LI-Care: A LabVIEW and IoT Based eHealth Monitoring System
Abstract
:1. Introduction
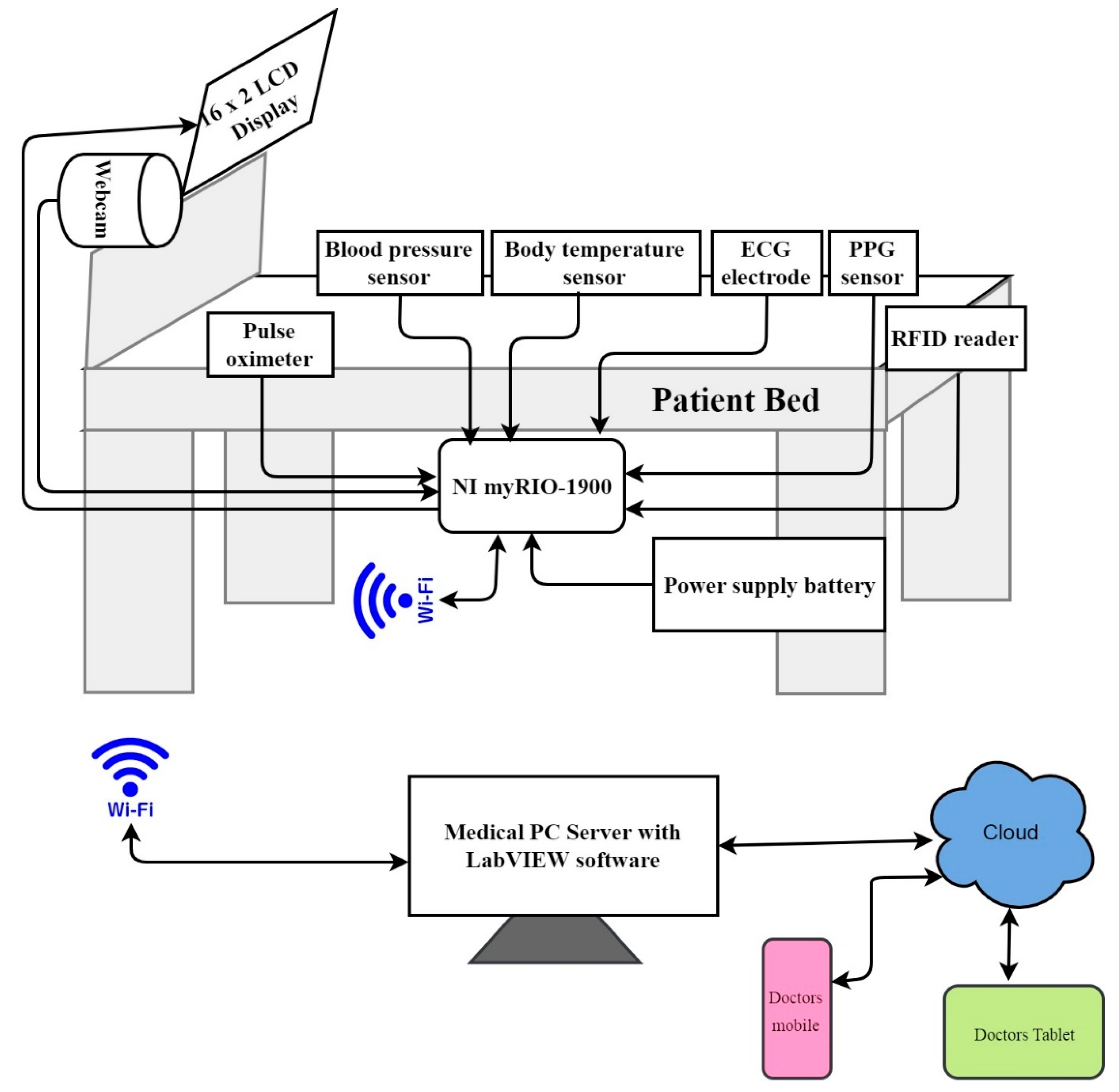
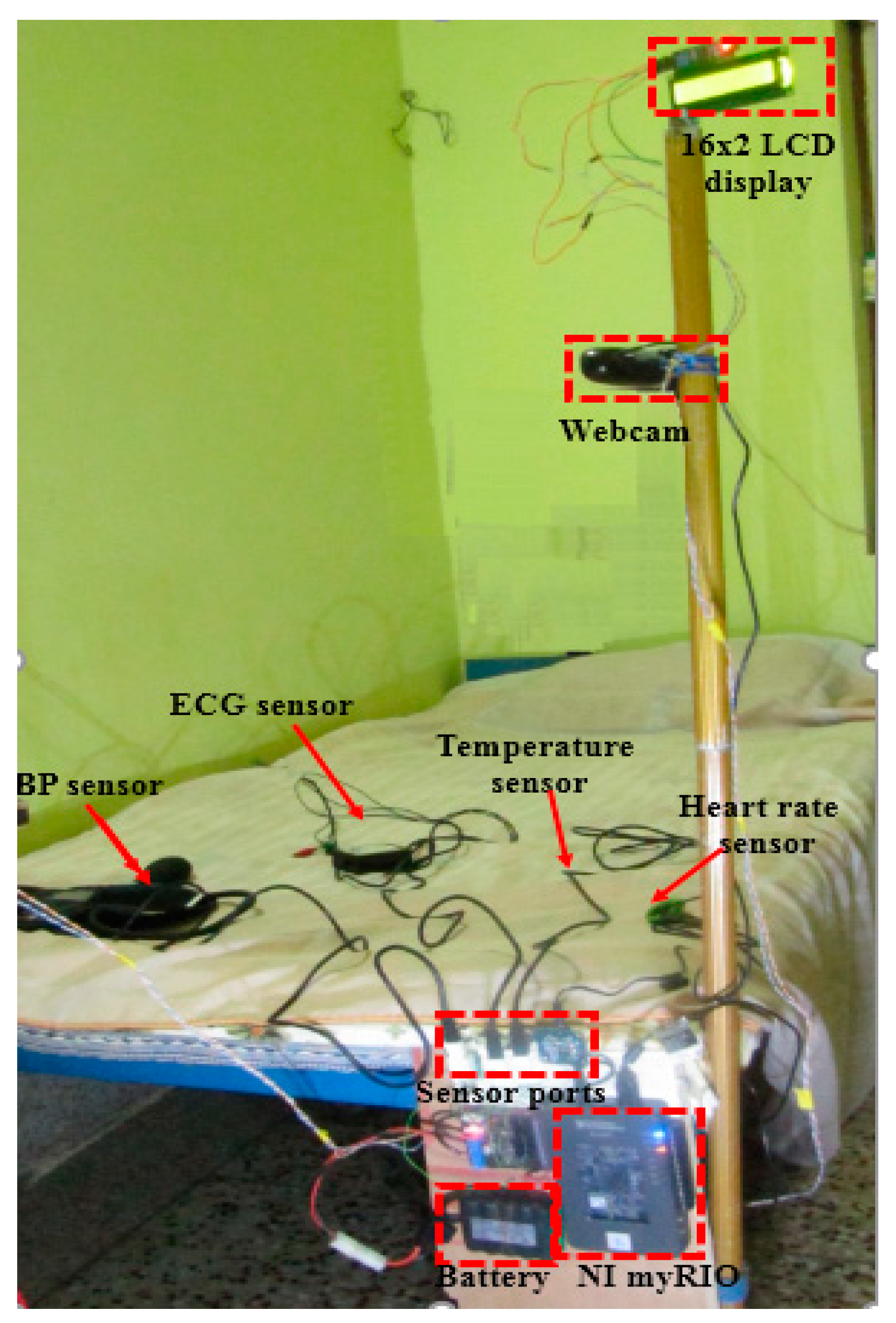
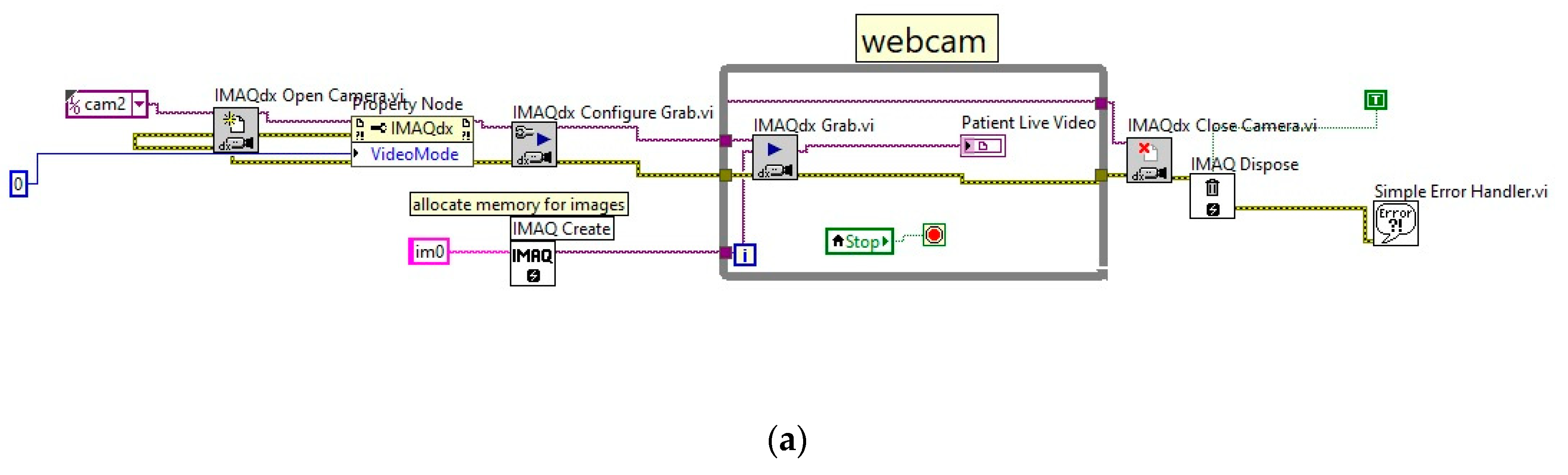
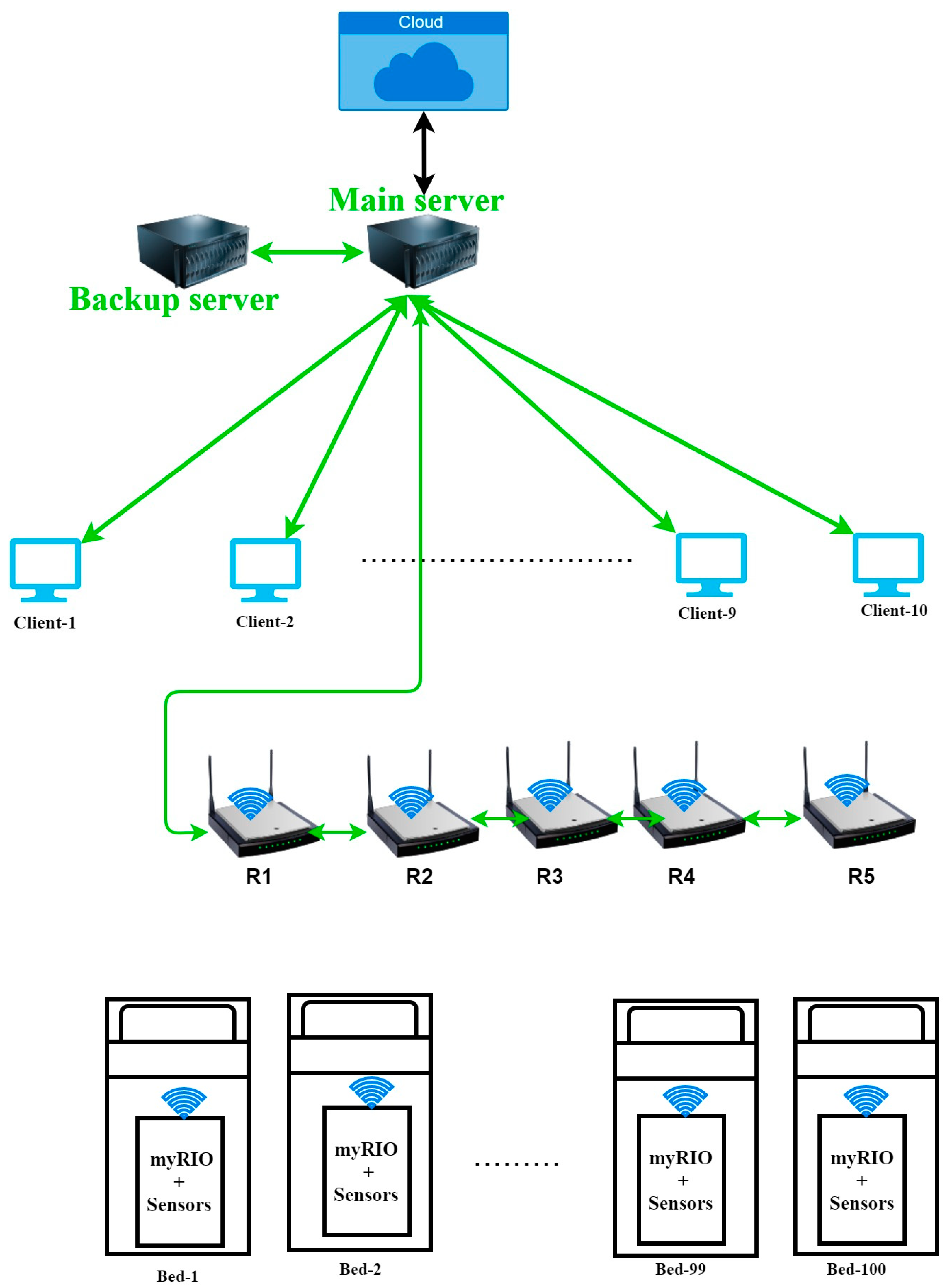
2. Setup of the LI-Care System
Sensor Interfacing with myRIO-1900
3. Real-Time Implementation and Discussion of Results
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Miraz, M.H.; Ali, M.; Excell, P.S.; Picking, R. A Review on Internet of Things (IoT): Internet of Everything (IoE) and Internet of Nano Things (IoNT). In Proceedings of the 2015 Internet Technologies and Applications (ITA), Wrexham, UK, 8–11 September 2015; pp. 219–224. [Google Scholar] [CrossRef] [Green Version]
- Elkhodr, M.; Shahrestani, S.; Cheung, H. Internet of Things Applications: Current and Future Development. In Innovative Research and Applications in Next-Generation High Performance Computing; IGI Global: Hershey, PA, USA, 2016; pp. 397–427. [Google Scholar]
- Mustafa, T.; Varol, A. Review of the Internet of Things for Healthcare Monitoring. In Proceedings of the 8th International Symposium on Digital Forensics and Security (ISDFS), Beirut, Lebanon, 1–2 June 2020; pp. 1–6. [Google Scholar] [CrossRef]
- Vedaei, S.S.; Fotovvat, A.; Mohebbian, M.R.; Rahman, G.M.; Wahid, K.A.; Babyn, P.; Marateb, H.R.; Mansourian, M.; Sami, R. COVID-SAFE: An IoT-Based System for Automated Health Monitoring and Surveillance in Post-Pandemic Life. IEEE Access 2020, 8, 188538–188551. [Google Scholar] [CrossRef] [PubMed]
