Assessment of Machine Learning Techniques in IoT-Based Architecture for the Monitoring and Prediction of COVID-19
Abstract
:1. Introduction
1.1. Theoretical Background
- (1)
- Data collection of real-time symptoms (using IoT devices);
- (2)
- Quarantine/isolation center medication and result information;
- (3)
- Data processing center using Artificial Intelligent techniques;
- (4)
- Health caregivers and doctors; and
- (5)
- Cloud visualization.
1.2. Novel Contribution
- Incorporating an IoT–fog–cloud platform for the analysis of COVID-19 cases over geographical distribution patterns;
- Presenting a fog computing environment for the prediction of the disease spread of COVID-19;
- Analyzing state-of-the-art prediction techniques for the assessment of the disease spread of COVID-19 in real-time with a fog computing platform;
- Delivering real-time information to relevant doctors and caregivers for time-sensitive precautionary decision-making;
- Validating the proposed model to assess the overall performance enhancement in comparison to the state-of-the-art prediction models.
2. Related Work
2.1. IoT in Healthcare
2.2. Machine Learning in Healthcare
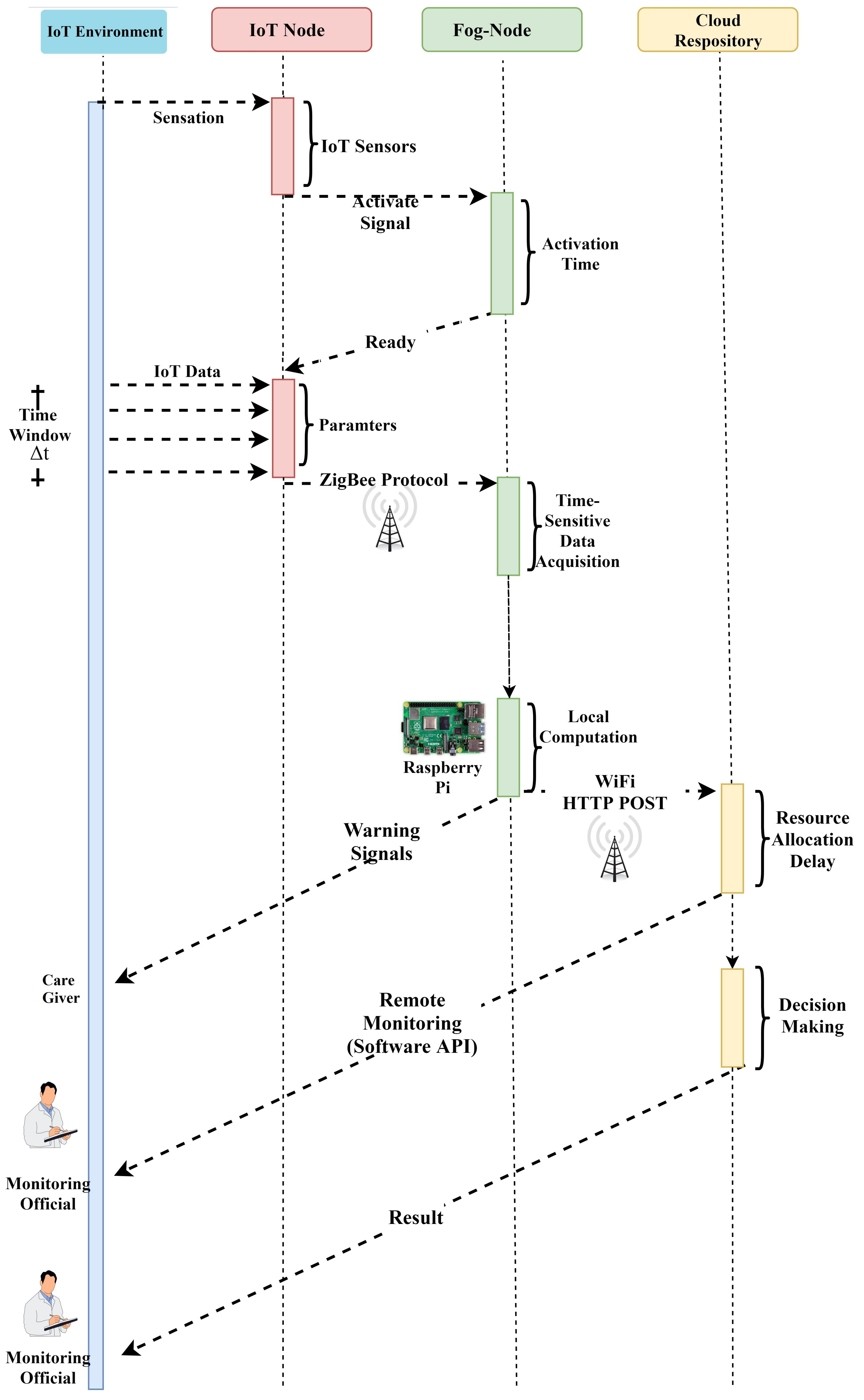
3. Proposed Approach
3.1. Fundamentals of Deep/Machine Learning Approaches
3.1.1. Support Vector Machine (SVM)
3.1.2. Artificial Neural Network (ANN)
3.1.3. Naive Bayes
3.1.4. K-Nearest Neighbors (K-NN)
3.1.5. Decision Table
3.1.6. Dense Neural Network
3.1.7. One Rule (OneR)
3.1.8. Long Short-Term Memory (LSTM) Technique
3.2. Research Methodology
3.2.1. Data Accumulation
3.2.2. Quarantine Center
3.2.3. Data Analytics
3.2.4. Medical Doctors
3.2.5. Cloud Data Repository
