Abstract
A persistent problem in UK hospitals is that of delayed discharges, where patients who are fit for discharge continue to occupy beds whilst awaiting care packages from Social Care. Integrated Care Systems (ICSs) in which Health and Social Care collaborate are now a major NHS initiative, the thinking being that such spending will have direct cost savings to health by freeing up expensive beds. The premise of this paper is that the benefits to health of assisting Social Care could also reduce a number of serious indirect costs and provide wide-ranging benefits to hospital patients, staff and budgets. This is accomplished by reducing the congestion arising from the use of many painful internal coping strategies and unintended consequences, which hospitals have to resort to when constrained by a lack of discharge solutions. The paper explores new and novel ways of using generic systems archetypes to create a hypothesis linking general Integrated Care Systems to congestion reduction throughout hospitals. Rather than use archetypes individually, they are applied here collectively in tandem. These are named ‘cascaded archetypes’, where the unintended consequence of one archetype becomes the driver for the next and are useful where fundamental solutions to problems are difficult to implement and unintended consequences must be dealt with.
1. Introduction
For many years, hospitals in the UK and other government-funded health systems have struggled with the problem of delayed discharges. Typically, a relatively small number of usually older patients cannot be discharged due to a lack of continuing Health and Social Care capacity (care packages) although they have been declared as “medically fit” for discharge. The problem has been well documented [1,2,3] but despite many attempts at rectification it remains [4,5,6].
This paper builds on two very recent developments in Health and Systems Thinking, which have the potential to help the problem. The first is the formation of Integrated Care Systems (ICSs) within Health and Social Care [7], and the second is the development of new methods for communicating complex feedback structure.
1.1. Developments in Health—Integrated Care Systems
Integrated Care Systems denotes ways of coordinating the delivery of diverse health and social care services to the same person, based on the belief that services should be centred on the person, not the provider [8]. Within the UK, there are now different variations in each of England, Scotland, Wales, and Northern Ireland [9], mainly aimed at interventions to keep people out of hospital to reduce delayed hospital discharges. Rather than wait for government action to improve the funding of Social Care, trials are underway in places for health to both subsidise domiciliary social care wages and ‘discharge to assess’ facilities [10,11,12]. The benefits to health of these trials are being assessed mainly in terms of their direct benefits, such as maintaining the viability of Social Care delivery in the face of government spending cuts and saving the costs of expensive hospital beds. The flow of patients through health and social care is analogous to a supply chain and it seems logical that the most powerful actor in the chain (health) should subsidise the weakest for a win/win outcome.
However, it is the premise of this paper that the potential savings to health from integrated care initiatives are being significantly underestimated by not taking into account their potential to reduce many indirect costs associated with delayed discharges. These costs result from congestion which builds up at both the front and rear end of hospitals pathways. Delayed discharges reduce hospital capacity and admissions and increase patient waiting times. However, more damagingly, they cause hospitals to resort to numerous unofficial coping strategies to maintain patient throughput, each of which have numerous and serious unintended consequences for patients, staff and costs and which, ultimately, tend to defeat their purpose. These strategies are becoming so necessary and common that that they have become embedded in hospital practice and their unintended consequences, by necessity, overlooked.
Increases in congestion in hospital accident and emergency departments and wards is undoubtably due in part to increases in population aging and there are ongoing attempts to reduce demand by such things as same day emergency care, urgent treatment centres and primary care networks. However, it is too easy to blame all congestion on external demand and a cornerstone of system dynamics is to look for internal system drivers of problems. It is suggested here that hospital congestion is significantly compounded by the use of internal coping strategies. Indeed, as shown later the use of coping strategies can cause both health service supply problems as well as latent demand surges.
1.2. Developments in Systems Thinking
Determining and communication of complex feedback structure to facilitate system change is one of the axioms of system dynamics and this paper uses a new and novel approach which represents the cumulation of work over many years by the author to trace and demonstrate feedback connections between Health and Social Care [13,14,15,16,17,18,19,20]. One of the cornerstones of this work has been the judicial blend of qualitative and quantitative system dynamics, with qualitative hypotheses leading to testing with quantitative models and to further qualitative hypotheses. Numerous early models were quantitative and embedded the benefits to health of eliminating elements of coping strategies and individual generic archetypes were often used to explain unintended consequences. Discussions of the early quantitative work with health care staff have led over time to the surfacing of a much wider range of coping strategies with multiple unintended consequences. System dynamics has proven to be a valuable tool in teasing out the way in which organisations really work in response to the stress of capacity constraints. These coping strategies are all embodied in the next stage of qualitative analysis described in this paper. The resultant hypothesis is an amalgam of knowledge captured from health and social care professionals and from the modeler. A modeler who is also a domain expert, may be able to trace interconnections that those inside the field can sometimes miss and to link them to new initiatives such as ICSs.
The medium for communicating the hypothesis is to use generic systems archetypes collectively in tandem, rather than the more conventional approach of using them individually. These collective archetypes are named cascaded archetypes, where the unintended consequence of one archetype becomes the driver for the next and they are particularly useful in communicating situations where solutions are difficult to implement, and unintended consequences must be dealt with. The approach provides a balance between the use of individual system archetypes and the use of full causal loop diagrams. Some interesting choices must be made between keeping each archetype free-standing for simplicity, whilst showing important interlocking between them. The generic nature of the method could have wide application in other systems where capacity constraints inhibit achievement and informal strategies need to be surfaced.
1.3. The Aims, Impact and Shape of the Paper
It is hoped that approach described herein will communicate better the need to balance Health and Social Care capacities, lead to hospitals working more within their design capacities and justify further specific ICS initiatives to reduce the costs of internal coping strategies and congestion. Whilst no specific integrated care initiatives are defined in the paper, it is postulated that linking Integrated Care Systems generally to hospital congestion and communicating the wider benefits in a succinct and compelling manor could boost the case for and number and shape of specific initiatives.
Indeed, the use of cascading archetypes is already making a significant impact on Health policy within the NHS and will be subject to further quantification studies:
‘We have found the thinking in this paper tremendously useful. It is a revelation and my favourite new idea. It provides a new way of thinking about the problems of Health and Social Care and how to improve our justification of Integrated Care Systems’.Steven Wyatt, Head of Research and Policy, NHS Strategy Unit
The paper will:
- Restate and recast the essence of coping strategies,
- Review generic system archetypes and introduce cascaded archetypes
- Apply cascaded archetypes to tracing the linkages between delayed discharges and hospital congestion, together with the role of ICSs in reducing negative outcomes.
- Reflect on the benefits and limitations of cascaded archetypes as a tool of system dynamics
2. A Brief Summary and Clustering of Hospital Coping Strategies
Five hospital internal coping strategies have been identified that are becoming permanent features of hospital practice (This list of hospital coping strategies first appeared in Chapter 10 in The Dynamics of Care. Springer, Cham, and is published here with the permission of Springer). These are effectively complex ‘unofficial’ pathways into, through and out of hospital. A summary of the literature on these strategies has been presented elsewhere [19].
A new way of thinking about these coping strategies introduced here is to cluster them into two groups. The first group is entitled ‘patient absorption’. It is suggested that this group is usually employed in the first instance as capacity becomes constrained. The second is entitled ‘patient expulsion and exclusion’ and it is suggested that this group is usually employed as a last resort when hospital space, costs and congestion are approaching breaking point. The strategies are:
2.1. Patient Absorption Strategies
- Overspill wait areas (escalation beds): When pressure on accident and emergency departments in hospitals is high there is little choice but to accommodate patients as best as possible, which means using temporary admission wards, corridors and ambulances.
- Transfer of unscheduled patients to scheduled beds (boarders or outliers): Another way of making room for unscheduled (emergency) patients is to transfer them to scheduled (elective) beds.
2.2. Patient Expulsion and Exclusion Strategies
- Early/premature hospital discharge: The early discharge of patients is a means of freeing up beds on an individual basis.
- Hospital demand management: Demand management is defined here to mean reductions in GPs referrals from primary to secondary health care, which is now often carried out with commissioning group approval.
- Spot purchase of social care beds: The purchase of Social Care beds directly by hospitals to facilitate patient discharge is a way of freeing up beds on a group basis, with some hospitals actually buying Care Homes for this purpose.
The unintended consequences of these coping strategies are complex and will be described in the cascaded archetypes presented later in the paper.
3. A Review of Generic Systems Archetypes
Causal loop diagrams (CLDs) have long been part of the system dynamics approach as a way of extracting the underlying feedback loops in organisations and models, responsible for their behaviour over time. However, CLDs can themselves be complex.
System archetypes simplify understanding of feedback structure by capturing and categorising common groups of feedback loops [21,22] responsible for generic patterns of behaviour over time and numerous archetypes have been reported [23,24,25,26].
Since there are only two types of feedback loop (reinforcing and balancing), it was suggested by this author that archetypes could be simplified even more. That is by condensing them down to 4 core types, representing the four ways of ordering the two loop types [17] and defining them in two forms; problem and solution archetypes. This core group were shown to be capable of subsuming a wide range of existing archetypes [17].