- Ko, J.; Lu, C.; Srivastava, M.B.; Stankovic, J.A.; Terzis, A.; Welsh, M. Wireless Sensor Networks for Healthcare. Proc. IEEE 2010, 98, 1947–1960. [Google Scholar] [CrossRef] [Green Version]
- Yang, G.; Xie, L.; Mäntysalo, M.; Zhou, X.; Pang, Z.; Da Xu, L.; Kao-Walter, S.; Chen, Q.; Zheng, L.R. A Health-IoT Platform Based on the Integration of Intelligent Packaging, Unobtrusive Bio-Sensor, and Intelligent Medicine Box. IEEE Trans. Ind. Inform. 2014, 10, 2180–2191. [Google Scholar] [CrossRef] [Green Version]
- Hussain, A.; Zafar, K.; Baig, A.R. Fog-Centric IoT Based Framework for Healthcare Monitoring, Management and Early Warning System. IEEE Access 2021, 9, 74168–74179. [Google Scholar] [CrossRef]
- Escobedo, P.; Bhattacharjee, M.; Nikbakhtnasrabadi, F.; Dahiya, R. Smart Bandage with Wireless Strain and Temperature Sensors and Batteryless NFC Tag. IEEE Internet Things J. 2021, 8, 5093–5100. [Google Scholar] [CrossRef]
- Liu, Y.; Wang, H.; Zhao, W.; Zhang, M.; Qin, H.; Xie, Y.F. Stretchable Sensors for Wearable Health Monitoring: Sensing Mechanisms, Materials, Fabrication Strategies and Features. Sensors 2018, 18, 645. [Google Scholar] [CrossRef] [Green Version]
- Wang, X.; Liu, Z.; Zhang, T. Flexible Sensing Electronics for Wearable/Attachable Health Monitoring. Small 2017, 13, 1602790. [Google Scholar] [CrossRef] [PubMed]
