Natural Peptide Toxins as an Option for Renewed Treatment of Type 2 Vasopressin Receptor-Related Diseases
Abstract
Simple Summary
Abstract
1. Introduction
2. V2R Structure and Function
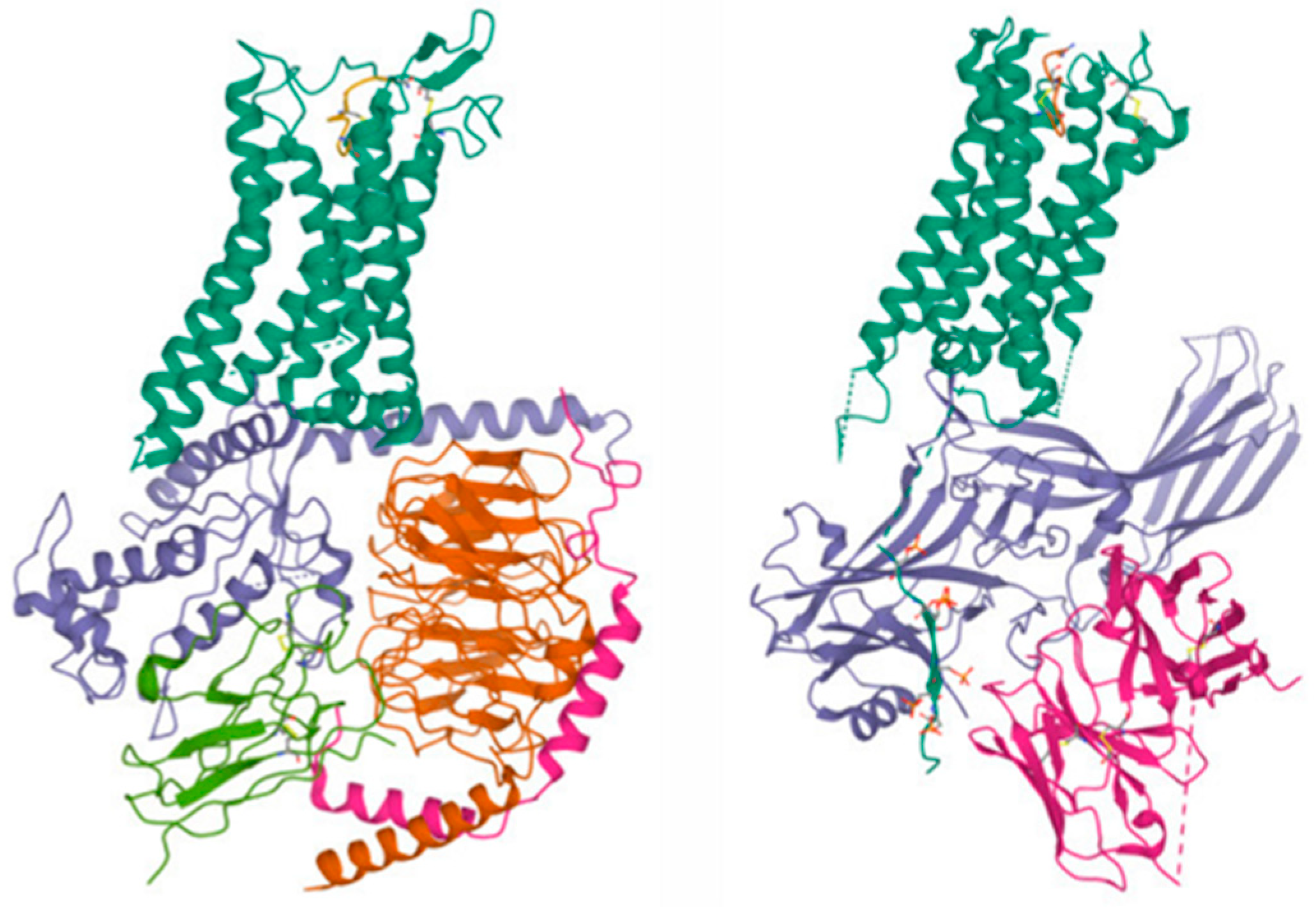
2.1. V2R Structures
2.2. V2R Natural Mutations
2.3. V2R Expression and Functions
2.4. AVP Secretion
3. V2R, an Unexploited Target, Links to Unmet Therapeutic Needs
4. Natural Peptide Toxins Targeting V2R
4.1. AVP-like Toxins
4.2. The Non-Related AVP-like Toxins
5. From a Natural Toxin to a Drug Candidate?
5.1. In Vivo Activity of MQ1
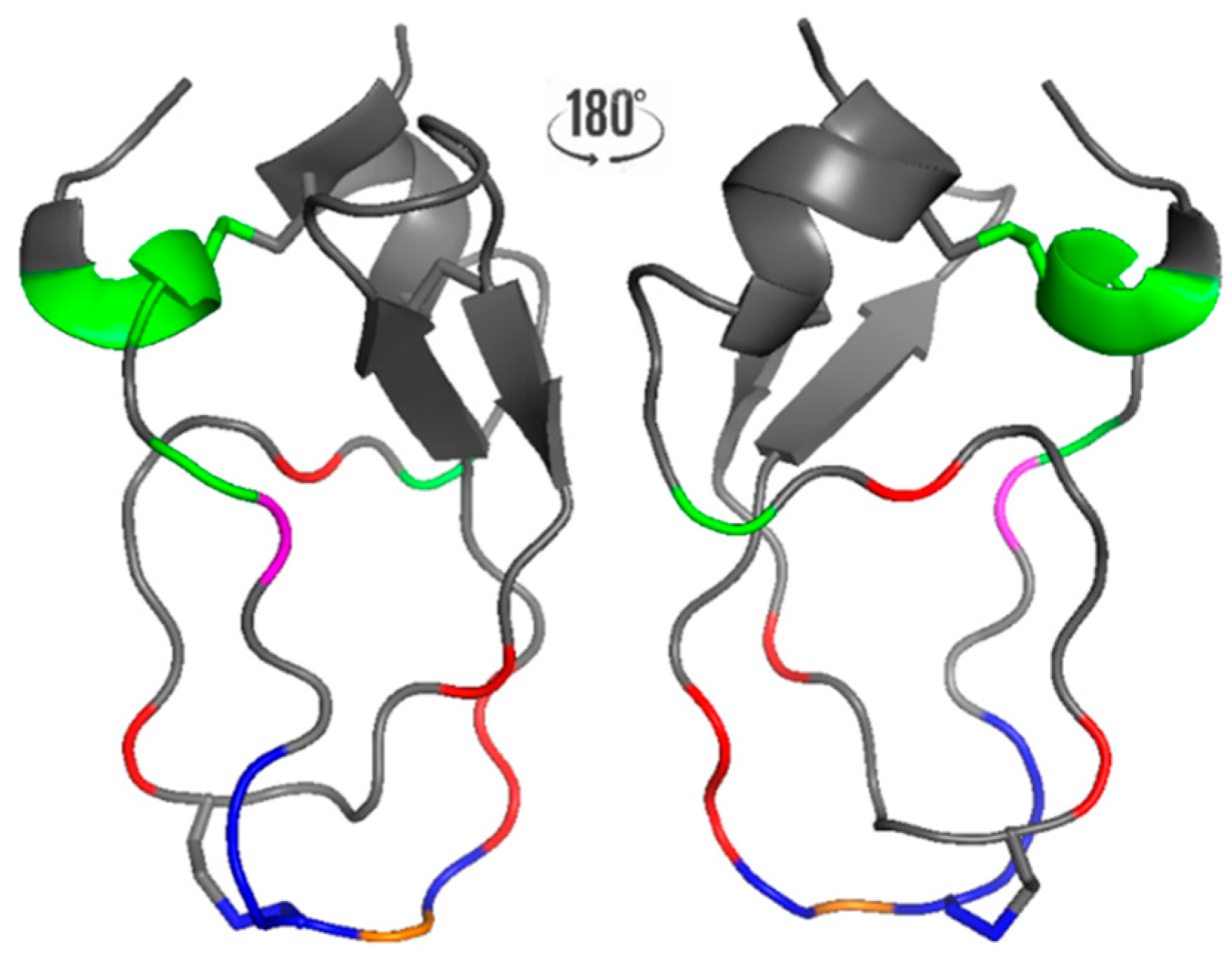
5.2. MQ1/V2R Mode of Interaction and Engineering
6. Discussion, Conclusions and Future Directions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Birnbaumer, M.; Seibold, A.; Gilbert, S.; Ishido, M.; Barberis, C.; Antaramian, A.; Brabet, P.; Rosenthal, W. Molecular Cloning of the Receptor for Human Antidiuretic Hormone. Nature 1992, 357, 333–335. [Google Scholar] [CrossRef] [PubMed]
- Bankir, L. Antidiuretic Action of Vasopressin: Quantitative Aspects and Interaction between V1a and V2 Receptor-Mediated Effects. Cardiovasc. Res. 2001, 51, 372–390. [Google Scholar] [CrossRef] [PubMed]
- Bous, J.; Fouillen, A.; Orcel, H.; Granier, S.; Bron, P.; Mouillac, B. Structures of the Arginine-Vasopressin and Oxytocin Receptor Signaling Complexes. In Vitamins and Hormones; Academic Press Inc.: Cambridge, MA, USA, 2023. [Google Scholar]
- Bous, J.; Fouillen, A.; Orcel, H.; Trapani, S.; Cong, X.; Fontanel, S.; Saint-Paul, J.; Lai-Kee-Him, J.; Urbach, S.; Sibille, N.; et al. Structure of the Vasopressin Hormone-V2 Receptor-β-Arrestin1 Ternary Complex. Sci. Adv. 2022, 8, eabo7761. [Google Scholar] [CrossRef] [PubMed]
- Bous, J.; Orcel, H.; Floquet, N.; Leyrat, C.; Lai-Kee-Him, J.; Gaibelet, G.; Ancelin, A.; Saint-Paul, J.; Trapani, S.; Louet, M.; et al. Cryo–Electron Microscopy Structure of the Antidiuretic Hormone Arginine-Vasopressin V2 Receptor Signaling Complex. Sci. Adv. 2021, 7, abg5628. [Google Scholar] [CrossRef]
- Wang, L.; Xu, J.; Cao, S.; Sun, D.; Liu, H.; Lu, Q.; Liu, Z.; Du, Y.; Zhang, C. Cryo-EM Structure of the AVP-Vasopressin Receptor 2-Gs Signaling Complex. Cell Res. 2021, 31, 932–934. [Google Scholar] [CrossRef]
- Lin, H.; Sassano, M.M.F.; Roth, B.B.L.; Shoichet, B.B.K. A Pharmacological Organization of G Protein-Coupled Receptors. Nat. Methods 2013, 10, 140–146. [Google Scholar] [CrossRef]
- Zhou, F.; Ye, C.; Ma, X.; Yin, W.; Croll, T.I.; Zhou, Q.; He, X.; Zhang, X.; Yang, D.; Wang, P.; et al. Molecular Basis of Ligand Recognition and Activation of Human V2 Vasopressin Receptor. Cell Res. 2021, 31, 929–931. [Google Scholar] [CrossRef]
- Makita, N.; Manaka, K.; Sato, J.; Iiri, T. V2 Vasopressin Receptor Mutations, 1st ed.; Elsevier Inc.: Amsterdam, The Netherlands, 2019; Volume 113. [Google Scholar]
