Managing SARS-CoV-2 Testing in Schools with an Artificial Intelligence Model and Application Developed by Simulation Data
Abstract
:1. Introduction
2. Background
2.1. School Testing and Its Challenges
2.2. Simulation Modeling Option and Artificial Intelligence
2.3. AI in Simulation Modeling for School Testing Scenarios
3. Materials and Methods
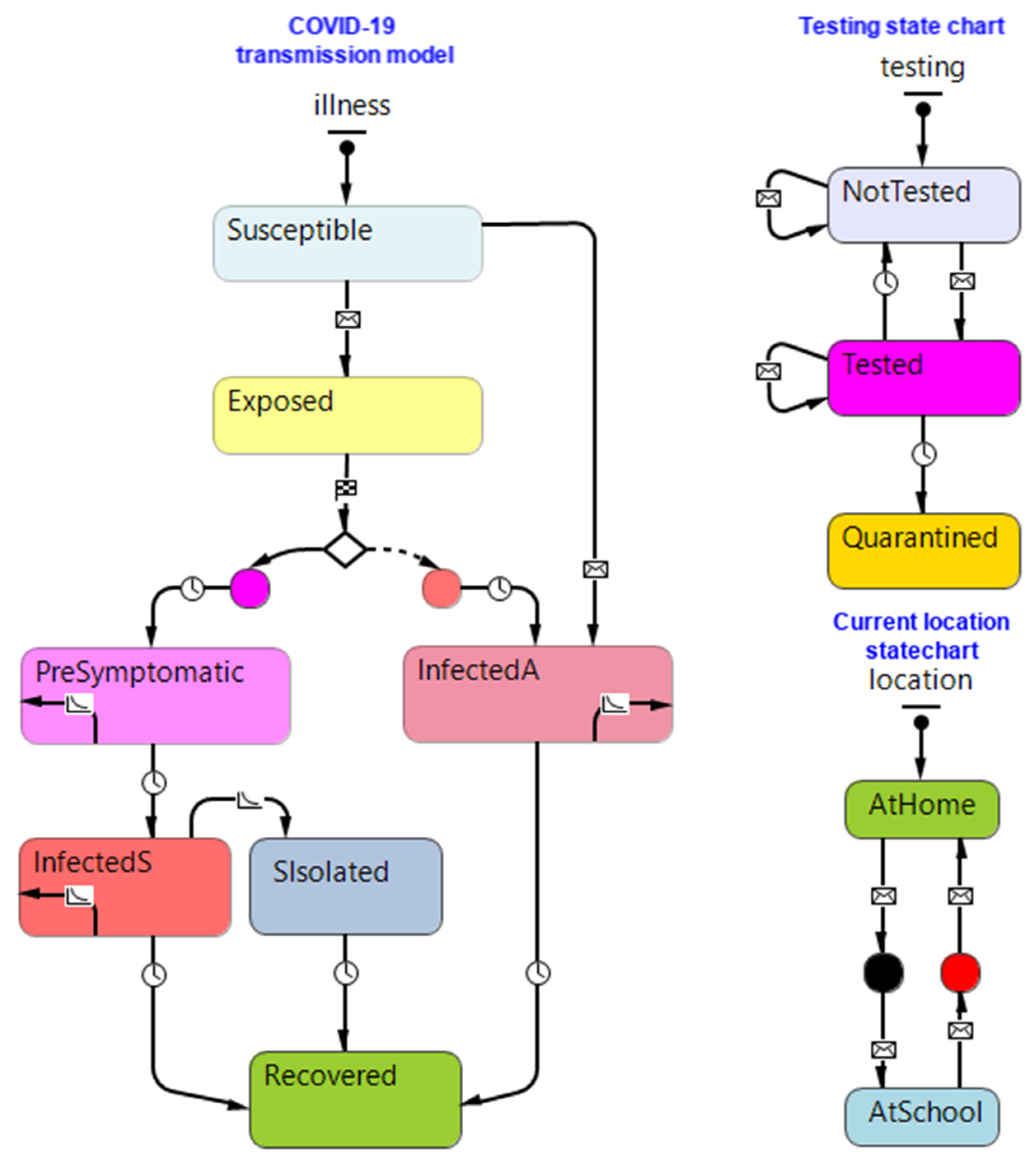
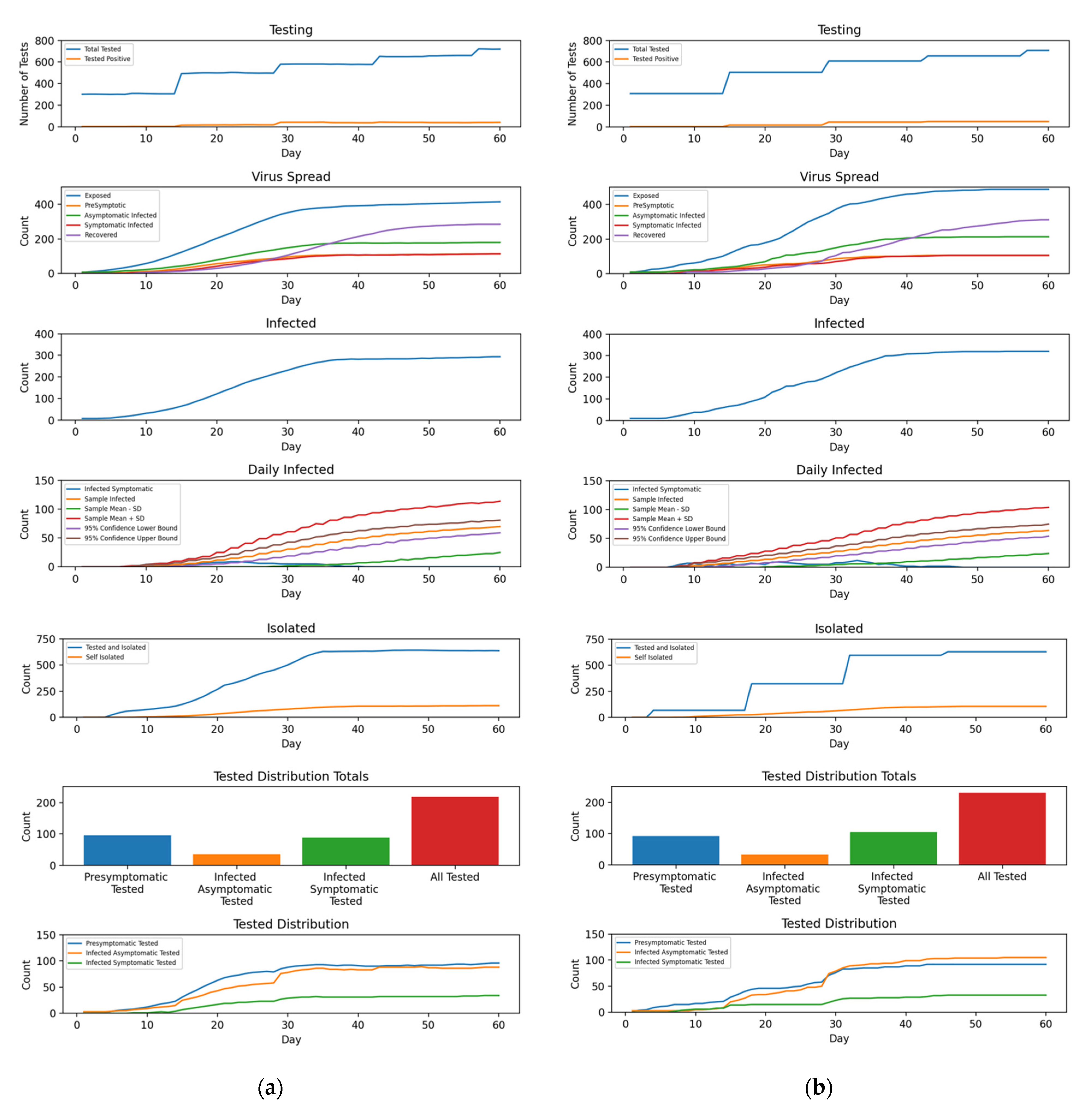
3.1. School Testing Simulation
3.2. Data Preparation for the AI Network Model
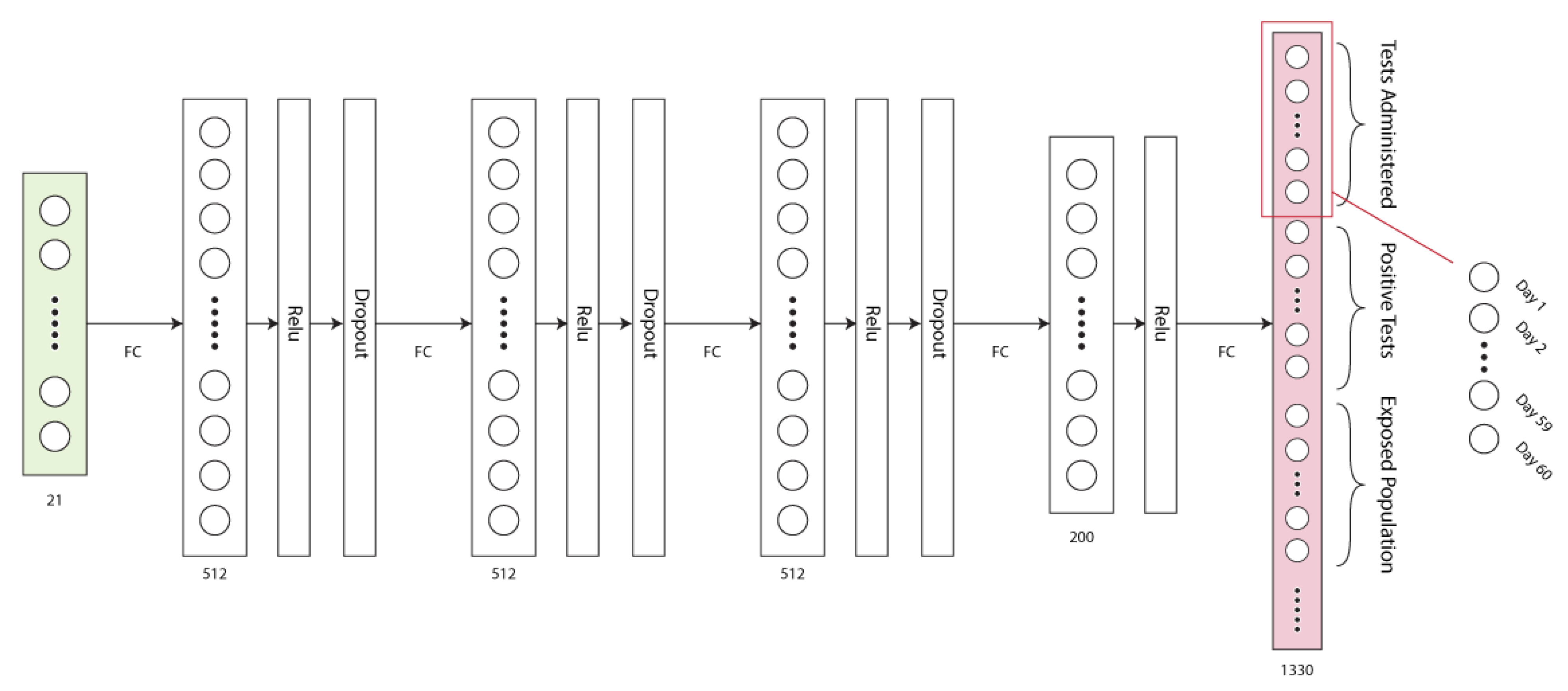
3.3. Network Design
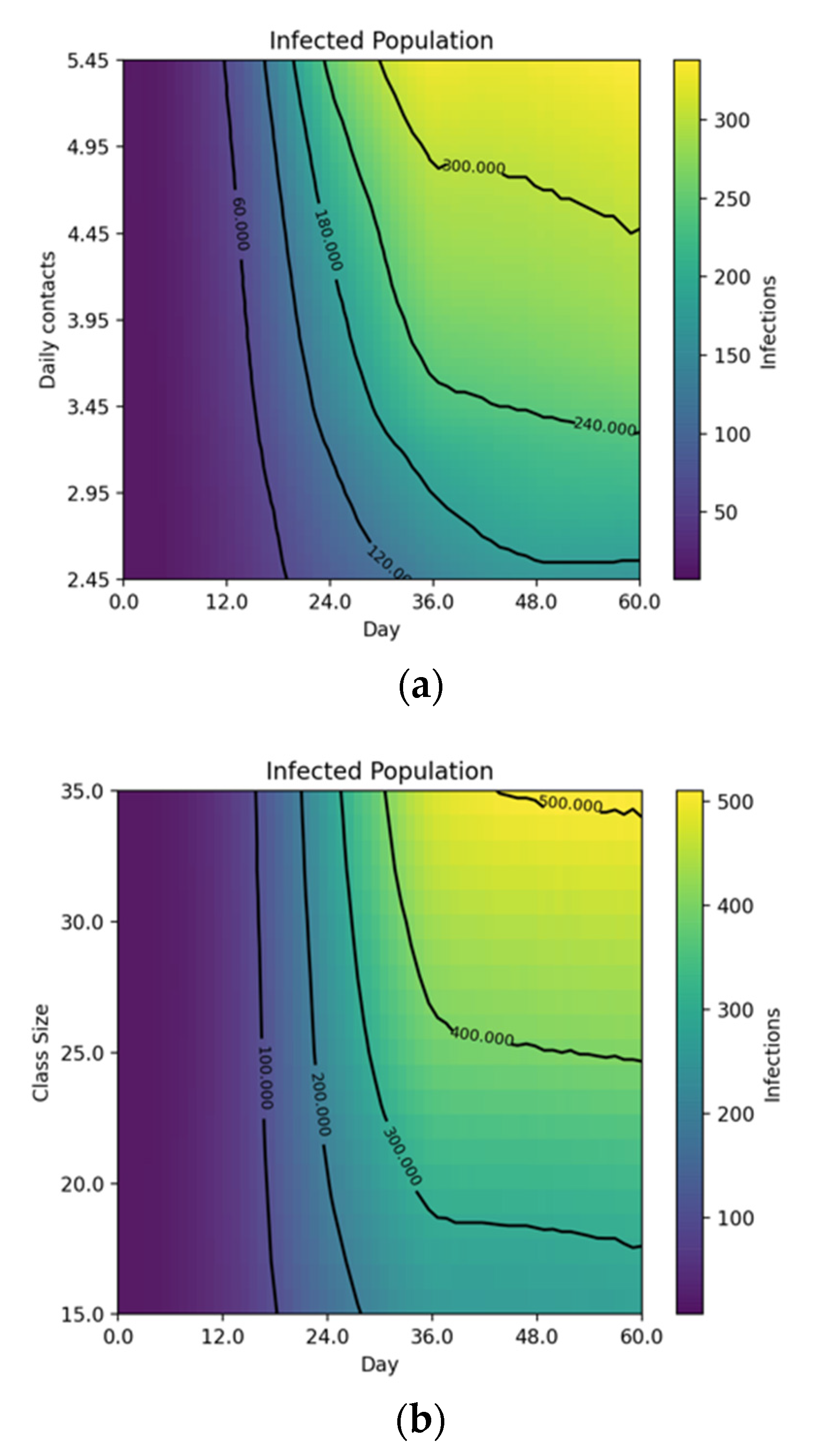
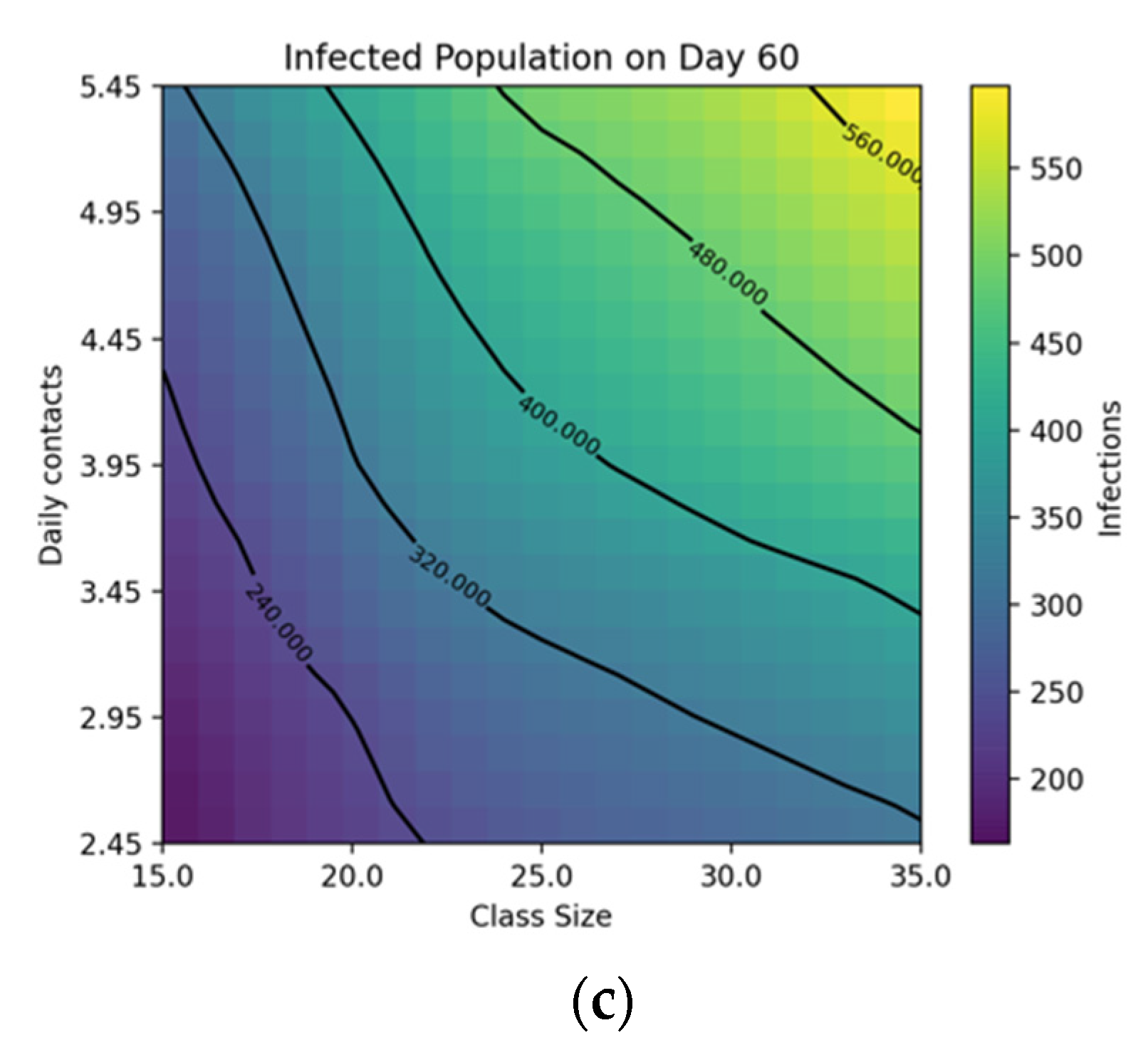
4. Results
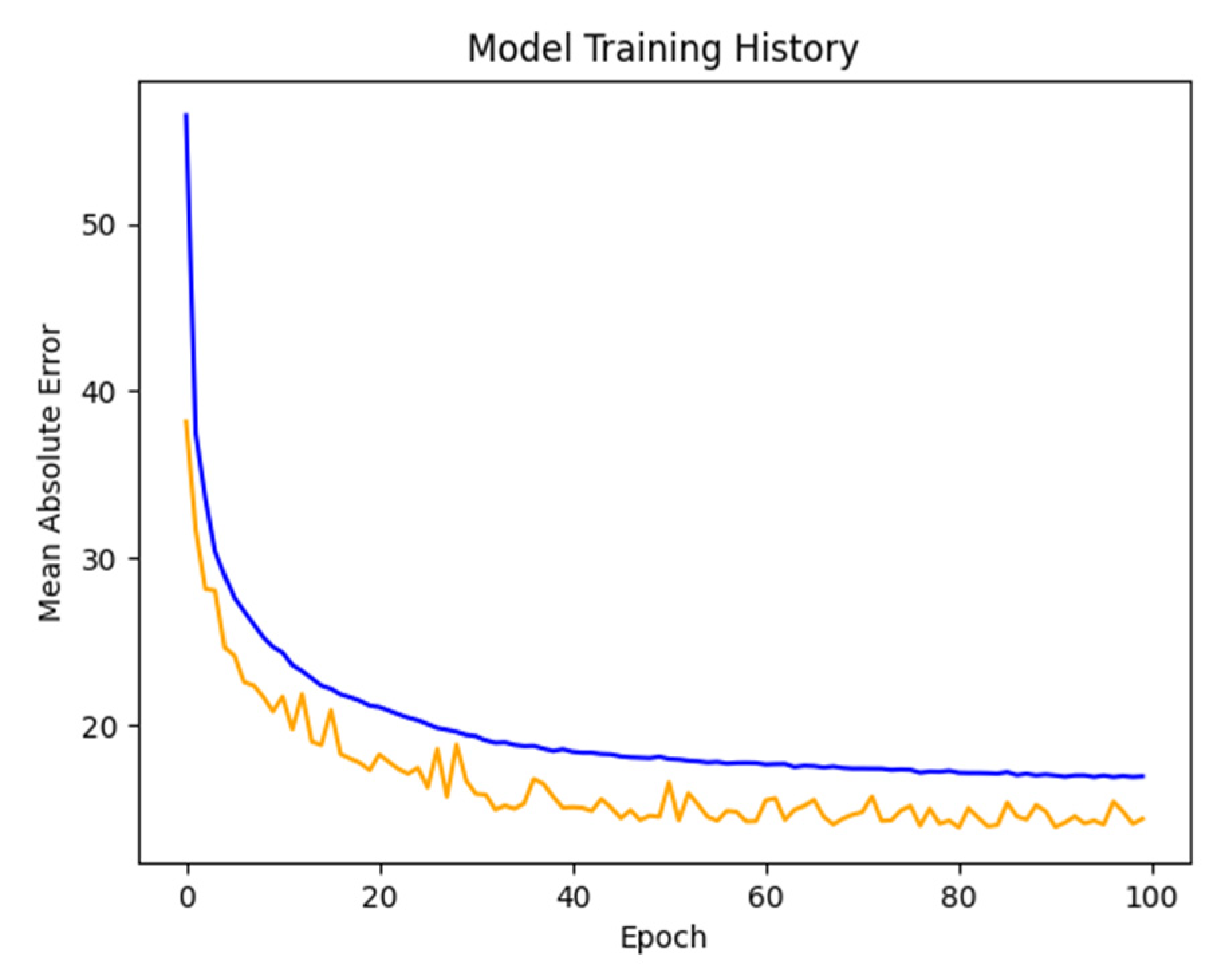
4.1. Network Training
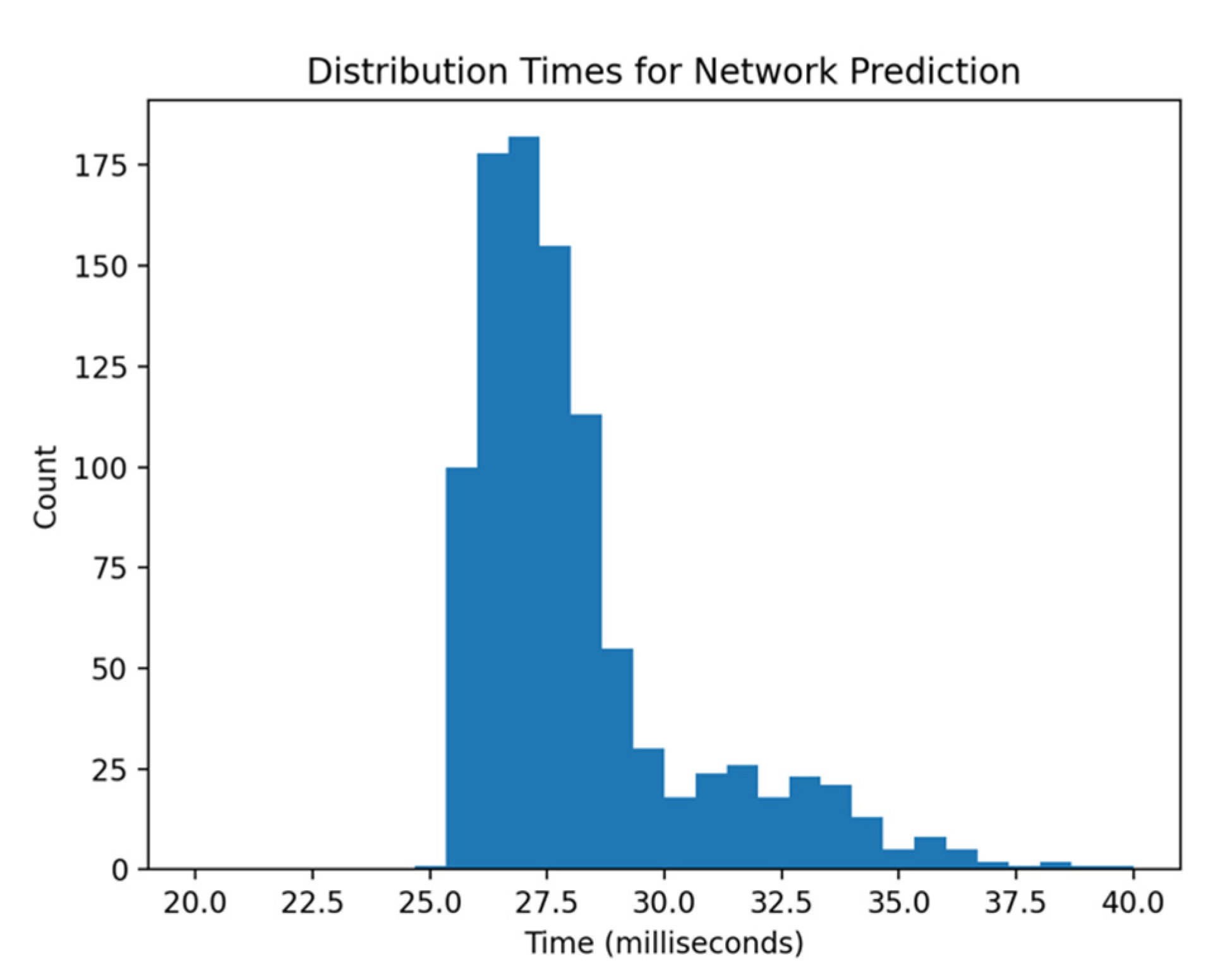