- Alibakhshikenari, M.; Virdee, B.S.; Limiti, E. Wideband Planar Array Antenna Based on SCRLH-TL for Airborne Synthetic Aperture Radar Application. J. Electromagn. Waves Appl. 2018, 32, 1586–1599. [Google Scholar] [CrossRef]
- Alibakhshikenari, M.; Virdee, B.S.; Ali, A.; Limiti, E. Extended Aperture Miniature Antenna Based on CRLH Metamaterials for Wireless Communication Systems Operating over UHF to C-band. Radio Sci. 2018, 53, 154–165. [Google Scholar] [CrossRef]
- Alibakhshikenari, M. Printed Planar Patch Antennas Based on Metamaterial. Int. J. Electron. Lett. 2013, 2, 37–42. [Google Scholar] [CrossRef]
- Castillejo, P.; Martinez, J.; Rodriguez-Molina, J.; Cuerva, A. Integration of Wearable Devices in a Wireless Sensor Network for an E-Health Application. IEEE Wirel. Commun. 2013, 20, 38–49. [Google Scholar] [CrossRef] [Green Version]
- Dimitrov, D.V. Medical Internet of Things and Big Data in Healthcare. Healthc. Inform. Res. 2016, 22, 156–163. [Google Scholar] [CrossRef]
- Firouzi, F.; Rahmani, A.M.; Mankodiya, K.; Badaroglu, M.; Merrett, G.V.; Wong, P.; Farahani, B. Internet-of-Things and Big Bata for Smarter Healthcare: From Device to Architecture, Applications and Analytics. Future Gener. Comput. Syst. 2018, 78, 583–586. [Google Scholar] [CrossRef] [Green Version]
- Haq, A.U.; Li, J.P.; Khan, J.; Memon, M.H.; Nazir, S.; Ahmad, S.; Khan, G.A.; Ali, A. Intelligent Machine Learning Approach for Effective Recognition of Diabetes in E-Healthcare Using Clinical Data. Sensors 2020, 20, 2649. [Google Scholar] [CrossRef] [PubMed]