- Ciolek, J.; Reinfrank, H.; Quinton, L.; Viengchareun, S.; Stura, E.A.; Vera, L.; Sigismeau, S.; Mouillac, B.; Orcel, H.; Peigneur, S.; et al. Green Mamba Peptide Targets Type-2 Vasopressin Receptor against Polycystic Kidney Disease. Proc. Natl. Acad. Sci. USA 2017, 114, 7154–7159. [Google Scholar] [CrossRef]
- Avet, C.; Mancini, A.; Breton, B.; Le Gouill, C.; Hauser, A.S.; Normand, C.; Kobayashi, H.; Gross, F.; Hogue, M.; Lukasheva, V.; et al. Effector Membrane Translocation Biosensors Reveal G Protein and Βarrestin Coupling Profiles of 100 Therapeutically Relevant GPCRs. Elife 2022, 11, 74101. [Google Scholar] [CrossRef]
- Inoue, A.; Raimondi, F.; Kadji, F.M.N.; Singh, G.; Kishi, T.; Uwamizu, A.; Ono, Y.; Shinjo, Y.; Ishida, S.; Arang, N.; et al. Illuminating G-Protein-Coupling Selectivity of GPCRs. Cell 2019, 177, 1933–1947.e25. [Google Scholar] [CrossRef]
- Mutig, K.; Paliege, A.; Kahl, T.; Jöns, T.; Mü Ller-Esterl, W.; Bachmann, S. Vasopressin V 2 Receptor Expression along Rat, Mouse, and Human Renal Epithelia with Focus on TAL. Am. J. Physiol. Renal. Physiol. 2007, 293, 1166–1177. [Google Scholar] [CrossRef]
- Bankir, L.; Bichet, D.G.; Bouby, N. Vasopressin V2 Receptors, ENaC, and Sodium Reabsorption: A Risk Factor for Hypertension? Am. J. Physiol. Renal. Physiol. 2010, 299, F917–F928. [Google Scholar] [CrossRef] [PubMed]
- Fenton, R.A. Essential Role of Vasopressin-Regulated Urea Transport Processes in the Mammalian Kidney. Pflugers Arch. 2009, 458, 169–177. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, S.; Chou, C.L.; Marples, D.; Christensen, E.I.; Kishore, B.K.; Knepper, M.A. Vasopressin Increases Water Permeability of Kidney Collecting Duct by Inducing Translocation of Aquaporin-CD Water Channels to Plasma Membrane. Proc. Natl. Acad. Sci. USA 1995, 92, 1013–1017. [Google Scholar] [CrossRef] [PubMed]
- Eckhard, A.; Gleiser, C.; Arnold, H.; Rask-Andersen, H.; Kumagami, H.; Müller, M.; Hirt, B.; Löwenheim, H. Water Channel Proteins in the Inner Ear and Their Link to Hearing Impairment and Deafness. Mol. Aspects Med. 2012, 33, 612–637. [Google Scholar] [CrossRef]
- Maekawa, C.; Kitahara, T.; Kizawa, K.; Okazaki, S.; Kamakura, T.; Horii, A.; Imai, T.; Doi, K.; Inohara, H.; Kiyama, H. Expression and Translocation of Aquaporin-2 in the Endolymphatic Sac in Patients with Meniere’s Disease. J. Neuroendocrinol. 2010, 22, 1157–1164. [Google Scholar] [CrossRef]
- Kitahara, T.; Doi, K.; Maekawa, C.; Kizawa, K.; Horii, A.; Kubo, T.; Kiyama, H. Meniere’s Attacks Occur in the Inner Ear with Excessive Vasopressin Type-2 Receptors. J. Neuroendocrinol. 2008, 20, 1295–1300. [Google Scholar] [CrossRef]
