Enabling Mobility: A Simulation Model of the Health Care System for Major Lower-Limb Amputees to Assess the Impact of Digital Prosthetics Services
Abstract
1. Introduction
2. Materials and Methods
2.1. Literature Review
2.2. Data Collection
2.3. Model Description
2.3.1. Health Care System
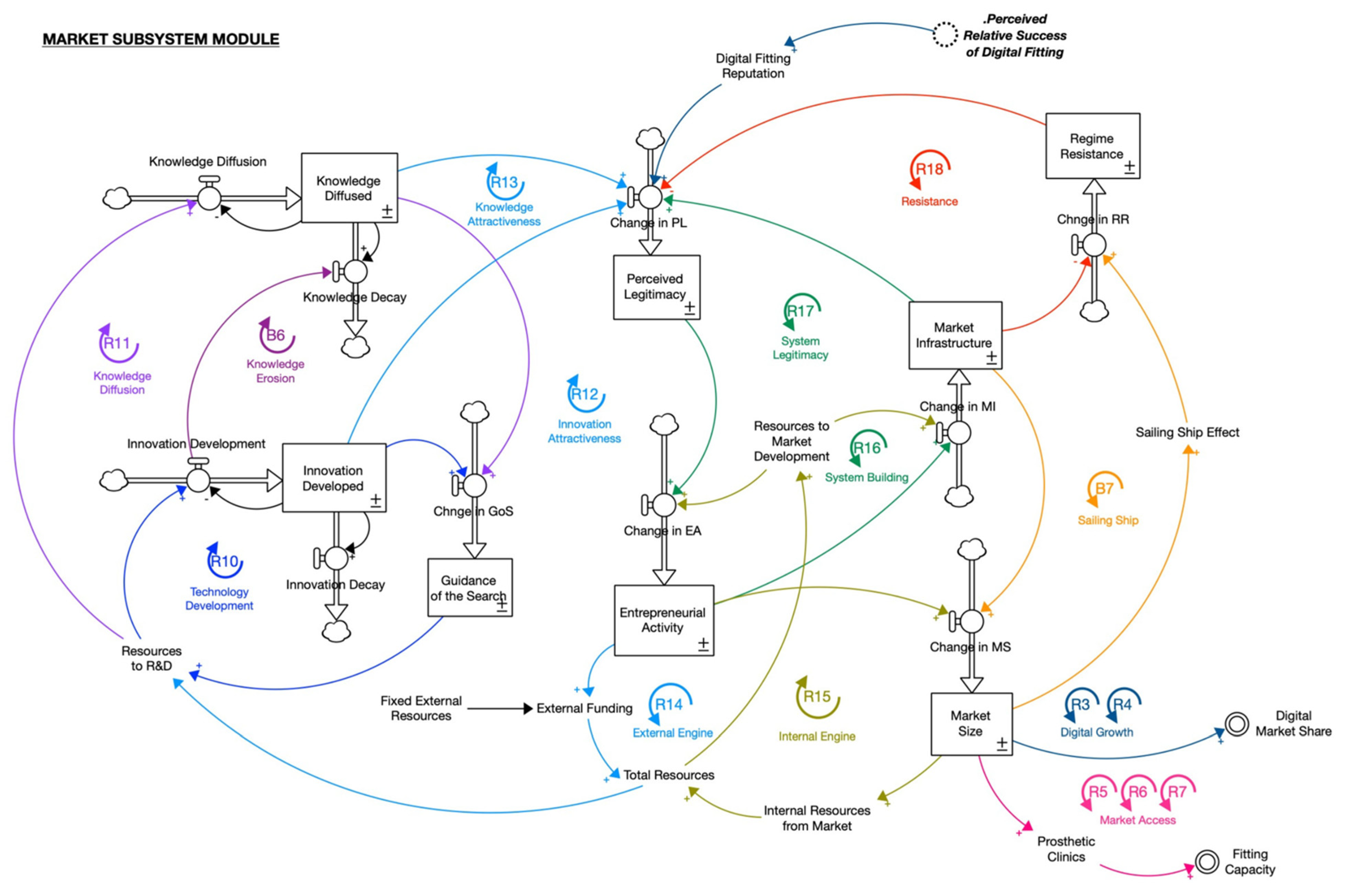
2.3.2. Market Subsystem
2.4. Model Validation
3. Simulation Results
3.1. Baseline Setup
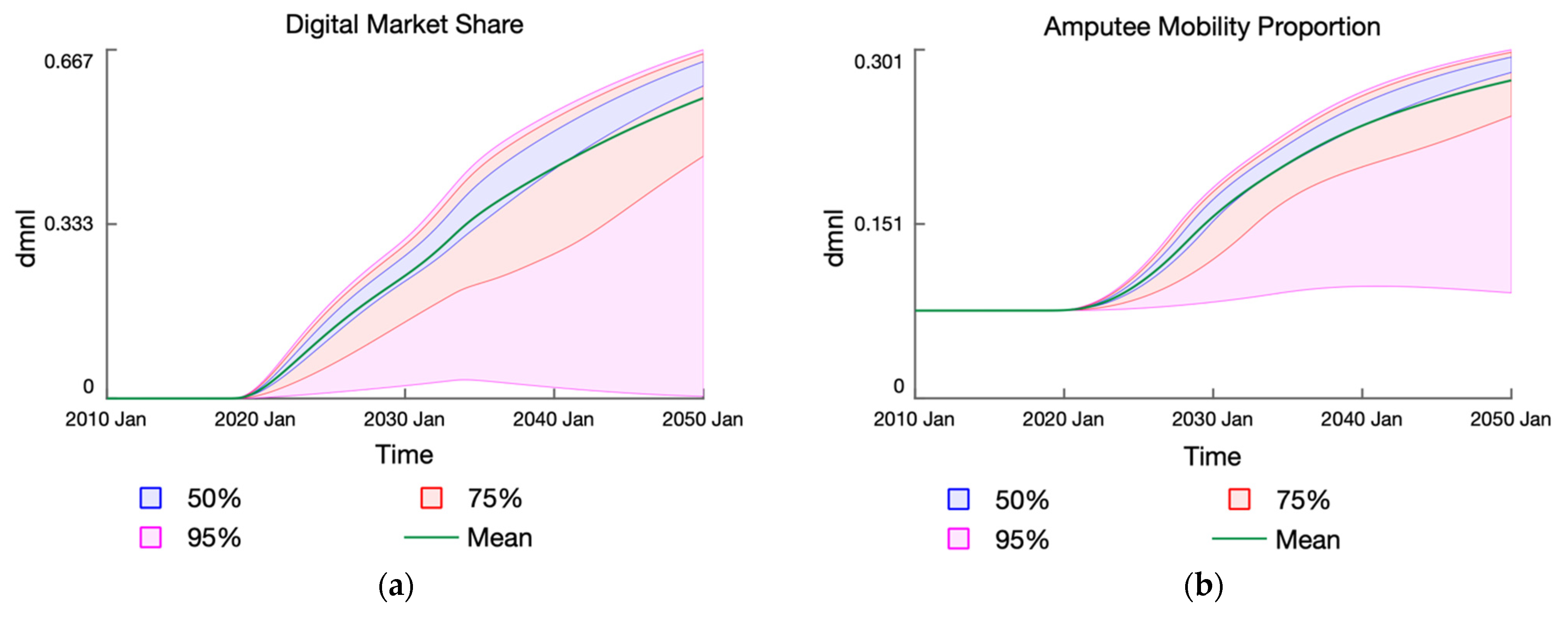
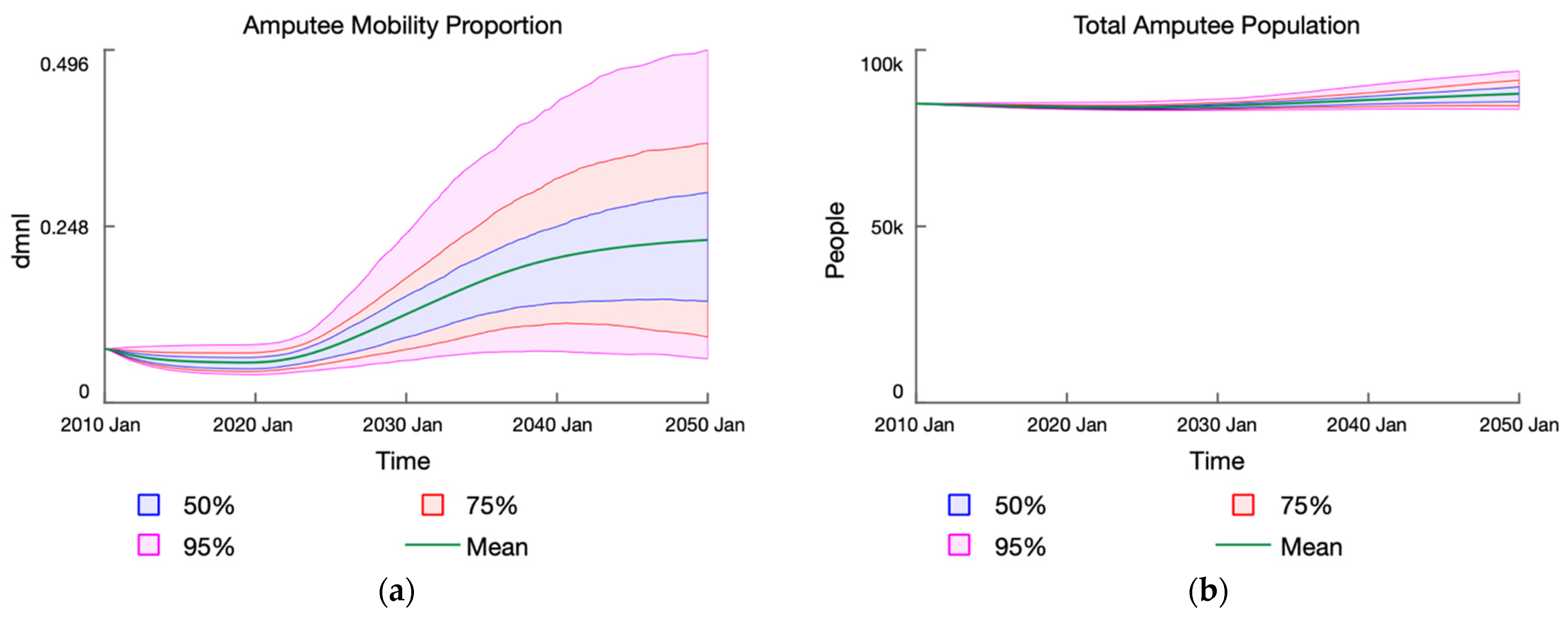
3.2. Baseline Results
3.3. Experimental Setup
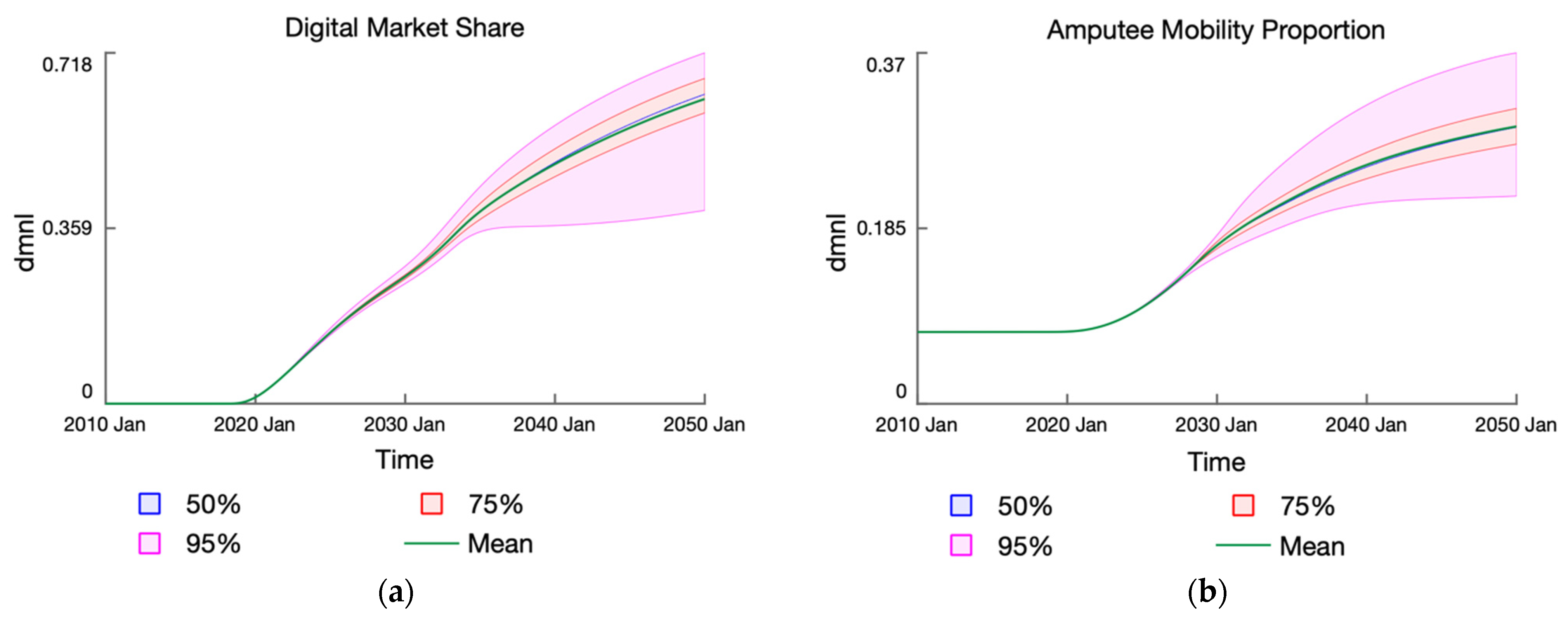
3.4. Experimental Results
3.5. Scenario Setup
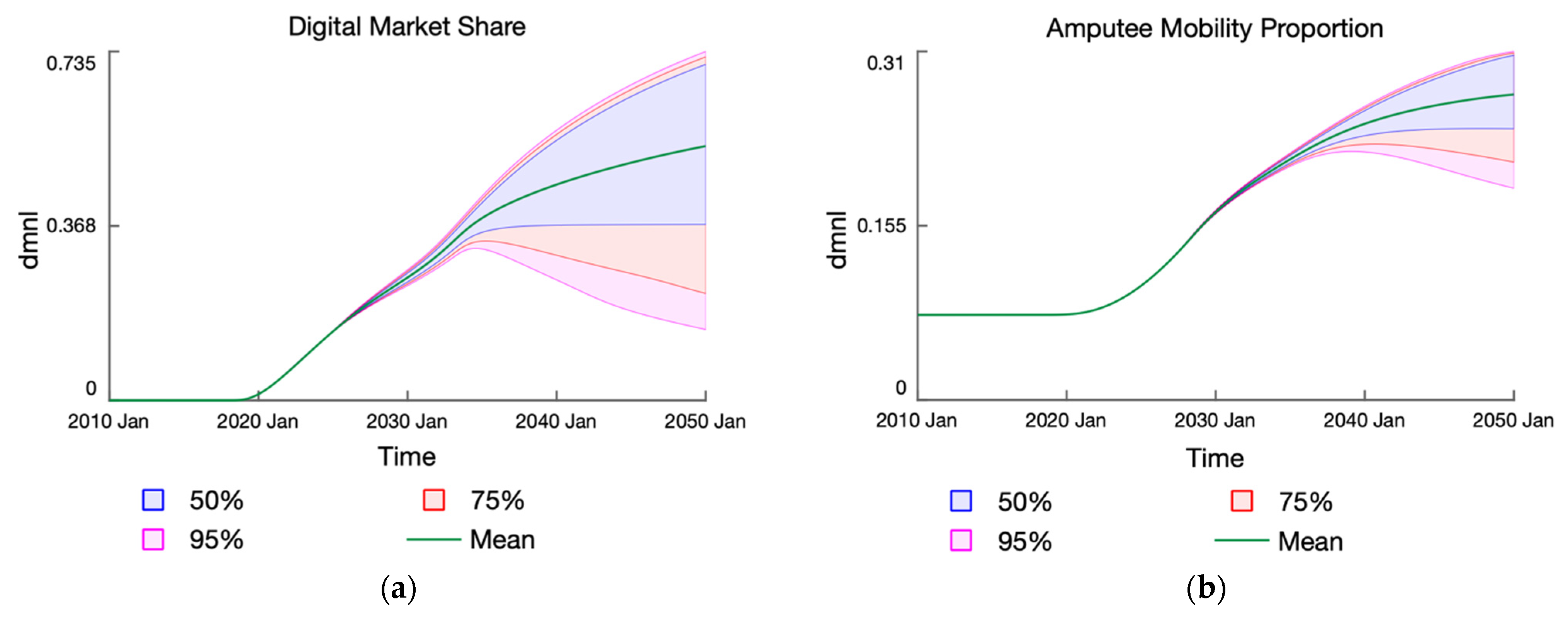
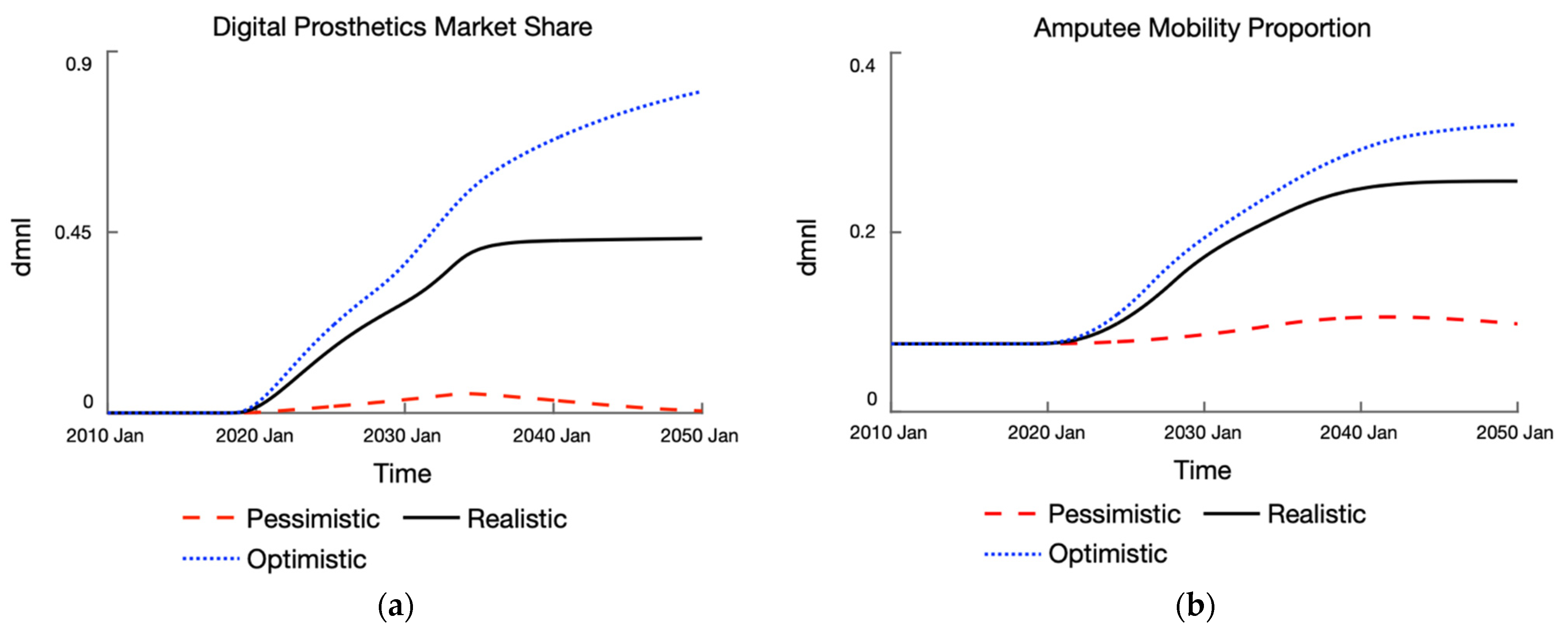
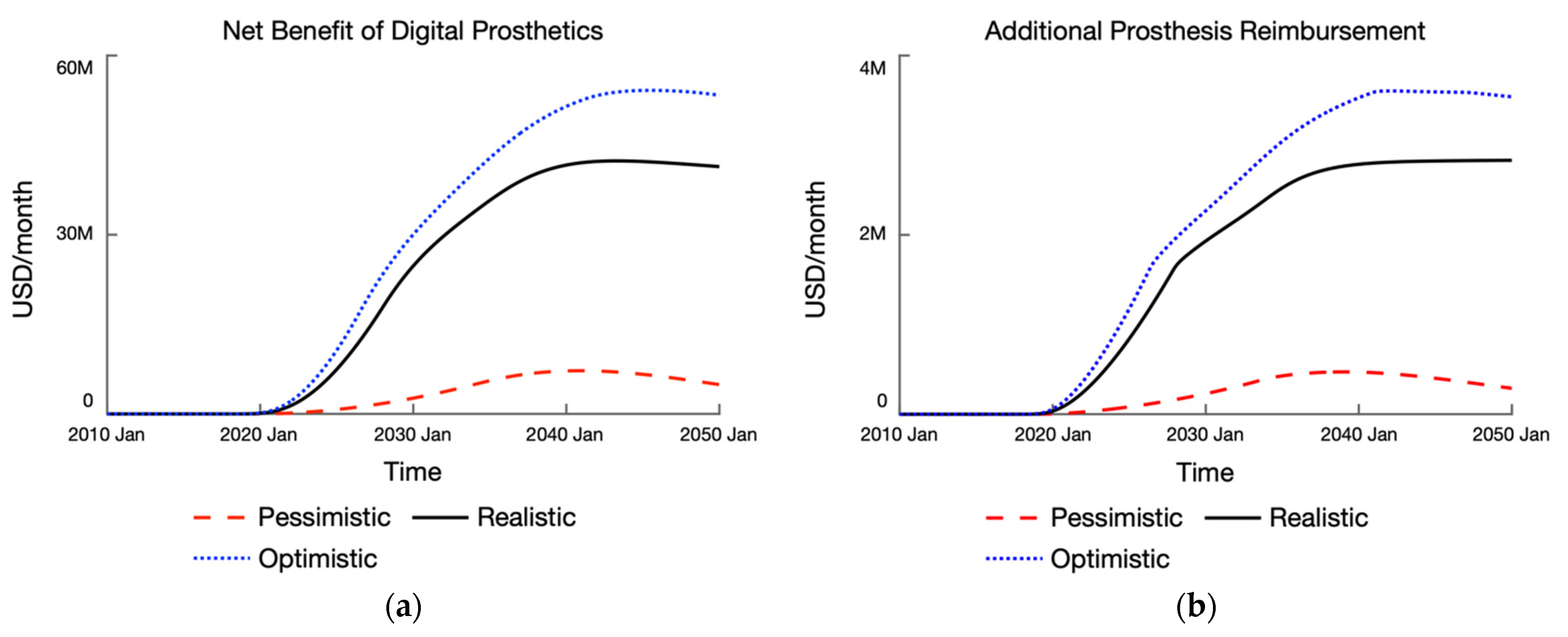
3.6. Scenario Results
4. Discussion
4.1. Strategic Insights
