A Review on Risk Factors, Traditional Diagnostic Techniques, and Biomarkers for Pneumonia Prognostication and Management in Diabetic Patients
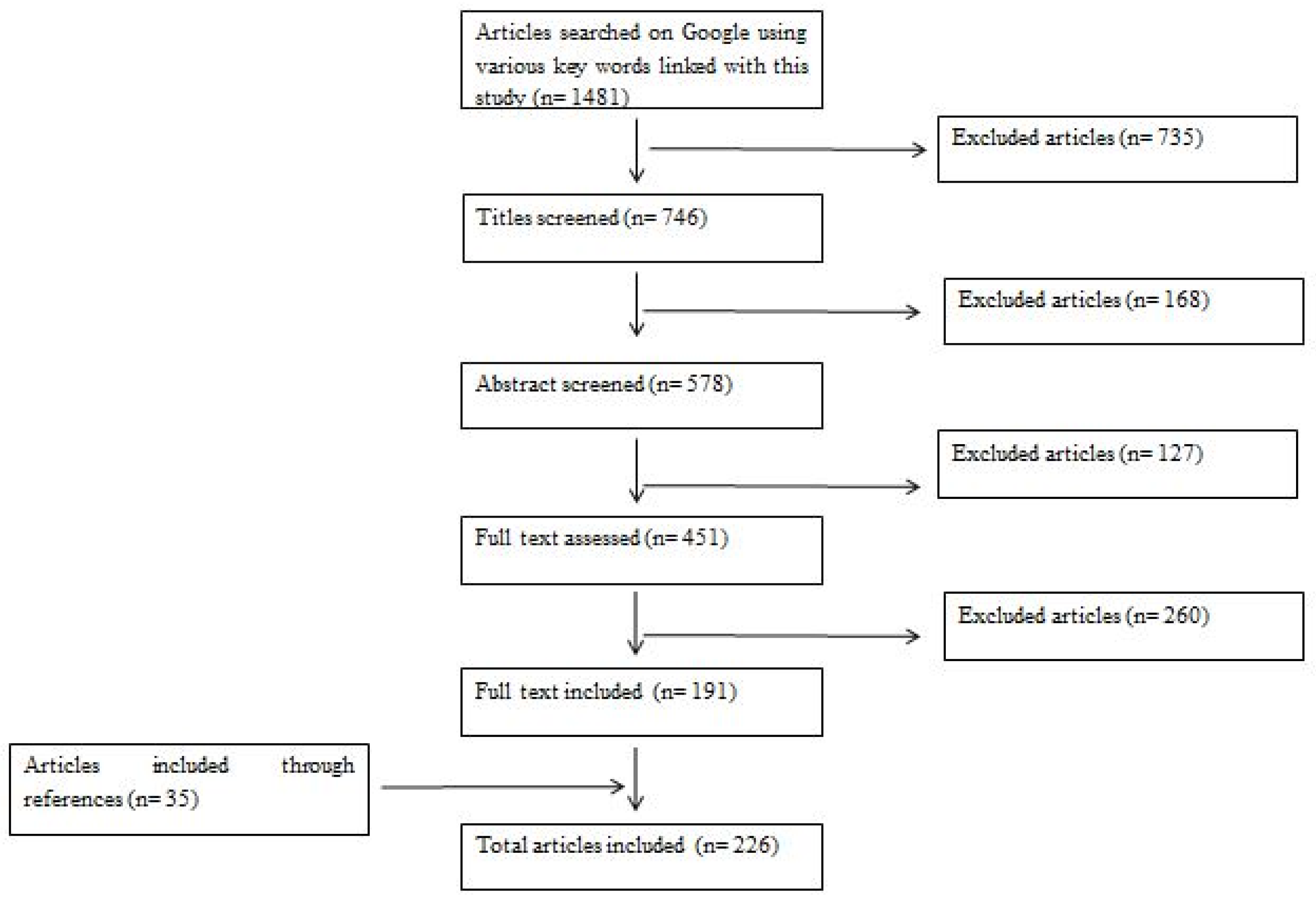
Abstract
:1. Introduction
2. Causes of Pneumonia
2.1. Typical Bacteria
2.2. Atypical Bacteria
2.3. Respiratory Viruses
2.4. Mycotic Causes
2.5. Parasitic Cause: Parasitic Pneumonia
2.5.1. Protozoal Pneumonia
2.5.2. Helminths in Respiratory Diseases
3. Risk Factors of Pneumonia Infection
3.1. Hyperglycemia
3.2. Glycemic Variability
3.3. Oxidative Stress
3.4. Glycation
3.5. Abnormal Complement
3.6. Abnormal Inflammatory Cytokines
3.7. Abnormal Mono- and Polymorphonuclear Leukocytes
3.8. Antibody Impairment or Reduced Antibody Response
3.9. Deficiency of Micronutrient
3.10. Metformin Use
3.11. Neuropathy
4. Clinical Predictors of Pneumonia
5. Systemic Symptoms and Signs
6. Types of Bacterial Pneumonia
6.1. Community-Acquired Pneumonia (CAP)
6.2. Nosocomial Pneumonia
6.2.1. Hospital-Acquired Pneumonia (HAP)
6.2.2. Ventilator-Associated Pneumonia (VAP)
6.2.3. HCAP (Healthcare-Associated Pneumonia)
6.2.4. Aspiration Pneumonia
7. Pathophysiology of Pneumonia
8. Diagnosis of Pneumonia
8.1. Common Laboratory Examination
8.1.1. Complete Blood Count (CBC) and Differential Leucocyte Count
8.1.2. Pro-Inflammatory Cytokines
8.1.3. Chemistry Panel
8.1.4. Sputum Smear and Culture
8.1.5. Bronchoalveolar Lavage (BAL)
8.1.6. Blood Culture
8.1.7. CD4 Counts
8.2. Chest X-Ray (CXR)
8.3. Computer Tomography (CT)
8.4. Additional Techniques
8.4.1. Legionella and Pneumococcus Urine Antigen Testing
8.4.2. ELISA and PCR
8.4.3. Beta-D-Glucan Testing
8.5. Lung Ultrasound
9. Biomarkers for Detection of CAP
10. Next-Generation Sequencing and Its Application in Pneumonia Diagnosis
11. COVID-19 and Pneumonia
12. Association Between HIV Infection, Corticosteroid Treatment for Rheumatic Disease, and Diabetes and Pneumonia Infection
13. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Hossain, M.J.; Al-Mamun, M.; Islam, M.R. Diabetes mellitus, the fastest growing global public health concern: Early detection should be focused. Health Sci. Rep. 2024, 7, e2004. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Galicia-Garcia, U.; Benito-Vicente, A.; Jebari, S.; Larrea-Sebal, A.; Siddiqi, H.; Uribe, K.B.; Ostolaza, H.; Martín, C. Pathophysiology of Type 2 Diabetes Mellitus. Int. J. Mol. Sci. 2020, 21, 6275. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Antar, S.A.; Ashour, N.A.; Sharaky, M.; Khattab, M.; Ashour, N.A.; Zaid, R.T.; Roh, E.J.; Elkamhawy, A.; Al-Karmalawy, A.A. Diabetes mellitus: Classification, mediators, and complications; A gate to identify potential targets for the development of new effective treatments. Biomed. Pharmacother. 2023, 168, 115734. [Google Scholar] [CrossRef] [PubMed]
- Berbudi, A.; Rahmadika, N.; Tjahjadi, A.I.; Ruslami, R. Type 2 Diabetes and its Impact on the Immune System. Curr. Diabetes Rev. 2020, 16, 442–449. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Marshall, J.S.; Warrington, R.; Watson, W.; Kim, H.L. An introduction to immunology and immunopathology. Allergy Asthma Clin. Immunol. 2018, 14 (Suppl. S2), 49. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Holt, R.I.G.; Cockram, C.S.; Ma, R.C.W.; Luk, A.O.Y. Diabetes and infection: Review of the epidemiology, mechanisms and principles of treatment. Diabetologia 2024, 67, 1168–1180. [Google Scholar] [CrossRef]
- Puca, E. Infections in immunocompromised patients from diabetes mellitus. Int. J. Health Sci. 2017, 5, 583–587. [Google Scholar]
- Chávez-Reyes, J.; Escárcega-González, C.E.; Chavira-Suárez, E.; León-Buitimea, A.; Vázquez-León, P.; Morones-Ramírez, J.R.; Villalón, C.M.; Quintanar-Stephano, A.; Marichal-Cancino, B.A. Susceptibility for Some Infectious Diseases in Patients With Diabetes: The Key Role of Glycemia. Front. Public Health 2021, 9, 559595. [Google Scholar] [CrossRef]
- Zhou, K.; Lansang, M.C. Diabetes Mellitus and Infection. [Updated 30 June 2024]. In Endotext [Internet]; Feingold, K.R., Anawalt, B., Blackman, M.R., Boyce, A., Chrousos, G., Corpas, E., de Herder, W.W., Dhatariya, K., Dungan, K., Hofland, J., et al., Eds.; MDText.com, Inc.: South Dartmouth, MA, USA, 2000. Available online: https://www.ncbi.nlm.nih.gov/books/NBK569326/ (accessed on 10 May 2024).
- Falcone, M.; Tiseo, G.; Russo, A.; Giordo, L.; Manzini, E.; Bertazzoni, G.; Palange, P.; Taliani, G.; Cangemi, R.; Farcomeni, A.; et al. Hospitalization for Pneumonia is Associated With Decreased 1-Year Survival in Patients With Type 2 Diabetes: Results From a Prospective Cohort Study. Medicine 2016, 95, e2531. [Google Scholar] [CrossRef]
- Pahal, P.; Rajasurya, V.; Sharma, S. Typical Bacterial Pneumonia. [Updated 1 August 2022]. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2022. Available online: https://www.ncbi.nlm.nih.gov/books/NBK534295/ (accessed on 11 May 2024).
