The Influence of Personality Traits on Postpartum Depression: A Systematic Review Based on the NEO-FFI Scale
Abstract
1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Information Sources
2.3. Search Strategy
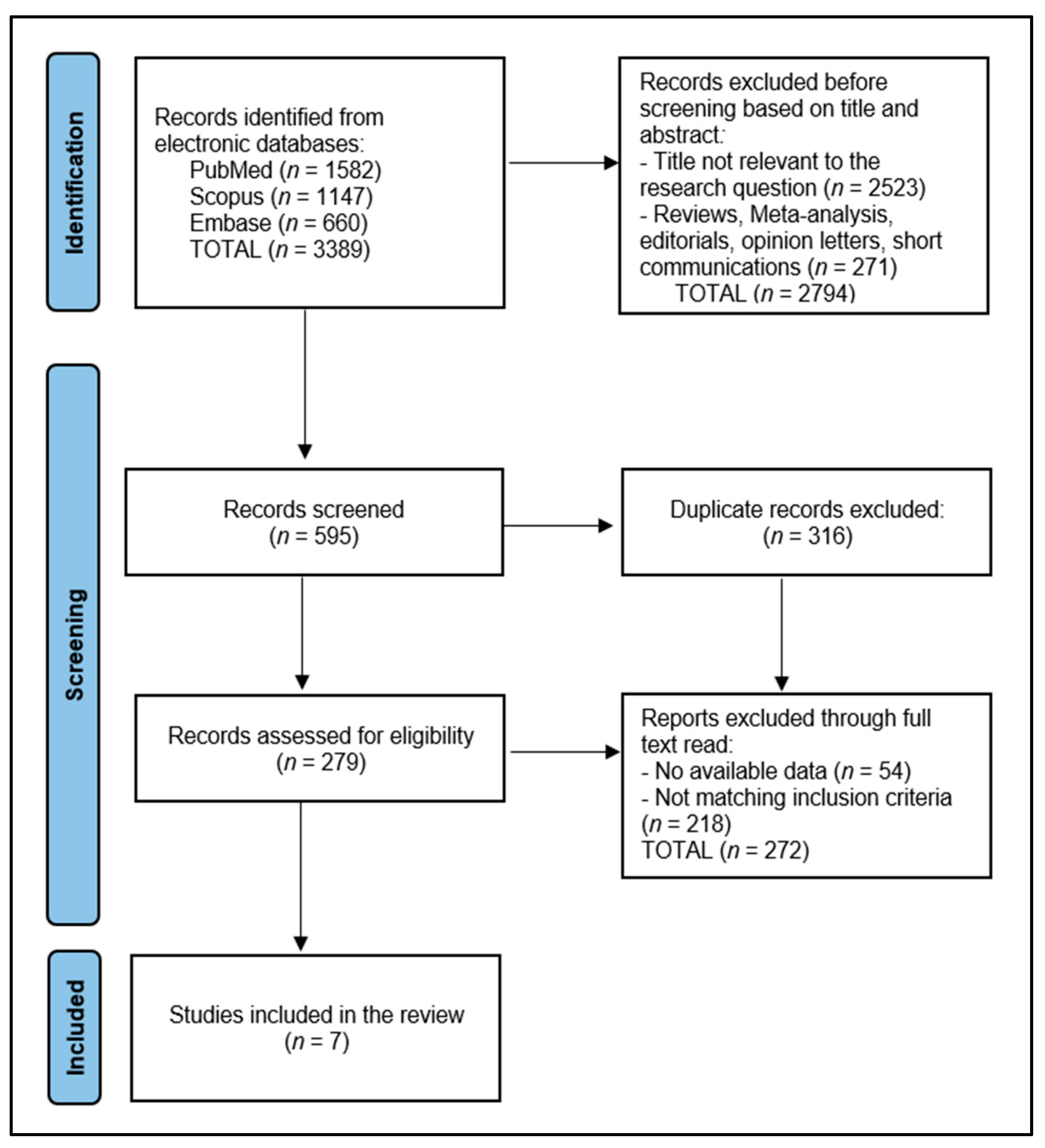
2.4. Selection Process
2.5. Data Selection Process and Quality Assessment
2.6. Data Items
3. Results
3.1. Study Characteristics
3.2. Patients’ Characteristics
3.3. Pregnancy Characteristics
3.4. NEO-FFI Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Suryawanshi, O., 4th; Pajai, S. A Comprehensive Review on Postpartum Depression. Cureus 2022, 14, e32745. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Atuhaire, C.; Rukundo, G.Z.; Nambozi, G.; Ngonzi, J.; Atwine, D.; Cumber, S.N.; Brennaman, L. Prevalence of postpartum depression and associated factors among women in Mbarara and Rwampara districts of south-western Uganda. BMC Pregnancy Childbirth 2021, 21, 503. [Google Scholar] [CrossRef] [PubMed]
- Saharoy, R.; Potdukhe, A.; Wanjari, M.; Taksande, A.B. Postpartum Depression and Maternal Care: Exploring the Complex Effects on Mothers and Infants. Cureus 2023, 15, e41381. [Google Scholar] [CrossRef] [PubMed]
- Oşvar, F.N.; Raţiu, A.C.; Voiţă-Mekereş, F.; Voiţă, G.F.; Bonţea, M.G.; Racoviţă, M.; Mekereş, G.M.; Bodog, F.D. Cardiac axis evaluation as a screening method for detecting cardiac abnormalities in the first trimester of pregnancy. Rom. J. Morphol. Embryol. 2020, 61, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Hrubaru, I.; Motoc, A.; Bratosin, F.; Rosca, O.; Folescu, R.; Moise, M.L.; Neagoe, O.; Citu, I.M.; Feciche, B.; Gorun, F.; et al. Exploring Clinical and Biological Features of Premature Births among Pregnant Women with SARS-CoV-2 Infection during the Pregnancy Period. J. Pers. Med. 2022, 12, 1871. [Google Scholar] [CrossRef] [PubMed]
- Slomian, J.; Honvo, G.; Emonts, P.; Reginster, J.-Y.; Bruyère, O. Consequences of maternal postpartum depression: A systematic review of maternal and infant outcomes. Women’s Health 2019, 15, 1745506519844044. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bellomo, A.; Severo, M.; Petito, A.; Nappi, L.; Iuso, S.; Altamura, M.; Marconcini, A.; Giannaccari, E.; Maruotti, G.; Palma, G.L.; et al. Perinatal depression screening and prevention: Descriptive findings from a multicentric program in the South of Italy. Front. Psychiatry 2022, 13, 962948. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Podolska, M.Z.; Bidzan, M.; Majkowicz, M.; Podolski, J.; Sipak-Szmigiel, O.; Ronin-Walknowska, E. Personality traits assessed by the NEO Five-Factor Inventory (NEO-FFI) as part of the perinatal depression screening program. Med. Sci. Monit. 2010, 16, PH77–PH81. [Google Scholar] [PubMed]