- Via wearable devices and sensors, the framework seamlessly captures time-sensitive information. A sore throat, cough, fever, exhaustion, and a low respiration rate are the most significant symptoms. The users also submit information about living in (or commuting to) contaminated areas through a smartphone application, as well as their potential interactions with people infected with COVID-19. The quarantine center presents information daily from its segregated patients. The context of the information is identical to the data obtained by users in real-time;
- Via the cloud infrastructure, intercepted COVID-19 data are submitted to the information processing module with the aid of smart devices. Via the cloud platform, automated documents from the hospitals can be periodically submitted to the data processing center. Deep learning techniques are used that constantly refine the models using the data obtained from the health care center. Based on the time-sensitive information acquired from each individual, the models are then used to classify possible events. The data are processed and presented on a time-sensitive dashboard. The dashboard can provide insights about the existence of the virus for doctors;
- The relevant specialists are contacted to check up with the patient if a possible case is found. For medical examinations with a Polymerase Chain Reaction, used to detect positive cases, the patient will be advised to attend the medical care center. The patient will be separated if the case is confirmed, and all connections will be contacted and quarantined.
3.2.6. Visualization
3.3. Case Prediction Analysis
Data Instances
3.4. Data Pre-Processing
3.4.1. Performance Assessment
3.4.2. Confusion Matrix
- True positive (TP): Total instances defined as positive and currently positive (using the statistical model);
- False positive (FP): Total instances labeled as positive (using the statistical model) but that are negative;
- False negative (FN): Total instances defined as negative (using the statistical model) that are positive;
- True negative (TN): Total instances defined as negative (using the predictive model) that are negative.
