What We Know about Sting-Related Deaths? Human Fatalities Caused by Hornet, Wasp and Bee Stings in Europe (1994–2016)
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
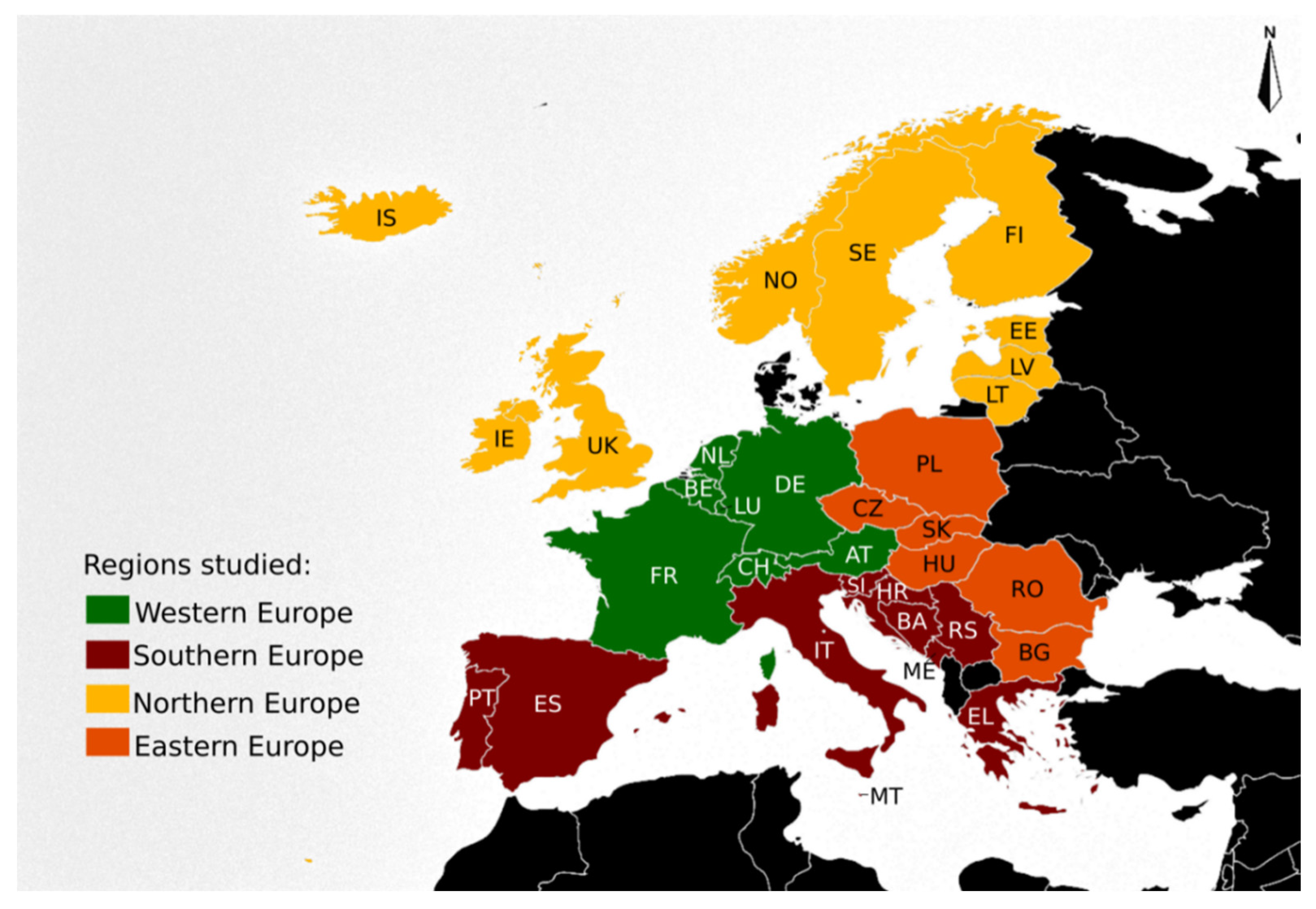
- − Country in which the fatality happened (n = 32) grouped into four regions (Eastern, Northern, Southern and Western Europe) (Figure 1).
