Antibacterial and Wound Healing Activity In Vitro of Individual and Combined Extracts of Tagetes nelsonii Greenm, Agave americana and Aloe vera
Abstract
1. Introduction
2. Materials and Methods
2.1. Plant Material
2.2. Preparation of Plant Extracts
2.3. Phytochemical Analysis
2.4. Identification of Components in Extracts by Gas Chromatography Coupled to Mass Spectrophotometry
2.5. Bacterial Strains
2.6. Determination of Antibacterial Activity Using the Disc Diffusion Method
2.7. Determination of Minimum Inhibitory Concentration (MIC) and Minimum Bactericidal Concentration (MBC)
2.8. Cell Maintenance
2.9. In Vitro Cytotoxicity Assay
2.10. In Vitro Scratch Assay
- 1.5 mL of T. nelsonii extract + 1.5 mL of A. americana extract
- 1.5 mL of T. nelsonii extract + 1.5 mL of A. vera gel
- 1.5 mL of A. americana extract + 1.5 mL of A. vera gel
- 1 mL of T. nelsonii extract + 1 mL of A. americana extract + 1 mL of A. vera gel
2.11. Statistical Analysis
3. Results
3.1. Phytochemical Analysis
3.2. Antimicrobial Activity, Minimum Inhibitory Concentration (MIC), and Minimum Bactericidal Concentration (MBC) of the Plant Extracts
3.3. Identification of Components by Gas Chromatography Coupled to Mass Spectrophotometry (GC-MS)
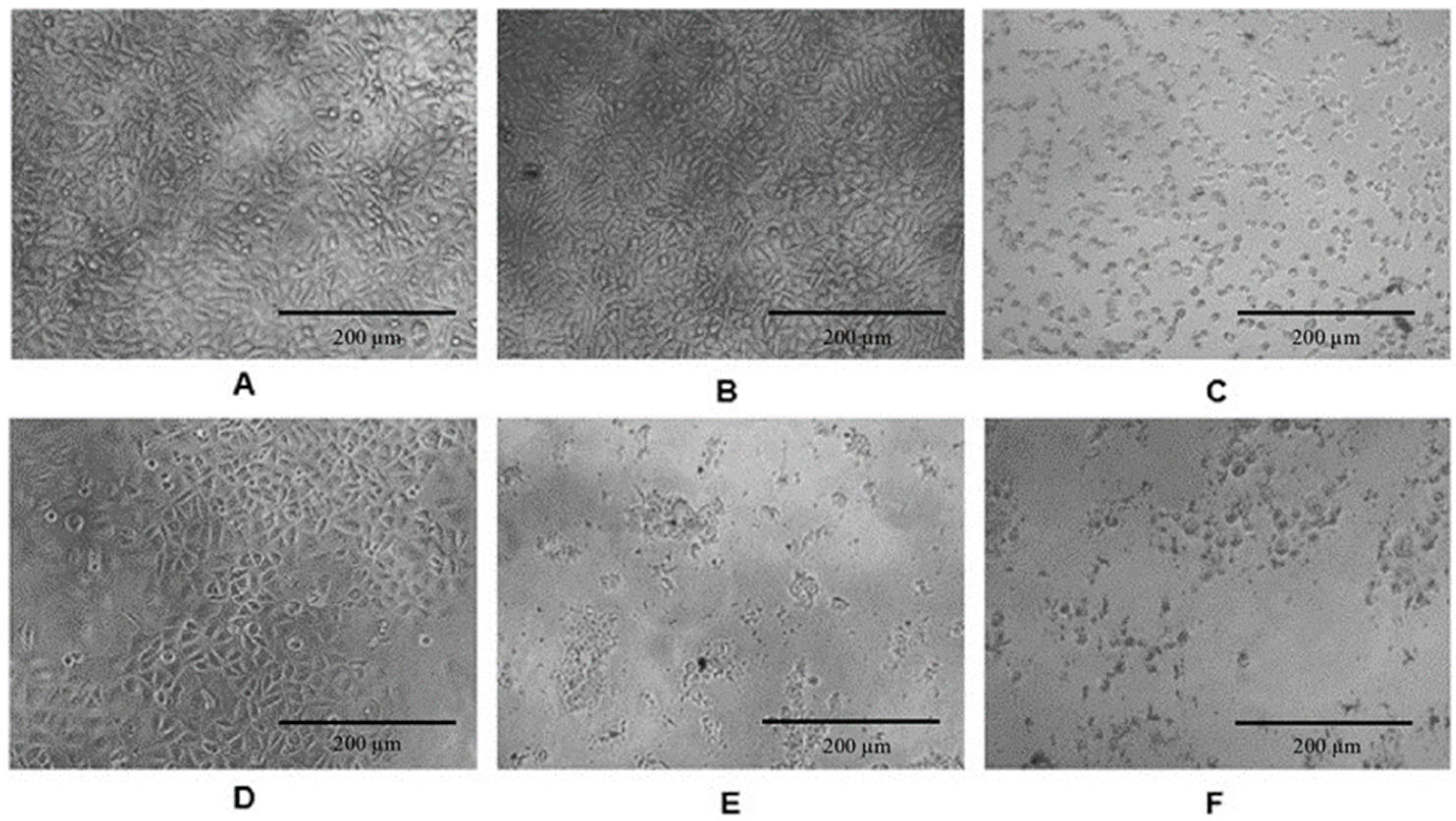
3.4. In Vitro Cytotoxicity of Plant Extracts
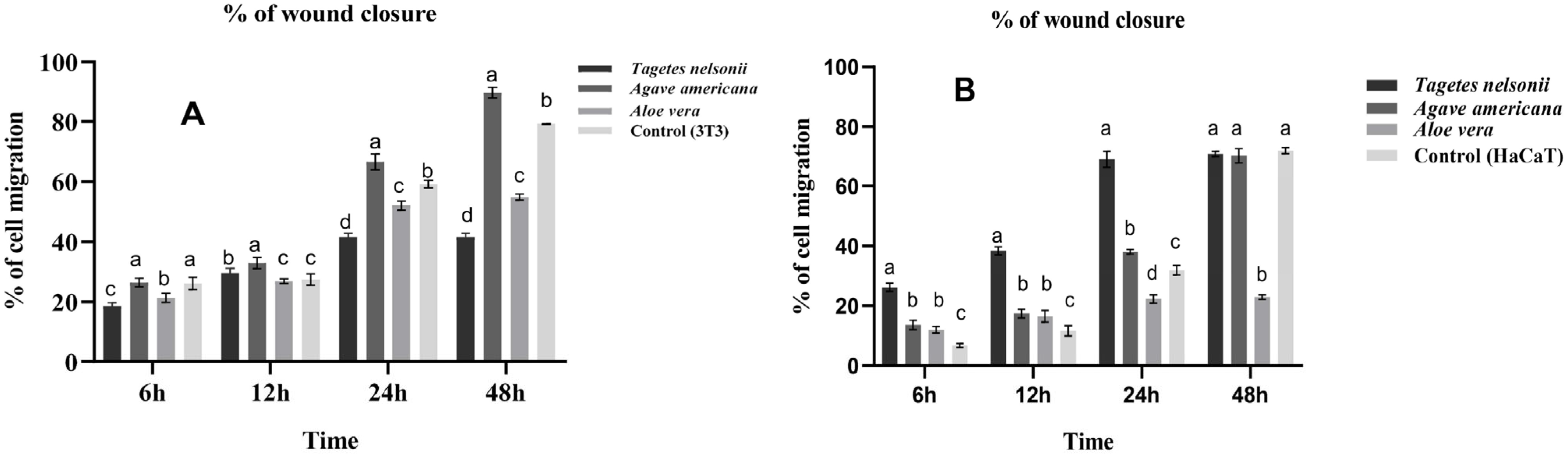
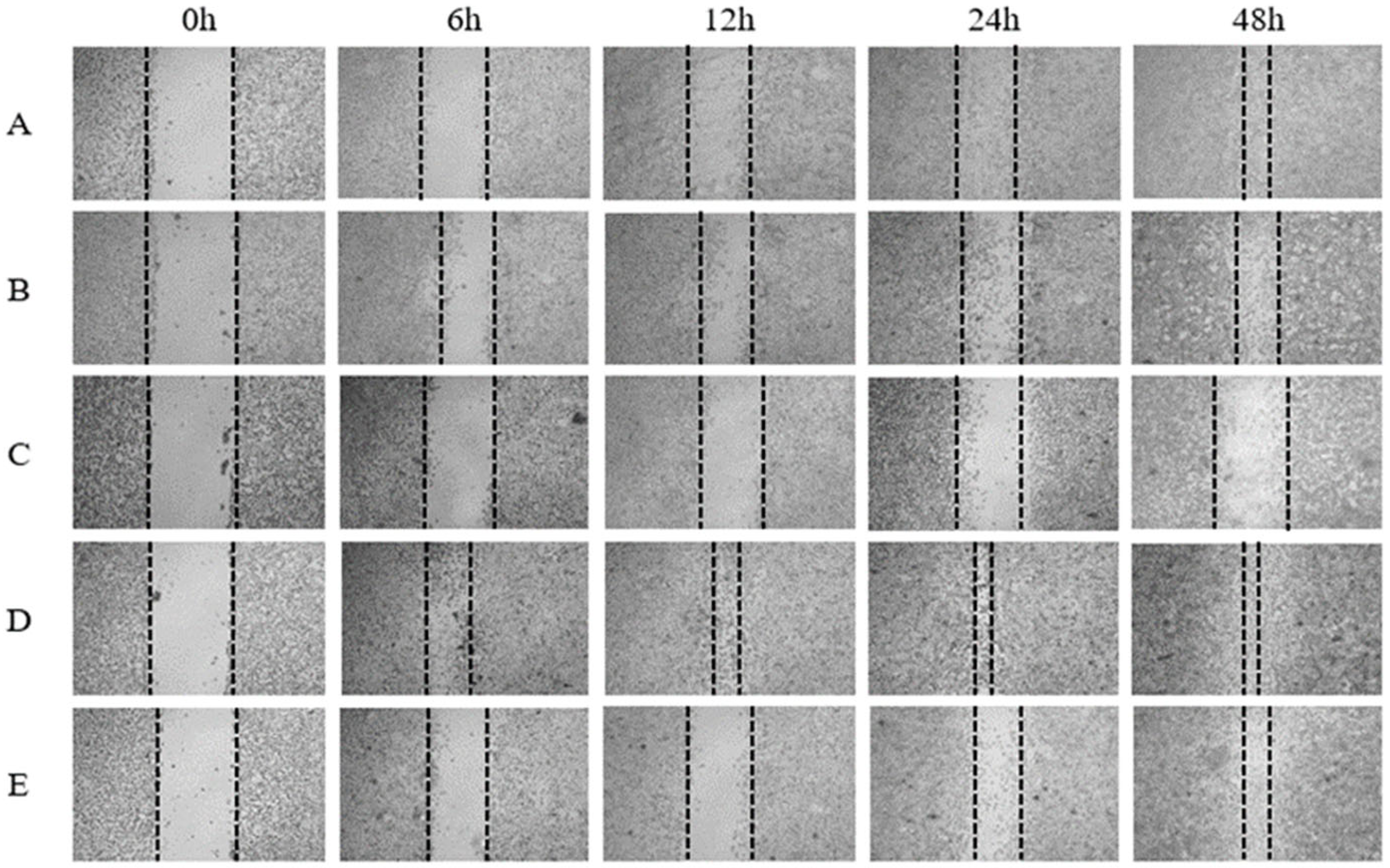
3.5. In Vitro Wound-Healing Activity with Scratch Assay of Individual Plant Extracts
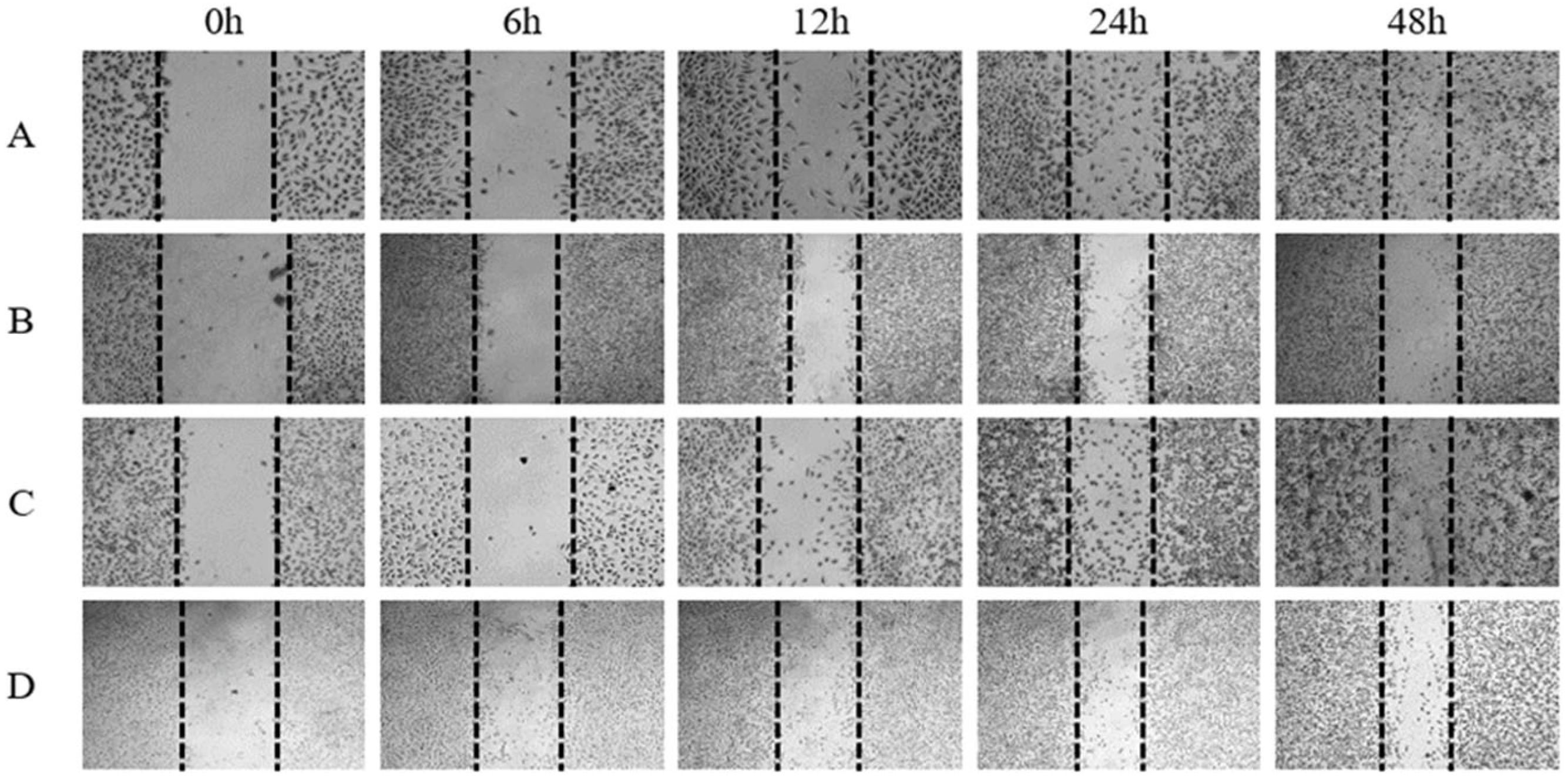
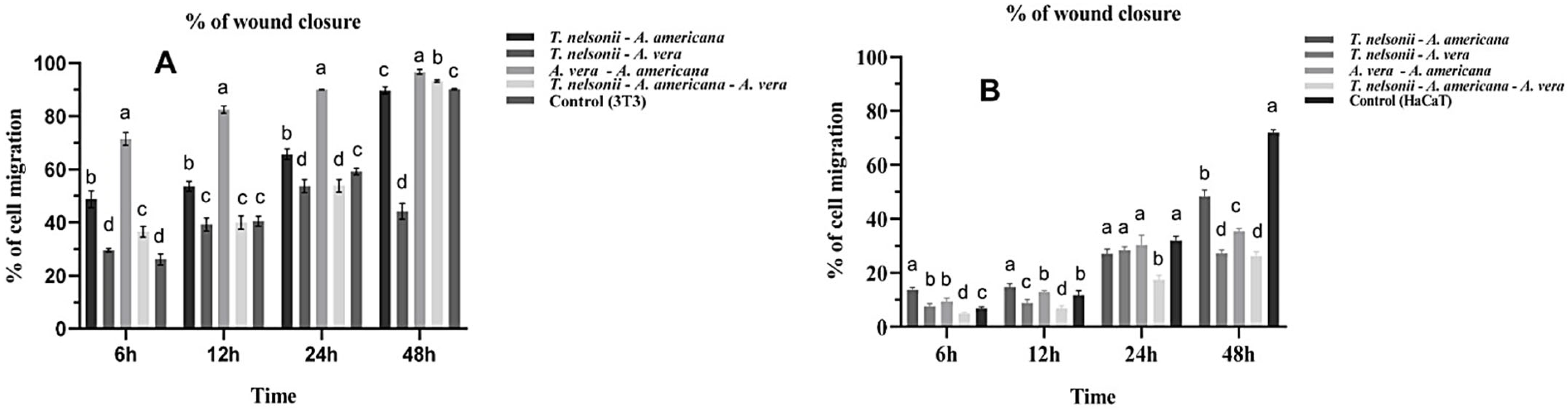
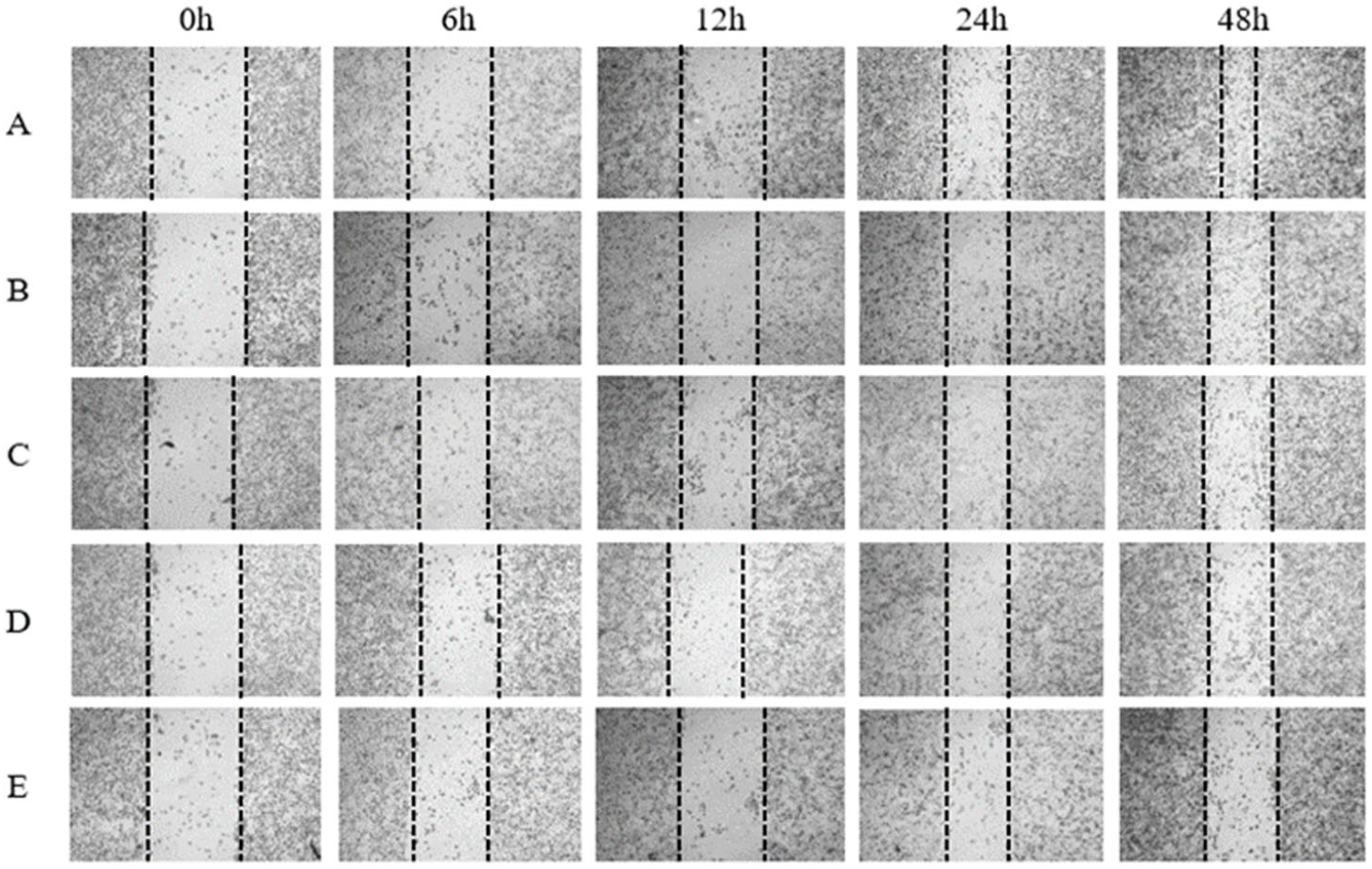
3.6. In Vitro Wound-Healing Activity with Scratch Assay of Combined Plant Extracts
4. Discussion
4.1. Phytochemical Analysis
4.2. Antimicrobial Activity of Plant Extracts
4.3. In Vitro Citotoxicity and Wound-Healing Activity
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chen, K.; Wang, F.; Liu, S.; Wu, X.; Xu, L.; Zhang, D. In situ reduction of silver nanoparticles by sodium alginate to obtain silver-loaded composite wound dressing with enhanced mechanical and antimicrobial property. Int. J. Biol. Macromol. 2020, 148, 501–509. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Han, S.; Gu, Z.; Wu, J. Advances and Impact of Antioxidant Hydrogel in Chronic Wound Healing. Adv. Healthc. Mater. 2020, 9, 1901502. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Young, A.; McNaught, C. The physiology of wound healing. Surgery 2017, 35, 473–477. [Google Scholar] [CrossRef]