- Nevoux, J.; Teixeira, M.; Viengchareun, S.; Cosson, C.; Butlen, D.; Lombès, M.; Ferrary, E. Vasopressin, ATP and Catecholamines Differentially Control Potassium Secretion in Inner Ear Cell Line. FEBS Lett. 2011, 585, 2703–2708. [Google Scholar] [CrossRef]
- Tamma, R.; Sun, L.; Cuscito, C. Regulation of Bone Remodeling by Vasopressin Explains the Bone Loss in Hyponatremia. Proc. Natl. Acad. Sci. USA 2013, 110, 18644–18649. [Google Scholar] [CrossRef]
- Bardoux, P.; Bichet, D.G.; Martin, H.; Gallois, Y.; Marre, M.; Arthus, M.-F.; Lonergan, M.; Ruel, N.; Bouby, N.; Bankir, L. Vasopressin Increases Urinary Albumin Excretion in Rats and Humans: Involvement of V2 Receptors and the Renin-Angiotensin System. Nephrol. Dial. Transplant. 2003, 18, 497–506. [Google Scholar] [CrossRef]
- Kaufmann, J.E.; Oksche, A.; Wollheim, C.B.; Günther, G.; Rosenthal, W.; Vischer, U.M. Vasopressin-Induced von Willebrand Factor Secretion from Endothelial Cells Involves V2 Receptors and CAMP. J. Clin. Investig. 2000, 106, 107–116. [Google Scholar] [CrossRef] [PubMed]
- Evers, K.S.; Wellmann, S. Arginine Vasopressin and Copeptin in Perinatology. Front. Pediatr. 2016, 4, 75. [Google Scholar] [CrossRef] [PubMed]
- North, W.G.; Fay, M.J.; Du, J. MCF-7 Breast Cancer Cells Express Normal Forms of All Vasopressin Receptors plus an Abnormal V2R. Peptides 1999, 20, 837–842. [Google Scholar] [CrossRef] [PubMed]
- Ripoll, G.V.; Garona, J.; Pifano, M.; Farina, H.G.; Gomez, D.E.; Alonso, D.F. Reduction of Tumor Angiogenesis Induced by Desmopressin in a Breast Cancer Model. Breast Cancer Res. Treat. 2013, 142, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Iannucci, N.B.; Ripoll, G.V.; Garona, J.; Cascone, O.; Ciccia, G.N.; Gomez, D.E.; Alonso, D.F. Antiproliferative Effect of 1-Deamino-8-D-Arginine Vasopressin Analogs on Human Breast Cancer Cells. Future Med. Chem. 2011, 3, 1987–1993. [Google Scholar] [CrossRef]
- Garona, J.; Sobol, N.T.; Pifano, M.; Segatori, V.I.; Gomez, D.E.; Ripoll, G.V.; Alonso, D.F. Preclinical Efficacy of [V4Q5]dDAVP, a Second Generation Vasopressin Analog, on Metastatic Spread and Tumor-Associated Angiogenesis in Colorectal Cancer. Cancer Res. Treat. Off. J. Korean Cancer Assoc. 2019, 51, 438–450. [Google Scholar] [CrossRef]
- Bolignano, D.; Medici, M.A.; Coppolino, G.; Sciortino, M.T.; Merlo, F.M.; Campo, S.; Donato, V.; Venuti, A.; Sturiale, A.; Zaccaria, D.; et al. Aquaretic Inhibits Renal Cancer Proliferation: Role of Vasopressin Receptor-2 (V2-R). Urol. Oncol. Semin. Orig. Investig. 2010, 28, 642–647. [Google Scholar] [CrossRef]
- Pifano, M.; Garona, J.; Capobianco, C.S.; Gonzalez, N.; Alonso, D.F.; Ripoll, G.V. Peptide Agonists of Vasopressin V2 Receptor Reduce Expression of Neuroendocrine Markers and Tumor Growth in Human Lung and Prostate Tumor Cells. Front. Oncol. 2017, 7, 11. [Google Scholar] [CrossRef]
