Uncovering a Causal Connection between Gut Microbiota and Six Thyroid Diseases: A Two-Sample Mendelian Randomization Study
Abstract
:Simple Summary
Abstract
1. Introduction
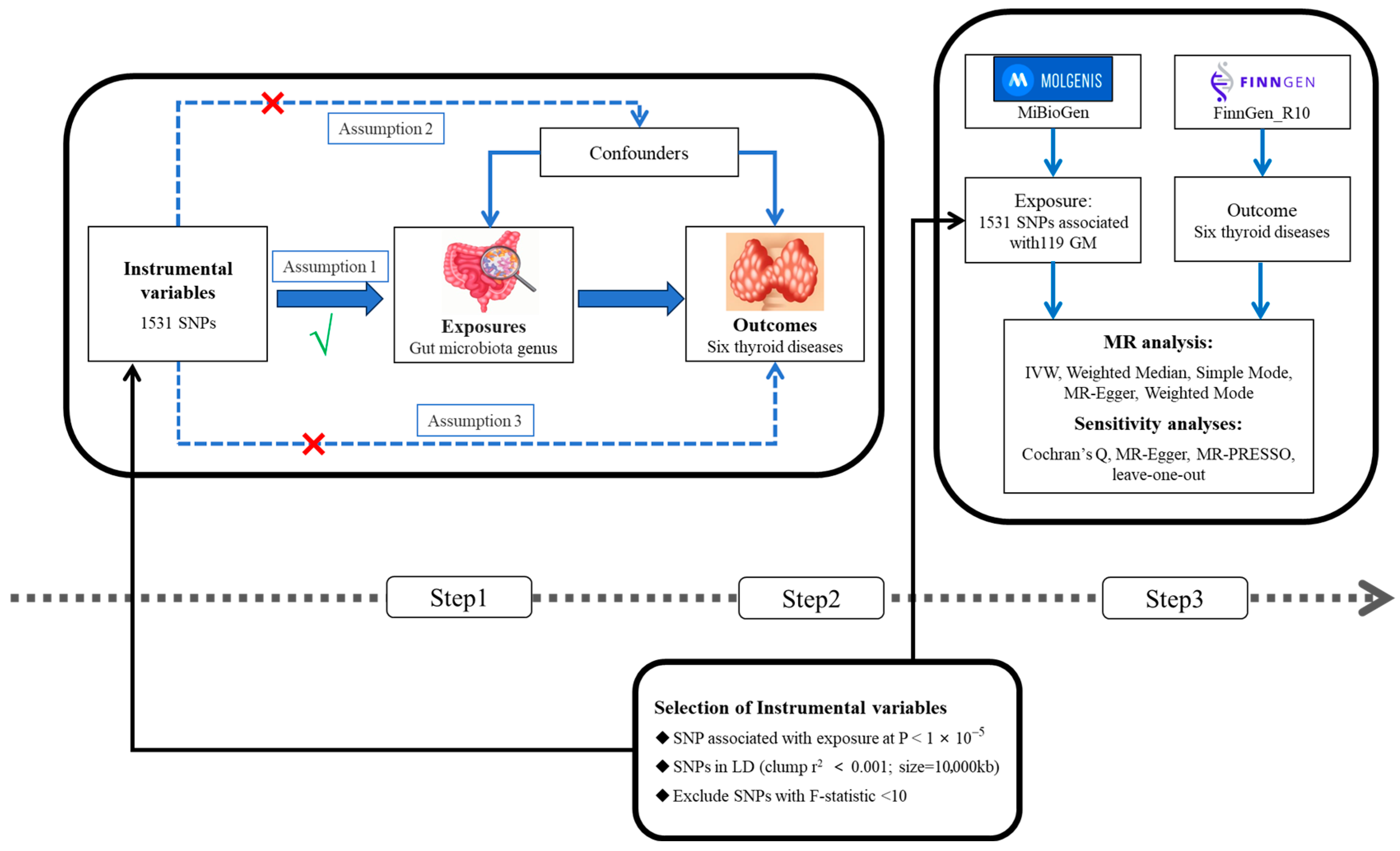
2. Materials and Methods
2.1. Study Overview
2.2. Data Sources
2.3. Selection of Instrumental Variables
2.4. Mendelian Randomization Analysis and Sensitivity Analysis
3. Results
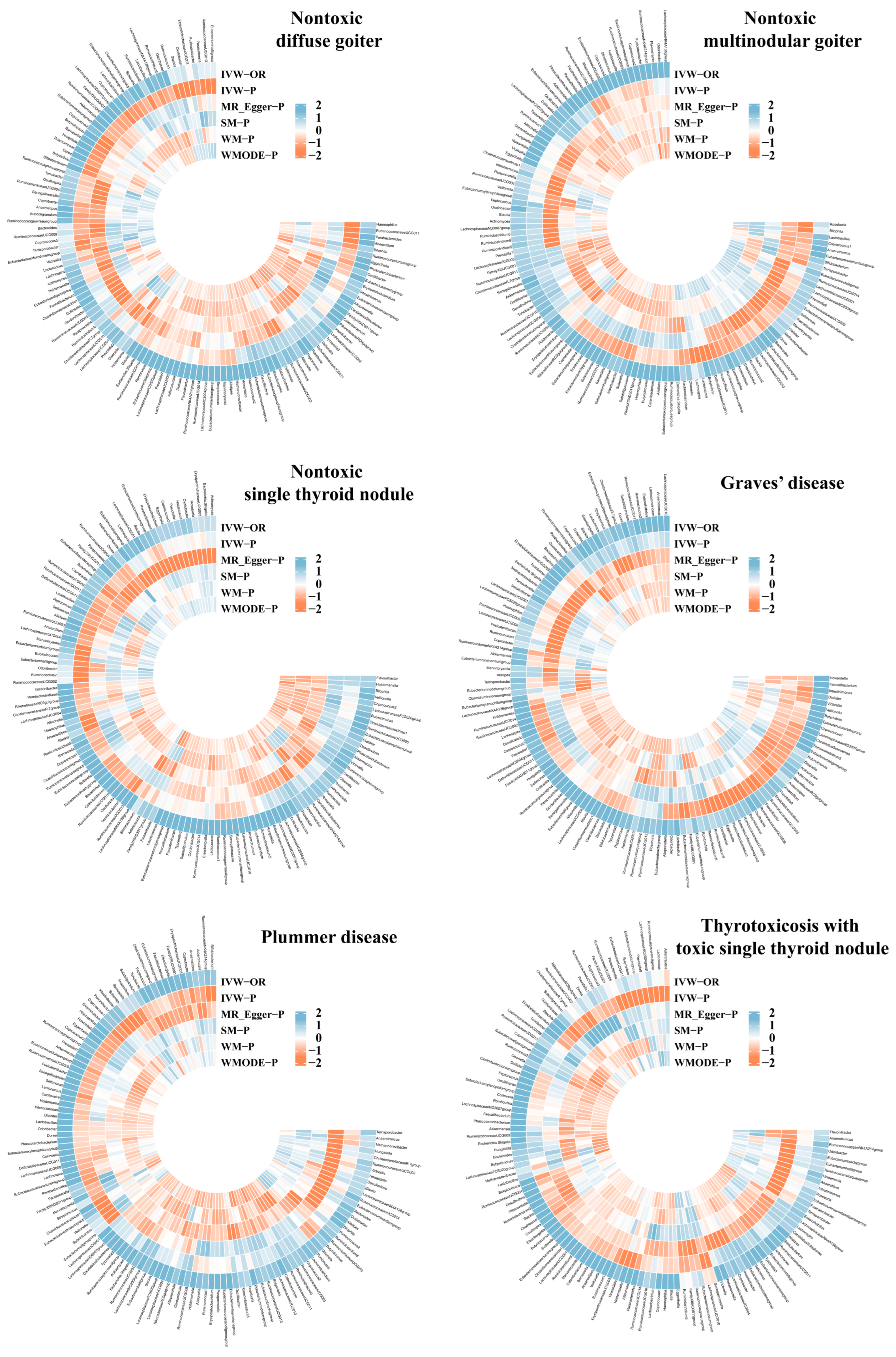
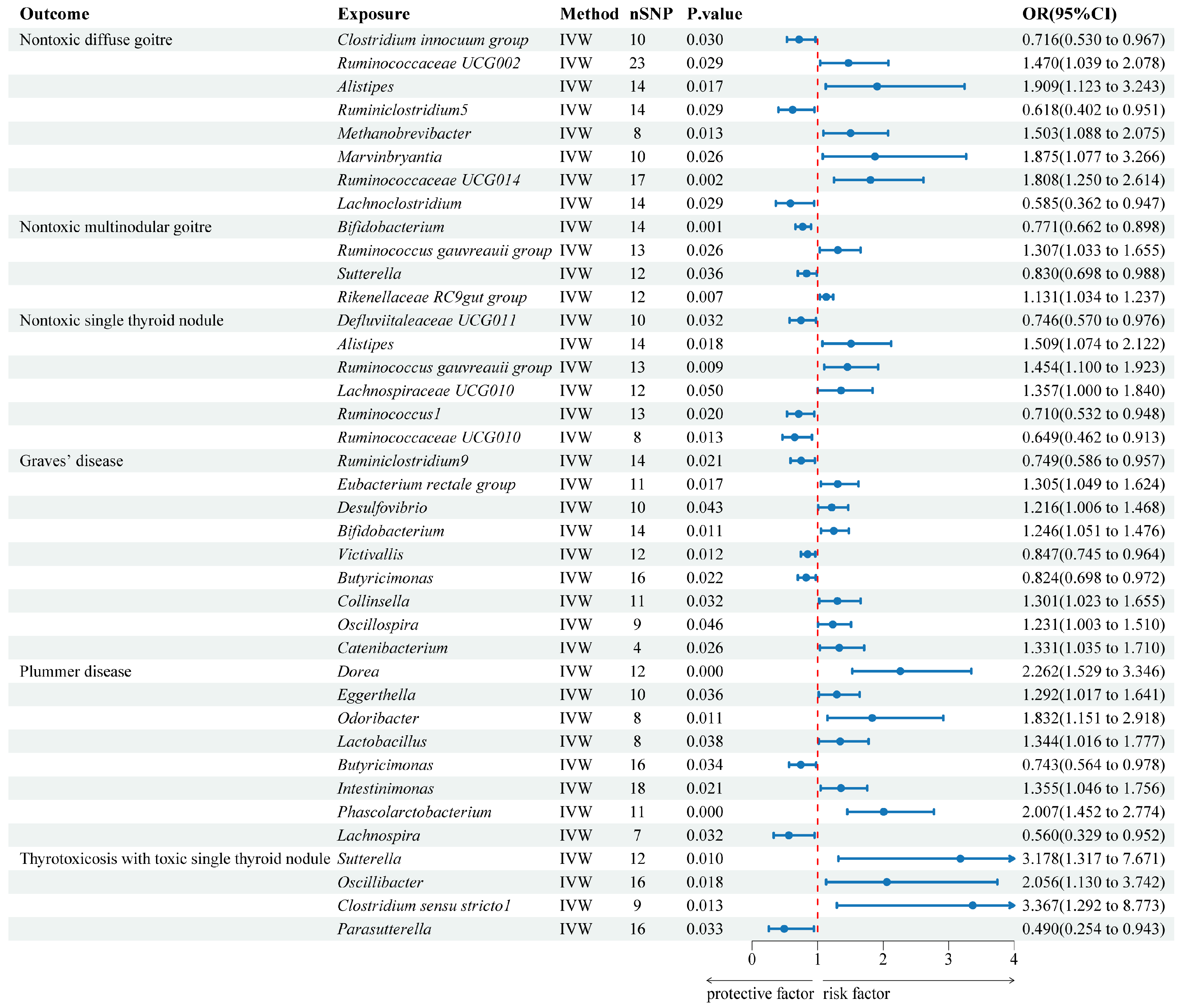
3.1. Instrumental Variables and Mendelian Randomization Results
3.2. Causal Relationships between Gut Microbiota and Thyroid Diseases
3.3. Sensitivity Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lisco, G.; De Tullio, A.; Triggiani, D.; Zupo, R.; Giagulli, V.A.; De Pergola, G.; Piazzolla, G.; Guastamacchia, E.; Sabbà, C.; Triggiani, V. Iodine Deficiency and Iodine Prophylaxis: An Overview and Update. Nutrients 2023, 15, 1004. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, M.B.; Boelaert, K. Iodine Deficiency and Thyroid Disorders. Lancet Diabetes Endocrinol. 2015, 3, 286–295. [Google Scholar] [CrossRef] [PubMed]
- Kawicka, A.; Regulska-Ilow, B.; Regulska-Ilow, B. Metabolic Disorders and Nutritional Status in Autoimmune Thyroid Diseases. Adv. Hyg. Exp. Med. 2015, 69, 80–90. [Google Scholar] [CrossRef] [PubMed]
- Ludgate, M.E.; Masetti, G.; Soares, P. The Relationship between the Gut Microbiota and Thyroid Disorders. Nat. Rev. Endocrinol. 2024, 20, 511–525. [Google Scholar] [CrossRef] [PubMed]
- Mendoza-León, M.J.; Mangalam, A.K.; Regaldiz, A.; González-Madrid, E.; Rangel-Ramírez, M.A.; Álvarez-Mardonez, O.; Vallejos, O.P.; Méndez, C.; Bueno, S.M.; Melo-González, F.; et al. Gut Microbiota Short-Chain Fatty Acids and Their Impact on the Host Thyroid Function and Diseases. Front. Endocrinol. 2023, 14, 1192216. [Google Scholar] [CrossRef]
