Preoperative Virtual Reality Surgical Rehearsal of Renal Access during Percutaneous Nephrolithotomy: A Pilot Study
Abstract
:1. Introduction
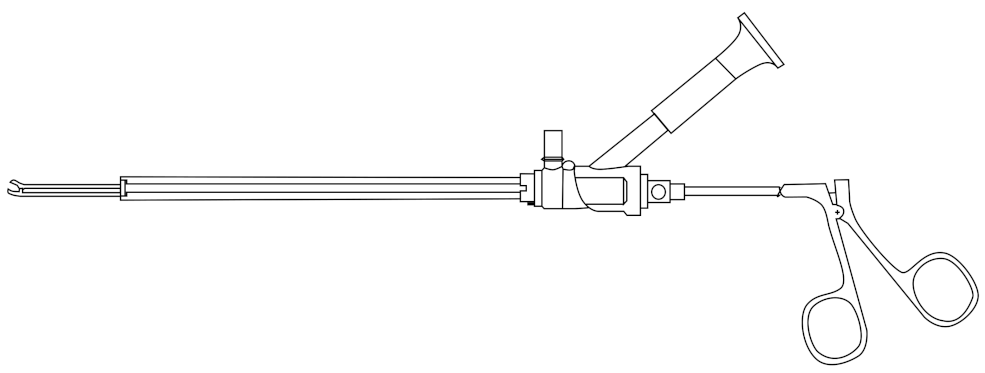
2. Marion K181 PCNL Simulator
Preliminary Testing of Simulator
3. Generating 3D Model Patient CT Scans
3.1. Method
3.2. Haptic Feedback Based on 3D Models
4. Results from Surgical Rehearsal
4.1. Experimental Procedure
4.2. Results
4.3. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Appendix A. Surgical Rehearsal Questionnaires and Results
| Questionnaire Part 1: User Demographics | ||
|---|---|---|
| 1. | How many PCNL access procedures have you performed in the last year | |
| with a C-arm? | 44 | |
| 2. | Have you experienced any intraoperative errors during PCNL procedures? | Yes |
| 3. | Was there error due to: | |
| Answer: Technical error (i.e., excessive force, tissue injury, etc.) | ||
| Questionnaire Part 2: Face Validation | ||
| How would you rate the virtual reality PCNL simulator with respect to: | ||
| 1. | Visual realism | 4/5 |
| 2. | Tactile feedback | 4/5 |
| 3. | Movement and instruments | 4/5 |
| 4. | Anatomical realism | 4/5 |
| 5. | How stable were the graphics and your sense of self inside the simulator? | 5/5 |
| 6. | Describe your experience/comment on any areas for improvement in realistic | |
| representation of the operating environment: | ||
| Answer: Graphics were very good. Graphics sometimes jumpy. | ||
| Questionnaire Part 3: Construct Validation | ||
| 1. | Were you able to interpret the shape and texture of the skin and kidney | |
| using the needle tool? | Yes | |
| 2. | Do you feel the tactile information was amplified in the simulation? | No |
| 3. | If applicable, did motion and force feedback influence your decision? | No |
| Questionnaire Part 4: Content Validation | ||
| 1. | Do you feel the tasks performed in the simulator reflected the real | |
| surgical procedure? | Yes | |
| 2. | Please provide comments of the overall simulation experience (VR) | |
| in content accuracy? | ||
| Answer: Location of rib impacting access was excellent. | ||
| Help me for real life access. | ||
| Overall Rating | ||
| 1. | Rate the experience training with the Marion Surgical PCNL simulator: | 4/5 |
| Questionnaire Part 1: Face Validation | ||
|---|---|---|
| How would you rate the virtual reality PCNL simulator with respect to: | ||
| 1. | Visual realism | 4/5 |
| 2. | Tactile feedback | 4/5 |
| 3. | Movement and instruments | 4/5 |
| 4. | Anatomical realism | 5/5 |
| 6. | How stable were the graphics and your sense of self inside the simulator? | 4/5 |
| 7. | Describe your experience/ comment on any areas for improvement in realistic | |
| representation of the operating environment: | ||
| Answer: The virtual rendering are an excellent simulation of actual | ||
| patient anatomy. Tactile feedback can always be improved | ||
| Questionnaire Part 2: Construct Validation | ||
| 1. | Were you able to interpret the shape and texture of the skin and kidney | |
| using the needle tool? | Yes | |
| 2. | Do you feel the tactile information was amplified in the simulation? | Yes |
| 3. | If applicable, did motion and force feedback influence your decision? | Yes |
| Questionnaire Part 3: Content Validation | ||
| 1. | Visual simulation is the most important factor in learning surgical motor skills: | 4/5 |