- Pochepnia, S.; Grabczak, E.M.; Johnson, E.; Eyuboglu, F.O.; Akkerman, O.; Prosch, H. Imaging in pulmonary infections of immunocompetent adult patients. Breathe Mar. 2024, 20, 230186. [Google Scholar] [CrossRef]
- Alcon, A.; Fàbregas, N.; Torres, A. Pathophysiology of pneumonia. Clin. Chest Med. 2005, 26, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Cilloniz, C.; Martin-Loeches, I.; Garcia-Vidal, C.; San Jose, A.; Torres, A. Microbial Etiology of Pneumonia: Epidemiology, Diagnosis and Resistance Patterns. Int. J. Mol. Sci. 2016, 17, 2120. [Google Scholar] [CrossRef] [PubMed]
- Moldoveanu, B.; Otmishi, P.; Jani, P.; Walker, J.; Sarmiento, X.; Guardiola, J.; Saad, M.; Yu, J. Inflammatory mechanisms in the lung. J. Inflamm. Res. 2009, 2, 1–11. [Google Scholar] [PubMed] [PubMed Central]
- Htun, T.P.; Sun, Y.; Chua, H.L.; Pang, J. Clinical features for diagnosis of pneumonia among adults in primary care setting: A systematic and meta-review. Sci. Rep. 2019, 9, 7600. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Conway Morris, A. Management of pneumonia in intensive care. J. Emerg. Crit. Care Med. 2018, 2, 101. [Google Scholar] [CrossRef]
- Pletz, M.W.; Jensen, A.V.; Bahrs, C.; Davenport, C.; Rupp, J.; Witzenrath, M.; Rohde, G. Unmet needs in pneumonia research: A comprehensive approach by the CAPNETZ study group. Respir. Res. 2022, 23, 239. [Google Scholar] [CrossRef]
- Grief, S.N.; Loza, J.K. Guidelines for the Evaluation and Treatment of Pneumonia. Prim. Care 2018, 45, 485–503. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Scott, J.A.; Brooks, W.A.; Peiris, J.S.; Holtzman, D.; Mulholland, E.K. Pneumonia research to reduce childhood mortality in the developing world. J. Clin. Investig. 2008, 118, 1291–1300. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dela Cruz, C.S.; Evans, S.E.; Restrepo, M.I.; Dean, N.; Torres, A.; Amara-Elori, I.; Awasthi, S.; Caler, E.; Cao, B.; Chalmers, J.D.; et al. Understanding the Host in the Management of Pneumonia. An Official American Thoracic Society Workshop Report. Ann. Am. Thorac. Soc. 2021, 18, 1087–1097. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Niederman, M.S. PNEUMONIA|Community Acquired Pneumonia, Bacterial and Other Common Pathogens. Encycl. Respir. Med. 2006, 417–431. [Google Scholar] [CrossRef] [PubMed Central]
- Sattar, S.B.A.; Nguyen, A.D.; Sharma, S. Bacterial Pneumonia. [Updated 26 February 2024]. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK513321/ (accessed on 12 May 2024).
- Torres, A.; Menéndez, R.; Wunderink, R.G. Bacterial Pneumonia and Lung Abscess. Murray Nadels Textb. Respir. Med. 2016, 1, 557–582.e22. [Google Scholar] [CrossRef]
- Ljubin-Sternak, S.; Meštrović, T.; Lukšić, I.; Mijač, M.; Vraneš, J. Seasonal Coronaviruses and Other Neglected Respiratory Viruses: A Global Perspective and a Local Snapshot. Front. Public Health 2021, 9, 691163. [Google Scholar] [CrossRef] [PubMed]
- Al-Tawfiq, J.A.; Kim, H.; Memish, Z.A. Parasitic lung diseases. Eur. Respir. Rev. 2022, 31, 220093. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cheepsattayakorn, A.; Cheepsattayakorn, R. Parasitic pneumonia and lung involvement. BioMed Res. Int. 2014, 2014, 874021. [Google Scholar] [CrossRef]
- Yang, X.; Leng, T.; Tang, C. Parasitic Infection Misdiagnosed As Bacterial Pneumonia: A Case Report. Altern. Ther. Health Med. 2021, 27, 54–57. [Google Scholar]
- Kunst, H.; Mack, D.; Kon, O.M.; Banerjee, A.K.; Chiodini, P.; Grant, A. Parasitic infections of the lung: A guide for the respiratory physician. Thorax 2010, 66, 528–536. [Google Scholar] [CrossRef]
- Martínez-Girón, R.; Esteban, J.G.; Ribas, A.; Doganci, L. Protozoa in respiratory pathology: A review. Eur. Respir. J. 2008, 32, 1354–1370. [Google Scholar] [CrossRef] [PubMed]
- Debnath, S.K.; Debnath, M.; Srivastava, R. Opportunistic etiological agents causing lung infections: Emerging need to transform lung-targeted delivery. Heliyon 2022, 8, e12620. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Weatherhead, J.E.; Gazzinelli-Guimaraes, P.; Knight, J.M.; Fujiwara, R.; Hotez, P.J.; Bottazzi, M.E.; Corry, D.B. Host Immunity and Inflammation to Pulmonary Helminth Infections. Front. Immunol. 2020, 11, 594520. [Google Scholar] [CrossRef]
- Morelli, S.; Diakou, A.; Colombo, M.; Di Cesare, A.; Barlaam, A.; Dimzas, D.; Traversa, D. Cat Respiratory Nematodes: Current Knowledge, Novel Data and Warranted Studies on Clinical Features, Treatment and Control. Pathogens 2021, 10, 454. [Google Scholar] [CrossRef]
- Nonnis, F.; Tamponi, C.; Tosciri, G.; Manconi, M.; Pudda, F.; Cabras, P.; Dessì, G.; Scala, A.; Varcasia, A. Cardio-pulmonary nematodes of the red fox (Vulpes vulpes) of Sardinia, Italy. Parasitol. Res. 2023, 122, 1685–1688. [Google Scholar] [CrossRef] [PubMed]
- Krishna, G.; Manuel, S.M.; Ananthakrishnan, V.M. Tropical eosinophilia: Case series on varying presentations. J. Fam. Med. Prim. Care 2024, 13, 4727–4729. [Google Scholar] [CrossRef]
- Katru, S.C.; Balakrishnan, A.S.; Munirathinam, G.; Hadadianpour, A.; Smith, S.A.; Kalyanasundaram, R. Identification and characterization of a novel nematode pan allergen (NPA) from Wuchereria bancrofti and their potential role in human filarial tropical pulmonary eosinophilia (TPE). PLoS Negl. Trop. Dis. 2024, 18, e0011972. [Google Scholar] [CrossRef]
- Sinha, N.; Kumar, A.; Sinha, R. Wuchereria bancrofti infection causing pleural effusion. Indian. J. Respir. Care 2021, 10, 246. [Google Scholar] [CrossRef]
- de Waal, T.; Mehmood, K. Editorial: Trematode Infection in Ruminants. Front. Vet. Sci. 2021, 8, 719577. [Google Scholar] [CrossRef]
- Rivera-Pérez, C.I.; Mignucci-Giannoni, A.A.; Freeman, M.A.; Orcera-Iglesias, J.M.; Cabrias-Contreras, L.J.; Dennis, M.M. Verminous bronchitis and pneumonia by nasal trematodes in Greater Caribbean manatees from Puerto Rico. Dis. Aquat. Organ. 2024, 159, 49–63. [Google Scholar] [CrossRef] [PubMed]
- Jensen, A.V.; Egelund, G.B.; Andersen, S.B.; Trier Petersen, P.; Benfield, T.; Faurholt-Jepsen, D.; Rohde, G.; Ravn, P. The impact of blood glucose on community-acquired pneumonia: A retrospective cohort study. ERJ Open Res. 2017, 3, 00114–02016. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kim, S.H.; Kim, J.Y.; Kim, E.S.; Park, I.R.; Ha, E.Y.; Chung, S.M.; Moon, J.S.; Yoon, J.S.; Won, K.C.; Lee, H.W. Early glycaemic variability increases 28-day mortality and prolongs intensive care unit stay in critically ill patients with pneumonia. Ann. Med. 2022, 54, 2724–2731. [Google Scholar] [CrossRef] [PubMed]
- Muravlyova, L.; Molotov-Luchankiy, V.; Bakirova, R.; Klyuyev, D.; Demidchik, L.; Lee, V. Characteristic of the Oxidative Stress in Blood of Patients in Dependence of Community-Acquired Pneumonia Severity. Open Access Maced. J. Med. Sci. 2016, 4, 122–127. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jabaudon, M.; Berthelin, P.; Pranal, T.; Roszyk, L.; Godet, T.; Faure, J.S.; Constantin, J.M. Receptor for advanced glycation end-products and ARDS prediction: A multicentre observational study. Sci. Rep. 2018, 8, 2603. [Google Scholar] [CrossRef]
- Lin, C.H.; Li, Y.R.; Lin, P.R.; Wang, B.Y.; Lin, S.H.; Huang, K.Y.; Kor, C.T. Blood monocyte levels predict the risk of acute exacerbations of chronic obstructive pulmonary disease: A retrospective case–control study. Sci. Rep. 2022, 12, 21057. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Hou, X.F.; Feng, C.M.; Zheng, L.; Xu, D.X.; Zhao, H.; Fu, L. The association between serum complement C3a and severity in patients with community-acquired pneumonia. Front. Immunol. 2023, 14, 1034233. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Criner, G.J.; Lang, F.M.; Gottlieb, R.L.; Mathews, K.S.; Wang, T.S.; Rice, T.W.; Madduri, D.; Bellam, S.; Jeanfreau, R.; Case, A.H.; et al. Anti-granulocyte–macrophage colony–stimulating factor monoclonal antibody gimsilumab for COVID-19 pneumonia: A randomized, double-blind, Placebo-controlled Trial. Am. J. Respir. Crit. Care Med. 2022, 205, 1290–1299. [Google Scholar] [CrossRef]
- Kuti, B.P.; Adetola, H.H.; Oyelami, O.A. Serum Micronutrients as related to Childhood Pneumonia Severity and Outcome in a Nigerian Health Facility. J. Infect. Dev. Ctries 2021, 15, 953–961. [Google Scholar] [CrossRef]
- Yang, A.; Shi, M.; Wu, H.; Lau, E.S.; Ma, R.C.; Kong, A.P.; Chow, E. Long-term metformin use and risk of pneumonia and related death in type 2 diabetes: A registry-based cohort study. Diabetologia 2021, 64, 1760–1765. [Google Scholar] [CrossRef]