- Lawton, S. Skin 1: The structure and functions of the skin. Nurs. Times 2019, 115, 30–33. [Google Scholar]
- Brook, I. Aerobic and Anaerobic Bacteriology of Wounds and Cutaneous Abscesses. Arch. Surg. 1990, 125, 1445. [Google Scholar] [CrossRef] [PubMed]
- Paladini, F.; Pollini, M. Antimicrobial Silver Nanoparticles for Wound Healing Application: Progress and Future Trends. Materials 2019, 16, 2540. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Liang, Y.; Chen, J.; Duan, X.; Guo, B. Mussel-inspired adhesive antioxidant antibacterial hemostatic composite hydrogel wound dressing via photo-polymerization for infected skin wound healing. Bioact. Mater. 2022, 8, 341–354. [Google Scholar] [CrossRef]
- Shedoeva, S.; Leavesley, D.; Upton, Z.; Fan, C. Wound Healing and the Use of Medicinal Plants. J. Evid. Based Complement. Altern. Med. 2019, 1, 1–30. [Google Scholar] [CrossRef]
- Vitale, S.; Colanero, S.; Placidi, M.; Di Emidio, G.; Tatone, C.; Amicarelli, F.; D’Alessandro, A.M. Phytochemistry and Biological Activity of Medicinal Plants in Wound Healing: An Overview of Current Research. Molecules 2022, 27, 3566. [Google Scholar] [CrossRef] [PubMed]
- Albahri, G.; Badran, A.; Hijazi, A.; Daou, A.; Baydoun, E.; Nasser, M.; Merah, O. The Therapeutic Wound Healing Bioactivities of Various Medicinal Plants. Life 2023, 13, 317. [Google Scholar] [CrossRef]
- Carod-Artal, F.J.; Vázquez-Cabrera, C. An Anthropological Study About Headache and Migraine in Native Cultures From Central and South America. J. Headache Pain 2007, 47, 834–841. [Google Scholar] [CrossRef] [PubMed]
- De la Cruz-Jimenez, L.; Guzman-Lucio, M.; Viveros-Valdez, E. Traditional Medicinal Plants Used for the Treatment of Gastrointestinal Diseases in Chiapas, México. World Appl. Sci. J. 2014, 31, 508–515. [Google Scholar] [CrossRef]
- Céspedes, C.L.; Avila, J.G.; Martínez, A.; Serrato, B.; Calderón-Mugica, J.C.; Salgado-Garciglia, R. Antifungal and antibacterial activities of Mexican tarragon (Tagetes lucida). J. Agric. Food Chem. 2006, 54, 3521–3527. [Google Scholar] [CrossRef]
- Singh, P.; Krishna, A.; Kumar, V.; Krishna, S.; Singh, K.; Gupta, M.; Singh, S. Chemistry and biology of industrial crop Tagetes Species: A review. J. Essent. Oil Res. 2015, 28, 1–14. [Google Scholar] [CrossRef]
