Towards Optimal pH of the Skin and Topical Formulations: From the Current State of the Art to Tailored Products
Abstract
1. Introduction
2. Methodology
3. Skin Barrier
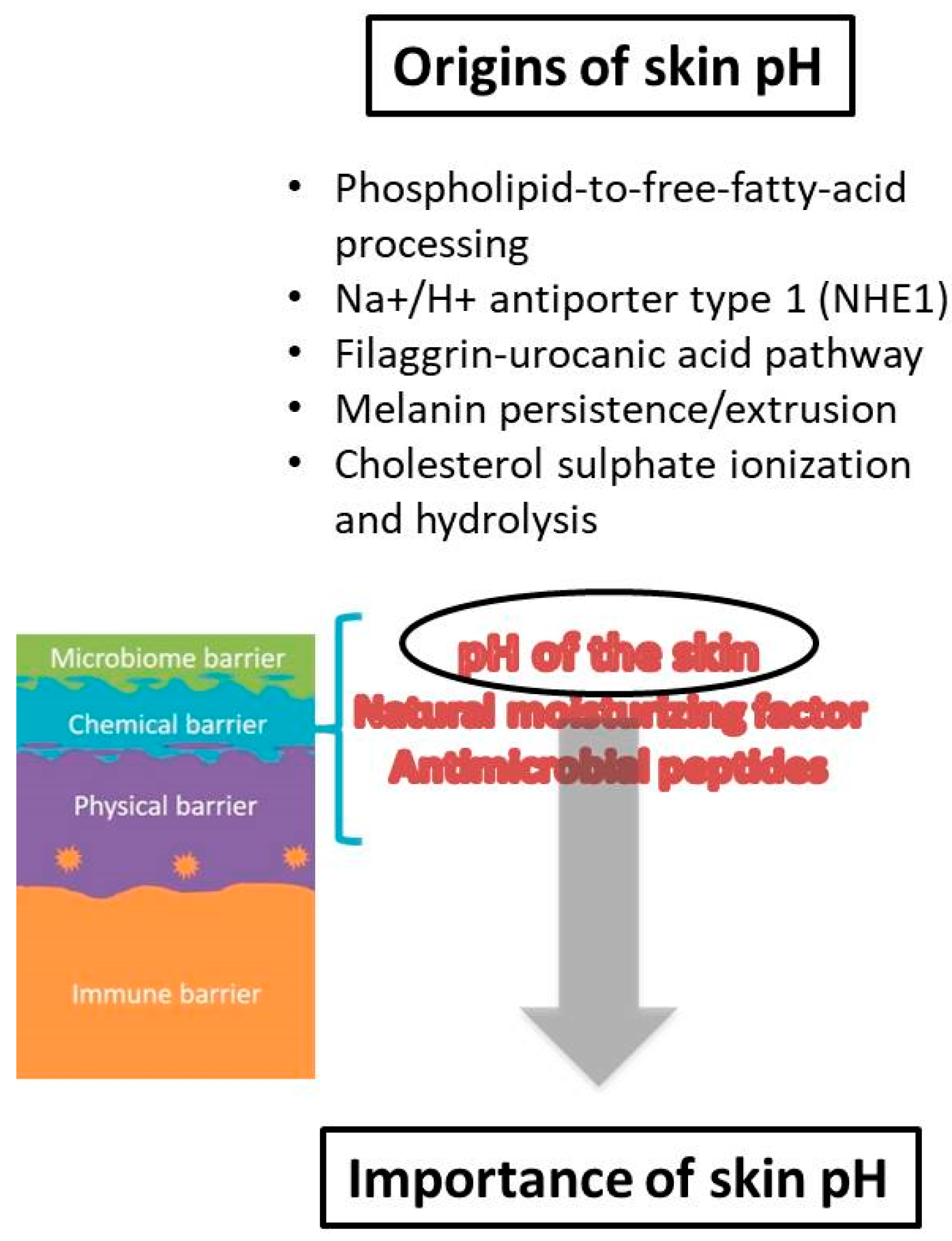
4. Skin pH
5. Origins, Formation and Maintenance of Skin pH
6. Importance of Acidic Skin pH
7. pH of the Skin and Topical Formulations
7.1. Cleansers
7.2. Skin Care Products
8. Skin Health Maintenance
9. Concluding Remarks
Author Contributions
Funding
Conflicts of Interest
References
- Rippke, F.; Schreiner, V.; Schwanitz, H.V. The Acidic Milieu of the Horny Layer New Findings on the Physiology and Path-ophysiology of Skin pH. Am. J. Clin. Dermatol. 2002, 3, 261–272. [Google Scholar] [CrossRef]
- Eyerich, S.; Eyerich, K.; Traidl-Hoffmann, C.; Biedermann, T. Cutaneous Barriers and Skin Immunity: Differentiating A Connected Network. Trends Immunol. 2018, 39, 315–327. [Google Scholar] [CrossRef]
- Wierzbicka, D.M.; Karczewski, J.; Dobrowolska-Zachwieja, A.; Adamski, Z. The microbiome and dermatological diseases. Postepy Hig. Med. Dosw. 2015, 7, 978–985. [Google Scholar]
- Kong, J.; Segre, H. The Molecular Revolution in Cutaneous Biology: Investigating the Skin Microbiome. J. Investig. Dermatol. 2017, 137, e119–e122. [Google Scholar] [CrossRef]
- Belkaid, Y.; Segre, J.A. Dialogue between skin microbiota and immunity. Science 2014, 346, 954–959. [Google Scholar] [CrossRef] [PubMed]
- Harder, J.; Schröder, J.-M.; Gläser, R. The skin surface as antimicrobial barrier: Present concepts and future outlooks. Exp. Dermatol. 2012, 22, 1–5. [Google Scholar] [CrossRef]
- Fry, L.; Baker, B.S.; Powles, A.V.; Fahlen, A.; Engstrand, L. Is chronic plaque psoriasis triggered by microbiota in the skin? Br. J. Dermatol. 2013, 169, 47–52. [Google Scholar] [CrossRef]
- Fowler, J. Understanding the Role of Natural Moisturizing Factor in Skin Hydration. Pract. Dermatol. 2012, 7, 36–40. [Google Scholar]
- Baroni, A.; Buommino, E.; De Gregorio, V.; Ruocco, E.; Ruocco, V.; Wolf, R. Structure and function of the epidermis related to barrier properties. Clin. Dermatol. 2012, 30, 257–262. [Google Scholar] [CrossRef]
- Menon, G.K.; Cleary, G.W.; Lane, M.E. The structure and function of the stratum corneum. Int. J. Pharm. 2012, 435, 3–9. [Google Scholar] [CrossRef]
- Haftek, M. Epidermal barrier disorders and corneodesmosome defects. Cell Tissue Res. 2015, 360, 483–490. [Google Scholar] [CrossRef] [PubMed]
- Matsui, T.; Amagai, M. Dissecting the formation, structure and barrier function of the stratum corneum. Int. Immunol. 2015, 27, 269–280. [Google Scholar] [CrossRef]
- Van Smeden, J.; Janssens, M.; Gooris, G.; Bouwstra, J. The important role of stratum corneum lipids for the cutaneous barrier function. BBA Mol. Cell Biol. Lipids 2014, 1841, 295–313. [Google Scholar] [CrossRef]
- Ishida-Yamamoto, A.; Igawa, S. Genetic skin diseases related to desmosomes and corneodesmosomes. J. Dermatol. Sci. 2014, 74, 99–105. [Google Scholar] [CrossRef]
- Bäsler, K.; Brandner, J.M. Tight junctions in skin inflammation. Pflugers Arch. 2017, 469, 3–14. [Google Scholar] [CrossRef]
- Elias, P.M.; Gruber, R.; Crumrine, D.; Menon, G.; Williams, M.L.; Wakefield, J.S.; Holleran, W.M.; Uchida, Y. Formation and functions of the corneocyte lipid envelope (CLE). BBA Mol. Cell Biol. Lipids 2014, 1841, 314–318. [Google Scholar] [CrossRef] [PubMed]
- Van Smeden, J.; Bouwstra, J.A. Stratum corneum lipids: Their role for the skin barrier function in healthy subjects and atopic dermatitis patients. Curr. Probl. Dermatol. 2016, 49, 8–26. [Google Scholar] [PubMed]
- Bhattacharya, N.; Sato, W.J.; Kelly, A.; Ganguli-Indra, G.; Indra, A.K. Epidermal Lipids: Key Mediators of Atopic Dermatitis Pathogenesis. Trends Mol. Med. 2019, 25, 551–562. [Google Scholar] [CrossRef]
- Proksch, E. pH in nature, humans and skin. J. Dermatol. 2018, 45, 1044–1052. [Google Scholar] [CrossRef]
- Schade, H.; Marchionini, A. Zur physikalischen Chemie der Hautoberfläche. Arch. Dermatol. Res. 1928, 154, 690–716. [Google Scholar] [CrossRef]
- Braun-Falco, O.; Korting, H.C. Normal pH value of the skin. Hautarzt 1986, 37, 126–129. [Google Scholar] [PubMed]
