilted and Straight Implants in the Posterior Maxilla with Immediate Loading Protocol: A Retrospective Cohort Study with 5-Year Follow-up. Int. J. Oral Maxillofac. Implant. 2016, 31, 891–899. [Google Scholar] [CrossRef]
- Albrektsson, T.; Zar, G.; Worthington, P.; Eriksson, A. The long-term ef cacy of currently used dental implants: A review and proposed criteria of success. Int. J. Oral Maxillofac. Implant. 1986, 1, 11–25. [Google Scholar]
- Pjetursson, B.E.; Heimisdottir, K. Dental implants – are they better than natural teeth? Eur. J. Oral Sci. 2018, 126, 81–87. [Google Scholar] [CrossRef] [Green Version]
- Inchingolo, F.; Tatullo, M.; Abenavoli, F.M.; Marrelli, M.; Inchingolo, A.D.; Palladino, A.; Inchingolo, A.M.; Dipalma, G. Oral Piercing and Oral Diseases: A Short Time Retrospective Study. Int. J. Med. Sci. 2011, 8, 649–652. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Papaspyridakos, P.; Mokti, M.; Chen, C.-J.; Benic, G.I.; Gallucci, G.O.; Chronopoulos, V. Implant and Prosthodontic Survival Rates with Implant Fixed Complete Dental Prostheses in the Edentulous Mandible after at Least 5 Years: A Systematic Review. Clin. Implant. Dent. Relat. Res. 2013, 16, 705–717. [Google Scholar] [CrossRef]
- Polido, W.D.; Aghaloo, T.; Emmett, T.W.; Taylor, T.D.; Morton, D. Number of implants placed for complete-arch fixed prostheses: A systematic review and meta-analysis. Clin. Oral Implant. Res. 2018, 29, 154–183. [Google Scholar] [CrossRef]
- Papaspyridakos, P.; Chen, C.-J.; Singh, M.; Weber, H.-P.; Gallucci, G. Success Criteria in Implant Dentistry. J. Dent. Res. 2012, 91, 242–248. [Google Scholar] [CrossRef] [PubMed]
- Del Fabbro, M.; Ceresoli, V. The fate of marginal bone around axial vs. tilted implants: A systematic review. Eur. J. Oral Implant. 2014, 7, S171–S179. [Google Scholar]
- Apaza Alccayhuaman, K.A.; Soto-Peñaloza, D.; Nakajima, Y.; Papageorgiou, S.N.; Botticelli, D.; Lang, N.P. Biological and technical complications of tilted implants in comparison with straight implants supporting fixed dental prostheses. A systematic review and meta-analysis. Clin. Oral Implant. Res. 2018, 29, 295–308. [Google Scholar] [CrossRef] [PubMed]
- Lin, W.-S.; Eckert, S.E. Clinical performance of intentionally tilted implants versus axially positioned implants: A systematic review. Clin. Oral Implant. Res. 2018, 29, 78–105. [Google Scholar] [CrossRef]
- Tatullo, M.; Marrelli, M.; Amantea, M.; Paduano, F.; Santacroce, L.; Gentile, S.; Scacco, S. Bioimpedance Detection of Oral Lichen Planus Used as Preneoplastic Model. J. Cancer 2015, 6, 976–983. [Google Scholar] [CrossRef] [Green Version]
- Zhou, W.; Liu, Z.; Song, L.; Kuo, C.-L.; Shafer, D.M. Clinical Factors Affecting the Accuracy of Guided Implant Surgery—A Systematic Review and Meta-analysis. J. Evid. Based Dent. Pr. 2018, 18, 28–40. [Google Scholar] [CrossRef]
- Papageorgiou, S.N.; Xavier, G.M.; Cobourne, M. Basic study design influences the results of orthodontic clinical investigations. J. Clin. Epidemiology 2015, 68, 1512–1522. [Google Scholar] [CrossRef]



| Authors and Year | Study | Patients Number | Implants (n) | Implants Axial (n) | Implants Tilted (n) | Implants (Length and Width) (mm) | Follow-Up | Full Arch/Partial | Location (Maxilla/Mandible) |
|---|---|---|---|---|---|---|---|---|---|
| Francetti et al. 2012 [21] | Prospective Cohort Study | 12 (47 total study) | 48 (196 total study) | n = 24 (98 total study) | n= 24 (98 total study) | NR and 4 | Maxilla: 22–40 months (mean 33.8 months). Mandible: 30–60 months (mean 52.8 months) | Full Arch-All on 4 | Both |