- Walia, S.; Mukhia, S.; Bhatt, V.; Kumar, R.; Kumar, R. Variability in chemical composition and antimicrobial activity of Tagetes minuta L. essential oil collected from different locations of Himalaya. Ind. Crops Prod. 2020, 150, 112449. [Google Scholar] [CrossRef]
- Burlec, A.F.; Pecio, L.; Kozachok, S.; Mircea, C.; Corciovă, A.; Vereștiuc, L.; Cioancă, O.; Oleszek, W.; Hăncianu, M. Phytochemical Profile, Antioxidant Activity, and Cytotoxicity Assessment of Tagetes erecta Flowers. Molecules 2021, 26, 1201. [Google Scholar] [CrossRef] [PubMed]
- De La Cruz-Jiménez, L.; Hernández-Torres, M.A.; Monroy-García, I.N.; Rivas-Morales, C.; Verde-Star, M.J.; Gonzalez-Villasana, V.; Viveros-Valdez, E. Biological Activities of Seven Medicinal Plants Used in Chiapas, Mexico. Plants 2022, 11, 1790. [Google Scholar] [CrossRef] [PubMed]
- Espinoza, R.M.; Palomeque, R.M.A.; Salazar, S.I.; Domínguez, A.S.; Canseco, A.L.M. Análisis preliminar de la actividad antimicrobiana de la planta medicinal Chik chawa (Tagetes nelsonii Greenm.). Rev. Cuba. Plantas Med. 2009, 14, 4. [Google Scholar]
- Abdoul-Latif, F.M.; Elmi, A.; Merito, A.; Nour, M.; Risler, A.; Ainane, A.; Bignon, J.; Ainane, T. Essential Oils of Tagetes minuta and Lavandula coronopifolia from Djibouti: Chemical Composition, Antibacterial Activity and Cytotoxic Activity against Various Human Cancer Cell Lines. Int. J. Plant Biol. 2022, 13, 315–329. [Google Scholar] [CrossRef]
- Alvarado-Sansininea, J.J.; Sánchez-Sánchez, L.; López-Muñoz, H.; Escobar, M.L.; Flores-Guzmán, F.; Tavera-Hernández, R.; Jiménez-Estrada, M. Quercetagetin and patuletin: Antiproliferative, necrotic and apoptotic activity in tumor cell lines. Molecules 2018, 23, 2579. [Google Scholar] [CrossRef]
- Bermúdez-Bazán, M.; Castillo-Herrera, G.A.; Urias-Silvas, J.E.; Escobedo-Reyes, A.; Estarrón-Espinosa, M. Hunting Bioactive Molecules from the Agave Genus: An Update on Extraction and Biological Potential. Molecules 2021, 26, 6789. [Google Scholar] [CrossRef]
- López-Salazar, H.; Camacho-Díaz, B.H.; Ávila-Reyes, S.V.; Pérez-García, M.D.; González- Cortazar, M.; Arenas Ocampo, M.L.; Jiménez-Aparicio, A.R. Identification and Quantification of β-Sitosterol β-d-Glucoside of an Ethanolic Extract Obtained by Microwave-Assisted Extraction from Agave angustifolia Haw. Molecules 2019, 24, 3926. [Google Scholar] [CrossRef] [PubMed]
