Technological Advancements and Elucidation Gadgets for Healthcare Applications: An Exhaustive Methodological Review-Part-I (AI, Big Data, Block Chain, Open-Source Technologies, and Cloud Computing)
Abstract
:1. Introduction
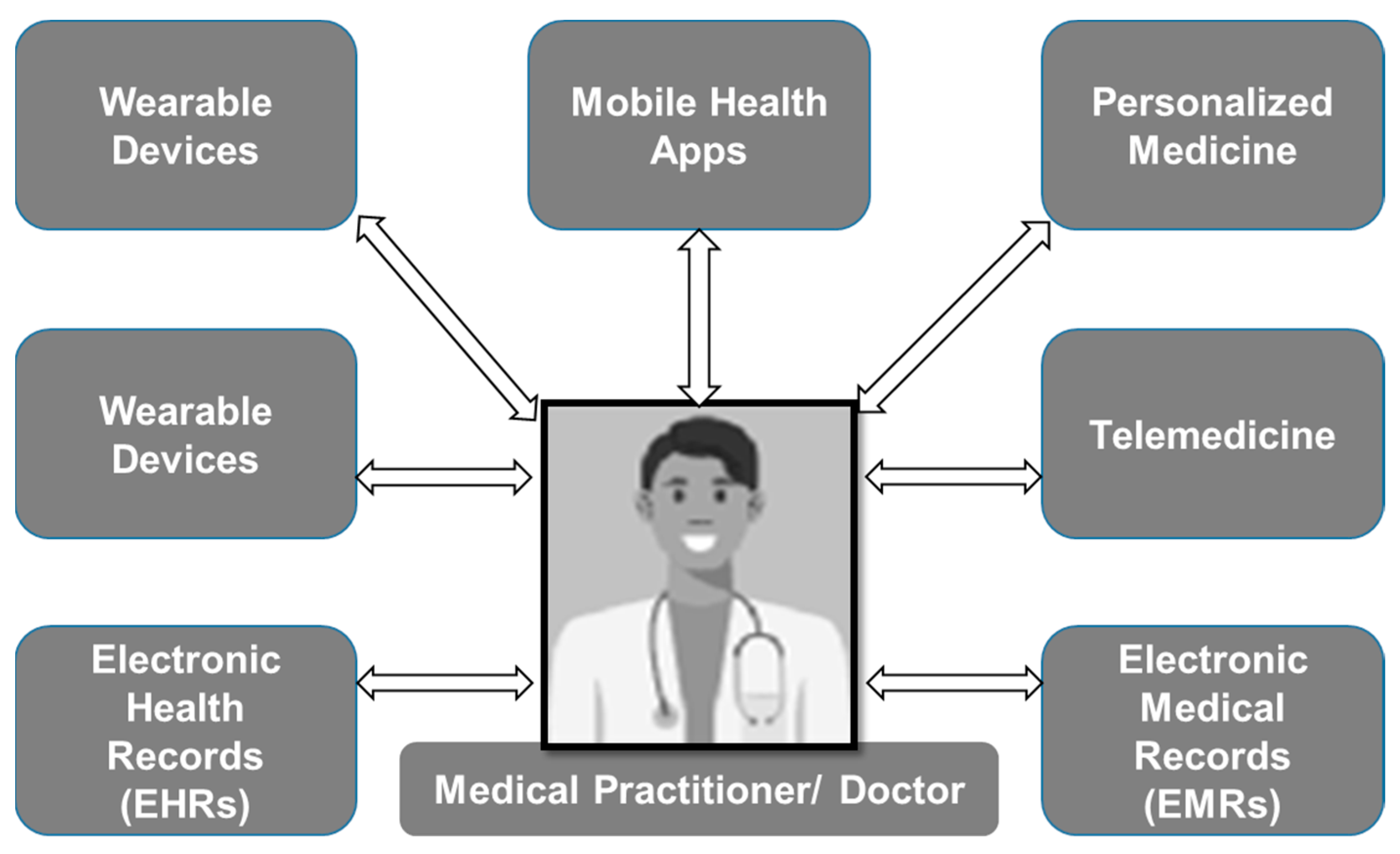
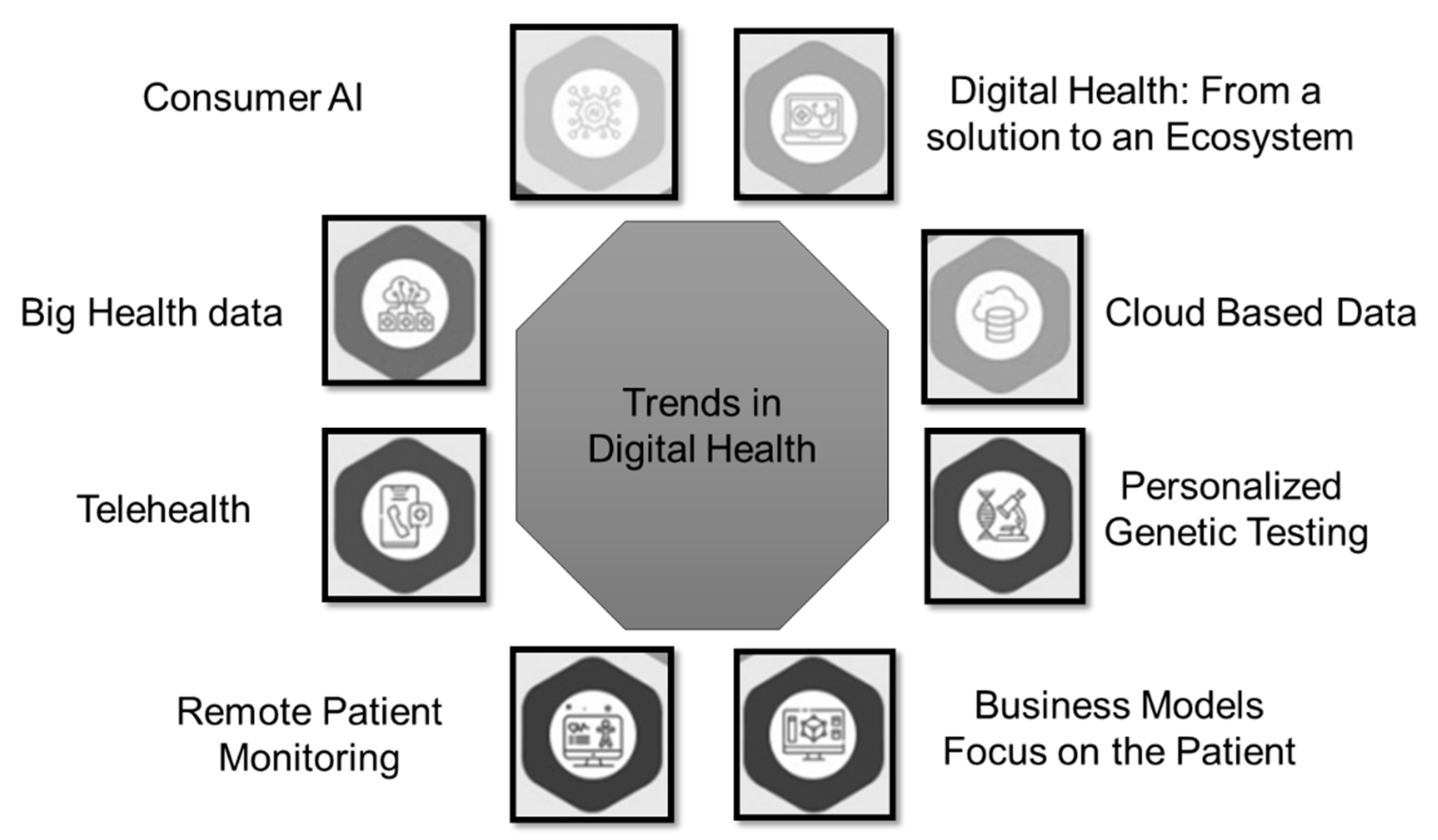
2. Overview of Technological Contributions to Healthcare Sector
3. Emerging Technologies
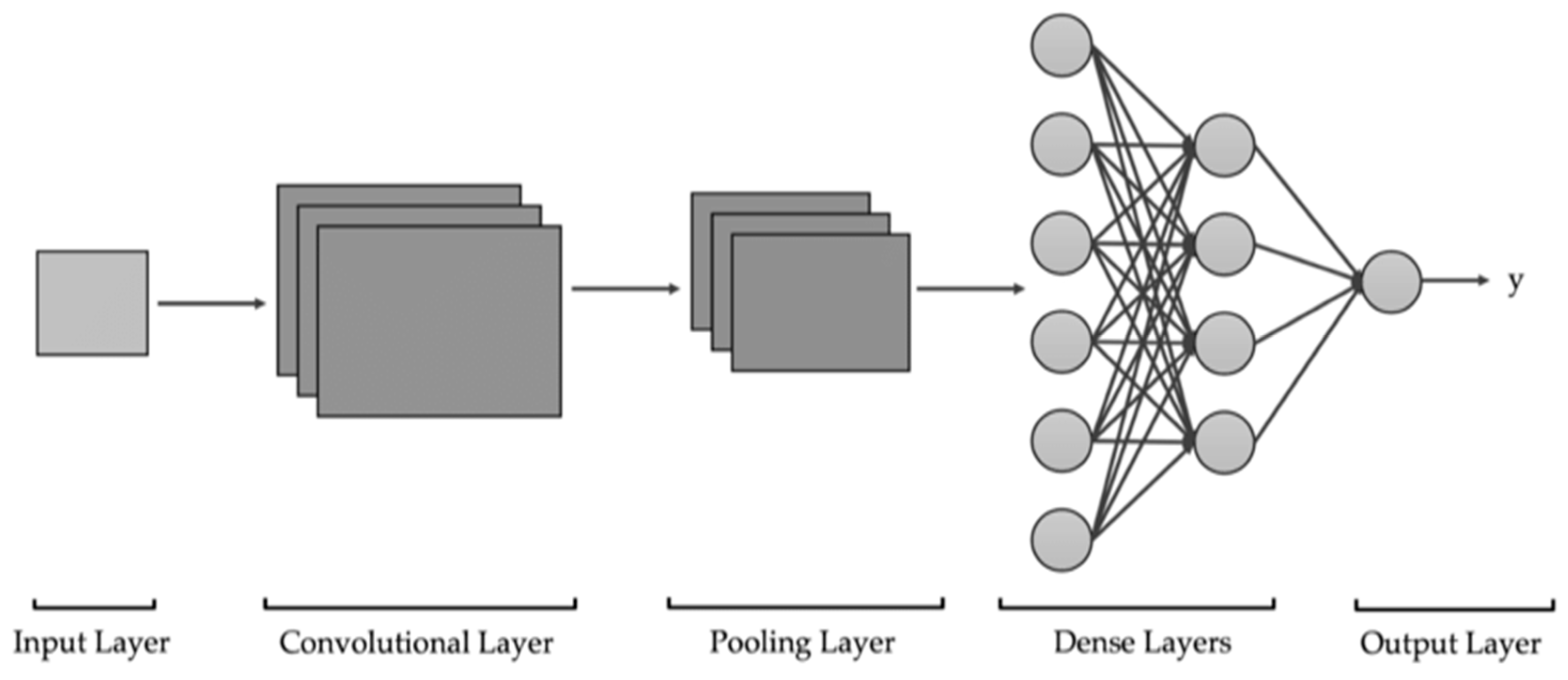
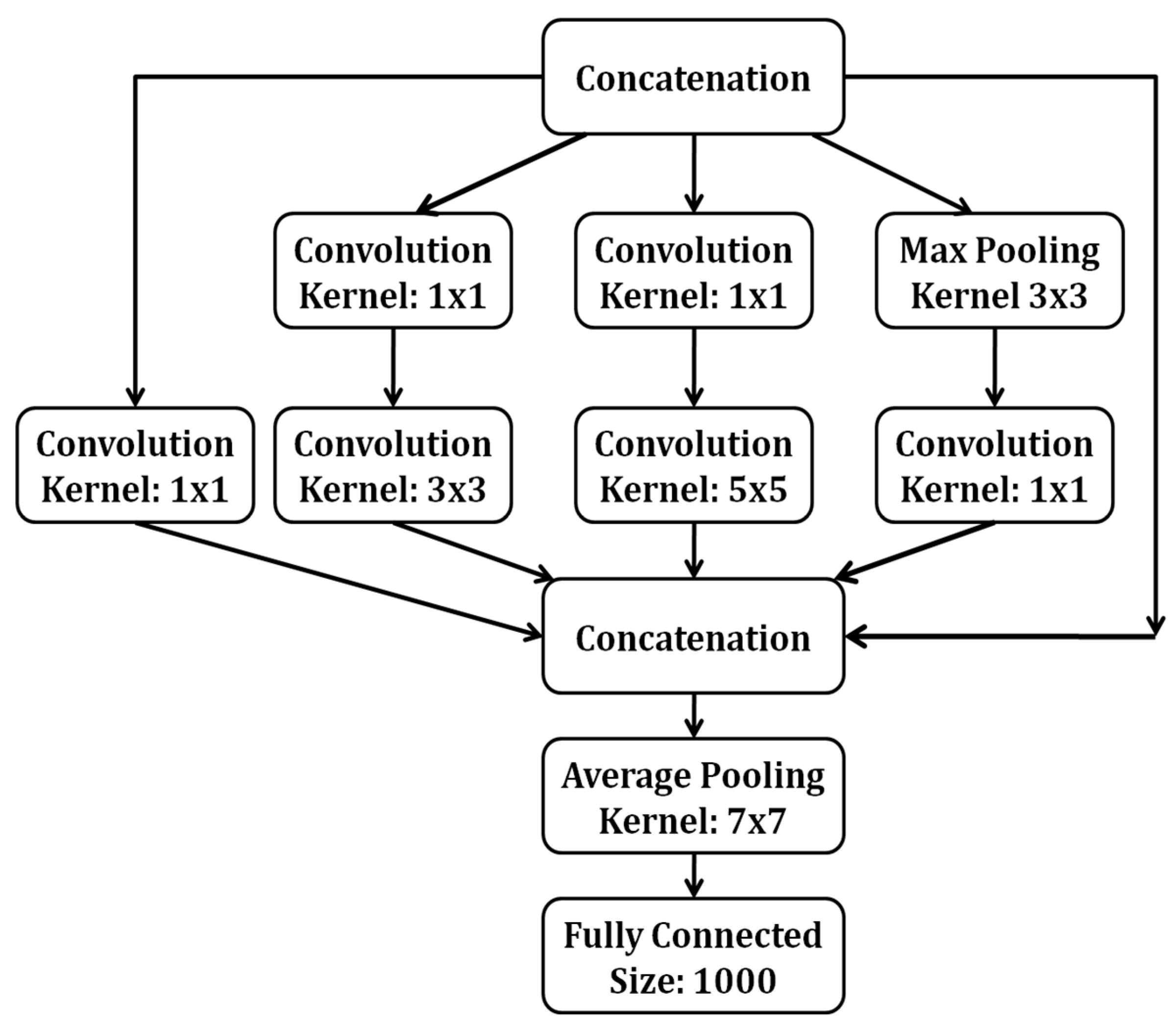
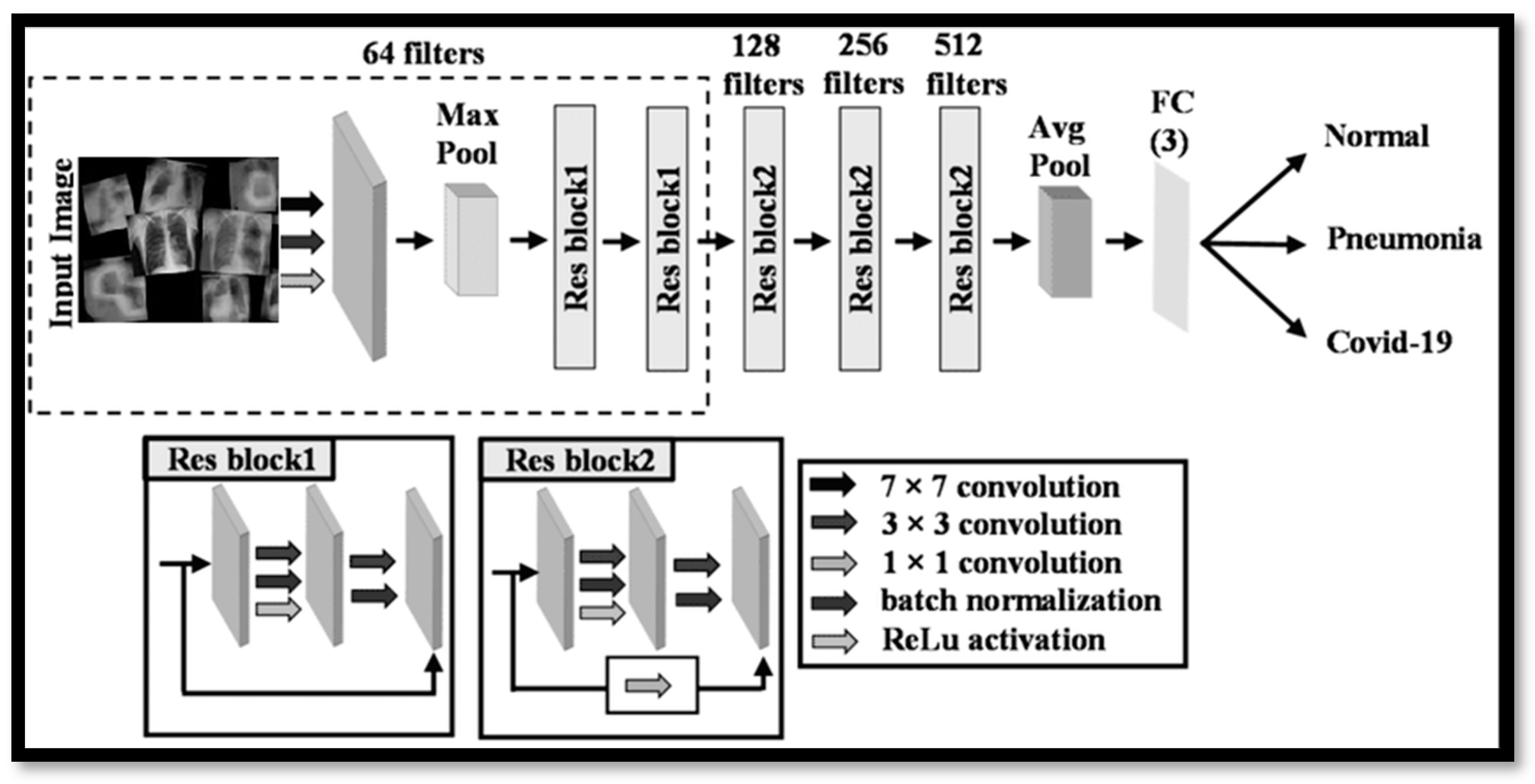
