QoS-Ledger: Smart Contracts and Metaheuristic for Secure Quality-of-Service and Cost-Efficient Scheduling of Medical-Data Processing
Abstract
:1. Introduction
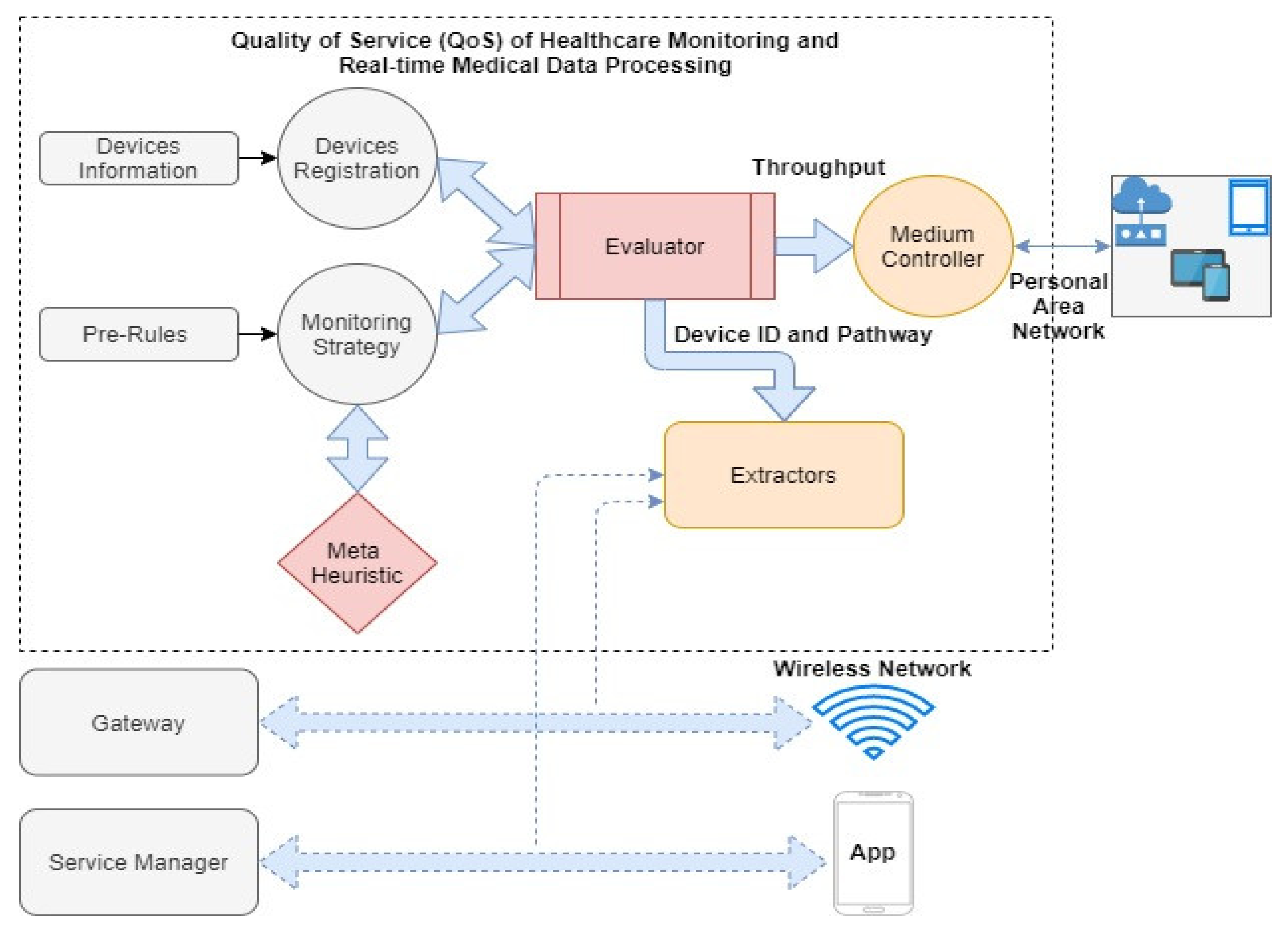
- This paper contributed to three different aspects. First, we proposed a detailed design for a metaheuristic-genetic-algorithm-based cost-efficient scheduler of medical-data processing and optimization of service records in real-time healthcare, accounting for environment-related challenges, scheduler optimization (rate of services) issues, and service delivery lifecycle.