The 4 core, generic archetypes representing the four ways of ordering a pair of reinforcing and balancing feedback loops, were defined as:
- Underachievement: where intended reinforcing action is diminished by balancing unintended consequences,
- Out of Control: where intended balancing control is diminished by reinforcing unintended consequences,
- Relative achievement: where intended reinforcing action is diminished by reinforcing unintended consequences,
- Relative control: where intended balancing control is diminished by balancing unintended consequences.
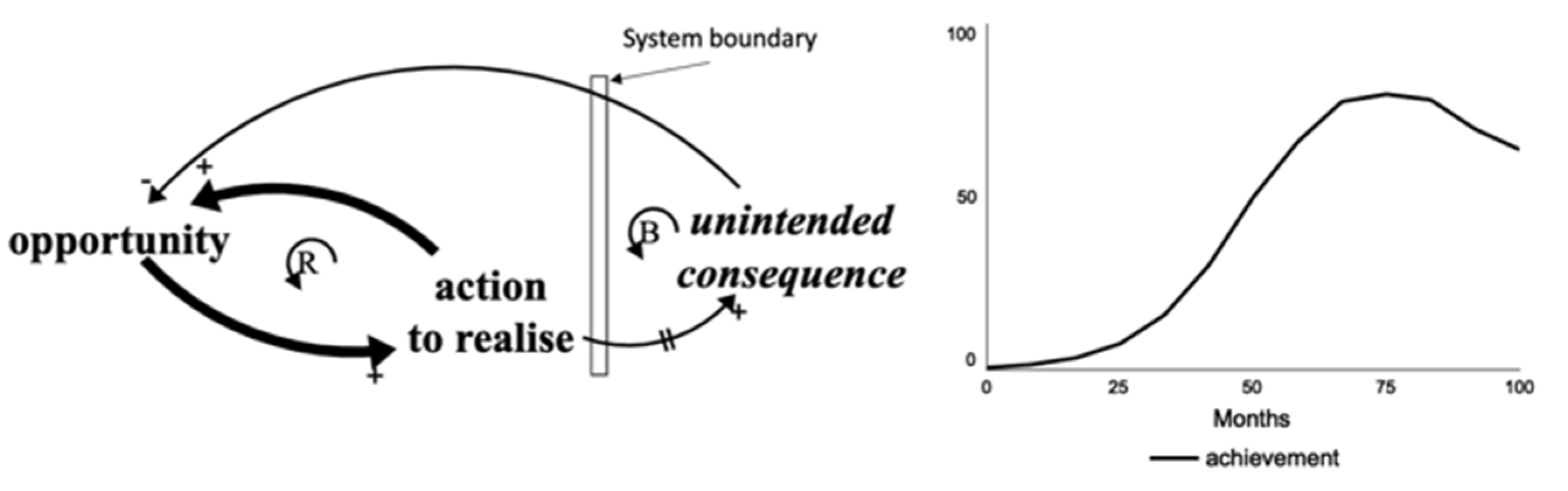
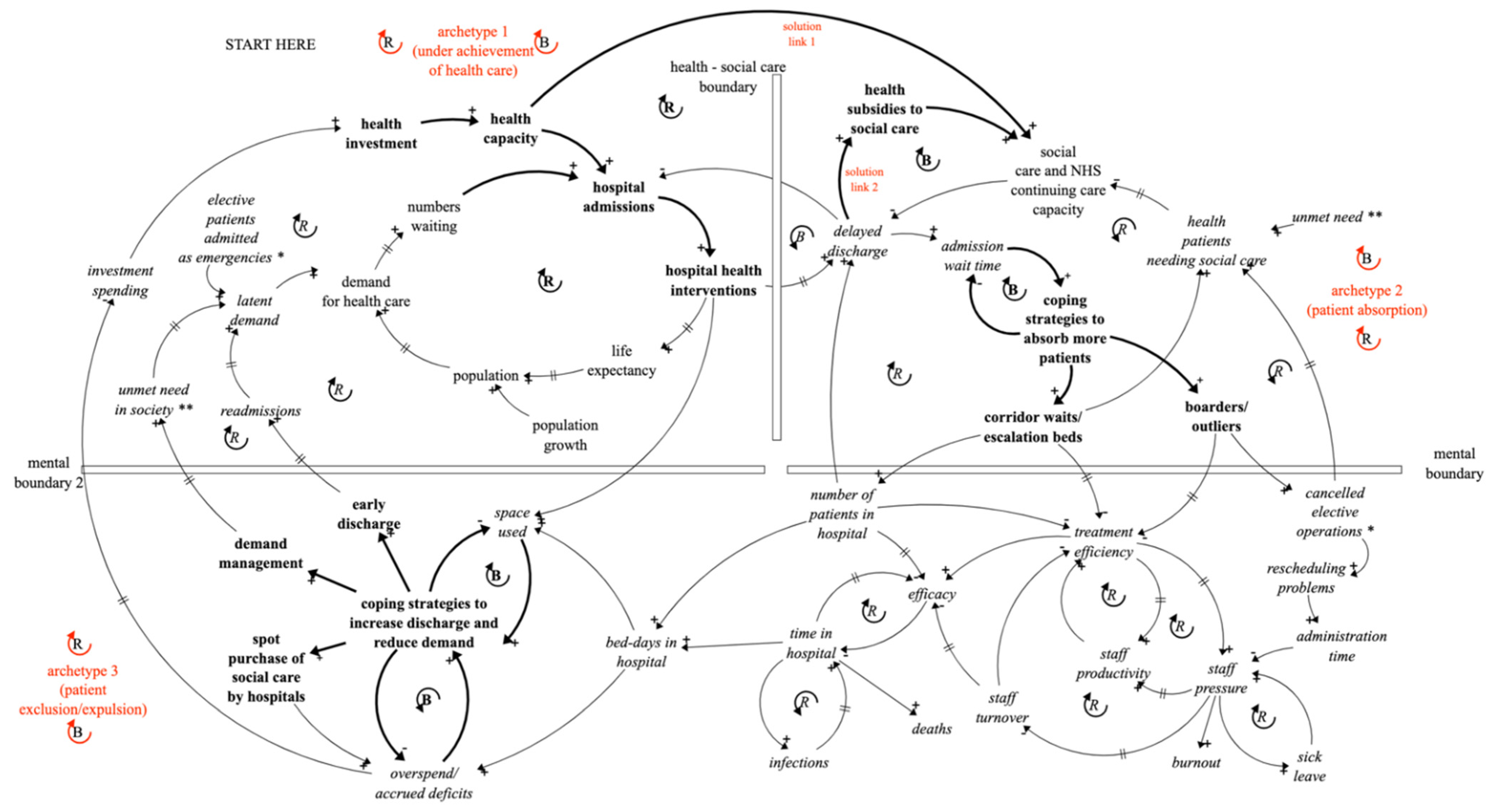
This paper will focus on under-achievement and out-of-control archetypes since they are the ones used in the later hospital analysis. Figure 1, Figure 2, Figure 3 and Figure 4 show these two archetypes in problem and solution forms.
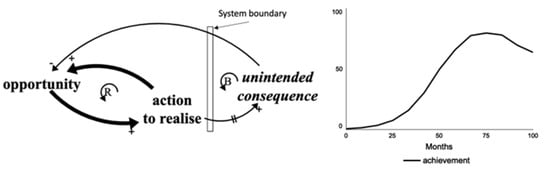
Figure 1.
The generic underachievement problem archetype and an example of its behaviour over time.