3.4.3. Cross-Validation
Accuracy
Root Mean Square Error
F-Measure
ROC Curve
4. Results and Discussion
4.1. Confusion Matrix
4.2. Performance Measures
5. Conclusions
Funding
Conflicts of Interest
References
- Birhane, M.; Bressler, S.; Chang, G.; Clark, T.; Dorough, L.; Fischer, M.; Watkins, L.F.; Goldstein, J.M.; Kugeler, K.; Langley, G.; et al. COVID-19 Vaccine Breakthrough Infections Reported to CDC—United States, January 1–April 30, 2021. Morb. Mortal. Wkly. Rep. 2021, 70, 792–793. [Google Scholar]
- Singh, R.P.; Javaid, M.; Haleem, A.; Suman, R. Internet of things (IoT) applications to fight against COVID-19 pandemic. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 521–524. [Google Scholar] [CrossRef]
- Ding, W.; Levine, R.; Lin, C.; Xie, W. Corporate immunity to the COVID-19 pandemic. J. Financ. Econ. 2021, 141, 802–830. [Google Scholar] [CrossRef]
- He, W.; Zhang, Z.J.; Li, W. Information technology solutions, challenges, and suggestions for tackling the COVID-19 pandemic. Int. J. Inf. Manag. 2021, 57, 102287. [Google Scholar] [CrossRef] [PubMed]
- Otoom, M.; Otoum, N.; Alzubaidi, M.A.; Etoom, Y.; Banihani, R. An IoT-based framework for early identification and monitoring of COVID-19 cases. Biomed. Signal Process. Control 2020, 62, 102149. [Google Scholar] [CrossRef] [PubMed]
- Javaid, M.; Khan, I.H. Internet of Things (IoT) enabled healthcare helps to take the challenges of COVID-19 Pandemic. J. Oral Biol. Craniofac. Res. 2021, 11, 209–214. [Google Scholar] [CrossRef] [PubMed]
- Jung, Y.; Agulto, R. A Public Platform for Virtual IoT-Based Monitoring and Tracking of COVID-19. Electronics 2021, 10, 12. [Google Scholar] [CrossRef]
- Mukherjee, R.; Kundu, A.; Mukherjee, I.; Gupta, D.; Tiwari, P.; Khanna, A.; Shorfuzzaman, M. IoT-cloud based healthcare model for COVID-19 detection: An enhanced k-Nearest Neighbour classifier based approach. Computing 2021, 1–21. [Google Scholar] [CrossRef]
- Sapkal, G.; Yadav, P.D.; Sahay, R.R.; Deshpande, G.; Gupta, N.; Nyayanit, D.A.; Patil, D.Y.; Kumar, S.; Abraham, P.; Panda, S.; et al. Neutralization of Delta variant with sera of Covishield vaccinees and COVID-19 recovered vaccinated individuals. bioRxiv 2021. [Google Scholar] [CrossRef]
- Ramallo-González, A.P.; González-Vidal, A.; Skarmeta, A.F. CIoTVID: Towards an Open IoT-Platform for Infective Pandemic Diseases such as COVID-19. Sensors 2021, 21, 484. [Google Scholar] [CrossRef] [PubMed]
- Bhatia, M.; Kaur, S.; Sood, S.K. IoT-Inspired Smart Toilet System for Home-Based Urine Infection Prediction. ACM Trans. Comput. Healthc. 2020, 1, 1–25. [Google Scholar] [CrossRef]
- Singh, V.; Chandna, H.; Kumar, A.; Kumar, S.; Upadhyay, N.; Utkarsh, K. IoT-Q-Band: A low cost internet of things based wearable band to detect and track absconding COVID-19 quarantine subjects. EAI Endorsed Trans. Internet Things 2020, 6. [Google Scholar] [CrossRef] [Green Version]
- Khan, P.I.; Razzak, I.; Dengel, A.; Ahmed, S. Understanding Information Spreading Mechanisms During COVID-19 Pandemic by Analyzing the Impact of Tweet Text and User Features for Retweet Prediction. arXiv 2021, arXiv:2106.07344. [Google Scholar]