- Shuai, Y.; Wang, S.; Liu, X.; Kueh, Y.C.; Kuan, G. The influence of the five-factor model of personality on performance in competitive sports: A review. Front. Psychol. 2023, 14, 1284378. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dong, J.; Xiao, T.; Xu, Q.; Liang, F.; Gu, S.; Wang, F.; Huang, J.H. Anxious Personality Traits: Perspectives from Basic Emotions and Neurotransmitters. Brain Sci. 2022, 12, 1141. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nieto, M.; Visier, M.E.; Silvestre, I.N.; Navarro, B.; Serrano, J.P.; Martínez-Vizcaíno, V. Relation between resilience and personality traits: The role of hopelessness and age. Scand. J. Psychol. 2023, 64, 53–59. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lica, M.M.; Papai, A.; Salcudean, A.; Crainic, M.; Covaciu, C.G.; Mihai, A. Assessment of Psychopathology inAdolescents with Insulin-Dependent Diabetes (IDD) and the Impact on Treatment Management. Children 2021, 8, 414. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Han, L.; Zhang, J.; Yang, J.; Yang, X.; Bai, H. Between Personality Traits and Postpartum Depression: The Mediated Role of Maternal Self-Efficacy. Neuropsychiatr. Dis. Treat. 2022, 18, 597–609. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bînă, A.M.; Sturza, A.; Iancu, I.; Mocanu, A.G.; Bernad, E.; Chiriac, D.V.; Borza, C.; Craina, M.L.; Popa, Z.L.; Muntean, D.M.; et al. Placental oxidative stress and monoamine oxidase expression are increased in severe preeclampsia: A pilot study. Mol. Cell. Biochem. 2022, 477, 2851–2861. [Google Scholar] [CrossRef] [PubMed]
- Homorogan, C.; Enatescu, V.R.; Nitusca, D.; Marcu, A.; Seclaman, E.; Marian, C. Distribution of microRNAsassociated with major depressive disorder among blood compartments. J. Int. Med. Res. 2021, 49, 03000605211006633. [Google Scholar] [CrossRef] [PubMed]
- Ciolac, L.; Craina, M.L.; Enatescu, V.R.; Tudor, A.; Bernad, E.S.; Nitu, R.; Hogea, L.; Boscu, L.; Bernad, B.-C.; Timircan, M.O.; et al. The Impact of the COVID-19 Pandemic on Depressive Disorder with Postpartum Onset: A Cross-Sectional Study. Healthcare 2023, 11, 2857. [Google Scholar] [CrossRef] [PubMed]
- Răchită, A.; Strete, G.E.; Suciu, L.M.; Ghiga, D.V.; Sălcudean, A.; Mărginean, C. Psychological StressPerceived by Pregnant Women in the Last Trimester of Pregnancy. Int. J. Environ. Res. Public Health 2022, 19, 8315. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Asselmann, E.; Garthus-Niegel, S.; Martini, J. Personality impacts fear of childbirth and subjective birth experiences: A prospective-longitudinal study. PLoS ONE 2021, 16, e0258696. [Google Scholar] [CrossRef] [PubMed]
- Alves, A.C.; Souza, R.T.; Mayrink, J.; Galvao, R.B.; Costa, M.L.; Feitosa, F.E.; Filho, E.A.R.; Leite, D.F.; Tedesco, R.P.; Santana, D.S.; et al. Measuring resilience and stress during pregnancy and its relation to vulnerability and pregnancy outcomes in a nulliparous cohort study. BMC Pregnancy Childbirth 2023, 23, 396. [Google Scholar] [CrossRef] [PubMed]