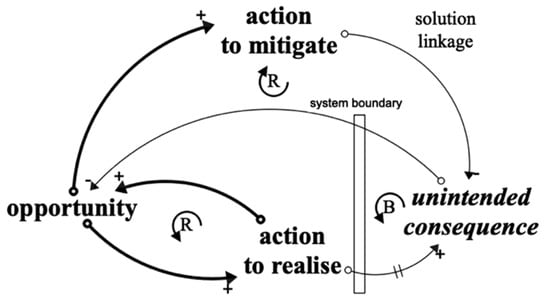
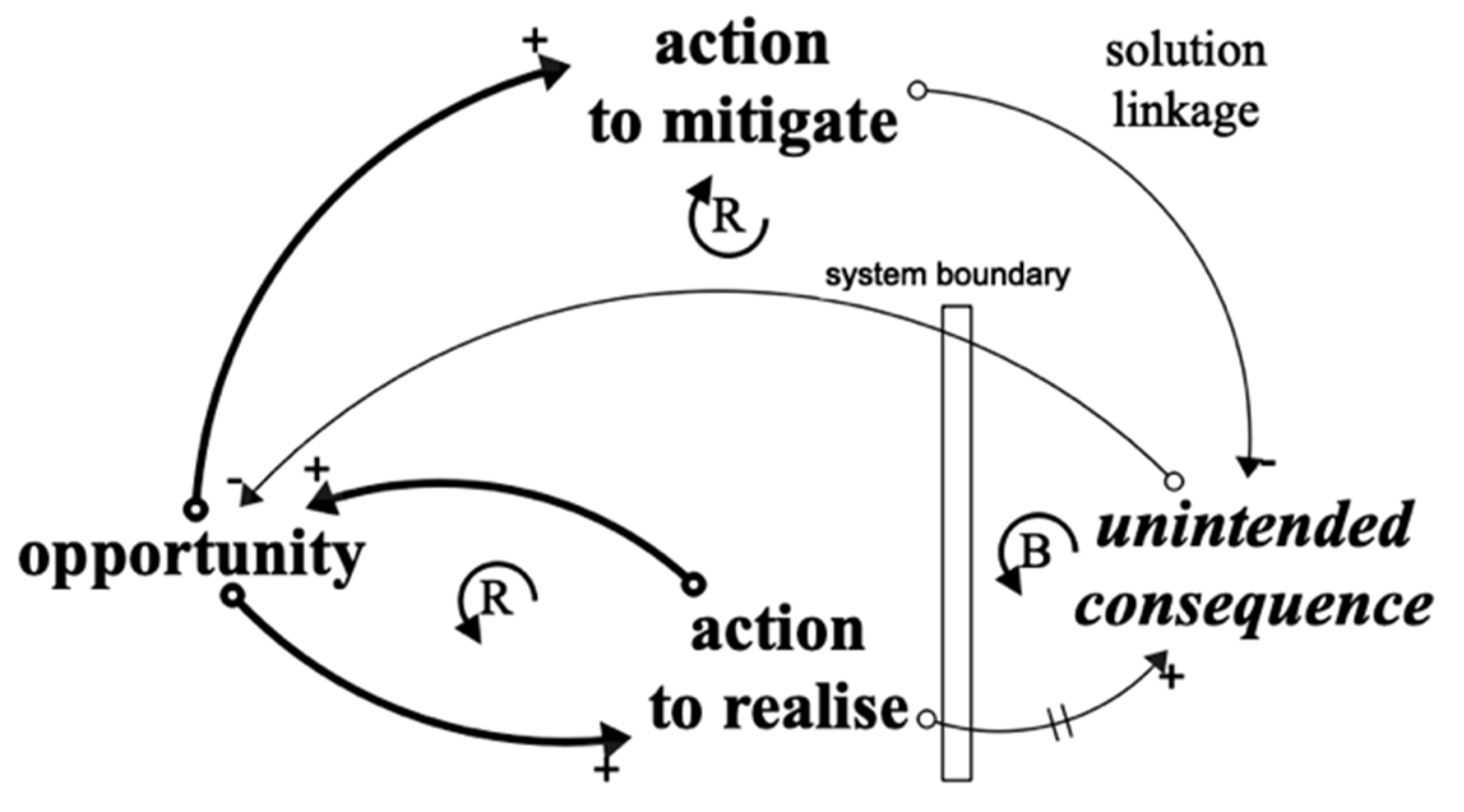
Figure 2.
The generic under-achievement solution archetype.
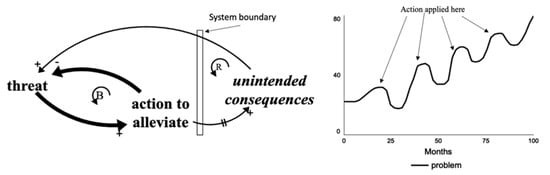
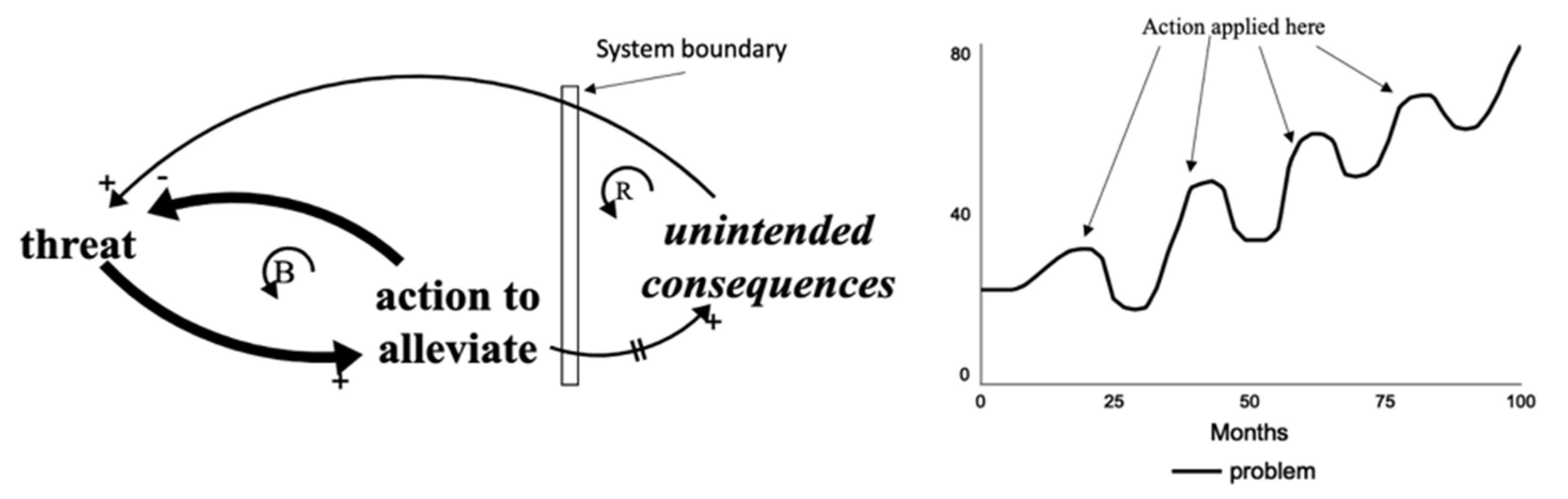
Figure 3.
The generic out-of-control problem archetype and an example of its behaviour over time.
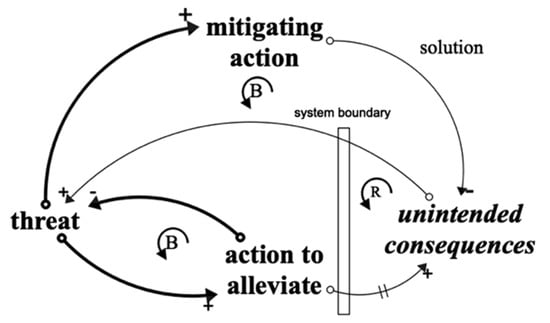
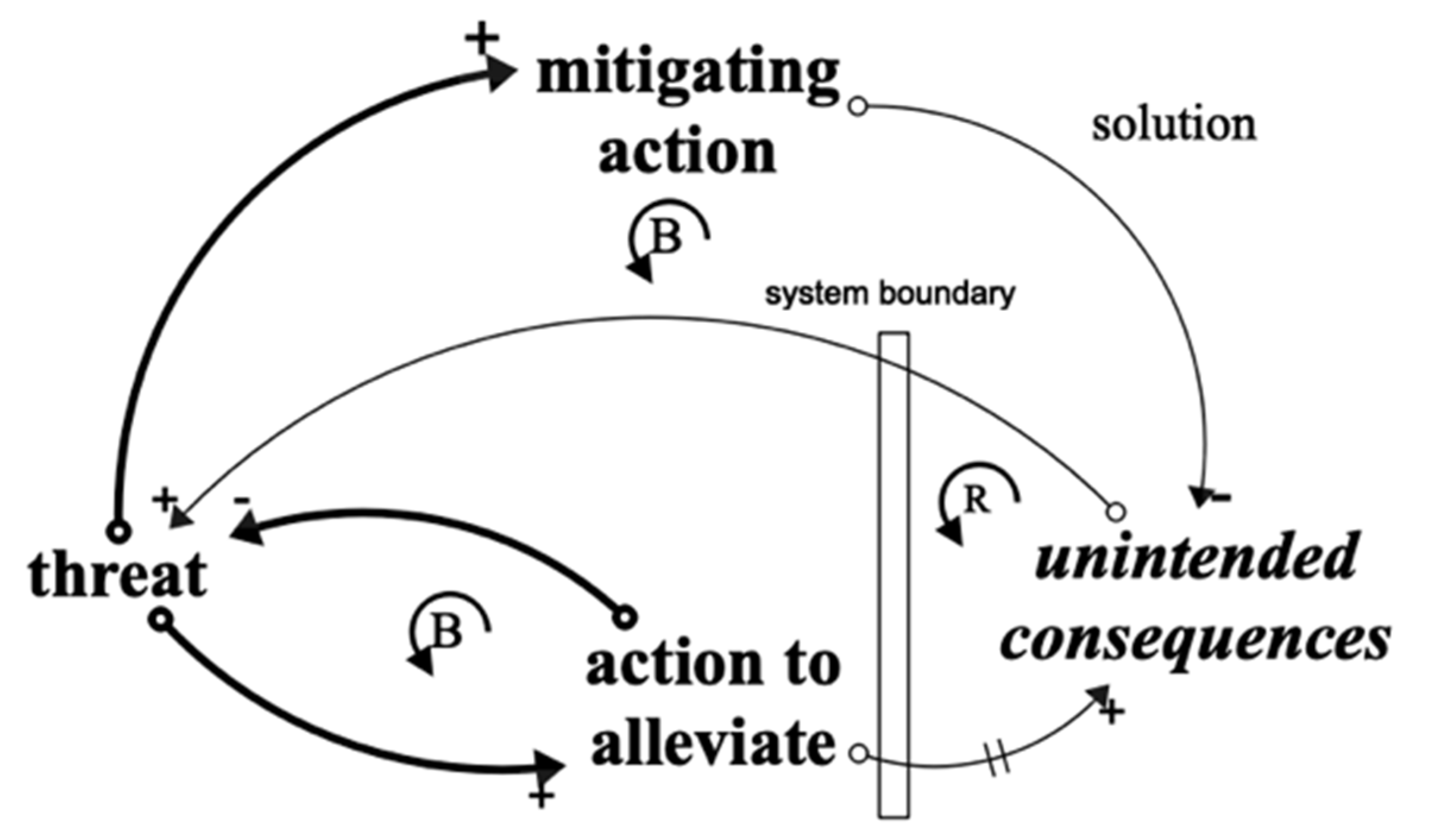
Figure 4.