- A novel and secure QoS efficient-computation framework is proposed, which effectively monitors QoS-indicator (range of parameter) performance, and provides a better experience to elderly recipients of medical services through applications (e-healthcare).
- In this paper, we design a blockchain-enabled serverless-distributed-network framework for medical-data transmission, process scheduling, service delivery, and computational task optimization and management. Smart contracts are designed and deployed to automate the execution of events and node transactions in a distributed medical environment. These medical nodes are connected in such a way that they create a chain-like chronological structure. Therefore, the system stores records of individual activities in the protected immutable blockchain storage.
- The working operations of the proposed QoS-ledger are demonstrated through a sequence diagram. It shows the events of the system’s execution in a sequential manner, which creates a better understanding and development of the overall architecture. The authors adopted a blockchain-enabled serverless-distributed P2P permissionless network, since it is an open-source, decentralized platform, employing intelligent smart-contract functionality.
- Finally, we evaluate and discuss QoS-ledger implementation-related issues, challenges, and limitations, and mention critical open research areas with potential for future developments.
2. Related Work
2.1. Quality-of-Service (QoS) and Cost-Efficient Scheduling
2.2. Efficient Computation of Medical-Data Processing and Service Delivery Optimization Solutions in e-healthcare Applications
3. Problem Formulation and Preliminaries
3.1. Notations and Problem Formulation
- Online medical assistant services (emergency medical services task scheduling).
- Offline patients’ record process scheduling.
- Online patients’ records process scheduling.
- Online requesting medical services data scheduling.
- Offline requesting medical consultant services data scheduling.
3.2. System Framework
4. The Proposed Smart Contracts-Enabled QoS for Real-Time Medical-Data Processing
4.1. Smart Contracts
4.2. Simulation Results and Discussion
5. Operations of the Proposed QoS-Ledger
5.1. QoS-Ledger Deployment Limitations and Challenges
5.1.1. Cross-Chain Platform Issues
5.1.2. Medical Sensitive Data-Related Protection and Privacy Challenges
5.1.3. Security Costs and Scalability Limitations for Medical Data
5.1.4. Compliance and Regulation Issues in e-healthcare Systems
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ashfaq, M.; Manzoor, A.; Ali, L.; Sheikh, K.A. Quality of Service as a Predictor of Customer Satisfaction in Healthcare Sector. IBT J. Bus. Stud. 2020, 16, 71–87. [Google Scholar] [CrossRef]
- Patan, R.; Ghantasala, G.S.P.; Sekaran, R.; Gupta, D.; Ramachandran, M. Smart healthcare and quality of service in IoT using grey filter convolutional based cyber physical system. Sustain. Cities Soc. 2020, 59, 102141. [Google Scholar] [CrossRef]
- Aboelfotoh, R.M.A. Quality of Service and Privacy in Internet of Things Dedicated to Healthcare. Ph.D. Thesis, Université d’Avignon, Avignon, France, 2021. [Google Scholar]
- Kurstjens, S.; Gemen, E.; Walk, S.; Njo, T.; Krabbe, J.; Gijzen, K.; Elisen, M.G.; Kusters, R. Performance of commercially-available cholesterol self-tests. Ann. Clin. Biochem. Int. J. Lab. Med. 2021, 58, 289–296. [Google Scholar] [CrossRef]
- Jeong, S.-M.; Choi, T.; Kim, D.; Han, K.; Kim, S.J.; Rhee, S.Y.; Giovannucci, E.L.; Shin, D.W. Association between high-density lipoprotein cholesterol level and risk of hematologic malignancy. Leukemia 2021, 35, 1356–1364. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.M.; Yan, X.; Shah, S.A.A.; Mamirkulova, G. Mining patient opinion to evaluate the service quality in healthcare: A deep-learning approach. J. Ambient Intell. Humaniz. Comput. 2019, 11, 2925–2942. [Google Scholar] [CrossRef]