- Martín-Santos, R.; Gelabert, E.; Subirà, S.; Gutierrez-Zotes, A.; Langorh, K.; Jover, M.; Torrens, M.; Guillamat, R.; Mayoral, F.; Canellas, F.; et al. Research letter: Is neuroticism a risk factor for postpartum depression? Psychol. Med. 2012, 42, 1559–1565. [Google Scholar] [CrossRef]
- Iliadis, S.I.; Koulouris, P.; Gingnell, M.; Sylvén, S.M.; Sundström-Poromaa, I.; Ekselius, L.; Papadopoulos, F.C.; Skalkidou, A. Personality and risk for postpartum depressive symptoms. Arch. Women’s Ment. Health 2015, 18, 539–546. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 89. [Google Scholar] [CrossRef] [PubMed]
- Schiavo, J.H. PROSPERO: An International Register of Systematic Review Protocols. Med. Ref. Serv. Q. 2019, 38, 171–180. [Google Scholar] [CrossRef] [PubMed]
- Rosellini, A.J.; Brown, T.A. The NEO Five-Factor Inventory: Latent structure and relationships with dimensions of anxiety and depressive disorders in a large clinical sample. Assessment 2011, 18, 27–38. [Google Scholar] [CrossRef] [PubMed]
- Srkalović, I.; Azijada, D.B.; Iris, S.V.; Livija, Š.; Tanja, J. Multivariate analysis of predictors of depression symptomatology after childbirth. Psychiatr. Danub. 2014, 26 (Suppl. 3), 416–421. [Google Scholar]
- Maliszewska, K.; Mariola, B.; Małgorzata, Ś.-F.; Krzysztof, P. Medical and psychosocial determinants of risk of postpartum depression: A cross-sectional study. Acta Neuropsychiatr. 2017, 29, 347–355. [Google Scholar] [CrossRef] [PubMed]
- Marín-Morales, D.; Carmona-Monge, F.J.; Peñacoba-Puente, C. Personality, depressive symptoms during pregnancy and their influence on postnatal depression in Spanish pregnant Spanish women. [Personalidad, síntomas depresivos en el embarazo y su influencia en la depresión postparto en gestantes españolas]. An. Psicol./Ann. Psychol. 2014, 30, 908–915. [Google Scholar] [CrossRef]
- Maliszewska, K.; Świątkowska-Freund, M.; Bidzan, M.; Krzysztof, P. Screening for maternal postpartum depression and associations with personality traits and social support. A Polish follow-up study 4 weeks and 3 months after delivery. Psychiatr. Pol. 2017, 51, 889–898. [Google Scholar] [CrossRef]
- Tian, T.; Li, Y.; Xie, D.; Shen, Y.; Ren, J.; Wu, W.; Guan, C.; Zhang, Z.; Zhang, D.; Gao, C.; et al. Clinical features and risk factors for post-partum depression in a large cohort of Chinese women with recurrent major depressive disorder. J. Affect. Disord. 2012, 136, 983–987. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Maryami, F.; Maryami, Z.; Bigdeli, I.; Najafi, M.; Kiani, M. The role of social support and personality traits in the incidence of postpartum depression. J. Gorgan Univ. Med. Sci. 2020, 22, 88–94. Available online: https://sid.ir/paper/368789/en (accessed on 23 December 2023).