- Segger, D.; Aßmus, U.; Brock, M.; Erasmy, J.; Finkel, P.; Fitzner, A.; Heuss, H.; Kortemeier, U.; Munke, S.; Rheinländer, T.; et al. Multicenter study on measurement of the natural pH of the skin surface. Int. J. Cosmet. Sci. 2008, 30, 75. [Google Scholar] [CrossRef]
- Kleesz, P.; Darlenski, R.; Fluhr, J. Full-Body Skin Mapping for Six Biophysical Parameters: Baseline Values at 16 Anatomical Sites in 125 Human Subjects. Skin Pharmacol. Physiol. 2012, 25, 25–33. [Google Scholar] [CrossRef]
- Schmitt, T.; Neubert, R.H. State of the art in Stratum Corneum research: The biophysical properties of ceramides. Chem. Phys. Lipids 2018, 216, 91–103. [Google Scholar] [CrossRef]
- Levin, J.; Maibach, H. pH buffering considerations in mature skin. Cosm. Toil. 2011, 126, 422–428. [Google Scholar]
- Levin, J.; Maibach, H. Human skin buffering capacity: An overview. Skin Res. Technol. 2008, 14, 121–126. [Google Scholar] [CrossRef]
- Fluhr, J.W.; Behne, M.J.; Brown, B.E.; Moskowitz, D.G.; Selden, A.; Mao-Qiang, M.; Mauro, T.M.; Elias, P.M.; Feingold, K.R. Stratum Corneum Acidification in Neonatal Skin: Secretory Phospholipase A2 and the Sodium/Hydrogen Antiporter-1 Acidify Neonatal Rat Stratum Corneum. J. Investig. Dermatol. 2004, 122, 320–329. [Google Scholar] [CrossRef]
- Fluhr, J.; Darlenski, R.; Lachmann, N.; Baudouin, C.; Msika, P.; De Belilovsky, C.; Hachem, J.-P. Infant epidermal skin physiology: Adaptation after birth. Br. J. Dermatol. 2012, 166, 483–490. [Google Scholar] [CrossRef] [PubMed]
- Luebberding, S.; Krueger, N.; Kerscher, M. Age-related changes in skin barrier function—Quantitative evaluation of 150 female subjects. Int. J. Cosmet. Sci. 2013, 35, 183–190. [Google Scholar] [CrossRef] [PubMed]
- Man, M.; Xin, S.; Song, S.; Cho, S.; Zhang, X.; Tu, C.; Feingold, K.; Elias, P. Variation of Skin Surface pH, Sebum Content and Stratum Corneum Hydration with Age and Gender in a Large Chinese Population. Skin Pharmacol. Physiol. 2009, 22, 190–199. [Google Scholar] [CrossRef]
- Bailey, S.H.; Oni, G.; Brown, S.A.; Kashefi, N.; Cheriyan, S.; Maxted, M.; Stewart, C.; Jones, C.; Maluso, P.; Kenkel, A.M.; et al. The use of non-invasive instruments in characterizing human facial and abdominal skin. Lasers Surg. Med. 2012, 44, 131–142. [Google Scholar] [CrossRef] [PubMed]
- Ehlers, C.; Ivens, U.I.; Møller, M.L.; Senderovitz, T.; Serup, J. Females have lower skin surface pH than men. A study on the influence of gender, forearm site variation, right/left difference and time of the day on the skin surface pH. Skin Res. Technol. 2001, 7, 90–94. [Google Scholar] [CrossRef]
- Man, M.-Q.; Lin, T.-K.; Santiago, J.L.; Celli, A.; Zhong, L.; Huang, Z.-M.; Roelandt, T.; Hupe, M.; Sundberg, J.P.; Silva, K.A.; et al. Basis for Enhanced Barrier Function of Pigmented Skin. J. Investig. Dermatol. 2014, 134, 2399–2407. [Google Scholar] [CrossRef] [PubMed]
- Gunathilake, R.; Schurer, N.Y.; Shoo, B.A.; Celli, A.; Hachem, J.P.; Crumrine, D.; Sirimanna, G.; Feingold, K.R.; Mauro, T.M.; Elias, P.M. pH-regulated mechanisms account for pigment-type differences in epidermal barrier function. J. Investig. Dermatol. 2009, 129, 1719–1729. [Google Scholar] [CrossRef]
- Hanson, K.M.; Behne, M.J.; Barry, N.P.; Mauro, T.M.; Gratton, E.; Clegg, R.M. Two-Photon Fluorescence Lifetime Imaging of the Skin Stratum Corneum pH Gradient. Biophys. J. 2002, 83, 1682–1690. [Google Scholar] [CrossRef]
- Behne, M.J.; Meyer, J.W.; Hanson, K.M.; Barry, N.P.; Murata, S.; Crumrine, D.; Clegg, R.W.; Gratton, E.; Holleran, W.M.; Elias, P.M.; et al. NHE1 regulates the stratum corneum permeability barrier homeostasis. Microenvironment acidification assessed with fluorescence lifetime imaging. J. Biol. Chem. 2002, 277, 47399–47406. [Google Scholar] [CrossRef]
- Hachem, J.-P.; Behne, M.; Aronchik, I.; Demerjian, M.; Feingold, K.; Elias, P.; Mauro, T. Extracellular pH Controls NHE1 Expression in Epidermis and Keratinocytes: Implications for Barrier Repair. J. Investig. Dermatol. 2005, 125, 790–797. [Google Scholar] [CrossRef] [PubMed]
- Matousek, J.L.; Campbell, K.L. A comparative review of cutaneous pH. Vet. Dermatol. 2002, 13, 293–300. [Google Scholar] [CrossRef]
- Yosipovitch, G.; Maayan-Metzger, A.; Merlob, P.; Sirota, L. Skin barrier properties in different body areas in neonates. Pediatrics 2000, 106, 105–108. [Google Scholar] [CrossRef]