3.1. Artificial Intelligence
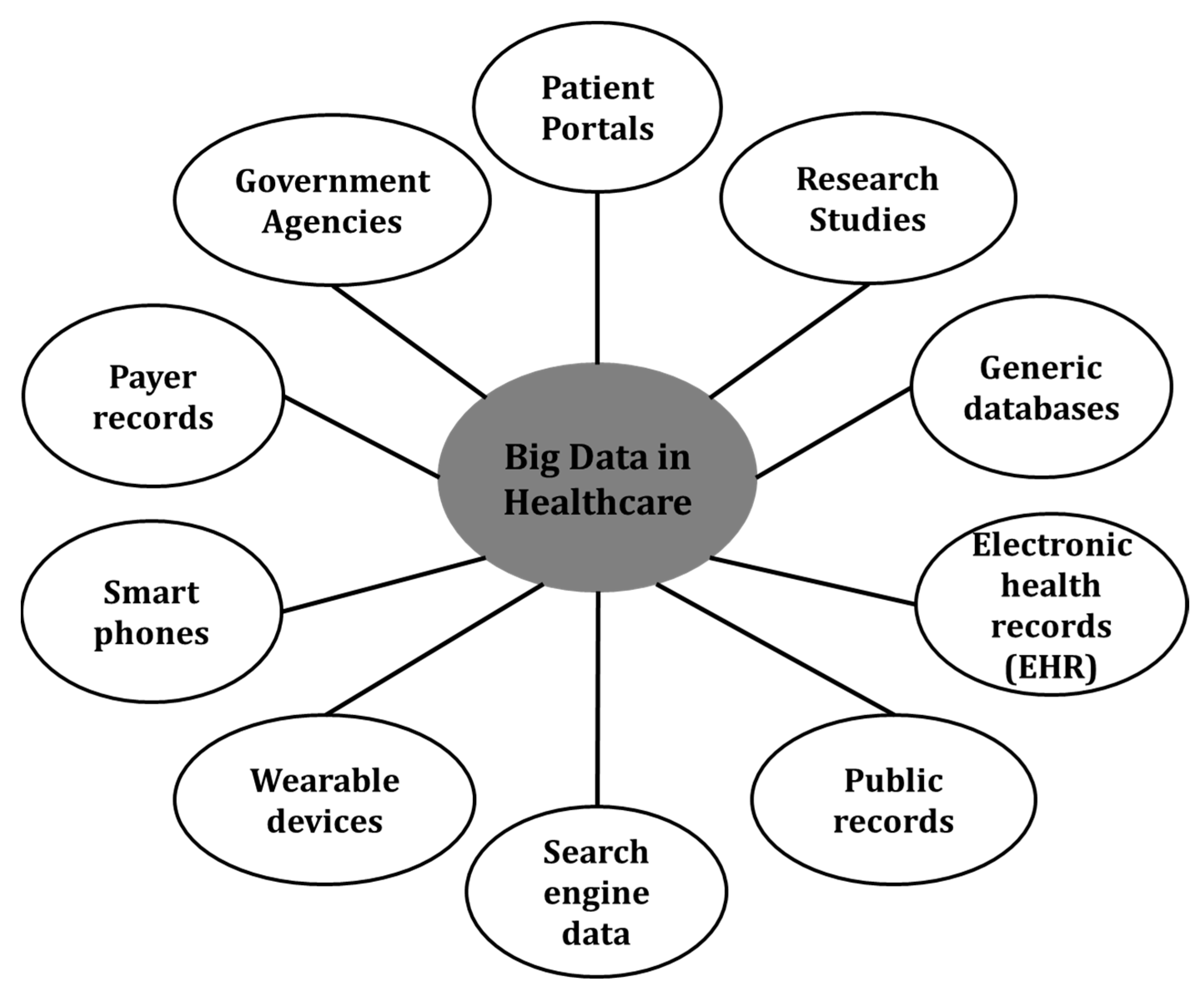
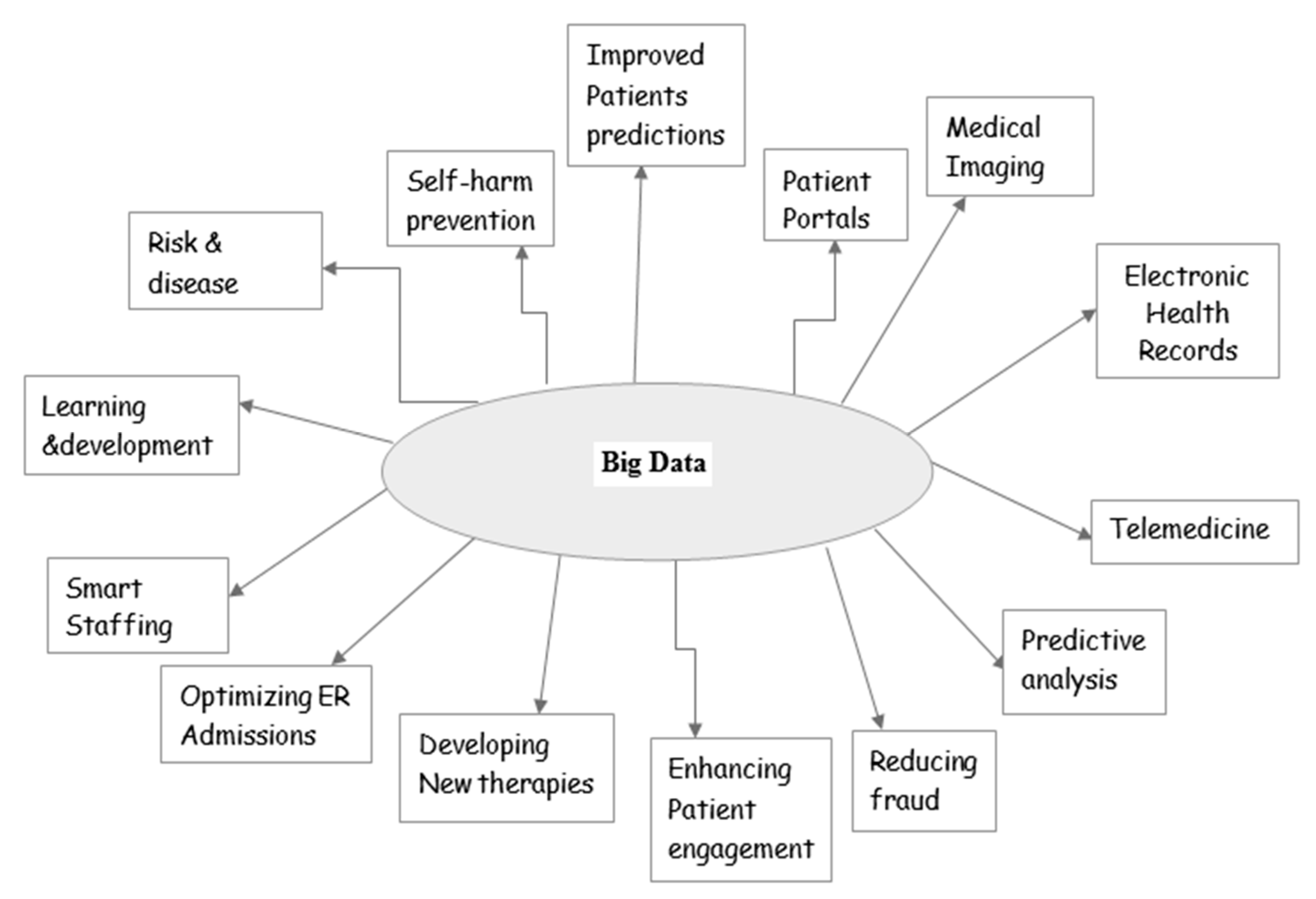
3.2. Big Data
- (A)
- Prediction of staffing requirements in hospitals, based on patient count.
- (B)
- Patients’ electronic health records (EHRs) maintenance, warning them of pending lab tests in synchronization with doctor’s instructions.
- (C)
- Provision of on-the-spot real-time medical data analysis to healthcare practitioners by continuously gathering patient’s health data and pumping the same to the cloud instantly.
