Abstract
Stress is a concerning issue in today’s world. Stress in pregnancy harms both the development of children and the health of pregnant women. As a result, assessing the stress levels of working pregnant women is crucial to aid them in developing and growing professionally and personally. In the past, many machine-learning (ML) and deep-learning (DL) algorithms have been made to predict the stress of women. It does, however, have some problems, such as a more complicated design, a high chance of misclassification, a high chance of making mistakes, and less efficiency. With these considerations in mind, our article will use a deep-learning model known as the deep recurrent neural network (DRNN) to predict the stress levels of working pregnant women. Dataset preparation, feature extraction, optimal feature selection, and classification with DRNNs are all included in this framework. Duplicate attributes are removed, and missing values are filled in during the preprocessing of the dataset.
1. Introduction
The term “stress” was coined by Hans Selye. It is “the body’s nonspecific response to any demand” [1]. A study was carried out on 14,600 employees, HR leaders, managers, and C-level executives from 13 nations, including 1100 working professionals from India. About 91% of the working professionals from India who answered the survey said they were very affected by it, which is more than the average of 80% around the world [2]. Working women seem to have a hard time at work. A study showed that work–family stress affects 28% of men and 53% of women. It also makes it hard for them to focus on the job [3]. Research shows that most women around the world are stressed out and overworked and rarely have time to relax. Even more than women in developed countries, women in developing countries feel stressed. In India, it is hard for 87% of women to find time for work and family [4]. The International Labor Organization (ILO) says that about 2.3 million women and men die every year from work-related accidents or diseases. That is more than 6000 deaths every single day. Every year, there are about 340 million work-related accidents as well as 160 million people who get sick because of their job. The ILO releases these stats from time to time, and the updates show that accidents and health problems are getting worse [5].
The World Health Organization (WHO) estimates that 14% of the worldwide burden of disease among both men and women is caused by neurological, psychiatric, and substance-use disorders [6]. Women are more deeply affected by family responsibilities and tend to report higher stress levels than men [7]. The lifestyle of women during pregnancy has long-term effects on their overall health, and pregnancy is identified as a sensitive period of increased risk for psychosocial symptoms and poor oral health [8]. Pregnancy-related stress is quite common among women [9], and it might have a negative impact during delivery such as a low birth rate [10,11].
In the literature, multiple studies found that between 10% and 15% [12,13,14,15] of pregnant women in wealthy nations experience psychosocial symptoms, while 33% [16] of pregnant women in developing nations experience these symptoms. There is a link between psychological symptoms and issues with oral health [17]. Pregnancy-related psychological symptoms do exist, are common, and are shown to have a variety of harmful impacts on both the health of the pregnant woman and her unborn child [18,19,20]. According to a study, dental disorders are most likely to affect pregnant women who negatively experience psychological symptoms [21]. Up to 30% of pregnant women experience periodontal disease [22], and two more studies found a link between stress and the hormonal changes brought on by periodontal disease [22,23]. Deep 1D convolutional and multilayer perceptron neural networks were created. Both deep neural networks fared better than typical machine-learning algorithms. Deep neural networks (DNNs) can develop noninvasive, robust algorithms for emotion recognition and emotion classification, enhancing the quality of life [24]. A study of 3569 women from five nations (1939 pregnant and 1630 postpartum) was performed. ML algorithms were evaluated for their ability to predict depression and anxiety symptoms.
The random forest (RF) and gradient boosting (GB) models provide better results in comparison with other ML algorithms evaluated, with accuracy scores of 83.3% and 83.2% for depression, and 82.9% and 81.3% for anxiety, respectively. When compared with other techniques, deep-learning-based classification models [25] give effective and precise performance results for each difficult challenge. Convolutional neural networks (CNNs), DNNs, and deep belief networks (DBNs) are all covered, as well as long short-term memory (LSTM). Deep-learning-based categorization methods are better suited to accurately predict the attitude and stress levels of pregnant workers. They provide precise prediction results, improved performance levels, efficiency, and shorter turnaround times. The main contributions of the study are as follows:
- A DRNN-based deep-learning model is utilized to accurately determine whether working pregnant women are stressed or not.
- The given dataset is normalized by deleting the unnecessary set of attributes and filling in the missing values, and then the optimal number of features was extracted and selected from the normalized dataset for training the data model to enhance the classifier’s prediction performance.
- Several assessment metrics, such as precision, accuracy, recall, sensitivity, specificity, F1-score, and error rate, have been validated to measure the performance of the proposed model.
2. Overview of Pregnant Women Stress and CNN-LSTM
Physical, mental, or emotional stress at work is harmful to the developing baby. Miscarriage, early labor, premature birth, a low birth weight, and hypertension are all more likely when a pregnant woman is under a lot of stress. The risk of problems during pregnancy increases in proportion to the level of stress experienced [26]. Women who have had trouble having healthy pregnancies in the past should be encouraged to take more time off work to prepare for motherhood. Pregnant women who are exposed to high levels of stress at work should be constantly monitored for signs of preterm labor or delayed fetal growth, and their stress levels at work should be reduced or eliminated if necessary. Teratogens, including organic solvents, heavy metals, or pesticides, can be present in the environments where pregnant women work. Women frequently work outside their home in the United States, including mothers and expectant women.
In 2015, 70% over all women with children under the age of 18 worked [27]; 82% were nulliparous women who continued to work up to 1 month before the due dates, whereas 56% of pregnant women worked full time during their pregnancies. Six months after giving delivery, the majority of women (73%) resume their jobs [28]. The World Health Organization (WHO) indicated that over 10% of pregnant women as well as 13% of postpartum women have a mental health disorder [29] before the COVID-19 pandemic. As the perinatal period is a time of great change, anxiety is a prevalent problem among new mothers [30,31]. Pregnant mothers and their unborn children are particularly vulnerable to the harmful effects of anxiety disorders. Preterm birth, decreased bonding between mother and child, and difficulties in cognitive and emotional development in babies are all linked to antenatal anxiety, and these effects can last far into childhood [32].
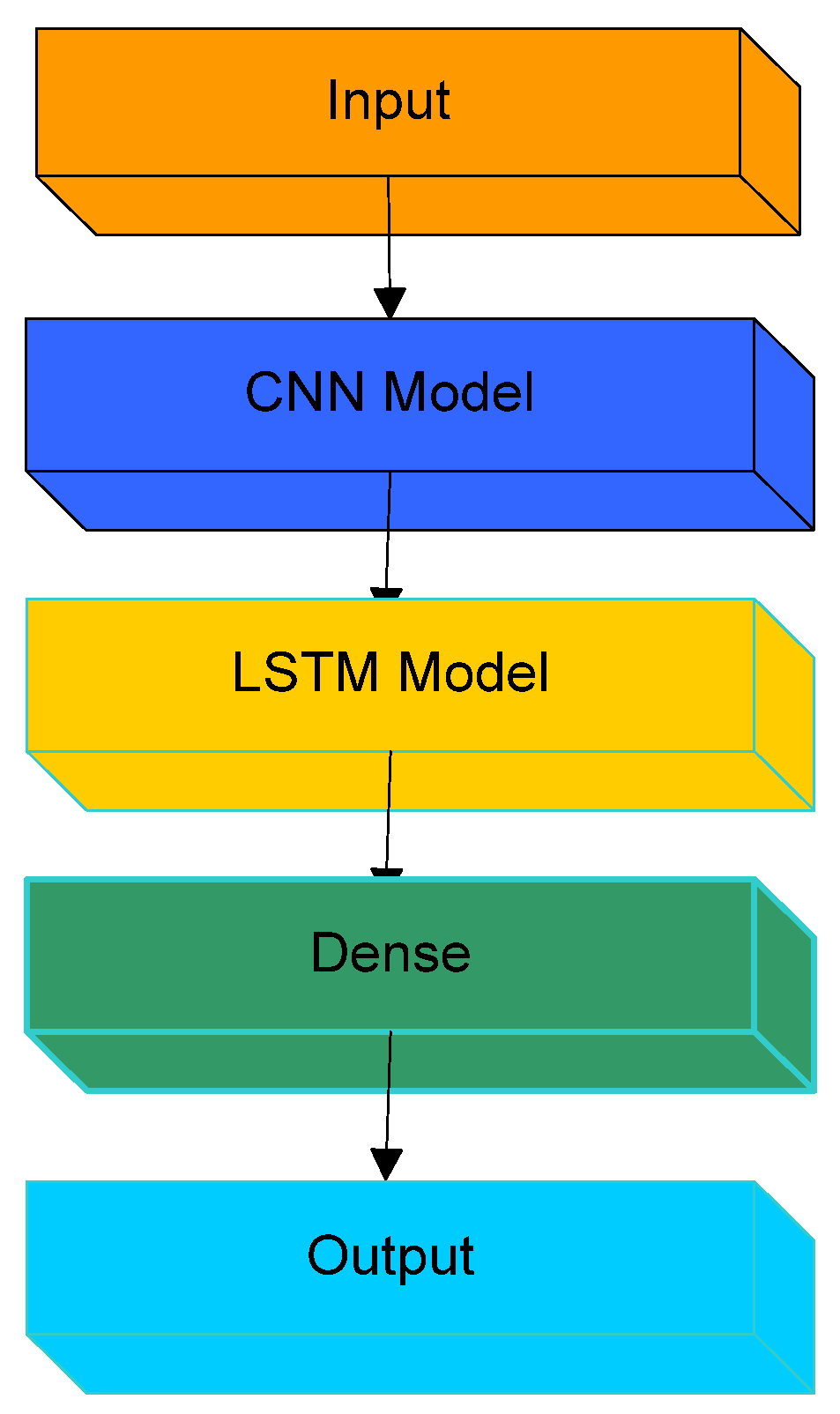
Long-term stress can induce heart disease and high blood pressure. Stress during pregnancy might lead to premature or underweight babies. Premature or tiny babies are at risk for health issues. CNN LSTM (Figure 1), which stands for CNN long short-term memory network, is an LSTM architecture that was expressly developed to solve sequence prediction problems including spatial inputs, such as photos or videos.