- Fox, C.; Nelson, D.; Wareham, J. The timing of skin acidification in very low birth weight infants. J. Perinatol. 1998, 18, 272–275. [Google Scholar] [PubMed]
- Behne, M.J.; Barry, N.P.; Hanson, K.M.; Aronchik, I.; Clegg, R.W.; Gratton, E.; Feingold, K.; Holleran, W.M.; Elias, P.M.; Mauro, T.M. Neonatal Development of the Stratum Corneum pH Gradient: Localization and Mechanisms Leading to Emergence of Optimal Barrier Function. J. Investig. Dermatol. 2003, 120, 998–1006. [Google Scholar] [CrossRef][Green Version]
- Visscher, M.O.; Adam, R.; Brink, S.; Odio, M. Newborn infant skin: Physiology, development, and care. Clin. Dermatol. 2015, 33, 271–280. [Google Scholar] [CrossRef]
- Pickens, W.L.; Warner, R.R.; Boissy, Y.L.; Boissy, R.E.; Hoath, S.B. Characterization of Vernix Caseosa: Water Content, Morphology, and Elemental Analysis. J. Investig. Dermatol. 2000, 115, 875–881. [Google Scholar] [CrossRef]
- Visscher, M.O.; Narendran, V.; Pickens, W.L.; LaRuffa, A.A.; Meinzen-Derr, J.; Allen, K.; Hoath, S.B. Vernix caseosa in neo-natal adaptation. J. Perinatol. 2005, 25, 440–446. [Google Scholar] [CrossRef]
- Fluhr, J.W.; Kao, J.; Ahn, S.K.; Feingold, K.R.; Elias, P.M.; Jain, M. Generation of Free Fatty Acids from Phospholipids Regulates Stratum Corneum Acidification and Integrity. J. Investig. Dermatol. 2001, 117, 44–51. [Google Scholar] [CrossRef]
- Jang, H.; Matsuda, A.; Jung, K.; Karasawa, K.; Matsuda, K.; Oida, K.; Ishizaka, S.; Ahn, G.; Amagai, Y.; Moon, C.; et al. Skin pH Is the Master Switch of Kallikrein 5-Mediated Skin Barrier Destruction in a Murine Atopic Dermatitis Model. J. Investig. Dermatol. 2016, 136, 127–135. [Google Scholar] [CrossRef] [PubMed]
- Vávrová, K.; Henkes, D.; Strüver, K.; Sochorová, M.; Školová, B.; Witting, M.Y.; Friess, W.; Schreml, S.; Meier, R.J.; Schäfer-Korting, M.; et al. Filaggrin Deficiency Leads to Impaired Lipid Profile and Altered Acidification Pathways in a 3D Skin Construct. J. Investig. Dermatol. 2014, 134, 746–753. [Google Scholar] [CrossRef] [PubMed]
- Hman, H.; Vahlquist, A. The pH Gradient over the Stratum Corneum Differs in X-Linked Recessive and Autosomal Dominant Ichthyosis: A Clue to the Molecular Origin of the “Acid Skin Mantle”? J. Investig. Dermatol. 1998, 111, 674–677. [Google Scholar]
- Houben, E.; Hachem, J.; De Paepe, K.; Rogiers, V. Epidermal Ceramidase Activity Regulates Epidermal Desquamation via Stratum Corneum Acidification. Skin Pharmacol. Physiol. 2008, 21, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Fluhr, J.W.; Elias, P.M. Stratum corneum pH: Formation and function of the‘Acid Mantle’. Exogen. Dermatol. 2002, 1, 163–175. [Google Scholar] [CrossRef]
- Rawlings, A.V.; Harding, C.R. Moisturization and skin barrier function. Dermatol. Ther. 2004, 17, 43–48. [Google Scholar] [CrossRef]
- Krien, P.M.; Kermici, M. Evidence for the Existence of a Self-Regulated Enzymatic Process within the Human Stratum Corneum –An Unexpected Role for Urocanic Acid. J. Investig. Dermatol. 2000, 115, 414–420. [Google Scholar] [CrossRef] [PubMed]
- Fluhr, J.W.; Elias, P.M.; Man, M.Q.; Hupe, M.; Selden, C.; Sundberg, J.P.; Tschachler, E.; Eckhart, L.; Mauro, T.M.; Feingold, T.R. Is the Filaggrin-Histidine-Urocanic Acid Pathway Essential for Stratum Corneum Acidification? J. Investig. Dermatol. 2010, 130, 2141–2144. [Google Scholar] [CrossRef]
- Thyssen, J.P.; Kezic, S. Causes of epidermal filaggrin reduction and their role in the pathogenesis of atopic dermatitis. J. Allergy Clin. Immunol. 2014, 134, 792–799. [Google Scholar] [CrossRef] [PubMed]
- Rawlings, A.V.; Matts, P.J. Stratum Corneum Moisturization at the Molecular Level: An Update in Relation to the Dry Skin Cycle. J. Investig. Dermatol. 2005, 124, 1099–1110. [Google Scholar] [CrossRef] [PubMed]
- Elias, P.M. The how, why and clinical importance of stratum corneum acidification. Exp. Dermatol. 2017, 26, 999–1003. [Google Scholar] [CrossRef] [PubMed]
- Biro, T.; Olah, A.; Toth, B.I.; Szollosi, A.G. Endogenous Factors That Can Influence Skin pH. In pH of the Skin: Issues and Challenges; Surber, C., Abels, C., Maibach, H., Eds.; Karger: Basel, Switzerland, 2018; Volume 54, pp. 54–63. [Google Scholar]