- − Year of occurrence, from 1994 to 2016.
- − X23 code extension to four-digit. Comprising nine categories relative to the place of occurrence: X23.0 (home), X23.1 (residential institution), X23.2 (school, other institution and public administrative area), X23.3 (sports and athletics area), X23.4 (street and highway), X23.5 (trade and service area), X23.6 (industrial and construction area, X23.7 (farm), X23.8 (other specified places) and X23.9 (unspecified place). Supplementary Table S1 lists the included and excluded places in each category.
- − Gender, males (♂X23) and females (♀X23).
- − Age categories: children (0–14 years), youth (15–24 years), adults (25–64) and seniors (65 years and older).
3. Results
3.1. Countries and Study Period
3.2. Hymenopteran Sting-Related Deaths
3.3. Specific Locations where Hymenopteran Sting-Related Deaths Occurred
3.4. Age Distribution of Hymenopteran Sting-Related Deaths
3.5. Hymenopteran Sting-Related Deaths by Gender
3.6. Hymenopteran Sting-Related Deaths Features by Region: Eastern, Northern, Southern and Western Europe
3.7. Hymenopteran Sting-Related Deaths, X23 Mortality Rates (X23MR)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cianferoni, A. Non-IgE-mediated anaphylaxis. J. Allergy Clin. Immunol. 2021, 147, 1123–1131. [Google Scholar] [CrossRef]
- Worm, M.; Eckermann, O.; Dölle, S.; Aberer, W.; Beyer, K.; Hawranek, T.; Hompes, S.; Koehli, A.; Mahler, V.; Nemat, K.; et al. Triggers and treatment of anaphylaxis: An analysis of 4000 cases from Germany, Austria and Switzerland. Dtsch. Arztebl. Int. 2014, 111, 367–375. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Demain, J.G.; Minaei, A.A.; Tracy, J.M. Anaphylaxis and insect allergy. Curr. Opin. Allergy Clin. Immunol. 2010, 10, 318–322. [Google Scholar] [CrossRef] [PubMed]
- Yoon, K.A.; Kim, K.; Kim, W.-J.; Bang, W.Y.; Ahn, N.-H.; Bae, C.-H.; Yeo, J.-H.; Lee, S.H. Characterization of venom components and their phylogenetic properties in some Aculeate bumblebees and wasps. Toxins 2020, 12, 47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pucca, M.B.; Cerni, F.A.; Oliveira, I.S.; Jenkins, T.P.; Argemí, L.; Sørensen, C.V.; Ahmadi, S.; Barbosa, J.E.; Laustsen, A.H. Bee updated: Current knowledge on bee venom and bee envenoming therapy. Front. Immunol. 2019, 10, 2090. [Google Scholar] [CrossRef] [Green Version]
- Pak, S.C. An introduction to the toxins special issue on “bee and wasp venoms: Biological characteristics and therapeutic application”. Toxins 2016, 8, 315. [Google Scholar] [CrossRef] [Green Version]
- Feindor, M.; Heath, M.D.; Hewings, S.J.; Carreno Velazquez, T.L.; Blank, S.; Grosch, J.; Jakob, T.; Schmid-Grendelmeier, P.; Klimek, L.; Golden, D.B.K.; et al. Venom immunotherapy: From proteins to product to patient protection. Toxins 2021, 13, 616. [Google Scholar] [CrossRef]
- Perez-Riverol, A.; Justo-Jacomini, D.L.; Zollner, R.D.L.; Brochetto-Braga, M.R. Facing hymenoptera venom allergy: From natural to recombinant allergens. Toxins 2015, 7, 2551–2570. [Google Scholar] [CrossRef]
- Pascoal, A.; Estevinho, M.M.; Choupina, A.B.; Sousa-Pimenta, M.; Estevinho, L.M. An overview of the bioactive compounds, therapeutic properties and toxic effects of apitoxin. Food Chem. Toxicol. 2019, 134, 110864. [Google Scholar] [CrossRef]