- Misra, A.K.; Varma, S.K. Effect of an Extract of Agave americana on Wound Healing Model in Experimental Animals. J. Basic Clin. Physiol. Pharmacol. 2017, 8, 45–48. [Google Scholar]
- Misra, A.K.; Varma, S.K.; Kumar, R. Anti-inflammatory Effect of an Extract of Agave americana on Experimental Animals. Pharmacogn. Res. 2018, 10, 104–108. [Google Scholar] [CrossRef]
- Elferjane, M.R.; Jovanović, A.A.; Milutinović, V.; Čutović, N.; Jovanović Krivokuća, M.; Marinković, A. From Aloe vera Leaf Waste to the Extracts with Biological Potential: Optimization of the Extractions, Physicochemical Characterization, and Biological Activities. Plants 2023, 12, 2744. [Google Scholar] [CrossRef]
- Pandey, B.R.; Shrestha, A.; Sharma, N.; Shrestha, B.G. Evaluation of Phytochemical, Antimicrobial, Antioxidant Activity and Cytotoxic Potentials of Agave americana. Nepal J. Biotechnol. 2019, 7, 30–38. [Google Scholar] [CrossRef]
- Hulle, A.; Kadole, P.; Katkar, P. Agave americana Leaf Fibers. Fibers 2015, 3, 64–75. [Google Scholar] [CrossRef]
- Shegute, T.; Wasihun, Y. Antibacterial Activity and Phytochemical Components of Leaf Extracts of Agave americana. J. Exp. Pharmacol. 2020, 12, 447–454. [Google Scholar] [CrossRef] [PubMed]
- Hamman, J.H. Composition and applications of Aloe vera leaf gel. Molecules 2008, 13, 1599–1616. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Cui, Y.; Pi, F.; Cheng, Y.; Guo, Y.; Qian, H. Extraction, Purification, Structural Characteristics, Biological Activities and Pharmacological Applications of Acemannan, a Polysaccharide from Aloe vera: A Review. Molecules 2019, 24, 1554. [Google Scholar] [CrossRef]
- Reynolds, T.; Dweck, A.C. Aloe vera leaf gel: A review update. J. Ethnopharmacol. 1999, 68, 3–37. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, M.; Misawa, E.; Yamauchi, K.; Abe, F.; Ishizaki, C. Effects of plant sterols derived from Aloe vera gel on human dermal fibroblasts in vitro and on skin condition in Japanese women. Clin. Cosmet. Investig. Dermatol. 2015, 8, 95–104. [Google Scholar] [CrossRef] [PubMed]