- (D)
- Enhance patient’s self-health monitoring engagement using smart devices, for example, counting steps walked upon, monitoring heart beats, blood pressure levels, sugar levels, sleeping habits, etc., connecting them to physicians as, and when, required.
- (E)
- Promoting patients to opt for advanced medical treatments based on factors that are really discouraging them from taking up treatments.
- (F)
- In cancer, curing enables medical researchers to examine tumor samples and predict the interaction of certain mutations based on patient treatment records (in bio-banks) to chalk out the highest rates of recovery and success in cancer patients.
- (G)
- It is helpful in sequencing cancer samples genetically and deploying them to a cancer database and the global researcher’s community.
- (H)
- Predictive analytics help doctors to arrive at life-saving conclusive treatments, in the case of patients suffering from complex ailments and disorders.
- (I)
- Big Data analytics promote telemedicine services to prevent the further worsening of patient’s health conditions in remote areas.
- (J)
- Integration of Big Data analytics into medical imaging for healthcare drastically saves the time incurred by radiologists by quickly finalizing the clinical procedures to be adopted for every patient.
- (K)
- Big Data analytics helps healthcare institutions in preventing suicide deaths and self-harm (as globally, around eight lakhs people expiring every year due to suicides).
- (L)
- Big Data analytics provides end-to-end effective supply chain management solutions to hospitals and healthcare institutions by leveraging the analytics tools to arrive at accurate decisions.
- (M)
- Big Data analytics play a pivotal role in developing ground-breaking new drugs and forward-thinking therapies, based on gene cloning information analysis and intransigent patient predictions.
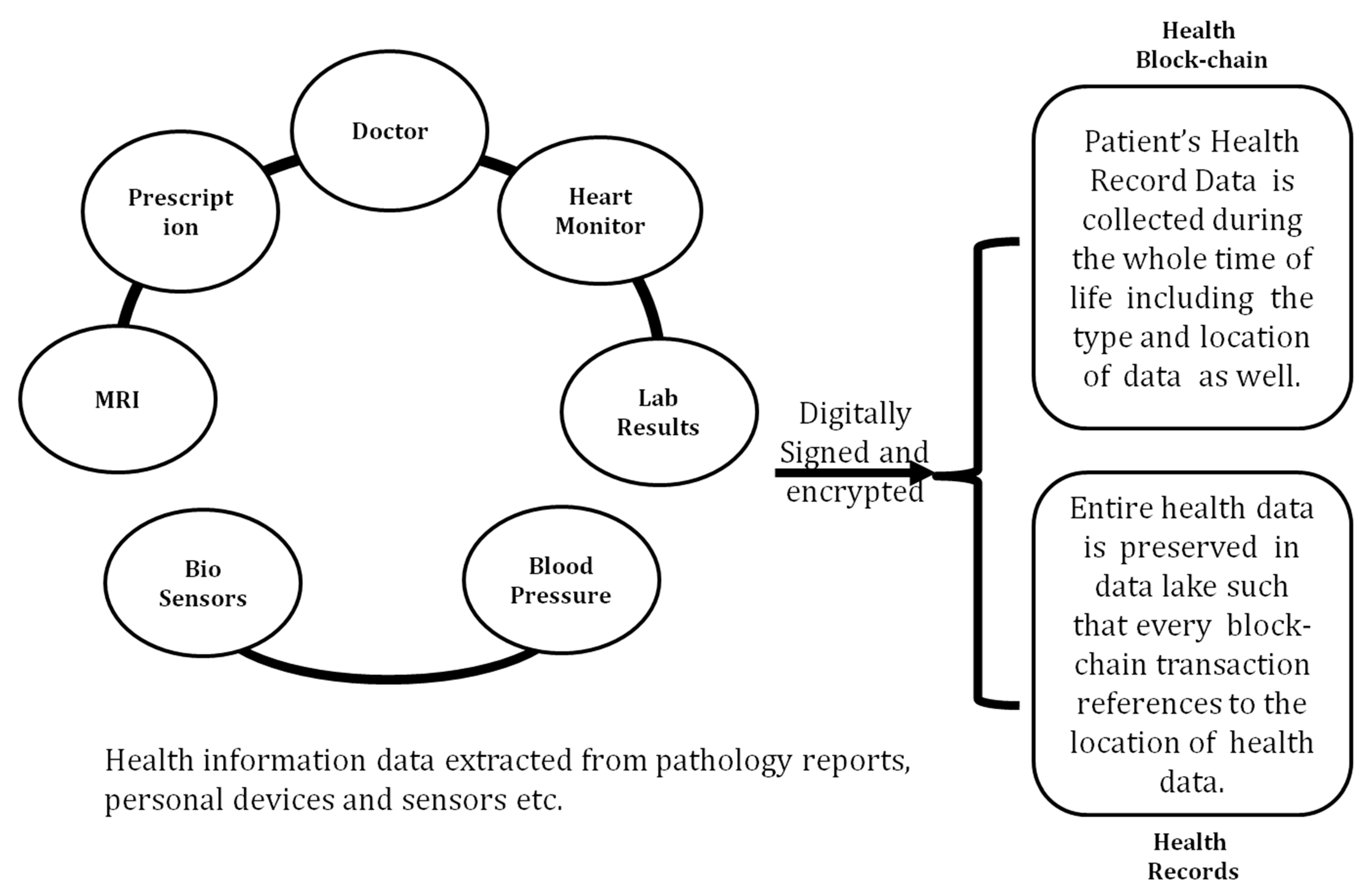
3.3. Block Chain Technology
3.4. Open-Source Technologies
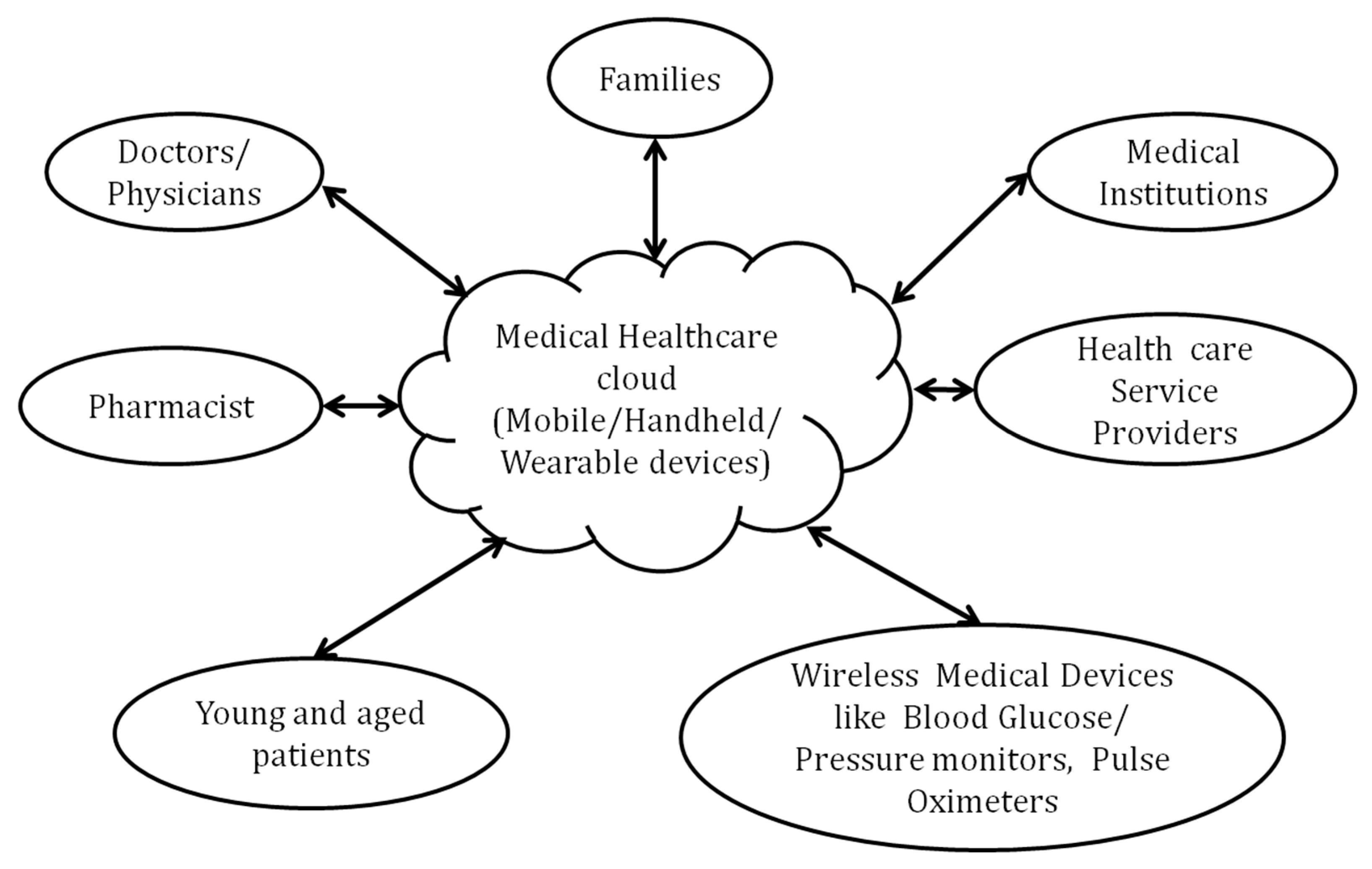
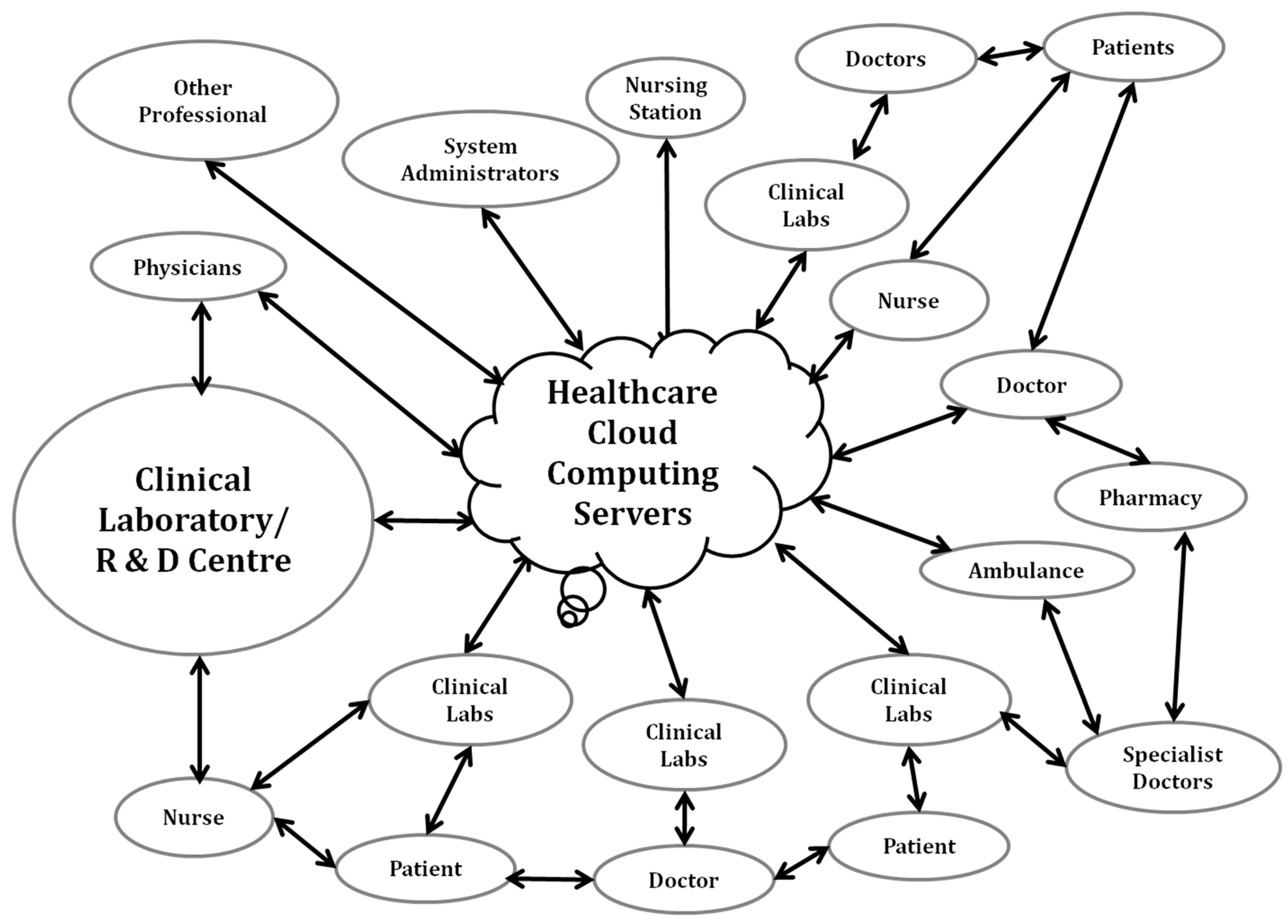
3.5. Cloud Computing for Healthcare
- A.
- An efficient electronic medical health record (EMHR) ensures hospitals and healthcare institutions facilitate the storage of the entire patient health history, in order to provide enhanced medical services with the fullest security and privacy of data.
- B.
- Cloud storage machinery for the EMHR of patients paved the way for a collaborative patient caring mechanism, ensuring the easy sharing of patient’s medical records with other physicians and surgeons, in order to formulate the treatment methodologies to be adopted for every patient, thereby preventing over-prescribed medications and repeated tests for the patients.
