The Metabolic Activation of Sofosbuvir Is Impaired in an Experimental Model of NAFLD
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Animal Study and Histological Analysis
2.2. Quantification of GS-331007 Plasma Concentration by HPLC-MS
2.3. Quantification of Gene Expression by Means of qRT-PCR
2.4. Quantification of Protein Expression by Western Blot
2.5. Pharmacokinetic Analysis
2.6. Statistical Analysis
3. Results
3.1. The Administration of HFHF Diet Causes Liver Steatosis in Rats and Affects Liver Function
3.2. Liver Steatosis Affects the Pharmacokinetic Parameters of GS331007
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bhattacharjee, C.; Singh, M.; Das, D.; Chaudhuri, S.; Mukhopadhyay, A. Current Therapeutics against HCV. VirusDisease 2021, 32, 228–243. [Google Scholar] [CrossRef] [PubMed]
- Bukh, J.; Miller, R.; Purcell, R. Genetic Heterogeneity of Hepatitis C Virus: Quasispecies and Genotypes. Semin. Liver Dis. 1995, 15, 41–63. [Google Scholar] [CrossRef] [PubMed]
- Abenavoli, L. Insulin Resistance and Liver Steatosis in Chronic Hepatitis C Infection Genotype 3. World J. Gastroenterol. 2014, 20, 15233. [Google Scholar] [CrossRef] [PubMed]
- Adinolfi, L.; Rinaldi, L.; Guerrera, B.; Restivo, L.; Marrone, A.; Giordano, M.; Zampino, R. NAFLD and NASH in HCV Infection: Prevalence and Significance in Hepatic and Extrahepatic Manifestations. Int. J. Mol. Sci. 2016, 17, 803. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, C.-C.; Cheng, P.-N.; Kao, J.-H. Systematic Review: Chronic Viral Hepatitis and Metabolic Derangement. Aliment. Pharmacol. Ther. 2020, 51, 216–230. [Google Scholar] [CrossRef] [PubMed]
- Palatini, P.; De Martin, S.; Pegoraro, P.; Orlando, R. Enzyme Inhibition and Induction in Liver Disease. Curr. Clin. Pharmacol. 2008, 3, 56–69. [Google Scholar] [CrossRef]
- Renaud, H.J.; Cui, J.Y.; Khan, M.; Klaassen, C.D. Tissue Distribution and Gender-Divergent Expression of 78 Cytochrome P450 MRNAs in Mice. Toxicol. Sci. 2011, 124, 261–277. [Google Scholar] [CrossRef] [Green Version]
- Donato, M.T.; Jiménez, N.; Serralta, A.; Mir, J.; Castell, J.V.; Gómez-Lechón, M.J. Effects of Steatosis on Drug-Metabolizing Capability of Primary Human Hepatocytes. Toxicol. Vitro 2007, 21, 271–276. [Google Scholar] [CrossRef]
- Dietrich, C.G.; Rau, M.; Jahn, D.; Geier, A. Changes in Drug Transport and Metabolism and Their Clinical Implications in Non-Alcoholic Fatty Liver Disease. Expert. Opin. Drug Metab. Toxicol. 2017, 13, 625–640. [Google Scholar] [CrossRef]