- Fox, L.T.; Mazumder, A.; Dwivedi, A.; Gerber, M.; du Plessis, J.; Hamman, J.H. In vitro wound healing and cytotoxic activity of the gel and whole-leaf materials from selected aloe species. J. Ethnopharmacol. 2017, 200, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Bajpai, S. Chapter 8—Biological Importance of Aloe vera and its Active Constituents. In Synthesis of Medical Agents from Plants; Tewari, A., Tiwari, S., Eds.; Elsevier: Amsterdam, The Netherlands, 2018; pp. 177–203. [Google Scholar] [CrossRef]
- Kumar, D.S.; Choudhury, P.K.; Srivastava, R.; Sharma, M. Antimicrobial, anti-inflammatory and wound healing activity of polyherbal formulation. Biomed. Pharmacother. 2019, 111, 555–567. [Google Scholar] [CrossRef]
- Niknam, S.; Tofighi, Z.; Faramarzi, M.A.; Abdollahifar, M.A.; Sajadi, E.; Dinarvand, R.; Toliyat, T. Polyherbal combination for wound healing: Matricaria chamomilla L. and Punica granatum L. DARU J. Pharm. Sci. 2021, 29, 133–145. [Google Scholar] [CrossRef] [PubMed]
- Hattingh, A.; Laux, J.P.; Willers, C.; Hamman, J.; Steyn, D.; Hamman, H. In vitro wound healing effects of combinations of Aloe vera gel with different extracts of Bulbine frutescens. S. Afr. J. Bot. 2023, 158, 254–264. [Google Scholar] [CrossRef]
- Kuete, V.; Nguemeving, J.R.; Beng, V.P.; Blaise, A.A.G.; Etoa, F.X.; Meyer, M.; Bodo, B.; Nkengfack, A.E. Antimicrobial activity of the methanolic extracts and compounds from Vismia laurentii De Wild (Guttiferae). J. Ethnopharmacol. 2007, 109, 372–379. [Google Scholar] [CrossRef]
- Tereschuk, M.R.; Riera, M.V.; Castro, G.R.; Abdala, L.R. Antimicrobial activity of flavonoids from leaves of Tagetes minuta. J. Ethnopharmacol. 1997, 56, 227–232. [Google Scholar] [CrossRef] [PubMed]
- Chin, C.J. Development and formulation of Moringa oleifera standardised leaf extract film dressing for wound healing application. J. Ethnopharmacol. 2018, 212, 188–199. [Google Scholar] [CrossRef]
- Torres-Aguirre, G.A.; Muñoz-Bernal, O.A.; Álvarez-Parrilla, E.; Núñez-Gastélum, J.A.; Wall-Medrano, A.; Sáyago-Ayerdi, S.G.; de la Rosa, L.A. Optimización de la extracción e identificación de compuestos polifenólicos en anís (Pimpinella anisum), clavo (Syzygium aromaticum) y cilantro (Coriandrum sativum) mediante HPLC acoplado a espectrometría de masas. Rev. Espec. Cienc. Quim. Biol. 2018, 21, 103–115. [Google Scholar] [CrossRef]
- Tessema, Z.; Molla, Y. Evaluation of the wound healing activity of the crude extract of root bark of Brucea antidysentrica, the leaves of Dodonaea angustifolia and Rhamnus prinoides in mice. Heliyon 2021, 7, e05901. [Google Scholar] [CrossRef]