- C.
- Since cloud-based healthcare service providers alone handle the maintenance of cloud services, healthcare providers need not worry about the initial expenditures and can focus more upon rendering the best services to patients, except to arrange provisions for their own storage space and hardware setups.
- D.
- With the EMHR mechanism, healthcare providers can maintain an onsite data storage system, with IT staff totally waiving having reams of patient data physically, which is prone to theft/damage or being affected by natural disasters etc.
- E.
- Truly speaking, cloud healthcare paved the way for Big Data applications because the EMHR mechanism today enables physicians and doctors to predict effective treatment options for patients, based on subtle correlations in patients past medical data using, many complex computer algorithms.
- F.
- Cloud healthcare provides long-term financial benefits to organizations because it ensures fully scalable healthcare solutions, with provisions for the in-line expansion of the business.
- G.
- The cloud healthcare EMHR-based data storage mechanism promotes researchers to derive more benefits from digitized healthcare information and open access to massive, previously inaccessible data sets.
- H.
- Cloud healthcare provides an interoperability platform to facilitate rapid data transfer between IoT-enabled devices that can interface freely, such that organizations with cloud computing capabilities can acclimatize to the changing scenario of the healthcare landscape in the future [207].
4. Future Scope and Challenges
- Though artificial intelligence penetrated into chat bots, CAD (computer-aided detection) systems for diagnosis, and surgeries leveraging analytics, human surveillance cannot be avoided in surgeries because surgical robots can operate logically, but not empathetically - on the other hand AI applications and relevant data are not totally free from (i.e., they are susceptible to) cyber-attacks.
- With the healthcare organizations adopting Big Data in large numbers, multiple sources of Big Data include data from hospital records, patients’ health records, the results of medical examinations, wearable devices, the Internet of Things (IoT), etc., and the challenges associated with handling Big Data demands adequate infrastructure to systematically analyze Big Data. On the other hand, incompetent and incompatible data systems render the interfacing of big data sets difficult, thereby posing problems to ensuring the confidentiality of patient’s data.
- Though fullest deployment of block chain technology bears a potential to revolutionize healthcare sector by ensuring medical records to be well-organized and secured. Storage of patient EHR (electronic health records) on block chain is not economically viable for implementation (especially in the developing and middle-eastern countries). Further it is difficult to query data with block chain technology; data redundancy, data privacy infringement, data ownership, etc., are the additional challenges associated left for being addressed by research community.
- Though open-source technologies (OST) hold the potential to bring various healthcare service providers together, i.e., pharmaceutical vendors, medical institutions, patient communities, and researchers, and by slashing down the IT infrastructure costs, they remain agile to adopt novel IT solutions, while the shared availability of OST elevates the risk of hacking and data breaches, as well as the lack of standardization in utility, when compared with software’s provided by the standard vendors.
- Cloud computing transformed the healthcare sector by hastening the migration of workloads from data centers to the cloud, significantly changing the way information systems are deployed, operated, and maintained inside a sole informative system. Cloud computing data in the healthcare sector is prone to data breaches and security issues, thereby raising concerns in protecting the privacy of real-time data; henceforth, the types and levels of security issues are left open to be taken care of.
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Salehi, A.W.; Baglat, P.; Gupta, G. Review on machine and deep learning models for the detection and prediction of Coronavirus. Mater. Today Proc. 2020, 33, 3896–3901. [Google Scholar] [CrossRef]
- Wilson, D.; Falush, D.; McVean, G. Germs, genomes and genealogies. Trends Ecol. Evol. 2005, 20, 39–45. [Google Scholar] [CrossRef]
- Jamshidi, M.B.; Lalbakhsh, A.; Talla, J.; Peroutka, Z.; Hadjilooei, F.; Lalbakhsh, P.; Jamshidi, M.; La Spada, L.; Mirmozafari, M.; Dehghani, M.; et al. Artificial Intelligence and COVID-19: Deep Learning Approaches for Diagnosis and Treatment. IEEE Access 2020, 8, 109581–109595. [Google Scholar] [CrossRef]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef]
- Chen, N.; Zhou, M.; Dong, X.; Qu, J.; Gong, F.; Han, Y.; Qiu, Y.; Wang, J.; Liu, Y.; Wei, Y.; et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 2020, 395, 507–513. [Google Scholar] [CrossRef]
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus—Infected Pneumonia in Wuhan, China. JAMA 2020, 323, 1061–1069. [Google Scholar] [CrossRef]
- Liu, K.; Fang, Y.-Y.; Deng, Y.; Liu, W.; Wang, M.-F.; Ma, J.-P.; Xiao, W.; Wang, Y.-N.; Zhong, M.-H.; Li, C.-H.; et al. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. Chin. Med. J. 2020, 133, 1025–1031. [Google Scholar] [CrossRef]
- Manolis, A.S.; Manolis, T.A. Cardiovascular Complications of the Coronavirus (COVID-19) Infection: COVID-19 and the Heart. Rhythmos 2020, 15, 23–28. [Google Scholar]
- McCloskey, B.; Dar, O.; Zumla, A.; Heymann, D.L. Emerging infectious diseases, and pandemic potential: Status quo and reducing risk of global spread. Lancet Infect. Dis. 2014, 14, 1001–1010. [Google Scholar] [CrossRef]
- Wang, Z.; Tang, K. Combating COVID-19: Health equity matters. Nat. Med. 2020, 26, 2019–2021. [Google Scholar] [CrossRef]
- Jiang, F.; Jiang, Y.; Zhi, H.; Dong, Y.; Li, H.; Ma, S.; Wang, Y.; Dong, Q.; Shen, H.; Wang, Y. Artificial intelligence in healthcare: Past, present and future. Stroke Vasc. Neurol. 2017, 2, 230–243. [Google Scholar] [CrossRef] [Green Version]
- Daveport, T.; Karakota, R. The potential for artificial intelligence in health-care. Future Health-Care J. 2019, 6, 92–98. [Google Scholar] [CrossRef]
- Javeed, A.; Khan, S.U.; Ali, L.; Ali, S.; Imrana, Y.; Rahman, A. Machine Learning-Based Automated Diagnostic Systems Developed for Heart Failure Prediction Using Different Types of Data Modalities: A Systematic Review and Future Directions. Comput. Math. Methods Med. 2022, 2022, 9288452. [Google Scholar] [CrossRef]
- Alaus, T.B.; Turkoglu, I. Detection of pre-epileptic seizure by using wavelet packet decomposition and artificial neural networks. In Proceedings of the 10th International Conference on Electrical and Electronic Engineering, Bursa, Turkey, 30 November–2 December 2017; pp. 511–515. [Google Scholar]
- Memarian, N.; Kim, S.; Dewar, S.; Engel, J.; Staba, R.J. Multimodal data and machine learning for surgery outcome prediction in complicated cases of mesial temporal lobe epilepsy. Comput. Biol. Med. 2015, 64, 67–78. [Google Scholar] [CrossRef]
- Yousefi, J.; Hamilton-Wright, A. Characterizing EMG data using machine-learning tools. Comput. Biol. Med. 2014, 51, 1–13. [Google Scholar] [CrossRef]
- Karthick, P.; Ghosh, D.M.; Ramakrishnan, S. Surface electromyography based muscle fatigue detection using high-resolution time-frequency methods and machine learning algorithms. Comput. Methods Programs Biomed. 2018, 154, 45–56. [Google Scholar] [CrossRef]
- Alfaras, M.; Soriano, M.C.; Ortín, S. A Fast Machine Learning Model for ECG-Based Heartbeat Classification and Arrhythmia Detection. Front. Phys. 2019, 7, 103. [Google Scholar] [CrossRef]
- Ledezma, C.A.; Zhou, X.; Rodríguez, B.; Tan, P.J.; Díaz-Zuccarini, V. A modeling and machine learning approach to ECG feature engineering for the detection of ischemia using pseudo-ECG. PLoS ONE 2019, 14, e0220294. [Google Scholar] [CrossRef]
- Munir, K.; Elahi, H.; Ayub, A.; Frezza, F.; Rizzi, A. Cancer Diagnosis Using Deep Learning: A Bibliographic Review. Cancers 2019, 11, 1235. [Google Scholar] [CrossRef]
- Andriasyan, V.; Yakimovich, A.; Georgi, F.; Petkidis, A.; Witte, R.; Puntener, D.; Greber, U.F. Deep learning of virus infections reveals mechanics of lytic cells. bioRxiv 2019. [Google Scholar] [CrossRef]
- Senior, A.W.; Evans, R.; Jumper, J.; Kirkpatrick, J.; Sifre, L.; Green, T.; Qin, C.; Žídek, A.; Nelson, A.W.R.; Bridgland, A.; et al. Improved protein structure prediction using potentials from deep learning. Nature 2020, 577, 706–710. [Google Scholar] [CrossRef]
- Nelson, A.E. A machine learning approach to knee osteoarthritis phenol typing: Data from the FNIH Biomarkers Consortium. Osteoarthr. Cartil. 2019, 27, 994.e1001. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.M.; Mstafa, R.J. A Comprehensive Survey on Bone Segmentation Techniques in Knee Osteoarthritis Research: From Conventional Methods to Deep Learning. Diagnostics 2022, 12, 611. [Google Scholar] [CrossRef] [PubMed]
- Yeoh, P.S.Q.; Lai, K.W.; Goh, S.L.; Hasikin, K.; Hum, Y.C.; Tee, Y.K.; Dhanalakshmi, S. Emergence of Deep Learning in Knee Osteoarthritis Diagnosis. Comput. Intell. Neurosci. 2021, 2021, 4931437. [Google Scholar] [CrossRef] [PubMed]
- Panfilov, E. Deep learning-based segmentation of knee MRI for fully automatic sub-regional morphological assessment of cartilage tissues: Data from the Osteoarthritis Initiative. J. Orthop. Res. 2022, 40, 1113–1124. [Google Scholar] [CrossRef]
- Tan, J.-S.; Tippaya, S.; Binnie, T.; Davey, P.; Napier, K.; Caneiro, J.P.; Kent, P.; Smith, A.; O’Sullivan, P.; Campbell, A. Predicting Knee Joint Kinematics from Wearable Sensor Data in People with Knee Osteoarthritis and Clinical Considerations for Future Machine Learning Models. Sensors 2022, 22, 446. [Google Scholar] [CrossRef]
- Zhao, H.; Li, G.; Feng, W. Research on application of artificial intelligence in medical education. In Proceedings of the 2018 International Conference on Engineering Simulation and Intelligent Control, Changsha, China, 10–11 August 2018; pp. 340–342. [Google Scholar]
- Al-Turjman, F.; Nawaz, M.H.; Ulusar, U.D. Intelligence in the Internet of Medical Things era: A systematic review of current and future trends. Comput. Commun. 2020, 150, 644–660. [Google Scholar] [CrossRef]
- Chan, Y.-K.; Chen, Y.-F.; Pham, T.; Chang, W.; Hsieh, M.-Y. Artificial Intelligence in Medical Applications. J. Health Eng. 2018, 2018, 4827875. [Google Scholar] [CrossRef]
- Longo, U.; De Salvatore, S.; Candela, V.; Zollo, G.; Calabrese, G.; Fioravanti, S.; Giannone, L.; Marchetti, A.; De Marinis, M.; Denaro, V. Augmented Reality, Virtual Reality and Artificial Intelligence in Orthopedic Surgery: A Systematic Review. Appl. Sci. 2021, 11, 3253. [Google Scholar] [CrossRef]
- Bragazzi, N.L.; Dai, H.; Damiani, G.; Behzadifar, M.; Martini, M.; Wu, J. How Big Data and Artificial Intelligence Can Help Better Manage the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 17, 3176. [Google Scholar] [CrossRef]