- Eberting, C.L.; Blickenstaff, N.; Goldenberg, A. Pathophysiologic Treatment Approach to Irritant Contact Dermatitis. Curr. Treat. Options Allergy 2014, 1, 317–328. [Google Scholar] [CrossRef][Green Version]
- Jia, Y.; Gan, Y.; He, C.; Chen, Z.; Zhou, C. The mechanism of skin lipids influencing skin status. J. Dermatol. Sci. 2018, 89, 112–119. [Google Scholar] [CrossRef]
- Danso, M.; Boiten, W.; van Drongelen, V.; Meijling, K.G.; Gooris, G.; El Ghalbzouri, A.; Absalah, S.; Vreeken, R.; Kezic, S.; van Smeden, J.; et al. Altered expression of epidermal lipid bio-synthesis enzymes in atopic dermatitis skin is accompanied by changes in stratum corneum lipid composition. J. Dermatol. Sci. 2017, 88, 57–66. [Google Scholar] [CrossRef]
- Fluhr, J.W.; Mao-Qiang, M.; Brown, B.E.; Hachem, J.-P.; Moskowitz, D.G.; Demerjian, M.; Haftek, M.; Serre, G.; Crumrine, D.; Mauro, T.M.; et al. Functional Consequences of a Neutral pH in Neonatal Rat Stratum Corneum. J. Investig. Dermatol. 2004, 123, 140–151. [Google Scholar] [CrossRef]
- Goñi, F.M.; Alonso, A. Sphingomyelinases: Enzymology and membrane activity. FEBS Lett. 2002, 531, 38–46. [Google Scholar] [CrossRef]
- Lieckfeldt, R.; Villalaín, J.; Gómez-Fernández, J.C.; Lee, G. Apparent pK a of the fatty acids within ordered mixtures of model human stratum corneum lipids. Pharm. Res. 1995, 12, 1614–1617. [Google Scholar] [CrossRef] [PubMed]
- Plasencia, I.; Norlén, L.; Bagatolli, L.A. Direct Visualization of Lipid Domains in Human Skin Stratum Corneum’s Lipid Membranes: Effect of pH and Temperature. Biophys. J. 2007, 93, 3142–3155. [Google Scholar] [CrossRef] [PubMed]
- Haftek, M.; Simon, M.; Kanitakis, J.; Maréchal, S.; Claudy, A.; Serre, G.; Schmitt, D. Expression of corneodesmosin in the granular layer and stratum corneum of normal and diseased epidermis. Br. J. Dermatol. 1997, 137, 864–873. [Google Scholar] [CrossRef] [PubMed]
- Kitajima, Y. Implications of normal and disordered remodeling dynamics of corneodesmosomes in stratum corneum. Dermatol. Sin. 2015, 33, 58–63. [Google Scholar] [CrossRef]
- Hachem, J.-P.; Roelandt, T.; Schürer, N.; Pu, X.; Fluhr, J.; Giddelo, C.; Man, M.-Q.; Crumrine, D.; Roseeuw, D.; Feingold, K.R.; et al. Acute Acidification of Stratum Corneum Membrane Domains Using Polyhydroxyl Acids Improves Lipid Processing and Inhibits Degradation of Corneodesmosomes. J. Investig. Dermatol. 2010, 130, 500–510. [Google Scholar] [CrossRef]
- Caubet, C.; Jonca, N.; Brattsand, M.; Guerrin, M.; Bernard, D.; Schmidt, R.; Egelrud, T.; Simon, M.; Serre, G. Degradation of Corneodesmosome Proteins by Two Serine Proteases of the Kallikrein Family, SCTE/KLK5/hK5 and SCCE/KLK7/hK7. J. Investig. Dermatol. 2004, 122, 1235–1244. [Google Scholar] [CrossRef]
- Blum, H.E. The human microbioma. Adv. Med. Sci. 2017, 62, 414–420. [Google Scholar] [CrossRef]
- Nakatsuji, T.; Chen, T.H.; Narala, S.; Chun, K.A.; Two, A.M.; Yun, T.; Shafiq, F.; Kotol, P.F.; Bouslimani, A.; Melnik, A.V.; et al. Antimicrobials from human skin commensal bacteria protect against Staphylococcus aureus and are deficient in atopic dermatitis. Sci. Transl. Med. 2017, 9, 1–12. [Google Scholar] [CrossRef]
- Gallo, R.L.; Nakatsuji, T. Microbial Symbiosis with the Innate Immune Defense System of the Skin. J. Investig. Dermatol. 2011, 131, 1974–1980. [Google Scholar] [CrossRef]
- Sugimoto, S.; Iwamoto, T.; Takada, K.; Okuda, K.-I.; Tajima, A.; Iwase, T.; Mizunoe, Y. Staphylococcus epidermidis Esp Degrades Specific Proteins Associated with Staphylococcus aureus Biofilm Formation and Host-Pathogen Interaction. J. Bacteriol. 2013, 195, 1645–1655. [Google Scholar] [CrossRef]
- Yuki, T.; Yoshida, H.; Akazawa, Y.; Komiya, A.; Sugiyama, Y.; Inoue, S.; Mesin, L.; Di Niro, R.; Thompson, K.M.; Lundin, K.E.A.; et al. Activation of TLR2 Enhances Tight Junction Barrier in Epidermal Keratinocytes. J. Immunol. 2011, 187, 3230–3237. [Google Scholar] [CrossRef] [PubMed]
- Naik, S.; Bouladoux, N.; Wilhelm, C.; Molloy, M.J.; Salcedo, R.; Kastenmuller, W.; Deming, C.; Quinones, M.; Koo, L.; Conlan, S.; et al. Compartmentalized Control of Skin Immunity by Resident Commensals. Science 2012, 337, 1115–1119. [Google Scholar] [CrossRef] [PubMed]