- Chen, Y.; Zhou, J.; Wang, L. Role and Mechanism of Gut Microbiota in Human Disease. Front. Cell. Infect. Microbiol. 2021, 11, 625913. [Google Scholar] [CrossRef]
- Zhu, Y.; Yang, Q.; Yang, Q.; He, Y.; Zhou, W. Intestinal Microbes and Hematological Malignancies. Cancers 2023, 15, 2284. [Google Scholar] [CrossRef]
- Lerner, A.; Jeremias, P.; Matthias, T. Gut-Thyroid Axis and Celiac Disease. Endocr. Connect. 2017, 6, R52–R58. [Google Scholar] [CrossRef]
- Jiang, W.; Lu, G.; Gao, D.; Lv, Z.; Li, D. The Relationships between the Gut Microbiota and Its Metabolites with Thyroid Diseases. Front. Endocrinol. 2022, 13, 943408. [Google Scholar] [CrossRef]
- Venkatesh, S.S.; Ferreira, T.; Benonisdottir, S.; Rahmioglu, N.; Becker, C.M.; Granne, I.; Zondervan, K.T.; Holmes, M.V.; Lindgren, C.M.; Wittemans, L.B.L. Obesity and Risk of Female Reproductive Conditions: A Mendelian Randomisation Study. PLoS Med. 2022, 19, e1003679. [Google Scholar] [CrossRef]
- Hou, T.; Wang, Q.; Dai, H.; Hou, Y.; Zheng, J.; Wang, T.; Lin, H.; Wang, S.; Li, M.; Zhao, Z.; et al. Interactive Association between Gut Microbiota and Thyroid Cancer. Endocrinology 2023, 165, bqad184. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Wu, M.; Pan, Y.; Wang, Q.; Zhang, L.; Tang, F.; Lu, B.; Zhong, S. Causal Relationships between Gut Microbiota and Hypothyroidism: A Mendelian Randomization Study. Endocrine 2024, 83, 708–718. [Google Scholar] [CrossRef] [PubMed]
- Xiong, Y.; Zhu, X.; Luo, Q. Causal Relationship between Gut Microbiota and Autoimmune Thyroiditis: A Mendelian Study. Heliyon 2024, 10, e25652. [Google Scholar] [CrossRef]