- While the External Engine loop provides the initial fuel for the various endogenous market formation processes, the System Legitimacy loop ultimately determines the trajectory of market growth for digital prosthetics. This loop generates internal resources from the market to sustain the growth in entrepreneurial activities, market infrastructure, perceived legitimacy of digital prosthetics, and its market size.
- The Digital Growth loops and Prosthesis Attractive loops are the key drivers for improving prosthetic accessibility and enabling mobility. With a higher market share of digital prosthetics, more amputees can receive prosthetics services and are incentivized to remain in or re-adopt prosthetics care.
- The Market Access loops are particularly important for driving the expansion of prosthetics clinics and service capacity, thus improving prosthetics accessibility over time. The strength of this loop determines the extent of the counteracting effect on the Access Constraint loops, which limits the mobility proportion.
- To best ensure the sustainability of the digital prosthetics market over the longer term, investment is needed in this emerging technological system to garner sufficient resources and momentum for sustained market growth. As seen in the sensitivity analyses, the model is behaviorally sensitive to parameters related to the internal and external resources in the market subsystem. High-leverage policies would thus seek to influence the resource flows in the system.
- Investments in digital prosthetics could improve accessibility and ameliorate the underuse of prosthesis amongst amputees, which enables mobility. Importantly, this results in a positive net benefit for society in terms of higher economic productivity and reduced economic costs.
- Besides the economic value of individuals, improving mobility appears to improve health, also preventing more amputee deaths over time.
- To maximize the impact on the mobility outcomes and net benefit of prosthetics services, policy planning must ensure that service capacity is expanded to meet fitting demand. The scenario analysis revealed that prosthetics accessibility is limited by service capacity even under optimistic market growth conditions. Policy planners should be cognizant of the effect of Prosthesis Lifecycle loop, which drives the pressure on fitting demand as the mobility outcomes improve over time.