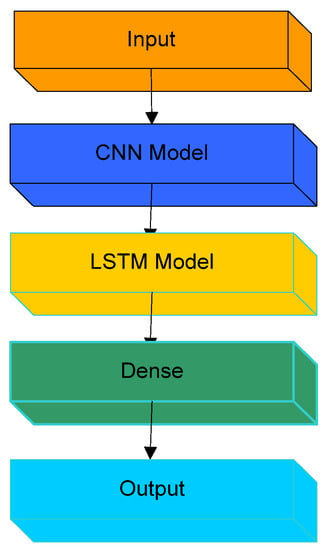
Figure 1.
CNN LSTM structure.
Deep LSTM is a recurrent neural network and is a type of long short-term memory. The output from the previous phase is sent into the current step of an RNN as input. Hochreiter and Schmidhuber created the LSTM. It addressed the issue of long-term RNN dependency, in which the RNN can predict words from current data but cannot predict words held in long-term memory. The RNN’s performance becomes less effective as the gap length increases. By default, LSTM can save the data for a very long time. It is utilized for time-series data processing, forecasting, and classification.
3. Associate Work
Various ML and DL techniques for forecasting working pregnant women’s stress levels are summarized in this section. As a result, it takes into account the advantages and disadvantages of various techniques, as well as the way they operate and behave. Multitask learning was proposed by [33] to accurately predict mood and stress components. Individual needs were analyzed using hierarchical Bayesian modeling to make predictions about future emotions. The stochastic gradient descent (SGD) method, which forecasts label values based on cluster weights, was also utilized to find the most pertinent qualities from the input data. The study examined various mood-prediction machine-learning algorithms, including logistic regression (LR), multikernel learning (MKL), and support vector machine, (SVM). To examine the effectiveness of various techniques, this study estimated the ROC of each mood-prediction mechanism using the mood-prediction dataset. Among the advantages of this work were a higher performance rate and classification sampling design processes. It, nevertheless, has several drawbacks, such as a longer training period and lower classification accuracy [34].
Finite-element analysis was used to improve the deep-learning approach to forecasting stress in humans. These DNNs are effective in predicting stress components from supplied data, as stated in this paper. For forecasting mood, health, and stress levels, a multitask learning mechanism was designed. The domain adaptation (DA) technique was also used to improve the automatic prediction process. Gaussian progression (GP) was employed to study the nonlinear relationship. Accurate predictions can be made using the deep neural network (DNN) technique, according to this paper. As a result, the system’s overall performance is hampered by the rising complexity of the algorithm [35].
An effective stress management strategy was created for determining the degree of stress faced by female educators [36]. Experiencing stress while pregnant can have a lasting impact not only on the health of the mother and unborn child but also on the development of the progeny. The authors of [37] aimed to use machine-learning methodologies to develop solutions for monitoring real-time stress levels. SVM, LDA, NB, KNN, and decision tree (DT) were among the techniques tested in the study. All of these strategies’ training and testing challenges have also been estimated based on their work stages and computations. Preprocessing, feature extraction, and classification are the three stages of this system [38].
It was discovered that mental stress during pregnancy is highly linked to depression and has a significant impact on pregnant women’s daily lives. A general regression neural network (GRNN) model was advocated for evaluating the individual stress component based on data clustering. The purpose of this study was to exactly calculate a person’s stress level by analyzing data and categorizing information. The stress level was determined using the baseline, task load, and recovery stages. The underlying fault in this paper was that it encountered considerable problems in task-handling procedures. [39] Five machine-learning (ML) algorithms were used in a 2020 study to predict anxiety, depression, and stress in people around the world using the Depression, Anxiety, and Stress Scale questionnaire (DASS 21). When it came to accurately forecasting psychological situations, the random forest classifier, a machine-learning system used for data classification, performed the best [40]. Psychosocial stress caused by a woman’s employment is an undetermined risk factor for pregnancy problems [41].
A new data-mining method for calculating a person’s stress level based on their actions was suggested. The multilayer perceptron (MLP) model was utilized in this system to aid in detecting the cause of depression [42]. The bibliometric analysis using Vosviewer was discussed, and we investigated why very little work is carried out to detect the stress of working pregnant women; also we focused upon the thrust areas of future work [43]. This work offers a technique for stress classification based on EEG signals obtained from a commercially available Interaxon Muse 4-channel headband device. Stress and nonstress participants’ EEG signals were recorded. LSTM 2 classified stress with 93.17% accuracy (with two LSTM layers). These results improved on EEG-based approaches [44].
The study aimed to show that several predictive models can be employed to give more accurate and fine-grained stress-tracking using the suggested solution’s physiological data. To do so, the authors used ML and DL models to solve regression challenges [45] and highlighted the promise of deep neural networks for the development of reliable, continuous, and noninvasive techniques for emotion classification and stress detection, with the ultimate goal of enhancing life quality. The accuracy of the model was 99.50%, which is the accuracy for both binary and three-level classifications. This study employed prediction models built with machine-learning approaches to investigate how the recent COVID-19 epidemic has affected prenatal mental health and well-being [46]. The authors presented a DNN-based stress prediction for human resource management in terms of involvement, training, development, education, work circumstances, and remuneration and rewards [47].
The literature review revealed that most of the work has been conducted using traditional techniques of stress prediction. Less research work has been performed to predict the stress of working pregnant women. However, current systems are limited by fundamental concerns such as increased algorithm complexity, increased training time, and high misclassification rates. As a result, the purpose of this research was to develop an accurate deep-learning model for projecting working pregnant women’s stress levels.