4.2. Network Prediction
4.3. Analysis
5. Discussion
6. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AI | Artificial Intelligence |
| ECDC | European Centre for Disease Control |
| KPI | Key Performance Indicator |
| IOT | Internet of Things |
| WHO | World Health Organization |
| MAE | Mean Absolute Error |
References
- Panovska-Griffiths, J.; Kerr, C.C.; Stuart, R.M.; Mistry, D.; Klein, D.J.; Viner, R.M.; Bonell, C. Determining the optimal strategy for reopening schools, the impact of test and trace interventions, and the risk of occurrence of a second COVID-19 epidemic wave in the UK: A modelling study. Lancet Child Adolesc. Health 2020, 4, 817–827. [Google Scholar] [CrossRef]
- Ziauddeen, N.; Woods-Townsend, K.; Saxena, S.; Gilbert, R.; Alwan, N.A. Schools and COVID-19: Reopening Pandora’s box? Public Health Pr. 2020, 1, 100039. [Google Scholar] [CrossRef] [PubMed]
- Asgary, A.; Valtchev, S.Z.; Chen, M.; Najafabadi, M.M.; Wu, J. Artificial intelligence model of drive-through vaccination simulation. Int. J. Environ. Res. Public Health 2020, 18, 268. [Google Scholar] [CrossRef] [PubMed]
- Asgary, A.; Cojocaru, M.G.; Najafabadi, M.M.; Wu, J. Simulating preventative testing of SARS-CoV-2 in schools: Policy implications. BMC Public Health 2021, 21, 125. [Google Scholar] [CrossRef]
- Asgary, A.; Najafabadi, M.; Karsseboom, R.; Wu, J. A Drive-through simulation tool for mass vaccination during COVID-19 Pandemic. Healthcare 2020, 8, 469. [Google Scholar] [CrossRef]
- Latif, S.; Usman, M.; Manzoor, S.; Iqbal, W.; Qadir, J.; Tyson, G.; Crowcroft, J. Leveraging data science to combat COVID-19: A comprehensive review. IEEE Trans. Artif. Intell. 2020, 1, 85–103. [Google Scholar]
- Torrealba-Rodriguez, O.; Conde-Gutiérrez, R.; Hernández-Javier, A. Modeling and prediction of COVID-19 in Mexico applying mathematical and computational models. Chaos Solitons Fractals 2020, 138, 109946. [Google Scholar] [CrossRef] [PubMed]
- Williams, C.M.; Chaturvedi, R.; Urman, R.D.; Waterman, R.S.; Gabriel, R.A. Artificial intelligence and a pandemic: An analysis of the potential uses and drawbacks. J. Med Syst. 2021, 45, 26. [Google Scholar] [CrossRef]
- Naudé, W. Artificial Intelligence against Covid-19: An Early Review. 2020. Available online: https://papers.ssrn.com/abstract=3568314 (accessed on 12 May 2021).
