The Role of Extracellular Vesicles in Ischemic Stroke Severity
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
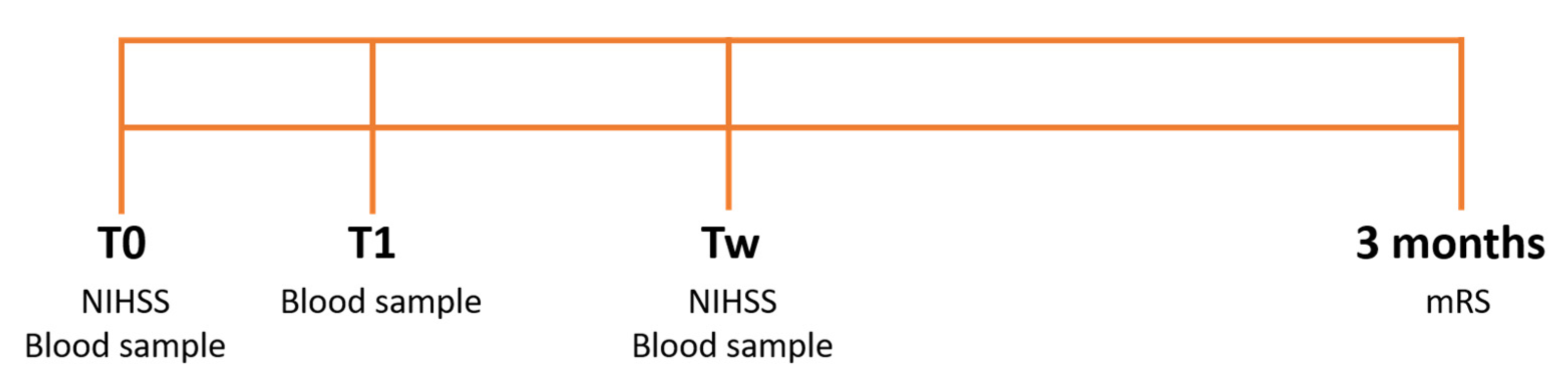
2.2. Experimental Protocol
2.3. EV Isolation
2.4. Nanosight Analysis
2.5. Flow Cytometry
2.6. Statistical Analysis
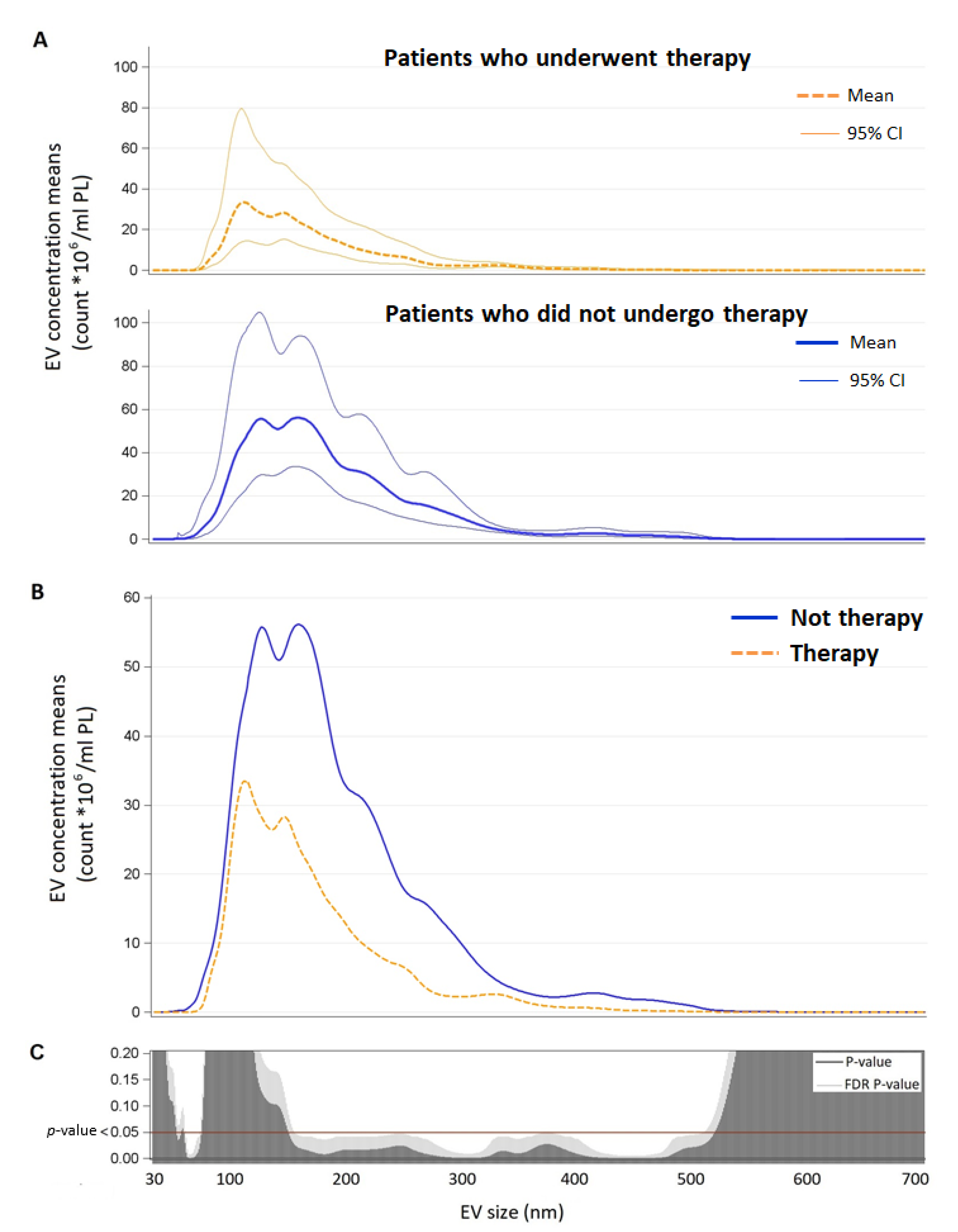
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Raposo, G.; Stoorvogel, W. Extracellular Vesicles: Exosomes, Microvesicles, and Friends. J. Cell Biol. 2013, 200, 373–383. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neven, K.Y.; Nawrot, T.S.; Bollati, V. Extracellular Vesicles: How the External and Internal Environment Can Shape Cell-to-Cell Communication. Curr. Environ. Health Rep. 2017, 4, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Dickhout, A.; Koenen, R.R. Extracellular Vesicles as Biomarkers in Cardiovascular Disease; Chances and Risks. Front. Cardiovasc. Med. 2018, 5, 113. [Google Scholar] [CrossRef] [PubMed]
- Femminò, S.; Penna, C.; Margarita, S.; Comità, S.; Brizzi, M.F.; Pagliaro, P. Extracellular Vesicles and Cardiovascular System: Biomarkers and Cardioprotective Effectors. Vasc. Pharmacol. 2020, 135, 106790. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The Top 10 Causes of Death. Available online: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death (accessed on 26 April 2021).
- Béjot, Y.; Bailly, H.; Durier, J.; Giroud, M. Epidemiology of Stroke in Europe and Trends for the 21st Century. Presse Méd. 2016, 45, e391–e398. [Google Scholar] [CrossRef] [PubMed]
- Gattringer, T.; Posekany, A.; Niederkorn, K.; Knoflach, M.; Poltrum, B.; Mutzenbach, S.; Haring, H.-P.; Ferrari, J.; Lang, W.; Willeit, J.; et al. Predicting Early Mortality of Acute Ischemic Stroke. Stroke 2019, 50, 349–356. [Google Scholar] [CrossRef] [Green Version]
- Ovbiagele, B.; Lyden, P.D.; Saver, J.L. Disability Status at 1 Month Is a Reliable Proxy for Final Ischemic Stroke Outcome. Neurology 2010, 75, 688–692. [Google Scholar] [CrossRef]
- Feigin, V.L.; Forouzanfar, M.H.; Krishnamurthi, R.; Mensah, G.A.; Connor, M.; Bennett, D.A.; Moran, A.E.; Sacco, R.L.; Anderson, L.; Truelsen, T.; et al. Global and Regional Burden of Stroke during 1990–2010: Findings from the Global Burden of Disease Study 2010. Lancet 2014, 383, 245–255. [Google Scholar] [CrossRef]