4. Methodology
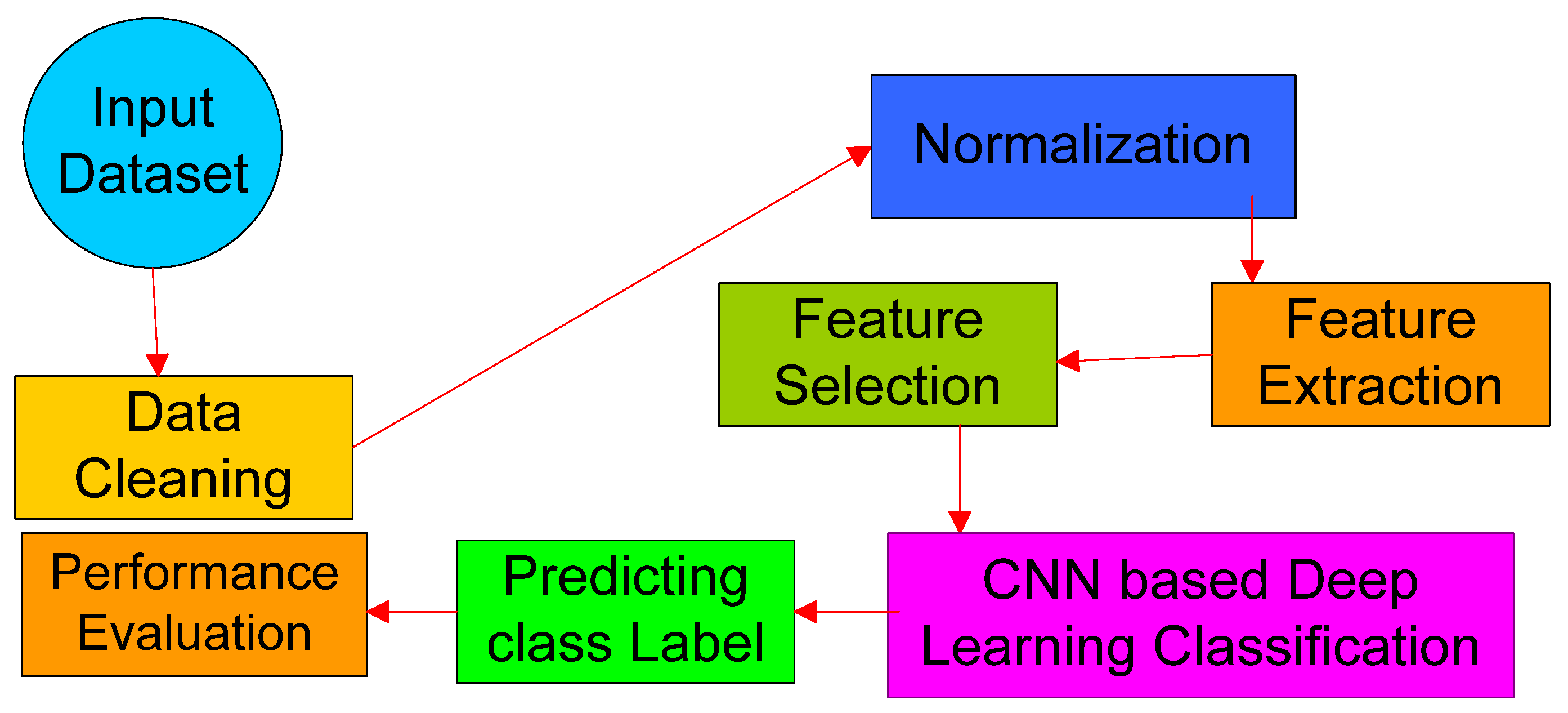
This section provides a comprehensive analysis of the proposed stress prediction system for employed pregnant women, complete with flow diagrams and computational examples. The objective of this study was to use an advanced deep-learning classification technique to increase the precision and effectiveness of a stress prediction system. The suggested system’s entire flow is shown in Figure 2, which comprises steps such as feature extraction, feature selection, and classification, as well as data pretreatment. The dataset is normalized by adding the missing and inaccurate values after it has been loaded. A set of dependent and independent variables has been defined throughout this procedure to forecast the missing values. The most pertinent features are then chosen from the set of features in the normalized dataset to increase the prediction accuracy. Finally, the stress level of working pregnant women is accurately predicted using a deep recurrent neural network (DRNN)-based DL model.
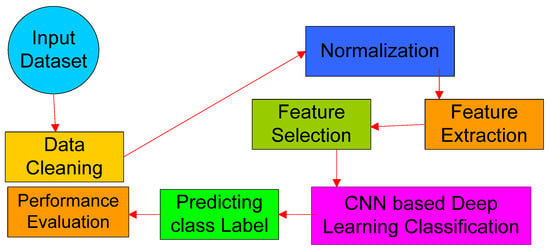
Figure 2.
Work flow.
4.1. Preprocessing of Data
The processing starts with the original working pregnant women dataset, which has some useless attribute information and missing values. This kind of data could make it harder to classify and takes longer to train. Therefore, the properties and fields of the dataset need to be normalized before it can be used. In this step, the original dataset was cleaned up and filtered to get rid of any data that were not needed. To obtain the normalized dataset, the missing values are filled in and the fields as a whole are filtered. The perceived stress scale (PSS) was made to find out what kinds of situations make working pregnant women stressed and how well they can deal with those situations. It can be figured out by looking at things such as how they feel and how stressed they are in common situations. This dataset can be used to extract features and categories because the data in the dataset influence how well the system as a whole works.
4.2. Features Extraction
In every prediction or classification system, feature extraction is a vital step in creating new features from the data’s original features. Learning outcomes are strongly dependent on working pregnant women’s qualities and performance; hence, this is an important step in classifying individuals. The normalized dataset was utilized to extract five features: average time, total activities, average idle time, keystrokes, and other activities (Algorithm 1).
| Algorithm 1 Extraction of Feature |