- Issai, B.O.; Jarmajo, A.M. Relationship between Healthcare Facilities and Quality Delivery in Covid-19 Isolation Centers in Nigeria. Fudma J. Manag. Sci. 2021, 4, 326–335. [Google Scholar]
- Tsai, C.-W. Toward Blockchain for Intelligent Systems. IEEE Consum. Electron. Mag. 2021, 1. [Google Scholar] [CrossRef]
- Khan, A.; Laghari, A.; Awan, S. Machine Learning in Computer Vision: A Review. Scalable Inf. Syst. 2021, 8, e4. [Google Scholar] [CrossRef]
- Kashani, M.H.; Rahmani, A.M.; Navimipour, N.J. Quality of service-aware approaches in fog computing. Int. J. Commun. Syst. 2020, 33, e4340. [Google Scholar] [CrossRef]
- Stiglic, G.; Kocbek, P.; Fijacko, N.; Zitnik, M.; Verbert, K.; Cilar, L. Interpretability of machine learning-based prediction models in healthcare. Wiley Interdiscip. Rev. Data Min. Knowl. Discov. 2020, 10, 1379. [Google Scholar] [CrossRef]
- Chehri, A.; Mouftah, H.T. Internet of Things-integrated IR-UWB technology for healthcare applications. Concurr. Comput. Pract. Exp. 2021, 32, e5454. [Google Scholar] [CrossRef]
- Khan, A.A.; Shaikh, A.A.; Cheikhrouhou, O.; Laghari, A.A.; Rashid, M.; Shafiq, M.; Hamam, H. IMG-forensics: Multimedia-enabled information hiding investigation using convolutional neural network. IET Image Process. 2021, 1–19. [Google Scholar] [CrossRef]
- Bonaccorsi, G.; Romiti, A.; Ierardi, F.; Innocenti, M.; Del Riccio, M.; Frandi, S.; Bachini, L.; Zanobini, P.; Gemmi, F.; Lorini, C. Health-literate healthcare organizations and quality of care in hospitals: A cross-sectional study conducted in Tuscany. Int. J. Environ. Res. Public Health 2020, 17, 2508. [Google Scholar] [CrossRef] [Green Version]
- Khan, A.A.; Laghari, A.A.; Awan, S.; Jumani, A.K. Fourth Industrial Revolution Application: Network Forensics Cloud Security Issues. In Security Issues and Privacy Concerns in Industry 4.0 Applications; John Wiley & Sons: Hoboken, NJ, USA, 2021; pp. 15–33. [Google Scholar]
- Tuli, S.; Tuli, S.; Wander, G.; Wander, P.; Gill, S.S.; Dustdar, S.; Sakellariou, R.; Rana, O. Next generation technologies for smart healthcare: Challenges, vision, model, trends and future directions. Internet Technol. Lett. 2020, 3, e145. [Google Scholar] [CrossRef] [Green Version]
- Selvaraj, S.; Sundaravaradhan, S. Challenges and opportunities in IoT healthcare systems: A systematic review. SN Appl. Sci. 2020, 2, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Laghari, A.A.; Wu, K.; Laghari, R.A.; Ali, M.; Khan, A.A. A Review and State of Art of Internet of Things (IoT). Arch. Comput. Methods Eng. 2021. [Google Scholar] [CrossRef]
- Aoudia, I.; Benharzallah, S.; Kahloul, L.; Kazar, O. A Multi-Population Genetic Algorithm for Adaptive QoS-Aware Service Composition in Fog-IoT Healthcare Environment. Int. Arab. J. Inf. Technol. 2021, 18, 464–475. [Google Scholar] [CrossRef]
- Valkanis, A.; Nicopolitidis, P.; Papadimitriou, G.; Kallergis, D.; Douligeris, C.; Bamidis, P.D. Efficient resource allocation in tactile-capable Ethernet passive optical healthcare LANs. IEEE Access 2020, 8, 52981–52995. [Google Scholar] [CrossRef]
- Yuan, X.; Tian, H.; Wang, H.; Su, H.; Liu, J.; Taherkordi, A. Edge-enabled wbans for efficient qos provisioning healthcare monitoring: A two-stage potential game-based computation offloading strategy. IEEE Access 2020, 8, 92718–92730. [Google Scholar] [CrossRef]