- VanderWeele, T.J.; Tchetgen Tchetgen, E.J.; Cornelis, M.; Kraft, P. Methodological Challenges in Mendelian Randomization. Epidemiology 2014, 25, 427–435. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Xu, H.; Zhao, Z.; Dong, Y.; Wang, X.; Niu, J. No Evidence for a Causal Link between Helicobacter Pylori Infection and Nonalcoholic Fatty Liver Disease: A Bidirectional Mendelian Randomization Study. Front. Microbiol. 2022, 13, 1018322. [Google Scholar] [CrossRef]
- Kurilshikov, A.; Medina-Gomez, C.; Bacigalupe, R.; Radjabzadeh, D.; Wang, J.; Demirkan, A.; Le Roy, C.I.; Raygoza Garay, J.A.; Finnicum, C.T.; Liu, X.; et al. Large-Scale Association Analyses Identify Host Factors Influencing Human Gut Microbiome Composition. Nat. Genet. 2021, 53, 156–165. [Google Scholar] [CrossRef]
- Xia, D.; Wang, J.; Zhao, X.; Shen, T.; Ling, L.; Liang, Y. Association between Gut Microbiota and Benign Prostatic Hyperplasia: A Two-Sample Mendelian Randomization Study. Front. Cell. Infect. Microbiol. 2023, 13, 1248381. [Google Scholar] [CrossRef]
- Kurki, M.I.; Karjalainen, J.; Palta, P.; Sipilä, T.P.; Kristiansson, K.; Donner, K.M.; Reeve, M.P.; Laivuori, H.; Aavikko, M.; Kaunisto, M.A.; et al. FinnGen Provides Genetic Insights from a Well-Phenotyped Isolated Population. Nature 2023, 613, 508–518. [Google Scholar] [CrossRef]
- Chen, S.; Zhou, G.; Han, H.; Jin, J.; Li, Z. Causal Effects of Specific Gut Microbiota on Bone Mineral Density: A Two-Sample Mendelian Randomization Study. Front. Endocrinol. 2023, 14, 1178831. [Google Scholar] [CrossRef]
- Lee, C.H.; Cook, S.; Lee, J.S.; Han, B. Comparison of Two Meta-Analysis Methods: Inverse-Variance-Weighted Average and Weighted Sum of Z-Scores. Genom. Inform. 2016, 14, 173–180. [Google Scholar] [CrossRef]