| 1: Input: dataset that has been normalized; 2: Output: A collection of features that have been extracted; 3: Step 1: for e = 1 to EID//EID—The number of working pregnant women who have their ID; 4: Calculate how long it will take them to complete their desired tasks; 5: End for; 6: Step 2: With their respective ID, estimate the unique activities of working pregnant women. 7: Step 3: For q = 1 to size 8: For w = 1 to size 9: For p = 1 to size 10: Calculate the average amount of time A T that each working pregnant woman needs to complete their tasks; 11: Calculate the total E T of all working pregnant women’s activities for completing their tasks; 12: Compute the idle time I_T of every working pregnant woman; 13: Calculate the average number of key strokes.〖Av〗_Ks; 14: Calculate each working pregnant women professional’s other activities, OA T, to complete the tasks; 15: The end for p; 16: The end for w; 17: The end for q; 18: Step 4: Extracted feature set Es = {AT,ST,IT,〖Av〗Ks,〖OA〗T |
4.3. Selection of Features
The process of choosing the features that are most optimal for correctly predicting the results of the classification is referred to as feature selection. In this case, the extracted feature set is used to choose the most pertinent properties, which assists in reducing the dimensionality of the feature set. The performance of the classifier may be hampered by the added characteristics during the training and testing phases. The alpha-investing method is used to choose the pertinent qualities in the best way possible to resolve this issue. The technique’s primary benefit is that it precisely identifies all plausible pairings of features, improving the suggested working pregnant women stress prediction system’s overall accuracy.
4.4. Classification Based on DRNN
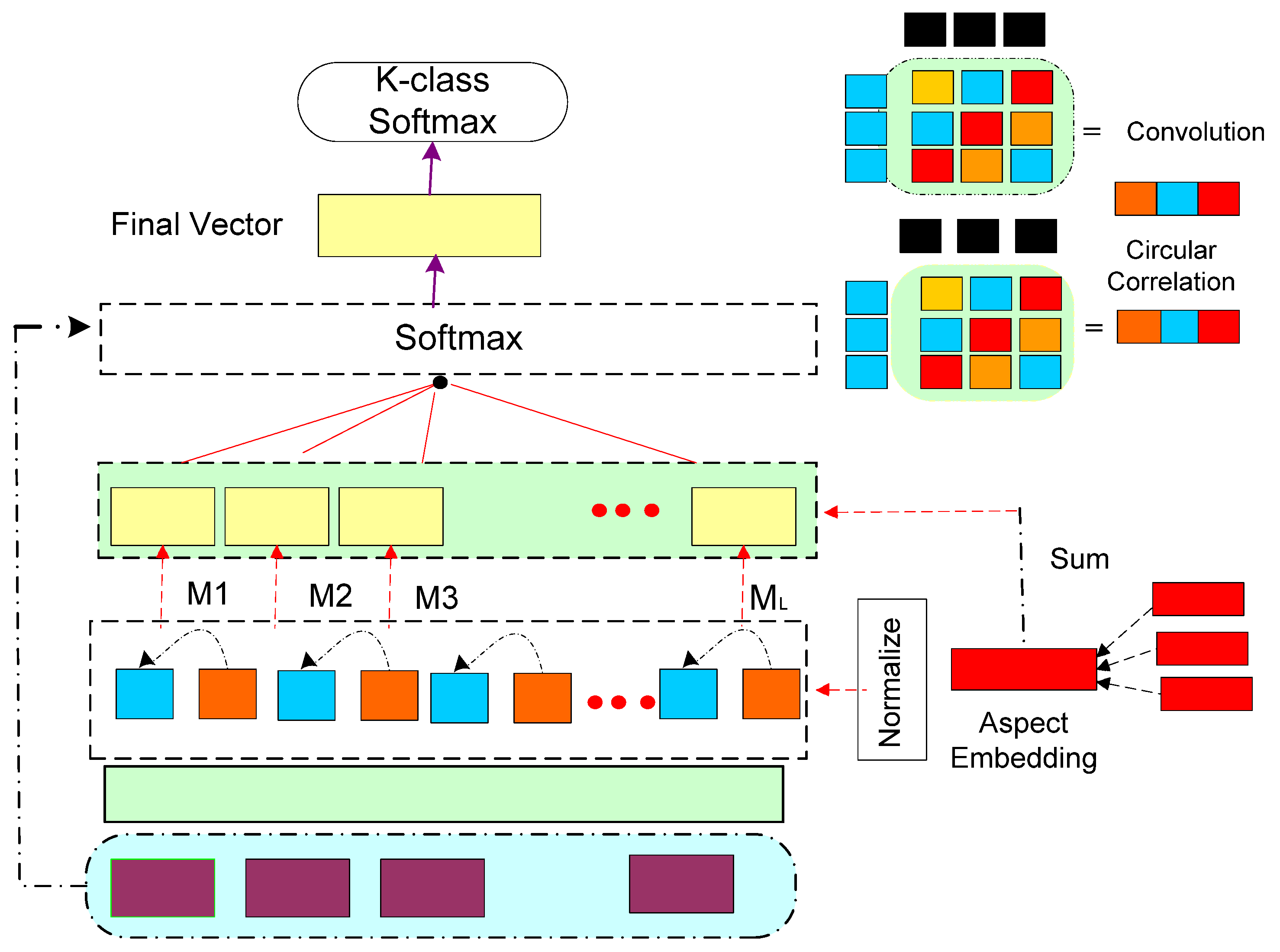
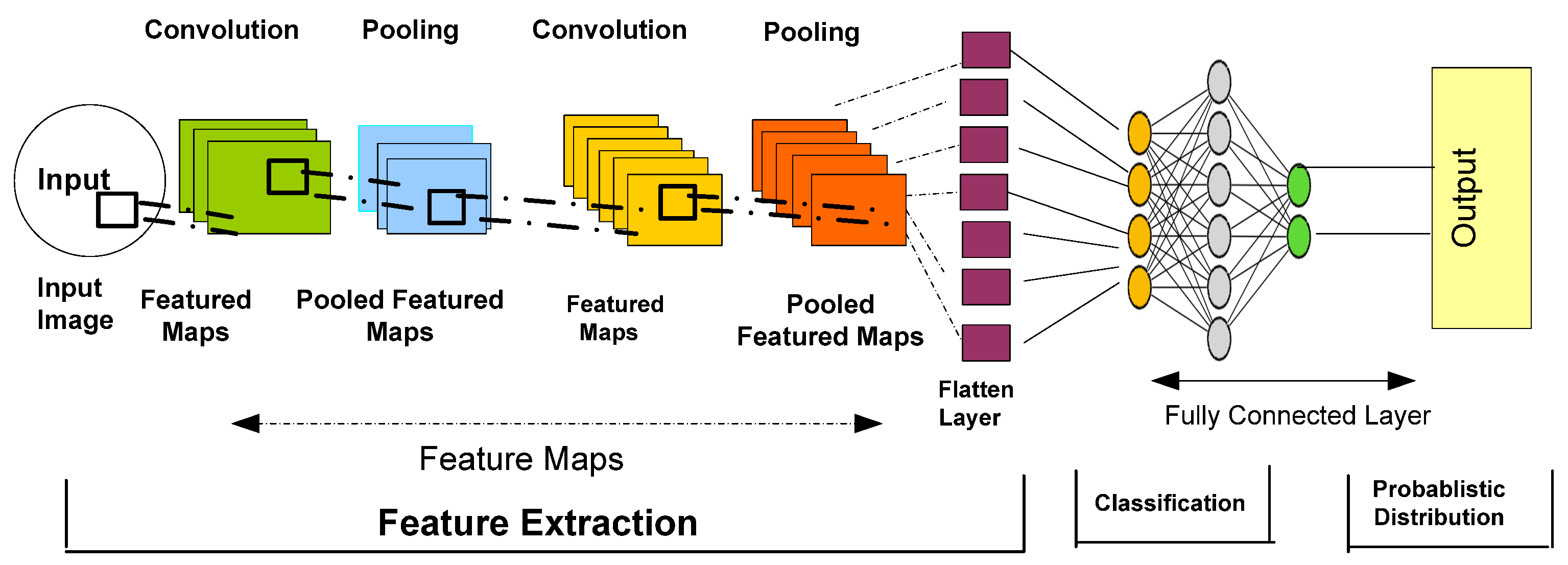
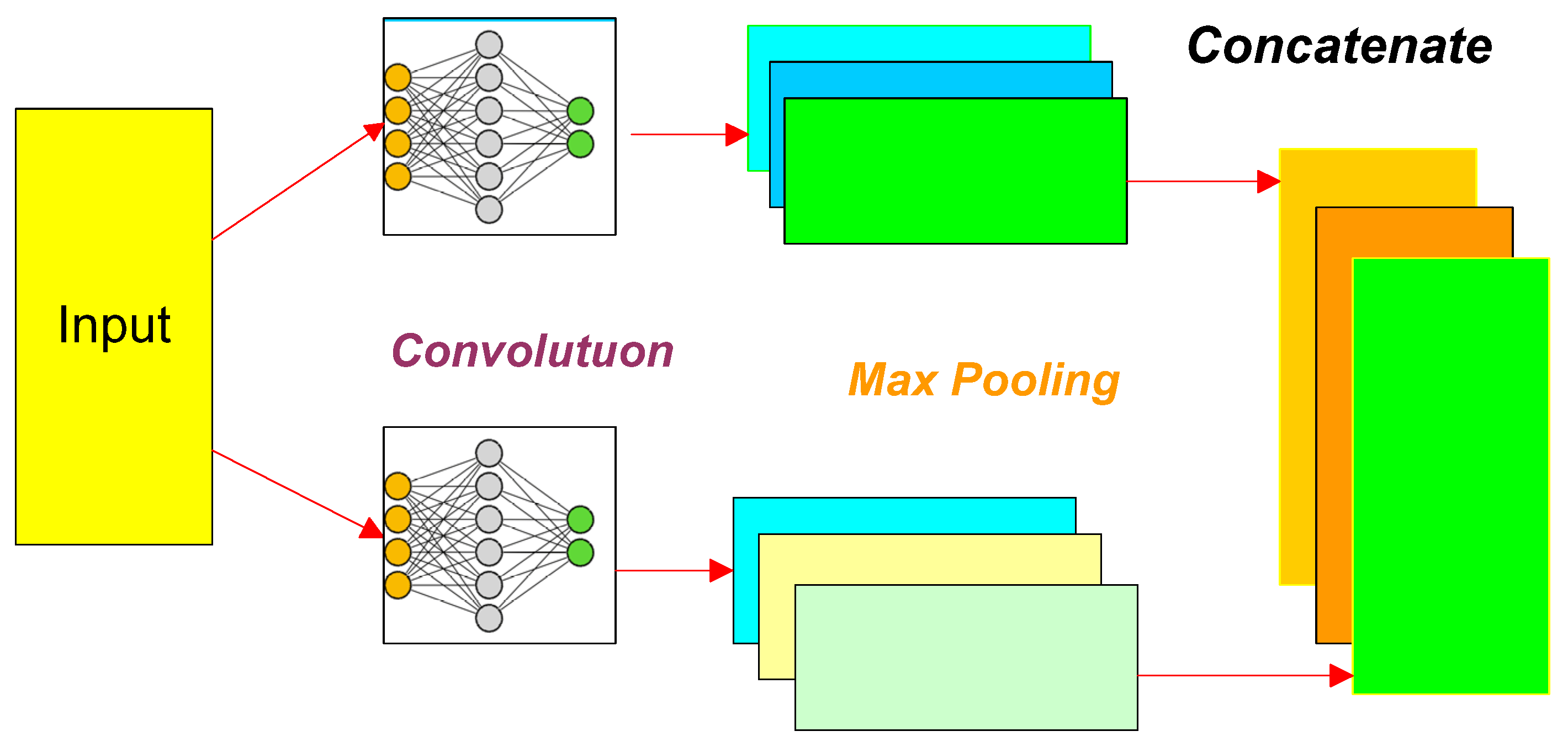
As an input to the processing, the best set of characteristics was found, and as an output, the predicted label was made. The DRNN, the deep-learning algorithm that is used most often, was used in this work to achieve this goal. The main goal of using this method is to teach the model to more accurately solve the given problem and in less time. It also trains the network in a good way several times to obtain a high-performance rate. The RNN is usually an extension of the LSTM, (Figure 3) which is often used to predict mood. Therefore, the suggested system uses the DRNN method to predict how stressed out working pregnant women will be. This model is made up of a lot of stacked recurrent hidden RNN states. When compared with the traditional LSTM and RNN techniques, the DRNN (Figure 4) technique speeds up the process of computing while making it more accurate. In addition, it collects high-level information well so that the label can be correctly predicted. The parameters of this method are tweaked to obtain the best results based on the feature vectors.
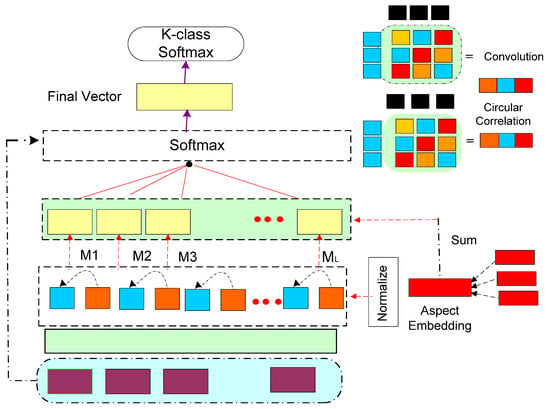
Figure 3.