- Roman, M.; Bostan, C.M.; Diaconu-Gherasim, L.R.; Constantin, T. Personality Traits and Postnatal Depression: The Mediated Role of Postnatal Anxiety and Moderated Role of Type of Birth. Front. Psychol. 2019, 10, 1625. [Google Scholar] [CrossRef] [PubMed]
- Ghaedrahmati, M.; Kazemi, A.; Kheirabadi, G.; Ebrahimi, A.; Bahrami, M. Postpartum depression risk factors: A narrative review. J. Educ. Health Promot. 2017, 6, 60. [Google Scholar] [CrossRef] [PubMed]
- Oancea, R.; Timar, B.; Papava, I.; Cristina, B.A.; Ilie, A.C.; Dehelean, L. Influence of depression and self-esteem on oral health-related quality of life in students. J. Int. Med. Res. 2020, 48, 300060520902615. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, I.; Mehendale, A.M.; Malhotra, R. Risk Factors of Postpartum Depression. Cureus 2022, 14, e30898. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Puyané, M.; Subirà, S.; Torres, A.; Roca, A.; Garcia-Esteve, L.; Gelabert, E. Personality traits as a risk factor for postpartum depression: A systematic review and meta-analysis. J. Affect. Disord. 2022, 298 Pt A, 577–589. [Google Scholar] [CrossRef]
- Chen, J.; Sun, M.; Huang, C.; Xiao, J.; Tang, S.; Chen, Q. Pathways from Neuroticism, Social Support, and Sleep Quality to Antenatal Depression during the Third Trimester of Pregnancy. Int. J. Environ. Res. Public Health 2022, 19, 5602. [Google Scholar] [CrossRef] [PubMed]
- Axfors, C.; Hellgren, C.; Volgsten, H.; Skoog Svanberg, A.; Ekselius, L.; Wikström, A.K.; Ramklint, M.; Skalkidou, A.; Sundström-Poromaa, I. Neuroticism is associated with higher antenatal care utilization in obstetric low-risk women. Acta Obstet. Gynecol. Scand. 2019, 98, 470–478. [Google Scholar] [CrossRef] [PubMed]
- Leikas, S.; Lahti-Pulkkinen, M.; Räikkönen, K. Facet-level changes in mothers’ neuroticism and extraversion from early pregnancy to 6 months post-partum. Eur. J. Pers. 2023, 37, 435–452. [Google Scholar] [CrossRef]
- Serra, R.; Giacchetti, N.; Bersani, F.S.; Cappannini, G.; Martucci, M.; Panfili, M.; Sogos, C.; Aceti, F. The relationship between personality traits and individual factors with perinatal depressive symptoms: A cross-sectional study. BMC Pregnancy Childbirth 2023, 23, 382. [Google Scholar] [CrossRef]
- Van Bussel, J.C.; Spitz, B.; Demyttenaere, K. Depressive symptomatology in pregnant and postpartum women. An exploratory study of the role of maternal antenatal orientations. Arch. Women’s Ment. Health 2009, 12, 155–166. [Google Scholar] [CrossRef] [PubMed]
- Spry, E.A.; Olsson, C.A.; Aarsman, S.R.; Mohamad Husin, H.; Macdonald, J.A.; Dashti, S.G.; Moreno-Betancur, M.; Letcher, P.; Biden, E.J.; Thomson, K.C.; et al. Parental personality and early life ecology: A prospective cohort study from preconception to postpartum. Sci. Rep. 2023, 13, 3332. [Google Scholar] [CrossRef] [PubMed]