- Allam, Z.; Jones, D.S. On the coronavirus (COVID-19) outbreak and the smart city network: Universal data sharing standards coupled with artificial intelligence (AI) to benefit urban health monitoring and management. Health 2020, 8, 46. [Google Scholar] [CrossRef] [Green Version]
- Gatto, M.; Bertuzzo, E.; Mari, L.; Miccoli, S.; Carraro, L.; Casagrandi, R.; Rinaldo, A. Spread and dynamics of the COVID-19 epidemic in Italy: Effects of emergency containment measures. Proc. Natl. Acad. Sci. USA 2020, 117, 10484–10491. [Google Scholar] [CrossRef] [Green Version]
- Mohanty, S.; Sharma, R.; Saxena, M.; Saxena, A. Heuristic Approach towards COVID-19: Big Data Analytics and Classification with Natural Language Processing; Springer: Singapore, 2021; pp. 775–791. [Google Scholar]
- Asif, S.; Wenhui, Y.; Jin, H.; Jinhai, S. Classification of COVID-19 from chest X-ray images using deep convolutional neural network. In Proceedings of the 2020 IEEE 6th International Conference on Computer and Communications (ICCC), Chengdu, China, 11–14 December 2020; pp. 426–433. [Google Scholar]
- Mei, X.; Lee, H.-C.; Diao, K.; Huang, M.; Lin, B.; Liu, C.; Xie, Z.; Ma, Y.; Robson, P.M.; Chung, M.; et al. Artificial intelligence-enabled rapid diagnosis of COVID-19 patients. medRxiv 2020. medRxiv:2020.04.12.20062661. [Google Scholar] [CrossRef]
- Patel, H.R.; Patel, A.M.; Parikh, S.M. Analytical study on COVID-19 to predict future infected cases ratio in India using machine leaning. IOP Conf. Ser. Mater. Sci. Eng. 2021, 1022, 012022. [Google Scholar] [CrossRef]
- Rahmatizadeh, S.; Valizadeh-Haghi, S.; Dabbagh, A. The role of artificial intelligence in management of critical COVID-19 patients. J. Cell. Mol. Anesth. 2020, 5, 16–22. [Google Scholar]
- McCall, B. COVID-19 and artificial intelligence: Protecting health-care workers and curbing the spread. Lancet Digit. Health 2020, 2, e166–e167. [Google Scholar] [CrossRef]
- Vaishya, R.; Javaid, M.; Khan, I.H.; Haleem, A. Artificial intelligence (AI) applications for COVID-19 pandemic. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 337–339. [Google Scholar] [CrossRef]
- Abd-Alrazaq, A.; Alajlani, M.; Alhuwail, D.; Schneider, J.; Al-Kuwari, S.; Shah, Z.; Hamdi, M.; Househ, M. Artificial intelligence in the fight against COVID-19: Scoping review. J. Med. Internet Res. 2020, 22, e20756. [Google Scholar] [CrossRef]
- Shantani, K.; Kannan, S.; Sheeza, A.; Hemalatha, K. The role of artificial intelligence and machine learning techniques: Race for COVID-19 vaccine. Arch. Clin. Infect. Dis. 2020, 15. [Google Scholar] [CrossRef]
- Jamshidi, M.B.; Lalbakhsh, A.; Talla, J.; Peroutka, Z.; Hadjilooei, F.; Lalbakhsh, P.; Jamshidi, M.; La Spada, L.; Mirmozafari, M.; Dehghani, M.; et al. Artificial intelligence and COVID-19: Deep learning approaches for diagnosis and treatment. IEEE Access 2020, 8, 109581–109595. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Wang, F.; Tang, J.; Nussinov, R.; Cheng, F. Artificial intelligence in COVID-19 drug repurposing. Lancet Digit. Health 2020, 2, e667–e676. [Google Scholar] [CrossRef]
- Shahid, O.; Nasajpour, M.; Pouriyeh, S.; Parizi, R.M.; Han, M.; Valero, M.; Li, F.; Aledhari, M.; Sheng, Q.Z. Machine learning research towards combating COVID-19: Virus detection, spread prevention, and medical assistance. arXiv 2020, arXiv:2010.07036. Available online: http://arxiv.org/abs/2010.07036 (accessed on 11 May 2021).
- Islam, M.N.; Inan, T.T.; Rafi, S.; Akter, S.S.; Sarker, I.H.; Najmul, A.K. A Survey on the Use of AI and ML for Fighting the COVID-19 Pandemic. arXiv 2020, arXiv:2008.07449. Available online: http://arxiv.org/abs/2008.07449 (accessed on 11 May 2021).
- Saxena, N.; Gupta, P.; Raman, R.; Rathore, A.S. Role of data science in managing COVID-19 pandemic. Indian Chem. Eng. 2020, 62, 385–395. [Google Scholar] [CrossRef]
- Khan, F.N.; Khanam, A.A.; Ramlal, A.; Ahmad, S. A Review on predictive systems and data models for COVID-19. In Econometrics for Financial Applications; Springer: Singapore, 2020; pp. 123–164. [Google Scholar]
- Nguyen, T.T. Artificial intelligence in the battle against coronavirus (COVID-19): A survey and future research directions. arXiv 2020, arXiv:2008.07343. Available online: http://arxiv.org/abs/2008.07343 (accessed on 12 May 2021).