LSTM model.
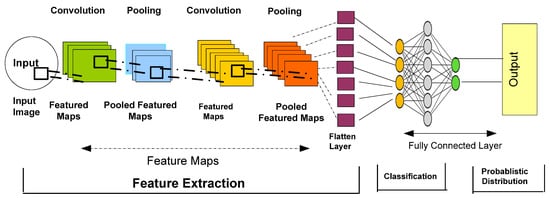
Figure 4.
DRNN architecture.
The activation function is computed with the number of filters in this model, which uses a 1D convolutional layer to convolve the given input. The feature map’s dimensionality is then calculated using the following model:
where FMH2 specifies the height of the feature map, IH1 signifies the input height before convolution, CK H denotes the height of the convolutional kernel, denotes the padding size, S si refers to the step size, and CKH denotes the height of the convolutional kernel. The local input characteristics were then extracted using a single convolution kernel, as seen below:
where, indicates the convolution kernel function with height , and represents the output after the convolution. Consequently, the maximum pooling layer is utilized to pool all convolved results with respect to the extracted feature set of text as shown in the following equations:
Finally, the output has been produced as the concatenated output, and it generates the classed label to identify whether working pregnant women are stressed or not. Figure 5 shows the Structure of DRNN.
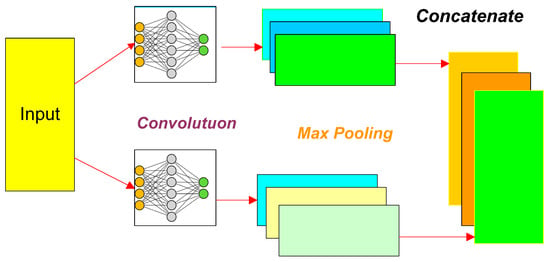
Figure 5.
Structure of DRNN.
The following are some of this research’s most significant advantages:
- ➢
- Simple layout;
- ➢
- Accurate prediction of results;
- ➢
- Reduced time spent training and testing models;
- ➢
- Improved performance rate.
5. Result and Discussion
This section explores the outcomes of existing and proposed techniques in terms of various evaluation metrics such as accuracy, precision, recall, sensitivity, specificity, F1-score, and error rate. These figures are then calculated as follows:
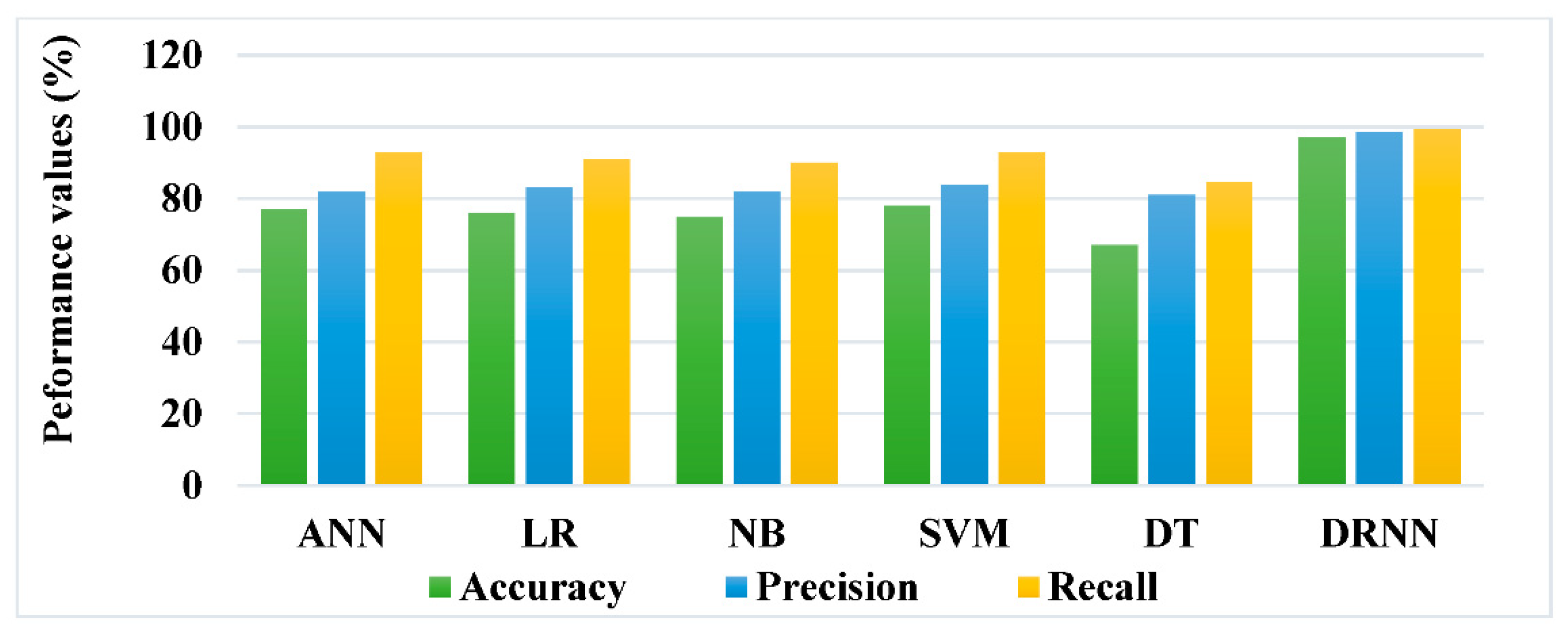
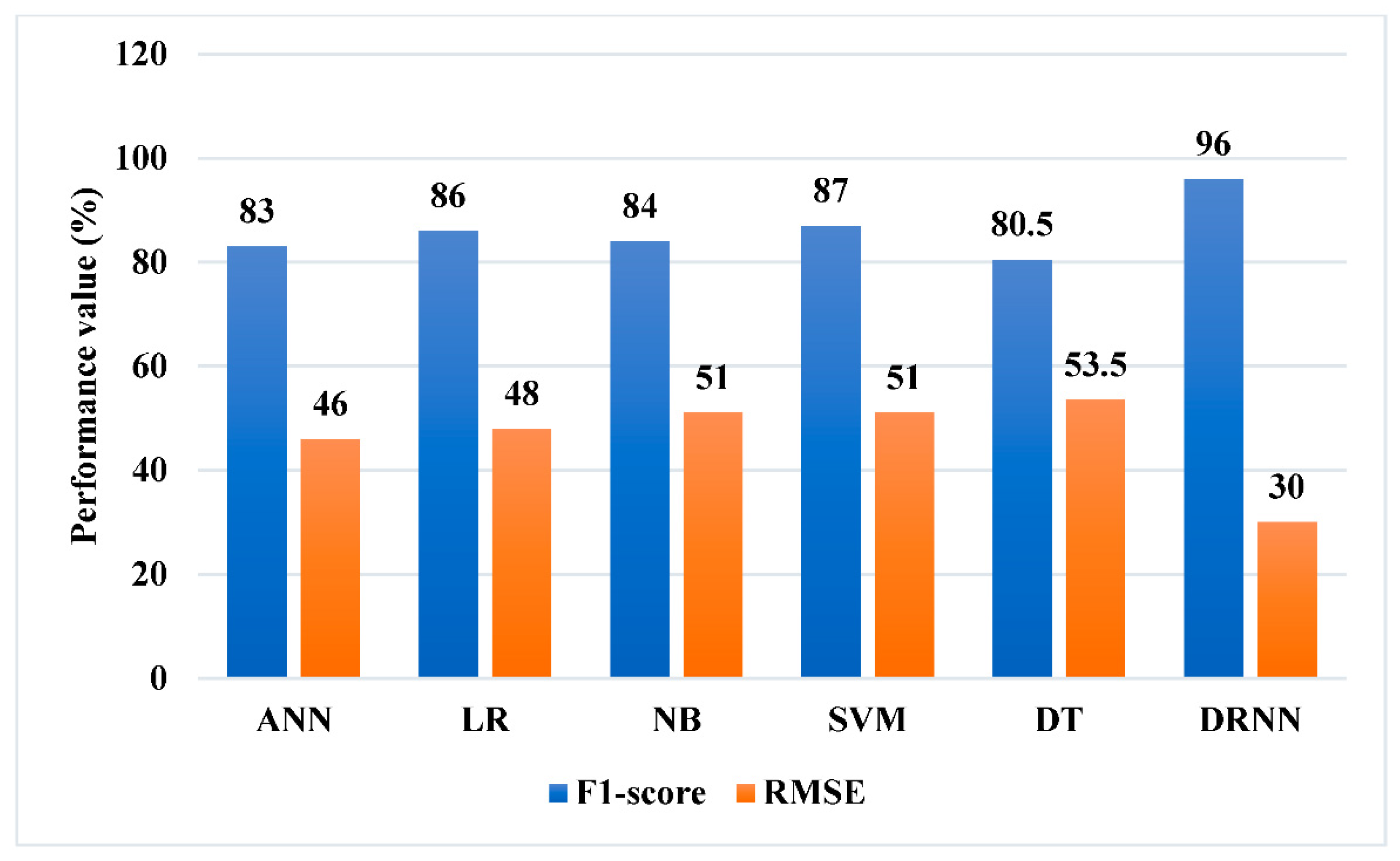
TP represents the true positives, TN represents the true negatives, FP represents the false positives, and FN represents the false negatives. Table 1 and Figure 6 illustrate the accuracy, precision, and recall measurements of both existing and proposed classification systems. Table 2 and Figure 7 present the RMSE and F1-score of known and proposed classification approaches, such as ANN, LR, NB, SVM, and DT. Typically, these criteria affect the effectiveness of a prediction system, with the number of features and attributes utilized to train the data model having a major effect on the accuracy of working pregnant women stress prediction. The results prove that the suggested DRNN model is far better than the other algorithms in terms of accuracy, precision, recall, F1-score, and RMSE values. It demonstrates that the DRNN-based technique provided for predicting working pregnant women’s stress beats other techniques in terms of overall performance.