| Agnini et al. 2014 [22] | Prospective Cohort Study | 30 (total study) | 52 (202 total study) | 50 (165 total study) | 2 (37 total study) | NR and ≥3, 7 | 18–67 months (mean 44 months) | Full Arch | Both |
| Gherlone et al. 2018 [23] | Prospective Cohort Study | 29 (total study) | 128 at 5 years (total study) | 64 at 5 years (total study) | 64 at 5 years (total study) | 13 mm (axial); 13 and 15 mm (tilted). Axial (3.8, 4.5 mm); Tilted (4.5 mm) | 5 year | Full Arch-All on 4 | Both |
| Ayna et al. 2015 [24] | Prospective Cohort Study | 27 (total study) | 108 | 54 | 54 | 13 (axial); 15 (tilted) and 4 | 5 year | Full Arch-All on 4 | Mandible |
| Toljanic et al. 2018 [25] | Retrospective Cohort Study | 51 (total study) | 86 at 5 years (total study 102) | 35 (total study 38) | 51 (total study 64) | NR and NR | Intervals 1, 3, 5 year | Full Arch-All on 4 | Both |
| Barnea et al. 2016 [26] | Retrospective Cohort Study | 13 (29 total study) | 26 (58 total study) | 13 (29 total study) | 13 (29 total study) | 11.5–16 and 3.75, 4.2 | 1–17 year (mean 4.86 year) | Partial | Posterior Maxilla |
| Hopp et al. 2017 [27] | Retrospective Cohort Study | 891 (total study) | 3419 at 5 years (total study 3564) | 1706 at 5 years (total study 1782) | 1713 at 5 years (total study 1782) | 7–18 and 3.3, 3.75, 4, 5 | 5 year | Full Arch-All on 4 | Maxilla |
| Queridinha et al. 2016 [28] | Retrospective Cohort Study | 60 (total study) | 120 | 90 at 5 yearss (total study) | 30 at 5 years (total study) | 7–18 and 3.75, 4.2 | 5 year | Partial | Posterior Maxilla |
| Authors and Year | Restorations (n) | Loading | Angulation of Implant | Abutment Y/N | MBL and Desviation MBL (Axial) (mm) | MBL and Desviation MBL (Tilted) (mm) |
|---|---|---|---|---|---|---|
| Francetti et al. 2012 [21] | 12 (49 total study) | Inmediate | 30° | Y (0°, 30°) | 0.51 ± 0.17 | 0.39 ± 0.18 |
| Agnini et al. 2014 [22] | 8 (36 total study) | Inmediate | 20–40° | Y (angulation not specified) | 1.73 ± 0.14 (maxilla); 1.70 ± 0.18 (mandible) | 2 (maxilla) ± 0.14 |
| Gherlone et al. 2018 [23] | 12 max; 20 mandible | Inmediate | 25–30° | Y (30°) | 1.08 ± 0.45 (maxilla); 1.04 ± 0.61 (mandible) | 1.02 ± 0.67 (maxilla); 1.09 ± 0.56 (mandible) |
| Ayna et al. 2015 [24] | 27 | Inmediate | 45° | Y (30°) | 0.78 ± 0.10 (region 32); 0.78 ± 0.10 (region 42 | 1.24 ± 0.13 (region 35); 1.30 ± 0.13 (region 45) |
| Toljanic et al. 2018 [25] | 51 | Inmediate | NR | Y (angulation not specified) | 0.14 ± 0.34 | 0.79 ± 1.42 |
| Barnea et al. 2016 [26] | 13 (29 total study) | Delayed | 20–50° | Y (15–25°) | 1.50 ± 0.81 | 1.50 ± 0.67 |
| Hopp et al. 2017 [27] | 891 | Inmediate | 30–45° | Y (0°, 17°, 30°) | 1.14 ± 0.71 | 1.19 ± 0.82 |
| Queridinha et al. 2016 [28] | 60 | Inmediate | 30–45° | Y (30°) | 2.11 ± 0.44 | 1.92 ± 0.48 |
| Authors and Year | Success of Axial Implants | Success of Tilted Implants | Survival of Tilted Implants | Survival of Axial Implants | Complications |
|---|---|---|---|---|---|
| Francetti et al. 2012 [21] | NR | NR | 24/24 (100%) | 24/24 (100%) | Three axial mandibular implants in two patients showed peri-implantitis; fracture of the acrylic prosthesis (15%) in the mandible and (19%) in the maxilla (19%); fracture of the framework after 3 years of loading (3%). |
| Agnini et al. 2014 [22] | NR | NR | 37/37 (100%) | 161/165 (97.57%) | Breaking of esthetic veneering of the temporary prostheses (5.5% of cases). |
| Gherlone et al. 2018 [23] | NR | NR | 63//64 (98.44%) | 64/64 (100%) (maxilla and mandible) | Prosthetic survival rate (100%). Occlusal screw loosening was observed in 3.03% of cases (4 implants) within 6 months of follow-up. |