- Abd El-Wahed, A.; Yosri, N.; Sakr, H.H.; Du, M.; Algethami, A.F.M.; Zhao, C.; Abdelazeem, A.H.; Tahir, H.E.; Masry, S.H.D.; Abdel-Daim, M.M.; et al. Wasp venom biochemical components and their potential in biological applications and nanotechnological interventions. Toxins 2021, 13, 206. [Google Scholar] [CrossRef]
- Elieh Ali Komi, D.; Shafaghat, F.; Zwiener, R.D. Immunology of bee venom. Clin. Rev. Allergy Immunol. 2018, 54, 386–396. [Google Scholar] [CrossRef] [PubMed]
- Sahiner, U.M.; Durham, S.R. Hymenoptera venom allergy: How does venom immunotherapy prevent anaphylaxis from bee and wasp stings? Front. Immunol. 2019, 10, 1959. [Google Scholar] [CrossRef] [PubMed]
- Mingomataj, E.Ç.; Bakiri, A.H.; Ibranji, A.; Sturm, G.J. Unusual reactions to hymenoptera stings: What should we keep in mind? Clin. Rev. Allergy Immunol. 2014, 47, 91–99. [Google Scholar] [CrossRef] [PubMed]
- Nittner-Marszalska, M.; Cichocka-Jarosz, E. Insect sting allergy in adults: Key messages for clinicians. Pol. Arch. Med. Wewn. 2015, 125, 929–937. [Google Scholar] [CrossRef] [Green Version]
- Forrester, J.A.; Weiser, T.G.; Forrester, J.D. An update on fatalities due to venomous and nonvenomous animals in the United States (2008–2015). Wilderness Environ. Med. 2018, 29, 36–44. [Google Scholar] [CrossRef] [Green Version]
- Ferreira, R.S., Jr.; Almeida, R.A.; Barraviera, S.R.; Barraviera, B. Historical perspective and human consequences of Africanized bee stings in the Americas. J. Toxicol. Environ. Health B Crit. Rev. 2012, 15, 97–108. [Google Scholar] [CrossRef] [PubMed]
- Herrera, C.; Leza, M.; Martínez-López, E. Diversity of compounds in Vespa spp. venom and the epidemiology of its sting: A global appraisal. Arch. Toxicol. 2020, 94, 3609–3627. [Google Scholar] [CrossRef] [PubMed]
- Tanno, L.K.; Calderon, M.A.; Smith, H.E.; Sanchez-Borges, M.; Sheikh, A.; Demoly, P.; Joint Allergy Academies. Dissemination of definitions and concepts of allergic and hypersensitivity conditions. World Allergy Organ. J. 2016, 9, 24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Linard, A.T.S.; Barros, R.M.; Sousa, J.A.; Leite, R.S. Epidemiology of bee stings in Campina Grande, Paraíba state, Northeastern Brazil. J. Venom. Anim. Toxins Incl. Trop. Dis. 2014, 20, 13. [Google Scholar] [CrossRef] [Green Version]
- Golden, D.B.; Demain, J.; Freeman, T.; Graft, D.; Tankersley, M.; Tracy, J.; Blessing-Moore, J.; Bernstein, D.; Dinakar, C.; Greenhawt, M.; et al. Stinging insect hypersensitivity: A practice parameter update 2016. Ann. Allergy Asthma Immunol. 2017, 118, 28–54. [Google Scholar] [CrossRef]
- Bilò, M.B.; Bonifazi, F. The natural history and epidemiology of insect venom allergy: Clinical implications. Clin. Exp. Allergy 2009, 39, 1467–1476. [Google Scholar] [CrossRef]
- Biló, B.M.; Rueff, F.; Mosbech, H.; Bonifazi, F.; Oude-Elberink, J.N.; EAACI Interest Group on Insect Venom Hypersensitivity. Diagnosis of hymenoptera venom allergy. Allergy 2005, 60, 1339–1349. [Google Scholar] [CrossRef]
- International Statistical Classification of Diseases and Related Health Problems (Icd-10) Version: 2019. Available online: https://icd.who.int/browse10/2019/en (accessed on 11 May 2021).