- Muriel, P.; López-Sánchez, P.; Ramos-Tovar, E. Fructose and the Liver. Int. J. Mol. Sci. 2021, 22, 6969. [Google Scholar] [CrossRef]
- Gabbia, D.; Roverso, M.; Guido, M.; Sacchi, D.; Scaffidi, M.; Carrara, M.; Orso, G.; Russo, F.P.; Floreani, A.; Bogialli, S.; et al. Western Diet-Induced Metabolic Alterations Affect Circulating Markers of Liver Function before the Development of Steatosis. Nutrients 2019, 11, 1602. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zarezadeh, M.; Saedisomeolia, A.; Shekarabi, M.; Khorshidi, M.; Emami, M.R.; Müller, D.J. The Effect of Obesity, Macronutrients, Fasting and Nutritional Status on Drug-Metabolizing Cytochrome P450s: A Systematic Review of Current Evidence on Human Studies. Eur. J. Nutr. 2021, 60, 2905–2921. [Google Scholar] [CrossRef] [PubMed]
- Park, H.; Wang, W.; Henry, L.; Nelson, D.R. Impact of All-Oral Direct-Acting Antivirals on Clinical and Economic Outcomes in Patients with Chronic Hepatitis C in the United States: Hepatology. Hepatology 2019, 69, 1032–1045. [Google Scholar] [CrossRef] [PubMed]
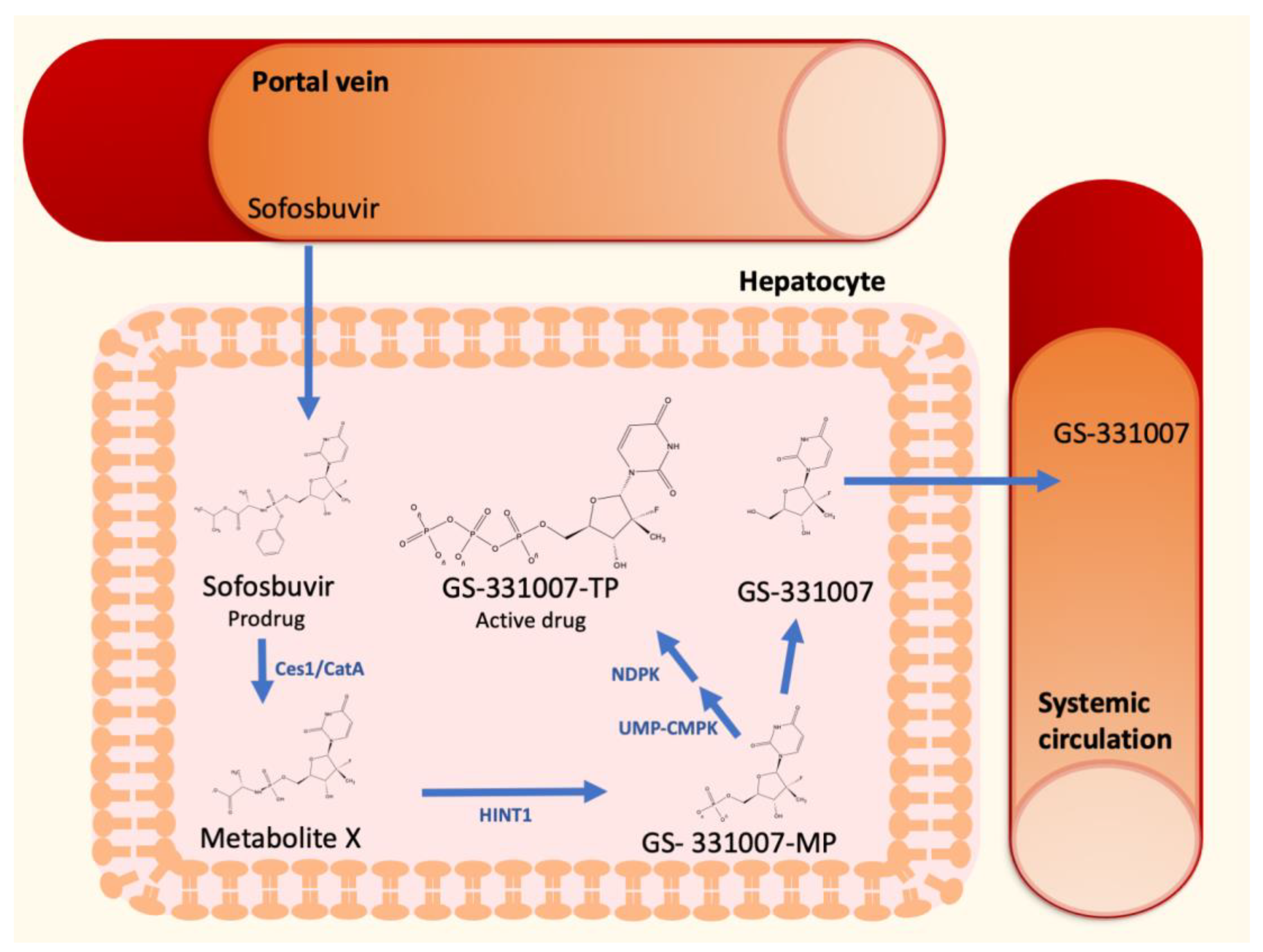
- Kirby, B.J.; Symonds, W.T.; Kearney, B.P.; Mathias, A.A. Pharmacokinetic, Pharmacodynamic, and Drug-Interaction Profile of the Hepatitis C Virus NS5B Polymerase Inhibitor Sofosbuvir. Clin. Pharmacokinet. 2015, 54, 677–690. [Google Scholar] [CrossRef]
- Lam, A.M.; Murakami, E.; Espiritu, C.; Steuer, H.M.M.; Niu, C.; Keilman, M.; Bao, H.; Zennou, V.; Bourne, N.; Julander, J.G.; et al. PSI-7851, a Pronucleotide of β-d-2′-Deoxy-2′-Fluoro-2′-C-Methyluridine Monophosphate, Is a Potent and Pan-Genotype Inhibitor of Hepatitis C Virus Replication. Antimicrob. Agents Chemother. 2010, 54, 3187–3196. [Google Scholar] [CrossRef] [Green Version]
- Jacobson, I.M.; Gordon, S.C.; Kowdley, K.V.; Yoshida, E.M.; Rodriguez-Torres, M.; Sulkowski, M.S.; Shiffman, M.L.; Lawitz, E.; Everson, G.; Bennett, M.; et al. Sofosbuvir for Hepatitis C Genotype 2 or 3 in Patients without Treatment Options. N. Engl. J. Med. 2013, 368, 1867–1877. [Google Scholar] [CrossRef] [Green Version]
- Zaiou, M.; Amrani, R.; Rihn, B.; Hajri, T. Dietary Patterns Influence Target Gene Expression through Emerging Epigenetic Mechanisms in Nonalcoholic Fatty Liver Disease. Biomedicines 2021, 9, 1256. [Google Scholar] [CrossRef]
- Gabbia, D.; Dalla Pozza, A.; Albertoni, L.; Lazzari, R.; Zigiotto, G.; Carrara, M.; Baldo, V.; Baldovin, T.; Floreani, A.; De Martin, S. Pregnane X Receptor and Constitutive Androstane Receptor Modulate Differently CYP3A-Mediated Metabolism in Early- and Late-Stage Cholestasis. World J. Gastroenterol. 2017, 23, 7519–7530. [Google Scholar] [CrossRef]