Table 1.
Accuracy, precision, and recall measures of existing and proposed techniques.
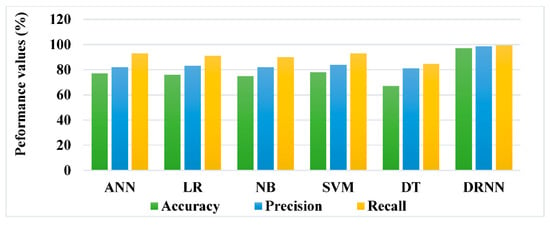
Figure 6.
Precision, accuracy, and recall of existing and planned procedures.

Table 2.
F1-scores and RMSE measures of existing and proposed techniques.
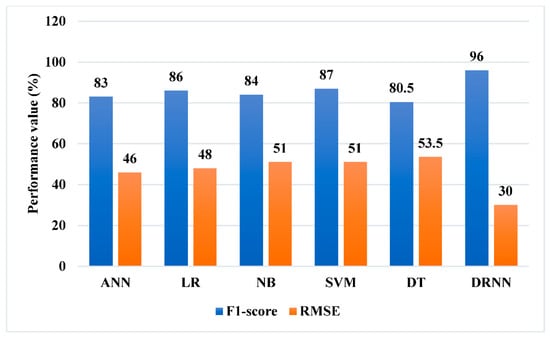
Figure 7.
RMSE and F1-score of both existing and proposed techniques.
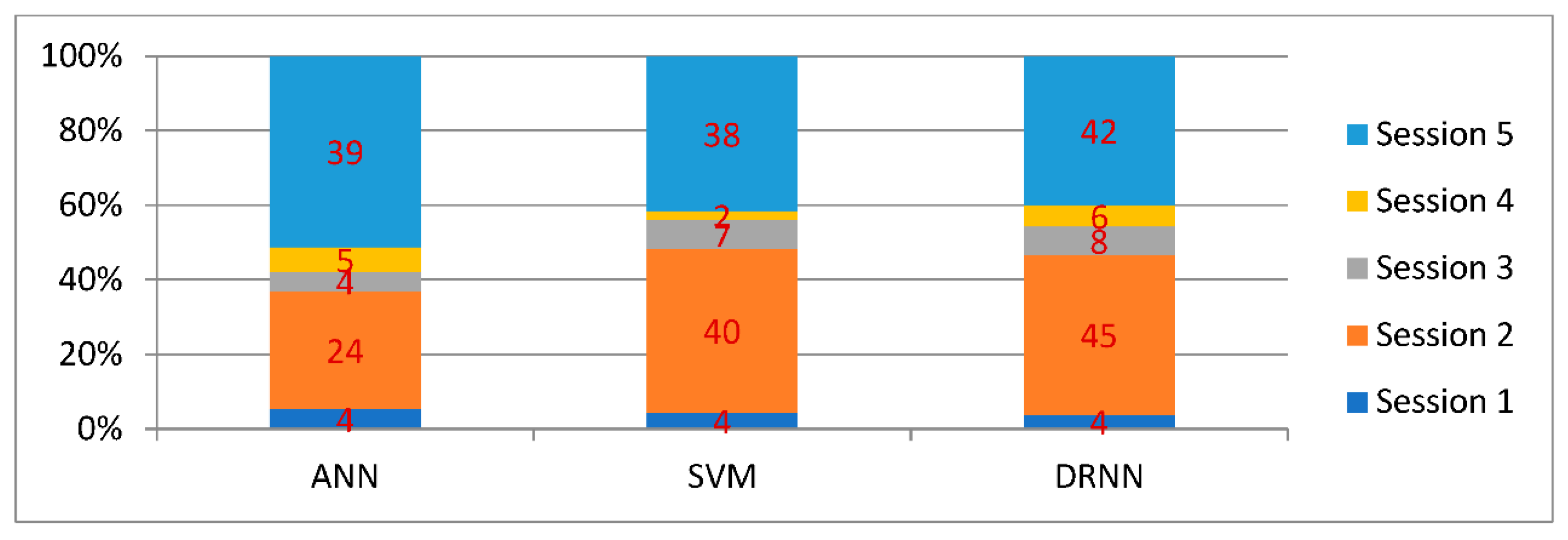
Furthermore, the prediction performance of the existing SVM, ANN, and proposed DRNN techniques is assessed using a variety of working pregnant women sessions, as shown in Figure 8 and Table 3. Based on these findings, it has been determined that the proposed DRNN technique outperforms existing techniques. This is because, in the proposed system, working pregnant women’s stress is predicted before and after work, as well as their participation in all of the official events. Additionally, working pregnant women feedback has been collected and updated with the dataset, in which the most appropriate features for improving classification performance have been extracted.
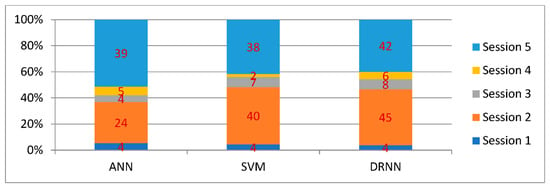
Figure 8.
Comparative analysis between existing and proposed classification techniques for varying sessions.

Table 3.
Prediction performance under varying sessions.