- Zuhra, F.T.; Bin Abu Bakar, K.; Arain, A.A.; Khan, U.A.; Bhangwar, A.R. MIQoS-RP: Multi-Constraint Intra-BAN, QoS-Aware Routing Protocol for Wireless Body Sensor Networks. IEEE Access 2020, 8, 99880–99888. [Google Scholar] [CrossRef]
- Sefati, S.; Navimipour, N.J. A QoS-aware service composition mechanism in the Internet of things using a hidden Markov model-based optimization algorithm. IEEE Internet Things J. 2021, 8, 15620–15627. [Google Scholar] [CrossRef]
- Aoudia, L.; Kahloul, L.; Benharzallah, S.; Kazar, O. QoS-aware service composition in Fog-IoT computing using multi-population genetic algorithm. In Proceedings of the 21st International Arab Conference on Information Technology (ACIT), Al Ain, UAE, 28–30 November 2020; pp. 1–9. [Google Scholar]
- Napoli, D.; Ribino, P.; Serino, L. Customisable assistive plans as dynamic composition of services with normed-QoS. J. Ambient Intell. Humaniz. Comput. 2021, 12, 9667–9692. [Google Scholar] [CrossRef]
- Tan, L.; Yu, K.; Bashir, A.K.; Cheng, X.; Ming, F.; Zhao, L.; Zhou, X. Toward real-time and efficient cardiovascular monitoring for COVID-19 patients by 5G-enabled wearable medical devices: A deep learning approach. Neural Comput. Appl. 2021, in press. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Zhang, H.; Pirbhulal, S.; Wu, W.; Albuquerque, V.H.C.D. Active balancing mechanism for imbalanced medical data in deep learning—Based classification models. ACM Trans. Multimed. Comput. Commun. Appl. 2020, 16, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Wang, X.; Yang, L.T.; Wang, Y.; Ren, L.; Deen, M.J. ADTT: A highly efficient distributed tensor-train decomposition method for IIoT big data. IEEE Trans. Ind. Inform. 2021, 17, 1573–1582. [Google Scholar] [CrossRef]
- Vizitiu, A.; Niƫă, C.I.; Puiu, A.; Suciu, C.; Itu, L.M. Applying deep neural networks over homomorphic encrypted medical data. Comput. Math. Methods Med. 2020, 2020, 3910250. [Google Scholar] [CrossRef]
- Lu, M.Y.; Williamson, D.F.K.; Chen, T.Y.; Chen, R.J.; Barbieri, M.; Mahmood, F. Data-efficient and weakly supervised computational pathology on whole-slide images. Nat. Biomed. Eng. 2021, 5, 555–570. [Google Scholar] [CrossRef] [PubMed]
- Saba, T.; Haseeb, K.; Ahmed, I.; Rehman, A. Secure and energy-efficient framework using Internet of Medical Things for e-healthcare. J. Infect. Public Health 2020, 13, 1567–1575. [Google Scholar] [CrossRef] [PubMed]
- Tang, S.; He, B.; Yu, C.; Li, Y.; Li, K. A survey on spark ecosystem: Big data processing infrastructure, machine learning, and applications. IEEE Trans. Knowl. Data Eng. 2020. [Google Scholar] [CrossRef]
- Pérez-García, F.; Sparks, R.; Ourselin, S. TorchIO: A Python library for efficient loading, preprocessing, augmentation and patch-based sampling of medical images in deep learning. Comput. Methods Programs Biomed. 2021, 208, 106236. [Google Scholar] [CrossRef]
- Singh, M.; Baranwal, G.; Tripathi, A.K. QoS-Aware Selection of IoT-Based Service. Arab. J. Sci. Eng. 2020, 45, 10033–10050. [Google Scholar] [CrossRef]
- Qiu, Y.; Zhang, H.; Long, K. Computation Offloading and Wireless Resource Management for Healthcare Monitoring in Fog-Computing based Internet of Medical Things. IEEE Internet Things J. 2021, 8, 15875–15883. [Google Scholar] [CrossRef]
- Hassan, S.R.; Ahmad, I.; Ahmad, S.; AlFaify, A.; Shafiq, M. Remote pain monitoring using fog computing for e-Healthcare: An efficient architecture. Sensors 2020, 20, 6574. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Huang, C. Microservice based computational offloading framework and cost-efficient task scheduling algorithm in heterogeneous fog cloud network. IEEE Access 2020, 8, 56680–56694. [Google Scholar] [CrossRef]