- Yao, H.; Chen, J.; Wang, Y.; Li, Y.; Jiang, Q. Assessing Causal Relationships between Gut Microbiota and Abortion: Evidence from Two Sample Mendelian Randomization Analysis. Front. Endocrinol. 2024, 15, 1415730. [Google Scholar] [CrossRef] [PubMed]
- Yao, Y.; Hu, H.; Chen, L.; Zheng, H. Association between Gut Microbiota and Menstrual Disorders: A Two-Sample Mendelian Randomization Study. Front. Microbiol. 2024, 15, 1321268. [Google Scholar] [CrossRef] [PubMed]
- Jiang, W.; Yu, X.; Kosik, R.O.; Song, Y.; Qiao, T.; Tong, J.; Liu, S.; Fan, S.; Luo, Q.; Chai, L.; et al. Gut Microbiota May Play a Significant Role in the Pathogenesis of Graves’ Disease. Thyroid 2021, 31, 810–820. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; Sun, W.; Zhang, H. Interaction of Gut Microbiota with Endocrine Homeostasis and Thyroid Cancer. Cancers 2022, 14, 2656. [Google Scholar] [CrossRef]
- Ejtahed, H.-S.; Angoorani, P.; Soroush, A.-R.; Siadat, S.-D.; Shirzad, N.; Hasani-Ranjbar, S.; Larijani, B. Our Little Friends with Big Roles: Alterations of the Gut Microbiota in Thyroid Disorders. Endocr. Metab. Immune Disord. Drug Targets 2020, 20, 344–350. [Google Scholar] [CrossRef]
- Zhang, L.; Zi, L.; Kuang, T.; Wang, K.; Qiu, Z.; Wu, Z.; Liu, L.; Liu, R.; Wang, P.; Wang, W. Investigating Causal Associations among Gut Microbiota, Metabolites, and Liver Diseases: A Mendelian Randomization Study. Front. Endocrinol. 2023, 14, 1159148. [Google Scholar] [CrossRef]
- Gong, B.; Wang, C.; Meng, F.; Wang, H.; Song, B.; Yang, Y.; Shan, Z. Association Between Gut Microbiota and Autoimmune Thyroid Disease: A Systematic Review and Meta-Analysis. Front. Endocrinol. 2021, 12, 774362. [Google Scholar] [CrossRef]