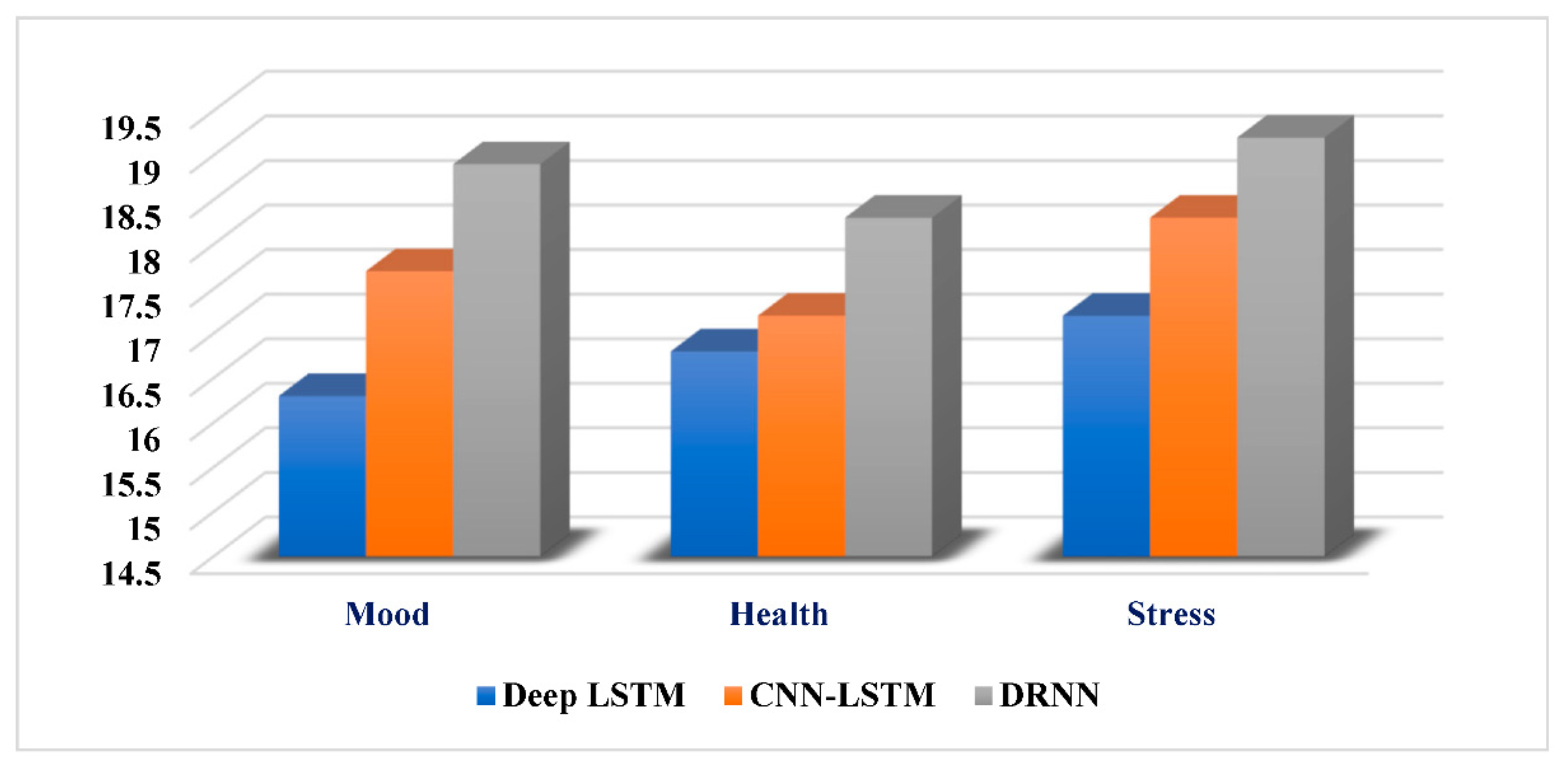
The prediction results of both existing and proposed deep-learning models for the categories of mood, health, and stress factors are shown in Table 4 and Figure 9. The results show that by training the model with the optimal set of features, the proposed DRNN-based deep learning accurately predicts the mood of working pregnant women. It aids in improving the system performance as well as accurate stress prediction in working pregnant women. The proposed model will assist to predict the stress level of women and can assist them from the side effects of stress; the accuracy of the model is better than that of the previous model, and the same is also showed by the table and figure given below.

Table 4.
Mood, health, and stress prediction outcomes of existing and proposed classification techniques.
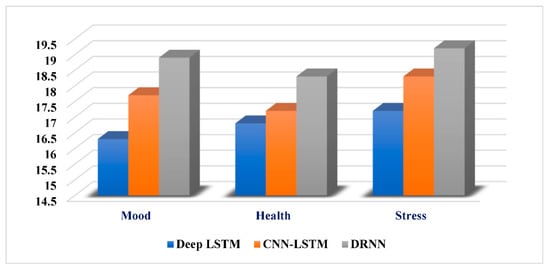
Figure 9.
Prediction results of existing and proposed deep-learning models.
6. Conclusions
Stress is a concerning issue in today’s world especially when it comes to working pregnant women; it leaves a more harmful impact on the woman and child. Therefore, in this article, we proposed a DRNN model to detect the stress level of women with high accuracy. Our proposed DRNN model achieves more than 96.00% accuracy. This research proposed an enhanced framework for estimating the stress level of working pregnant women using the DRNN. This article’s purpose was to select the optimal features for categorization to increase prediction accuracy. This article includes preprocessing, feature extraction, selection, and classification. The original dataset was initially preprocessed to normalize the content by removing unnecessary data and filling in missing values from working pregnant women. The features were then extracted and optimally picked to enhance the overall efficacy of the classification. The DRNN method was then utilized to accurately forecast whether or not a working pregnant woman is stressed based on the optimal quantity of features and feedback from the learner. There are several advantages to this system: a simple design, efficient performance, precise classification, and a decreased training time for the model. An experimental evaluation of the suggested method’s performance is used to compare it with other current models. Because of its superior performance in all of these areas, the DRNN strategy is superior to the other approaches under consideration.
In the future, this research can be expanded to include more real-time applications, and the system can be trained to give higher accuracy. Researchers can use new algorithms to predict the stress level of pregnant working women and help the society.
Author Contributions
Conceptualization, R.S. and A.G.; methodology, S.D.S.; software, S.S.; validation, S.D.S. and S.S.; formal analysis, N.P.; investigation, S.D.S.; resources, S.S; data curation, A.G.; writing—original draft preparation, R.S.; writing—review and editing, S.D.S.; visualization, N.P.; supervision, R.S.; project administration, N.P.; funding acquisition, B.T. All authors have read and agreed to the published version of the manuscript.
Funding
The APC was funded by Tshwane University of Technology, South Africa.
Data Availability Statement
Data available on request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Available online: https://www.stress.org/what-is-stress (accessed on 25 July 2022).
- Available online: https://economictimes.indiatimes.com/news/company/corporate-trends/indians-professionals-suffer-higher-stress-level-than-most-workers-globally-shows-study/articleshow/87328039.cms?from=mdr (accessed on 25 July 2022).
- Rodgers, F.S. When the business case is common sense: Coming to terms with America’s family challenge. ACA J. 1992, 1, 84–93. [Google Scholar]
- Available online: https://economictimes.indiatimes.com/indian-women-most-stressed-in-the-world-nielsen-survey/articleshow/9031890.cms (accessed on 12 March 2020).
- Available online: https://www.ilo.org/moscow/areas-of-work/occupational-safety-and-health/WCMS_249278/lang--en/index.htm (accessed on 27 July 2022).
- World Health Organization. Scaling Up Care for Mental, Neurological, and Substance Use Disorders: Mental Health Gap Action Programme (mhGAP); World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Herrero, S.G.; Saldaña, M.Á.; Rodriguez, J.G.; Ritzel, D.O. Influence of task demands on occupational stress: Gender differences. J Saf. Res. 2012, 43, 365–374. [Google Scholar] [CrossRef] [PubMed]
- Vamos, C.A.; Walsh, M.L.; Thompson, E.; Daley, E.M.; Detman, L.; DeBate, R. Oral-systemic health during pregnancy: Exploring prenatal and oral health providers’ information, motivation and behavioral skills. Matern. Child Health J. 2015, 19, 1263–1275. [Google Scholar] [CrossRef] [PubMed]
- Woods, S.M.; Melville, J.L.; Guo, Y.; Fan, M.Y.; Gavin, A. Psychosocial stress during pregnancy. Am. J. Obstet. Gynecol. 2010, 202, 61.e1–61.e7. [Google Scholar] [CrossRef] [PubMed]
- Newton, R.W.; Hunt, L.P. Psychosocial stress in pregnancy and its relation to low birth weight. Br. Med. J. 1984, 288, 1191–1194. [Google Scholar] [CrossRef]
- Loomans, E.M.; Van Dijk, A.E.; Vrijkotte, T.G.; van Eijsden, M.; Stronks, K.; Gemke, R.J.B.J.; van den Bergh, B.R.H. Psychosocial stress during pregnancy is related to adverse birth outcomes: Results from a large multi-ethnic community-based birth cohort. Eur. J. Public Health 2013, 23, 485–491. [Google Scholar] [CrossRef]
- Evans, J.; Heron, J.; Francomb, H.; Oke, S.; Golding, J. Cohort study of depressed mood during pregnancy and after childbirth. BMJ 2001, 323, 257–260. [Google Scholar] [CrossRef] [PubMed]
- Heron, J.; O’Connor, T.G.; Evans, J.; Golding, J.; Glover, V. ALSPAC Study Team The course of anxiety and depression through pregnancy and the postpartum in a community sample. J. Affect Disord. 2004, 80, 65–73. [Google Scholar] [CrossRef]
- Grote, N.K.; Bridge, J.A.; Gavin, A.R.; Melville, J.L.; Iyengar, S.; Katon, W.J. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch. Gen Psychiatry 2010, 67, 1012–1024. [Google Scholar] [CrossRef]
- Meijer, J.L.; Beijers, C.; van Pampus, M.G.; Verbeek, T.; Stolk, R.; Milgrom, J.; Bockting, C.; Burger, H. Predictive accuracy of Edinburgh postnatal depression scale assessment during pregnancy for the risk of developing postpartum depressive symptoms: A prospective cohort study. BJOG Int. J. Obstet. Gynaecol. 2014, 121, 1604–1610. [Google Scholar] [CrossRef]
- Gausia, K.; Fisher, C.; Ali, M.; Oosthuizen, J. Antenatal depression and suicidal ideation among rural Bangladeshi women: A community-based study. Arch. Womens Ment. Health 2009, 12, 351–358. [Google Scholar] [CrossRef] [PubMed]
- Peruzzo, D.C.; Benatti, B.B.; Ambrosano, G.M.; Nogueira-Filho, G.R.; Sallum, E.A.; Casati, M.Z.; Nociti, F. A systematic review of stress and psychological factors as possible risk factors for periodontal disease. J. Periodontol. 2007, 78, 1491–1504. [Google Scholar] [CrossRef] [PubMed]