- Rueda, A.M.; Ormond, M.; Gore, M.; Matloobi, M.; Giordano, T.P.; Musher, D.M. Hyperglycemia in diabetics and non-diabetics: Effect on the risk for and severity of pneumococcal pneumonia. J. Infect. 2010, 60, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Abbasi, E.; Mirzaei, F.; Tavilani, H.; Khodadadi, I. Diabetes and COVID-19: Mechanism of pneumonia, treatment strategy and vaccine. Metabol. Open 2021, 11, 100122. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rahmani, A.H.; Anwar, S.; Raut, R.; Almatroudi, A.; Babiker, A.Y.; Khan, A.A.; Alsahli, M.A.; Almatroodi, S.A. Therapeutic Potential of Myrrh, a Natural Resin, in Health Management through Modulation of Oxidative Stress, Inflammation, and Advanced Glycation End Products Formation Using In Vitro and In Silico Analysis. Appl. Sci. 2022, 12, 9175. [Google Scholar] [CrossRef]
- Hulkower, R.D.; Pollack, R.M.; Zonszein, J. Understanding hypoglycemia in hospitalized patients. Diabetes Manag. 2014, 4, 165–176. [Google Scholar] [CrossRef]
- Mendez, C.E.; Mok, K.T.; Ata, A.; Tanenberg, R.J.; Calles-Escandon, J.; Umpierrez, G.E. Increased glycemic variability is independently associated with length of stay and mortality in noncritically ill hospitalized patients. Diabetes Care 2013, 36, 4091–4097. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ali, T.M.; Salem, H.M.; Sultan, D.R. The impact of admission blood glucose level on patients with community-acquired pneumonia. Egypt. J. Bronchol. 2019, 13, 551–555. [Google Scholar] [CrossRef]
- Barmanray, R.D.; Cheuk, N.; Fourlanos, S.; Worth, L.J. In-hospital hyperglycemia but not diabetes mellitus alone is associated with increased in- hospital mortality in community-acquired pneumonia (CAP): A systematic review and meta- analysis of observational studies prior to COVID-19. BMJ Open Diab Res. Care 2022, 10, e002880. [Google Scholar] [CrossRef] [PubMed]
- Hulme, K.D.; Gallo, L.A.; Short, K.R. Influenza virus and glycemic variability in diabetes: A killer combination? Front. Microbiol. 2017, 8, 861. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, L.; Moniz, A.C.; Carneiro, A.S.; Miranda, A.S.; Fangueiro, C.; Fernandes, D.; Silva, I.; Palhinhas, I.; Lemos, J.; Antunes, J.; et al. The impact of glycemic variability on length of stay and mortality in diabetic patients admitted with community-acquired pneumonia or chronic obstructive pulmonary disease. Diabetes Metab. Syndr. 2019, 13, 149–153. [Google Scholar] [CrossRef] [PubMed]
- Olsen, M.T.; Dungu, A.M.; Klarskov, C.K.; Jensen, A.K.; Lindegaard, B.; Kristensen, P.L. Glycemic variability assessed by continuous glucose monitoring in hospitalized patients with community-acquired pneumonia. BMC Pulm. Med. 2022, 22, 83. [Google Scholar] [CrossRef]
- Rahmani, A.H.; Babiker, A.Y.; Anwar, S. Hesperidin, a Bioflavonoid in Cancer Therapy: A Review for a Mechanism of Action through the Modulation of Cell Signaling Pathways. Molecules 2023, 28, 5152. [Google Scholar] [CrossRef]
- Anwar, S.; Raut, R.; Kanwal, B.; Yahia, E. In vitro investigation of antiinflammatory and antioxidant activities of Curcuma longa rhizome methanol extract. Int. J. Creat. Res. Thoughts (IJCRT) 2022, 10, c559–c581. Available online: https://www.researchgate.net/publication/364950380_In_Vitro_Investigation_of_Antiinflammatory_and_Antioxidant_Activities_of_Curcuma_Longa_Rhizome_Methanol_Extract (accessed on 13 May 2024).
- Anwar, S.; Alrumaihi, F.; Sarwar, T.; Babiker, A.Y.; Khan, A.A.; Prabhu, S.V.; Rahmani, A.H. Exploring Therapeutic Potential of Catalase: Strategies in Disease Prevention and Management. Biomolecules 2024, 14, 697. [Google Scholar] [CrossRef]
- Anwar, S.; Almatroudi, A.; Allemailem, K.S.; Jacob Joseph, R.; Khan, A.A.; Rahmani, A.H. Protective Effects of Ginger Extract against Glycation and Oxidative Stress-Induced Health Complications: An In Vitro Study. Processes 2020, 8, 468. [Google Scholar] [CrossRef]
- Sharifi-Rad, M.; Anil Kumar, N.V.; Zucca, P.; Varoni, E.M.; Dini, L.; Panzarini, E.; Rajkovic, J.; Tsouh Fokou, P.V.; Azzini, E.; Peluso, I.; et al. Lifestyle, Oxidative Stress, and Antioxidants: Back and Forth in the Pathophysiology of Chronic Diseases. Front. Physiol. 2020, 11, 694. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bezerra, F.S.; Lanzetti, M.; Nesi, R.T.; Nagato, A.C.; Silva CPe Kennedy-Feitosa, E.; Melo, A.C.; Cattani-Cavalieri, I.; Porto, L.C.; Valenca, S.S. Oxidative Stress and Inflammation in Acute and Chronic Lung Injuries. Antioxidants 2023, 12, 548. [Google Scholar] [CrossRef] [PubMed]
- Anwar, S.; Khan, M.A.; Sadaf, A.; Younus, H. A structural study on the protection of glycation of superoxide dismutase by thymoquinone. Int. J. Biol. Macromol. 2014, 69, 476–481. [Google Scholar] [CrossRef] [PubMed]
- Tepebaşı, M.Y.; İlhan, İ.; Temel, E.N.; Sancer, O.; Öztürk, Ö. Investigation of inflammation, oxidative stress, and DNA damage in COVID-19 patients. Cell Stress. Chaperones 2023, 28, 191–199. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lee, Y.H.; Lee, S.J.; Lee, M.K.; Lee, W.Y.; Yong, S.J.; Kim, S.H. Serum selenium levels in patients with respiratory diseases: A prospective observational study. J. Thorac. Dis. 2016, 8, 2068–2078. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bargagli, E.; Olivieri, C.; Bennett, D.; Prasse, A.; Muller-Quernheim, J.; Rottoli, P. Oxidative stress in the pathogenesis of diffuse lung diseases: A review. Respir. Med. 2009, 103, 1245–1256. [Google Scholar] [CrossRef]
- Anwar, S.; Raut, R.; Alhumaydhi, F.A. A comprehensive investigation on alleviating oxidative stress and inflammation in hyperglycaemic conditions through in vitro experiments and computational analysis. Saudi J. Biol. Sci. 2024, 31, 104003. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Younus, H.; Anwar, S. Antiglycating activity of Aloe vera gel extract and its active component aloin. Proteins Proteom. 2018, 9, 115–125. [Google Scholar]
- Martinez, P.J.; Mathews, C.; Actor, J.K.; Hwang, S.A.; Brown, E.L.; De Santiago, H.K.; Fisher Hoch, S.P.; McCormick, J.B.; Mirza, S. Impaired CD4+ and T-helper 17 cell memory response to Streptococcus pneumoniae is associated with elevated glucose and percent glycated hemoglobin A1c in Mexican Americans with type 2 diabetes mellitus. Transl. Res. 2014, 163, 53–63. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Motamed, B.; Alavi Foumani, A.; Tangestaninezhad, A.; Almasi, M.; Faraji, N.; Jafarinezhad, A. The relationship between glycated hemoglobin A1c levels and exacerbation status in the patients with chronic obstructive pulmonary disease. BMC Res. Notes 2022, 15, 326. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yang, G.; Han, Y.Y.; Forno, E.; Yan, Q.; Rosser, F.; Chen, W.; Celedón, J.C. Glycated Hemoglobin A1c, Lung Function, and Hospitalizations Among Adults with Asthma. J. Allergy Clin. Immunol. Pract. 2020, 8, 3409–3415.e1. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sánchez Díaz, J.S.; Peniche Moguel, K.G.; González Escudero, E.A.; Del Carpio Orantes, L.; Monares Zepeda, E.; Perez Nieto, O.R.; Zamarron Lopez, E.I.; Deloya Tomas, E.; Estrada Gonzalez, F.E.; Díaz Torres, J.; et al. Glycosylated hemoglobin as a predictor of mortality in severe pneumonia by COVID-19. Expert Rev. Respir. Med. 2021, 15, 1077–1082. [Google Scholar] [CrossRef] [PubMed]
- Campo, I.G.; Villarreal, M.A.G.; Echeverria, J.F.M.; Villalba, J.C.M.; Taborda, N.T.; Velasquez, Y.L.F.; Mejia, C.A.G. Glycosylated Haemoglobin as a Predictor of Mortality in Severe Pneumonia by COVID-19. Health Sci. J. 2022, 16, 928. [Google Scholar]
- Mann, R.; Holmes, A.; McNeilly, O.; Cavaliere, R.; Sotiriou, G.A.; Rice, S.A.; Gunawan, C. Evolution of biofilm-forming pathogenic bacteria in the presence of nanoparticles and antibiotic: Adaptation phenomena and cross-resistance. J. Nanobiotechnol. 2021, 19, 291. [Google Scholar] [CrossRef] [PubMed]
- Casqueiro, J.; Casqueiro, J.; Alves, C. Infections in patients with diabetes mellitus: A review of pathogenesis. Indian. J. Endocr. Metab. 2012, 16, S27–S36. [Google Scholar]
- Sarma, J.V.; Ward, P.A. The complement system. Cell Tissue Res. 2011, 343, 227–235. [Google Scholar] [CrossRef]
- Bardhan, M.; Kaushik, R. Physiology, Complement Cascade. [Updated 14 February 2023]. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK551511/ (accessed on 21 May 2024).