- Arpaia, N.; Campbell, C.; Fan, X.; Dikiy, S.; van der Veeken, J.; deRoos, P.; Liu, H.; Cross, J.R.; Pfeffer, K.; Coffer, P.J.; et al. Metabolites Produced by Commensal Bacteria Promote Peripheral Regulatory T-Cell Generation. Nature 2013, 504, 451–455. [Google Scholar] [CrossRef]
- Furusawa, Y.; Obata, Y.; Fukuda, S.; Endo, T.A.; Nakato, G.; Takahashi, D.; Nakanishi, Y.; Uetake, C.; Kato, K.; Kato, T.; et al. Commensal Microbe-Derived Butyrate Induces the Differentiation of Colonic Regulatory T Cells. Nature 2013, 504, 446–450. [Google Scholar] [CrossRef]
- Chang, S.-C.; Lin, S.-F.; Chen, S.-T.; Chang, P.-Y.; Yeh, Y.-M.; Lo, F.-S.; Lu, J.-J. Alterations of Gut Microbiota in Patients with Graves’ Disease. Front. Cell. Infect. Microbiol. 2021, 11, 663131. [Google Scholar] [CrossRef]
- Huo, D.; Cen, C.; Chang, H.; Ou, Q.; Jiang, S.; Pan, Y.; Chen, K.; Zhang, J. Probiotic Bifidobacterium Longum Supplied with Methimazole Improved the Thyroid Function of Graves’ Disease Patients through the Gut-Thyroid Axis. Commun. Biol. 2021, 4, 1046. [Google Scholar] [CrossRef] [PubMed]
- Dai, W.; Cai, D.; Zhou, S.; Li, A.; Xie, J.; Zhang, J. Uncovering a Causal Connection between the Lachnoclostridium Genus in Fecal Microbiota and Non-Alcoholic Fatty Liver Disease: A Two-Sample Mendelian Randomization Analysis. Front. Microbiol. 2023, 14, 1276790. [Google Scholar] [CrossRef] [PubMed]
- Hiippala, K.; Kainulainen, V.; Kalliomäki, M.; Arkkila, P.; Satokari, R. Mucosal Prevalence and Interactions with the Epithelium Indicate Commensalism of Sutterella spp. Front. Microbiol. 2016, 7, 1706. [Google Scholar] [CrossRef] [PubMed]
- Legakis, I.; Chrousos, G.P.; Chatzipanagiotou, S. Thyroid Diseases and Intestinal Microbiome. Horm. Metab. Res. 2023, 55, 813–818. [Google Scholar] [CrossRef] [PubMed]