- Sanford, J.; Gallo, R.L. Functions of the skin microbiota in health and disease. Semin. Immunol. 2013, 25, 370–377. [Google Scholar] [CrossRef] [PubMed]
- Seidenari, S.; Giusti, G. Objective assessment of the skin of children affected by atopic dermatitis: A study of pH, capacitance and TEWL in eczematous and clinically uninvolved skin. Acta Derm. Venereol. 1995, 75, 429–433. [Google Scholar] [CrossRef] [PubMed]
- Bonifaz, A.; Rojas, R.; Tirado-Sánchez, A.; Chávez-López, D.; Mena, C.; Calderón, L.; María, P.O. Superficial Mycoses Asso-ciated with Diaper Dermatitis. Mycopathologia 2016, 181, 671–679. [Google Scholar] [CrossRef]
- Farage, M.A.; Miller, K.W.; Berardesca, E.; Maibach, H.I. Incontinence in the aged: Contact dermatitis and other cutaneous consequences. Contact Dermat. 2007, 57, 211–217. [Google Scholar] [CrossRef]
- Danby, S.G.; Cork, M.J. pH in Atopic Dermatitis. In pH of the Skin: Issues and Challenges; Surber, C., Abels, C., Maibach, H., Eds.; Karger: Basel, Switzerland, 2018; Volume 54, pp. 95–107. [Google Scholar]
- Kong, H.H. Skin microbiome: Genomics-based insights into the diversity and role of skin microbes. Trends Mol. Med. 2011, 17, 320–328. [Google Scholar] [CrossRef]
- Oh, J.; Freeman, A.F.; Park, M.; Sokolic, R.; Candotti, F.; Holland, S.M.; Segre, J.A.; Kong, H.; Program, N.C.S. The altered landscape of the human skin microbiome in patients with primary immunodeficiencies. Genome Res. 2013, 23, 2103–2114. [Google Scholar] [CrossRef]
- Percival, S.L.; Mccarty, S.; Hunt, J.; Woods, E.J. The effects of pH on wound healing, biofilms, and antimicrobial efficacy. Wound Repair Regen. 2014, 22, 174–186. [Google Scholar] [CrossRef]
- Dissemond, J.; Witthoff, M.; Brauns, T.C.; Haberer, D.; Goos, M. pH values in chronic wounds. Evaluation during modern wound therapy. Hautarzt 2003, 54, 959–965. [Google Scholar] [CrossRef] [PubMed]
- Scheuplein, R.J.; Ross, L. Effects of surfactants and solvents on the permeability of the epidermis. J. Soc. Cosmet. Chem. 1970, 21, 853–873. [Google Scholar]
- Madison, K.C. Barrier function of the skin: “la raison d’etre” of the epidermis. J. Investig. Dermatol. 2003, 121, 231–241. [Google Scholar] [CrossRef] [PubMed]
- Rawlings, A.V.; Watkinson, A.; Rogers, J.; Mayo, A.; Hope, J.; Scott, I.A. Abnormalities in stratum corneum structure, lipid composition, and desmosome degradation in soap-induced winter xerosis. J. Soc. Cosmet. Chem. 1994, 45, 203–220. [Google Scholar]
- Lukic, M.; Pantelic, I.; Savic, S. An Overview of Novel Surfactants for Formulation of Cosmetics with Certain Emphasis on Acidic Active Substances. Tenside Surfactants Deterg. 2016, 53, 7–19. [Google Scholar] [CrossRef]
- Ananthapadmanabhan, K.P.; Moore, D.J.; Subramanyan, K.; Misra, M.; Meyer, F. Cleansing without compromise: The impact of cleansers on the skin barrierand the technology of mild cleansing. Dermatol. Ther. 2004, 7, 16–25. [Google Scholar] [CrossRef] [PubMed]
- Rhein, L.D. Review of properties of surfactants that determine their interactions with stratum corneum. J. Soc. Cosmet. Chem. 1997, 48, 253–274. [Google Scholar]
- Corazza, M.; Lauriola, M.M.; Zappaterra, M.; Bianchi, A.; Virgili, A. Surfactants, skin cleansing protagonists. J. Eur. Acad. Dermatol. Venereol. 2010, 24, 1–6. [Google Scholar] [CrossRef]
- Seweryn, A. Interactions between surfactants and the skin–Theory and practice. Adv. Colloid Interface Sci. 2018, 256, 242–255. [Google Scholar] [CrossRef]
- Jackson, C.T.; Paye, M.; Maibach, H.I. Mechanism of skin irritation by surfactants and anti-irritants for surfactant-based products. In Handbook of Cosmetic Science and Technology, 4th ed.; Barel, A.O., Paye, M., Maibach, H.I., Eds.; CRC Press: Boca Raton, FL, USA, 2014; pp. 353–365. [Google Scholar]
- Draelos, Z.; Hornby, S.; Walters, R.; Appa, Y. Hydrophobically modified polymers can minimize skin irritation potential caused by surfactant-based cleansers. J. Cosmet. Dermatol. 2013, 12, 314–321. [Google Scholar] [CrossRef]
- Goddard, E.D.; Ananthapadmanabhan, K.P. Interactions of Surfactants with Polymers and Proteins; CRC Press: Boca Raton, FL, USA, 1993. [Google Scholar]