- Syeda, H.B.; Syed, M.; Sexton, K.W.; Syed, S.; Begum, S.; Syed, F.; Prior, F.; Yu, F., Jr. Role of machine learning techniques to tackle the COVID-19 crisis: Systematic review. JMIR Med. Inform. 2021, 9, e23811. [Google Scholar] [CrossRef] [PubMed]
- Mahmood, S.; Hasan, K.; Carras, M.C.; Labrique, A. Global preparedness against COVID-19: We must leverage the power of digital health (Preprint). JMIR Public Health Surveill. 2020, 6, e18980. [Google Scholar] [CrossRef] [Green Version]
- Shinde, G.R.; Kalamkar, A.B.; Mahalle, P.N.; Dey, N.; Chaki, J.; Hassanien, A.E. Forecasting models for coronavirus disease (COVID-19): A survey of the state-of-the-art. SN Comput. Sci. 2020, 1, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Adly, A.S.; Adly, A.S.; Adly, M.S. Approaches Based on artificial intelligence and the internet of intelligent things to prevent the spread of COVID-19: Scoping review. J. Med. Internet Res. 2020, 22, e19104. [Google Scholar] [CrossRef] [PubMed]
- Chen, B.; Marvin, S.; While, A. Containing COVID-19 in China: AI and the robotic restructuring of future cities. Dialog Hum. Geogr. 2020, 10, 238–241. [Google Scholar] [CrossRef]
- Kielienyu, S.; Kantarci, B.; Turgut, D.; Khan, S. Bridging predictive analytics and mobile crowdsensing for future risk maps of communities against COVID-19. In Proceedings of the 18th ACM Symposium on Mobility Management and Wireless Access, New York, NY, USA, 16–20 November 2020; Association for Computing Machinery (ACM): New York, NY, USA, 2020; pp. 37–45. [Google Scholar]
- McBryde, E.S.; Meehan, M.T.; Adegboye, O.A.; Adekunle, A.I.; Caldwell, J.M.; Pak, A.; Rojas, D.P.; Williams, B.M.; Trauer, J.M. Role of modelling in COVID-19 policy development. Paediatr. Respir. Rev. 2020, 35, 57–60. [Google Scholar] [CrossRef]
- Leslie, D. Tackling COVID-19 through responsible AI innovation: Five steps in the right direction. Harv. Data Sci. Rev. 2020. [Google Scholar] [CrossRef]
- Kühn, M.J.; Abele, D.; Mitra, T.; Koslow, W.; Abedi, M.; Rack, K.; Siggel, M.; Khailaie, S.; Klitz, M.; Binder, S.; et al. Assessment of effective mitigation and prediction of the spread of SARS-CoV-2 in Germany using demographic information and spatial resolution. medRxiv 2020. medRxiv2020.12.18.20248509. [Google Scholar] [CrossRef]
- Richardson, G.P. Reflections on the foundations of system dynamics. Syst. Dyn. Rev. 2011, 27, 219–243. [Google Scholar] [CrossRef]
- Nah, K.; Chen, S.; Xiao, Y.; Tang, B.; Bragazzi, N.; Heffernan, J.; Asgary, A.; Ogden, N.; Wu, J. Scenario tree and adaptive decision making on optimal type and timing for intervention and social-economic activity changes to manage the COVID-19 pandemic. Eur. J. Pure Appl. Math. 2020, 13, 710–729. [Google Scholar] [CrossRef]
- Currie, C.S.; Fowler, J.W.; Kotiadis, K.; Monks, T.; Onggo, B.S.; Robertson, D.A.; Tako, A.A. How simulation modelling can help reduce the impact of COVID-19. J. Simul. 2020, 14, 83–97. [Google Scholar] [CrossRef] [Green Version]
- Cronemberger, F.; Gil-Garcia, J. Problem conceptualization as a foundation of data analytics in local governments: Lessons from the city of Syracuse, New York. In Proceedings of the 53rd Hawaii International Conference on System Sciences, Maui, HI, USA, 7–10 January 2020; Hawaii International Conference on System Sciences: Maui, HI, USA, 2020. [Google Scholar]
- Luna-Reyes, L.F.; Black, L.J.; Ran, W.; Andersen, D.L.; Jarman, H.; Richardson, G.P.; Andersen, D.F. Modeling and simulation as boundary objects to facilitate interdisciplinary research. Syst. Res. Behav. Sci. 2019, 36, 494–513. [Google Scholar] [CrossRef]
- Wolstenholme, E. Using generic system archetypes to support thinking and modelling. Syst. Dyn. Rev. 2004, 20, 341–356. [Google Scholar] [CrossRef]
- Sturniolo, S.; Waites, W.; Colbourn, T.; Manheim, D.; Panovska-Griffiths, J. Testing, tracing and isolation in compartmental models. medRxiv 2020. medRxiv:2020.05.14.20101808. [Google Scholar] [CrossRef]
- Paul, A.; Bhattacharjee, J.K.; Pal, A.; Chakraborty, S. Emergence of universality in the transmission dynamics of COVID-19. arXiv 2021, arXiv:2101.12556. Available online: http://arxiv.org/abs/2101.12556 (accessed on 12 May 2021).
- Cristianini, N. On the current paradigm in artificial intelligence. AI Commun. 2014, 27, 37–43. [Google Scholar] [CrossRef]
- Secinaro, S.; Calandra, D.; Secinaro, A.; Muthurangu, V.; Biancone, P. The role of artificial intelligence in healthcare: A structured literature review. BMC Med. Inform. Decis. Mak. 2021, 21, 125. [Google Scholar]
- Alimadadi, A.; Aryal, S.; Manandhar, I.; Munroe, P.B.; Joe, B.; Cheng, X. Artificial intelligence and machine learning to fight COVID-19. Physiol. Genom. 2020, 52, 200–202. [Google Scholar] [CrossRef]
- Pan, X. The application and legal issues of artificial intelligence in the global prevention and control of the COVID-19 epidemic. In Proceedings of the 6th Annual International Conference on Social Science and Contemporary Humanity Development (SSCHD 2020), Xi’an, China, 18–19 December 2020; Atlantis Press: Paris, France, 2021; pp. 440–445. [Google Scholar] [CrossRef]
- Jiang, L.; Wu, Z.; Xu, X.; Zhan, Y.; Jin, X.; Wang, L.; Qiu, Y. Opportunities and challenges of artificial intelligence in the medical field: Current application, emerging problems, and problem-solving strategies. J. Int. Med. Res. 2021, 49, 3000605211000157. [Google Scholar] [CrossRef]
- Raza, K. Artificial intelligence against COVID-19: A Meta-analysis of current research. In Big Data Analytics and Artificial Intelligence against COVID-19: Innovation Vision and Approach; Hassanien, A.-E., Dey, N., Elghamrawy, S., Eds.; Springer: Cham, Switzerland, 2020; pp. 165–176. [Google Scholar]
- Bullock, J.; Luccioni, A.; Pham, K.H.; Lam, C.S.N.; Luengo-Oroz, M. Mapping the landscape of Artificial Intelligence applications against COVID-19. J. Artif. Intell. Res. 2020, 69, 807–845. [Google Scholar] [CrossRef]
- Krishnaratne, S.; Pfadenhauer, L.M.; Coenen, M.; Geffert, K.; Jung-Sievers, C.; Klinger, C.; Kratzer, S.; Littlecott, H.; Movsisyan, A.; Rabe, J.E.; et al. Measures implemented in the school setting to contain the COVID-19 pandemic: A rapid scoping review. Cochrane Database Syst. Rev. 2020, 12, CD013812. [Google Scholar] [CrossRef] [PubMed]
- Lalmuanawma, S.; Hussain, J.; Chhakchhuak, L. Applications of machine learning and artificial intelligence for Covid-19 (SARS-CoV-2) pandemic: A review. Chaos Solitons Fractals 2020, 139, 110059. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Li, K.; Zhang, Z.; Li, K.; Yu, P.S. A Survey on applications of artificial intelligence in fighting against COVID-19. arXiv 2020, arXiv:2007.02202. Available online: http://arxiv.org/abs/2007.02202 (accessed on 11 May 2021).