| 2. | Do you feel the tasks performed in the simulator reflected real | |
| surgical skills? | Yes | |
| 3. | You see the value in VR PNCL tool as a useful tool in Training PCNL skills: | 4/5 |
| 4. | You think this VR PCNL simulator is useful for Assessing/Testing PCNL skills: | 4/5 |
| 5. | What is the most difficult skill to learn during a full PCNL procedure? | |
| Answer: Actual renal access | ||
| 6. | Please provide comments of the overall simulation experience (VR) | |
| in having an educational role? | ||
| Answer: Being able to practice targeting of calyx/stone with needle | ||
| is valuable. Also without having excess radiation exposure | ||
| or harm to patient. | ||
| 7. | Please provide comments of the overall simulation experience (VR) | |
| in content accuracy? | ||
| Answer: It was help to rehearse access. Became aware of rib in the | ||
| way of calyx of interest. | ||
| Overall Rating | ||
| 1. | Rate the experience training with the Marion Surgical PCNL simulator: | 5/5 |
| Rehearsal | ||
|---|---|---|
| Did the rehearsal help you determine: | ||
| 1. | The location of the stone (with regard to the bulk of the stone)? | 9/10 |
| (a) Specifically, where is the bulk of the stone? | Lower Pole | |
| 2. | The size of the stone? | 10/10 |
| (a) What is the size of the largest stone in three dimensions? | 2 cm | |
| (b) What is the total volume of the largest stone? | 2 cm | |
| 3. | The shape and orientation of each stone-bearing calix? | 10/10 |
| 4. | The optimal calix of entry to perform the PCNL? | |
| (a) Into which calix (upper, mid, lower, and anterior or post- | ||
| erior) are you planning to place the nephrostomy track? | Lower Posterior | |
| 5. | How easily do you think you can navigate this patient’s pelvic | |
| caliceal system from your planned approach with a rigid | ||
| nephroscope? | 9/10 | |
| When you performed the actual surgery on this patient: | ||
| 6. | How close was the location of the stone relative to the rehearsal | |
| (specifically, with regard to the bulk of the stone)? | 9/10 | |
| (a) Specifically, where is the bulk of the stone: | Lower Posterior | |
| 7. | The size of the stone? | 10/10 |
| (a) What is the size of the largest stone in three dimensions? | 2 cm | |
| (b) What is the total volume of the largest stone? | 2 cm | |
| 8. | The shape and orientation of each stone-bearing calix? | 9/10 |
| 9. | The optimal calix of entry to perform the PCNL? | 9/10 |
| (a) Into which calix (upper, mid, lower, and anterior | ||
| or posterior) did you place the nephrostomy track? | Lower Posterior | |
| 10. | How easily were you able to navigate to this patient’s pelvic | |
| caliceal system from your planned rehearsal approach with a | ||
| rigid nephroscope? | 9/10 | |
References
- Aydın, A.; Al-Jabir, A.; Smith, B.; Ahmed, K. Training in Percutaneous Nephrolithotomy. In Percutaneous Nephrolithotomy; Zeng, G., Sarica, K., Eds.; Springer: Singapore, 2020; pp. 195–202. [Google Scholar] [CrossRef]
- Khan, S.R.; Pearle, M.S.; Robertson, W.G.; Gambaro, G.; Canales, B.K.; Doizi, S.; Traxer, O.; Tiselius, H.G. Kidney stones. Nat. Rev. Dis. Prim. 2016, 2, 1–23. [Google Scholar]
- Bird, V.G.; Fallon, B.; Winfield, H.N. Practice patterns in the treatment of large renal stones. J. Endourol. 2003, 17, 355–363. [Google Scholar] [CrossRef] [PubMed]
- Ng, C.F. Training in percutaneous nephrolithotomy: The learning curve and options. Arab J. Urol. 2014, 12, 54–57. [Google Scholar] [CrossRef] [PubMed]