- International Standard ISO 3166-1; Codes for the Representation of Names of Countries and Their Subdivisions—Part 1: Country Codes, ISO 3166-1: 2006 (E/F); International Organization on Standardization: Geneva, Switzerland, 2006; Available online: https://www.iso.org/iso-3166-country-codes.html (accessed on 11 May 2021).
- Standard Country or Area Codes for Statistical Use, Series M, No. 49 (M49), United Nations, Statistics Division, New York. Available online: https://unstats.un.org/unsd/methodology/m49/ (accessed on 11 May 2021).
- Tanno, L.K.; Ganem, F.; Demoly, P.; Toscano, C.M.; Bierrenbach, A.L. Undernotification of anaphylaxis deaths in Brazil due to difficult coding under the ICD-10. Allergy 2012, 67, 783–789. [Google Scholar] [CrossRef] [PubMed]
- Tanno, L.K.; Bierrenbach, A.L.; Simons, F.; Cardona, V.; Thong, B.Y.; Molinari, N.; Calderon, M.A.; Worm, M.; Chang, Y.S.; Papadopoulos, N.G.; et al. Critical view of anaphylaxis epidemiology: Open questions and new perspectives. Allergy Asthma Clin. Immunol. 2018, 14, 12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tanno, L.K.; Chalmers, R.J.; Calderon, M.A.; Aymé, S.; Demoly, P.; on behalf the Joint Allergy Academies. Reaching multidisciplinary consensus on classification of anaphylaxis for the eleventh revision of the World Health Organization’s (WHO) International Classification of Diseases (ICD-11). Orphanet J. Rare Dis. 2017, 12, 53. [Google Scholar] [CrossRef] [Green Version]
- Tanno, L.K.; Chalmers, R.; Jacob, R.; Kostanjsek, N.; Bierrenbach, A.L.; Martin, B.; Molinari, N.; Annesi-Maesano, I.; Papadopoulos, N.G.; Sanchez-Borges, M.; et al. Global implementation of the world health organization’s International Classification of Diseases (ICD)-11: The allergic and hypersensitivity conditions model. Allergy 2020, 75, 2206–2218. [Google Scholar] [CrossRef]
- Fung, K.W.; Xu, J.; Bodenreider, O. The new international classification of diseases 11th edition: A comparative analysis with ICD-10 and ICD-10-CM. J. Am. Med. Inform. Assoc. 2020, 27, 738–746. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, Y.; Hirata, H.; Watanabe, M.; Yoshida, N.; Yokoyama, T.; Murayama, Y.; Sugiyama, K.; Arima, M.; Fukushima, Y.; Fukuda, T.; et al. Epidemiologic investigation of hornet and paper wasp stings in forest workers and electrical facility field workers in Japan. Allergol. Int. 2014, 63, 21–26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arcangeli, G.; Traversini, V.; Tomasini, E.; Baldassarre, A.; Lecca, L.I.; Galea, R.P.; Mucci, N. Allergic anaphylactic risk in farming activities: A systematic review. Int. J. Environ. Res. Public Health 2020, 17, 4921. [Google Scholar] [CrossRef]
- Stanhope, J.; Carver, S.; Weinstein, P. Health outcomes of beekeeping: A systematic review. J. Apic. Res. 2017, 56, 100–111. [Google Scholar] [CrossRef]
- Salvati, L.; Vitiello, G.; Parronchi, P. Gender differences in anaphylaxis. Curr. Opin. Allergy Clin. Immunol. 2019, 19, 417–424. [Google Scholar] [CrossRef] [PubMed]