| First Author | Country | Year of Publication | Study Design | Quality Assessment |
|---|---|---|---|---|
| Imsiragic et al. [25] | Croatia | 2014 | Prospective cohort | Medium |
| Maliszewska et al. [26] | Poland | 2017 | Cross-sectional | Low |
| Marin-Morales et al. [27] | Spain | 2014 | Prospective cohort | Medium |
| Maliszewska et al. [28] | Poland | 2017 | Cross-sectional | Medium |
| Tian et al. [29] | China | 2012 | Case-control | Medium |
| Farzaneh et al. [30] | Iran | 2020 | Cross-sectional | Low |
| Roman et al. [31] | Romania | 2019 | Cross-sectional | Medium |
| First Author | Number of Patients | Age | Psychiatric/Psychological Assessments | Time of Assessment | Other Characteristics |
|---|---|---|---|---|---|
| Imsiragic et al. [25] | 262 | 30 years (median) | Constant fear of labor outcome: 38.9%; EPDS score: 51.7% clinically significant; IES-R score: 45.6% clinically significant | 3–5 days and 6–9 weeks after delivery | 51.1% had secondary school or less; 24.1% were unemployed. |
| Maliszewska et al. [26] | 387 | 30.37 years (average) | Positive psychiatric history: 7.5%; positive family history: 4.4%; EPDS score: 28.9% clinically significant | 4–8 weeks after delivery | 79.1% had higher education; 9.9% were unemployed; 81.1% were married and primiparous (56.9%). |
| Marin-Morales et al. [27] | 116 | 31.31 years (average) | EPDS score: 19.2% clinically significant; SCL-90 mean score: 0.73 | 1st trimester and 4 months after delivery | 82.8% planned pregnancies; 50.5% multiparous; 27.5% had primary education, 45.4% secondary, and 27.1% university; 65.1% were employed at the time of pregnancy. |
| Maliszewska et al. [28] | 548 | 30.19 years (average) | EPDS score: 10.6% clinically significant; PHQ-9 score: 13.3% clinically significant; 6.25% had a history of psychiatric disorder | 1st week after delivery, 4 weeks, and 3 months after delivery | 80% had higher education; 88% were employed and married (80.1%); 54.2% were primiparas. |
| Tian et al. [29] | 1785 | NR | NR | NR | Postpartum depression risk (OR): age 0.95(0.03–0.06); premenstrual symptoms 1.11(1.07–1.15); education 0.88(0.83–0.93); occupation 0.93(0.88–0.98); lifetime stressful events 1.23(1.15–132); childhood sexual abuse 1.80(1.27–2.54). |
| Farzaneh et al. [30] | 200 | 17–41 (range) | EPDS score: 24.5% clinically significant for depression | 6 weeks to 6 months after delivery | 47.5% had a body mass index (BMI) of less than 18.5 (underweight), 5.5% had more than one child, 81.5% were housewives, and 69.5% had a diploma or higher education. |
| Roman et al. [31] | 672 | 29.33 years (average) | 24.3% had postnatal anxiety | 3–4 days after birth and 2 weeks after delivery | 63.8% lived in urban areas; 40.9% had a college degree or higher; 83% were married |