- Abbas, S.; Goldberg, J.W.; Massaro, M. Personal cleanser technology and clinical performance. Dermatol. Ther. 2004, 17, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Mücke, H.; Mohr, K.T.; Rümmler, A.; Wutzler, T. Untersuchungen über den Haut-pH-Wert der Hand nach Anwendung von Seife, Reinigungs- und Händedesinfektionsmitteln. Pharmazie 1993, 48, 468–469. [Google Scholar]
- Trobaugh, C.M.; Wickett, R.R. Personal care products: Effects on skin surface pH. Cosm. Toil. 1990, 105, 41–46. [Google Scholar]
- Firooz, A.; Aghazadeh, N.; Estarabadi, A.R.; Hejazi, P. The effects of water exposure on biophysical properties of normal skin. Skin Res. Technol. 2015, 21, 131–136. [Google Scholar] [CrossRef]
- Voegeli, D. The Effect of Washing and Drying Practices on Skin Barrier Function. J. Wound Ostomy Cont. Nurs. 2008, 35, 84–90. [Google Scholar] [CrossRef] [PubMed]
- Gfatter, R.; Hackl, P.; Braun, F. Effects of Soap and Detergents on Skin Surface pH, Stratum corneum Hydration and Fat Content in Infants. Dermatology 1997, 195, 258–262. [Google Scholar] [CrossRef] [PubMed]
- Korting, H.; Megele, M.; Mehringer, L.; Vieluf, D.; Zienicke, H.; Hamm, G.; Braun-Falco, O. Influence of skin cleansing preparation acidity on skin surface properties. Int. J. Cosmet. Sci. 1991, 13, 91–102. [Google Scholar] [CrossRef]
- Duncan, C.N.; Riley, T.V.; Carson, K.C.; Budgeon, C.A.; Siffleet, J. The effect of an acidic cleanser versus soap on the skin pH and micro-flora of adult patients: A non-randomized two group crossover study in an intensive care unit. Intensive Crit. Care Nurs. 2013, 29, 291–296. [Google Scholar] [CrossRef] [PubMed]
- Baranda, L.; González-Amaro, R.; Torres-Alvarez, B.; Alvarez, C.; Ramírez, V. Correlation between pH and irritant effect of cleansers marketed for dry skin. Int. J. Dermatol. 2002, 41, 494–499. [Google Scholar] [CrossRef]
- Lu, G.; Moore, D.J. Study of surfactant-skin interactions by skin impedance measurements. Int. J. Cosmet. Sci. 2012, 34, 74–80. [Google Scholar] [CrossRef]
- Korting, H.C.; Kober, M.; Mueller, M.; Braun-Falco, O. Influence of repeated washings with soap and synthetic detergents on pH and resident flora of the skin of forehead and forearm. Results of a cross-over trial in health probationers. Acta Derm. Venereol. 1987, 67, 41–47. [Google Scholar]
- Korting, H.C.; Braun-Falco, O. The effect of detergents on skin pH and its consequences. Clin. Dermatol. 1996, 14, 23–27. [Google Scholar] [CrossRef]
- Barel, A.O.; Lambrecht, R.; Clarys, P.; Morrison, B.M., Jr.; Paye, M. A comparative study of the effects on the skin of a classical bar soap and a syndet cleansing bar in normal use conditions and in the soap chamber test. Skin Res. Technol. 2001, 7, 98–104. [Google Scholar] [CrossRef] [PubMed]
- Takagi, Y.; Kaneda, K.; Miyaki, M.; Matsuo, K.; Kawada, H.; Hosokawa, H. The long-term use of soap does not affect the pH-maintenance mechanism of human skin. Skin Res. Technol. 2015, 21, 144–148. [Google Scholar] [CrossRef] [PubMed]
- Bornkessel, A.; Flach, M.; Elsner, P.; Fluhr, J.W.; Arens-Corell, M. Functional assessment of a washing emulsion for sensitive skin: Mild impairment of stratum corneum hydration, pH, barrier function, lipid content, integrity and cohesion in a controlled washing test. Skin Res. Technol. 2005, 11, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Mendes, B.R.; Shimabukuro, D.M.; Uber, M.; Abagge, K.T. Critical assessment of the pH of children’s soap. J. Pediatr. 2016, 92, 290–295. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tarun, J.; Susan, V.J.; Susan, J.; Suria, J.; Criton, S. Evaluation of pH of bathing soaps and shampoos for skin and hair care. Indian J. Dermatol. 2014, 59, 442–444. [Google Scholar] [CrossRef] [PubMed]
- Mauro, T.; Grayson, S.; Gao, W.N.; Man, M.-Q.; Kriehuber, E.; Behne, M.; Feingold, K.R.; Elias, P.M. Barrier recovery is impeded at neutral pH, independent of ionic effects: Implications for extracellular lipid processing. Arch. Dermatol. Res. 1998, 290, 215–222. [Google Scholar] [CrossRef]
- Hachem, J.-P.; Crumrine, D.; Fluhr, J.; Brown, B.E.; Feingold, K.R.; Elias, P.M. pH Directly Regulates Epidermal Permeability Barrier Homeostasis, and Stratum Corneum Integrity/Cohesion. J. Investig. Dermatol. 2003, 121, 345–353. [Google Scholar] [CrossRef]