- Santosh, K.C. AI-driven tools for coronavirus outbreak: Need of Active learning and cross-population train/test models on multitudinal/multimodal data. J. Med. Syst. 2020, 44, 1–5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wadali, J.S.; Khosla, P.K. Healthcare 4.0 in future capacity building for pandemic control. In Predictive and Preventive Measures for Covid-19 Pandemic; Khosla, P.K., Mittal, M., Sharma, D., Goyal, L.M., Eds.; Springer: Singapore, 2021; pp. 87–107. [Google Scholar]
- Wang, C.J.; Ng, C.Y.; Brook, R.H. Response to COVID-19 in Taiwan: Big data analytics, new technology, and proactive testing. JAMA 2020. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.P.; Javaid, M.; Haleem, A.; Suman, R. Internet of things (IoT) applications to fight against COVID-19 pandemic. Diabetes Metab. Syndr. 2020, 14, 521–524. [Google Scholar] [CrossRef]
- Song, J.; Gu, T.; Feng, X.; Ge, Y.; Mohapatra, P. Blockchain meets COVID-19: A framework for contact information sharing and risk notification system. arXiv 2020, arXiv:2007.10529. Available online: http://arxiv.org/abs/2007.10529 (accessed on 12 May 2021).
- Khanday, A.M.U.D.; Rabani, S.T.; Khan, Q.R.; Rouf, N.; Mohi Ud Din, M. Machine learning based approaches for detecting COVID-19 using clinical text data. Int. J. Inform. Technol. 2020, 16, 1–9. [Google Scholar] [CrossRef]
- Baclic, O.; Tunis, M.; Young, K.; Doan, C.; Swerdfeger, H.; Schonfeld, J. Challenges and opportunities for public health made possible by advances in natural language processing. Can. Commun. Dis. Rep. 2020, 46, 161–168. [Google Scholar] [CrossRef] [PubMed]
- Khmaissia, F.; Haghighi, P.S.; Jayaprakash, A.; Wu, Z.; Papadopoulos, S.; Lai, Y. An unsupervised machine learning approach to assess the ZIP code level impact of COVID-19 in NYC. arXiv 2020, arXiv:2006.08361. Available online: http://arxiv.org/abs/2006.08361 (accessed on 11 May 2021).
- Qeadan, F.; Honda, T.; Gren, L.H.; Dailey-Provost, J.; Benson, L.S.; Vanderslice, J.A.; Porucznik, C.A.; Waters, A.B.; Lacey, S.; Shoaf, K. Naive forecast for COVID-19 in Utah based on the South Korea and Italy models-the fluctuation between two extremes. Int. J. Environ. Res. Public Health 2020, 17, 2750. [Google Scholar] [CrossRef] [PubMed]
- Askarian, M.; Groot, G.; Taherifard, E.; Taherifard, E.; Akbarialiabad, H.; Borazjani, R.; Askarian, A.; Taghrir, M.H. Basics of developing a COVID-19 reopening roadmap: A systematic scoping review. Iran. J. Public Health 2021, 50, 232–244. [Google Scholar] [PubMed]
- Keeling, M.J.; Tildesley, M.J.; Atkins, B.D.; Penman, B.; Southall, E.; Guyver-Fletcher, G.; Holmes, A.; McKimm, H.; Gorsich, E.E.; Hill, E.M.; et al. The impact of school reopening on the spread of COVID-19 in England. medRxiv 2020. medRxiv:10.1101/2020.06.04.20121434. [Google Scholar] [CrossRef]
- World Health Organization. Key Messages and Actions for COVID-19 Prevention and Control in Schools. 2020. Available online: https://covid19-evidence.paho.org/handle/20.500.12663/792 (accessed on 12 May 2021).
- Vlacha, V.; Feketea, G.M. Return-to-school evaluation criteria for children with suspected coronavirus disease 2019. Front. Public Health 2020, 8, 618642. [Google Scholar] [CrossRef]
- Sheikh, A.; Sheikh, A.; Sheikh, Z.; Dhami, S. Reopening schools after the COVID-19 lockdown. J. Glob. Health 2020, 10, 010376. [Google Scholar] [CrossRef]
- Contreras, S.; Dehning, J.; Loidolt, M.; Zierenberg, J.; Spitzner, F.P.; Urrea-Quintero, J.H. The challenges of containing SARS-CoV-2 via test-trace-and-isolate. Nat. Commun. 2021, 12, 378. [Google Scholar] [CrossRef]
- Grundel, S.; Heyder, S.; Hotz, T.; Ritschel, T.K.S.; Sauerteig, P.; Worthmann, K. How to coordinate vaccination and social distancing to mitigate SARS-CoV-2 outbreaks. medRxiv 2020. medRxiv:2020.12.22.20248707. [Google Scholar] [CrossRef]
- Shayak, B.; Sharma, M.M.; Mishra, A.K. Impact of immediate and preferential relaxation of social and travel restrictions for vaccinated people on the spreading dynamics of COVID-19: A model-based analysis. medRxiv 2021. medRxiv:2021.01.19.21250100. [Google Scholar] [CrossRef]
- Aspinall, W.P.; Sparks, R.S.J.; Cooke, R.M.; Scarrow, J. Quantifying threat from COVID-19 infection hazard in primary schools in England. medRxiv 2020. medRxiv:2020.08.07.20170035. [Google Scholar]
- Kreck, M.; Scholz, E. Studying the course of Covid-19 by a recursive delay approach. medRxiv 2021. medRxiv:2021.01.18.21250012. [Google Scholar] [CrossRef]
- Thampi, N.; Sander, B.; Science, M. Preventing the introduction of SARS-CoV-2 into school settings. CMAJ Can. Med. Assoc. J. 2021, 193, E24–E25. [Google Scholar] [CrossRef] [PubMed]
- Colbourn, T.; Waites, W.; Panovska-Griffiths, J.; Manheim, D.; Sturniolo, S.; Colbourn, G. Modelling the health and economic impacts of population-wide testing, contact tracing and isolation (PTTI) strategies for COVID-19 in the UK. SSRN Electron. J. 2020. [Google Scholar] [CrossRef]
- Benneyan, J.C.; Gehrke, C.; Ilies, I.; Nehls, N. Potential community and campus Covid-19 outcomes under university and college reopening scenarios. medRxiv 2020. medRxiv:10.1101/2020.08.29.20184366. [Google Scholar] [CrossRef]
- Pavelka, M.; Van-Zandvoort, K.; Abbott, S.; Sherratt, K.; Majdan, M.; Analýz, I.Z.; Jarčuška, P.; Krajčí, M.; Flasche, S.; Funk, S. The effectiveness of population-wide, rapid antigen test based screening in reducing SARS-CoV-2 infection prevalence in Slovakia. medRxiv 2020. medRxiv:2020.12.02.20240648. [Google Scholar]
- Mina, M.J.; Andersen, K.G. COVID-19 testing: One size does not fit all. Science 2021, 371, 126–127. [Google Scholar] [CrossRef]
- Waites, W.; Cavaliere, M.; Manheim, D.; Panovska-Griffiths, J.; Danos, V. Scaling up epidemiological models with rule-based modelling. arXiv 2020, arXiv:2006.12077. Available online: http://arxiv.org/abs/2006.12077 (accessed on 11 May 2021).