- Pfaffl, M.W. A New Mathematical Model for Relative Quantification in Real-Time RT-PCR. Nucleic Acids Res. 2001, 29, e45. [Google Scholar] [CrossRef]
- De Martin, S.; Paliuri, G.; Belloni, A.; Orso, G.; Zanarella, E.; Stellin, G.; Milanesi, O.; Basso, G.; Ruga, E.M.; Frasson, C.; et al. Expression and Distribution of the Adrenomedullin System in Newborn Human Thymus. PLoS ONE 2014, 9, e97592. [Google Scholar] [CrossRef]
- Orlando, R.; De Martin, S.; Andrighetto, L.; Floreani, M.; Palatini, P. Fluvoxamine Pharmacokinetics in Healthy Elderly Subjects and Elderly Patients with Chronic Heart Failure. Br. J. Clin. Pharmacol. 2010, 69, 279–286. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gabbia, D.; Cannella, L.; De Martin, S. The Role of Oxidative Stress in NAFLD–NASH–HCC Transition—Focus on NADPH Oxidases. Biomedicines 2021, 9, 687. [Google Scholar] [CrossRef] [PubMed]
- Renton, K.W. Regulation of Drug Metabolism and Disposition during Inflammation and Infection. Expert Opin. Drug Metab. Toxicol. 2005, 1, 629–640. [Google Scholar] [CrossRef] [PubMed]
- Stanke-Labesque, F.; Gautier-Veyret, E.; Chhun, S.; Guilhaumou, R. Inflammation Is a Major Regulator of Drug Metabolizing Enzymes and Transporters: Consequences for the Personalization of Drug Treatment. Pharmacol. Ther. 2020, 215, 107627. [Google Scholar] [CrossRef]
- Jamwal, R.; Barlock, B.J. Nonalcoholic Fatty Liver Disease (NAFLD) and Hepatic Cytochrome P450 (CYP) Enzymes. Pharmaceuticals 2020, 13, 222. [Google Scholar] [CrossRef]
- Aljomah, G.; Baker, S.S.; Liu, W.; Kozielski, R.; Oluwole, J.; Lupu, B.; Baker, R.D.; Zhu, L. Induction of CYP2E1 in Non-Alcoholic Fatty Liver Diseases. Exp. Mol. Pathol. 2015, 99, 677–681. [Google Scholar] [CrossRef] [Green Version]
- Cobbina, E.; Akhlaghi, F. Non-Alcoholic Fatty Liver Disease (NAFLD)—Pathogenesis, Classification, and Effect on Drug Metabolizing Enzymes and Transporters. Drug Metab. Rev. 2017, 49, 197–211. [Google Scholar] [CrossRef]
- Cave, M.C.; Clair, H.B.; Hardesty, J.E.; Falkner, K.C.; Feng, W.; Clark, B.J.; Sidey, J.; Shi, H.; Aqel, B.A.; McClain, C.J.; et al. Nuclear Receptors and Nonalcoholic Fatty Liver Disease. Biochim. Biophys. Acta 2016, 1859, 1083–1099. [Google Scholar] [CrossRef] [Green Version]
- Das, D.; Paul, A.; Lahiri, A.; Adak, M.; Maity, S.K.; Sarkar, A.; Paul, S.; Chakrabarti, P. Proteasome Dysfunction under Compromised Redox Metabolism Dictates Liver Injury in NASH through ASK1/PPARγ Binodal Complementary Modules. Redox Biol. 2021, 45, 102043. [Google Scholar] [CrossRef]