- Jafar, N.; Edriss, H.; Nugent, K. The Effect of Short-Term Hyperglycemia on the Innate Immune System. Am. J. Med. Sci. 2016, 351, 201–211. [Google Scholar] [CrossRef] [PubMed]
- Bermejo-Martin, J.F.; Almansa, R.; Martin-Fernandez, M.; Menendez, R.; Torres, A. Immunological profiling to assess disease severity and prognosis in community-acquired pneumonia. Lancet Respir. Med. 2017, 5, e35–e36. [Google Scholar] [CrossRef] [PubMed]
- Pandya, P.H.; Wilkes, D.S. Complement system in lung disease. Am. J. Respir. Cell Mol. Biol. 2014, 51, 467–473. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Coonrod, J.D.; Rylko-Bauer, B. Complement levels in pneumococcal pneumonia. Infect. Immun. 1977, 18, 14–22. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Paton, J.C.; Rowan-Kelly, B.; Ferrante, A. Activation of human complement by the pneumococcal toxin pneumolysin. Infect. Immun. 1984, 43, 1085–1087. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kolling, U.K.; Hansen, F.; Braun, J.; Rink, L.; Katus, H.A.; Dalhoff, K. Leucocyte response and anti-inflammatory cytokines in community acquired pneumonia. Thorax 2001, 56, 121–125. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Du, X.; Meng, Q.; Sharif, A.; Abdel-Razek, O.A.; Zhang, L.; Wang, G.; Cooney, R.N. Surfactant Proteins SP-A and SP-D Ameliorate Pneumonia Severity and Intestinal Injury in a Murine Model of Staphylococcus Aureus Pneumonia. Shock 2016, 46, 164–172. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, E.; Van Eeden, S.; English, D.; Hogg, J.C. Polymorphonuclear leukocyte (PMN) migration in streptococcal pneumonia: Comparison of older PMN with those recently released from the marrow. Am. J. Respir. Cell Mol. Biol. 1996, 14, 217–224. [Google Scholar] [CrossRef] [PubMed]
- Terashima, T.; Wiggs, B.; English, D.; Hogg, J.C.; van Eeden, S.F. Polymorphonuclear leukocyte transit times in bone marrow during streptococcal pneumonia. Am. J. Physiol. 1996, 271 Pt 1, L587–L592. [Google Scholar] [CrossRef] [PubMed]
- de Souza, P.R.K.; Ferreira, S.S.; Nunes, F.P.B.; Casagrande, F.B.; Tessaro, F.H.G.; Silva, M.C.F.; Cruz, J.W.M.C.; Mamizuka, E.M.; Martins, J.O. Cytokine and Adhesion Molecule Expression Induced by Different Strains of Staphylococcus aureus in Type 1 Diabetic Rats: Role of Insulin. Front. Immunol. 2019, 9, 3165. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mathews, C.E.; Brown, E.L.; Martinez, P.J.; Bagaria, U.; Nahm, M.H.; Burton, R.L.; Fisher-Hoch, S.P.; McCormick, J.B.; Mirza, S. Impaired function of antibodies to pneumococcal surface protein A but not to capsular polysaccharide in Mexican American adults with type 2 diabetes mellitus. Clin. Vaccine Immunol. 2012, 19, 1360–1369. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sadarangani, M. Protection Against Invasive Infections in Children Caused by Encapsulated Bacteria. Front. Immunol. 2018, 9, 2674. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Visan, L.; Rouleau, N.; Proust, E.; Peyrot, L.; Donadieu, A.; Ochs, M. Antibodies to PcpA and PhtD protect mice against Streptococcus pneumoniae by a macrophage- and complement-dependent mechanism. Hum. Vaccin. Immunother. 2018, 14, 489–494. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wilson, R.; Cohen, J.M.; Reglinski, M.; Jose, R.J.; Chan, W.Y.; Marshall, H.; Brown, J.S. Correction: Naturally Acquired Human Immunity to Pneumococcus Is Dependent on Antibody to Protein Antigens. PLoS Pathog. 2017, 13, e1006259. [Google Scholar] [CrossRef]
- Gombart, A.F.; Pierre, A.; Maggini, S. A Review of Micronutrients and the Immune System-Working in Harmony to Reduce the Risk of Infection. Nutrients 2020, 12, 236. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Prietl, B.; Treiber, G.; Pieber, T.R.; Amrein, K. Vitamin D and immune function. Nutrients 2013, 5, 2502–2521. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- White, J.H. Emerging Roles of Vitamin D-Induced Antimicrobial Peptides in Antiviral Innate Immunity. Nutrients 2022, 14, 284. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lips, P.; Eekhoff, M.; van Schoor, N.; Oosterwerff, M.; de Jongh, R.; Krul-Poel, Y.; Simsek, S. Vitamin D and type 2 diabetes. J. Steroid Biochem. Mol. Biol. 2017, 173, 280–285. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.F.; Luo, B.A.; Qin, L.L. The association between vitamin D deficiency and community-acquired pneumonia: A meta-analysis of observational studies. Medicine 2019, 98, e17252. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bhat, M.H.; Mudassir Rather, A.B.; Dhobi, G.N.; Koul, A.N.; Bhat, F.A.; Hussain, A. Zinc Levels in community acquired pneumonia in hospitalized patients; a case control study. Egypt. J. Chest Dis. Tuberc. 2016, 65, 485–489. [Google Scholar] [CrossRef]
- Lassi, Z.S.; Haider, B.A.; Bhutta, Z.A. Zinc supplementation for the prevention of pneumonia in children aged 2 months to 59 months. Cochrane Database Syst. Rev. 2010, 12, CD005978. [Google Scholar] [CrossRef]
- Zmijewski, J.W.; Lorne, E.; Zhao, X.; Tsuruta, Y.; Sha, Y.; Liu, G.; Abraham, E. Mitochondrial respiratory complex I regulates neutrophil activation and severity of lung injury. Am. J. Respir. Crit. Care Med. 2008, 178, 168–179. [Google Scholar] [CrossRef]
- Garnett, J.P.; Baker, E.H.; Naik, S.; Lindsay, J.A.; Knight, G.M.; Gill, S.; Baines, D.L. Metformin reduces airway glucose permeability and hyperglycaemia-induced Staphylococcus aureus load independently of effects on blood glucose. Thorax 2013, 68, 835–845. [Google Scholar] [CrossRef]
- Yen, F.S.; Wei, J.C.; Shih, Y.H.; Hsu, C.C.; Hwu, C.M. Metformin use and the risk of bacterial pneumonia in patients with type 2 diabetes. Sci. Rep. 2022, 12, 3270. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tseng, C.-H. Metformin Decreases Risk of Tuberculosis Infection in Type 2 Diabetes Patients. J. Clin. Med. 2018, 7, 264. [Google Scholar] [CrossRef]
- Pitocco, D.; Fuso, L.; Conte, E.G.; Zaccardi, F.; Condoluci, C.; Scavone, G.; Incalzi, R.A.; Ghirlanda, G. The diabetic lung--a new target organ? Rev. Diabet. Stud. 2012, 9, 23–35. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cheng, S.; Hou, G.; Liu, Z.; Lu, Y.; Liang, S.; Cang, L.; Zhang, X.; Zou, C.; Kang, J.; Chen, Y. Risk prediction of in-hospital mortality among patients with type 2 diabetes mellitus and concomitant community-acquired pneumonia. Ann. Palliat. Med. 2020, 9, 3313–3325. [Google Scholar] [CrossRef] [PubMed]
- Mani, C.S. Acute Pneumonia and Its Complications. In Principles and Practice of Pediatric Infectious Diseases, 5th ed.; Elsevier: Amsterdam, The Netherlands, 2018; pp. 238–249.e4. [Google Scholar] [CrossRef]
- American Lung Association. Available online: https://www.lung.org/lung-health-diseases/lung-disease-lookup/pneumonia/symptoms-and-diagnosis (accessed on 15 September 2024).