The generic out-of-control solution archetype.
In contrast to earlier writing by this author [17], the intended outcome for a reinforcing feedback loop will be defined as the realisation of an opportunity and the intended outcome for a balancing feedback loop will be defined as containment of a threat.
Notation: Actions and intended consequences will be shown in thick causal links and bold text. Unintended consequences will be shown in thin causal links and italics. A positive sign will be used to depict a causal link between variables in the same direction. A negative sign will be used to depict a causal link between variables in the opposite directions. A balancing feedback loop is defined as one which contains an odd number of negative causal links which gives rise to its control behaviour over time towards a target. A reinforcing feedback loop is defined as one which contains none or an even number of negative causal links which gives rise to its exponential behaviour over time (virtuous or vicious).
3.1. Underachievement Archetype
The problem version of this archetype (Figure 1) consists of a reinforcing loop intended to generate growth in an opportunity over time, but this is countered by a balancing unintended consequence loop which inhibits the growth, occurring across a boundary (physical or mental barrier) and after a delay, both of which can mask the unintended consequence. Although shown as two loops, in practice the unintended consequence loop of the archetype may subsume a number of detrimental balancing effects giving rise to a variety of behaviours over time. Figure 1 shows an example of one such behaviour.
When the underachievement happens it is only too easy to blame external factors, rather than accept it as being seeded by the earlier action—a realisation of the systems message that today’s problems are often yesterday’s solutions.
The solution version of the archetype is shown in Figure 2. This suggests that if the unintended consequence can be pre-empted, a possible solution exit by introducing a second action in parallel with the first to reduce the impact of the unintended consequence and hence compliment the intended reinforcing loop.
A health-related example of this archetype would be investment in hospital capacity to increase the number of interventions, but this might result in more delayed discharges and actually reduce the effective capacity. A solution might be to make a corresponding investment in Social Care capacity.
3.2. Out-of-Control Archetype (Figures 3 and 4)
In this case, the problem archetype consists of a balancing feedback loop intended to reduce an exogenous rising threat (Figure 3), perhaps to a target level, but this is undermined by a reinforcing unintended consequence loop, again occurring across a boundary and after a delay, which mask the unintended consequences. Again, in practice, the unintended consequence loop may subsume a number of (this time) detrimental reinforcing effects giving rise to a variety of behaviours over time. Figure 3 shows one of these where each time the action is applied control is re-established, but only for limited periods.
As before, if the unintended consequence can be pre-empted, a possible solution exit by introducing a second action in parallel with the first to reduce the impact of the unintended consequence and hence compliment the intended balancing loop (Figure 4).
A health-related example would be the introduction of additional beds to control (reduce) patient waiting times, but these might stimulate demand and quickly fill up with waiting times increasing again. A solution might be to combine this action with measures to inhibit demand.
4. An Introduction to Cascaded and Interlocking Systems Archetypes
The generic archetypes in the last section were originally perceived as being useful in an individual context. However, it is suggested here that they can have a wider role collectively in tandem to capture actions and reactions in complex feedback situations. This is particularly true where solution links in individual archetypes have been identified, but proved difficult, if not impossible, to implement.
Rather than deploy solution links, it is far more common for new reactive strategies to be employed by groups of stakeholders to deal with unintended consequences. Such reactions can spawn a new archetype to address the unintended consequence of the first archetype. The key to drawing this situation is to understand that the unintended consequence variable of the first archetype becomes the driving variable of the second archetype. It is then possible to consider that the action of the second archetype (in addition to countering the unintended consequence of the first archetype), may have its own unintended consequence(s) which could be depicted with in a third archetype.
This sequence can happen repeatedly and give rise to chains of archetypes, defined here as a set of cascaded archetypes.
Each archetype in a chain may well be linked to the same system and these links would all be shown in a full causal loop diagram. Such causal maps can be self-defeating as a means of communication due to the number of interconnections contained and cascaded archetypes strive to reduce the links. In order to achieve this simplifying role, each archetype can be introduced separately in turn within a story telling context, before the composite picture of the full cascade is presented.
Some interesting choices must be made between keeping each archetype free-standing for simplicity, whilst showing important interlocking between them. The term interlocking archetypes applies to those cascaded archetypes whose unintended consequences link directly to an opportunity or threat variable of earlier ones. They may in fact be the same variables.
Within the overall picture, the pattern of each archetype (opportunity/threat-action-unintended consequence) provides familiar structure and simplicity. It is suggested that this approach has an intermediate role in communication between the more conventional use of individual system archetypes and the use of full causal loop diagrams.
It is of interest to note that reactions in each cascaded archetype may be carried out by different stakeholders reacting in their own interests or by the same group as in the first archetype, perhaps trying multiple attempts to solve the original problem.
Figure 5 shows an example of a generic representation of cascaded and interlocking archetypes. This is a cascade of 4 archetypes starting with an underachievement archetype (top) and 3 out-of-control archetypes. The last of which feeds back on the first. This is a similar sequence to the one used later to describe hospital congestion. The choice of the number of archetypes to use is subjective and should be made on the basis of clarity, ease of grouping of coping actions and their dynamic phasing.

Figure 5.
A cascade of 4 archetypes with the last one interlocking with the first.
Starting at the top of Figure 5:
- archetype 1, underachievement: a reinforcing action to exploit an opportunity is undermined by balancing unintended consequence 1.
- archetype 2, out-of-control: in the absence of a solution link, a balancing action to address the threat of unintended consequence 1 is undermined by reinforcing unintended consequence 2.
- archetype 3, out-of-control: again, in the absence of a solution link, a balancing action to address the threat of unintended consequence 2 is undermined by a reinforcing unintended consequence 3.
- archetype 4, out-of-control: again, in the absence of a solution link, a balancing action to address the threat of unintended consequence 3 is undermined by a reinforcing unintended consequence 4. This unintended consequence has strong links to the variables in the opportunity loop of archetype 1 (or may be the same variables), hence it is referred to as interlocking with archetype 1.
The important point is that the original actions in the first (prime) archetype in the chain are not only undermined by their own unintended consequences, but also by the unintended consequences arising from subsequent actions to counter them.
Cascaded archetypes raise an interesting question not encountered in using individual archetypes. The convention with individual archetypes is to either start with a reinforcing feedback loop (opportunity) or a balancing loop (threat) as described earlier. However, if an archetype is started with a balancing feedback loop, cascaded thinking begs the question as to whether this threat is already an unintended consequence of a preceding archetype? It may have a linear source, but it is always worth exploring whether there is some reinforcing driver of the threat. It there is, it leads to the further question as to whether all cascaded archetypes should begin with a reinforcing feedback loop? This is certainly true in the hospital congestion example to follow.