- Man, M.Q.; Feingold, K.R.; Elias, P.M. Exogenous lipids influence permeability barrier recovery in acetone-treated murine skin. Arch. Dermatol. 1993, 129, 728–738. [Google Scholar] [CrossRef]
- Mao-Qiang, M.; Feingold, K.R.; Thornfeldt, C.R.; Elias, P.M. Optimization of Physiological Lipid Mixtures for Barrier Repair. J. Investig. Dermatol. 1996, 106, 1096–1101. [Google Scholar] [CrossRef]
- Zhang, Z.; Lukic, M.; Savic, S.; Lunter, D.J. Reinforcement of barrier function—Skin repair formulations to deliver physiological lipids into skin. Int. J. Cosmet. Sci. 2018, 40, 494–501. [Google Scholar] [CrossRef] [PubMed]
- Vávrová, K.; Hrabalek, A.; Mac-Mary, S.; Humbert, P.; Muret, P. Ceramide analogue 14S24 selectively recovers perturbed human skin barrier. Br. J. Dermatol. 2007, 157, 704–712. [Google Scholar] [CrossRef] [PubMed]
- Takagi, Y.; Nakagawa, H.; Higuchi, K.; Imokawa, G. Characterization of Surfactant-Induced Skin Damage through Barrier Recovery Induced by Pseudoacylceramides. Dermatology 2005, 211, 128–134. [Google Scholar] [CrossRef]
- Fukunaga, K.; Yoshida, M.; Nakajima, F.; Uematsu, R.; Hara, M.; Inoue, S.; Kondo, H.; Nishimura, S. Design, synthesis, and evaluation of beta-galactosylceramide mimics promoting beta-glucocerebrosidase activity in keratinocytes. Bioorg. Med. Chem. Lett. 2003, 13, 813–885. [Google Scholar] [CrossRef]
- Darmstadt, G.L.; Man, M.Q.; Chi, E.; Saha, S.K.; Ziboh, V.A.; Black, R.E.; Santosham, M.; Elias, P.M. Impact of topical oils on the skin barrier: Possible implications for neonatal health in developing countries. Acta Paediatr. 2002, 91, 546–554. [Google Scholar] [CrossRef]
- Buraczewska, I.; Lodén, M. Treatment of Surfactant-Damaged Skin in Humans with Creams of Different pH Values. Pharmacology 2005, 73, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Cork, M.; Danby, S. Aqueous cream damages the skin barrier. Br. J. Dermatol. 2011, 164, 1179–1180. [Google Scholar] [CrossRef]
- Zhai, H.; Maibach, H.I. Barrier creams—Skin protectants: Can you protect skin? J. Cosmet. Dermatol. 2002, 1, 20–23. [Google Scholar] [CrossRef]
- Pavlačková, J.; Egner, P.; Sedláček, T.; Mokrejš, P.; Sedlaříková, J.; Polášková, J. In vivo efficacy and properties of semisolid formulations containing panthenol. J. Cosmet. Dermatol. 2019, 18, 346–354. [Google Scholar] [CrossRef]
- Glatz, M.; Jo, J.-H.; Kennedy, E.A.; Polley, E.C.; Segre, J.A.; Simpson, E.L.; Kong, H.H. Emollient use alters skin barrier and microbes in infants at risk for developing atopic dermatitis. PLoS ONE 2018, 13, e0192443. [Google Scholar] [CrossRef] [PubMed]
- Luebberding, S.; Krueger, N.; Kerscher, M. Age-Related Changes in Male Skin: Quantitative Evaluation of One Hundred and Fifty Male Subjects. Skin Pharmacol. Physiol. 2014, 27, 9–17. [Google Scholar] [CrossRef]
- Kilic, A.; Masur, C.; Reich, H.; Knie, U.; Dähnhardt, D.; Dähnhardt-Pfeiffer, S.; Abels, C. Skin acidification with a water-in-oil emulsion (pH 4) restores disrupted epidermal barrier and improves structure of lipid lamellae in the elderly. J. Dermatol. 2019, 46, 457–465. [Google Scholar] [CrossRef] [PubMed]
- Blaak, J.; Dähnhardt, D.; Dähnhardt-Pfeiffer, S.; Bielfeldt, S.; Wilhelm, K.P.; Wohlfart, R.; Staib, P. A plant oil-containing pH 4 emulsion improves epidermal barrierstructure and enhances ceramide levels in aged skin. Int. J. Cosmet. Sci. 2017, 39, 284–291. [Google Scholar] [CrossRef]
- Angelova-Fischer, I.; Fischer, T.W.; Abels, C.; Zillikens, D. Accelerated barrier recovery and enhancement of the barrier in-tegrity and properties by topical application of a pH 4 vs. a pH 5.8 water-in-oil emulsion in aged skin. Br. J. Dermatol. 2018, 179, 471–477. [Google Scholar]
- Tasic-Kostov, M.; Savic, S.; Lukic, M.; Tamburic, S.; Pavlovic, M.; Vuleta, G. Lactobionic acid in a natural alkylpolygluco-side-based vehicle: Assessing safety and efficacy aspects in comparison to glycolic acid. J. Cosmet. Dermatol. 2010, 9, 3–10. [Google Scholar] [CrossRef]
- Yu, R.J.; Van Scott, E.J. Alpha-hydroxyacids and carboxylic acids. J. Cosmet. Dermatol. 2004, 3, 76–87. [Google Scholar] [CrossRef]