- The European Stroke Organisation (ESO) Executive Committee; ESO Writing Committee. Guidelines for Management of Ischaemic Stroke and Transient Ischaemic Attack 2008. CED 2008, 25, 457–507. [Google Scholar] [CrossRef]
- Schlegel, D.; Kolb Stephen, J.; Luciano Jean, M.; Tovar Jennifer, M.; Cucchiara Brett, L.; Liebeskind David, S.; Kasner Scott, E. Utility of the NIH Stroke Scale as a Predictor of Hospital Disposition. Stroke 2003, 34, 134–137. [Google Scholar] [CrossRef]
- Banks Jamie, L.; Marotta Charles, A. Outcomes Validity and Reliability of the Modified Rankin Scale: Implications for Stroke Clinical Trials. Stroke 2007, 38, 1091–1096. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Italian Stroke Organization. SPREAD—Stroke Prevention and Educational Awareness Diffusion Ictus Cerebrale: Linee Guida Italiane Di Prevenzione e Trattamento; Modena, Italy, 2016. Available online: https://www.sifel.it/wp-content/uploads/2017/09/LG-SPREAD-ictus-cerebrale.pdf (accessed on 26 April 2021).
- Ahmed, N.; Steiner, T.; Caso, V.; Wahlgren, N.; ESO-KSU Session Participants. Recommendations from the ESO-Karolinska Stroke Update Conference, Stockholm 13–15 November 2016. Eur. Stroke J. 2017, 2, 95–102. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Powers, W.J.; Derdeyn, C.P.; Biller, J.; Coffey, C.S.; Hoh, B.L.; Jauch, E.C.; Johnston, K.C.; Claiborne Johnston, S.; Khalessi, A.A.; Kidwell, C.S.; et al. 2015 American Heart Association/American Stroke Association Focused Update of the 2013 Guidelines for the Early Management of Patients with Acute Ischemic Stroke Regarding Endovascular Treatment. Stroke 2015, 46, 3020–3035. [Google Scholar] [CrossRef] [Green Version]
- Cherian, P.; Hankey, G.J.; Eikelboom, J.W.; Thom, J.; Baker, R.I.; McQuillan, A.; Staton, J.; Yi, Q. Endothelial and Platelet Activation in Acute Ischemic Stroke and Its Etiological Subtypes. Stroke 2003, 34, 2132–2137. [Google Scholar] [CrossRef] [Green Version]
- Chiva-Blanch, G.; Laake, K.; Myhre, P.; Bratseth, V.; Arnesen, H.; Solheim, S.; Badimon, L.; Seljeflot, I. Platelet-, Monocyte-Derived and Tissue Factor-Carrying Circulating Microparticles Are Related to Acute Myocardial Infarction Severity. PLoS ONE 2017, 12, e0172558. [Google Scholar] [CrossRef]