5. Using Cascaded and Interlocking Archetypes to Trace the Links between Delayed Hospital Discharges, Hospital Congestion and Integrated Care Systems—A Case of 3 Interlocking Archetypes
5.1. Archetype 1
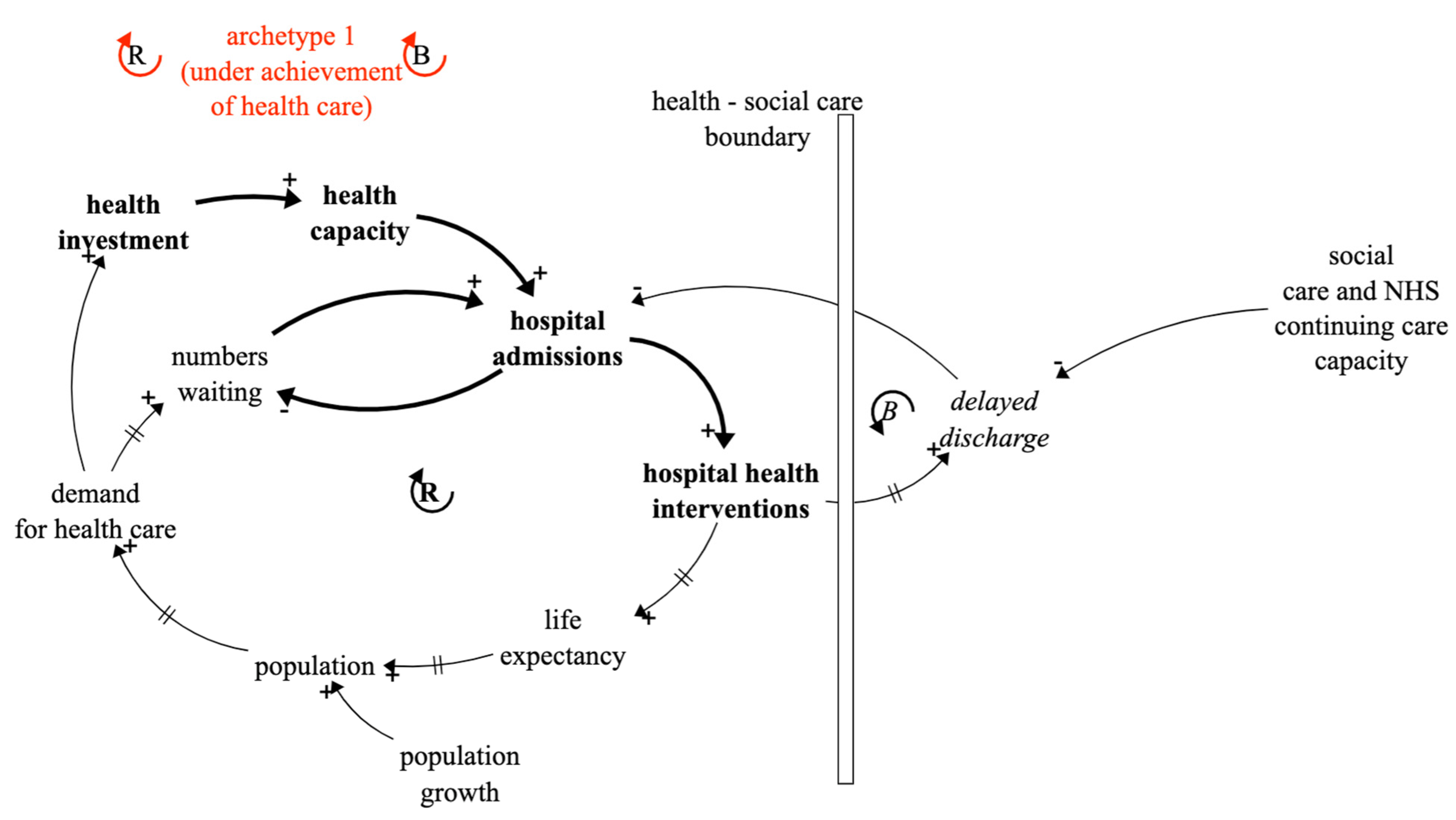
Health service underachievement (an underachievement archetype): investment in successful hospital interventions increases demand and is limited by delayed discharges, Figure 6.
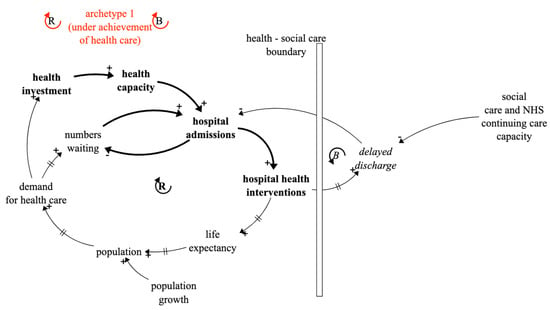
Figure 6.
Archetype 1: The underachievement problem archetype involving health and social care.
This archetype is a classic example of underachievement and captures the way in which the demand for health services is driven by both population growth and aging, but also by health services being a victim of their own success by increasing longevity [27]. The supply response is investment in all types of hospital capacity with the intention of facilitating admissions and interventions. However, even if this is forthcoming, it results in problems with delayed discharges resulting from inadequate social care capacity, which feedback to reduce admissions and to cause underachievement in the number of hospital interventions.
The good news is that solutions do exist for this archetype which are shown in Figure 7.
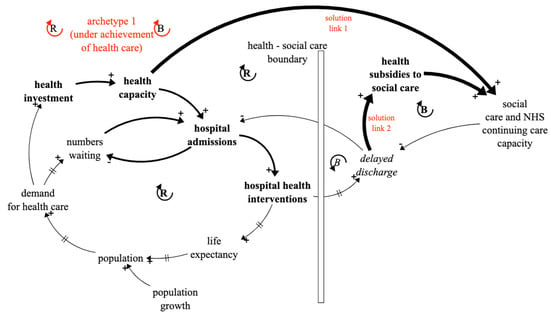
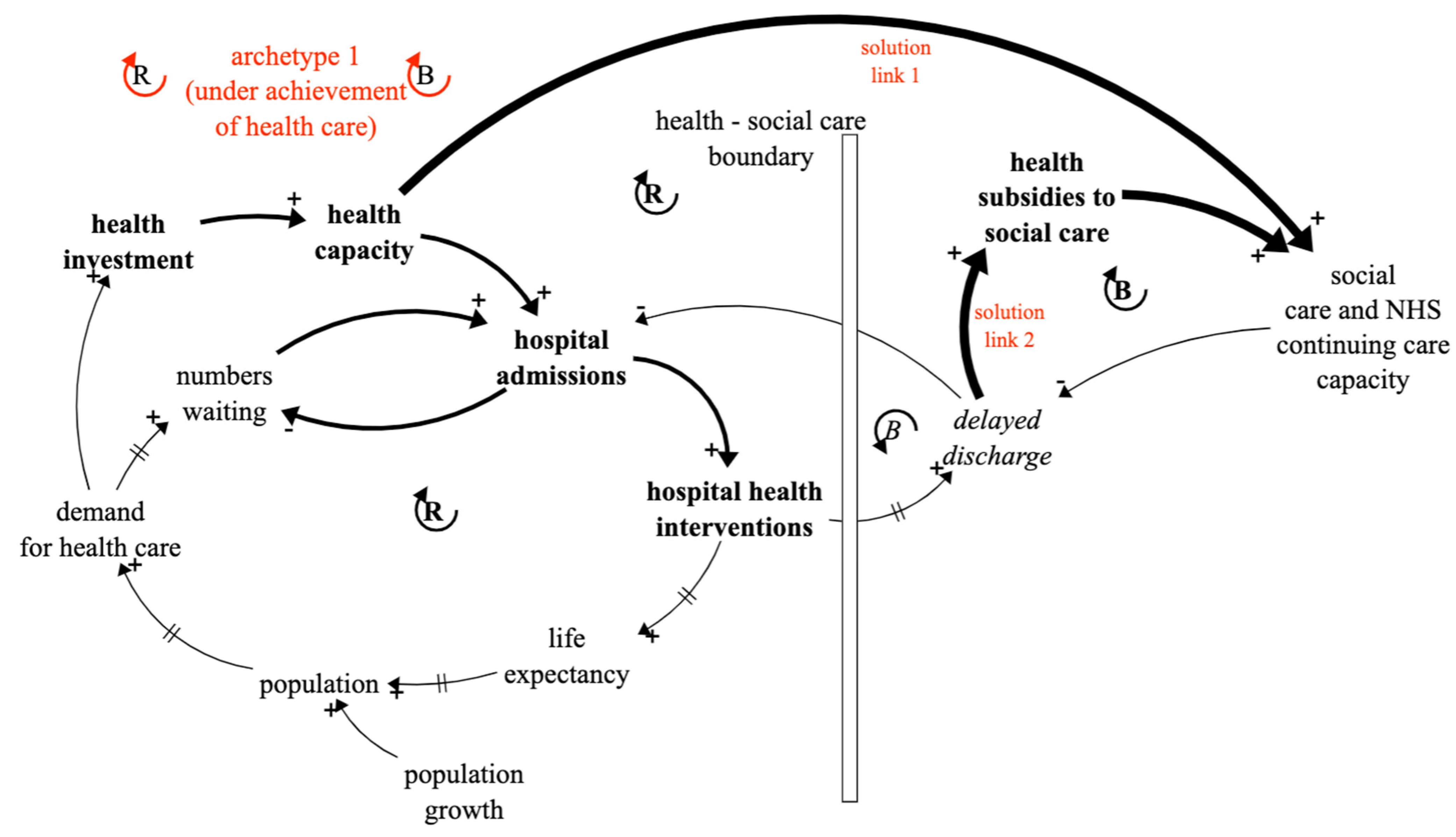
Figure 7.
Archetype 1: The underachievement solution archetype involving health and social care.
First, solution link 1 is to expand Social Care capacity in line with Heath capacity and much previous has work has been aimed at demonstrating the merits of this link. The assumption has been that being that the government would provide this spending. However, the reality of implementing this solution has remained elusive since Health is funded from central government and Social Care is funded from local government. The new approach, motivating the thinking in this paper, is that an alternative solution might be pursued. That is for Health to subsidise Social Care to the benefit of both. Figure 7 shows this as solution link 2 and it is the purpose of this paper is to provide more justification for it by showing the congestion that arises from not doing so.
In the absence of solutions, hospitals have had to resort to numerous coping strategies, which can disguise the plight of their predicament.