- Barczyński, M. Current Approach to Surgical Management of Hyperthyroidism. Q. J. Nucl. Med. Mol. Imaging 2021, 65, 124–131. [Google Scholar] [CrossRef]
- Smith, T.J.; Hegedüs, L. Graves’ Disease. N. Engl. J. Med. 2016, 375, 1552–1565. [Google Scholar] [CrossRef]
- Zhang, J.; Zhang, F.; Zhao, C.; Xu, Q.; Liang, C.; Yang, Y.; Wang, H.; Shang, Y.; Wang, Y.; Mu, X.; et al. Dysbiosis of the Gut Microbiome Is Associated with Thyroid Cancer and Thyroid Nodules and Correlated with Clinical Index of Thyroid Function. Endocrine 2019, 64, 564–574. [Google Scholar] [CrossRef]
- Khakisahneh, S.; Zhang, X.-Y.; Nouri, Z.; Wang, D.-H. Cecal Microbial Transplantation Attenuates Hyperthyroid-Induced Thermogenesis in Mongolian Gerbils. Microb. Biotechnol. 2022, 15, 817–831. [Google Scholar] [CrossRef]
- Yu, X.; Jiang, W.; Kosik, R.O.; Song, Y.; Luo, Q.; Qiao, T.; Tong, J.; Liu, S.; Deng, C.; Qin, S.; et al. Gut Microbiota Changes and Its Potential Relations with Thyroid Carcinoma. J. Adv. Res. 2022, 35, 61–70. [Google Scholar] [CrossRef]
| Trait | Data Type | N_Cases | N_Controls | Consortium | Phenocode |
|---|---|---|---|---|---|
| GM | Exposure | 18,340 | MiBioGen | ||
| NDG | Outcome | 906 | 349,717 | FinnGen_R10 | E4_GOITREDIFF |
| NMG | Outcome | 6699 | 349,717 | FinnGen_R10 | E4_GOITREMULTINOD |
| NSTN | Outcome | 2203 | 349,717 | FinnGen_R10 | E4_GOITRENOD |
| GD | Outcome | 4846 | 349,717 | FinnGen_R10 | E4_THYTOXGOITDIF |
| PD | Outcome | 1717 | 403,309 | FinnGen_R10 | E4_THYTOXGOITMULT |
| TSTN | Outcome | 246 | 403,309 | FinnGen_R10 | E4_THYTOXNOD |
| Outcome | Exposure | Heterogeneity | Directional Pleiotropy | MR-PRESSO | ||