- Tran, B.X.; Vu, G.T.; Ha, G.H.; Vuong, Q.-H.; Ho, M.-T.; Vuong, T.-T.; La, V.-P.; Nghiem, K.-C.P.; Nguyen, H.L.T.; Latkin, C.A.; et al. Global Evolution of Research in Artificial Intelligence in Health and Medicine: A Bibliometric Study. J. Clin. Med. 2019, 8, 360. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cabitza, F.; Locoro, A.; Banfi, G. Machine Learning in Orthopedics: A Literature Review. Front. Bioeng. Biotechnol. 2018, 6, 75. [Google Scholar] [CrossRef] [PubMed]
- Soma shekhar, S.; Kumar, R.; Kumar, A.; Patil, P.; Rauthan, A. Validation Study to Assess performance of IBM Cognitive Computing System Watson for Oncology with Manipal Multidisciplinary Tumour Board for 1000 Consecutive Cases: An Indian Experience. Ann. Oncol. 2016, 27, 1–2. [Google Scholar]
- Ramesh, A.; Kambhampati, C.; Monson, J.; Drew, P. Artificial Intelligence in Medicine. Ann. R. Coll. Surg. Engl. 2004, 86, 334–338. [Google Scholar] [CrossRef] [PubMed]
- Luo, J.; Wu, M.; Gopukumar, D.; Zhao, Y. Big Data Application in Biomedical Research and Health Care: A Literature Review. Biomed. Inform. Insights 2016, 8, 1–10. [Google Scholar] [CrossRef]
- Lin, W.; Dou, W.; Zhou, Z.; Liu, C. A cloud-based framework for Home-diagnosis service over big medical data. J. Syst. Softw. 2015, 102, 192–206. [Google Scholar] [CrossRef]
- Wang, W.; Krishnan, E. Big Data and Clinicians: A Review on the State of the Science. JMIR Med. Inform. 2014, 2, e1. [Google Scholar] [CrossRef]
- Qiu, J.; Wu, Q.; Ding, G.; Xu, Y.; Feng, S. A survey of machine learning for big data processing. EURASIP J. Adv. Signal Process. 2016, 2016, 67. [Google Scholar] [CrossRef]
- Krichen, M.; Ammi, M.; Mihoub, A.; Almutiq, M. Blockchain for Modern Applications: A Survey. Sensors 2022, 22, 5274. [Google Scholar] [CrossRef]
- Iftikhar, Z.; Javed, Y.; Zaidi, S.; Shah, M.; Khan, Z.I.; Mussadiq, S.; Abbasi, K. Privacy Preservation in Resource-Constrained IoT Devices Using Blockchain—A Survey. Electronics 2021, 10, 1732. [Google Scholar] [CrossRef]
- Imran, M. Comprehensive Survey of IoT, Machine Learning, and Block Chain for Health Care Applications: A Topical Assessment for Pandemic Preparedness, Challenges, and Solutions. Electronics 2021, 10, 2501. [Google Scholar] [CrossRef]
- Shi, S.; He, D.; Li, L.; Kumar, N.; Khan, M.K.; Choo, K.K. Applications of blockchain in ensuring the security and privacy of electronic health record systems: A survey. Comput. Secur. 2020, 97, 101966. [Google Scholar] [CrossRef] [PubMed]
- Ratta, P.; Kaur, A.; Sharma, S.; Shabaz, M.; Dhiman, G. Application of Blockchain and Internet of Things in Healthcare and Medical Sector: Applications, Challenges, and Future Perspectives. Hindawi J. Food Qual. 2021, 2021, 7608296. [Google Scholar] [CrossRef]
- Jahantigh, M.N. Integration of Internet of Things and cloud computing: A systematic survey. IET Commun. 2020, 14, 165–176. [Google Scholar] [CrossRef]
- Chenthara, S.; Ahmed, K.; Wang, H.; Whittaker, F. Security and Privacy-Preserving Challenges of e-Health Solutions in Cloud Computing. IEEE Access 2019, 7, 74361–74382. [Google Scholar] [CrossRef]
- Dang, L.M.; Piran, J.; Han, D.; Min, K.; Moon, H. A Survey on Internet of Things and Cloud Computing for Healthcare. Electronics 2019, 8, 768. [Google Scholar] [CrossRef]
- Selvaraju, R.R.; Cogswell, M.; Das, A.; Vedantam, R.; Parikh, D.; Batra, D. Grad-cam: Visual explanations from deep networks via gradient-based localization. In Proceedings of the International Conference on Computer Vision (ICCV), Venice, Italy, 22–29 October 2017; IEEE: Piscataway, NJ, USA, 2017; pp. 618–626. [Google Scholar]
- Armato, S.G.; McLennan, G.; Bidaut, L.; McNitt-Gray, M.F.; Meyer, C.R.; Reeves, A.P.; Zhao, B.; Aberle, D.R.; Henschke, C.I.; Hoffman, E.A.; et al. The Lung Image Database Consortium (LIDC) and Image Database Resource Initiative (IDRI): A Completed Reference Database of Lung Nodules on CT Scans. Med. Phys. 2011, 38, 915–931. [Google Scholar] [CrossRef]
- Jiang, X.; Coffee, M.; Bari, A.; Wang, J.; Jiang, X.; Huang, J.; Shi, J.; Dai, J.; Cai, J.; Zhang, T.; et al. Towards an Artificial Intelligence Framework for Data-Driven Prediction of Coronavirus Clinical Severity. Comput. Mater. Contin. 2020, 62, 537–551. [Google Scholar] [CrossRef]
- Alakus, T.B.; Turkoglu, I. Comparison of deep learning approaches to predict COVID-19 infection. Chaos Solitons Fractals 2020, 140, 110120. [Google Scholar] [CrossRef]
- Narin, A.; Kaya, C.; Pamuk, Z. Automatic detection of coronavirus disease (COVID-19) using X-ray images and deep convolutional neural networks. Pattern Anal. Appl. 2021, 24, 1207–1220. [Google Scholar] [CrossRef]
- Zhang, J.; Xie, Y.; Li, Y.; Shen, C.; Xia, Y. COVID-19 Screening on Chest X-ray Images Using Deep Learning based Anomaly Detection. arXiv 2020, arXiv:2003.12338v1. [Google Scholar]
- Alqudah, A.M.; Qazan, S.; Alqudah, A. Automated Systems for Detection of COVID-19 Using Chest X-ray Images and Lightweight Convolutional Neural Networks. Available online: https://assets.researchsquare.com/files/rs-24305/v1/2eaad4f3-e08b-4726-ab8c-0298a586d83a.pdf?c=1631833615 (accessed on 25 March 2022).
- Jamil, M.; Hussain, I. Automatic Detection of COVID-19 Infection from Chest X-ray using Deep Learning. medRxiv 2020. [Google Scholar] [CrossRef]
- Afshar, P.; Heidarian, S.; Naderkhani, F.; Oikonomou, A.; Plataniotis, K.N.; Mohammadi, A. COVID-CAPS: A Capsule Network-based Framework for Identification of COVID-19 cases from X-ray Images. arXiv 2020, arXiv:2004.02696v2. [Google Scholar] [CrossRef]
- de Moraes Batista, A.F.; Miraglia, J.L.; Rizzi Donato, T.H.; Porto Chiavegatto Filho, A.D. COVID-19 diagnosis prediction in emergency care patients: A machine learning approach. bioRxiv 2020. [Google Scholar] [CrossRef]
- Schwab, P.; Schütte, A.D.; Dietz, B.; Bauer, S. Pred COVID-19: A systematic study of clinical predictive models for coronavirus disease 2019. arXiv 2020, arXiv:2005.08302. [Google Scholar]
- Kumar, P.; Kumari, S. Detection of Coronavirus Disease (COVID-19) Based on Deep Features. 2020, p. 9. Available online: https://www.Preprints.Org/Manuscript/202003.0300/V1 (accessed on 25 March 2022).
- Sharma, L.; Gupta, G.; Jaiswal, V. Classification and development of tool for heart diseases (MRI images) using machine learning. In Proceedings of the 2016 Fourth International Conference on Parallel, Distributed and Grid Computing (PDGC), Waknaghat, India, 22–24 December 2016; IEEE: Piscataway, NJ, USA, 2016; pp. 219–224. [Google Scholar]
- Ghassemi, N.; Shoeibi, A.; Rouhani, M. Deep neural network with generative adversarial networks pre-training for brain tumor classification based on MR images. Biomed. Signal Process. Control. 2020, 57, 101678. [Google Scholar] [CrossRef]
- MTalo, M.; Yildirim, O.; Baloglu, U.B.; Aydin, G.; Acharya, U.R. Convolutional neural networks for multi-class brain disease detection using MRI images. Comput. Med. Imaging Graph. 2019, 78, 101673. [Google Scholar]
- Ghassemi, N.; Shoeibi, A.; Rouhani, M.; Hosseini-Nejad, H. Epileptic seizures detection in eeg signals using tqwt and ensemble learning. In Proceedings of the 2019 9th International Conference on Computer and Knowledge Engineering (ICCKE), Mashhad, Iran, 24–25 October 2019; IEEE: Piscataway, NJ, USA, 2019; pp. 403–408. [Google Scholar]
- Acharya, U.R.; Oh, S.L.; Hagiwara, Y.; Tan, J.H.; Adeli, H. Deep convolutional neural network for the automated detection and diagnosis of seizure using EEG signals. Comput. Biol. Med. 2018, 100, 270–278. [Google Scholar] [CrossRef]
- Mohammadpoor, M.; Shoeibi, A.; Zare, H.; Shojaee, H. A hierarchical classification method for breast tumor detection. Iran. J. Med. Phys. 2016, 13, 261–268. [Google Scholar]
- Arefan, D.; Mohamed, A.A.; Berg, W.A.; Zuley, M.L.; Sumkin, J.H.; Wu, S. Deep learning modeling using normal mammograms for predicting breast cancer risk. Med. Phys. 2020, 47, 110–118. [Google Scholar] [CrossRef]
- Khuzani, A.Z.; Heidari, M.; Shariati, S.A. COVID-classifier: An automated machine learning model to assist in the diagnosis of COVID-19 infection in chest X-ray images. medRxiv 2020. [Google Scholar]
- Mei, X.; Lee, H.-C.; Diao, K.-Y.; Huang, M.; Lin, B.; Liu, C.; Xie, Z.; Ma, Y.; Robson, P.M.; Chung, M.; et al. Artificial intelligence–enabled rapid diagnosis of patients with COVID-19. Nat. Med. 2020, 26, 1224–1228. [Google Scholar] [CrossRef] [PubMed]
- Esteva, A.; Kuprel, B.; Novoa, R.A.; Ko, J.; Swetter, S.M.; Blau, H.M.; Thrun, S. Dermatologist-level classification of skin cancer with deep neural networks. Nature 2017, 542, 115–118. [Google Scholar] [CrossRef] [PubMed]
- Mazurowski, M.A.; Buda, M.; Saha, A.; Bashir, M.R. Deep learning in radiology: An overview of the concepts and a survey of the state of the art with focus on MRI. J. Magn. Reson. Imaging 2019, 49, 939–954. [Google Scholar] [CrossRef]
- Malhotra, P.; Vig, L.; Shroff, G.; Agarwal, P. Long Short Term Memory Networks for Anomaly Detection in Time Series. In Proceedings of the ESANN 2015, Bruges, Belgium, 22–24 April 2014; Presses University de Louvain: Louvain-la-Neuve, Belgium, 2015. [Google Scholar]
- Hochreiter, S.; Schmidhuber, J. Long short-term memory. Neural Comput. 1997, 9, 1735–1780. [Google Scholar] [CrossRef]
- Ma, X.; Tao, Z.; Wang, Y.; Yu, H.; Wang, Y. Long short-term memory neural network for traffic speed prediction using remote microwave sensor data. Transp. Res. Part C Emerg. Technol. 2015, 54, 187–197. [Google Scholar] [CrossRef]
- Cai, M.; Liu, J. Maxout neurons for deep convolutional and LSTM neural networks in speech recognition. Speech Commun. 2016, 77, 53–64. [Google Scholar] [CrossRef]
- Farzad, A.; Mashayekhi, H.; Hassanpour, H. A comparative performance analysis of different activation functions in LSTM networks for classification. Neural Comput. Appl. 2019, 31, 2507–2521. [Google Scholar] [CrossRef]
- Kawakami, K. Supervised Sequence Labelling with Recurrent Neural Networks. Ph.D. Dissertation, Carnegie Mellon University, Pittsburgh, PA, USA, 2008. [Google Scholar]
- Mou, L.; Ghamisi, P.; Zhu, X.X. Deep Recurrent Neural Networks for Hyperspectral Image Classification. IEEE Trans. Geosci. Remote Sens. 2017, 55, 3639–3655. [Google Scholar] [CrossRef]
- Rao, A.; Spasojevic, N. Actionable and political text classification using word embeddings and LSTM. arXiv 2016, arXiv:1607.02501. Available online: http://arxiv.org/abs/1607.02501 (accessed on 30 March 2022).
- Yuan, M.; Wu, Y.; Lin, L. Fault diagnosis and remaining useful life estimation of aero engine using LSTM neural network. In Proceedings of the 2016 IEEE International Conference on Aircraft Utility Systems (AUS), Beijing, China, 10–12 October 2016; pp. 135–140. [Google Scholar]
- Yang, J.; Guo, Y.; Zhao, W. Long short-term memory neural network based fault detection and isolation for electro-mechanical actuators. Neuro Comput. 2019, 360, 85–96. [Google Scholar] [CrossRef]
- Yi, X.; Walia, E.; Babyn, P. Generative adversarial network in medical imaging: A review. Med. Image Anal. 2019, 58, 101552. [Google Scholar] [CrossRef] [PubMed]
- Wolterink, J.M.; Leiner, T.; Viergever, M.A.; Isgum, I. Generative Adversarial Networks for Noise Reduction in Low-Dose CT. IEEE Trans. Med. Imaging 2017, 36, 2536–2545. [Google Scholar] [CrossRef] [PubMed]
- Kohl, S.; Bonekamp, D.; Schlemmer, H.-P.; Yaqubi, K.; Hohenfellner, M.; Hadaschik, B.; Radtke, J.-P.; Maier-Hein, K. Adversarial networks for the detection of aggressive prostate cancer. arXiv 2017, arXiv:1702.08014. Available online: http://arxiv.org/abs/1702.08014 (accessed on 30 March 2022).