- Tadhani, M.; Subhash, R. Preliminary Studies on Stevia rebaudiana Leaves: Proximal Composition, Mineral Analysis and Phytochemical Screening. J. Med. Sci. 2006, 6, 321–326. [Google Scholar] [CrossRef]
- Yadav, R.N.S.; Agarwala, M. Phytochemical Analysis of Some Medicinal Plants. J. Phytol. 2011, 3, 10–14. [Google Scholar]
- Anburaj, G.; Marimuthu, M.; Manikandan, R.; Rajasudha, V. Phytochemical screening and GC-MS analysis of ethanolic extract of Tecoma stans (Family: Bignoniaceae) Yellow Bell Flowers. J. Pharmacogn. Phytochem. 2016, 5, 172–175. [Google Scholar]
- Suganandam, K.; Jeevalatha, A.; Kandeepan, C.; Kavitha, N.; Senthilkumar, N.; Sutha, S.; Seyed, M.A.; Gandhi, S.; Ramya, S.; Lydial, G.; et al. Profile of Phytochemicals and GCMS Analysis of Bioactive Compounds in Natural Dried-Seed Removed Ripened Pods Methanolic Extracts of Moringa oleifera. J. Drug Deliv. Ther. 2022, 12 (Suppl. S5), 133–141. [Google Scholar] [CrossRef]
- Wagner, H.; Bladt, S. Plant Drug Analysis. A Thin Layer Chromatography Atlas, 2nd ed.; Springer Science & Business Media: Berlin/Heidelberg, Germany, 1996. [Google Scholar] [CrossRef]
- Singleton, V.L.; Orthofer, R.; Lamuela-Raventos, R.M. Analysis of total phenols and other oxidation substrates and antioxidants by means of folin-ciocalteu reagent. Meth. Enzymol. 1999, 299, 152–178. [Google Scholar] [CrossRef]
- Ying, C.; Wan, D. Quantitative determination of total and individual flavonoids in stems and leaves of Buddleja davidii and Buddleja albiflora. Pharmacogn. Mag. 2012, 8, 273–279. [Google Scholar] [CrossRef] [PubMed]
- Sim, E.W.; Lai, S.Y.; Chang, Y.P. Antioxidant capacity, nutritional and phytochemical content of peanut (Arachis hypogaea L.) shells and roots. Afr. J. Biotechnol. 2012, 11, 11547–11551. [Google Scholar] [CrossRef]
- Broadhurst, R.B.; Jones, W.T. Analysis of condensed tannins using acidified vanillin. J. Sci. Food Agric. 1978, 29, 788–794. [Google Scholar] [CrossRef]
- Akyar, I. (Ed.) Latest Research into Quality Control; InTech: Rijeka, Croatia, 2012. [Google Scholar] [CrossRef]
- EPA. Method 8270D Semivolatile Organic Compounds by Gas Chromatography/Mass Spectrometry (GC/MS). 2014. Available online: https://archive.epa.gov/epa/sites/production/files/2015-12/documents/8270d.pdf (accessed on 16 March 2022).