- Qayyum, A.; Razzak, I.; Tanveer, M.; Kumar, A. Depth-wise dense neural network for automatic COVID19 infection detection and diagnosis. Ann. Oper. Res. 2021, 1–21. [Google Scholar] [CrossRef]
- Alhasan, A.; Audah, L.; Ibrahim, I.; Al-Sharaa, A.; Al-Ogaili, A.S.; Mohammed, J.M. A case-study to examine doctors’ intentions to use IoT healthcare devices in Iraq during COVID-19 pandemic. Int. J. Pervasive Comput. Commun. 2020. [Google Scholar] [CrossRef]
- Ghimire, A.; Thapa, S.; Jha, A.K.; Kumar, A.; Kumar, A.; Adhikari, S. AI and IoT Solutions for Tackling COVID-19 Pandemic. In Proceedings of the 2020 4th International Conference on Electronics, Communication and Aerospace Technology (ICECA), Coimbatore, India, 5–7 November 2020; pp. 1083–1092. [Google Scholar]
- Razzak, I.; Naz, S.; Rehman, A.; Khan, A.; Zaib, A. Improving coronavirus (COVID-19) diagnosis using deep transfer learning. MedRxiv 2020. [Google Scholar] [CrossRef] [Green Version]
- Jaafari, S.; Alhasani, A.; Alghosn, E.; Alfahhad, R.; Almutairi, S.M. Certain Investigations on IoT system for COVID-19. In Proceedings of the 2020 International Conference on Computing and Information Technology (ICCIT-1441), Tabuk, Saudi Arabia, 9–10 September 2020; pp. 1–4. [Google Scholar] [CrossRef] [Green Version]
- Vedaei, S.S.; Fotovvat, A.; Mohebbian, M.R.; Rahman, G.M.; Wahid, K.A.; Babyn, P.; Marateb, H.R.; Mansourian, M.; Sami, R. COVID-SAFE: An IoT-Based System for Automated Health Monitoring and Surveillance in Post-Pandemic Life. IEEE Access 2020, 8, 188538–188551. [Google Scholar] [CrossRef]
- Kumar, S.; Raut, R.D.; Narkhede, B.E. A proposed collaborative framework by using artificial intelligence-internet of things (AI-IoT) in COVID-19 pandemic situation for healthcare workers. Int. J. Healthc. Manag. 2020, 13, 337–345. [Google Scholar] [CrossRef]
- Usak, M.; Kubiatko, M.; Shabbir, M.S.; Viktorovna Dudnik, O.; Jermsittiparsert, K.; Rajabion, L. Health care service delivery based on the Internet of things: A systematic and comprehensive study. Int. J. Commun. Syst. 2020, 33, e4179. [Google Scholar] [CrossRef]
- Wu, F.; Wu, T.; Yuce, M.R. An internet-of-things (IoT) network system for connected safety and health monitoring applications. Sensors 2019, 19, 21. [Google Scholar] [CrossRef] [Green Version]
- Hamidi, H. An approach to develop the smart health using Internet of Things and authentication based on biometric technology. Future Gener. Comput. Syst. 2019, 91, 434–449. [Google Scholar] [CrossRef]
- Rath, M.; Pattanayak, B. Technological improvement in modern health care applications using Internet of Things (IoT) and proposal of novel health care approach. Int. J. Hum. Rights Healthc. 2019, 12, 148–162. [Google Scholar] [CrossRef]
- Darwish, A.; Hassanien, A.E.; Elhoseny, M.; Sangaiah, A.K.; Muhammad, K. The impact of the hybrid platform of internet of things and cloud computing on healthcare systems: Opportunities, challenges, and open problems. J. Ambient. Intell. Humaniz. Comput. 2019, 10, 4151–4166. [Google Scholar] [CrossRef]
- Zhong, C.L.; Li, Y.-L. Internet of things sensors assisted physical activity recognition and health monitoring of college students. Measurement 2020, 159, 107774. [Google Scholar] [CrossRef]