- Haarburger, C.; Horst, N.; Truhn, D.; Broeckmann, M.; Schrading, S.; Kuhl, C.; Merhof, D.D. Multiparametric magnetic resonance image synthesis using generative adversarial networks. In Proceedings of the Eurographics Workshop on Visual Computing for Biology and Medicine, Brno, Czech Republic, 26 December 2019. [Google Scholar]
- Greenhalgh, T.; Koh, G.C.H.; Car, J. COVID-19: A remote assessment in primary care. BMJ 2020, 368, m1182. [Google Scholar] [CrossRef]
- Liu, X.; Guo, S.; Yang, B.; Ma, S.; Zhang, H.; Li, J.; Sun, C.; Jin, L.; Li, X.; Yang, Q.; et al. Automatic Organ Segmentation for CT Scans Based on Super-Pixel and Convolutional Neural Networks. J. Digit. Imaging 2018, 31, 748–760. [Google Scholar] [CrossRef]
- Gharbi, M.; Chen, J.; Barron, J.T.; Hasinoff, S.W.; Durand, F. Deep bilateral learning for real-time image enhancement. ACM Trans. Graph. 2017, 36, 118. [Google Scholar] [CrossRef]
- Bouhassoune, I.; Chaibi, H.; Saadane, R.; Chehri, A. Performance of On-Skin RFID Miniaturized Dual Loop Tag for Body-Centric Applications. In Human Centred Intelligent Systems. KES-HCIS 2021. Smart Innovation, Systems and Technologies; Zimmermann, A., Howlett, R.J., Jain, L.C., Schmidt, R., Eds.; Springer: Singapore, 2021; Volume 244. [Google Scholar] [CrossRef]
- Wu, J.T.; Leung, K.; Leung, G.M. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: A modelling study. Lancet 2020, 26, 506–510. [Google Scholar] [CrossRef] [Green Version]
- TNyíri, T.; Kiss, A. Novel Ensembling Methods for Dermatological Image Classification. In Proceedings of the International Conference on Theory and Practice of Natural Computing, Dublin, Ireland, 12–14 December 2018; Springer: Cham, Switzerland, 2018; pp. 438–448. [Google Scholar]
- Ahmed, I.; Chehri, A.; Jeon, G. A Sustainable Deep Learning-Based Framework for Automated Segmentation of COVID-19 Infected Regions: Using U-Net with an Attention Mechanism and Boundary Loss Function. Electronics 2022, 11, 2296. [Google Scholar] [CrossRef]
- Bi, L.; Kim, J.; Ahn, E.; Feng, D. Automatic skin lesion analysis using large-scale dermoscopy images and deep residual networks. arXiv 2017, arXiv:1703.04197. Available online: https://arxiv.org/abs/1703.04197 (accessed on 5 April 2022).
- Ravi, D.; Wong, C.; Deligianni, F.; Berthelot, M.; Andreu-Perez, J.; Lo, B.; Yang, G.-Z. Deep Learning for Health Informatics. IEEE J. Biomed. Health Inform. 2017, 21, 4–21. [Google Scholar] [CrossRef] [PubMed]
- Chamola, V.; Hassija, V.; Gupta, V.; Guizani, M. A Comprehensive Review of the COVID-19 Pandemic and the Role of IoT, Drones, AI, Blockchain, and 5G in Managing its Impact. IEEE Access 2020, 8, 90225–90265. [Google Scholar] [CrossRef]
- Mohamadou, Y.; Halidou, A.; Kapen, P.T. A review of mathematical modeling, artificial intelligence and datasets used in the study, prediction and management of COVID-19. Appl. Intell. 2020, 50, 3913–3925. [Google Scholar] [CrossRef] [PubMed]
- Sufian, A.; Ghosh, A.; Sadiq, A.S.; Smarandache, F. A Survey on Deep Transfer Learning to Edge Computing for Mitigating the COVID-19 Pandemic. J. Syst. Arch. 2020, 108, 101830. [Google Scholar] [CrossRef]
- Deshpande, G.; Schuller, B. An overview on audio, signal, speech, & language processing for COVID-19. arXiv 2020, arXiv:2005.08579. [Google Scholar]
- Lalmuanawma, S.; Hussain, J.; Chhakchhuak, L. Applications of machine learning and artificial intelligence for COVID-19 (SARS-CoV-2) pandemic: A review. Chaos Solitons Fractals 2020, 139, 110059. [Google Scholar] [CrossRef]
- Naudé, W. Artificial intelligence vs COVID-19: Limitations, constraints and pitfalls. AI Soc. 2020, 35, 761–765. [Google Scholar] [CrossRef]
- Mohammed, H.A.; Abdulkareem, A.A.; Zardawi, F.M.; Gul, S.S. Determination of the Accuracy of Salivary Biomarkers for Periodontal Diagnosis. Diagnostics 2022, 12, 2485. [Google Scholar] [CrossRef]
- Sedik, A. Deploying Machine and Deep Learning Models for Efficient Data-Augmented Detection of COVID-19 Infections. Viruses 2020, 12, 769. [Google Scholar] [CrossRef]
- Liu, Z.; Shi, Y.; Yang, B. Open Innovation in Times of Crisis: An Overview of the Healthcare Sector in Response to the COVID-19 Pandemic. J. Open Innov. Technol. Mark. Complex. 2022, 8, 21. [Google Scholar] [CrossRef]
- Su, R.; Obrenovic, B.; Du, J.; Godinic, D.; Khudaykulov, A. COVID-19 Pandemic Implications for Corporate Sustainability and Society: A Literature Review. Int. J. Environ.Res. Public Health 2022, 19, 1592. [Google Scholar] [CrossRef] [PubMed]
- Hassan, R.; Ismail, W.N.; Chowdhury, A.; Hossain, S.; Huda, S.; Hassan, M.M. A framework of genetic algorithm-based CNN on multi-access edge computing for automated detection of COVID-19. J. Supercomput. 2022, 78, 10250–10274. [Google Scholar] [CrossRef] [PubMed]
- Sridhar, S.; Amutharaj, J.; Valsalan, P.; Arthi, B.; Ramkumar, S.; Mathupriya, S.; Rajendran, T.; Waji, Y.A. A Torn ACL Mapping in Knee MRI Images Using Deep Convolution Neural Network with Inception-v3. J. Health Eng. 2022, 2022, 7872500. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Chung, S.W. Deep Learning for Orthopedic Disease Based on Medical Image Analysis: Present and Future. Appl. Sci. 2022, 12, 681. [Google Scholar] [CrossRef]
- Shin, H. Development of convolutional neural network model for diagnosing tear of anterior cruciate ligament using only one knee magnetic resonance image. Medicine 2022, 101, 44. [Google Scholar] [CrossRef] [PubMed]
- Joshi, K.; Suganthi, K. Anterior Cruciate Ligament Tear Detection Based on Deep Convolutional Neural Network. Diagnostics 2022, 12, 2314. [Google Scholar] [CrossRef]
- Rahim, M.J. Automated Knee MR Images Segmentation of Anterior Cruciate Ligament Tears. Sensors 2022, 22, 1552. [Google Scholar] [CrossRef]
- Abdul razzaq, A.A.; Al-Douri, A.T.; Hamad, A.A.; Jaber, M.M.; Meraf, Z. Assessing Deep Learning Techniques for the Recognition of Tropical Disease in Images from Parasitological Exams. Bioinorg. Chem. Appl. 2022, 2022, 2682287. [Google Scholar] [CrossRef]
- Liu, Z.Y.-C.; Chamberlin, A.J.; Tallam, K.; Jones, I.J.; Lamore, L.L.; Bauer, J.; Bresciani, M.; Wolfe, C.M.; Casagrandi, R.; Mari, L.; et al. Deep Learning Segmentation of Satellite Imagery Identifies Aquatic Vegetation Associated with Snail Intermediate Hosts of Schistosomiasis in Senegal, Africa. Remote Sens. 2022, 14, 1345. [Google Scholar] [CrossRef]
- Van der Schaar, M.; Alaa, A. How artificial intelligence and machine learning can help health-care systems respond to COVID-19. Mach. Learn. 2021, 110, 1–14. [Google Scholar] [CrossRef]
- Ahmad, I.; Wang, X.; Zhu, M.; Wang, C.; Pi, Y.; Khan, J.A.; Li, G. EEG-based epileptic seizure detection via machine/deep learning approaches: A Systematic Review. Comput. Intell. Neurosci. 2022, 2020, 6486570. [Google Scholar] [CrossRef] [PubMed]
- Abbas, A.; Abdelsamea, M.M.; Gaber, M.M. Classification of COVID-19 in chest X-ray images using DeTraC deep convolutional neural network. arXiv 2020, arXiv:2003.13815. [Google Scholar] [CrossRef] [PubMed]
- Hu, Z.; Ge, Q.; Li, S.; Boerwincle, E.; Jin, L.; Xiong, M. Forecasting and evaluating intervention of COVID-19 in the World. arXiv 2020, arXiv:2003.09800. [Google Scholar]
- Chen, Y.; Li, C.; Wang, H. Big Data and Predictive Analytics for Business Intelligence: A Bibliographic Study (2000–2021). Forecasting 2022, 4, 767–786. [Google Scholar] [CrossRef]
- Gozes, O.; Frid-Adar, M.; Greenspan, H.; Browning, P.D.; Zhang, H.; Ji, W.; Bernheim, A.; Siegel, E. Rapid AI Development Cycle for the Coronavirus (COVID-19) Pandemic: Initial Results for Automated Detection & Patient Monitoring using Deep Learning CT Image Analysis. arXiv 2020, arXiv:2003.05037. [Google Scholar]
- Pinter, G.; Felde, I.; Mosavi, A.; Ghamisi, P.; Gloaguen, R. COVID-19 Pandemic Prediction for Hungary;A Hybrid Machine Learning Approach. Mathematics 2020, 8, 890. [Google Scholar] [CrossRef]
- Saleem, F.; AL-Ghamdi, A.S.A.-M.; Alassafi, M.O.; AlGhamdi, S.A. Machine Learning, Deep Learning, and Mathematical Models to Analyze Forecasting and Epidemiology of COVID-19: A Systematic Literature Review. Int. J.Environ. Res. Public Health 2022, 19, 5099. [Google Scholar] [CrossRef]
- Chenthamarakshan, V.; Das, P.; Padhi, I.; Strobelt, H.; Lim, K.W.; Hoover, B.; Hoffman, S.C.; Mojsilovic, A. Target-specific and selective drug design for COVID-19 using deep generative models. arXiv 2020, arXiv:2004.01215. [Google Scholar]
- McKinney, S.M.; Sieniek, M.; Godbole, V.; Godwin, J.; Antropova, N.; Ashrafian, H.; Back, T.; Chesus, M.; Corrado, G.S.; Darzi, A.; et al. International evaluation of an AI system for breast cancer screening. Nature 2020, 577, 89–94. [Google Scholar] [CrossRef]
- Patel, T.A.; Puppala, M.; Ogunti, R.O.; Ensor, J.E.; He, T.; Shewale, J.B.; Ankerst, D.P.; Kaklamani, V.G.; Rodriguez, A.A.; Wong, S.T.C.; et al. Correlating mammographic and pathologic findings in clinical decision support using natural language processing and data mining methods. Cancer 2017, 123, 114–121. [Google Scholar] [CrossRef]
- Chambers, D.; Cantrell, A.J.; Johnson, M.; Preston, L.; Baxter, S.K.; Booth, A.; Turner, J. Digital and online symptom checkers and health assessment/triage services for urgent health problems: Systematic review. BMJ Open 2019, 9, e027743. [Google Scholar] [CrossRef]
- Sensely: An Integrated Payer/Provider Wanted to Intervene in a Timelier Manner with Its Chronic Heart Failure (CHF) Patients. 11 October 2019. Available online: https://www.sensely.com/wp-content/uploads/2019/10/SenselyCHFCaseStudy.pdf (accessed on 19 May 2022).
- Haddad, T.C.; Helgeson, J.; Pomerleau, K.; Makey, M.; Lombardo, P.; Coverdill, S.; Urman, A.; Rammage, M.; Goetz, M.P.; LaRusso, N. Impact of a cognitive computing clinical trial matching system in an ambulatory oncology practice. J. Clin. Oncol. 2018, 36, 6550. [Google Scholar] [CrossRef]
- Corcoran, C.M.; Carrillo, F.; Fernández-Slezak, D.; Bedi, G.; Klim, C.; Javitt, D.C.; Bearden, C.E.; Cecchi, G.A. Prediction of psychosis across protocols and risk cohorts using automated language analysis. World Psychiatry 2018, 17, 67–75. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Fauw, J.; Ledsam, J.R.; Romera-Paredes, B.; Nikolov, S.; Tomasev, N.; Blackwell, S.; Askham, H.; Glorot, X.; O’Donoghue, B.; Visentin, D.; et al. Clinically applicable deep learning for diagnosis and referral in retinal disease. Nat. Med. 2018, 24, 1342–1350. [Google Scholar] [CrossRef] [PubMed]
- Kristensen, S.E.; Mosgaard, B.J.; Rosendahl, M.; Dalsgaard, T.; Bjørn, S.F.; Frøding, L.P.; Kehlet, H.; Høgdall, C.K.; Lajer, H. Robot-assisted surgery in gynecological oncology: Current status and controversies on patient benefits, cost and surgeon conditions—A systematic review. Acta Obstet. Gynecol. Scand. 2017, 96, 274–285. [Google Scholar] [CrossRef]
- Labovitz, D.L.; Shafner, L.; Gil, M.R.; Virmani, D.; Hanina, A.; Holt, T.A.; Dalton, A.; Marshall, T.; Fay, M.; Qureshi, N.; et al. Using Artificial Intelligence to Reduce the Risk of Nonadherence in Patients on Anticoagulation Therapy. Stroke 2017, 48, 1416–1419. [Google Scholar] [CrossRef] [PubMed]
- Bain, E.E.; Shafner, L.; Walling, D.P.; Othman, A.A.; Chuang-Stein, C.; Hinkle, J.; Hanina, A. Use of a Novel Artificial Intelligence Platform on Mobile Devices to Assess Dosing Compliance in a Phase 2 Clinical Trial in Subjects With Schizophrenia. JMIR mHealth uHealth 2017, 5, e18. [Google Scholar] [CrossRef] [PubMed]
- Christiansen, M.P.; Garg, S.K.; Brazg, R.; Bode, B.W.; Bailey, T.S.; Slover, R.H.; Sullivan, A.; Huang, S.; Shin, J.; Lee, S.W.; et al. Accuracy of a Fourth-Generation Subcutaneous Continuous Glucose Sensor. Diabetes Technol. Ther. 2017, 19, 446–456. [Google Scholar] [CrossRef]
- Lakhani, P.; Sundaram, B. Deep Learning at Chest Radiography: Automated Classification of Pulmonary Tuberculosis by Using Convolutional Neural Networks. Radiology 2017, 284, 574–582. [Google Scholar] [CrossRef]
- Qidwai, U.; Chaudhry, J.; Jabbar, S.; Zeeshan HM, A.; Janjua, N.; Khalid, S. Using casual reasoning for anomaly detection among ECG live data streams in ubiquitous healthcare monitoring systems. J. Ambient. Intell. Humaniz. Comput. 2019, 10, 4085–4097. [Google Scholar] [CrossRef]
- Guidi, G.; Iadanza, E.; Pettenati, M.C.; Milli, M.; Pavone, F.; Gentili, G.B. Heart failure artificial intelligence-based computer aided diagnosis telecare system. In Proceedings of the International Conference on Smart Homes and Health Telematics, Artimino, Italy, 13–15 June 2012; Springer: Berlin/Heidelberg, Germany, 2012; pp. 278–281. [Google Scholar]
- Pham, Q.V.; Nguyen, D.C.; Huynh-The, T.; Hwang, W.J.; Pathirana, P.N. Artificial intelligence (ai) and Bigdata for coronavirus (COVID-19) pandemic: A survey on the state of-the-arts. IEEE Access 2020, 8, 130820. [Google Scholar] [CrossRef] [PubMed]
- Naude, W. Artificial Intelligence versus COVID-19 in Developing Countries. Available online: https://www.wider.unu.edu/sites/default/files/Publications/Background-note/PDF/bn2020-4-ai-vs-covid-19-developing-%20countries.pdf (accessed on 5 April 2022).