- Jiang, F.; Jiang, Y.; Zhi, H.; Dong, Y.; Li, H.; Ma, S.; Wang, Y.; Dong, Q.; Shen, H.; Wang, Y. Artificial Intelligence in Healthcare: Past, Present and Future. Stroke Vasc. Neurol. 2017, 2, 230–243. [Google Scholar] [CrossRef] [PubMed]
- Evangeline, C.S.; Ashmiya, L. Human Health Monitoring Using Wearable. Sens. Rev. 2019, 39, 364–376. [Google Scholar] [CrossRef]
- Rathy, G.A.; Sivasankar, P.; Tamara, Z.F. An efficient IoT based biomedical health monitoring and diagnosing system using myRIO. Telecommun. Comput. Electron. Control. 2020, 18, 3050–3057. [Google Scholar]
- User Guide. NI myRIO-1900. Available online: https://www.ni.com/pdf/manuals/376047c.pdf (accessed on 10 October 2021).
- Alibakhshikenari, M.; Babaeian, F.; Virdee, B.S.; Aïssa, S.; Azpilicueta, L.; See, C.H.; Althuwayb, A.A.; Huynen, I.; Abd-Alhameed, R.A.; Falcone, F.; et al. A Comprehensive Survey on Various Decoupling Mechanisms with Focus on Metamaterial and Metasurface Principles Applicable to SAR and MIMO Antenna Systems. IEEE Access 2020, 8, 192965–193004. [Google Scholar] [CrossRef]
- Alibakhshikenari, M.; Virdee, B.S.; Azpilicueta, L.; Naser-Moghadasi, M.; Akinsolu, M.O.; See, C.H.; Liu, B.; Abd-Alhameed, R.A.; Falcone, F.; Huynen, I.; et al. A Comprehensive Survey of Metamaterial Transmission-Line Based Antennas: Design, Challenges, and Applications. IEEE Access 2020, 8, 144778–144808. [Google Scholar] [CrossRef]