5.2. Archetype 2
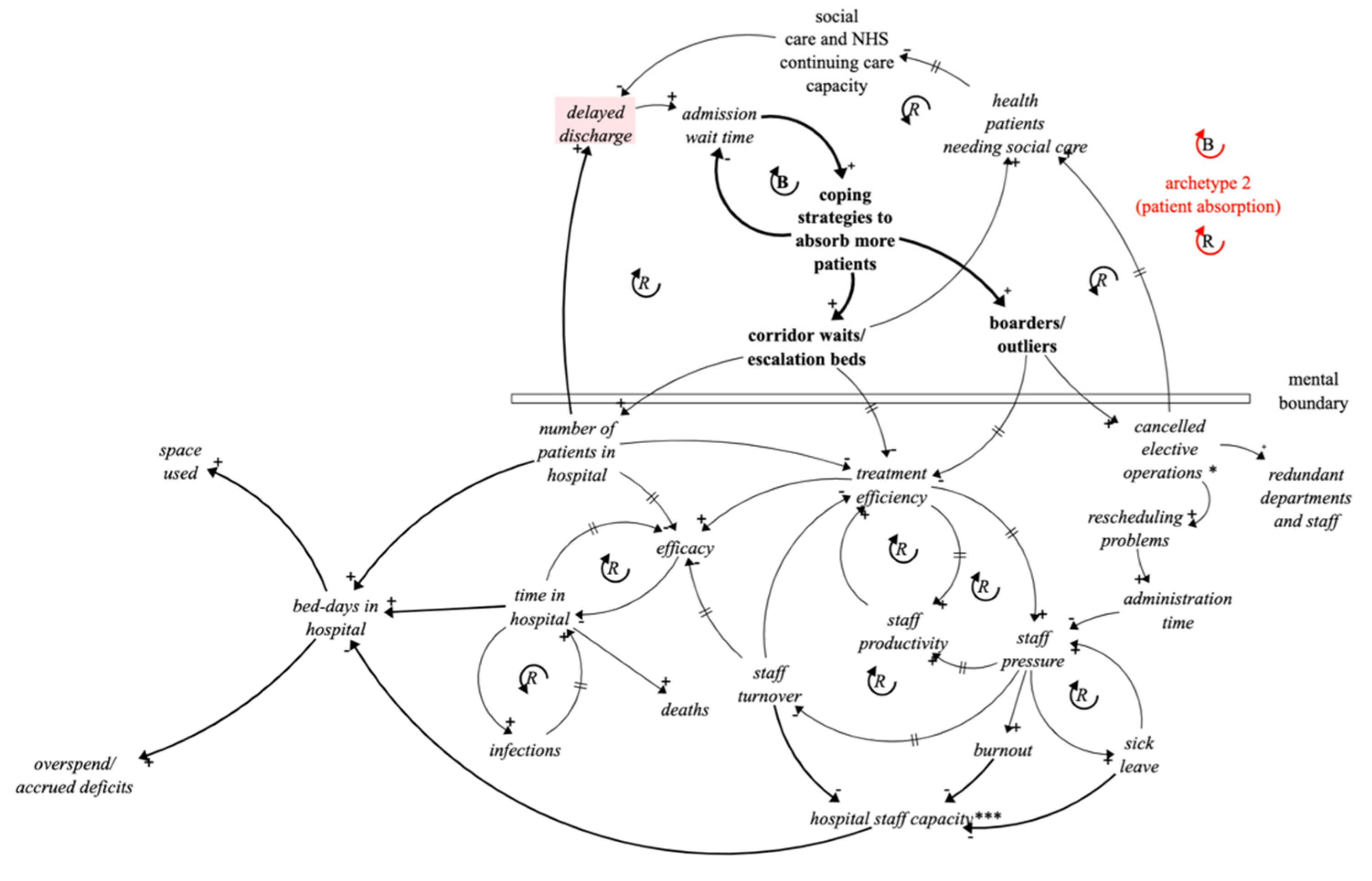
Patient absorption (an out-of-control archetype): using boarders and overspill waiting areas to counter delayed discharges leads to deteriorating services and rising costs, Figure 8.
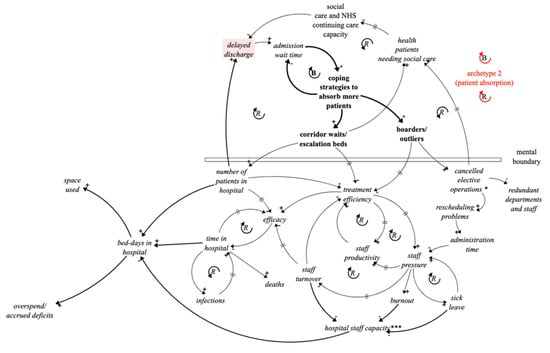
Figure 8.
Archetype 2: The out-of-control archetype arising from patient absorption coping strategies.
The idea of using cascaded archetypes for improved communication is that they can be introduced one at a time. So, at this point archetype 1 is put to one side and archetype 2 starts with the threat from the unintended consequence of archetype 1—delayed discharges (highlighted).
However, rather than tackle delayed discharges head on, attention in hospitals is usually focussed on the consequential problem of delayed admissions at the ‘front end’ of the patient pathways. In fact, delayed admissions have often not been linked to delayed discharges, but more to lack of emergency room capacity. A clear case of looking for obvious solutions close to the symptoms of problems, when the best levers might be quite remote from the symptoms. This situation is changing, and hospitals now have sophisticated bed management systems and see freeing up discharges as a key to improving admissions.
These ‘front end’ issues are addressed by ‘patient absorption’ strategies comprising ‘boarders’ and ‘overspill waiting areas.
Archetype 2 shows how these 2 coping strategies, are applied in response to admission problems. Both strategies lead to multiple and reinforcing unintended consequences.
The use of corridor and ambulance waits can lead to treatment inefficiencies and complications for patients. The use of temporary admissions wards restricts space for other conditions, and regular out-patient clinics, particularly long-term conditions clinics, have to be suspended. The use of boarders leads to the cancellation of elective procedures, redundant surgical teams, unused theatres and increases in the hospital elective waiting list. The resulting prioritising and rescheduling of elective procedures, places a massive demand on management and clinical time. Additionally, patients awaiting suspended clinics and elective operations may need social care, taking valuable capacity away from hospital discharges.
Both of these coping measures, like any form of bed capacity expansion, can quickly fill up without solving the flow problem. It is somewhat ironic that, whilst acknowledging the need for long term bed reductions, hospitals are forced into short term bed expansion. The coping measures are intended to provide a temporary solution to congestion, but periods of high demand and suspension of regular treatments are becoming more frequent and of longer duration. In recent years, there have been times when UK hospitals have formally cancelled elective operations during periods of high emergency demand.
Boarders and temporary admissions accommodation can also result in patients having longer stays in hospital, increased mortality rates [28] and reductions in treatment efficiency and efficacy [29,30]. Treatment efficiency is vital to care and recovery and when diminished has implications for both patients and staff. The longer patients are in hospital the greater the chance of infection and increased risk of fatalities. There are significant external issues in recruiting and retaining Health staff, but these are compounded by internal coping strategies. As patient to staff ratios increase staff disillusionment quickly shows up in staff productivity decline, increases in sick leave, burnout and higher staff turnover, with its associated loss of knowledge. Space becomes at a premium and budget deficits rise, perhaps to a point where new investment funds have to go to pay off accrued deficits rather than to enhance the supply of services [31].
It becomes more and more difficult for hospital management to address these vicious spirals of declining services and the net effect of the coping strategies is more patient bed-days in hospital and rising costs with delayed discharges increasing, rather than reducing.
An interesting question is whether there is a solution link for this second archetype on its own. It is easy to see in hindsight how absorbing more patients might inevitably lead to congestion and impact staff and patients. However, essential firefighting gives little time to think ahead to mitigate against these eventualities.
5.3. Archetype 3
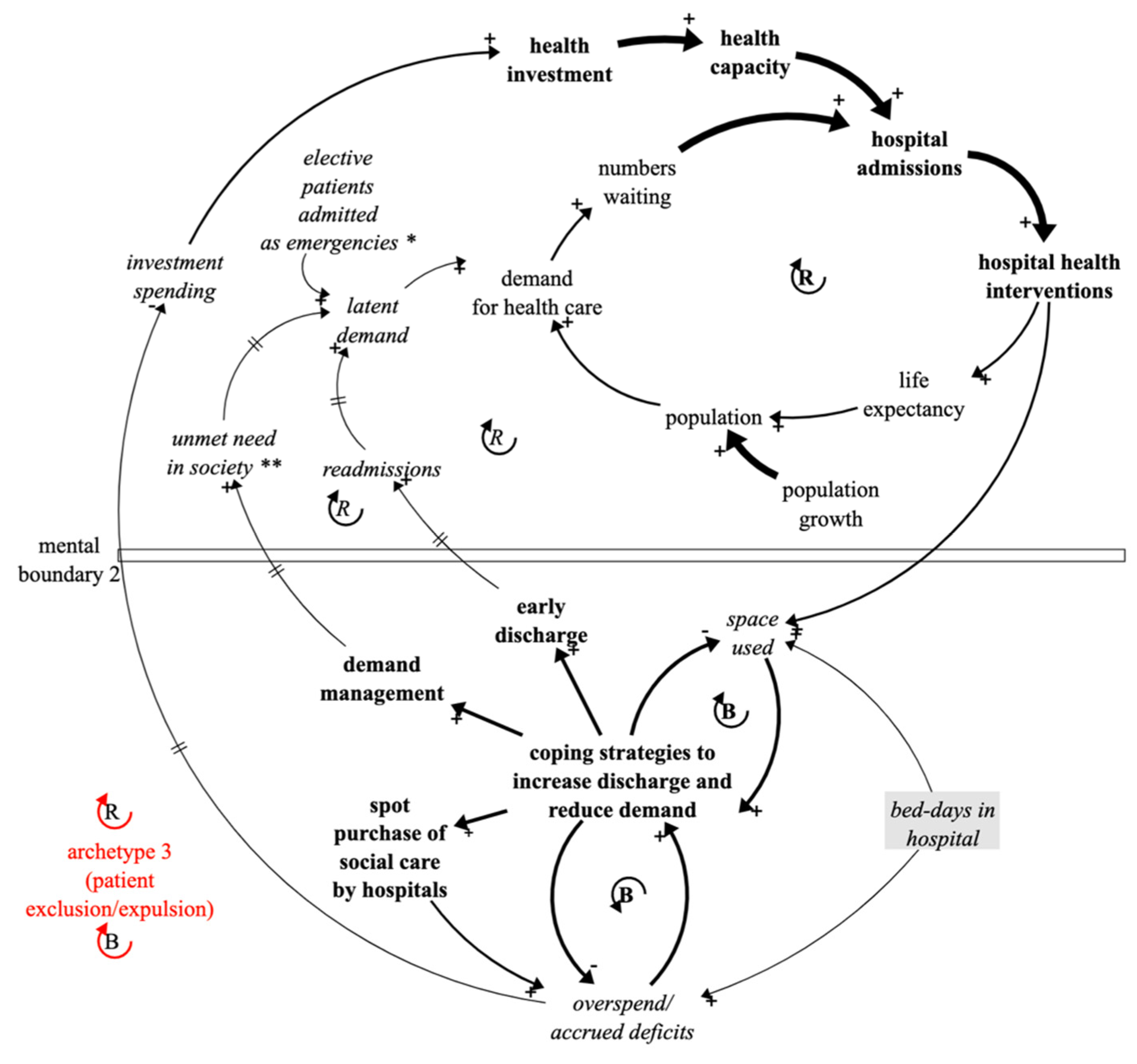
Patient expulsion and exclusion (an out-of-control archetype): using early discharge, demand management and spot purchase of social care to counter deteriorating services and rising costs leads to reduced investment and increases in unmet need and latent demand Figure 9.