| First Author | Mode of Delivery | Breastfeeding | Smoking | Other Complications |
|---|---|---|---|---|
| Imsiragic et al. [25] | 78.2% vaginal | 83.3% | NR | Emergency C-section: 10.2%; complications during or after labor: 28.8% |
| Maliszewska et al. [26] | 69.8% vaginal | 82.2% in the first week, 86.3% in the fourth week | 9.54% | C-section: 30.2% |
| Marin-Morales et al. [27] | 51.7% vaginal | NR | NR | APGAR score < 7: 1.7% |
| Maliszewska et al. [28] | 68.7% vaginal | 65.7% | 9.26% | 10.2% preterm delivery; 24.2% hospitalized |
| Tian et al. [29] | NR | NR | NR | NR |
| Farzaneh et al. [30] | NR | NR | NR | There was a significant negative relationship between postpartum depression and social support (r = −0.027, p < 0.01). |
| Roman et al. [31] | 46.1% vaginal | NR | NR | C-section: 53.9% |
| First Author | Neuroticism | Extraversion | Conscientiousness | Openness | Agreeableness |
|---|---|---|---|---|---|
| Imsiragic et al. [25] | 1.07 (0.96–1.20) | 0.95 (0.88–1.03) | 0.97 (0.90–1.04) | 0.98 (0.93–1–04) | 1.04 (0.97–1.12) |
| Maliszewska et al. [26] | 1.87 (1.53–2.27) | 0.69 (0.57–0.82) | 0.79 (0.67–0.92) | 0.84 (0.72–0.99) | 0.87 (0.75–1.01) |
| Marin-Morales et al. [27] | NR | −0.104 (Beta coefficient) | NR | NR | NR |
| Maliszewska et al. [28] | 1.64 (1.34–2.01) | 0.76 (0.58–0.87) | 0.78 (0.66–0.93) | NR | NR |
| Tian et al. [29] | 1.12 (1.09–1.21) | NR | NR | NR | NR |
| Farzaneh et al. [30] | 0.368 (Beta coefficient) | −0.171 (Beta coefficient) | −0.162 (Beta coefficient) | NR | NR |
| Roman et al. [31] | 0.01 (0.03–0.10) | −0.03 (0.02–0.04) | −0.05 (−0.06–0.007) | −0.01(0.02–0.005) | −0.02(−0.02–0.06) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Neda-Stepan, O.; Giurgi-Oncu, C.; Sălcudean, A.; Bernad, E.; Bernad, B.-C.; Enătescu, V.R. The Influence of Personality Traits on Postpartum Depression: A Systematic Review Based on the NEO-FFI Scale. Diseases 2024, 12, 82. https://doi.org/10.3390/diseases12050082
Neda-Stepan O, Giurgi-Oncu C, Sălcudean A, Bernad E, Bernad B-C, Enătescu VR. The Influence of Personality Traits on Postpartum Depression: A Systematic Review Based on the NEO-FFI Scale. Diseases. 2024; 12(5):82. https://doi.org/10.3390/diseases12050082
Chicago/Turabian StyleNeda-Stepan, Oana, Cătălina Giurgi-Oncu, Andreea Sălcudean, Elena Bernad, Brenda-Cristiana Bernad, and Virgil Radu Enătescu. 2024. "The Influence of Personality Traits on Postpartum Depression: A Systematic Review Based on the NEO-FFI Scale" Diseases 12, no. 5: 82. https://doi.org/10.3390/diseases12050082
APA StyleNeda-Stepan, O., Giurgi-Oncu, C., Sălcudean, A., Bernad, E., Bernad, B.-C., & Enătescu, V. R. (2024). The Influence of Personality Traits on Postpartum Depression: A Systematic Review Based on the NEO-FFI Scale. Diseases, 12(5), 82. https://doi.org/10.3390/diseases12050082