- Xin, Z.; Yang, W.; Duan, Y.; Wang, W.; Niu, L.; Sun, D.; Zhang, Y. Bioactive components and antibacterial activities of hydrolate extracts by optimization conditions from Paeonia ostii T. Hong and J. X. Zhang. Ind. Crops Prod. 2022, 188, 115737. [Google Scholar] [CrossRef]
- Vaghasiya, Y.; Chanda, S.V. Screening of methanol and acetone extracts of fourteen indian medicinal plants for antimicrobial activity. Turk. J. Biol. 2007, 31, 243–248. [Google Scholar]
- NCCLS. Performance Standards for Antimicrobial Disk Susceptibility Test, 11th ed.; M02-A11; NCCLS: Wayne, PA, USA, 2012; 76p. [Google Scholar]
- Kim, Y.G.; Lee, J.H.; Park, S.; Kim, S.; Lee, J. Inhibition of polymicrobial biofilm formation by saw palmetto oil, lauric acid and myristic acid. Microb. Biotechnol. 2022, 15, 590–602. [Google Scholar] [CrossRef]
- Clinical and Laboratory Standards Institute (CLSI). Methods for Dilution Microbial Susceptibility Tests for Bacteria That Grow Aerobically; Approved Standard—Ninth Edition, CLSI Document M07-A9; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2006. [Google Scholar]
- Canche-Escamilla, G.; Colli-Acevedo, P.; Borges-Argaez, R.; Quintana-Owen, P.; May-Crespo, J.F.; Cáceres-Farfan, M.; Yam Puc, J.A.; Sansores-Peraza, P.; Vera-Ku, B.M. Extraction of phenolic components from an Aloe vera (Aloe barbadensis Miller) crop and their potential as antimicrobials and textile dyes. Sustain. Chem. Pharm. 2019, 14, 100168. [Google Scholar] [CrossRef]
- Malbrán, G. Método de determinación de sensibilidad antimicrobiana por dilución. In MIC Testing; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2012; Volume 32. [Google Scholar]
- Chanda, S.V.; Menpara, D.; Desai, D.; Rathod, T. Evaluation of Nutraceutical Bottle Gourd (Lagenaria siceraria) as a Potential Source of Natural Antimicrobial Agent. Am. J. Phtyomed. Clin. Ther. 2014, 2, 375–389. [Google Scholar]
- Lopez, T.V.; Lappin, T.R.; Maxwell, P.; Shi, Z.; Lopez-Marure, R.; Aguilar, C.; Rocha-Zavaleta, L. Autocrine/paracrine erythropoietin signalling promotes JAK/STAT-dependent proliferation of human cervical cancer cells. Int. J. Cancer 2011, 129, 2566–2576. [Google Scholar] [CrossRef] [PubMed]
- Fragoso-Ontiveros, V.; Alvarez-García, R.M.; Contreras-Paredes, A.; Vaca-Paniagua, F.; Alonso-Herrera, L.; López-Camarillo, C.; Jacobo-Herrera, N.; Lizano-Soberón, M.; Pérez-Plasencia, C. Gene expression profiles induced by E6 from non-European HPV18 variants reveals a differential activation on cellular processes driving to carcinogenesis. Virology 2012, 432, 81–90. [Google Scholar] [CrossRef]
- Basu, P.N.; Narendrakumar, U.; Arunachalam, R.; Devi, S.; Manjubala, I. Characterization and evaluation of carboxymethyl cellulose-based films for healing of full-thickness wounds in normal and diabetic rats. ACS Omega 2018, 3, 12622–12632. [Google Scholar] [CrossRef]
- Xie, H.C.; Chen, X.; Shen, X.; He, Y.; Chen, W.; Luo, Q.; Ge, W.; Yuan, W.; Tang, X.; Hou, D.; et al. Preparation of chitosan-collagen-alginate composite dressing and its promoting effects on wound healing. Int. J. Biol. Macromol. 2017, 107 Part A, 93–104. [Google Scholar] [CrossRef]
- Kisanga, E.P.; Tang, Z.; Guller, S.; Whirledge, S. In vitro Assays to Evaluate the Migration, Invasion, and Proliferation of Immortalized Human First-trimester Trophoblast Cell Lines. J. Vis. Exp. 2019, 145, 58942. [Google Scholar] [CrossRef]
- Nicolaus, C.J.; Junghanns, S.; Hartmann, A.; Murillo, R.; Ganzera, M.; Merfort, I. In vitro studies to evaluate the wound healing properties of Calendula officinalis extracts. J. Ethnopharmacol. 2017, 196, 94–103. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Pasteur, G.; Silva-Bermúdez, P.S.; Reyes-Chilpa, R.; Vibrans, H.; Soto-Hernández, M. In vitro evaluation of the healing and antimicrobial activity of extracts of Buddleja cordata kunth and Vismia baccifera (L.) triana and planch. Rev. Fitotec. 2019, 42, 93–99. [Google Scholar]
- López-Romero, J.C.; Ayala-Zavala, J.F.; Peña-Ramos, E.A.; Hernández, J.; González-Ríos, H. Antioxidant and antimicrobial activity of Agave angustifolia extract on overall quality and shelf life of pork patties stored under refrigeration. J. Food Sci. Technol. 2018, 55, 4413–4423. [Google Scholar] [CrossRef] [PubMed]
- Soto-Rueda, E.M.; Rodríguez-Ruiz, Y.L.; Loango-Chamorro, N.; Landázuri, P. Extracts of Tagetes patula L. (Asteraceae): A bactericidal potential against Moko. Rev. Mex. Cienc. Agric. 2018, 9, 949–959. [Google Scholar] [CrossRef]
- Ammar, A.T.; Arif, A.M. Phytochemical screening and in vitro antibacterial and anticancer activities of the aqueous extract of Cucumis sativus. Saudi J. Biol. Sci. 2019, 26, 600–604. [Google Scholar] [CrossRef]