- Shrestha, S.; Chaudhary, N.; Shrestha, S.; Pathak, S.; Sharma, A.; Shrestha, L.; Kurmi, O.P. Clinical predictors of radiological pneumonia: A cross-sectional study from a tertiary hospital in Nepal. PLoS ONE 2020, 15, e0235598. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ebrahim, H.; Fiseha, T.; Ebrahim, Y.; Bisetegn, H. Comparison of hematological parameters between type 2 diabetes mellitus patients and healthy controls at Dessie comprehensive specialized hospital, Northeast Ethiopia: Comparative cross-sectional study. PLoS ONE 2022, 17, e0272145. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Liu, X.; Zhao, Q.; He, X.; Min, J.; Yao, R.S.Y.; Chen, Z.; Ma, J.; Hu, W.; Huang, J.; Wan, H.; et al. Clinical characteristics and microbial signatures in the lower airways of diabetic and nondiabetic patients with pneumonia. J. Thorac. Dis. 2024, 16, 5262–5273. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Prabhakar, K.; Moosa, P.E.; Jayaram, N.; Yashwant, A.L. A Comparative Study of Bacterial Pneumonia in Diabetic and Non-diabetic Patients From A Rural Tertiary Center. J. Clin. Biomed. Sci. 2011, 1, 104. [Google Scholar]
- Sun, Y.; Zhao, R.; Hu, Z.; Wang, W.; Wang, S.; Gao, L.; Fei, J.; Jian, X.; Li, Y.; Zheng, H.; et al. Differences in the Clinical and Hematological Characteristics of COVID-19 Patients with and without Type 2 Diabetes. J. Diabetes Res. 2020, 2020, 1038585. [Google Scholar] [CrossRef]
- Atwah, B.; Iqbal, M.S.; Kabrah, S.; Kabrah, A.; Alghamdi, S.; Tabassum, A.; Baghdadi, M.A.; Alzahrani, H. Susceptibility of Diabetic Patients to COVID-19 Infections: Clinico-Hematological and Complications Analysis. Vaccines 2023, 11, 561. [Google Scholar] [CrossRef]
- Francis, J.S.; Doherty, M.C.; Lopatin, U.; Johnston, C.P.; Sinha, G.; Ross, T.; Bartlett, J.G. Severe community-onset pneumonia in healthy adults caused by methicillin-resistant Staphylococcus aureus carrying the Panton-Valentine leukocidin genes. Clin. Infect. Dis. 2005, 40, 100. [Google Scholar] [CrossRef]
- Delclaux, C.; Azoulay, E. Inflammatory response to infectious pulmonary injury. Eur. Respir. J. Aug. 2003, 22 (Suppl. S42), 10s–14s. [Google Scholar] [CrossRef]
- Korkmaz, F.T.; Traber, K.E. Innate immune responses in pneumonia. Pneumonia 2023, 15, 4. [Google Scholar] [CrossRef] [PubMed]
- Ott, L.W.; Resing, K.A.; Sizemore, A.W.; Heyen, J.W.; Cocklin, R.R.; Pedrick, N.M.; Woods, H.C.; Chen, J.Y.; Goebl, M.G.; Witzmann, F.A.; et al. Tumor Necrosis Factor-alpha- and interleukin-1-induced cellular responses: Coupling proteomic and genomic information. J. Proteome Res. 2007, 6, 2176–2185. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jang, D.I.; Lee, A.H.; Shin, H.Y.; Song, H.R.; Park, J.H.; Kang, T.B.; Lee, S.R.; Yang, S.H. The Role of Tumor Necrosis Factor Alpha (TNF-α) in Autoimmune Disease and Current TNF-α Inhibitors in Therapeutics. Int. J. Mol. Sci. 2021, 22, 2719. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rider, A.C.; Frazee, B.W. Community-Acquired Pneumonia. Emerg. Med. Clin. N. Am. 2018, 36, 665–683. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shebl, E.; Gulick, P.G. Nosocomial Pneumonia. [Updated 29 May 2023]. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK535441/ (accessed on 17 May 2024).
- Kohbodi, G.A.; Rajasurya, V.; Noor, A. Ventilator-Associated Pneumonia. 2023 Sep 4. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar] [PubMed]
- Poovieng, J.; Sakboonyarat, B.; Nasomsong, W. Bacterial etiology and mortality rate in community-acquired pneumonia, healthcare-associated pneumonia and hospital-acquired pneumonia in Thai university hospital. Sci. Rep. 2022, 12, 9004. [Google Scholar] [CrossRef]
- Sanivarapu, R.R.; Gibson, J. Aspiration Pneumonia. [Updated 8 May 2023]. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK470459/ (accessed on 17 May 2024).
- Yoshimatsu, Y.; Melgaard, D.; Westergren, A.; Skrubbeltrang, C.; Smithard, D.G. The diagnosis of aspiration pneumonia in older persons: A systematic review. Eur. Geriatr. Med. 2022, 13, 1071–1080. [Google Scholar] [CrossRef]
- Lee, K.-Y. Pneumonia, Acute Respiratory Distress Syndrome, and Early Immune-Modulator Therapy. Int. J. Mol. Sci. 2017, 18, 388. [Google Scholar] [CrossRef]
- Aleem, M.S.; Sexton, R.; Akella, J. Pneumonia in an Immunocompromised Patient. [Updated 25 July 2023]. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK557843/ (accessed on 17 May 2024).
- Kany, S.; Vollrath, J.T.; Relja, B. Cytokines in Inflammatory Disease. Int. J. Mol. Sci. 2019, 20, 6008. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Freeman, A.M.; Leigh, T.R., Jr. Viral Pneumonia. 4 July 2022. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar] [PubMed]
- Shaaban, L.H.; Ahmed, Y. Hemogram values in community acquired pneumonia. Egypt. J. Chest Dis. Tuberc. 2015, 64, 617–623. [Google Scholar] [CrossRef]
- Camon, S.; Quiros, C.; Saubi, N.; Moreno, A.; Marcos, M.A.; Eto, Y.; Rofael, S.; Monclus, E.; Brown, J.; McHugh, T.D.; et al. Full blood count values as a predictor of poor outcome of pneumonia among HIV-infected patients. BMC Infect. Dis. 2018, 18, 189. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Curbelo, J.; Luquero Bueno, S.; Galván-Román, J.M.; Ortega-Gómez, M.; Rajas, O.; Fernández-Jiménez, G.; Aspa, J. Correction: Inflammation biomarkers in blood as mortality predictors in community-acquired pneumonia admitted patients: Importance of comparison with neutrophil count percentage or neutrophil-lymphocyte ratio. PLoS ONE 2019, 14, e0212915. [Google Scholar] [CrossRef] [PubMed]
- Bordon, J.; Aliberti, S.; Fernandez-Botran, R.; Uriarte, S.M.; Rane, M.J.; Duvvuri, P.; Peyrani, P.; Morlacchi, L.C.; Blasi, F.; Ramirez, J.A. Understanding the roles of cytokines and neutrophil activity and neutrophil apoptosis in the protective versus deleterious inflammatory response in pneumonia. Int. J. Infect. Dis. 2013, 17, e76–e83. [Google Scholar] [CrossRef] [PubMed]
- Kurt, C.; Altunçeki Ç Yildirim, A. Contribution of Erythrocyte Sedimentation Rate to Predict Disease Severity and Outcome in COVID-19 Patients. Can. J. Infect. Dis. Med. Microbiol. 2022, 2022, 6510952. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sartori, L.F.; Zhu, Y.; Grijalva, C.G.; Ampofo, K.; Gesteland, P.; Johnson, J.; McHenry, R.; Arnold, D.H.; Pavia, A.T.; Edwards, K.M.; et al. Pneumonia Severity in Children: Utility of Procalcitonin in Risk Stratification. Hosp. Pediatr. 2021, 11, 215–222. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kellum, J.A.; Kong, L.; Fink, M.P.; Weissfeld, L.A.; Yealy, D.M.; Pinsky, M.R.; Fine, J.; Krichevsky, A.; Delude, R.L.; Angus, D.C.; et al. Understanding the inflammatory cytokine response in pneumonia and sepsis: Results of the Genetic and Inflammatory Markers of Sepsis (GenIMS) Study. Arch. Intern. Med. 2007, 167, 1655–1663. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wu, J.; Jin, Y.U.; Li, H.; Xie, Z.; Li, J.; Ao, Y.; Duan, Z. Evaluation and significance of C-reactive protein in the clinical diagnosis of severe pneumonia. Exp. Ther. Med. 2015, 10, 175–180. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shen, F.; Sergi, C. Sputum Analysis. [Updated 20 February 2023]. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK563195/ (accessed on 17 May 2024).
- Reed, W.W.; Byrd, G.S.; Gates, R.H., Jr.; Howard, R.S.; Weaver, M.J. Sputum gram’s stain in community-acquired pneumococcal pneumonia. A meta-analysis. West. J. Med. 1996, 165, 197–204. [Google Scholar] [PubMed] [PubMed Central]
- Adhya, A.K. Grocott Methenamine Silver Positivity in Neutrophils. J. Cytol. 2019, 36, 184. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wright, A.M.; Mody, D.R.; Anton, R.C.; Schwartz, M.R. Aberrant staining with Grocott’s methenamine silver: Utility beyond fungal organisms. J. Am. Soc. Cytopathol. 2017, 6, 223–227. [Google Scholar] [CrossRef] [PubMed]
- Patel, P.H.; Antoine, M.H.; Ullah, S. Bronchoalveolar Lavage. [Updated 28 August 2022]. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK430762/ (accessed on 17 May 2024).