- Sinha, S.; Dwivedi, N.; Tao, S.; Jamadar, A.; Kakade, V.R.; Neil, M.O.; Weiss, R.H.; Enders, J.; Calvet, J.P.; Thomas, S.M.; et al. Targeting the Vasopressin Type-2 Receptor for Renal Cell Carcinoma Therapy. Oncogene 2020, 39, 1231–1245. [Google Scholar] [CrossRef]
- Droctové, L.; Lancien, M.; Tran, V.L.; Susset, M.; Jego, B.; Theodoro, F.; Kessler, P.; Mourier, G.; Robin, P.; Diarra, S.S.; et al. A Snake Toxin as a Theranostic Agent for the Type 2 Vasopressin Receptor. Theranostics 2020, 10, 11580–11594. [Google Scholar] [CrossRef]
- Giron, S.; Tejera, A.M.; Ripoll, G.V.; Gomez, D.E.; Alonso, D.F. Desmopressin Inhibits Lung and Lymph Node Metastasis in a Mouse Mammary Carcinoma Model of Surgical Manipulation. J. Surg. Oncol. 2002, 81, 38–44. [Google Scholar] [CrossRef] [PubMed]
- McKinley, M.J.; McAllen, R.M.; Davern, P.; Giles, M.E.; Penschow, J.; Sunn, N.; Uschakov, A.; Oldfield, B.J. The Sensory Circumventricular Organs of the Mammalian Brain. Adv. Anat. Embryol. Cell Biol. 2003, 172, 1–122. [Google Scholar] [CrossRef]
- Zerbe, R.L.; Robertson, G.L. Osmoregulation of Thirst and Vasopressin Secretion in Human Subjects: Effect of Various Solutes. Am. J. Physiol. 1983, 244, E607–E614. [Google Scholar] [CrossRef] [PubMed]
- Robertson, G.L. The Regulation of Vasopressin Function in Health and Disease. Recent Prog. Horm. Res. 1976, 33, 333–385. [Google Scholar] [CrossRef] [PubMed]
- Mandelblat-Cerf, Y.; Kim, A.; Burgess, C.R.; Subramanian, S.; Tannous, B.A.; Lowell, B.B.; Andermann, M.L. Bidirectional Anticipation of Future Osmotic Challenges by Vasopressin Neurons. Neuron 2017, 93, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.; Wang, T.; Oka, Y. Predicting Changes in Osmolality. Elife 2021, 10, 74551. [Google Scholar] [CrossRef] [PubMed]
- Gizowski, C.; Bourque, C.W. The Neural Basis of Homeostatic and Anticipatory Thirst. Nat. Rev. Nephrol. 2018, 14, 11–25. [Google Scholar] [CrossRef] [PubMed]
- Bichet, D.G. Regulation of Thirst and Vasopressin Release. Annu. Rev. Physiol. 2019, 81, 359–373. [Google Scholar] [CrossRef]
- Arroyo, J.P.; Terker, A.S.; Zuchowski, Y.; Watts, J.A.; Bock, F.; Meyer, C.; Luo, W.; Kapp, M.E.; Gould, E.R.; Miranda, A.X.; et al. Kidney Collecting Duct Cells Make Vasopressin in Response to NaCl-Induced Hypertonicity. CI Insight 2022, 6, e149217. [Google Scholar] [CrossRef]
- Bankir, L.; Bichet, D.G.; Morgenthaler, N.G. Vasopressin: Physiology, Assessment and Osmosensation. J. Intern. Med. 2017, 282, 284–297. [Google Scholar] [CrossRef]
- Boeckel, J.N.; Oppermann, J.; Anadol, R.; Fichtlscherer, S.; Zeiher, A.M.; Keller, T. Analyzing the Release of Copeptin from the Heart in Acute Myocardial Infarction Using a Transcoronary Gradient Model. Sci. Rep. 2016, 6, 20812. [Google Scholar] [CrossRef] [PubMed]