- Tupper, P.; Colijn, C. COVID-19’s unfortunate events in schools: Mitigating classroom clusters in the context of variable transmission. medRxiv 2020. medRxiv:2020.10.20.20216267. [Google Scholar] [CrossRef]
- Wise, J. Covid-19: NHS test and trace must improve for schools to reopen safely, say researchers. BMJ 2020, 370, m3083. [Google Scholar] [CrossRef]
- Nguyen, L.L.K.; Howick, S.; McLafferty, D.; Anderson, G.H.; Pravinkumar, S.J.; Van Der Meer, R. Evaluating intervention strategies in controlling coronavirus disease 2019 (COVID-19) spread in care homes: An agent-based model. Infect. Control. Hosp. Epidemiol. 2020, 41, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Tayarani, N.M.-H. Applications of artificial intelligence in battling against covid-19: A literature review. Chaos Solitons Fractals 2021, 142, 110338. [Google Scholar] [CrossRef] [PubMed]
- Musulin, J.; Baressi Šegota, S.; Štifanić, D.; Lorencin, I.; Anđelić, N.; Šušteršič, T. Application of artificial intelligence-based regression methods in the problem of COVID-19 spread prediction: A systematic review. Int. J. Environ. Res. Public Health 2021, 18, 4287. [Google Scholar] [CrossRef] [PubMed]
- Marini, M.; Chokani, N.; Abhari, R.S. COVID-19 epidemic in Switzerland: Growth prediction and containment strategy using artificial intelligence and Big Data. medRxiv 2020. medRxiv:2020.03.30.20047472. [Google Scholar] [CrossRef] [Green Version]
- Gianquintieri, L.; Brovelli, M.A.; Pagliosa, A.; Dassi, G.; Brambilla, P.M.; Bonora, R.; Sechi, G.M.; Caiani, E.G. Mapping spatiotemporal diffusion of COVID-19 in Lombardy (Italy) on the base of emergency medical services activities. ISPRS Int. J. Geo. Inf. 2020, 9, 639. [Google Scholar] [CrossRef]
- Simsek, M.; Kantarci, B. Artificial intelligence-empowered mobilization of assessments in COVID-19-like pandemics: A case study for early flattening of the curve. Int. J. Environ. Res. Public Health 2020, 17, 3437. [Google Scholar] [CrossRef]
- The Python Standard Library—Python 3.9.1 Documentation. Available online: https://docs.python.org/3/library/ (accessed on 6 October 2020).

| Parameter | Range | Notes |
|---|---|---|
| Number of contacts per school day | 2.45–5.45 | Double |
| Transmission probability of pre-symptomatic | 0.01–0.1 | Double |
| Transmission probability of symptomatic | 0.1–0.2 | Double |
| Transmission probability of asymptomatic | 0.1–0.2 | Double |
| Pre-symptomatic rate (portion) | 0.35–0.65 | Double |
| Pre-symptomatic latent period | 1.3–3.3 | Double |
| Asymptomatic latent period | 3.47–5.47 | Double |
| Symptomatic latent period | 1.63–3.63 | Double |
| Self-isolation rate | 0.4–0.7 | Double |
| Symptomatic recovery period | 7–19 | Integer |
| Asymptomatic recovery period | 6–12 | Integer |
| Number of initially infected students | 1–10 | Integer |
| Class size | 15–35 | Integer |
| Number of classes | 10–50 | Integer |
| Isolate class | True or False | Boolean |
| Cross transmission | True or False | Boolean |
| Test class | True or False | Boolean |
| Number of tests in each class | 1–10 | Integer |
| Test results time (days) | 0–6 | Integer |
| Test expiry time (days) | 7–21 | Integer |
| Test frequency (days) | 1, 7, 14, 21 or 28 | Integer |
| Neurons per Layer | 2 Layers | 3 Layers | 4 Layers | 5 Layers |
|---|---|---|---|---|
| 128 | 21.1877 | 23.063 | 27.5082 | 31.5405 |
| 256 | 19.3726 | 17.6099 | 20.9791 | 23.8443 |
| 512 | 18.2007 | 15.5868 | 15.3118 * | 15.8596 |
| 1024 | 18.5459 | 14.7874 | 15.1074 | 14.9054 |
| Validation | Test | ||||
|---|---|---|---|---|---|
| Fold 1 | Fold 2 | Fold 3 | Fold 4 | Fold 5 | - |
| 14.8616 | 15.0594 | 14.8956 | 14.6614 | 14.9990 | 14.4264 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Valtchev, S.Z.; Asgary, A.; Chen, M.; Cronemberger, F.A.; Najafabadi, M.M.; Cojocaru, M.G.; Wu, J. Managing SARS-CoV-2 Testing in Schools with an Artificial Intelligence Model and Application Developed by Simulation Data. Electronics 2021, 10, 1626. https://doi.org/10.3390/electronics10141626
Valtchev SZ, Asgary A, Chen M, Cronemberger FA, Najafabadi MM, Cojocaru MG, Wu J. Managing SARS-CoV-2 Testing in Schools with an Artificial Intelligence Model and Application Developed by Simulation Data. Electronics. 2021; 10(14):1626. https://doi.org/10.3390/electronics10141626
Chicago/Turabian StyleValtchev, Svetozar Zarko, Ali Asgary, Michael Chen, Felippe A. Cronemberger, Mahdi M. Najafabadi, Monica Gabriela Cojocaru, and Jianhong Wu. 2021. "Managing SARS-CoV-2 Testing in Schools with an Artificial Intelligence Model and Application Developed by Simulation Data" Electronics 10, no. 14: 1626. https://doi.org/10.3390/electronics10141626
APA StyleValtchev, S. Z., Asgary, A., Chen, M., Cronemberger, F. A., Najafabadi, M. M., Cojocaru, M. G., & Wu, J. (2021). Managing SARS-CoV-2 Testing in Schools with an Artificial Intelligence Model and Application Developed by Simulation Data. Electronics, 10(14), 1626. https://doi.org/10.3390/electronics10141626