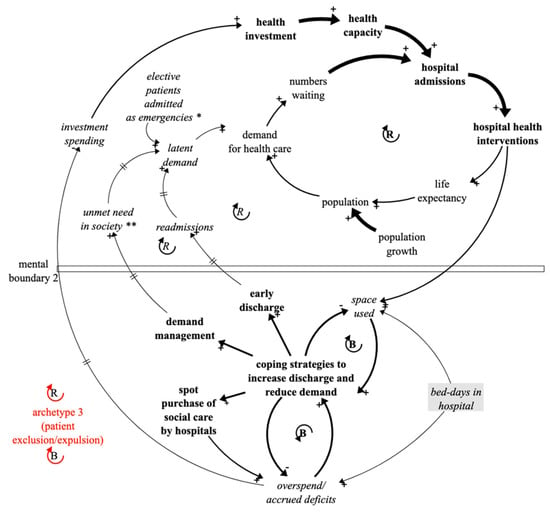
Figure 9.
Archetype 3: The out-of-control archetype arising from patient exclusion/expulsion coping strategies. (The links between variables with asterisks exist but are not shown explicitly).
As overspending and provision of extra space become more and more difficult to address, attention of hospital managers and clinicians are inclined towards more radical coping strategies to relieve congestion pressures. In control engineering terms, from which System Dynamics emerged, there is a need to find a safety valve. The actions taken tend to have a ‘rear end’ focus with the intention of directly accelerating hospital discharge, but they also include stemming demand and hence admissions. They consist of early discharge of patients, the ‘spot’ purchase by health of social care capacity and demand management. This second group of coping strategies, in contrast to ‘patient absorption’, are referred to here as ‘patient expulsion/exclusion’ strategies.
In methodological terms Archetypes 1 and 2 are now put to one side and archetype 3 starts with how to address bed days in hospital (highlighted), space limitation and accrued deficits.
Early discharge can have serious unintended consequences by compromising patient safety. It can lead to readmissions and despite many guidelines poor hospital discharge is a recurring problem [32,33,34,35,36].
Demand management results in pushing demand further back upstream and ultimately this has to be absorbed by primary health care and society [37]. Demand can get pushed back on to families, charities and communities to create a cumulative unmet need which can result in further demands on Social Care.
The latent demand associated with early discharge and demand management eventually adds to demand on hospital services and interventions which add to the need for more coping strategies and space rather than to relieve them. Interestingly, due to delays, when extra demand impacts it can be puzzling as why it has happened, rather than seen as an inevitable consequence of earlier actions.
Purchasing Social Care beds by hospitals can be much more expensive than beds bought from social care under block contracts [38,39,40] and can also result in more variable quality of care. The cost of spot purchases also adds further to budget deficits.
The important point about archetype 3 is that it impacts directly on (interlocks with) variables which were the fundamental drivers of archetype 1. There is a double impact on achievement with investment reducing and demand increasing.
Again, the question might be raised as to whether there is a solution loop for this archetype, perhaps associated with providing help in the community to support early discharges and unmet need. Ironically, this would require more Social Care, the shortage of which caused the problems in the first place.
5.4. The Composite Picture
Figure 10 shows a composite picture of the 3 cascaded and interlocking archetypes, all on one page and without any crossed lines.
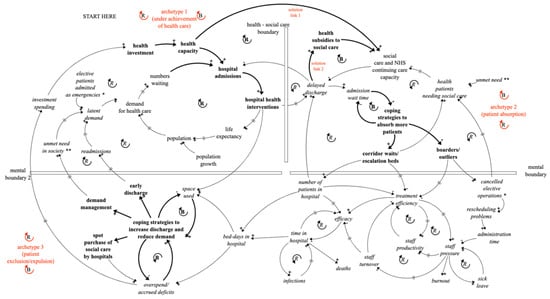
Figure 10.
A composite picture of the 3 interlocking archetypes linking health and social care though delayed discharges and hospital congestion coping strategies. (The links between variables with asterisks exist but are not shown explicitly).
Whilst still complex, the structure of each individual generic archetype can be recognised in Figure 10, comprising opportunities/threats, actions and unintended consequences. The picture captures the phases of the coping strategies (patient absorption and patient expulsion/exclusion) and conveys the barriers and time delays conspiring to mask the unintended consequences in the early stages of action. In the composite picture it is also perhaps easier to see some of the feedback effects through the whole picture, rather than just within each archetype.
The key point, and a core point about interlocking archetypes, is that not only is archetype 1 inhibited by its own unintended consequence (delayed discharges), but this leads to a series of cascaded reactions which have implications for patients, staff and costs that undermine its achievement even more.
Figure 10 also includes the solution links and the message hopefully communicated is that investment in social care by government of Health in the form of Integrated Care Systems has the potential to both reduce delayed hospital discharges (direct cost saving), but to greatly reduce the use of coping strategies and congestion (indirect cost saving).
The financial costs of coping strategies are yet to be assessed but are underway and indications are that these could be much greater than a modest social care investment increase in the first place. However, financial costs pale into insignificance compared with the loss of efficacy and increased risk of patient illness and death arising from congestion. Additionally, eliminating the need for coping strategies would bring much-needed stress relief to both clinical and nursing staff.
6. Benefits and Limitations of the Cascaded Archetype Approach
Whilst feedback loops do not in themselves provide definitive quantitative solutions to problems, they are very important at each stage of system dynamics modelling. They are useful both for conceptualising models and to extract insights from them. The idea of alternating between these two modes to develop models and thinking makes maximum use of both attributes. The work here has extrapolated early quantitative modelling results into a broad and succinct hypothesis, capable of drawing attention for further testing, which is already starting. Qualitative thinking is particularly important when some consequences in the situation described, such as mortality are intangible.
Cascaded archetypes enable complex feedback structures to be easily understood at a high level of aggregation and are proving useful to explain interconnections between Health and Social Care. Whether this is true in other domains is yet to be seen, but they have the potential to be helpful wherever obvious solutions prove elusive and informal strategies dominate system performance.
7. Conclusions
This paper has created a hypothesis that indicates that additional spending on Social Care, either by the government or Health (NHS) to reduce hospital-delayed discharges could bring very significant benefits to hospital management, staff and patients. It suggests that health spending on social care though Integrated Care Systems can be justified not only in the direct cost savings of expensive hospital beds, but by the indirect and wide-ranging benefits and savings associated with reducing hospital congestion. Whilst no specific integrated care initiatives are defined, it is recommended that linking Integrated Care Systems generally to relieving coping strategies and communicating the wider savings in a compelling manner could boost the case for and number and shape of the initiatives.
Methodologically, the paper has suggested that individual generic two-loop system archetypes can be usefully deployed collectively to improve the clarity of communication and storytelling of complex issues and to explain why unintended consequences occur. This is achieved by decomposing complex causal loop maps into recognisable and understandable structures. The process is particularly apposite to situations where the solution links of individual archetypes can be very difficult to implement and reactive actions by multiple stakeholders dominate.
It is suggested that further research is necessary to explore the full potential and limitations of the approaches described in other contexts and involving other types and combinations of generic archetypes. The generic nature of the method could have wide application in other systems where capacity constraints inhibit achievement and informal strategies need to be surfaced.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
The author would like to thank ISEE Systems, the creator of the Stella Architect software used to draw the figures in this paper, for their continuing support of his research.