- Gross, A.J.; Steinberg, S.M.; Reilly, J.G.; Bliss, D.P.; Brennan, J.; Le, P.T.; Simmons, A.; Phelps, R.; Mulshine, J.L.; Ihde, D.C. Atrial Natriuretic Factor and Arginine Vasopressin Production in Tumor Cell Lines from Patients with Lung Cancer and Their Relationship to Serum Sodium. Cancer Res. 1993, 53, 67–74. [Google Scholar] [PubMed]
- Vávra, I.; Machová, A.; Holecek, V.; Cort, J.H.; Zaoral, M.; Sorm, F. Effect of a Synthetic Analogue of Vasopressin in Animals and in Patients with Diabetes Insipidus. Lancet 1968, 291, 948–952. [Google Scholar] [CrossRef] [PubMed]
- Manning, M.; Stoev, S.; Chini, B.; Durroux, T.; Mouillac, B.; Guillon, G. Peptide and Non-Peptide Agonists and Antagonists for the Vasopressin and Oxytocin V1a, V1b, V2 and OT Receptors: Research Tools and Potential Therapeutic Agents. Prog. Brain Res. 2008, 170, 473–512. [Google Scholar]
- Baumann, G.; Dingman, J.F. Distribution, Blood Transport, and Degradation of Antidiuretic Hormone in Man. J. Clin. Investig. 1976, 57, 1109–1116. [Google Scholar] [CrossRef]
- Köhler, M.; Harris, A. Pharmacokinetics and Haematological Effects of Desmopressin. Eur. J. Clin. Pharmacol. 1988, 35, 281–285. [Google Scholar] [CrossRef]
- Ellison, D.H.; Berl, T. Clinical Practice. The Syndrome of Inappropriate Antidiuresis. N. Engl. J. Med. 2007, 356, 2064–2072. [Google Scholar] [CrossRef]
- Gassanov, N.; Semmo, N.; Semmo, M.; Nia, A.M.; Fuhr, U.; Er, F. Arginine Vasopressin (AVP) and Treatment with Arginine Vasopressin Receptor Antagonists (Vaptans) in Congestive Heart Failure, Liver Cirrhosis and Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH). Eur. J. Clin. Pharmacol. 2011, 67, 333–346. [Google Scholar] [CrossRef]
- Slizgi, J.R.; Lu, Y.; Brouwer, K.R.; Claire, R.L.; Freeman, K.M.; Pan, M.; Brock, W.J.; Brouwer, K.L.R. Inhibition of Human Hepatic Bile Acid Transporters by Tolvaptan and Metabolites: Contributing Factors to Drug-Induced Liver Injury? Toxicol. Sci. 2016, 149, 237–250. [Google Scholar] [CrossRef]
- Gattone, V.H.; Wang, X.; Harris, P.C.; Torres, V.E. Inhibition of Renal Cystic Disease Development and Progression by a Vasopressin V2 Receptor Antagonist. Nat. Med. 2003, 9, 1323–1326. [Google Scholar] [CrossRef]
- Torres, V.E.; Harris, P.C. Polycystic Kidney Disease in 2011: Connecting the Dots toward a Polycystic Kidney Disease Therapy. Nat. Rev. Nephrol. 2012, 8, 66–68. [Google Scholar] [CrossRef] [PubMed]
- Gilles, N.; Servent, D. The European FP7 Venomics Project. Future Med. Chem. 2014, 6, 1611–1612. [Google Scholar] [CrossRef] [PubMed]
- Jin, A.; Muttenthaler, M.; Dutertre, S.; Himaya, S.W.A.; Kaas, Q.; Craik, D.J.; Lewis, R.J.; Alewood, P.F. Conotoxins: Chemistry and Biology. Chem. Rev. 2019, 119, 11510–11549. [Google Scholar] [CrossRef]