- Davidson, K.R.; Ha, D.M.; Schwarz, M.I.; Chan, E.D. Bronchoalveolar lavage as a diagnostic procedure: A review of known cellular and molecular findings in various lung diseases. J. Thorac. Dis. 2020, 12, 4991–5019. [Google Scholar] [CrossRef]
- Zhang, D.; Yang, D.; Makam, A.N. Utility of Blood Cultures in Pneumonia. Am. J. Med. 2019, 132, 1233–1238. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chela, H.K.; Vasudevan, A.; Rojas-Moreno, C.; Naqvi, S.H. Approach to Positive Blood Cultures in the Hospitalized Patient: A Review. Mo. Med. 2019, 116, 313–317. [Google Scholar] [PubMed] [PubMed Central]
- Huang, L.; Crothers, K. HIV-associated opportunistic pneumonias. Respirology 2009, 14, 474–485. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kundu, R.; Das, R.; Geem, Z.W.; Han, G.T.; Sarkar, R. Pneumonia detection in chest X-ray images using an ensemble of deep learning models. PLoS ONE 2021, 16, e0256630. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rousan, L.A.; Elobeid, E.; Karrar, M.; Khader, Y. Chest x-ray findings and temporal lung changes in patients with COVID-19 pneumonia. BMC Pulm. Med. 2020, 20, 245. [Google Scholar] [CrossRef]
- Garin, N.; Marti, C.; Scheffler, M.; Stirnemann, J.; Prendki, V. Computed tomography scan contribution to the diagnosis of community-acquired pneumonia. Curr. Opin. Pulm. Med. 2019, 25, 242–248. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nouvenne, A.; Ticinesi, A.; Folesani, G.; Cerundolo, N.; Prati, B.; Morelli, I.; Guida, L.; Lauretani, F.; Maggio, M.; Aloe, R.; et al. The association of serum procalcitonin and high-sensitivity C-reactive protein with pneumonia in elderly multimorbid patients with respiratory symptoms: Retrospective cohort study. BMC Geriatr. 2016, 16, 16. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Claessens, Y.E.; Debray, M.P.; Tubach, F.; Brun, A.L.; Rammaert, B.; Hausfater, P.; Duval, X. Early chest computed tomography scan to assist diagnosis and guide treatment decision for suspected community-acquired pneumonia. Am. J. Respir. Crit. Care Med. 2015, 192, 974–982. [Google Scholar] [CrossRef]
- Prendki, V.; Scheffler, M.; Huttner, B.; Garin, N.; Herrmann, F.; Janssens, J.P.; Stirnemann, J. Low-dose CT for the diagnosis of pneumonia in elderly patients: A prospective, interventional cohort study. Eur. Respir. J. 2018, 51, 1702375. [Google Scholar] [CrossRef]
- Bellew, S.; Grijalva, C.G.; Williams, D.J.; Anderson, E.J.; Wunderink, R.G.; Zhu, Y.; Waterer, G.W.; Bramley, A.M.; Jain, S.; Edwards, K.M.; et al. Pneumococcal and Legionella Urinary Antigen Tests in Community-acquired Pneumonia: Prospective Evaluation of Indications for Testing. Clin. Infect. Dis. 2019, 68, 2026–2033. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nilsson, A.C.; Björkman, P.; Persson, K. Polymerase chain reaction is superior to serology for the diagnosis of acute Mycoplasma pneumoniae infection and reveals a high rate of persistent infection. BMC Microbiol. 2008, 8, 93. [Google Scholar] [CrossRef] [PubMed]
- Stelmach, I.; Podsiadłowicz-Borzecka, M.; Sołoniewicz, A.; Grzelewski, T.; Kaczmarek, J.; Popławska, M.; Dziadek, J. Porównanie wyników uzyskanych metoda PCR i ELISA w diagnostyce zakazenia układu oddechowego Mycoplasma pneumoniae u dzieci [Comparison of PCR and ELISA techniques in the diagnosis of Mycoplasma pneumoniae airway infections in children]. Pneumonol. Alergol. Pol. 2004, 72, 383–388. (In Polish) [Google Scholar] [PubMed]
- Mercier, T.; Guldentops, E.; Patteet, S.; Beuselinck, K.; Lagrou, K.; Maertens, J. Beta-d-Glucan for Diagnosing Pneumocystis Pneumonia: A Direct Comparison between the Wako β-Glucan Assay and the Fungitell Assay. J. Clin. Microbiol. 2019, 57, e00322-19. [Google Scholar] [CrossRef] [PubMed]
- Del Corpo, O.; Butler-Laporte, G.; Sheppard, D.C.; Cheng, M.P.; McDonald, E.G.; Lee, T.C. Diagnostic accuracy of serum (1-3)-β-D-glucan for Pneumocystis jirovecii pneumonia: A systematic review and meta-analysis. Clin. Microbiol. Infect. 2020, 26, 1137–1143. [Google Scholar] [CrossRef] [PubMed]
- Allinovi, M.; Parise, A.; Giacalone, M.; Amerio, A.; Delsante, M.; Odone, A.; Franci, A.; Gigliotti, F.; Amadasi, S.; Delmonte, D.; et al. Lung Ultrasound May Support Diagnosis and Monitoring of COVID-19 Pneumonia. Ultrasound Med. Biol. 2020, 46, 2908–2917. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Long, L.; Zhao, H.T.; Zhang, Z.Y.; Wang, G.Y.; Zhao, H.L. Lung ultrasound for the diagnosis of pneumonia in adults: A meta-analysis. Medicine 2017, 96, e5713. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Peng, Q.Y.; Wang, X.T.; Zhang, L.N.; Chinese Critical Care Ultrasound Study Group (CCUSG). Findings of lung ultrasonography of novel corona virus pneumonia during the 2019-2020 epidemic. Intensive Care Med. 2020, 46, 849–850. [Google Scholar] [CrossRef] [PubMed]
- Zanforlin, A.; Strapazzon, G.; Falk, M.; Gallina, V.; Viteritti, A.; Valzolgher, L.; La Guardia, M.; Ferro, F.; Pagani, L.; Vezzali, N. Lung ultrasound in the emergency department for early identification of COVID-19 pneumonia. Respiration 2021, 100, 145–153. [Google Scholar] [CrossRef] [PubMed]
- Volpicelli, G.; Gargani, L.; Perlini, S.; Spinelli, S.; Barbieri, G.; Lanotte, A.; Casasola, G.G.; Nogué-Bou, R.; Lamorte, A.; Agricola, E.; et al. Lung ultrasound for the early diagnosis of COVID-19 pneumonia: An international multicenter study. Intensive Care Med. 2021, 47, 444–454. [Google Scholar] [CrossRef]
- Persona, P.; Valeri, I.; Zarantonello, F.; Forin, E.; Sella, N.; Andreatta, G.; Correale, C.; Serra, E.; Boscolo, A.; Volpicelli, G.; et al. Patients in intensive care unit for COVID-19 pneumonia: The lung ultrasound patterns at admission and discharge. An observational pilot study. Ultrasound J. 2021, 13, 1–7. [Google Scholar]
- de Alencar, J.C.; Marchini, J.F.; Marino, L.O.; da Costa Ribeiro, S.C.; Bueno, C.G.; da Cunha, V.P.; Lazar Neto, F.; Brandao Neto, R.A.; Souza, H.P. Lung ultrasound score predicts outcomes in COVID-19 patients admitted to the emergency department. Ann. Intensive Care 2021, 11, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Karakioulaki, M.; Stolz, D. Biomarkers in Pneumonia-Beyond Procalcitonin. Int. J. Mol. Sci. 2019, 20, 2004. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ito, A.; Ishida, T. Diagnostic markers for community-acquired pneumonia. Ann. Transl. Med. 2020, 8, 609. [Google Scholar] [CrossRef] [PubMed]
- Maisel, A.; Neath, S.X.; Landsberg, J.; Mueller, C.; Nowak, R.M.; Peacock, W.F.; Ponikowski, P.; Möckel, M.; Hogan, C.; Wu, A.H.; et al. Use of procalcitonin for the diagnosis of pneumonia in patients presenting with a chief complaint of dyspnoea: Results from the BACH (Biomarkers in Acute Heart Failure) trial. Eur. J. Heart Fail 2012, 14, 278–286. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Smith, R.P.; Lipworth, B.J.; Cree, I.A.; Spiers, E.M.; Winter, J.H. C-reactive protein. A clinical marker in community-acquired pneumonia. Chest 1995, 108, 1288–1291. [Google Scholar] [CrossRef] [PubMed]
- Daga, M.; Arora, N.; Prakash, S.K.; Jhamb, R.; Kumar, N.; Gupta, N. C-Revctive Protein in Lower Respiratory Tract Infections. Lung India 2005, 22, 41–44. [Google Scholar]
- Abdelgawad, T.A.; Anwar, M.A.; Magdy, S.M.; El-Sayed Abd El-Maksoud Abd El-Maksoud, M. Role of STREM-1 for early prediction of ventilator-associated pneumonia in pediatrics. Egypt. J. Bronchol. 2024, 18, 15. [Google Scholar] [CrossRef]
- Florin, T.A.; Ambroggio, L.; Brokamp, C.; Zhang, Y.; Nylen, E.S.; Rattan, M.; Crotty, E.; Belsky, M.A.; Krueger, S.; Epperson, T.N.; et al. Proadrenomedullin Predicts Severe Disease in Children With Suspected Community-acquired Pneumonia. Clin. Infect. Dis. 2021, 73, e524–e530. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kaufmann, C.C.; Ahmed, A.; Kassem, M.; Freynhofer, M.K.; Jäger, B.; Aicher, G.; Equiluz-Bruck, S.; Spiel, A.O.; Funk, G.C.; Gschwantler, M.; et al. Mid-regional pro-atrial natriuretic peptide independently predicts short-term mortality in COVID-19. Eur. J. Clin. Investig. 2021, 51, e13531. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Seligman, R.; Ramos-Lima, L.F.; Oliveira Vdo, A.; Sanvicente, C.; Pacheco, E.F.; Dalla Rosa, K. Biomarkers in community-acquired pneumonia: A state-of-the-art review. Clinics 2012, 67, 1321–1325. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Andrijevic, I.; Matijasevic, J.; Andrijevic, L.; Kovacevic, T.; Zaric, B. Interleukin-6 and procalcitonin as biomarkers in mortality prediction of hospitalized patients with community acquired pneumonia. Ann. Thorac. Med. 2014, 9, 162–167. [Google Scholar] [PubMed]
- Burgos, J.; Los-Arcos, I.; de la Sierra, D.A.; Falco, V.; Aguilo, A.; Sanchez, I.; Almirante, B.; Martinez-Gallo, M. Determination of neutrophil CD64 expression as a prognostic biomarker in patients with community-acquired pneumonia. Eur. J. Clin. Microbiol. Infect. Dis. 2016, 35, 1411–1416. [Google Scholar] [CrossRef] [PubMed]