Conflicts of Interest
The author declares no conflict of interest.
References
- Bate, A. Delayed Transfers of Care in the NHS—House of Commons Library. 2017. Available online: https://commonslibrary.parliament.uk/research-briefings/cbp-7415 (accessed on 2 June 2022).
- National Audit Office. Annual Report: Discharging Older Patients from Hospital; National Audit Office: London, UK, 2016.
- Age UK, 1.4 million Older People Aren’t Getting the Care and Support They Need—A Staggering Increase of Almost 20% in Just Two Years’. 2022. Available online: https://www.ageuk.org.uk/latest-news/articles/2018/july/1.4-million-older-people-arent-getting-the-care-and-support-they-need--a-staggering-increase-of-almost-20-in-just-two-years (accessed on 3 July 2018).
- Nuffield Trust, The Health Foundation and The King’s Fund. The Autumn Budget: Joint Statement on Health and Social Care. 2017. Available online: https://www.nuffieldtrust.org.uk/research/autumn-budget-2017 (accessed on 20 November 2017).
- Kings Fund Newsletter. The NHS Budget and How It Has Changed. Part of the NHS in a Nutshell. 2022. Available online: https://www.google.com/search?client=safari&rls=en&q=%5B5%5D+Kings+Fund%2C+Newsletter+(2022)+The+NHS+Budget+and+how+it+has+changed.+Part+of+the+NHS+in+a+nutshell.&ie=UTF-8&oe=UTF-8 (accessed on 14 July 2022).
- NHS England. Better Care Operating Guide; 2016. Available online: https://www.england.nhs.uk/ourwork/part-rel/transformation-fund/better-care-fund/ (accessed on 2 August 2019).
- Thorstensen, C. Integrated Care, The King’s Fund. 2022. Available online: https://www.kingsfund.org.uk/topics/integrated-care?gclid=Cj0KCQjw1tGUBhDXARIsAIJx01ln_mqVn2FZpj8A-zFip89t9MwoXcoimhbqTXiSMYLf1wIzCPp-kUEaAujyEALw_wcB (accessed on 4 August 2022).
- Ham, C. Making Sense of Integrated Care Systems, Integrated Care Partnerships and Accountable Care Organisations in the NHS in England, The King’s Fund. 2018. Available online: https://www.kingsfund.org.uk/publications/making-sense-integrated-care-systems (accessed on 4 June 2019).
- NHS England. Integrating Care: Next Steps to Building Strong and Effective Integrated Care Systems across England. 2022. Available online: https://www.england.nhs.uk/publication/integrating-care-next-steps-to-building-strong-and-effective-integrated-care-systems-across-england (accessed on 4 August 2022).
- Home Care Investment Plan to Help Residents Through Winter. 2022. Available online: https://www.northstaffsccg.nhs.uk/news-events/1758-home-care-investment-plan-to-help-residents-through-winter (accessed on 4 August 2022).
- The NHS Strategy Unit. Securing the Future of Domiciliary Care. 2022. Available online: https://www.strategyunitwm.nhs.uk/news/securing-future-domiciliary-care (accessed on 4 August 2022).
- Wolstenholme, E.F.; McKelvie, D. Integrated Care. In The Dynamics of Care; Springer: Cham, Switzerland, 2019. [Google Scholar] [CrossRef]
- Wolstenholme, E.F. A Case Study in Community Care using Systems Thinking. J. Oper. Res. Soc. 1993, 44, 925–934. [Google Scholar] [CrossRef]
- Wolstenholme, E.F. A Patient Flow Perspective of UK Health Services. Syst. Dyn. Rev. 1999, 15, 253–273. [Google Scholar] [CrossRef]
- Wolstenholme, E.F.; McKelvie, D. Hospital Delayed Transfer of Care (Delayed Discharges). In The Dynamics of Care; Springer: Cham, Switzerland, 2019. [Google Scholar] [CrossRef]
- Wolstenholme, E.F.; Monk, D.; McKelvie, D.; Smith, G. Influencing and Interpreting Health and Social Care Policy in the UK. In Complex Decision Making: Theory and Practice; Qudrat-Ullah, H., Spector, M., Davidsen, P., Eds.; New England Complex Systems Institute Book Series on Complexity; Springer: Berlin/Heidelberg, Germany, 2007. [Google Scholar]
- Wolstenholme, E.F. Towards the definition and use of a core set of archetypal structures in system dynamics. Syst. Dyn. Rev. 2003, 19, 7–26. [Google Scholar] [CrossRef]
- Wolstenholme, E.F. Using generic system archetypes to support thinking and learning. Syst. Dyn. Rev. 2004, 20, 341–356. [Google Scholar] [CrossRef]
- Wolstenholme, E.F.; McKelvie, D. Towards a Dynamic Theory of How Hospitals Cope in Times of High Demand. In The Dynamics of Care; Springer: Cham, Switzerland, 2019. [Google Scholar] [CrossRef]
- Wolstenholme, E.F.; Monk, D.; McKelvie, D.; Arnold, S. Coping but not Coping in Health and Social Care—masking the reality, of running organisations well beyond safe design capacity. Syst. Dyn. Rev. 2008, 23, 371–389. [Google Scholar] [CrossRef]
- Sterman, J.D. Business Dynamics: Systems Thinking and Modelling for a Complex World; Irwin McGraw-Hill: Boston, MA, USA, 2000. [Google Scholar]
- Richardson, G.P. Feedback Thought in Social Science and Systems Theory; University of Pennsylvania Press: Philadelphia, PA, USA; Pegasus Communications: Waltham, MA, USA, 1999. [Google Scholar]
- Senge, P.M. The Fifth Discipline: The Art and Practice of the Learning Organization; Doubleday/Currency: New York, NY, USA, 1990. [Google Scholar]
- Wolstenholme, E.F. System Enquiry: A System Dynamics Approach; John and Wiley and Sons: Chichester, UK, 1990. [Google Scholar]
- Stroth, P.L. Systems Thinking for Social Change; Chelsea Green Publishing: White River Junction, VT, USA, 2015. [Google Scholar]
- Sherwood, D. Seeing the Forest for the Trees: A Manager’s Guide to Applying Systems Thinking; Nicholas Brearley: London, UK, 2002. [Google Scholar]
- Nolte, E. NHS 70 Series—70 Years on, How Is the NHS Performing on Life Expectancy and Mortality? London School of Hygiene and Tropical Medicine: London, UK, 2018. [Google Scholar]
- Stylianou, N.; Fackrell, R.; Vasilakis, C. Are medical outliers associated with worse patient outcomes? BMJ Open 2017, 7, e015676. [Google Scholar] [CrossRef] [PubMed]
- Santamaria, J.D.; Tobin, A.E.; Anstey, M.H.; Smith, R.J.; Reid, D.A. Do outlier inpatients experience more emergency calls in hospital? An observational cohort study. Med. J. Aust. 2014, 200, 45–48. [Google Scholar] [CrossRef] [Green Version]
- Portsmouth Hospitals NHS Trust. Adult Outlier Policy, 5th ed.; Portsmouth Hospitals NHS Trust: Portsmouth, UK, 2018. [Google Scholar]
- Ewbank, L.; Thompson, J.; Mckenna, H. NHS Hospital Bed Numbers: Past, Present, Future; THE Kings Fund: London, UK, 2017. [Google Scholar]
- Nguyen, O.K.; Makam, A.N.; Clark, C. Vital Signs Are Still Vital: Instability on Discharge and the Risk of Post-Discharge Adverse Outcomes. J. Gen. Intern. Med. 2017, 32, 42–48. [Google Scholar] [CrossRef] [Green Version]
- Buie, V.C.; Owings, M.F.; DeFrances, C.J.; Golosinskiy, A. National Hospital Discharge Survey: Summary. Vital Health Stat. 2010, 13, 168. [Google Scholar]
- Smith, K.O.; Jackson, S. It’s Not All about Reducing Length of Stay; Carlike: Atlanta, GA, USA, 2017; Available online: https://stage.carelike.com/providers/resources/its-not-all-about-reducing-length-of-stay (accessed on 4 December 2018).
- Healthwatch News Report. NHS Needs to Do More to Understand Why People Are Returning to Hospital after Discharge; Healthwatch England: London, UK, 2017. [Google Scholar]
- Oxtoby, K. Preventing unsafe discharge from hospital. Nurs. Times 2018, 112, 14–15. [Google Scholar]
- Campbell, D. GPs Offered Cash to Refer Fewer People to Hospital. Health Policy Guardian, 28 February 2018. [Google Scholar]
- Triggle, N. Care Homes Could Solve NHS Bed-Blocking. BBC Health News, 1 March 2016. [Google Scholar]
- Smyth, C. NHS Hospitals Open Own Care Homes to Tackle Beds Crisis. Times Newspaper. 15 October 2016. Available online: https://www.thetimes.co.uk/article/nhs-hospitals-open-own-care-homes-to-tackle-beds-crisis-w8pvsztch (accessed on 10 June 2018).
- Adam. Moving on from Spot Purchasing in Domiciliary Care Commissioning. 2018. Available online: http://www.useadam.co.uk/news/moving-on-from-spot-purchasing-in-domiciliary-care-commissioning (accessed on 2 September 2019).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).