- Wang, T.; Babusis, D.; Park, Y.; Niu, C.; Kim, C.; Zhao, X.; Lu, B.; Ma, B.; Muench, R.C.; Sperger, D.; et al. Species Differences in Liver Accumulation and Metabolism of Nucleotide Prodrug Sofosbuvir. Drug Metab. Pharmacokinet. 2020, 35, 334–340. [Google Scholar] [CrossRef]
- Karlsen, T.H.; Sheron, N.; Zelber-Sagi, S.; Carrieri, P.; Dusheiko, G.; Bugianesi, E.; Pryke, R.; Hutchinson, S.J.; Sangro, B.; Martin, N.K.; et al. The EASL–Lancet Liver Commission: Protecting the next Generation of Europeans against Liver Disease Complications and Premature Mortality. Lancet 2022, 399, 61–116. [Google Scholar] [CrossRef]
- Pawlotsky, J.-M.; Negro, F.; Aghemo, A.; Berenguer, M.; Dalgard, O.; Dusheiko, G.; Marra, F.; Puoti, M.; Wedemeyer, H. EASL Recommendations on Treatment of Hepatitis C: Final Update of the Series. J. Hepatol. 2020, 73, 1170–1218. [Google Scholar] [CrossRef] [PubMed]



| Target | Forward | Reverse | Product Size (bp) |
|---|---|---|---|
| UMP-CMPK1 | ATGAAGCCGTTGGTCGTGT | GCAGAAAGGTGTGTGTAGCCA | 101 |
| NDPK | CGACTACACTTCTTGCTTCTGC | GGAACCCCTTCTGCTCGAAT | 128 |
| β−actin | GCCACCAGTTCGCCATGGA | TTCTGACCCATACCCACCAT | 163 |
| PK Parameter | Healthy Rats | Rats with NAFLD |
|---|---|---|
| AUC (μg × h/mL) | 199.7 ± 79.52 | 825.4 ± 141.8 |
| Cmax (μg/L) | 19.15 ± 11.18 | 136.2 ± 24.58 |
| Tmax (h) | 4 (0) | 3 (1) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gabbia, D.; Roverso, M.; Sarcognato, S.; Zanotto, I.; Ferri, N.; Russo, F.P.; Guido, M.; Bogialli, S.; De Martin, S. The Metabolic Activation of Sofosbuvir Is Impaired in an Experimental Model of NAFLD. Biology 2022, 11, 693. https://doi.org/10.3390/biology11050693
Gabbia D, Roverso M, Sarcognato S, Zanotto I, Ferri N, Russo FP, Guido M, Bogialli S, De Martin S. The Metabolic Activation of Sofosbuvir Is Impaired in an Experimental Model of NAFLD. Biology. 2022; 11(5):693. https://doi.org/10.3390/biology11050693
Chicago/Turabian StyleGabbia, Daniela, Marco Roverso, Samantha Sarcognato, Ilaria Zanotto, Nicola Ferri, Francesco Paolo Russo, Maria Guido, Sara Bogialli, and Sara De Martin. 2022. "The Metabolic Activation of Sofosbuvir Is Impaired in an Experimental Model of NAFLD" Biology 11, no. 5: 693. https://doi.org/10.3390/biology11050693
APA StyleGabbia, D., Roverso, M., Sarcognato, S., Zanotto, I., Ferri, N., Russo, F. P., Guido, M., Bogialli, S., & De Martin, S. (2022). The Metabolic Activation of Sofosbuvir Is Impaired in an Experimental Model of NAFLD. Biology, 11(5), 693. https://doi.org/10.3390/biology11050693