- Sahlin, A.; Edlund, F.; Lodén, M. A double-blind and controlled study on the influence of the vehicle on the skin susceptibility to stinging from lactic acid. Int. J. Cosmet. Sci. 2007, 29, 385–390. [Google Scholar] [CrossRef] [PubMed]
- Buraczewska, I.; Berne, B.; Lindberg, M.; Törmä, H.; Lodén, M. Changes in skin barrier function following long-termtreatment with moisturizers, a randomized controlled trial. Br. J. Dermatol. 2007, 156, 492–498. [Google Scholar] [CrossRef]
- Bashir, S.; Dreher, F.; Chew, A.; Zhai, H.; Levin, C.; Stern, R.; Maibach, H. Cutaneous bioassay of salicylic acid as a keratolytic. Int. J. Pharm. 2005, 292, 187–194. [Google Scholar] [CrossRef]
- Farage, M.A.; Hood, W.; Berardesca, E.; Maibach, H. Intrinsic and Extrinsic Factors Affecting Skin Surface pH. In pH of the Skin: Issues and Challenges; Surber, C., Abels, C., Maibach, H., Eds.; Karger: Basel, Switzerland, 2018; Volume 54, pp. 33–47. [Google Scholar]
- . Krutmann, J.; Bouloc, A.; Sore, G.; Bernard, B.A.; Passeron, T. The skin aging exposome. J. Dermatol. Sci. 2017, 85, 152–161. [Google Scholar] [CrossRef]
- Nash, J.F.; Matts, P.J.; Ertel, K.D. Maintenance of healthy skin: Cleansing, moisturization, and ultraviolet protection. J. Cosmet. Dermatol. 2007, 6, 7–11. [Google Scholar] [CrossRef]
- Jiang, M.; Qureshi, S. Assessment of in vitro percutaneous absorption of glycolic acid through human skin sections using a flow-through diffusion cell system. J. Dermatol. Sci. 1998, 18, 181–188. [Google Scholar] [CrossRef]
- Draelos, Z.D. α-Hydroxy acids, β-hydroxy acid, and other topical agents. Dermatol. Ther. 2000, 13, 154–158. [Google Scholar] [CrossRef]
- Lukic, M.; Filipovic, M.; Nevena, P.; Lunter, D.; Bozic, D.; Savic, S. Formulation of topical acidic products and acidification of the skin—Contribution of glycolic acid. Int. J. Cosmet. Sci. 2021. [Google Scholar] [CrossRef] [PubMed]
- Tasić-Kostov, M.; Lukić, M.; Savić, S. A 10% Lactobionic acid-containing moisturizer reduces skinsurface pH without irrita-tion—An in vivo/in vitro. J. Cosmet. Dermatol. 2019, 18, 1705–1710. [Google Scholar] [CrossRef]

| Source * | Claims on Product | pH-Related Claims on Website |
|---|---|---|
| https://www.aveneusa.com/skin-care/cleansers/oil-free-gel-cleanser | / | Physiological pH will not over-dry skin |
| https://misshaus.com/collections/cleansers2/products/cicadin-ph-blemish-cleansing-water | Cicadin pH Blemish Cleansing Water, pH balancing | A pH balancing cleansing water with Centella Asiatica extract to soothe irritated skin and reduce redness and inflammation. |
| https://www.drunkelephant.com/collections/cleansers/products/beste-no-9-jelly-cleanser | / | (Product) is formulated at an ideal, non-stripping pH level of 5.5. |
| https://sokoglam.com/products/acwell-licorice-ph-balancing-cleansing-toner | 5.5 | This toner has a pH level of 5.5 to effectively balance your skin. |
| https://www.laroche-posay.sg/en/physiological/lotion-apaisante | Physiological pH | SOOTHING LOTION soothes, tones and purifies the skin while respecting its physiological pH balance. |
| www.sebamed.com/products/product-page/item/269 | pH 5.5 | The pH 5.5 helps to protect against dryness as well as external irritants, allergens, and harmful micro-organisms. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lukić, M.; Pantelić, I.; Savić, S.D. Towards Optimal pH of the Skin and Topical Formulations: From the Current State of the Art to Tailored Products. Cosmetics 2021, 8, 69. https://doi.org/10.3390/cosmetics8030069
Lukić M, Pantelić I, Savić SD. Towards Optimal pH of the Skin and Topical Formulations: From the Current State of the Art to Tailored Products. Cosmetics. 2021; 8(3):69. https://doi.org/10.3390/cosmetics8030069
Chicago/Turabian StyleLukić, Milica, Ivana Pantelić, and Snežana D. Savić. 2021. "Towards Optimal pH of the Skin and Topical Formulations: From the Current State of the Art to Tailored Products" Cosmetics 8, no. 3: 69. https://doi.org/10.3390/cosmetics8030069
APA StyleLukić, M., Pantelić, I., & Savić, S. D. (2021). Towards Optimal pH of the Skin and Topical Formulations: From the Current State of the Art to Tailored Products. Cosmetics, 8(3), 69. https://doi.org/10.3390/cosmetics8030069