- Querol-Ribelles, J.M.; Tenias, J.M.; Grau, E.; Querol-Borras, J.M.; Climent, J.L.; Gomez, E.; Martinez, I. Plasma d-dimer levels correlate with outcomes in patients with community-acquired pneumonia. Chest 2004, 126, 1087–1092. [Google Scholar] [CrossRef] [PubMed]
- Zhao, T.; Zheng, Y.; Hao, D.; Jin, X.; Luo, Q.; Guo, Y.; Li, D.; Xi, W.; Xu, Y.; Chen, Y.; et al. Blood circRNAs as biomarkers for the diagnosis of community-acquired pneumonia. J. Cell. Biochem. 2019, 120, 16483–16494. [Google Scholar] [CrossRef]
- Scicluna, B.P.; Klein Klouwenberg, P.M.; van Vught, L.A.; Wiewel, M.A.; Ong, D.S.; Zwinderman, A.H.; Franitza, M.; Toliat, M.R.; Nürnberg, P.; Hoogendijk, A.J.; et al. A molecular biomarker to diagnose community-acquired pneumonia on intensive care unit admission. Am. J. Respir. Crit. Care Med. 2015, 192, 826–835. [Google Scholar] [CrossRef]
- Huang, S.; Feng, C.; Zhai, Y.Z.; Zhou, X.; Li, B.; Wang, L.L.; Chen, W.; Lv, F.Q.; Li, T.S. Identification of miRNA biomarkers of pneumonia using RNA sequencing and bioinformatics analysis. Exp. Ther. Med. 2017, 13, 1235–1244. [Google Scholar] [CrossRef]
- Holzinger, D.; Jorns, C.; Stertz, S.; Boisson-Dupuis, S.; Thimme, R.; Weidmann, M.; Kochs, G. Induction of MxA gene expression by influenza A virus requires type I or type III interferon signaling. J. Virol. 2007, 81, 7776–7785. [Google Scholar] [CrossRef] [PubMed]
- Hoshina, T.; Nanishi, E.; Kanno, S.; Nishio, H.; Kusuhara, K.; Hara, T. The utility of biomarkers in differentiating bacterial from non-bacterial lower respiratory tract infection in hospitalized children: Difference of the diagnostic performance between acute pneumonia and bronchitis. J. Infect. Chemother. 2014, 20, 616–620. [Google Scholar] [CrossRef]
- Angus, D.C.; Yang, L.; Kong, L.; Kellum, J.A.; Delude, R.L.; Tracey, K.J.; GenIMS Investigators. Circulating high-mobility group box 1 (HMGB1) concentrations are elevated in both uncomplicated pneumonia and pneumonia with severe sepsis. Crit. Care Med. 2007, 35, 1061–1067. [Google Scholar] [CrossRef]
- Summah, H.; Qu, J.M. Biomarkers: A definite plus in pneumonia. Mediat. Inflamm. 2009, 2009, 675753. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ozkan, S.; Kahveci, U.; Hur, I.; Halici, A. Prognostic importance of serum presepsin level in pneumonia focal sepsis and its relationship with other biomarkers and clinical severity scores. Saudi Med. J. 2021, 42, 994–1001. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Klouche, K.; Cristol, J.P.; Devin, J.; Gilles, V.; Kuster, N.; Larcher, R.; Amigues, L.; Corne, P.; Jonquet, O.; Dupuy, A.M. Diagnostic and prognostic value of soluble CD14 subtype (Presepsin) for sepsis and community-acquired pneumonia in ICU patients. Ann. Intensive Care 2016, 6, 59. [Google Scholar] [CrossRef] [PubMed]
- Yu, B.; Li, X.; Chen, J.; Ouyang, M.; Zhang, H.; Zhao, X.; Tang, J. Evaluation of variation in D-dimer levels among COVID-19 and bacterial pneumonia: A retrospective analysis. J. Thromb. Thrombolysis 2020, 50, 548–557. [Google Scholar] [CrossRef] [PubMed]
- Ozen, M.; Yilmaz, A.; Cakmak, V.; Beyoglu, R.; Oskay, A.; Seyit, M.; Senol, H. D-Dimer as a potential biomarker for disease severity in COVID-19. Am. J. Emerg. Med. 2021, 40, 55–59. [Google Scholar] [CrossRef] [PubMed]
- da Silva-Neto, P.V.; do Valle, V.B.; Fuzo, C.A.; Fernandes, T.M.; Toro, D.M.; Fraga-Silva, T.F.C.; Basile, P.A.; de Carvalho, J.C.S.; Pimentel, V.E.; Pérez, M.M.; et al. Matrix Metalloproteinases on Severe COVID-19 Lung Disease Pathogenesis: Cooperative Actions of MMP-8/MMP-2 Axis on Immune Response through HLA-G Shedding and Oxidative Stress. Biomolecules 2022, 12, 604. [Google Scholar] [CrossRef]
- Wang, F.; Yang, S.; Liu, C.; Xu, Z.; Jia, K.K.; Zhou, J.S.; Cui, L.Y. Matrix Metalloproteinase 3: A Novel Effective Biomarker for Predicting the Mortality and the Severity of Pneumonia. Clin. Lab. 2022, 68, 43. [Google Scholar] [CrossRef]
- Min, J.H.; Lee, H.; Chung, S.J.; Yeo, Y.; Park, T.S.; Park, D.W.; Moon, J.Y.; Kim, S.H.; Kim, T.H.; Sohn, J.W.; et al. Neutrophil Gelatinase-Associated Lipocalin for Predicting Intensive Care Unit Admission and Mortality in Patients with Pneumonia. Tohoku J. Exp. Med. 2020, 250, 243–251. [Google Scholar] [CrossRef]
- Švitek, L.; Zlosa, M.; Grubišić, B.; Kralik, K.; Perić, N.; Berišić, B.; Lišnjić, D.; Mandić, S. Urinary Neutrophil Gelatinase-Associated Lipocalin as a Predictor of COVID-19 Mortality in Hospitalized Patients. Acta Microbiol. Hell. 2024, 69, 224–235. [Google Scholar] [CrossRef]
- Satam, H.; Joshi, K.; Mangrolia, U.; Waghoo, S.; Zaidi, G.; Rawool, S.; Thakare, R.P.; Banday, S.; Mishra, A.K.; Das, G.; et al. Next-Generation Sequencing Technology: Current Trends and Advancements. Biology 2023, 12, 997. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhang, P.; Liu, B.; Zhang, S.; Chang, X.; Zhang, L.; Gu, D.; Zhang, X. Clinical application of targeted next-generation sequencing in severe pneumonia: A retrospective review. Crit. Care 2024, 28, 225. [Google Scholar] [CrossRef]
- Wang, Y.; Wu, Y.; Cao, L.; Niu, W. Application of metagenomic next-generation sequencing in the etiological diagnosis of refractory pneumonia in children. Front. Microbiol. 2024, 15, 1357372. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Ma, X.; Zhou, J.; Deng, J.; Gu, C.; Fei, C.; Cao, L.; Zhang, Q.; Tao, F. Clinical application of metagenomic next-generation sequencing technology in the diagnosis and treatment of pulmonary infection pathogens: A prospective single-center study of 138 patients. J. Clin. Lab. Anal. 2022, 36, e24498. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wang, H.; Lu, Z.; Bao, Y.; Yang, Y.; de Groot, R.; Dai, W.; de Jonge, M.I.; Zheng, Y. Clinical diagnostic application of metagenomic next-generation sequencing in children with severe nonresponding pneumonia. PLoS ONE 2020, 15, e0232610. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chen, Y.; Fan, L.C.; Chai, Y.H.; Xu, J.F. Advantages and challenges of metagenomic sequencing for the diagnosis of pulmonary infectious diseases. Clin. Respir. J. 2022, 16, 646–656. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Liu, H.; Zhang, Y.; Chen, G.; Sun, S.; Wang, J.; Chen, F.; Liu, C.; Zhuang, Q. Diagnostic Significance of Metagenomic Next-Generation Sequencing for Community-Acquired Pneumonia in Southern China. Front. Med. 2022, 9, 807174. [Google Scholar] [CrossRef]
- Huang, J.; Jiang, E.; Yang, D.; Wei, J.; Zhao, M.; Feng, J.; Cao, J. Metagenomic Next-Generation Sequencing versus Traditional Pathogen Detection in the Diagnosis of Peripheral Pulmonary Infectious Lesions. Infect. Drug Resist. 2020, 13, 567–576. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Overbeek, R.; Leitl, C.J.; Stoll, S.E.; Wetsch, W.A.; Kammerer, T.; Mathes, A.; Böttiger, B.W.; Seifert, H.; Hart, D.; Dusse, F. The Value of Next-Generation Sequencing in Diagnosis and Therapy of Critically Ill Patients with Suspected Bloodstream Infections: A Retrospective Cohort Study. J. Clin. Med. 2024, 13, 306. [Google Scholar] [CrossRef]
- Bălan, A.-M.; Bodolea, C.; Trancă, S.D.; Hagău, N. Trends in Molecular Diagnosis of Nosocomial Pneumonia Classic PCR vs. Point-of-Care PCR: A Narrative Review. Healthcare 2023, 11, 1345. [Google Scholar] [CrossRef]
- Lin, W.H.; Chiu, H.C.; Chen, K.F.; Tsao, K.C.; Chen, Y.Y.; Li, T.H.; Huang, Y.C.; Hsieh, Y.C. Molecular detection of respiratory pathogens in community-acquired pneumonia involving adults. J. Microbiol. Immunol. Infect. 2022, 55, 829–837. [Google Scholar] [CrossRef] [PubMed]
- Gadsby, N.J.; Russell, C.D.; McHugh, M.P.; Mark, H.; Conway Morris, A.; Laurenson, I.F.; Hill, A.T.; Templeton, K.E. Comprehensive Molecular Testing for Respiratory Pathogens in Community-Acquired Pneumonia. Clin. Infect. Dis. 2016, 62, 817–823. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Candel, F.J.; Salavert, M.; Basaras, M.; Borges, M.; Cantón, R.; Cercenado, E.; Cilloniz, C.; Estella, Á.; García-Lechuz, J.M.; Garnacho Montero, J.; et al. Ten Issues for Updating in Community-Acquired Pneumonia: An Expert Review. J. Clin. Med. 2023, 12, 6864. [Google Scholar] [CrossRef] [PubMed]
- Anwar, S.; Raut, R.; Kanwal, B.; Yahia, E.A. Vitamin B 12 deficiency and increased susceptibility and severity of COVID-19: A review. Int. J. Creat. Res. Thoughts 2022, 10, 623–651. [Google Scholar]
- Gattinoni, L.; Gattarello, S.; Steinberg, I.; Busana, M.; Palermo, P.; Lazzari, S.; Romitti, F.; Quintel, M.; Meissner, K.; Marini, J.J.; et al. COVID-19 pneumonia: Pathophysiology and management. Eur. Respir. Rev. 2021, 30, 210138. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mohammed, S.A.; Tawfeeq, A.A.; Noraldin, M.Y. Identification and antibiotics Sensitivity of Secondary Bacterial Infection in COVID-19 (SARS-CoV-2) Pneumonia patients in Kirkuk/Iraq. NTU J. Pure Sci. 2023, 2. [Google Scholar] [CrossRef]