- Din, S.; Paul, A. Smart health monitoring and management system: Toward autonomous wearable sensing for internet of things using big data analytics. Future Gener. Comput. Syst. 2019, 91, 611–619. [Google Scholar] [CrossRef]
- Alshraideh, H.; Otoom, M.; Al-Araida, A.; Bawaneh, H.; Bravo, J. A web based cardiovascular disease detection system. J. Med. Syst. 2015, 39, 1–6. [Google Scholar] [CrossRef]
- Nguyen, T.T. Artificial intelligence in the battle against coronavirus (COVID-19): A survey and future research directions. arXiv 2020, arXiv:2008.07343. [Google Scholar]
- Maghded, H.S.; Ghafoor, K.Z.; Sadiq, A.S.; Curran, K.; Rawat, D.B.; Rabie, K. A novel AI-enabled framework to diagnose coronavirus COVID-19 using smartphone embedded sensors: Design study. In Proceedings of the 2020 IEEE 21st International Conference on Information Reuse and Integration for Data Science (IRI), Las Vegas, NV, USA, 11–13 August 2020; pp. 180–187. [Google Scholar]
- Rao, A.S.S.; Vazquez, J.A. Identification of COVID-19 can be quicker through artificial intelligence framework using a mobile phone–based survey when cities and towns are under quarantine. Infect. Control Hosp. Epidemiol. 2020, 41, 826–830. [Google Scholar] [CrossRef] [Green Version]
- Allam, Z.; Jones, D.S. On the coronavirus (COVID-19) outbreak and the smart city network: Universal data sharing standards coupled with artificial intelligence (AI) to benefit urban health monitoring and management. Healthcare 2020, 8, 46. [Google Scholar] [CrossRef] [Green Version]
- Fatima, S.A.; Hussain, N.; Balouch, A.; Rustam, I.; Saleem, M.; Asif, M. IoT enabled smart monitoring of coronavirus empowered with fuzzy inference system. Int. J. Adv. Res. Ideas Innov. Technol 2020, 6. [Google Scholar] [CrossRef]
- Peeri, N.C.; Shrestha, N.; Rahman, M.S.; Zaki, R.; Tan, Z.; Bibi, S.; Baghbanzadeh, M.; Aghamohammadi, N.; Zhang, W.; Haque, U. The SARS, MERS and novel coronavirus (COVID-19) epidemics, the newest and biggest global health threats: What lessons have we learned? Int. J. Epidemiol. 2020, 49, 717–726. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bhatia, M.; Sood, S.K. A comprehensive health assessment framework to facilitate IoT-assisted smart workouts: A predictive healthcare perspective. Comput. Ind. 2017, 92, 50–66. [Google Scholar] [CrossRef]
- Bhatia, M.; Sood, S.K. Game theoretic decision making in IoT-assisted activity monitoring of defence personnel. Multimed. Tools Appl. 2017, 76, 21911–21935. [Google Scholar] [CrossRef]
- Bhatia, M.; Sood, S.K. Internet of Things based activity surveillance of defence personnel. J. Ambient. Intell. Humaniz. Comput. 2018, 9, 2061–2076. [Google Scholar] [CrossRef]
- Bhatia, M.; Sood, S.K. Exploring temporal analytics in fog-cloud architecture for Smart Office HealthCare. Mob. Netw. Appl. 2019, 24, 1392–1410. [Google Scholar] [CrossRef]
- Bhatia, M.; Sood, S.K.; Kaur, S. Quantumized approach of load scheduling in fog computing environment for IoT applications. Computing 2020, 1–19. [Google Scholar] [CrossRef]