4.2. Limitations and Further Research
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Feedback Loop Descriptions
à(+) PAD Amputation
Degradation à(+) Awaiting Replacement à(+) Prosthesis Replacement à(+) Amputees in Prosthetic Care
Prosthesis à(+) Amputees in Prosthetic Care
Digital Fitting à(+) Digital Market Size à(+) Digital Market Share à(+) Digital Prosthesis Referral à(+) Amputees in
Digital Prosthetic Care
Digital Fitting à(+) Digital Market Size à(+) Digital Market Share à(+) Digital Prosthesis Readoption à(+) Amputees in
Digital Prosthetic Care
Referral à(+) Amputees in Prosthetic Care
Accessibility à(+) Prosthesis Readoption
Prosthesis Replacement à(+) Amputees Awaiting Replacement
Fitting à(+) Digital Market Size à(+) Fitting Capacity à(+) Prosthetic Accessibility à(+) Prosthesis Referral à(+)
Amputees in Prosthetic Care
Fitting à(+) Digital Market Size à(+) Fitting Capacity à(+) Prosthetic Accessibility à(+) Readopt Prosthesis à(+)
Amputees in Prosthetic Care
Fitting à(+) Digital Market Size à(+) Fitting Capacity à(+) Prosthetic Accessibility à(+) Prosthesis Replacement à(+)
Amputees in Prosthetic Care
Digital Fitting à(–) Dropout Rate à(+) Abandon Prosthesis à(–) Amputees in Prosthetic Care
Digital Fitting à(+) Re-adoption Rate à(+) Readopt Prosthesis à(+) Amputees in Prosthetic Care
Digital Fitting à(–) Dropout Rate à(+) Abandon Prosthesis à(+) Limited Mobility à(+) Readopt Prosthesis à(+)
Amputees in Prosthetic Care
Development à(+) Innovation Developed
Diffusion à(+) Knowledge Diffused
à(+) Knowledge Decay à(–) Knowledge Diffused
External Funding à(+) Total Resources à(+) Resources to R&D à(+) Innovation Development à(+) Innovation
Developed
External Funding à(+) Total Resources à(+) Resources to R&D à(+) Knowledge Diffusion à(+) Knowledge Diffused
Development à(+) Entrepreneurial Activity
from Market à(+) Total Resources à(+) Resources to Market Development à(+) Entrepreneurial Activity
Legitimacy
Resources à(+) Resources to Market Development à(+) Market Infrastructure à(+)
Perceived Legitimacy à(+) Entrepreneurial Activity
Infrastructure à(–) Regime Resistance
Sailing Ship Effect à(+) Regime Resistance à(–) Perceived Legitimacy
Digital Fitting à(+) Digital Fitting Reputation à(+) Perceived Legitimacy à(+) Entrepreneurial Activity à(+) Market
Infrastructure à(+) Digital Market Size à(+) Digital Market Share à(+) Digital Prosthesis Referral à(+) Amputees in
Digital Prosthetic Care
Fitting à(+) Digital Fitting Reputation à(+) Perceived Legitimacy à(+) Entrepreneurial Activity à(+) Market
Infrastructure à(+) Digital Market Size à(+) Prosthetic Clinics à(+) Fitting Capacity à(+) Prosthetic Accessibility à(+)
Prosthesis Referral à(+) Amputees in Prosthetic Care
Appendix B. Sensitivity Analysis Results

References
- World Health Organization. WHO Standards for Prosthetics and Orthotics: Part 1; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Moxey, P.W.; Gogalniceanu, P.; Hinchliffe, R.J.; Loftus, I.M.; Jones, K.J.; Thompson, M.M.; Holt, P.J. Lower Extremity Amputations—A Review of Global Variability in Incidence: Lower Extremity Amputations-a Global Review. Diabet. Med. 2011, 28, 1144–1153. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, N.; Thomas, G.N.; Gill, P.; Torella, F. The Prevalence of Major Lower Limb Amputation in the Diabetic and Non-Diabetic Population of England 2003–2013. Diabetes Vasc. Dis. Res. 2016, 13, 348–353. [Google Scholar] [CrossRef] [PubMed]
- Geertzen, J.; van der Linde, H.; Rosenbrand, K.; Conradi, M.; Deckers, J.; Koning, J.; Rietman, H.S.; van der Schaaf, D.; van der Ploeg, R.; Schapendonk, J.; et al. Dutch Evidence-Based Guidelines for Amputation and Prosthetics of the Lower Extremity: Amputation Surgery and Postoperative Management. Part 1. Prosthet. Orthot. Int. 2015, 39, 351–360. [Google Scholar] [CrossRef] [PubMed]
- Kohler, F.; Cieza, A.; Stucki, G.; Geertzen, J.; Burger, H.; Dillon, M.P.; Schiappacasse, C.; Esquenazi, A.; Kistenberg, R.S.; Kostanjsek, N. Developing Core Sets for Persons Following Amputation Based on the International Classification of Functioning, Disability and Health as a Way to Specify Functioning. Prosthet. Orthot. Int. 2009, 33, 117–129. [Google Scholar] [CrossRef] [PubMed]
- Criqui, M.H.; Aboyans, V. Epidemiology of Peripheral Artery Disease. Circ. Res. 2015, 116, 1509–1526. [Google Scholar] [CrossRef] [PubMed]
- Meffen, A.; Pepper, C.J.; Sayers, R.D.; Gray, L.J. Epidemiology of Major Lower Limb Amputation Using Routinely Collected Electronic Health Data in the UK: A Systematic Review Protocol. BMJ Open 2020, 10, e037053. [Google Scholar] [CrossRef]
- Belch, J.J.F. Critical Issues in Peripheral Arterial Disease Detection and ManagementA Call to Action. Arch. Intern. Med. 2003, 163, 884. [Google Scholar] [CrossRef]
- Akarsu, S.; Tekin, L.; Safaz, I.; Göktepe, A.S.; Yazıcıoğlu, K. Quality of Life and Functionality after Lower Limb Amputations: Comparison between Uni- vs. Bilateral Amputee Patients. Prosthet. Orthot. Int. 2013, 37, 9–13. [Google Scholar] [CrossRef]
- Horgan, O.; MacLachlan, M. Psychosocial Adjustment to Lower-Limb Amputation: A Review. Disabil. Rehabil. 2004, 26, 837–850. [Google Scholar] [CrossRef]
- Roberts, T.L.; Pasquina, P.F.; Nelson, V.S.; Flood, K.M.; Bryant, P.R.; Huang, M.E. Limb Deficiency and Prosthetic Management. 4. Comorbidities Associated With Limb Loss. Arch. Phys. Med. Rehabil. 2006, 87, 21–27. [Google Scholar] [CrossRef]
- Darter, B.J.; Hawley, C.E.; Armstrong, A.J.; Avellone, L.; Wehman, P. Factors Influencing Functional Outcomes and Return-to-Work After Amputation: A Review of the Literature. J. Occup. Rehabil. 2018, 28, 656–665. [Google Scholar] [CrossRef] [PubMed]
- Stewart, C.C.; Berhaneselase, E.; Morshed, S. The Burden of Patients With Lower Limb Amputations in a Community Safety-Net Hospital. J. Am. Acad. Orthop. Surg. 2022, 30, e59–e66. [Google Scholar] [CrossRef] [PubMed]