- Pourajam, S.; Kalantari, E.; Talebzadeh, H.; Mellali, H.; Sami, R.; Soltaninejad, F.; Amra, B.; Sajadi, M.; Alenaseri, M.; Kalantari, F.; et al. Secondary Bacterial Infection and Clinical Characteristics in Patients With COVID-19 Admitted to Two Intensive Care Units of an Academic Hospital in Iran During the First Wave of the Pandemic. Front. Cell. Infect. Microbiol. 2022, 12, 784130. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Aktiz Bıçak, E.; Oğlak, S.C. Clinical characterisation and management outcome of obstetric patients following intensive care unit admission for COVID-19 pneumonia. J. Obstet. Gynaecol. 2023, 43, 2218915. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, Y. A review of Janus kinase inhibitors for the treatment of COVID-19 pneumonia. Inflamm. Regener. 2023, 43, 3. [Google Scholar] [CrossRef] [PubMed]
- van der Ven, F.S.; Blok, S.G.; Azevedo, L.C.; Bellani, G.; Botta, M.; Estenssoro, E.; Fan, E.; Ferreira, J.C.; Laffey, J.G.; Martin–Loeches, I.; et al. Epidemiology, ventilation management and outcomes of COVID–19 ARDS patients versus patients with ARDS due to pneumonia in the Pre–COVID era. Respir. Res. 2024, 25, 312. [Google Scholar] [CrossRef]
- Li, H.; Jia, X.; Wang, Y.; Lv, Y.; Wang, J.; Zhai, Y.; Xue, X. Differences in the severity and mortality risk factors for patients hospitalized for COVID-19 pneumonia between the early wave and the very late stage of the pandemic. Front. Med. 2023, 10, 1238713. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Le, D.T.; Vu, V.H.; Nguyen, D.H.; Vo, D.T.; Pham, Q.D.D.; Nguyen, K.D.; Truong, B.Q. Late Onset of Organizing Pneumonia Following SARS-CoV-2 Infection: A Case Report of Successful Management and Review Literature. Clin. Med. Insights Case Rep. 2023, 16, 11795476231152166. [Google Scholar] [CrossRef]
- Nestler, M.J.; Godbout, E.; Lee, K.; Kim, J.; Noda, A.J.; Taylor, P.; Pryor, R.; Markley, J.D.; Doll, M.; Bearman, G.; et al. Impact of COVID-19 on pneumonia-focused antibiotic use at an academic medical center. Infect. Control Hosp. Epidemiol. 2021, 42, 915–916. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hussien, S.M. The immunomodulatory properties of low-level ionizing radiation as a potential treatment for COVID-19’s life-threatening symptoms. Eur. J. Med. Res. 2023, 28, 73. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Akinosoglou, K.; Kapsokosta, G.; Mouktaroudi, M.; Rovina, N.; Kaldis, V.; Stefos, A.; Kontogiorgi, M.; Giamarellos-Bourboulis, E.; Gogos, C.; Hellenic Sepsis Study Group. Diabetes on sepsis outcomes in non-ICU patients: A cohort study and review of the literature. J. Diabetes Complicat. 2021, 35, 107765. [Google Scholar] [CrossRef] [PubMed]
- Akinosoglou, K.; Schinas, G.; Bletsa, E.; Bristianou, M.; Lanaras, L.; Michailides, C.; Katsikas, T.; Barkas, F.; Liberopoulos, E.; Kotsis, V.; et al. COVID-19 Outcomes and Diabetes Mellitus: A Comprehensive Multicenter Prospective Cohort Study. Microorganisms 2023, 11, 1416. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chinen, J.; Shearer, W.T. Secondary immunodeficiencies, including HIV infection. J. Allergy Clin. Immunol. 2010, 125 (Suppl. S2), S195–S203. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Avari, P.; Devendra, S. Human immunodeficiency virus and type 2 diabetes. London J. Prim. Care 2017, 9, 38–42. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chireshe, R.; Manyangadze, T.; Naidoo, K. Diabetes mellitus and associated factors among HIV-positive patients at primary health care facilities in Harare, Zimbabwe: A descriptive cross-sectional study. BMC Prim. Care 2024, 25, 28. [Google Scholar] [CrossRef]
- Reichardt, S.D.; Amouret, A.; Muzzi, C.; Vettorazzi, S.; Tuckermann, J.P.; Lühder, F.; Reichardt, H.M. The Role of Glucocorticoids in Inflammatory Diseases. Cells 2021, 10, 2921. [Google Scholar] [CrossRef]
- Okais, J.; Fayad, F.; Baddoura, R.; Tabesh, O.A.; Aouad, K.; Ghoubar, M.; Sunna, N.; Mysler, E. Association between Diabetes andRheumatoid Arthritis: A Systematic Literature Review. Open Rheumatol. J. 2022, 16, e187431292212020. [Google Scholar] [CrossRef]
- Angelopoulos, T.P.; Tentolouris, N.K.; Bertsias, G.K.; Boumpas, D.T. Steroid-induced diabetes in rheumatologic patients. Clin. Exp. Rheumatol. 2014, 32, 126–130. [Google Scholar] [PubMed]
- Gupta, V.; Santhi, S.S.; Ravi, S.; Ramanan, E.A. Rheumatological and musculoskeletal complications in diabetes patients. J. Endocrinol. Metab. 2022, 12, 117–124. [Google Scholar] [CrossRef]

| Risk Factor | Study | Total Subjects | Conclusion | Reference |
|---|---|---|---|---|
| Hyperglycemia | A retrospective cohort study | 1318 | An increase in blood glucose marks severity of CAP in patients without DM. | [40] |
| Glycemic variability | A retrospective study | 282 | Pneumonia patients in critical condition should have their early phase GV closely monitored. | [41] |
| Oxidative stress | A patient follow-up study | 54 | Damage to the redox state of erythrocytes and blood plasma components is crucial for the initiation and advancement of CAP processes. | [42] |
| Glycation and advanced glycation endproducts | Prospective study | 500 | In this cohort, AGER SNP rs2070600 (Ser/Ser) was linked to a greater plasma sRAGE and an elevated risk of ARDS. | [43] |
| Abnormal leucocyte | A retrospective case–control study | 444 | AECOPD was more likely to occur in patients with a monocyte proportion of >10% or <7.4% with an absolute count <0.62. | [44] |
| Impaired complement | A cross-sectional study | 285 | The severity of CAP patients is positively correlated with serum complement C3a at admission. Complement C3a is implicated in the pathophysiology of CAP, as evidenced by the attenuation of S. pneumoniae-induced inflammatory cytokine production in pulmonary epithelial cells with complement system inhibition. | [45] |
| Antibody response | A randomized, double-blind, placebo-controlled trial | 270 | Gimsilumab (a monoclonal antibody) did not reduce mortality or other important clinical outcomes in patients who had indications of systemic inflammation and COVID-19 pneumonia. | [46] |
| Micronutrient deficiency | A Nigerian tertiary health center | 144 | Incidence and severity of pneumonia in children from Nigeria were linked to low serum micronutrient levels, specifically zinc and vitamin A. | [47] |
| Metformin use | A retrospective analysis | 22,638 | Among Chinese people with diabetes, long-term metformin treatment was linked to a lower risk of pneumonia and pneumonia-related mortality. | [48] |
| Class of Biomarker | Name of Biomarker | Study Type and ID | Conclusion of Study | Reference |
|---|---|---|---|---|
| Inflammatory biomarker | Procalcitonin (PCT) | A prospective, international, study | Pneumonia diagnosis may be aided by procalcitonin, especially in patients with a high diagnostic ambiguity. | [167] |
| Inflammatory biomarker | CRP | Prospective hospital-based study | Pneumonia may use CRP as a clinical measure instead of TNF-alpha or IL-6. | [168] |
| Inflammatory biomarker | CRP | A prospective study | When treating pneumonia patients, serum CRP can help differentiate between endobronchial and parenchymal infections. | [169] |
| Inflammatory biomarker | Soluble triggering receptor expressed on myeloid cells-1 (sTREM-1) | A case–control study | In children who have undergone MV, serum sTREM-1 levels are a trustworthy biomarker for predicting VAP. | [170] |
| Inflammatory biomarker | Proadrenomedullin (proADM) | A prospective cohort study | Particularly in radiographic CAP, ProADM was linked to severe disease and distinguished between children who were reasonably well and those who did not acquire severe disease. | [171] |
| Inflammatory biomarker | MR-proANP (pro-atrial natriuretic peptide) | Prospective observational cohort study | MR-proANP levels are independent predictors of mortality in VAP and rise gradually with the severity of sepsis. | [172] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Anwar, S.; Alhumaydhi, F.A.; Rahmani, A.H.; Kumar, V.; Alrumaihi, F. A Review on Risk Factors, Traditional Diagnostic Techniques, and Biomarkers for Pneumonia Prognostication and Management in Diabetic Patients. Diseases 2024, 12, 310. https://doi.org/10.3390/diseases12120310
Anwar S, Alhumaydhi FA, Rahmani AH, Kumar V, Alrumaihi F. A Review on Risk Factors, Traditional Diagnostic Techniques, and Biomarkers for Pneumonia Prognostication and Management in Diabetic Patients. Diseases. 2024; 12(12):310. https://doi.org/10.3390/diseases12120310
Chicago/Turabian StyleAnwar, Shehwaz, Fahad A. Alhumaydhi, Arshad Husain Rahmani, Vikalp Kumar, and Faris Alrumaihi. 2024. "A Review on Risk Factors, Traditional Diagnostic Techniques, and Biomarkers for Pneumonia Prognostication and Management in Diabetic Patients" Diseases 12, no. 12: 310. https://doi.org/10.3390/diseases12120310
APA StyleAnwar, S., Alhumaydhi, F. A., Rahmani, A. H., Kumar, V., & Alrumaihi, F. (2024). A Review on Risk Factors, Traditional Diagnostic Techniques, and Biomarkers for Pneumonia Prognostication and Management in Diabetic Patients. Diseases, 12(12), 310. https://doi.org/10.3390/diseases12120310