- Coogan, N.; Marra, A.; Lomonaco, E. Assessing Accurate BP Measurement: Size and Technique Matter! Nursing 2015, 45, 16–18. [Google Scholar] [CrossRef]
- Queyam, A.B.; Meena, R.K.; Pahuja, S.K.; Singh, D. An IoT Based Multi-Parameter Data Acquisition System for Efficient Bio-Telemonitoring of Pregnant Women at Home. In Proceedings of the 2018 8th International Conference on Cloud Computing, Data Science & Engineering, Noida, India, 11–12 January 2018; pp. 14–15. [Google Scholar] [CrossRef]
- Farooq, A.; Seyedmahmoudian, M.; Stojcevski, A. A Wearable Wireless Sensor System Using Machine Learning Classification to Detect Arrhythmia. IEEE Sens. J. 2021, 21, 11109–11116. [Google Scholar] [CrossRef]






| Physiological Sensor | Application | Data Rate | Response Time |
|---|---|---|---|
| BSP-BTA | blood pressure | 120 bytes/s | <3 s |
| EKG-BTA | ECG | 10 kilobytes/s | <1 s |
| max30102 | Pulse oximeter | 120 bytes/s | <3 s |
| PPG | Heart rate | 2 kilobytes/s | <3 s |
| Thermistor | Body temperature, breathing rate | 120 bytes/s | <3 s |
| Description | Unit Price | Number of Items | Total |
|---|---|---|---|
| PowerEdge T340 Tower Server | $769.00 | 2 | $1538.00 |
| Thin Client | $100 | 10 | $1000.90 |
| NI-myRIO-1900 | $890.00 | 100 | $89,000.00 |
| Battery | $47.81 | 100 | $4781.00 |
| 16 × 2 LCD display | $5.99 | 100 | $599.00 |