- Pasquina, P.F.; Carvalho, A.J.; Sheehan, T.P. Ethics in Rehabilitation: Access to Prosthetics and Quality Care Following Amputation. AMA J. Ethics 2015, 17, 535–546. [Google Scholar] [CrossRef] [PubMed]
- Raichle, K.A.; Hanley, M.A.; Molton, I.; Kadel, N.J.; Campbell, K.; Phelps, E.; Ehde, D.; Smith, D.G. Prosthesis Use in Persons with Lower- and Upper-Limb Amputation. JRRD 2008, 45, 961–972. [Google Scholar] [CrossRef] [PubMed]
- ProsFit Technologies. Solution to Mobility and Quality of Life for Millions of Amputees at Scale; ProsFit Technologies JSC: Sofia, Bulgaria, 2022; (Unpublished). [Google Scholar]
- Wyss, D.; Lindsay, S.; Cleghorn, W.L.; Andrysek, J. Priorities in Lower Limb Prosthetic Service Delivery Based on an International Survey of Prosthetists in Low- and High-Income Countries. Prosthet. Orthot. Int. 2015, 39, 102–111. [Google Scholar] [CrossRef] [PubMed]
- Silva, K.; Rand, S.; Cancel, D.; Chen, Y.; Kathirithamby, R.; Stern, M. Three-Dimensional (3-D) Printing: A Cost-Effective Solution for Improving Global Accessibility to Prostheses. PMR 2015, 7, 1312–1314. [Google Scholar] [CrossRef]
- Kozbunarova, A. ProsFit: The Startup That Aims To Democratize the Prosthetic Industry. Trending Topics 2019. Available online: https://www.trendingtopics.eu/prosfit-prosthetic-industry-democratization-pandofit/ (accessed on 28 December 2022).
- Hutchison, A. Distributed Care: The Third Dimension! LinkedIn 2020. Available online: https://www.linkedin.com/pulse/distributed-care-third-dimension-alan-hutchison/ (accessed on 28 December 2022).
- Sterman, J. Business Dynamics: Systems Thinking and Modeling for a Complex World; Irwin/McGraw-Hill: Boston, MA, USA, 2000; ISBN 978-0-07-231135-8. [Google Scholar]
- Hovmand, P.S. Community Based System Dynamics; SpringerLink; Springer: New York, NY, USA, 2014; ISBN 978-1-4614-8763-0. [Google Scholar]
- Richardson, G.P. Core of System Dynamics. In Encyclopedia of Complexity and Systems Science; Meyers, R.A., Ed.; Springer: Berlin, Heidelberg, 2019; pp. 1–10. ISBN 978-3-642-27737-5. [Google Scholar]
- Forrester, J.W. Principles of Systems; Pegasus Communications, Inc.: Waltham, MA, USA, 1968; ISBN 978-1-883823-41-2. [Google Scholar]
- Richardson, G.P. Reflections on the Foundations of System Dynamics: Foundations of System Dynamics. Syst. Dyn. Rev. 2011, 27, 219–243. [Google Scholar] [CrossRef]
- Sohn, T.-W.; Surkis, J. System Dynamics: A Methodology for Testing Dynamic Behavioral Hypotheses. IEEE Trans. Syst. Man. Cybern. 1985, SMC-15, 399–408. [Google Scholar] [CrossRef]
- Darabi, N.; Hosseinichimeh, N. System Dynamics Modeling in Health and Medicine: A Systematic Literature Review. Syst. Dyn. Rev. 2020, 36, 29–73. [Google Scholar] [CrossRef]
- Davahli, M.R.; Karwowski, W.; Taiar, R. A System Dynamics Simulation Applied to Healthcare: A Systematic Review. IJERPH 2020, 17, 5741. [Google Scholar] [CrossRef] [PubMed]
- Homer, J.B.; Hirsch, G.B. System Dynamics Modeling for Public Health: Background and Opportunities. Am. J. Public Health 2006, 96, 452–458. [Google Scholar] [CrossRef] [PubMed]
- Rajah, J.K. Enabling Mobility for Persons with Major Lower-Limb Amputations: A Model-Based Study of the Impact of Digital Prosthetics Service Provision on Mobility Outcomes. Master Thesis, University of Bergen, Bergen, Norway, 2022. [Google Scholar]
- Rajah, J.K.; Hutchison, C.; Chernicoff, W.; Gonçalves, P. The Dynamics of Prosthetics Care Continuum for Persons with Amputation. In Proceedings of the International Conference of the System Dynamics Society 2022, Frankfurt, Germany, 19 July 2022. [Google Scholar]
- Paich, M.; Peck, C.; Valant, J.J. Pharmaceutical Product Strategy; CRC Press: Boca Raton, FL, USA, 2004; ISBN 978-0-203-49252-9. [Google Scholar]
- Homer, J.B. A Diffusion Model with Application to Evolving Medical Technologies. Technol. Forecast. Soc. Change 1987, 31, 197–218. [Google Scholar] [CrossRef]
- Uriona, M.; Grobbelaar, S.S. Innovation System Policy Analysis through System Dynamics Modelling: A Systematic Review. Sci. Public Policy 2019, 46, 28–44. [Google Scholar] [CrossRef]
- Hekkert, M.P.; Suurs, R.A.A.; Negro, S.O.; Kuhlmann, S.; Smits, R.E.H.M. Functions of Innovation Systems: A New Approach for Analysing Technological Change. Technol. Forecast. Soc. Change 2007, 74, 413–432. [Google Scholar] [CrossRef]
- Walrave, B.; Raven, R. Modelling the Dynamics of Technological Innovation Systems. Res. Policy 2016, 45, 1833–1844. [Google Scholar] [CrossRef]
- Wicki, S.; Hansen, E.G. Clean Energy Storage Technology in the Making: An Innovation Systems Perspective on Flywheel Energy Storage. J. Clean. Prod. 2017, 162, 1118–1134. [Google Scholar] [CrossRef]
- Walrave, B.; Raven, R. Modelling the Dynamics of TIS-Model Appendix. Res. Policy 2016, 45, 1833–1844. [Google Scholar]
- Lee, B.H.; Struben, J.; Bingham, C.B. Collective Action and Market Formation: An Integrative Framework. Strat Mgmt. J. 2018, 39, 242–266. [Google Scholar] [CrossRef]
- Forrester, J.W. Industrial Dynamics; M.I.T. Press: Cambridge, MA, USA, 1961; ISBN 978-0-262-06003-5. [Google Scholar]
- Király, G.; Miskolczi, P. Dynamics of Participation: System Dynamics and Participation-An Empirical Review. Syst. Res. Behav. Sci. 2019, 36, 199–210. [Google Scholar] [CrossRef]
- McCardle-Keurentjes, M.H.F.; Rouwette, E.A.J.A.; Vennix, J.A.M.; Jacobs, E. Potential Benefits of Model Use in Group Model Building: Insights from an Experimental Investigation. Syst. Dyn. Rev. 2018, 34, 354–384. [Google Scholar] [CrossRef]
- Office for National Statistics Population Estimates and Deaths by Single Year of Age for England and Wales and the United Kingdom, 1961 to 2014; UK Statistics Authority: London, UK, 2015.