| Parameters | Hamidi (2020) | Rath and Pattanayak (2020) | Otoom et al. (2020) | Usak et al. (2020) | Wu et al. (2020) | Proposed Work |
|---|---|---|---|---|---|---|
| Application domain (AD) | Medical emergency | Distant monitoring system | Smart healthcare model for COVID-19 | Healthcare assessment framework | Monitoring healthcare framework | Novel system for healthcare framework |
| Major contribution (MC) | Medical healthcare system | Customized health assessment | Technique for prediction and monitoring of COVID-19 | Monitoring mosquito-borne disease | Healthcare system for monitoring heart disease | COVID-19 healthcare system |
| IoT | Wearable sensor devices | Android application | Sensors | RFID | Wearable sensors | IoT |
| Cloud computing (CC) | N | Y | Y | N | Y | Y |
| Fog computing (FC) | N | Y | Y | N | Edge computing | Y |
| Alert generation (AT) | N | Y | N | Y | N | Alert Based |
| Prediction model (PM) | NA | N | Hybrid | NA | N | T-RNN |
| Data storage (DS) | Local | Cloud | NA | Cloud | Local | cloud |
| Data mining technique (DMT) | N | NA | Hybrid | RAKE technology | NA | Spatio-temporal |
| Security mechanism (SM) | Y | Y | N | N | N | Y |
| Visualization (VsL) | Y | Y | N | Y | N | Y |
| Symptoms | West Nile | Japanese Virus | COVID-19 |
|---|---|---|---|
| Fever | ↑↑↑ | ↑↑↑(High fever) | Sudden onset of high fever |
| Saturation Drop | ↑↑↑ | ↑↑↑ | ↑↑↑ |
| Head ache | ↑↑↑ | ↑↑↑ | ↑↑↑ |
| Muscle and joint pain | ↑↑ | ↑↑ | ↑↑↑(severe) |
| Nausea or Vomiting | ↑↑↑ | ↑↑↑ | ↑↑↑ |
| Seizures | ↓ | ↑↑ | ↑↑ |
| Loss of memory | ↓ | ↑↑ | ↑↑ |
| Coma | ↑↑↑ | ↑↑↑ | ↑↑↑ |
| Drowsiness | ↑↑↑ | ↑↑↑ | ↑↑↑(Extreme tiredness) |
| Paralysis | ↑↑↑ | ↑↑↑ | ↑↑↑ |
| Tremors | ↑↑↑ | ↑↑↑ | ↓ |
| Neck stiffness | ↑/↓ | ↑/↓ | ↑ |
| Unconsciousness | ↑/↓ | ↑↑ | ↑↑ |
| Aversion of bright light | ↓ | ↓ | ↑ |
| Problem with speech or hearing | ↓ | ↑/↓ | ↑↑ |
| Models | Accuracy | RMSE | F-Measure | ROC |
|---|---|---|---|---|
| SVM | 93.23 | 25.25 | 93.12 | 92.59 |
| Neural Network | 93.16 | 21.26 | 93.26 | 95.45 |
| Naive Bayes | 89.26 | 32.15 | 91.48 | 94.65 |
| K-NN | 88.14 | 29.56 | 93.21 | 93.56 |
| Decision Table | 87.14 | 2648 | 93.65 | 94.12 |
| DNN | 93.25 | 12.26 | 92.26 | 92.65 |
| OneR | 90.26 | 65.25 | 69.26 | 70.25 |
| LSTM | 92.25 | 12.66 | 90.48 | 91.69 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aljumah, A. Assessment of Machine Learning Techniques in IoT-Based Architecture for the Monitoring and Prediction of COVID-19. Electronics 2021, 10, 1834. https://doi.org/10.3390/electronics10151834
Aljumah A. Assessment of Machine Learning Techniques in IoT-Based Architecture for the Monitoring and Prediction of COVID-19. Electronics. 2021; 10(15):1834. https://doi.org/10.3390/electronics10151834
Chicago/Turabian StyleAljumah, Abdullah. 2021. "Assessment of Machine Learning Techniques in IoT-Based Architecture for the Monitoring and Prediction of COVID-19" Electronics 10, no. 15: 1834. https://doi.org/10.3390/electronics10151834
APA StyleAljumah, A. (2021). Assessment of Machine Learning Techniques in IoT-Based Architecture for the Monitoring and Prediction of COVID-19. Electronics, 10(15), 1834. https://doi.org/10.3390/electronics10151834