- Wang, B.; Cai, W.; Zhang, Z.; Zhang, H.; Tang, K.; Zhang, Q.; Wang, X. Circulating Microparticles in Patients after Ischemic Stroke: A Systematic Review and Meta-Analysis. Rev. Neurosci. 2021, 32, 1–10. [Google Scholar] [CrossRef]
- Kuriyama, N.; Nagakane, Y.; Hosomi, A.; Ohara, T.; Kasai, T.; Harada, S.; Takeda, K.; Yamada, K.; Ozasa, K.; Tokuda, T.; et al. Evaluation of Factors Associated with Elevated Levels of Platelet-Derived Microparticles in the Acute Phase of Cerebral Infarction. Clin. Appl. Thromb. Hemost. 2010, 16, 26–32. [Google Scholar] [CrossRef] [PubMed]
- Agouni, A.; Parray, A.S.; Akhtar, N.; Mir, F.A.; Bourke, P.J.; Joseph, S.; Morgan, D.M.; Santos, M.D.; Wadiwala, M.F.; Kamran, S.; et al. There Is Selective Increase in Pro-Thrombotic Circulating Extracellular Vesicles in Acute Ischemic Stroke and Transient Ischemic Attack: A Study of Patients From the Middle East and Southeast Asia. Front. Neurol. 2019, 10, 1–10. [Google Scholar] [CrossRef]
- Rosińska, J.; Ambrosius, W.; Maciejewska, J.; Narożny, R.; Kozubski, W.; Łukasik, M. Association of Platelet-Derived Microvesicles and Their Phenotypes with Carotid Atherosclerosis and Recurrent Vascular Events in Patients after Ischemic Stroke. Thromb. Res. 2019, 176, 18–26. [Google Scholar] [CrossRef]
- Bivard, A.; Lincz, L.F.; Maquire, J.; Parsons, M.; Levi, C. Platelet Microparticles: A Biomarker for Recanalization in RtPA-treated Ischemic Stroke Patients. Ann. Clin. Transl. Neurol. 2017, 4, 175–179. [Google Scholar] [CrossRef]
- Sinauridze, E.; Kireev, D.; Popenko, N.; Pichugin, A.; Panteleev, M.; Krymskaya, O.; Ataullakhanov, F. Platelet Microparticle Membranes Have 50- to 100-Fold Higher Specific Procoagulant Activity than Activated Platelets. Thromb. Haemost. 2007, 97, 425–434. [Google Scholar] [CrossRef] [PubMed]
- Jimenez, J.J.; Jy, W.; Mauro, L.M.; Soderland, C.; Horstman, L.L.; Ahn, Y.S. Endothelial Cells Release Phenotypically and Quantitatively Distinct Microparticles in Activation and Apoptosis. Thromb. Res. 2003, 109, 175–180. [Google Scholar] [CrossRef]
- Gallo, G.; Volpe, M.; Savoia, C. Endothelial Dysfunction in Hypertension: Current Concepts and Clinical Implications. Front. Med. 2022, 8, 798958. [Google Scholar] [CrossRef] [PubMed]
- Buffolo, F.; Monticone, S.; Camussi, G.; Aikawa, E. Role of Extracellular Vesicles in the Pathogenesis of Vascular Damage. Hypertension 2022, 79, 863–873. [Google Scholar] [CrossRef]