- Office for National Statistics. Long-Term International Migration 2.07, Age and Sex, UK and England and Wales; UK Statistics Authority: London, UK, 2020.
- Office for National Statistics United Kingdom Population Mid-Year Estimate; UK Statistics Authority: London, UK, 2021.
- Office for National Statistics 2020-Based Interim National Population Projections; UK Statistics Authority: London, UK, 2022.
- Office for National Statistics Age-Specific Fertility Rates (ASFRs) and Total Fertility Rates (TFRs) for UK-Born and Non-UK-Born Women Living in the UK, Scotland and Northern Ireland: 2004 to 2020; UK Statistics Authority: London, UK, 2022.
- Office for National Statistics. Mortality Rates (Mx), 2020-Based Principal Projection, UK (Ages 0 to 125 Years, 1961 to 2120); UK Statistics Authority: London, UK, 2022.
- Vascular Services Quality Improvement Programme. In 2015 Annual Report of the National Vascular Registry; Healthcare Quality Improvement Partnership: London, UK, 2015.
- Vascular Services Quality Improvement Programme. In 2016 Annual Report of the National Vascular Registry; Healthcare Quality Improvement Partnership: London, UK, 2016.
- Vascular Services Quality Improvement Programme. In 2017 Annual Report of the National Vascular Registry; Healthcare Quality Improvement Partnership: London, UK, 2017.
- Vascular Services Quality Improvement Programme. In 2018 Annual Report of the National Vascular Registry; Healthcare Quality Improvement Partnership: London, UK, 2018.
- Vascular Services Quality Improvement Programme. In 2019 Annual Report of the National Vascular Registry; Healthcare Quality Improvement Partnership: London, UK, 2019.
- Vascular Services Quality Improvement Programme. In 2020 Annual Report of the National Vascular Registry; Healthcare Quality Improvement Partnership: London, UK, 2020.
- Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Results; Institute for Health Metrics and Evaluation: Seattle, WA, USA, 2020. [Google Scholar]
- Hutchison, C. ProsFit Health Economics Model; ProsFit Technologies JSC: Sofia, Bulgaria, 2021; (Unpublished Data Set). [Google Scholar]
- Farndon, L.; Stephenson, J.; Binns-Hall, O.; Knight, K.; Fowler-Davis, S. The PodPAD Project: A Podiatry-Led Integrated Pathway for People with Peripheral Arterial Disease in the UK—A Pilot Study. J. Foot Ankle. Res. 2018, 11, 26. [Google Scholar] [CrossRef] [PubMed]
- Cea-Soriano, L.; Fowkes, F.G.R.; Johansson, S.; Allum, A.M.; García Rodriguez, L.A. Time Trends in Peripheral Artery Disease Incidence, Prevalence and Secondary Preventive Therapy: A Cohort Study in The Health Improvement Network in the UK. BMJ Open 2018, 8, e018184. [Google Scholar] [CrossRef] [PubMed]
- Rheinstein, J.; Carroll, K.; Stevens, P. Prosthetic Care for the Mangled Extremity. In The Mangled Extremity; Pensy, R.A., Ingari, J.V., Eds.; Springer International Publishing: Cham, Switzerland, 2021; pp. 257–283. ISBN 978-3-319-56647-4. [Google Scholar]
- Davie-Smith, F.; Hebenton, J.; Scott, H. A Survey of the Lower Limb Amputee Population in Scotland: 2015 Full Report; Scottish Physiotherapy Amputee Research Group: Scotland, UK, 2018. [Google Scholar]
- Chernicoff, W.; Naumov, S.; Sarkani, S.; Holzer, T. Modeling Market Dynamics in a Super Octane Ethanol Fuel Blend-Vehicle Power-Train System: Understanding the Role of Consumer Perception in Ethanol Market Growth. JPCS 2014, 1, 110–137. [Google Scholar] [CrossRef]
- Nieuwenhuijsen, J.; de Almeida Correia, G.H.; Milakis, D.; van Arem, B.; van Daalen, E. Towards a Quantitative Method to Analyze the Long-Term Innovation Diffusion of Automated Vehicles Technology Using System Dynamics. Transp. Res. Part C Emerg. Technol. 2018, 86, 300–327. [Google Scholar] [CrossRef]
- Suurs, R.A.A. Motors of Sustainable Innovation: Towards a Theory on the Dynamics of Technological Innovation Systems; Utrecht University: Utrecht, the Netherlands, 2009. [Google Scholar]
- De Liso, N.; Arima, S.; Filatrella, G. The “Sailing-Ship Effect” as a Technological Principle. Ind. Corp. Change 2022, 30, 1459–1478. [Google Scholar] [CrossRef]
- De Liso, N.; Filatrella, G. On Technology Competition: A Formal Analysis of the ‘Sailing-Ship Effect’. Econ. Innov. New Technol. 2008, 17, 593–610. [Google Scholar] [CrossRef]
- Senge, P.M.; Forrester, J.W. Tests for Building Confidence in System Dynamics Models. In System Dynamics; Legasto, A.A., Forrester, J.W., Lyneis, J.M., Eds.; North-Holland Publishing Company: Amsterdam, the Netherlands, 1980; pp. 209–228. [Google Scholar]
- Barlas, Y. Formal Aspects of Model Validity and Validation in System Dynamics. Syst. Dyn. Rev. 1996, 12, 183–210. [Google Scholar] [CrossRef]
- Burhenne, S.; Jacob, D.; Henze, G.P. Sampling Based on Sobol′ Sequences for Monte Carlo Techniques Applied to BuildingSimulations. In Proceedings of the Proceedings of the Building Simulation 2011: 12th Conference of International Building Performance SimulationAssociation, Sydney, Australia, 14 November 2011; pp. 1816–1823. [Google Scholar]
- Webster, J.B.; Hakimi, K.N.; Williams, R.M.; Turner, A.P.; Norvell, D.C.; Czerniecki, J.M. Prosthetic Fitting, Use, and Satisfaction Following Lower-Limb Amputation: A Prospective Study. JRRD 2012, 49, 1493. [Google Scholar] [CrossRef]