- Unberath, M.; Ghobadi, K.; Levin, S.; Hinson, J.; Hager, G.D. Artificial intelligence-based clinical decision support for COVID-19—Where art thou? arXiv 2020, arXiv:2006.03434. [Google Scholar] [CrossRef]
- Ulhaq, A.; Khan, A.; Gomes, D.; Paul, M. Computer vision for COVID-19 control: A survey. arXiv 2020, arXiv:2004.09420. [Google Scholar] [CrossRef] [PubMed]
- Shaikh, F.; Andersen, M.B.; Sohail, M.R.; Mulero, F.; Awan, O.; Dupont-Roettger, D.; Kubassova, O.; Bisdas, S. Current landscape of imaging and the potential role for artificial intelligencein the management of COVID-19. Curr. Probl. Indiagn. Radiol. 2021, 50, 430–435. [Google Scholar] [CrossRef] [PubMed]
- Sipior, J.C. Considerations for development and use of AI in response to COVID-19. Int. J. Inf. Manag. 2020, 55, 102170. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.; Yoon, S.N. Application of Artificial Intelligence-Based Technologies in the Healthcare Industry: Opportunities and Challenges. Int. J. Environ. Res. Public Health 2021, 18, 271. [Google Scholar] [CrossRef] [PubMed]
- Vinaya kumar, R.; Alazab, M.; Srinivasan, S.; Pham, Q.-V.; Padannayil, S.K.; Simran, K. A Visualized Botnet Detection System Based Deep Learning for the Internet of Things Networks of Smart Cities. IEEE Trans. Ind. Appl. 2020, 56, 4436–4456. [Google Scholar] [CrossRef]
- Tsai, C.-W.; Lai, C.-F.; Chao, H.-C.; Vasilakos, A.V. Bigdata analytics: A survey. J. Bigdata 2015, 2, 21. [Google Scholar]
- Sann, R.; Lai, P.-C.; Liaw, S.-Y.; Chen, C.-T. Predicting Online Complaining Behavior in the Hospitality Industry: Applicationof Big Data Analytics to Online Reviews. Sustainability 2022, 14, 1800. [Google Scholar] [CrossRef]
- Mehta, N.; Shukla, S. Pandemic Analytics: How Countries are Leveraging Big Data Analytics and Artificial Intelligence to Fight COVID-19? SN Comput. Sci. 2022, 3, 54. [Google Scholar] [CrossRef]
- Castorina, P.; Iorio, A.; Lanteri, D. Data analysis on corona virus spreading by macroscopic growth laws. arXiv 2020, arXiv:2003.00507. [Google Scholar]
- Peng, L.; Yang, W.; Zhang, D.; Zhuge, C.; Hong, L. Epidemic analysis of COVID-19 in China by dynamical modeling. arXiv 2020, arXiv:2002.06563. [Google Scholar]
- Özdemir, V.; Hekim, N. Birth of industry 5.0: Making sense of big data with artificial intelligence, “the internet ofthings” and next- generation technology policy. OMICS A J. Integr. Biol. 2018, 22, 65–76. [Google Scholar] [CrossRef] [PubMed]
- Chae, S.; Kwon, S.; Lee, D. Predicting infectious disease using deep learning and Bigdata. Int. J. Environ. Res. Public Health 2018, 15, 1596. [Google Scholar] [CrossRef]
- Bansal, S.; Chowell, G.; Simonsen, L.; Vespignani, A.; Viboud, C. Bigdata for infectious disease surveillance and modeling. J. Infect. Dis. 2016, 214 (Suppl. S4), S375–S379. [Google Scholar] [CrossRef]
- Eisenstein, M. Infection forecasts powered by Bigdata. Nature 2018, 555, 7695. [Google Scholar] [CrossRef] [Green Version]
- Buckee, C. Improving epidemic surveillance and response: Bigdata is dead, long live Bigdata. Lancet Digit. Health 2020, 2, e218–e220. [Google Scholar] [CrossRef]
- Chehri, A.; Moutah, H.T. Survivable and Scalable Wireless Solution for E-health and E-emergency Applications. EICS4Med. 2011, 727, 25–29. [Google Scholar]
- Sarkar, B.K. Big data for secure healthcare system: A conceptual design. Complex Intell. Syst. 2017, 3, 133–151. [Google Scholar] [CrossRef]
- Kumar, R.; Tripathi, R. Scalable and secure access control policy for health-care system using Blockchain and enhanced Bell–LaPadula model. J. Ambient. Intell. Humaniz. Comput. 2021, 12, 2321–2338. [Google Scholar] [CrossRef]
- Sun, Y.; Zhang, R.; Wang, X.; Gao, K.; Liu, L. A decentralizing attribute-based signature for healthcare blockchain. In Proceedings of the 2018 27th International Conference on Computer Communication and Networks (ICCCN), Hangzhou, China, 30 July 2018–2 August 2018; IEEE: Piscataway, NJ, USA, 2018; pp. 1–9. [Google Scholar]
- Hylock, R.H.; Zeng, X. A blockchain framework for patient-centered health records and exchange (HealthChain): Evaluation and proof-of-concept study. J. Med. Internet Res. 2019, 21, e13592. [Google Scholar] [CrossRef] [PubMed]
- Chehri, A.; Mouftah, H.T. Internet of Things—Integrated IR-UWB technology for healthcare applications. Concurr. Comput. Pr. Exper. 2020, 32, e5454. [Google Scholar] [CrossRef]
- Zhuang, Y.; Sheets, L.R.; Shae, Z.; Chen, Y.W.; Tsai, J.J.P.; Shyu, C.R. Applying blockchain technology to enhance clinical trial recruitment. AMIA Annu. Proc. 2020, 2019, 1276–1285. [Google Scholar]
- Zhuang, Y.; Sheets, L.; Shae, Z.; Tsai, J.J.P.; Shyu, C.R. Applying blockchain technology for health information exchange and persistent monitoring for clinical trials. AMIA Annu. Symp. 2018, 2018, 1167–1175. [Google Scholar]
- Zhou, L.; Wang, L.; Sun, Y. Mistore: A blockchain-based medical insurance storage system. J. Med. Syst. 2018, 42, 149. [Google Scholar] [CrossRef] [PubMed]
- Tan, T.-E.; Anees, A.; Chen, C.; Li, S.; Xu, X.; Li, Z.; Xiao, Z.; Yang, Y.; Lei, X.; Ang, M.; et al. Retinal photograph-based deep learning algorithms for myopia and a blockchain platform to facilitate artificial intelligence medical research: A retrospective multicohort study. Lancet Digit. Health 2021, 3, e317–e329. [Google Scholar] [CrossRef]
- Kuo, T.T.; Gabriel, R.A.; Cidambi, K.R.; Ohno-Machado, L. Expectation Propagation Logistic Regression on permissioned block chain (Explorer Chain): Decentralized online health-care/genomics predictive model learning. J. Am. Med. Inform. Assoc. 2020, 27, 747–756. [Google Scholar] [CrossRef]
- Jin, X.L.; Zhang, M.; Zhou, Z.; Yu, X. Application of a blockchain platform to manage and secure personal genomic data: A case study of LifeCODE.ai in China. J. Med. Internet Res. 2019, 21, e13587. [Google Scholar] [CrossRef]
- Tseng, J.-H.; Liao, Y.-C.; Chong, B.; Liao, S.-W. Governance on the Drug Supply Chain via Gcoin Blockchain. Int. J. Environ. Res. Public Health 2018, 15, 1055. [Google Scholar] [CrossRef] [Green Version]
- Lazrag, H.; Chehri, A.; Saadane, R.; Rahmani, M.D. A Blockchain-Based Approach for Optimal and Secure Routing in Wireless Sensor Networks and IoT. In Proceedings of the 2019 15th International Conference on Signal-Image Technology & Internet-Based Systems (SITIS), Sorrento, Italy, 26–29 November 2019; pp. 411–415. [Google Scholar] [CrossRef]
- Roehrs, A.; da Costa, C.A.; Righi, R.D.R. OmniPHR: A distributed architecture model to integrate personal health records. J. Biomed. Inform. 2017, 71, 70–81. [Google Scholar] [CrossRef]
- Tian, H.; He, J.; Ding, Y. Medical Data Management on Blockchain with Privacy. J. Med. Syst. 2019, 43, 26. [Google Scholar] [CrossRef] [PubMed]
- Rahman, M.A.; Hossain, M.S.; Islam, M.S.; Alrajeh, N.A.; Muhammad, G. Secure and Provenance Enhanced Internet of Health Things Framework: A Blockchain Managed Federated Learning Approach. IEEE Access 2020, 8, 205071–205087. [Google Scholar] [CrossRef] [PubMed]
- Połap, D.; Srivastava, G.; Yu, K. Agent architecture of an intelligent medical system based on federated learning and blockchain technology. J. Inf. Secur. Appl. 2021, 58, 102748. [Google Scholar] [CrossRef]
- Bouhassoune, I.; Chehri, A.; Saadane, R.; Minaoui, K. Optimization of UHF RFID Five-Slotted Patch Tag Design Using PSO Algorithm for Biomedical Sensing Systems. Int. J. Environ. Res. Public Health 2020, 17, 8593. [Google Scholar] [CrossRef] [PubMed]
- Dhillon, V.; Metcalf, D.; Hooper, M. Blockchain in Health-Care. In Blockchain Enabled Applications; Apress: Berkeley, CA, USA, 2021; pp. 201–220. [Google Scholar]
- Dimitrov, D.V. Blockchain applications for health-care data management. Health-Care Inform. Res. 2019, 25, 51. [Google Scholar] [CrossRef] [PubMed]
- Chehri, A.; Jeon, G.; Rivest, F.; Mouftah, H.T. Evolution and Trends in Artificial Intelligence of Things Security: When Good Enough is Not Good Enough! IEEE Internet Things Mag. 2022, 5, 62–66. [Google Scholar] [CrossRef]
- Clauson, K.; Breeden, E.; Davidson, C.; Mackey, T. Leveraging Blockchain technology to enhance supply chain management in health-care: An exploration of challenges and opportunities in the health supply chain. Blockchain Health-Care Today 2018, 1, 1–2. [Google Scholar]
- Pandey, P.; Litoriya, R. Securing and authenticating health-care records through blockchain technology. Cryptologia 2020, 44, 341–356. [Google Scholar] [CrossRef]
- Siyal, A.; Junejo, A.; Zawish, M.; Ahmed, K.; Khalil, A.; Soursou, G. Applications of blockchain technology in medicine and health-care: Challenges and future perspectives. Cryptography 2019, 3, 3. [Google Scholar] [CrossRef] [Green Version]
- Odeh, A.; Keshta, I.; Al-Haija, Q.A. Analysis of Blockchain in the Healthcare Sector: Application and Issues. Symmetry 2022, 14, 1760. [Google Scholar] [CrossRef]
- Bouhassoune, I.; Saadane, R.; Chehri, A. Wireless Body Area Network Based on RFID System for Healthcare Monitoring: Progress and Architectures. In Proceedings of the 2019 15th International Conference on Signal-Image Technology & Internet-Based Systems (SITIS), Sorrento, Italy, 26–29 November 2019; pp. 416–421. [Google Scholar] [CrossRef]
- Ejaz, M.; Kumar, T.; Kovacevic, I.; Ylianttila, M.; Harjula, E. Health-BlockEdge: Bloc kchain-edge framework for reliable low-latency digital healthcare applications. Sensors 2021, 21, 2502. [Google Scholar] [CrossRef] [PubMed]
- De Aguiar, E.J.; Faiçal, B.S.; Krishnamachari, B.; Ueyama, J. A Survey of Block chain-Based Strategies for Healthcare. ACM Comput. Surv. 2020, 53, 1–27. [Google Scholar] [CrossRef]
- Mackey, T.; Kuo, T.; Gummadi, B.; Clauson, K.; Church, G.; Grishin, D.; Obbad, K.; Barkovich, R.; Palombini, M. ‘Fit-for-purpose?’–challenges and opportunities for applications of block chain technology in the future of healthcare. BMC Med. 2019, 17, 68. [Google Scholar] [CrossRef] [PubMed]
- Khatoon, A. A blockchain-based innovative contract system for healthcare management. Electronics 2020, 9, 94. [Google Scholar] [CrossRef]
- Onik, M.; Aich, S.; Yang, J.; Kim, C.; Kim, H. Block chain in Healthcare: Challenges and Solutions. In Big Data Analytics for Intelligent Healthcare Management; Academic Press: Cambridge, MA, USA, 2019; pp. 197–226. [Google Scholar]
- Agbo, C.C.; Mahmoud, Q.H.; Eklund, J.M. Block chain Technology in Healthcare: A Systematic Review. Healthcare 2019, 7, 56. [Google Scholar] [CrossRef]
- Bhuiyan, M.; Zaman, A.; Wang, T.; Wang, G.; Tao, H.; Hassan, M. Blockchain and Bigdata to transform health-care. In Proceedings of the International Conference on Data Processing and Applications, Guangdong, China, 12–14 May 2018; pp. 62–68. [Google Scholar]
- Daniel, J.; Sargolzaei, A.; Abdelghani, M.; Sargolzaei, S.; Amaba, B. Blockchain technology, cognitive computing, and health-care innovations. J. Adv. Inf. Technol. 2017, 8, 194–198. [Google Scholar]
- Rector, A.L.; Rogers, J.E.; Zanstra, P.E.; Van Der Haring, E. OpenGALEN: Open Source Medical Terminology and Tools. 2011. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1480228/ (accessed on 29 April 2017).