| MAX30100 Heart Rate Oximeter Sensor | $10.49 | 100 | $1049.00 |
| Wi-Fi Router | $49.99 | 5 | $249.95 |
| Blood Pressure Sensor | $149.00 | 100 | $14,900.00 |
| Surface Temperature Sensor | $32.00 | 200 | $6400.00 |
| EKG Sensor | $215.00 | 100 | $21,500.00 |
| RFID Reader | $29.95 | 100 | $2995.00 |
| Webcam | $36.95 | 100 | $3695.00 |
| EKG Electrode | $0.08 | 1000 | $80.00 |
| LabVIEW software | $4000.00 | 1 | $4000.00 |
| Total | $151,786.95 |
| Parameter | RMS Error | %RMS Error |
|---|---|---|
| Temperature | 0.0298 °F | 0.159% |
| Systolic pressure | 0.613 bpm | 0.05% |
| Diastolic pressure | 0.022 bpm | 0.029% |
| Breathing rate | 0.00136 breaths/min | 0.059% |
| Heart rate | 0.0015 beats/min | 0.002% |
| Spo2 | 0.002% | 0.076% |
| ECG | 0.0395 mV | 0.015% |
| Parameters Analyzed | Reference | Platform Used | Technique Used | Communication | Maximum RMS Error | Power Consumption | Remarks |
|---|---|---|---|---|---|---|---|
| Heart rate, Bod temperature, Fall detection, SpO2 | [19] | Data acquisition card | Biomedical sensors measure the parameters and view in LabVIEW | Wi-Fi, Serial | NA | NA | Limited parameters and poor visual presentation. |
| Heart rate, Blood pressure, Body temperature | [20] | NI-myRIO, ESP 8266 | Biomedical sensors measure the parameters and view in LabVIEW and LCD | Wi-Fi | NA | NA | ESP 8266 module has a compatible issue due to a single Analog port. |