- Tasoulis, T.; Isbister, G.K. A Current Perspective on Snake Venom Composition and Constituent Protein Families. Arch. Toxicol. 2023, 97, 133–153. [Google Scholar] [CrossRef] [PubMed]
- Muiruri, P.K.; Zhong, J.; Yao, B.; Lai, R.; Luo, L. Bioactive Peptides from Scorpion Venoms: Therapeutic Scaffolds and Pharmacological Tools. Chin. J. Nat. Med. 2023, 21, 19–35. [Google Scholar]
- Lüddecke, T.; Herzig, V.; von Reumont, B.M.; Vilcinskas, A. The Biology and Evolution of Spider Venoms. Biol. Rev. 2022, 97, 163–178. [Google Scholar] [CrossRef]
- Han, Y.; Kamau, P.M.; Lai, R.; Luo, L. Bioactive Peptides and Proteins from Centipede Venoms. Molecules 2022, 27, 4423. [Google Scholar] [CrossRef]
- Madio, B.; King, G.F.; Undheim, E.A.B. Sea Anemone Toxins: A Structural Overview. Mar. Drugs 2019, 17, 325. [Google Scholar] [CrossRef]
- van Baelen, A.-C.; Robin, P.; Kessler, P.; Maïga, A.; Gilles, N.; Servent, D. Structural and Functional Diversity of Animal Toxins Interacting with GPCRs. Front. Mol. Biosci. 2022, 9, 811365. [Google Scholar] [CrossRef]
- Cruz, L.J.; de Santos, V.; Zafaralla, G.C.; Ramilo, C.A.; Zeikus, R.; Gray, W.R.; Olivera, B.M. Invertebrate Vasopressin/Oxytocin Homologs. Characterization of Peptides from Conus Geographus and Conus Straitus Venoms. J. Biol. Chem. 1987, 262, 15821–15824. [Google Scholar] [CrossRef]
- Manning, M.; Misicka, A.; Olma, A.; Bankowski, K.; Stoev, S.; Chini, B.; Durroux, T.; Mouillac, B.; Corbani, M.; Guillon, G. Oxytocin and Vasopressin Agonists and Antagonists as Research Tools and Potential Therapeutics. J. Neuroendocrinol. 2012, 24, 609–628. [Google Scholar] [CrossRef]
- Giribaldi, J.; Ragnarsson, L.; Pujante, T.; Enjalbal, C.; Wilson, D.; Daly, N.L.; Lewis, R.J.; Dutertre, S. Synthesis, Pharmacological and Structural Characterization of Novel Conopressins from Conus Miliaris. Mar. Drugs 2020, 18, 150. [Google Scholar] [CrossRef] [PubMed]
- Dutertre, S.; Croker, D.; Daly, N.L.; Andersson, A.; Muttenthaler, M.; Lumsden, N.G.; Craik, D.J.; Alewood, P.F.; Guillon, G.; Lewis, R.J. Conopressin-T from Conus Tulipa Reveals an Antagonist Switch in Vasopressin-like Peptides. J. Biol. Chem. 2008, 283, 7100–7108. [Google Scholar] [CrossRef] [PubMed]
- Möller, C.; Marí, F. A Vasopressin/Oxytocin-Related Conopeptide with γ-Carboxyglutamate at Position 8. Biochem. J. 2007, 404, 413–419. [Google Scholar] [CrossRef]
- Kunitz, M.; Northrop, J.H. Isolation from Beef Pancreas of Crystalline Trypsinogen, Trypsin, a Trypsin Inhibitor, and an Inhibitor-Trypsin Compound. J. Gen. Physiol. 1936, 19, 991–1007. [Google Scholar] [CrossRef]
- Harvey, A.L. Twenty Years of Dendrotoxins. Toxicon 2001, 39, 15–26. [Google Scholar] [CrossRef] [PubMed]