- Angelillo-Scherrer, A.; Weber, C.; Mause, S. Leukocyte-Derived Microparticles in Vascular Homeostasis. Circ. Res. 2012, 110, 356–369. [Google Scholar] [CrossRef] [Green Version]
- Martin, S.; Tesse, A.; Hugel, B.; Martínez, M.C.; Morel, O.; Freyssinet, J.-M.; Andriantsitohaina, R. Shed Membrane Particles from T Lymphocytes Impair Endothelial Function and Regulate Endothelial Protein Expression. Circulation 2004, 109, 1653–1659. [Google Scholar] [CrossRef] [Green Version]
- Wang, H.; Wang, Z.; Wu, Q.; Yuan, Y.; Cao, W.; Zhang, X. Regulatory T Cells in Ischemic Stroke. CNS Neurosci. Ther. 2021, 27, 643–651. [Google Scholar] [CrossRef]
- Santamaría-Cadavid, M.; Rodríguez-Castro, E.; Rodríguez-Yáñez, M.; Arias-Rivas, S.; López-Dequidt, I.; Pérez-Mato, M.; Rodríguez-Pérez, M.; López-Loureiro, I.; Hervella, P.; Campos, F.; et al. Regulatory T Cells Participate in the Recovery of Ischemic Stroke Patients. BMC Neurol. 2020, 20, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Deb, P.; Sharma, S.; Hassan, K.M. Pathophysiologic Mechanisms of Acute Ischemic Stroke: An Overview with Emphasis on Therapeutic Significance beyond Thrombolysis. Pathophysiology 2010, 17, 197–218. [Google Scholar] [CrossRef]
- Hervella, P.; Rodríguez-Castro, E.; Rodríguez-Yáñez, M.; Arias, S.; Santamaría-Cadavid, M.; López-Dequidt, I.; Estany-Gestal, A.; Maqueda, E.; López-Loureiro, I.; Sobrino, T.; et al. Intra- and Extra-Hospital Improvement in Ischemic Stroke Patients: Influence of Reperfusion Therapy and Molecular Mechanisms. Sci. Rep. 2020, 10, 3513. [Google Scholar] [CrossRef]
- Turovsky, E.A.; Golovicheva, V.V.; Varlamova, E.G.; Danilina, T.I.; Goryunov, K.V.; Shevtsova, Y.A.; Pevzner, I.B.; Zorova, L.D.; Babenko, V.A.; Evtushenko, E.A.; et al. Mesenchymal Stromal Cell-Derived Extracellular Vesicles Afford Neuroprotection by Modulating PI3K/AKT Pathway and Calcium Oscillations. Int. J. Biol. Sci. 2022, 18, 5345–5368. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Value |
|---|---|
| Age, years | 74.1 ± 14.1 |
| Gender (males) | 26 (55.3%) |
| BMI, kg/m2 | 24.8 ± 3.8 |
| Previous stroke or TIA | 12 (25.5%) |
| Hypertension | 31 (66.0%) |
| Diabetes | 7 (14.9%) |
| History of atrial fibrillation | 15 (31.9%) |
| History of heart failure | 6 (12.8%) |