|---|---|---|---|---|---|---|
| Cochran’s Q | p-Value | Egger Intercept | p-Value | p-Value | ||
| NDG | Clostridium innocuum group | 9.361 | 0.313 | −0.111 | 0.323 | 0.358 |
| Ruminococcaceae UCG002 | 20.528 | 0.488 | −0.015 | 0.672 | 0.561 | |
| Alistipes | 6.909 | 0.864 | 0.082 | 0.323 | 0.853 | |
| Ruminiclostridium5 | 8.642 | 0.733 | −0.007 | 0.870 | 0.842 | |
| Methanobrevibacter | 2.917 | 0.819 | −0.014 | 0.881 | 0.882 | |
| Marvinbryantia | 10.957 | 0.204 | 0.019 | 0.858 | 0.282 | |
| Ruminococcaceae UCG014 | 12.087 | 0.672 | 0.012 | 0.775 | 0.786 | |
| Lachnoclostridium | 10.957 | 0.533 | 0.027 | 0.648 | 0.598 | |
| NMG | Bifidobacterium | 12.431 | 0.412 | 0.019 | 0.271 | 0.421 |
| Ruminococcus gauvreauii group | 23.652 | 0.014 | −0.030 | 0.446 | 0.024 | |
| 8.311 | 0.503 | −0.022 | 0.418 | 0.567 | ||
| Sutterella | 4.991 | 0.892 | −0.004 | 0.892 | 0.933 | |
| Rikenellaceae RC9 gut group | 3.956 | 0.949 | −0.007 | 0.863 | 0.974 | |
| NSTN | Defluviitaleaceae UCG011 | 3.316 | 0.913 | 0.051 | 0.360 | 0.914 |
| Alistipes | 10.944 | 0.534 | −0.014 | 0.787 | 0.639 | |
| Ruminococcus gauvreauii group | 7.889 | 0.723 | −0.027 | 0.547 | 0.778 | |
| Lachnospiraceae UCG010 | 4.287 | 0.933 | −0.006 | 0.875 | 0.965 | |
| Ruminococcus1 | 6.486 | 0.839 | 0.021 | 0.524 | 0.865 | |
| Ruminococcaceae UCG010 | 1.724 | 0.943 | 0.010 | 0.795 | 0.973 | |
| GD | Ruminiclostridium9 | 16.142 | 0.185 | −0.027 | 0.540 | 0.239 |
| Eubacterium rectale group | 8.752 | 0.461 | −0.026 | 0.262 | 0.487 | |
| Desulfovibrio | 7.665 | 0.467 | 0.013 | 0.667 | 0.602 | |
| Bifidobacterium | 10.787 | 0.547 | 0.004 | 0.835 | 0.668 | |
| Victivallis | 14.821 | 0.139 | 0.065 | 0.281 | 0.138 | |
| Butyricimonas | 11.642 | 0.635 | 0.033 | 0.238 | 0.605 | |