- Saeed, W.; Ahmad, Z.; Jehangiri, A.I.; Mohamed, N.; Umar, A.I.; Ahmad, J. A fault tolerant data management scheme for healthcare Internet of Things in fog computing. KSII Trans. Internet Inf. Syst. 2021, 15, 35–57. [Google Scholar]
- Iqbal, N.; Ahmad, S.; Ahmad, R.; Kim, D. A Scheduling Mechanism Based on Optimization Using IoT-Tasks Orchestration for Efficient Patient Health Monitoring. Sensors 2021, 21, 5430. [Google Scholar] [CrossRef]
- Rivera, G.; Cisneros, L.; Sánchez-Solís, P.; Rangel-Valdez, N.; Rodas-Osollo, J. Genetic algorithm for scheduling optimization considering heterogeneous containers: A real-world case study. Axioms 2020, 9, 27. [Google Scholar] [CrossRef] [Green Version]
- Kishor, A.; Chakraborty, C.; Jeberson, W. Reinforcement learning for medical information processing over heterogeneous networks. Multimed. Tools Appl. 2021, 80, 23983–24004. [Google Scholar] [CrossRef]
- ElRahman, S.A.; Alluhaidan, A.S. Blockchain technology and IoT-edge framework for sharing healthcare services. Soft Comput. 2021, 25, 1–25. [Google Scholar] [CrossRef]
- Sammeta, N.; Parthiban, L. Hyperledger blockchain enabled secure medical record management with deep learning-based diagnosis model. Complex Intell. Syst. 2021, 1–16. [Google Scholar] [CrossRef]
- Singh, P.D.; Kaur, R.; Singh, K.D.; Dhiman, G.; Soni, M. Fog-centric IoT based smart healthcare support service for monitoring and controlling an epidemic of Swine Flu virus. Informatics Med. Unlocked 2021, 26, 100636. [Google Scholar] [CrossRef]
- Rajendran, S. Application of blockchain technique to reduce platelet wastage and shortage by forming hospital collaborative networks. IISE Trans. Healthc. Syst. Eng. 2021, 11, 128–144. [Google Scholar] [CrossRef]
- Khan, A.A.; Laghari, A.A.; Liu, D.S.; Shaikh, A.A.; Ma, D.A.; Wang, C.Y.; Wagan, A.A. EPS-Ledger: Blockchain Hyperledger Sawtooth-Enabled Distributed Power Systems Chain of Operation and Control Node Privacy and Security. Electronics 2021, 10, 2395. [Google Scholar] [CrossRef]
- Safa, M.; Pandian, A. A Review on Big IoT Data Analytics for Improving QoS-Based Performance in System: Design, Opportunities, and Challenges. In Artificial Intelligence Techniques for Advanced Computing Applications; Springer Nature: Basingstoke, UK, 2021; pp. 433–443. [Google Scholar]
- Jumani, A.K.; Laghari, A.A.; Khan, A.A. Blockchain and Big Data: Supportive Aid for Daily Life. In Security Issues and Privacy Concerns in Industry 4.0 Applications; John Wiley & Sons: Hoboken, NJ, USA, 2021; pp. 141–178. [Google Scholar]
- Ayub Khan, A.; Laghari, A.A.; Shaikh, A.A.; Bourouis, S.; Mamlouk, A.M.; Alshazly, H. Educational Blockchain: A Secure Degree Attestation and Verification Traceability Architecture for Higher Education Commission. Appl. Sci. 2021, 11, 10917. [Google Scholar] [CrossRef]
- Khan, A.A.; Shaikh, Z.A.; Laghari, A.A.; Bourouis, S.; Wagan, A.A.; Ali, G.A.A.A. Blockchain-Aware Distributed Dynamic Monitoring: A Smart Contract for Fog-Based Drone Management in Land Surface Changes. Atmosphere 2021, 12, 1525. [Google Scholar] [CrossRef]






| Research Method | Research Description | Challenges/Limitations | References |
|---|---|---|---|
| Efficient resource allocation in tactile-capable ethernet-passive optical healthcare LANs. | In this study, the authors proposed a two-stage potential game-based computation-offloading strategy that optimizes resource allocation, while taking into consideration users’ priority, and their tasks, in accordance with the wireless body area network. |
| [20] |