- Bushey, C. Cadaver supply: The last industry to face big changes. CRAIN’s Chic. Bus. 2016, 15. [Google Scholar]
- Mishra, S.; Kurien, A.; Ganpule, A.; Muthu, V.; Sabnis, R.; Desai, M. Percutaneous renal access training: Content validation comparison between a live porcine and a virtual reality (VR) simulation model. BJU Int. 2010, 106, 1753–1756. [Google Scholar] [CrossRef]
- Farcas, M.; Reynolds, L.F.; Lee, J.Y. Simulation-Based Percutaneous Renal Access Training: Evaluating a Novel 3D Immersive Virtual Reality Platform. J. Endourol. 2021, 35, 695–699. [Google Scholar] [CrossRef]
- Pottle, J. Virtual reality and the transformation of medical education. Future Healthc. J. 2019, 6, 181. [Google Scholar] [CrossRef] [Green Version]
- Sommer, G.M.; Broschewitz, J.; Huppert, S.; Sommer, C.G.; Jahn, N.; Jansen-Winkeln, B.; Gockel, I.; Hau, H.M. The role of virtual reality simulation in surgical training in the light of COVID-19 pandemic: Visual spatial ability as a predictor for improved surgical performance: A randomized trial. Medicine 2021, 100, e27844. [Google Scholar] [CrossRef]
- Chiang, P.; Zheng, J.; Yu, Y.; Mak, K.H.; Chui, C.K.; Cai, Y. A VR simulator for intracardiac intervention. IEEE Comput. Graph. Appl. 2012, 33, 44–57. [Google Scholar] [CrossRef]
- Staropoli, P.C.; Gregori, N.Z.; Junk, A.K.; Galor, A.; Goldhardt, R.; Goldhagen, B.E.; Shi, W.; Feuer, W. Surgical simulation training reduces intraoperative cataract surgery complications among residents. Simul. Healthc. J. Soc. Simul. Healthc. 2018, 13, 11. [Google Scholar] [CrossRef]
- Badash, I.; Burtt, K.; Solorzano, C.A.; Carey, J.N. Innovations in surgery simulation: A review of past, current and future techniques. Ann. Transl. Med. 2016, 4, 453. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wilz, O.; Sainsbury, B.; Rossa, C. Constrained haptic-guided shared control for collaborative human–robot percutaneous nephrolithotomy training. Mechatronics 2021, 75, 102528. [Google Scholar] [CrossRef]
- Arnold, J.; Cashin, M.; Olutoye, O.O. Simulation-based clinical rehearsals as a method for improving patient safety. JAMA Surg. 2018, 153, 1143–1144. [Google Scholar] [CrossRef] [PubMed]
- Yiasemidou, M.; Glassman, D.; Jayne, D.; Miskovic, D. Is patient-specific pre-operative preparation feasible in a clinical environment? A systematic review and meta-analysis. Comput. Assist. Surg. 2018, 23, 57–68. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parkhomenko, E.; O’Leary, M.; Safiullah, S.; Walia, S.; Owyong, M.; Lin, C.; James, R.; Okhunov, Z.; Patel, R.M.; Kaler, K.S.; et al. Pilot assessment of immersive virtual reality renal models as an educational and preoperative planning tool for percutaneous nephrolithotomy. J. Endourol. 2019, 33, 283–288. [Google Scholar] [CrossRef]
- Willaert, W.I.; Aggarwal, R.; Van Herzeele, I.; Cheshire, N.J.; Vermassen, F.E. Recent advancements in medical simulation: Patient-specific virtual reality simulation. World J. Surg. 2012, 36, 1703–1712. [Google Scholar] [CrossRef]
- Won, T.B.; Hwang, P.; Lim, J.H.; Cho, S.W.; Paek, S.H.; Losorelli, S.; Vaisbuch, Y.; Chan, S.; Salisbury, K.; Blevins, N.H. Early Experience with a Patient-Specific Virtual Surgical Simulation for Rehearsal of Endoscopic Skull-Base Surgery; Wiley Online Library: Hoboken, NJ, USA, 2018; Volume 8, pp. 54–63. [Google Scholar]