| Collinsella | 6.405 | 0.699 | 0.003 | 0.924 | 0.781 | |
| Oscillospira | 7.463 | 0.382 | 0.002 | 0.958 | 0.520 | |
| Catenibacterium | 4.388 | 0.111 | −0.177 | 0.501 | 0.225 | |
| PD | Dorea | 6.328 | 0.787 | −0.062 | 0.149 | 0.680 |
| Eggerthella | 8.349 | 0.400 | 0.019 | 0.768 | 0.516 | |
| Odoribacter | 5.514 | 0.480 | −0.085 | 0.155 | 0.351 | |
| Lactobacillus | 6.446 | 0.375 | −0.050 | 0.267 | 0.382 | |
| Butyricimonas | 10.576 | 0.719 | −0.058 | 0.213 | 0.695 | |
| Intestinimonas | 11.493 | 0.778 | 0.013 | 0.671 | 0.833 | |
| Phascolarctobacterium | 8.348 | 0.500 | −0.015 | 0.793 | 0.659 | |
| Lachnospira | 4.236 | 0.516 | 0.133 | 0.192 | 0.389 | |
| TSTN | Sutterella | 9.669 | 0.470 | −0.006 | 0.965 | 0.591 |
| Oscillibacter | 13.415 | 0.494 | 0.032 | 0.763 | 0.596 | |
| Clostridium sensu stricto1 | 6.494 | 0.483 | 0.090 | 0.473 | 0.554 | |
| Parasutterella | 14.629 | 0.404 | −0.003 | 0.968 | 0.504 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, J.; Wang, Y.; Yao, H.; Li, Y.; Song, H. Uncovering a Causal Connection between Gut Microbiota and Six Thyroid Diseases: A Two-Sample Mendelian Randomization Study. Biology 2024, 13, 714. https://doi.org/10.3390/biology13090714
Chen J, Wang Y, Yao H, Li Y, Song H. Uncovering a Causal Connection between Gut Microbiota and Six Thyroid Diseases: A Two-Sample Mendelian Randomization Study. Biology. 2024; 13(9):714. https://doi.org/10.3390/biology13090714
Chicago/Turabian StyleChen, Jiahao, Yu Wang, Hang Yao, Yuxin Li, and Hong Song. 2024. "Uncovering a Causal Connection between Gut Microbiota and Six Thyroid Diseases: A Two-Sample Mendelian Randomization Study" Biology 13, no. 9: 714. https://doi.org/10.3390/biology13090714