| Edge-enabled WBANs for efficient QoS-provisioning healthcare monitoring: a two-stage potential game-based computation-offloading strategy. | This study focuses on communication networks for the healthcare environment, and provides a required QoS to ensure reliability in data delivery, considerable data rate, and low latency, with accuracy. For this purpose, the authors of this paper introduced a passive optical network based on a new double-per-priority-queue dynamic wavelength and bandwidth allocation algorithm. |
| [21] |
| MIQoS-RP: multi-constraint intra-BAN, QoS-aware routing protocol for wireless body sensor networks. | The proposed multi-constraint intra-body-area sensor network provides an adoptive QoS aware routing protocol for smooth transactions of sensitive healthcare-data processing and delivery of services. |
| [22] |
| A QoS-aware service composition mechanism in the internet of things using a Hidden Markov Model-based optimization algorithm. | In this paper, the authors proposed an efficient method, based on the Hidden Markov Model and ant colony optimization, for the enhancement of QoS services and composition issues in real-time. |
| [23] |
| QoS-aware service composition in Fog-IoT computing using multi-population genetic algorithm. | A QoS composition approach presented for healthcare based on the multi-population of genetic algorithm in IoT-fog environment. Mainly focuses on the transport layer and divides the layer into four subparts for medical-data security, storage, pre-processing, and monitoring. |
| [24] |
| Customizable assistive plans as the dynamic composition of services with normed-QoS. | The integration of a service-oriented approach, with normative reasoning, to automatically generate assistive tasks. These tasks are customized for distinct users (profiles) of healthcare in the proposed environment. |
| [25] |
| Chaincode #1: deviceRegistration() |
| System Initialization: The QoS-ledger engineer initiates system and manages all transactions and addresses Data: The QoS-ledger engineer starts system and handle-application request; Engineer is only able to validate device registration request after verification; int main(): QoS.file[x].text; elderly patient’s device registration, (deviceReg); device ID; (DID); patients, physicians/consultants; patients, name; physicians/consultants, name; (name); Blockchain timestamp[execute]; QoS-Ledger deviceRegistration() contract addresses, elderly device registration, deviceRegistration, counter (deviceCount()); QoS-Ledger Engineer is responsible to authorize individual and set of devices and maintain registration addresses in the smart contract; if int main(): QoS.file[x].text is = true, then if deviceReg is not in the Ledger, then, change state of the contract and add new transaction of registration Also, QoS-Ledger Engineer manage the records of deviceReg(), DID(), patients, physician, name, timestamp[execute]; and update QoS-Ledger deviceRegistration() Addresses; calculate individual updates of deviceCount() through counter else verify, generated errors, and update state, rollback, terminate; else verify, generated errors, and update state, rollback, terminate; |
| Chaincode #2: AddTransactions() and secureDataPreservation() |
| System Initialization: The QoS-ledger engineer initiates system and manages all transactions and addresses Data: The QoS-ledger engineer starts system and handle-application request; Engineer is only able to validate new node transactions and update the state of distributed ledger device after analysis; int main(): QoS.file[x].text; QoS Logs, (QoSLogs); QoS node transactions and preservation in the distributed ledger; Authorize, (accessQoSNodeTransactions); real-time updates of QoS Logs; Blockchain timestamp[run], the QoS-Ledger Engineer manage AddTransactions() contract QoS-Ledger Engineer (QLE), QoS Logs counter (QoSLogsCount); QLE is responsible