- Droctové, L.; Ciolek, J.; Mendre, C.; Chorfa, A.; Huerta, P.; Carvalho, C.; Gouin, C.; Lancien, M.; Stanajic-Petrovic, G.; Braco, L.; et al. A New Kunitz-type Snake Toxin Family Associated with an Original Mode of Interaction with the Vasopressin 2 Receptor. Br. J. Pharmacol. 2022, 179, 3470–3481. [Google Scholar] [CrossRef] [PubMed]
- Nagao, S.; Kugita, M.; Yoshihara, D.; Yamaguchi, T. Animal Models for Human Polycystic Kidney Disease. Exp. Anim. 2012, 61, 477–488. [Google Scholar] [CrossRef]
- Harper, E.; Berger, A. On the Size of the Active Site in Proteases: I. Papain. Biochem. Biophys. Res. Commun. 1967, 27, 157–162. [Google Scholar] [CrossRef]
- Otlewski, J.; Jaskólski, M.; Buczek, O.; Cierpicki, T.; Czapińska, H.; Krowarsch, D.; Smalas, A.O.; Stachowiak, D.; Szpineta, A.; Dadlez, M. Structure-Function Relationship of Serine Protease-Protein Inhibitor Interaction. Acta Biochim. Pol. 2001, 48, 419–428. [Google Scholar] [CrossRef]
- Danse, J.M.; Rowan, E.G.; Gasparini, S.; Ducancel, F.; Vatanpour, H.; Young, L.C.; Poorheidari, G.; Lajeunesse, E.; Drevet, P.; Ménez, R. On the Site by Which Alpha-Dendrotoxin Binds to Voltage-Dependent Potassium Channels: Site-Directed Mutagenesis Reveals That the Lysine Triplet 28-30 Is Not Essential for Binding. FEBS Lett. 1994, 356, 153–158. [Google Scholar] [CrossRef] [PubMed]
- Gasparini, S.; Danse, J.M.; Lecoq, A.; Pinkasfeld, S.; Zinn-Justin, S.; Young, L.C.; de Medeiros, C.C.L.; Rowan, E.G.; Harvey, A.L.; Ménez, A. Delineation of the Functional Site of α-Dendrotoxin: The Functional Topographies of Dendrotoxins Are Different but Share a Conserved Core with Those of Other Kv1 Potassium Channel-Blocking Toxins. J. Biol. Chem. 1998, 273, 25393–25403. [Google Scholar] [CrossRef] [PubMed]
- Newman, D.J.; Cragg, G.M. Natural Products as Sources of New Drugs from 1981 to 2014. J. Nat. Prod. 2016, 79, 629–661. [Google Scholar] [CrossRef]
- Furman, B.L. The Development of Byetta (Exenatide) from the Venom of the Gila Monster as an Anti-Diabetic Agent. Toxicon 2012, 59, 464–471. [Google Scholar] [CrossRef]
- Bea, I.; Ramiro, L.; Bjørn-Yoshimoto, W.E.; Imperial, J.S.; Gajewiak, J.; Salcedo, P.F.; Watkins, M.; Taylor, D.; Resager, W.; Ueberheide, B.; et al. Somatostatin Venom Analogs Evolved by Fish-Hunting Cone Snails: From Prey Capture Behavior to Identifying Drug Leads. Sci. Adv. 2022, 8, eabk1410. [Google Scholar]
- Møller, L.N.; Stidsen, C.E.; Hartmann, B.; Holst, J.J. Somatostatin Receptors. Biochim. Biophys. Acta Biomembr. 2003, 1616, 1–84. [Google Scholar] [CrossRef] [PubMed]
- Lipinski, C.A. Rule of Five in 2015 and beyond: Target and Ligand Structural Limitations, Ligand Chemistry Structure and Drug Discovery Project Decisions. Adv. Drug. Deliv. Rev. 2016, 101, 34–41. [Google Scholar] [CrossRef]