- Prado, M.; Quirós, D.; Lomonte, B. Mortality due to Hymenoptera stings in Costa Rica, 1985–2006. Rev. Panam. Salud Publica 2009, 25, 389–393. [Google Scholar] [CrossRef] [Green Version]
- Choi, M.B.; Kim, T.G.; Kwon, O. Recent trends in wasp nest removal and hymenoptera stings in South Korea. J. Med. Entomol. 2018, 56, 254–260. [Google Scholar] [CrossRef]
- Turner, P.J.; Gowland, M.H.; Sharma, V.; Ierodiakonou, D.; Harper, N.; Garcez, T.; Pumphrey, R.; Boyle, R.J. Increase in anaphylaxis-related hospitalizations but no increase in fatalities: An analysis of United Kingdom national anaphylaxis data, 1992–2012. J. Allergy Clin. Immunol. 2015, 135, 956–963. [Google Scholar] [CrossRef] [Green Version]
- Tan, J.W.; Campbell, D.E. Insect allergy in children. J. Paediatr. Child Health 2013, 49, 381–387. [Google Scholar] [CrossRef]
- Golden, D.B.; Kagey-Sobotka, A.; Norman, P.S.; Hamilton, R.G.; Lichtenstein, L.M. Outcomes of allergy to insect stings in children, with and without venom immunotherapy. N. Engl. J. Med. 2004, 12, 668–674. [Google Scholar] [CrossRef] [Green Version]
- Giovannini, M.; Castagnoli, R.; Mori, F.; Arasi, S.; Barni, S.; Saretta, F.; Mastrorilli, C.; Pecoraro, L.; Liotti, L.; Caminiti, L.; et al. On behalf of the Rare Allergic Diseases Commission of the Italian Society of Pediatric Allergy and Immunology. Hymenoptera venom allergy among children in Italy: Time for pediatricians to take action. Allergol. Immunopathol. 2020, 48, 804–809. [Google Scholar] [CrossRef]
- Somerville, R.; Till, D.; Leclerq, M.; Lecomte, J. Les morts par piqûre d’hyménoptères aculéates en Angleterre et au Pays de Galles (statistique pour la periode 1959–1971). Rev. Med. Liege 1975, 30, 76–78. [Google Scholar]
- Johansson, B.; Eriksson, A.; Ornehult, L. Human fatalities caused by wasp and bee stings in Sweden. Int. J. Legal Med. 1991, 104, 99–103. [Google Scholar] [CrossRef]
- Przybilla, B.; Ring, J. Diagnostik und therapie der Allergic vom Sofort-Typ gegenuber Bienen-und Wespengift. Allergologie 1985, 8, 31–39. [Google Scholar]
- Mosbech, H. Death caused by wasp and bee stings in Denmark 1960–1980. Allergy 1983, 38, 195–200. [Google Scholar] [CrossRef]
- Charpin, D.; Birnbaum, J.; Vervloet, D. Epidemiology of hymenoptera allergy. Clin. Exp. Allergy 1994, 24, 1010–1015. [Google Scholar] [CrossRef]
- Muller, U. Prophylaxe und Therapie der Insektenstichallergic. Pharma-Klinik 1985, 7, 25–28. [Google Scholar]
- Feás, X. Human fatalities caused by hornet, wasp and bee stings in spain: Epidemiology at state and sub-state level from 1999 to 2018. Biology 2021, 10, 73. [Google Scholar] [CrossRef]
- Chauzat, M.P.; Cauquil, L.; Roy, L.; Franco, S.; Hendrikx, P.; Ribière-Chabert, M. Demographics of the European apicultural industry. PLoS ONE 2013, 8, e79018. [Google Scholar] [CrossRef]