| Smoking status | |
| Never smoker | 33 (70.2%) |
| Current smoker | 10 (21.3%) |
| Missing | 4 (8.5%) |
| Blood pressure, mmHg | |
| Systolic | 163 ± 26 |
| Diastolic | 89 ± 17 |
| Glucose, mg/dL | 120.3 ± 32.1 |
| Hb, g/dL | 13.9 ± 1.7 |
| Ht, % | 40.4 ± 4.3 |
| Plt *103, N/uL | 225 [193; 304] |
| AST, U/L | 22.4 ± 7.9 |
| ALT, U/L | 18.5 ± 7.5 |
| PT | 1.1 ± 0.4 |
| aPTT | 0.9 ± 0.1 |
| Albumin, g/dL | 4.0 ± 0.4 |
| Creatinine, mg/dL | 1.0 ± 0.35 |
| C-reactive protein, mg/dL | 0.38 [0.16; 0.75] |
| Total cholesterol, mg/dL | 185.5 ± 34.2 |
| NIHSS on admission | 8 [5; 14] |
| <14 | 34 (72.3%) |
| ≥14 | 13 (27.7%) |
| Therapy | |
| IV rtPA | 18 (38.3%) |
| Thrombectomy | 4 (8.5%) |
| IV rtPA+ thrombectomy | 6 (12.8%) |
| No therapy | 19 (40.4%) |
| TOAST Classification | |
| Cardioembolic stroke | 23 (48.9%) |
| Atherothrombotic stroke | 6 (12.8%) |
| Lacunar stroke | 2 (4.3%) |
| Undetermined etiology | 16 (34.0%) |
| Hemispheric stroke | |
| Right | 22 (46.8%) |
| Left | 23 (48.9%) |
| Bilateral | 2 (4.3%) |
| Vascular territory | |
| Anterior | 40 (85.1%) |
| Posterior | 7 (14.9%) |
| NIHSS after one week | 3 [2; 7] |
| <14 | 31 (66.0%) |
| ≥14 | 6 (12.8%) |
| Missing | 10 (21.2%) |
| Modified Rankin scale at 3 months | 2.8 ± 2.5 |
| 0–2 | 20 (42.5%) |
| 3–5 | 10 (21.3%) |
| 6 | 11 (23.4%) |
| Missing | 6 (12.8%) |
| T0 | ||||
|---|---|---|---|---|
| EV Count | ∆%* | 95% CI | p-Value | |
| Total EVs | −0.001 | −0.006 | 0.005 | 0.8317 |
| EV Subtype | ∆%** | 95% CI | p-Value | |
| CD14+ (macrophages/monocytes) | 0.044 | −0.111 | 0.199 | 0.5802 |
| CD61+ (platelets) | 0.177 | 0.065 | 0.289 | 0.0019 |
| CD105+ (endothelium) | 0.497 | −1.129 | 2.150 | 0.5515 |
| CD25+ (T-cells) | 0.255 | −1.876 | 2.432 | 0.8162 |
| CD62E+ (activated endothelial cells) | −0.567 | −1.665 | 0.544 | 0.3161 |
| T0 | T1 | Tw | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| EV count | ∆%* | 95% CI | p-Value | ∆%* | 95% CI | p-Value | ∆%* | 95% CI | p-Value | |||
| Total EVs | 0.005 | −0.002 | 0.013 | 0.1327 | 0.003 | −0.019 | 0.025 | 0.7847 | 0.016 | −0.008 | 0.040 | 0.1958 |
| EV subtype | ∆%** | 95% CI | p-Value | ∆%** | 95% CI | p-Value | ∆%** | 95% CI | p-Value | |||
| CD14+ (macrophages/monocytes) | −0.02 | −0.21 | 0.18 | 0.8763 | 0.91 | −0.44 | 2.28 | 0.1857 | 2.71 | −1.3 | 6.88 | 0.1877 |