- Ciolek, J.; Zoukimian, C.; Dhot, J.; Burban, M.; Triquigneaux, M.; Lauzier, B.; Guimbert, C.; Boturyn, D.; Ferron, M.; Ciccone, L.; et al. MT9, a Natural Peptide from Black Mamba Venom Antagonizes the Muscarinic Type 2 Receptor and Reverses the M2R-Agonist-Induced Relaxation in Rat and Human Arteries. Biomed. Pharmacother. 2022, 150, 113094. [Google Scholar] [CrossRef]
- Reynaud, S.; Laurin, S.A.; Ciolek, J.; Barbe, P.; van Baelen, A.C.; Susset, M.; Blondel, F.; Ghazarian, M.; Boeri, J.; vanden Driessche, M.; et al. From a Cone Snail Toxin to a Competitive MC4R Antagonist. J. Med. Chem. 2022, 65, 12084–12094. [Google Scholar] [CrossRef] [PubMed]
- Reynaud, S.; Ciolek, J.; Degueldre, M.; Saez, N.J.; Sequeira, A.F.; Duhoo, Y.; Brás, J.L.A.; Meudal, H.; Cabo Díez, M.; Fernández Pedrosa, V.; et al. A Venomics Approach Coupled to High-Throughput Toxin Production Strategies Identifies the First Venom-Derived Melanocortin Receptor Agonists. J. Med. Chem. 2020, 63, 8250–8264. [Google Scholar] [CrossRef]
- Van Baelen, A.-C.; Iturrioz, X.; Chaigneau, M.; Kessler, P.; Llorens-Cortes, C.; Servent, D.; Gilles, N.; Robin, P. Characterization of the First Animal Toxin Acting as an Antagonist on AT1 Receptor. Int. J. Mol. Sci. 2023, 24, 2330. [Google Scholar] [CrossRef] [PubMed]
| Peptide | V2R | |||||
|---|---|---|---|---|---|---|
| Name | Sequence | id% | Affinity | Function | ||
| AVP | CYFQNCPRG * | 100 | ||||
| Ba1 | CYITNCORG * | 70 | ND | ND | ||
| Ba3 | CFIRNCPRG * | 70 | ND | ND | ||
| S | CIIRNCPRG * | 70 | >10 µM (1) | |||
| T | CYIQNCLRV * | 70 | >10 µM (1) | |||
| G | CFIRNCPKG * | 70 | 299.2 nM (2) | agonist (2) | ||
| M | CFIRNCPEG * | 60 | ND | ND | ||
| Vil | CLIQDCP(Gla)G | 50 | ND | ND (3) | ||
| M1 | CFPGNCPDS * | 50 | >100 µM (2) | |||
| M2 | CFLGNCPDS * | 50 | >100 µM (2) | |||
| Ba2 | CFLGNCLND * | 40 | ND | ND | ||
| Ml1 | CFPGNCPDS | 40 | >100 µM (2) | |||
| Cn | CYIRDCPE- * | 40 | ND | ND | ||
| Tx | CFIRNCPO | 40 | ND | ND | ||
| Ml2 | CFLGNCPDS | 40 | >100 µM (2) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gilles, N. Natural Peptide Toxins as an Option for Renewed Treatment of Type 2 Vasopressin Receptor-Related Diseases. Biology 2023, 12, 544. https://doi.org/10.3390/biology12040544
Gilles N. Natural Peptide Toxins as an Option for Renewed Treatment of Type 2 Vasopressin Receptor-Related Diseases. Biology. 2023; 12(4):544. https://doi.org/10.3390/biology12040544
Chicago/Turabian StyleGilles, Nicolas. 2023. "Natural Peptide Toxins as an Option for Renewed Treatment of Type 2 Vasopressin Receptor-Related Diseases" Biology 12, no. 4: 544. https://doi.org/10.3390/biology12040544
APA StyleGilles, N. (2023). Natural Peptide Toxins as an Option for Renewed Treatment of Type 2 Vasopressin Receptor-Related Diseases. Biology, 12(4), 544. https://doi.org/10.3390/biology12040544