- Sumner, S.; Law, G.; Cini, A. Why we love bees and hate wasps. Ecol. Entomol. 2018, 43, 836–845. [Google Scholar] [CrossRef]
- Brock, R.E.; Cini, A.; Sumner, S. Ecosystem services provided by aculeate wasps. Biol. Rev. Camb. Philos. Soc. 2021, 96, 1645–1675. [Google Scholar] [CrossRef]
- Fernández, J. Distribution of vespid species in Europe. Curr. Opin. Allergy Clin. Immunol. 2004, 4, 319–324. [Google Scholar] [CrossRef]
- Feás Sánchez, X.; Charles, R.J. Notes on the nest architecture and colony composition in winter of the yellow-legged Asian Hornet, Vespa velutina Lepeletier 1836 (Hym.: Vespidae), in its introduced habitat in Galicia (NW Spain). Insects 2019, 10, 237. [Google Scholar] [CrossRef] [Green Version]
- Castro, L. Una nueva introducción accidental en el género Vespa Linnaeus, 1758: Vespa bicolor Fabricius, 1787 en la provincia de Málaga (España). Revta. Gad. Entom. 2019, 10, 47–56. [Google Scholar]
- Castro, L.; Arias, A.; Torralba-Burrial, A. First European records of an alien paper wasp: Polistes (Aphanilopterus) major Palisot de Beauvois, 1818 (Hymenoptera: Vespidae) in northern Spain. Zootaxa 2013, 3681, 89–92. [Google Scholar] [CrossRef]
- Hernández, R.; García-Gans, F.J.; Selfa, J.; Rueda, J. Primera cita de la avispa oriental invasora Vespa orientalis Linnaeus 1771 (Hymenoptera: Vespidae) en la Península Ibérica. Bol. SEA 2013, 52, 299–300. [Google Scholar]
- Sánchez, I.; Fajardo, M.C.; Castro, M. Primeras citas del avispón oriental Vespa orientalis Linnaeus 1771 (Hymenoptera: Vespidae) para Andalucía (España). Rev. Soc. Gad. Hist. Nat. 2019, 13, 11–14. [Google Scholar]
- Zachi, M.; Ruicănescu, A. Vespa orientalis, a new alien species in Romania. Trav. Du Muséum Natl. D’histoire Nat. Grigore Antipa 2021, 64, 67–72. [Google Scholar] [CrossRef]
- Gereys, B.; Coache, A.; Filippi, G. Présence en France métropolitaine d’un frelon allochtone: Vespa orientalis Linnaeus, 1771 (Le Frelon oriental) (Hymenoptera, Vespidae, Vespinae). Faunitaxys 2021, 9, 1–5. [Google Scholar]
- Graziani, F.; Cianferoni, F. The northernmost record of Vespa orientalis Linnaeus, 1771 (Hymenoptera: Vespidae) in peninsular Italy. Revta. Gad. Entom. 2021, 12, 173–178. [Google Scholar]
- Hammer, S.; Jensen, J.-K. The invasion of two species of social wasps (Hymenoptera, Vespidae) to the Faroe Islands. Bioinvasions Rec. 2019, 8, 558–567. [Google Scholar] [CrossRef]
- Vidal, C.; Armisén, M.; Monsalve, R.; González-Vidal, T.; Lojo, S.; López-Freire, S.; Méndez, P.; Rodríguez, V.; Romero, L.; Galán, A.; et al. Anaphylaxis to Vespa velutina nigrithorax: Pattern of sensitization for an emerging problem in Western countries. J. Investig. Allergol. Clin. Immunol. 2021, 31, 228–235. [Google Scholar] [CrossRef] [Green Version]
- Vidal, C. The Asian wasp Vespa velutina nigrithorax: Entomological and allergological characteristics. Clin. Exp. Allergy 2021, 1–10. [Google Scholar] [CrossRef]