- Evans, J.; Heron, J.; Patel, R.R.; Wiles, N. Depressive symptoms during pregnancy and low birth weight at term: Longitudinal study. Br. J. Psychiatry 2007, 191, 84–85. [Google Scholar] [CrossRef] [PubMed]
- Wadhwa, P.D.; Sandman, C.A.; Porto, M.; Dunkel-Schetter, C.; Garite, T.J. The association between prenatal stress and infant birth weight and gestational age at birth: A prospective investigation. Am. J. Obstet. Gynecol. 1993, 169, 858–865. [Google Scholar] [CrossRef]
- Lobel, M.; Cannella, D.L.; Graham, J.E.; DeVincent, C.; Schneider, J.; Meyer, B.A. Pregnancy-specific stress, prenatal health behaviors, and birth outcomes. Health Psychol. 2008, 27, 604–615. [Google Scholar] [CrossRef]
- Silveira, M.L.; Whitcomb, B.W.; Pekow, P.; Carbone, E.T.; Chasan-Taber, L. Anxiety, depression, and oral health among US pregnant women: 2010 Behavioral Risk Factor Surveillance System. J. Public Health Dent. 2016, 76, 56–64. [Google Scholar] [CrossRef]
- Ahmed, A.E.; Albalawi, A.N.; Alshehri, A.A.; AlBlaihed, R.M.; Alsalamah, M.A. Stress and its predictors in pregnant women: A study in Saudi Arabia. Psychol. Res. Behav. Manag. 2017, 10, 97–102. [Google Scholar] [CrossRef]
- Kumar, J.; Samelson, R. Oral Health Care during Pregnancy and Early Childhood: Practice Guidelines; New York State Department of Health: New York, NY, USA, 2006. [Google Scholar]
- Qasrawi, R.; Amro, M.; VicunaPolo, S.; Abu Al-Halawa, D.; Agha, H.; Abu Seir, R.; Hoteit, M.; Hoteit, R.; Allehdan, S.; Behzad, N.; et al. Machine learning techniques for predicting depression and anxiety in pregnant and postpartum women during the COVID-19 pandemic: A cross-sectional regional study. F1000Research 2022, 11, 390. [Google Scholar] [CrossRef]
- Taylor, S.; Jaques, N.; Nosakhare, E.; Sano, A.; Picard, R. Personalized multitask learning for predicting tomorrow’s mood, stress, and health. IEEE Trans. Affect. Comput. 2017, 11, 200–213. [Google Scholar] [CrossRef]
- Katz, V.L. Work and work-related stress in pregnancy. Clin. Obstet. Gynecol. 2012, 55, 765–773. [Google Scholar] [CrossRef]
- U.S. Bureau of Labor Statistics. Employment Characteristics of Families—2016; BLS: Washington, DC, USA, 2017. Available online: https://www.bls.gov/news.release/pdf/famee.pdf (accessed on 19 October 2017).
- U.S. Census Bureau. Maternity Leave and Employment Patterns of First-Time Mothers: 1961–2008: Current Population Reports P70-128; USCB: Washington, DC, USA, 2011. Available online: https://www.census.gov/prod/2011pubs/p70-128.pdf (accessed on 12 October 2017).
- World Health Organization. Mental Health and Substance Use; World Health Organization: Geneva, Switzerland, 2020; Available online: https://www.who.int/teams/mental-health-and-substance-use/maternal-mental-health (accessed on 20 July 2022).
- Biaggi, A.; Conroy, S.; Pawlby, S.; Pariante, C.M. Identifying the women at risk of antenatal anxiety and depression: A systematic review. J. Afect. Disord. 2016, 191, 62–77. [Google Scholar] [CrossRef] [PubMed]
- Dennis, C.L.; Falah-Hassani, K.; Shiri, R. Prevalence of antenatal and postnatal anxiety: Systematic review and meta-analysis. Br. J. Psychiatry 2017, 210, 315–323. [Google Scholar] [CrossRef] [PubMed]
- Glover, V. Prenatal stress and its efects on the fetus and the child: Possible underlying biological mechanisms. In Perinatal Programming of Neurodevelopment; Springer: New York, NY, USA, 2015; pp. 269–283. [Google Scholar] [CrossRef]
- Jaques, N.; Taylor, S.; Sano, A.; Picard, R. Predicting tomorrow’s mood, health, and stress level using personalized multitask learning and domain adaptation. In Proceedings of the IJCAI 2017 Workshop on Artificial Intelligence in Affective Computing, Melbourne, Australia, 20 August 2017; pp. 17–33. [Google Scholar]
- Sumathi, V.; Velmurugan, R.; Sudarvel, J.; Sathiyabama, P. Intelligent Classification of Women Working in ICT based Education. In Proceedings of the 2021 7th International Conference on Advanced Computing and Communication Systems (ICACCS), Coimbatore, India, 19–20 March 2021; pp. 1711–1715. [Google Scholar]
- Van Assche, F.A.; Holemans, K.; Aerts, L. Long-term consequences for offspring of diabetes during pregnancy. Br. Med. Bull. 2001, 60, 173–182. [Google Scholar] [CrossRef][Green Version]
- Nath, R.K.; Thapliyal, H.; Caban-Holt, A.; Mohanty, S.P. Machine learning based solutions for real-time stress monitoring. IEEE Consum. Electron. Mag. 2020, 9, 34–41. [Google Scholar] [CrossRef]
- Hsu, C.M.; Chen, C.H. The prevalence and predictors of prenatal depression. J. Evid.-Based Nurs. 2008, 42, 149–156. [Google Scholar]
- Xu, Q.; Nwe, T.L.; Guan, C. Cluster-based analysis for personalized stress evaluation using physiological signals. IEEE J. Biomed. Health Inform. 2014, 19, 275–281. [Google Scholar] [CrossRef] [PubMed]
- Priya, A.; Garg, S.; Tigga, N.P. Predicting anxiety, depression and stress in modern life using machine learning algorithms. Procedia Comput. Sci. 2020, 167, 1258–1267. [Google Scholar] [CrossRef]
- Figà-Talamanca, I. Occupational risk factors and reproductive health of women. Occup. Med. 2006, 56, 521–531. [Google Scholar] [CrossRef]
- Billah, M.; Raihan, M.; Alvi, N.; Akter, T.; Bristy, N.J. A Data Mining Approach to Identify the Stress Level Based on Different Activities of Human. In Proceedings of the 2021 International Conference on Information and Communication Technology for Sustainable Development (ICICT4SD), Dhaka, Bangladesh, 27–28 February 2021; pp. 31–34. [Google Scholar]
- Sharma, S.; Shah, P.; Dev Sharma, S.; Pathak, A. A bibliometric analysis of stress level prediction of working pregnant women. Intelligent Systems, River Publishers Series in Proceedings; pp. 234–243. Available online: https://www.riverpublishers.com/research_details.php?book_id=1004 (accessed on 25 July 2022).
- Phutela, N.; Relan, D.; Gabrani, G.; Kumaraguru, P.; Samuel, M. Stress Classification Using Brain Signals Based on LSTM Network. Comput. Intell. Neurosci. 2022, 2022, 7607592. [Google Scholar] [CrossRef]
- Martino, F.D.; Delmastro, F. High-Resolution Physiological Stress Prediction Models based on Ensemble Learning and Recurrent Neural Networks. In Proceedings of the 2020 IEEE Symposium on Computers and Communications (ISCC), Rennes, France, 7–10 July 2020; pp. 1–6. [Google Scholar] [CrossRef]
- Motrico, E.; Bina, R.; Domínguez-Salas, S.; Mateus, V.; Contreras-García, Y.; Carrasco-Portiño, M.; Ajaz, E.; Apter, G.; Christoforou, A.; Dikmen-Yildiz, P.; et al. Impact of the COVID-19 pandemic on perinatal mental health (Riseup-PPD-COVID-19): Protocol for an international prospective cohort study. BMC Public Health 2021, 21, 368. [Google Scholar] [CrossRef]
- Li, R.; Liu, Z. Stress detection using deep neural networks. BMC Med. Inform. Decis. Mak. 2020, 20, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Qi, E. Happy work: Improving enterprise human resource management by predicting workers’ stress using deep learning. PLoS ONE 2022, 17, e0266373. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).