- Jean, W.C. Virtual reality surgical rehearsal and 2-dimensional operative video of a paramedian supracerebellar infratentorial approach endoscopic resection of pineocytoma: 2-dimensional operative video. Oper. Neurosurg. 2021, 20, E51–E52. [Google Scholar] [CrossRef]
- Qiu, K.; Haghiashtiani, G.; McAlpine, M.C. 3D printed organ models for surgical applications. Annu. Rev. Anal. Chem. 2018, 11, 287–306. [Google Scholar] [CrossRef]
- Guerrera, F.; Nicosia, S.; Costardi, L.; Lyberis, P.; Femia, F.; Filosso, P.L.; Arezzo, A.; Ruffini, E. Proctor-guided virtual reality–enhanced three-dimensional video-assisted thoracic surgery: An excellent tutoring model for lung segmentectomy. Tumori J. 2021, 107, NP1–NP4. [Google Scholar] [CrossRef]
- Sainsbury, B.; Łącki, M.; Shahait, M.; Goldenberg, M.; Baghdadi, A.; Cavuoto, L.; Ren, J.; Green, M.; Lee, J.; Averch, T.D.; et al. Evaluation of a virtual reality percutaneous nephrolithotomy (PCNL) surgical simulator. Front. Robot. AI 2020, 6, 145. [Google Scholar] [CrossRef] [Green Version]
- Wu, C.O.; Sunderland, K.; Filippov, M.; Sainsbury, B.; Fichtinger, G.; Ungi, T. Workflow for creation and evaluation of virtual nephrolithotomy training models. In Proceedings of the Medical Imaging 2020: Image-Guided Procedures, Robotic Interventions, and Modeling, Houston, TX, USA, 15–20 February 2020; International Society for Optics and Photonics: Bellingham, WA, USA, 2020; Volume 11315, p. 1131524. [Google Scholar]
- Resad, S.; Parkhomenko, E.; Wang, D.S.; Wason, S.E. The Utility and Value of Immersive Virtual Reality Simulation for Percutaneous Nephrostomy Tract Access and Surgical Training; Boston University School of Medicine: Boston, MA, USA, 2019. [Google Scholar]
- Montemurro, N.; Condino, S.; Cattari, N.; D’Amato, R.; Ferrari, V.; Cutolo, F. Augmented reality-assisted craniotomy for parasagittal and convexity en plaque meningiomas and custom-made cranio-plasty: A preliminary laboratory report. Int. J. Environ. Res. Public Health 2021, 18, 9955. [Google Scholar] [CrossRef] [PubMed]
- Rais-Bahrami, S.; Friedlander, J.I.; Duty, B.D.; Okeke, Z.; Smith, A.D. Difficulties with access in percutaneous renal surgery. Ther. Adv. Urol. 2011, 3, 59–68. [Google Scholar] [CrossRef] [PubMed] [Green Version]




Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sainsbury, B.; Wilz, O.; Ren, J.; Green, M.; Fergie, M.; Rossa, C. Preoperative Virtual Reality Surgical Rehearsal of Renal Access during Percutaneous Nephrolithotomy: A Pilot Study. Electronics 2022, 11, 1562. https://doi.org/10.3390/electronics11101562
Sainsbury B, Wilz O, Ren J, Green M, Fergie M, Rossa C. Preoperative Virtual Reality Surgical Rehearsal of Renal Access during Percutaneous Nephrolithotomy: A Pilot Study. Electronics. 2022; 11(10):1562. https://doi.org/10.3390/electronics11101562
Chicago/Turabian StyleSainsbury, Ben, Olivia Wilz, Jing Ren, Mark Green, Martin Fergie, and Carlos Rossa. 2022. "Preoperative Virtual Reality Surgical Rehearsal of Renal Access during Percutaneous Nephrolithotomy: A Pilot Study" Electronics 11, no. 10: 1562. https://doi.org/10.3390/electronics11101562
APA StyleSainsbury, B., Wilz, O., Ren, J., Green, M., Fergie, M., & Rossa, C. (2022). Preoperative Virtual Reality Surgical Rehearsal of Renal Access during Percutaneous Nephrolithotomy: A Pilot Study. Electronics, 11(10), 1562. https://doi.org/10.3390/electronics11101562