for authorized individuals and groups and manages to add nodes transactions addresses if int main(): QoS.file[x].text is = QLE = true, then if QoSLogs node has not available, then, state of QoS-Ledger AddTransactions() change, and add new node transactions and records; Also, records state of QoSLogs(), accessQoSNodeTransactions(), real-time updates of QoS Logs, timestamp (run); store all these transactions and updates on QoS-Ledger contracts to the Blockchain Distributed Ledger secureDataTransactions() QoSLogsCount is + 1; else verify, generated errors, and update state, rollback, terminate; else verify, generated errors, and update state, rollback, terminate; |
| Research Method | Matrix of the Other State-of-the-Art Methods | Matrix of the Proposed QoS-Ledger | References |
|---|---|---|---|
| Blockchain technology and the IoT-edge framework for sharing healthcare services. | The authors presented the details of the proposed system as follows:
| The details of the proposed QoS-ledger are as follows:
| [42] |
| Hyperledger blockchain-enabled secure medical record management with a deep learning-based diagnosis model. | N. Sammeta and L. Parthiban proposed a model based on blockchain hyperledger with deep learning for users to control access to data, permit the hospital authority to read and write data, and manage contacts in emergencies. The performance matrix of this proposed model is as follows:
| [43] | |
| A smart healthcare support service based on fog-centric IoT for monitoring and controlling a Swine Flu virus epidemic. | P. D. Singh et al. presented fog-centric IoT-based intelligent services of healthcare for monitoring and controlling. The criteria of evaluation of performance matrix are as follows:
| [44] | |
| Application of blockchain technique to reduce platelet wastage and shortage by forming hospital collaborative networks. | The author of hospital-ledger presented an applicational blockchain infrastructure to reduce platelet wastage and form hospital networks and their collaboration by using multi-criteria culturing techniques. To analyze the proposed applicational model, the author defined some aspects of the investigation that are discussed as follows:
| [45] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khan, A.A.; Shaikh, Z.A.; Baitenova, L.; Mutaliyeva, L.; Moiseev, N.; Mikhaylov, A.; Laghari, A.A.; Idris, S.A.; Alshazly, H. QoS-Ledger: Smart Contracts and Metaheuristic for Secure Quality-of-Service and Cost-Efficient Scheduling of Medical-Data Processing. Electronics 2021, 10, 3083. https://doi.org/10.3390/electronics10243083
Khan AA, Shaikh ZA, Baitenova L, Mutaliyeva L, Moiseev N, Mikhaylov A, Laghari AA, Idris SA, Alshazly H. QoS-Ledger: Smart Contracts and Metaheuristic for Secure Quality-of-Service and Cost-Efficient Scheduling of Medical-Data Processing. Electronics. 2021; 10(24):3083. https://doi.org/10.3390/electronics10243083
Chicago/Turabian StyleKhan, Abdullah Ayub, Zaffar Ahmed Shaikh, Laura Baitenova, Lyailya Mutaliyeva, Nikita Moiseev, Alexey Mikhaylov, Asif Ali Laghari, Sahar Ahmed Idris, and Hammam Alshazly. 2021. "QoS-Ledger: Smart Contracts and Metaheuristic for Secure Quality-of-Service and Cost-Efficient Scheduling of Medical-Data Processing" Electronics 10, no. 24: 3083. https://doi.org/10.3390/electronics10243083
APA StyleKhan, A. A., Shaikh, Z. A., Baitenova, L., Mutaliyeva, L., Moiseev, N., Mikhaylov, A., Laghari, A. A., Idris, S. A., & Alshazly, H. (2021). QoS-Ledger: Smart Contracts and Metaheuristic for Secure Quality-of-Service and Cost-Efficient Scheduling of Medical-Data Processing. Electronics, 10(24), 3083. https://doi.org/10.3390/electronics10243083