| CD61+ (platelets) | −0.08 | −0.39 | 0.24 | 0.6363 | −0.20 | −0.48 | 0.07 | 0.1488 | −0.81 | −3.31 | 1.74 | 0.5287 |
| CD105+ (endothelium) | 1.86 | −0.84 | 4.63 | 0.1785 | −0.11 | −4.09 | 4.04 | 0.9571 | 1.03 | −4.38 | 6.73 | 0.7161 |
| CD25 + (T-cells) | 3.93 | 0.99 | 6.97 | 0.0086 | −0.79 | −2.00 | 0.44 | 0.2071 | 2.4 | −3.19 | 8.31 | 0.4081 |
| CD62E+ (activated endothelial cells) | 0.90 | −0.98 | 2.81 | 0.3523 | 2.32 | −0.91 | 5.65 | 0.1610 | 4.75 | −19.92 | 37.01 | 0.7351 |
| T0 | T1 | Tw | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| EV count | ∆%* | 95% CI | p-value | ∆%* | 95% CI | p-value | ∆%* | 95% CI | p-value | |||
| Total EVs | 0.006 | −0.001 | 0.013 | 0.0717 | −0.017 | −0.046 | 0.013 | 0.2672 | 0.016 | −0.008 | 0.040 | 0.1958 |
| EV subtype | ∆%** | 95% CI | p-value | ∆%** | 95% CI | p-value | ∆%** | 95% CI | p-value | |||
| CD14+ (macrophages/monocytes) | 0.05 | −0.10 | 0.19 | 0.5517 | 0.60 | −0.33 | 1.53 | 0.2073 | 2.71 | −1.3 | 6.88 | 0.1877 |
| CD61+ (platelets) | 0.30 | 0.06 | 0.55 | 0.0158 | 0.18 | −0.03 | 0.39 | 0.0958 | −0.81 | −3.31 | 1.74 | 0.5287 |
| CD105+ (endothelium) | 1.66 | −0.79 | 4.17 | 0.1861 | 2.78 | −1.21 | 6.92 | 0.1745 | 1.03 | −4.38 | 6.73 | 0.7161 |
| CD25 + (T-cells) | 3.94 | 0.96 | 7.01 | 0.0093 | 0.91 | 0.01 | 1.81 | 0.0468 | 2.4 | −3.19 | 8.31 | 0.4081 |
| CD62E+ (activated endothelial cells) | 1.79 | −0.43 | 4.06 | 0.1155 | 1.92 | −1.01 | 4.94 | 0.2015 | 4.75 | −19.92 | 37.01 | 0.7351 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carandina, A.; Favero, C.; Sacco, R.M.; Hoxha, M.; Torgano, G.; Montano, N.; Bollati, V.; Tobaldini, E. The Role of Extracellular Vesicles in Ischemic Stroke Severity. Biology 2022, 11, 1489. https://doi.org/10.3390/biology11101489
Carandina A, Favero C, Sacco RM, Hoxha M, Torgano G, Montano N, Bollati V, Tobaldini E. The Role of Extracellular Vesicles in Ischemic Stroke Severity. Biology. 2022; 11(10):1489. https://doi.org/10.3390/biology11101489
Chicago/Turabian StyleCarandina, Angelica, Chiara Favero, Roberto Maria Sacco, Mirjam Hoxha, Giuseppe Torgano, Nicola Montano, Valentina Bollati, and Eleonora Tobaldini. 2022. "The Role of Extracellular Vesicles in Ischemic Stroke Severity" Biology 11, no. 10: 1489. https://doi.org/10.3390/biology11101489