| Ayna et al. 2015 [24] | 100% | 100% | 54/54 (100%) | 54/54 (100%) | Ceramic supra-structures: only a single loosening of a fixation screw/acrylic restorations: abrasion in all restorations neither esthetically nor functionally relevant, and 28.6 % veneer fractures. |
| Toljanic et al. 2018 [25] | NR | NR | 44/51 (86.2%) | 30/35 (85.71%) | Fracture resin base/teeth (n = 30); framework fracture (n = 5); abutment screw loose(n = 4); abutment fracture(n = 2); food impaction (n = 2); excessive occlusion(n = 2); seating error of angled abutment (n = 2); bulky construction (n = 1); fractured provisional (n = 1); speech problems (n = 1). |
| Barnea et al. 2016 [26] | 26/29 (89.6%) | 27/29 (93.1%) | NR | NR | Prosthetic survival rate was 100%. One bridge (3.4%) was de-cemented, and two screws loosening (3.4%) occurred in the same patient. |
| Hopp et al. 2017 [27] | 76//1782 (95.7%) | 69//1782 (96.1%) | NR | NR | Prosthesis survival rate (99.8%). Biological complications (313 implants in 209 patients (23.5%): infection (24), fistula (4), mucositis (189), peri-implant pathology (95), or abscess (n = 1). Biological complications were observed with 131 axial and 182 tilted implants. |
| Queridinha et al. 2016 [28] | NR | NR | NR | NR | Five patients presented biologic complications (8.3%) and sixteen patients presented mechanical complications. |
| Selection | Comparability | Exposure | Number of Stars (out of 9) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Study | S1 | S2 | S3 | S4 | C1 | C2 | E1 | E2 | E3 | |
| Francetti et al. [21] | ★ | ★ | 0 | 0 | ★ | 0 | ★ | 0 | ★ | 5 |
| Agnini et al. [22] | ★ | ★ | ★ | 0 | ★ | 0 | ★ | 0 | 0 | 3 |
| Gherlone et al. [23] | ★ | ★ | ★ | 0 | ★ | 0 | ★ | 0 | ★ | 6 |
| Ayna et al. [24] | ★ | ★ | 0 | ★ | 0 | 0 | ★ | 0 | ★ | 5 |
| Toljanic et al. [25] | ★ | ★ | ★ | 0 | ★ | 0 | ★ | 0 | 0 | 5 |
| Barnea et al. [26] | ★ | ★ | ★ | 0 | ★ | 0 | 0 | ★ | 0 | 5 |
| Hopp et al. [27] | ★ | ★ | ★ | 0 | 0 | 0 | ★ | ★ | 0 | 5 |
| Queridinha et al. [28] | ★ | ★ | 0 | ★ | 0 | ★ | ★ | 0 | 0 | 5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cortés-Bretón Brinkmann, J.; García-Gil, I.; Pedregal, P.; Peláez, J.; Prados-Frutos, J.C.; Suárez, M.J. Long-Term Clinical Behavior and Complications of Intentionally Tilted Dental Implants Compared with Straight Implants Supporting Fixed Restorations: A Systematic Review and Meta-Analysis. Biology 2021, 10, 509. https://doi.org/10.3390/biology10060509
Cortés-Bretón Brinkmann J, García-Gil I, Pedregal P, Peláez J, Prados-Frutos JC, Suárez MJ. Long-Term Clinical Behavior and Complications of Intentionally Tilted Dental Implants Compared with Straight Implants Supporting Fixed Restorations: A Systematic Review and Meta-Analysis. Biology. 2021; 10(6):509. https://doi.org/10.3390/biology10060509
Chicago/Turabian StyleCortés-Bretón Brinkmann, Jorge, Ignacio García-Gil, Patricia Pedregal, Jesús Peláez, Juan Carlos Prados-Frutos, and María Jesús Suárez. 2021. "Long-Term Clinical Behavior and Complications of Intentionally Tilted Dental Implants Compared with Straight Implants Supporting Fixed Restorations: A Systematic Review and Meta-Analysis" Biology 10, no. 6: 509. https://doi.org/10.3390/biology10060509
APA StyleCortés-Bretón Brinkmann, J., García-Gil, I., Pedregal, P., Peláez, J., Prados-Frutos, J. C., & Suárez, M. J. (2021). Long-Term Clinical Behavior and Complications of Intentionally Tilted Dental Implants Compared with Straight Implants Supporting Fixed Restorations: A Systematic Review and Meta-Analysis. Biology, 10(6), 509. https://doi.org/10.3390/biology10060509