- Feás, X.; Vidal, C.; Vázquez-Tato, M.P.; Seijas, J.A. Asian Hornet, Vespa velutina Lepeletier 1836 (Hym.: Vespidae), Venom Obtention Based on an Electric Stimulation Protocol. Molecules 2022, 27, 138. [Google Scholar] [CrossRef]
- Neill, P.E.; Arim, M. Human health link to invasive species. Encycl. Environ. Health 2011, 116–123. [Google Scholar] [CrossRef]
- Feás, X.; Vázquez-Tato, M.P.; Seijas, J.A.; Pratima, G.; Nikalje, A.; Fraga-López, F. Extraction and physicochemical characterization of chitin derived from the Asian Hornet, Vespa velutina Lepeletier 1836 (Hym.: Vespidae). Molecules 2020, 25, 384. [Google Scholar] [CrossRef] [Green Version]
- Mazza, G.; Tricarico, E.; Genovesi, P.; Gherardi, F. Biological invaders are threats to human health: An overview. Ethol. Ecol. Evol. 2014, 26, 112–129. [Google Scholar] [CrossRef]
- Pali-Schöll, I.; Roth-Walter, F.; Jensen-Jarolim, E. One health in allergology: A concept that connects humans, animals, plants, and the environment. Allergy 2021, 76, 2630–2633. [Google Scholar] [CrossRef]
- Baker, T.W.; Forester, J.P.; Johnson, M.; Stolfi, A.; Stahl, M.C. The HIT study: Hymenoptera identification test—How accurate are people at identifying stinging insects? Ann. Allergy Asthma Immunol. 2014, 113, 267–270. [Google Scholar] [CrossRef]
- Baker, T.W.; Forester, J.P.; Johnson, M.L.; Sikora, J.M.; Stolfi, A.; Stahl, M.C. Stinging insect identification: Are the allergy specialists any better than their patients? Ann. Allergy Asthma Immunol. 2016, 116, 431–434. [Google Scholar] [CrossRef]

| Country 1 | Size | Sum | Minimum | Maximum | Range | Mode | Mean | Median | Standard Deviation | Variance |
|---|---|---|---|---|---|---|---|---|---|---|
| AT | 15 | 73 | 0 | 12 | 12 | 5 | 4.87 | 5 | 3.27 | 10.7 |
| BE | 18 | 27 | 0 | 5 | 5 | 1 | 1.5 | 1 | 1.42 | 2.03 |
| BG | 9 | 26 | 1 | 6 | 5 | 2 | 2.89 | 2 | 1.62 | 2.61 |
| HR | 19 | 35 | 0 | 6 | 6 | 1 | 1.84 | 1 | 1.71 | 2.92 |
| CZ | 23 | 111 | 0 | 14 | 14 | 4 | 4.83 | 4 | 3.04 | 9.24 |
| EE | 17 | 14 | 0 | 3 | 3 | 0 | 0.82 | 1 | 1.01 | 1.03 |
| FI | 20 | 25 | 0 | 4 | 4 | 0 | 1.25 | 1 | 1.25 | 1.57 |
| FR | 15 | 211 | 9 | 23 | 14 | 14 | 14.07 | 14 | 4.15 | 17.21 |
| DE | 18 | 327 | 6 | 32 | 26 | 18 | 18.17 | 18 | 6.97 | 48.62 |
| EL | 2 | 9 | 4 | 5 | 1 | 4 & 5 | 4.5 | 4.5 | 0.71 | 0.5 |
| HU | 21 | 112 | 0 | 13 | 13 | 4 | 5.33 | 4 | 3.54 | 12.53 |
| IE | 8 | 2 | 0 | 1 | 1 | 0 | 0.25 | 0 | 0.46 | 0.21 |
| IT | 13 | 69 | 1 | 12 | 11 | 5 & 3 | 5.31 | 5 | 3.4 | 11.56 |
| LV | 9 | 9 | 0 | 2 | 2 | 2 | 1 | 1 | 1 | 1 |
| LT | 7 | 7 | 0 | 4 | 4 | 1 & 0 | 1 | 1 | 1.41 | 2 |
| LU | 7 | 1 | 0 | 1 | 1 | 0 | 0.14 | 0 | 0.38 | 0.14 |
| NL | 21 | 20 | 0 | 5 | 5 | 0 | 0.95 | 1 | 1.2 | 1.45 |
| NO | 20 | 19 | 0 | 3 | 3 | 1 | 0.95 | 1 | 0.76 | 0.58 |
| PL | 17 | 125 | 3 | 12 | 9 | 7 & 8 & 9 | 7.35 | 8 | 2.67 | 7.12 |
| PT | 13 | 9 | 0 | 4 | 4 | 0 | 0.69 | 0 | 1.32 | 1.73 |
| RO | 18 | 149 | 2 | 16 | 14 | 10 | 8.28 | 9 | 3.44 | 11.86 |
| RS | 18 | 53 | 1 | 6 | 5 | 3 | 2.94 | 3 | 1.43 | 2.06 |