- Pell, J.P.; Donnan, P.T.; Fowkes, F.G.R.; Ruckley, C.V. Quality of Life Following Lower Limb Amputation for Peripheral Arterial Disease. Eur. J. Vasc. Surg. 1993, 7, 448–451. [Google Scholar] [CrossRef] [PubMed]
- Andersen, D.F.; Richardson, G.P.; Vennix, J.A.M. Group Model Building: Adding More Science to the Craft. Syst. Dyn. Rev. 1997, 13, 187–201. [Google Scholar] [CrossRef]




| Data Source | Description |
|---|---|
| UK Office for National Statistics [43,44,45,46,47,48] | UK population estimates for fertility rate and mortality rate |
| Healthcare Quality Improvement Partnership [49,50,51,52,53,54] | UK National Vascular Registry statistics on PAD-related major lower limb amputations and clinical outcomes |
| Global Burden of Disease Collaborative Network [55] | UK estimates for yearly prevalence and incidence estimates on PAD as well as lower limb amputations from injuries as a cause between 2010 and 2019 |
| ProsFit Technologies [56] | UK health economics data for estimating economic costs and net benefit of prosthetic service provision |
| Model Sector | Parameter | Range | Sensitivity |
|---|---|---|---|
| Prosthetic Care | Reference Dropout Fraction (Eligible for Prosthesis) | 0.01–0.50 | Numerical |
| Reference Dropout Fraction (Initial Device) | 0.01–0.50 | Numerical | |
| Reference Dropout Fraction (Matured Limb) | 0.01–0.50 | Numerical | |
| Reference Readoption Fraction | 0.01–0.50 | Numerical | |
| Market Formation | Market Size Threshold | 0.025–0.075 | Behavioral * |
| Relative External Resources Size | 0–9 | Behavioral * | |
| Sensitivity of Clinics to Market Size | 0.25–0.75 | Numerical | |
| Sensitivity of Resources to Market Size | 0.5–1.5 | Behavioral * | |
| Steepness Effect of Total Resources on EA | 1.25–3.75 | Numerical | |
| Steepness Effect of EA on Market Infrastructure | 0.2–0.6 | Numerical | |
| Steepness Effect of Legitimacy on EA | 0.2–0.6 | Numerical | |
| Steepness Effect of Total Resources on Infrastructure | 1.25–3.75 | Numerical | |
| Time to Adjust Clinics | 12–36 | Numerical | |
| Time to Adjust Entrepreneurial Activity | 6–18 | Numerical | |
| Time to Adjust Market Infrastructure | 30–90 | Numerical | |
| Time to Adjust Market Size | 12–36 | Numerical | |
| Time to Perceive Legitimacy | 6–18 | Numerical | |
| Weight of Entrepreneurial Activity | 0.25–0.75 | Behavioral * | |
| Weight of Perceived Legitimacy | 0.25–0.75 | Numerical | |
| Innovation Diffusion | Time to Decay | 30–90 | Numerical |
| Indicator | Result | Units |
|---|---|---|
| Total Amputee Population | 84.8 K | People |
| Medically Eligible Amputee Population | 71.9 K | People |
| Amputees fitted with Prosthesis | 5.5 K | People |
| Amputee Mobility Proportion | 0.07 | Dimensionless |
| Prosthetics Accessibility | 0.12 | Dimensionless |
| Economic Productivity | 14 M | USD/Month |
| Economic Cost | 210 M | USD/Month |
| Prosthesis Reimbursement | 1.94 M | USD/Month |
| Parameter | Pessimistic | Realistic | Optimistic | Remarks |
|---|---|---|---|---|
| Relative External Resources Size | 1.27 | 4.78 | 8.02 | The higher the figure, the larger the size of the external resources brought in from entrepreneurial activity relative to a certain normal size. |
| Market Size Threshold | 0.04 | 0.05 | 0.05 | The threshold is the base value of the Relative Market Size, which determines how much the internal resources generated by market grows beyond the normal amount. A higher threshold means that the nascent market must grow to a larger extent before becoming profitable. |
| Sensitivity of Resources to Market Size | 1.20 | 0.72 | 0.95 | A sensitivity of less than 1 results in a less than proportional change in the Relative Internal Resources to changes in the Relative Market. Conversely, a sensitivity of more than 1 results in a more than proportional relative change. |
| Weight of Entrepreneurial Activity | 0.65 | 0.32 | 0.27 | The smaller the value, the more weight is placed on the effect of total resources available for market development on market infrastructure than on the effect of entrepreneurial activities, vice versa. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rajah, J.K.; Chernicoff, W.; Hutchison, C.J.; Gonçalves, P.; Kopainsky, B. Enabling Mobility: A Simulation Model of the Health Care System for Major Lower-Limb Amputees to Assess the Impact of Digital Prosthetics Services. Systems 2023, 11, 22. https://doi.org/10.3390/systems11010022
Rajah JK, Chernicoff W, Hutchison CJ, Gonçalves P, Kopainsky B. Enabling Mobility: A Simulation Model of the Health Care System for Major Lower-Limb Amputees to Assess the Impact of Digital Prosthetics Services. Systems. 2023; 11(1):22. https://doi.org/10.3390/systems11010022
Chicago/Turabian StyleRajah, Jefferson K., William Chernicoff, Christopher J. Hutchison, Paulo Gonçalves, and Birgit Kopainsky. 2023. "Enabling Mobility: A Simulation Model of the Health Care System for Major Lower-Limb Amputees to Assess the Impact of Digital Prosthetics Services" Systems 11, no. 1: 22. https://doi.org/10.3390/systems11010022
APA StyleRajah, J. K., Chernicoff, W., Hutchison, C. J., Gonçalves, P., & Kopainsky, B. (2023). Enabling Mobility: A Simulation Model of the Health Care System for Major Lower-Limb Amputees to Assess the Impact of Digital Prosthetics Services. Systems, 11(1), 22. https://doi.org/10.3390/systems11010022