- McDonald, C.J. Open Source software in medical informatics—Why, how and what. Int. J. Med. Inform. 2003, 69, 175–184. [Google Scholar] [CrossRef]
- Mirth Corporation. 2011. Available online: http://www.mirthcorp.com (accessed on 29 April 2017).
- Hope, J. Biobazaar: The Open Source Revolution and Biotechnology; Harvard University Press: Cambridge, MA, USA, 2008. [Google Scholar]
- NHS England. Code4Health. 2017. Available online: https://www.england.nhs.uk/digitaltechnology/info-revolution/code4healt (accessed on 29 April 2017).
- ProtecodeSCCa. Health-Care Driven by Open Source Software. 2015. Available online: http://rippleosi.org/wp-content/uploads/2015/06/e-HealthWhitepaper-SCC.pdf (accessed on 29 April 2017).
- Code4Health. Welcome to Code4Health™. 2017. Available online: https://code4health.org (accessed on 29 April 2017).
- Webster, P.C. The rise of open-source electronic health records. Lancet 2011, 377, 1641–1642. [Google Scholar] [CrossRef]
- Neiman, J. OpenMRS Ebola Case Study: OpenMRS. 2016. Available online: http://openmrs.org/2016/08/openmrs-ebolacase-study (accessed on 11 June 2017).
- Care2X. Available online: http://www.care2x.org (accessed on 12 August 2022).
- Chehri, A. Energy-efficient modified DCC-MAC protocol for IoT in e-health applications. Internet Things 2021, 14, 100119. [Google Scholar] [CrossRef]
- Apache HTTP Server Project. Available online: http://httpd.apache.org (accessed on 5 August 2022).
- Mozilla Firefox Web Browser. Available online: http://www.mozilla.org/en-US/firefox/new (accessed on 5 August 2022).
- MySQL. Available online: http://www.mysql.com (accessed on 5 August 2022).
- PHP. Available online: http://www.php.net (accessed on 10 August 2022).
- GIMP. The GNU Image Manipulation Program. Available online: http://www.gimp.org (accessed on 10 August 2022).
- Mozilla Thunderbird. Available online: http://www.mozilla.org/en-US/thunderbird (accessed on 12 August 2022).
- Cloud Computing in the Health Care Industry. Available online: https://medium.com/@alex.raif86/cloud-computing-in-the-health-care-industry-744580a07868 (accessed on 15 August 2022).
- Available online: https://www.researchgate.net/figure/High-level-illustration-of-healthcare-cloud_fig6_320093536 (accessed on 15 August 2022).

| Year | Past Review Highlights | Reference |
|---|---|---|
| Artificial Intelligence | ||
| 2021 | Review to summarize the application of virtual and augmented reality technologies to orthopaedic surgery training and practice aims. | [31] |
| 2020 | Review aimed to provide an overview of potential applications of AI and Big Data in the global effort to manage the COVID-19 pandemic. | [32] |
| 2019 | Evolution of research in AI in health and medicine: A bibliometric study. | [33] |
| 2018 | Literature review depicting application of machine learning techniques and methods to solve orthopedic problems (covering articles of last two decades). | [34] |
| 2016 | IBM computing system Watson for oncology with Manipal Hospitals. | [35] |
| 2004 | AI-based technologies depicting innovations in medicine and healthcare industry. | [36] |
| 2016 | Big Data application review in bioinformatics, clinical informatics, imaging informatics, and public health informatics. | [37] |
| 2015 | Cloud framework to ensure concurrent and scalable medical record retrieval. | [38] |
| 2014 | Review on facilitating big data to predict hazards of disease incidence and improve primary care. | [39] |
| 2016 | Survey on research advancements in ML for Big Data processing. | [40] |
| 2022 | Review of blockchain technology in healthcare, finance, wireless networks, IoT, andsmart grids. | [41] |
| 2021 | Survey depicting various research works pertaining to deployment of block chain in Internet of Things (IoT). | [42] |
| 2021 | Comprehensive survey of emerging IoT technologies, machine learning, and blockchain for healthcare applications. | [43] |
| 2020 | Literature review of blockchain approaches for electronic health record systems. | [44] |
| 2019 | Review of block chain model implementation to existing and latest healthcare scenarios. | [45] |
| 2020 | Attempt to analyze combination of IoT and cloud computing for healthcare applications. | [46] |
| 2019 | Attempt to highlight research challenges to build a security model for EHR. | [47] |
| 2019 | Survey depicting development of IoT- and cloud computing-based healthcare applications. | [48] |
| Sl. No | Ref. | Category of Health Segment | Application Type | Year |
|---|---|---|---|---|
| 1 | [101,102,103,104] | AI in healthcare | Periodontal diagnosis, overview, literature review, genetic algorithm-based CNN for COVID detection | 2022 2020 |
| 2 | [105,106,107,108,109,110] | CNN-based knee MRI images mapping DL for orthopedic disease Anterior cruciate ligament tear detection based on deep CNN | 2022 | |
| 3 | [111] | DL techniques for recognition of tropical diseases in images | 2022 | |
| 4 | [112] | DL-based schistosomiasis in Africa and Senegal | 2022 | |
| 5 | [113] | Patient diagnosis and treatment activities | 2021 | |
| 6 | [114] | Epileptic seizure detection | ML and deep CNN for seizure detection in EEG signals | 2022 |
| 7 | [64,65] | 2019, 2018 | ||
| 8 | [115] | Pandemic detection and diagnosis | CNN-based framework using transfer learning d | 2020 |
| 9 | [116,117,118,119,120] | Auto encoder framework to model transmission dynamics, DL CT image analysis, and ML-DL models for COVID detection | 2020 | |
| 10 | [121] | Deep generative model (CogMol) to investigate protein structure of corona virus | 2020 | |
| 11 | [95] | Pandemic data analysis | IoT, block chain, and AI models | 2020 |
| 12 | [66,122,123] | Breast cancer | NLP-based mammography interpretation system | 2020, 2017 |
| 13 | [82] | Medical imaging | Generative adversarial networks in medical imaging applications for screening | 2020 |
| 14 | [62,63] | Brain tumor | DNN with generative adversarial neural networks for brain tumor detection | 2017, 2020 |
| 15 | [124] | Home diagnosis | ML-and NLP-based personalized home care and diagnosis | 2019 |
| 16 | [125] | Nursing | ML-based home nurse avatar | 2019 |
| 17 | [126] | Oncology clinical trial | ML-, DL-,andNLP-based IBM deploying Watson AI platform | 2018 |
| 18 | [127] | Psychiatric diagnosis | Predicting development of psychosis in people | 2018 |
| 19 | [128] | Opthalmology | ML for predicting eye diseases | 2018 |
| 20 | [129] | Robot-assisted surgery | Robotic prostatectomy, cardiac, oncology | 2017 |
| 21 | [130] | Cardiology | ML-based mobile platform on anticoagulation therapy | 2017 |
| 22 | [131] | Drugs distribution | ANN-based software to detect patient and drug for ingestion | 2017 |
| 23 | [132] | Diabetics | ML-based glucose monitoring system | 2017 |
| 24 | [133] | Tuberculosis | Alexa and GoogleNet CNNs for diagnosing tuberculosis | 2017 |
| 25 | [70] | Skin cancer detection | ANN and ML for cancer detection using skin lesions | 2017, 2019 |
| 26 | [134,135] | Cardiac arrest monitoring | ANN for monitoring heart conditions based on patient history | 2012, 2017 |
| 27 | [136,137,138,139,140,141] | COVID Pandemic Survey | AI (and Bigdata) for clinical decision support and management of COVID-19 | 2020, 2021 |
| 28 | [142] | Health care | AI applications in health care | 2021 |
| Sl. No | Paper | Category of Health Segment | Application Type | Year |
|---|---|---|---|---|
| 1 | [146,147] | Pandemic surveillance | Big Data analytics platform to estimate the risk of pandemic spreading and surveillance | 2022,2020 |
| 2 | [148] | COVID | Analysis of COVID-19 in China | 2020 |
| 3 | [149,150,151,152,153] | Infectious disease surveillance and healthcare | DL, Big Data analytics, AI, and IoT to monitor spread of bacteria, viruses, and pulmonary diseases | 2018, 2016, 2020 |
| 4 | [154] | Electronic health records | Big Data for risk estimation in cancer patients | 2011 |
| 5 | [155] | Safety and prediction | Big Data for secured healthcare | 2017 |
| Sl. No | Paper | Category of Health Segment | Application Type | Year |
|---|---|---|---|---|
| 1 | [175,179,180] | Healthcare applications | Block chain technology’s future challenges | 2022, 2019 |
| 2 | [181,182] | Patient Health care | Preserve patient information and data, such as blood tests, quality assessments, and estimates, in electronic health record formats | 2021, 2020 |
| 3 | [172,178] | Secured healthcare | Intelligent block chain framework for secured biomedical applications | 2020,2019 |
| 4 | [163] | Research on myopia treatment | Deep learning and block chain framework study | 2021 |
| 5 | [183] | Wide services to patients community | Block chain infrastructure challenges in future health care applications | 2020 |
| 6 | [170] | Secured healthcare | Provenance enhanced IoT and block chain framework | 2020 |
| 7 | [160,161,184] | Enhanced clinical trials | Block chain framework to ensure best clinical treatments, healthcare management | 2020, 2018 |
| 8 | [185,186] | Validation | Block chain enabling healthcare industries to obtain validated data of patients | 2019 |
| 9 | [157] | False content detection | Block chain ensures identification of false data to healthcare insurance companies | 2018 |
| 10 | [187] | Patient healthcare | Block chain and Big Data for transforming patient healthcare segments | 2018 |
| 11 | [162] | Medical insurance | Block chain-based genuine insurance claiming system | 2018 |
| 12 | [166,176] | Drugs distribution | Supply chain distribution framework for distributing drugs | 2018 |
| 13 | [188] | Healthcare Innovations | Block chain technology innovations for health care applications | 2017 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Siripurapu, S.; Darimireddy, N.K.; Chehri, A.; Sridhar, B.; Paramkusam, A.V. Technological Advancements and Elucidation Gadgets for Healthcare Applications: An Exhaustive Methodological Review-Part-I (AI, Big Data, Block Chain, Open-Source Technologies, and Cloud Computing). Electronics 2023, 12, 750. https://doi.org/10.3390/electronics12030750
Siripurapu S, Darimireddy NK, Chehri A, Sridhar B, Paramkusam AV. Technological Advancements and Elucidation Gadgets for Healthcare Applications: An Exhaustive Methodological Review-Part-I (AI, Big Data, Block Chain, Open-Source Technologies, and Cloud Computing). Electronics. 2023; 12(3):750. https://doi.org/10.3390/electronics12030750
Chicago/Turabian StyleSiripurapu, Sridhar, Naresh K. Darimireddy, Abdellah Chehri, B. Sridhar, and A. V. Paramkusam. 2023. "Technological Advancements and Elucidation Gadgets for Healthcare Applications: An Exhaustive Methodological Review-Part-I (AI, Big Data, Block Chain, Open-Source Technologies, and Cloud Computing)" Electronics 12, no. 3: 750. https://doi.org/10.3390/electronics12030750
APA StyleSiripurapu, S., Darimireddy, N. K., Chehri, A., Sridhar, B., & Paramkusam, A. V. (2023). Technological Advancements and Elucidation Gadgets for Healthcare Applications: An Exhaustive Methodological Review-Part-I (AI, Big Data, Block Chain, Open-Source Technologies, and Cloud Computing). Electronics, 12(3), 750. https://doi.org/10.3390/electronics12030750