| SK | 21 | 17 | 0 | 2 | 2 | 0 | 0.81 | 1 | 0.81 | 0.66 |
| SI | 19 | 21 | 0 | 4 | 4 | 0 | 1.11 | 1 | 1.37 | 1.88 |
| ES | 17 | 60 | 1 | 8 | 7 | 4 & 3 | 3.53 | 3 | 1.81 | 3.26 |
| SE | 20 | 44 | 0 | 6 | 6 | 1 | 2.2 | 2 | 1.61 | 2.59 |
| CH | 21 | 65 | 1 | 8 | 7 | 4 | 3.1 | 3 | 1.61 | 2.59 |
| UK | 15 | 51 | 1 | 7 | 6 | 2 | 3.4 | 4 | 1.84 | 3.4 |
| Items | Items | Eastern Europe 1 1994–2016 | Northern Europe 2 1996–2016 | Southern Europe 3 1995–2015 | Western Europe 4 1995–2016 | Europe 1994–2016 |
|---|---|---|---|---|---|---|
| Deaths | Total | 540 | 171 | 256 | 724 | 1691 |
| Men | 425 (78.7%) | 127 (74.3%) | 223 (87.1%) | 545 (75.3%) | 1320 (78.1%) | |
| Woman | 115 (21.3%) | 44 (25.7%) | 33 (12.9%) | 179 (24.7%) | 371 (21.9%) | |
| Ratio | X23GR | 3.7 | 2.9 | 6.8 | 3 | 3.6 |
| X23GD | 310 | 83 | 190 | 366 | 949 | |
| Age | ≤14 years | 3 (0.6%) | - | 2 (0.8%) | 3 (0.4%) | 8 (0.5%) |
| 15–24 years | 10 (1.9%) | 1 (0.6%) | 3 (1.2%) | 7 (1%) | 21 (1.2%) | |
| 25–64 years | 418 (77.4%) | 101 (59.1%) | 169 (66%) | 440 (60.8%) | 1128 (66.7%) | |
| ≥65 years | 109 (20.2%) | 55 (32.2%) | 82 (32%) | 274 (37.8%) | 520 (30.8%) | |
| Place | Not reported | 33 (6.1%) | 52 (30.4%) | 73 (28.5%) | 1 (0.1%) | 159 (9.4%) |
| X23 code extension to four-digit reported 5 | 507 (93.9%) | 119 (69.6%) | 183 (71.5%) | 723 (99.9%) | 1532 (90.6%) | |
| X23.0 (home) | 241 (44.6%) | 35 (20.5%) | 19 (7.4%) | 202 (27.9%) | 497 (29.4%) | |
| X23.1 (residential institution) | 5 (0.9%) | 1 (0.6%) | - | 2 (0.3%) | 8 (0.5%) | |
| X23.2 (school, other institution and public administrative area) | 5 (0.9%) | - | 1 (0.4%) | 1 (0.1%) | 7 (0.4%) | |
| X23.3 (sports and athletics area) | 1 (0.2%) | - | - | - | 1 (0.1%) | |
| X23.4 (street and highway) | 17 (3.1%) | 1 (0.6%) | 6 (2.3%) | 30 (4.1%) | 54 (3.2%) | |
| X23.5 (trade and service area) | - | - | - | - | - | |
| X23.6 (industrial and construction area) | 1 (0.2%) | - | - | - | 1 (0.1%) | |
| X23.7 (farm) | 18 (3.3%) | 1 (0.6%) | 6 (2.3%) | 1 (0.1%) | 26 (1.5%) | |
| X23.8 (other specified place) | 48 (8.9%) | 9 (5.3%) | 21 (8.2%) | 112 (15.5%) | 190 (11.2%) | |
| X23.9 (unspecified place) | 171 (31.7%) | 72 (42.1%) | 130 (50.8%) | 375 (51.8%) | 748 (44.2%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Feás, X.; Vidal, C.; Remesar, S. What We Know about Sting-Related Deaths? Human Fatalities Caused by Hornet, Wasp and Bee Stings in Europe (1994–2016). Biology 2022, 11, 282. https://doi.org/10.3390/biology11020282
Feás X, Vidal C, Remesar S. What We Know about Sting-Related Deaths? Human Fatalities Caused by Hornet, Wasp and Bee Stings in Europe (1994–2016). Biology. 2022; 11(2):282. https://doi.org/10.3390/biology11020282
Chicago/Turabian StyleFeás, Xesús, Carmen Vidal, and Susana Remesar. 2022. "What We Know about Sting-Related Deaths? Human Fatalities Caused by Hornet, Wasp and Bee Stings in Europe (1994–2016)" Biology 11, no. 2: 282. https://doi.org/10.3390/biology11020282