| Respiration rate, Heart rate, Body temperature | [25] | NI-myRIO | Biomedical sensors measure the parameters and view in LabVIEW and android application | Wi-Fi | NA | NA | Limited to pregnant women. Limited visual representation. |
| ECG | [26] | NI-myRIO | Machine Learning | Wires Serial port | NA | NA | Only for ECG |
| Heart Rate, Blood pressure, ECG, Body temperature, SpO2, live video | Proposed system | NI-myRIO | Biomedical sensors measure the parameters and view in LabVIEW | Wi-Fi, Ethernet. | 0.159% | 1 watt/h |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Swain, K.; Cherukuri, M.; Mishra, S.K.; Appasani, B.; Patnaik, S.; Bizon, N. LI-Care: A LabVIEW and IoT Based eHealth Monitoring System. Electronics 2021, 10, 3137. https://doi.org/10.3390/electronics10243137
Swain K, Cherukuri M, Mishra SK, Appasani B, Patnaik S, Bizon N. LI-Care: A LabVIEW and IoT Based eHealth Monitoring System. Electronics. 2021; 10(24):3137. https://doi.org/10.3390/electronics10243137
Chicago/Turabian StyleSwain, Kunjabihari, Murthy Cherukuri, Sunil Kumar Mishra, Bhargav Appasani, Suprava Patnaik, and Nicu Bizon. 2021. "LI-Care: A LabVIEW and IoT Based eHealth Monitoring System" Electronics 10, no. 24: 3137. https://doi.org/10.3390/electronics10243137
APA StyleSwain, K., Cherukuri, M., Mishra, S. K., Appasani, B., Patnaik, S., & Bizon, N. (2021). LI-Care: A LabVIEW and IoT Based eHealth Monitoring System. Electronics, 10(24), 3137. https://doi.org/10.3390/electronics10243137