- Ahumada-Santos, Y.P.; Montes-Avila, J.; Uribe-Beltrán, M.J.; Díaz-Camacho, S.P.; López-Angulo, G.; Vega-Aviña, R.; López-Valenzuela, J.A.; Heredia, J.B.; Delgado-Vargas, F. Chemical characterization, antioxidant and antibacterial activities of six Agave species from Sinaloa, Mexico. Ind. Crops Prod. 2013, 49, 143–149. [Google Scholar] [CrossRef]
- Singh, P.; Tanwar, N.; Saha, T.; Gupta, A.; Verma, S. Phytochemical Screening and Analysis of Carica papaya, Agave americana and Piper nigrum. Int. J. Curr. Microbiol. Appl. Sci. 2018, 7, 1786–1794. [Google Scholar] [CrossRef]
- Sun, W.; Shahrajabian, M.H. Therapeutic Potential of Phenolic Compounds in Medicinal Plants—Natural Health Products for Human Health. Molecules 2023, 28, 1845. [Google Scholar] [CrossRef] [PubMed]
- Swallah, M.S.; Sun, H.; Affoh, R.; Fu, H.; Yu, H. Antioxidant Potential Overviews of Secondary Metabolites (Polyphenols) in Fruits. Int. J. Food Sci. 2020, 2020, 9081686. [Google Scholar] [CrossRef] [PubMed]
- Taukoorah, U.; Mahomoodally, M.F. Crude Aloe vera gel shows antioxidant propensities and inhibits pancreatic lipase and glucose movement in vitro. Adv. Pharmacol. Sci. 2016, 1, 3720850. [Google Scholar] [CrossRef]
- Tabatabaei, S.R.F.; Ghaderi, S.; Bahrami-Tapehebur, M.; Farbood, Y.; Rashno, M. Aloe vera gel improves behavioral deficits and oxidative status in streptozotocin-induced diabetic rats. Biomed. Pharmacother. 2017, 96, 279–290. [Google Scholar] [CrossRef]
- Nejatzadeh-Barandozi, F. Antibacterial activities and antioxidant capacity of Aloe vera. Org. Med. Chem. Lett. 2013, 3, 5. [Google Scholar] [CrossRef] [PubMed]
- Soto-Castro, D.; Pérez-Herrera, A.; García-Sánchez, E.; Santiago-García, P.A. Identification and Quantification of Bioactive Compounds in Agave potatorum Zucc. Leaves at Different Stages of Development and a Preliminary Biological Assay. Waste Biomass Valorization 2021, 12, 4537–4547. [Google Scholar] [CrossRef]
- Sidana, J.S.; Singh, B.; Sharma, O.P. Saponins of Agave: Chemistry and bioactivity. Phytochemistry 2016, 130, 22–46. [Google Scholar] [CrossRef] [PubMed]
- Devi, T.S.; Vijay, K.; Vidhyavathi, R.M.; Kumar, P.; Govarthanan, M.; Kavitha, T. Antifungal activity and molecular docking of phenol, 2,4-bis(1,1-dimethylethyl) produced by plant growth-promoting actinobacterium Kutzneria sp. strain TSII from mangrove sediments. Arch. Microbiol. 2021, 203, 4051–4064. [Google Scholar] [CrossRef]
- Bayer, G.; Shayganpour, A.; Bayer, I.S. Antioxidant activity of limonene modified cellulose pulp fiber-polylactic acid (PLA) composites. Cellulose 2023, 30, 1599–1622. [Google Scholar] [CrossRef]
- Marchese, A.; Barbieri, R.; Coppo, E.; Orhan, I.E.; Daglia, M.; Nabavi, S.F.; Izadi, M.; Abdollahi, M.; Nabavi, S.M.; Ajami, M. Antimicrobial activity of eugenol and essential oils containing eugenol: A mechanistic viewpoint. Crit. Rev. Microbiol. 2017, 43, 668–689. [Google Scholar] [CrossRef] [PubMed]
- Yarkent, Ç.; Oncel, S.S. Recent Progress in Microalgal Squalene Production and Its Cosmetic Application. Biotechnol. Bioprocess. Eng. 2022, 27, 295–305. [Google Scholar] [CrossRef] [PubMed]
- Islam, M.T.; Ali, E.S.; Uddin, S.J.; Shaw, S.; Islam, M.A.; Ahmed, M.I.; Chandra, S.M.; Karmakar, U.K.; Yarla, N.S.; Khan, I.N.; et al. Phytol: A review of biomedical activities. Food Chem. Toxicol. 2018, 121, 82–94. [Google Scholar] [CrossRef]
- Weimann, E.; Silva, M.B.B.; Murata, G.M.; Bortolon, J.R.; Dermargos, A.; Curi, R.; Hatanaka, E. Topical anti-inflammatory activity of palmitoleic acid improves wound healing. PLoS ONE 2018, 13, e0205338. [Google Scholar] [CrossRef]
- Jin, X.J.; Kim, E.J.; Oh, I.K.; Kim, Y.K.; Park, C.H.; Chung, J.H. Prevention of UV-induced skin damages by 11,14,17-eicosatrienoic acid in hairless mice in vivo. J. Korean Med. Sci. 2010, 25, 930–937. [Google Scholar] [CrossRef]
- Vanitha, V.; Vijayakumar, S.; Nilavukkarasi, M.; Punitha, V.N.; Vidhya, E.; Praseetha, P.K. Heneicosane—A novel microbicidal bioactive alkane identified from Plumbago zeylanica L. Ind. Crops Prod. 2020, 154, 112748. [Google Scholar] [CrossRef]
- Umaru, I.J.; Badruddin, F.A.; Umaru, H.A. Phytochemical Screening of Essential Oils and Antibacterial Activity and Antioxidant Properties of Barringtonia asiatica (L.) Leaf Extract. Biochem. Res. Int. 2019, 2019, 7143989. [Google Scholar] [CrossRef] [PubMed]
- Leyva-Jimenez, F.J.; Sanchez, J.J.; Borras-Linares, I.; Cadiz-Gurrea, M.L.; Mahmoodi-Khaledi, E. Potential antimicrobial activity of honey phenolic compounds against Gram positive and Gram negative bacteria. LWT 2019, 101, 236–245. [Google Scholar] [CrossRef]
- Orczyk, M.; Wojciechowski, K.; Brezesinski, G. The influence of steroidal and triterpenoid saponins on monolayer models of the outer leaflets of human erythrocytes, E. coli and S. cerevisiae cell membranes. J. Colloid. Interface Sci. 2020, 563, 207–217. [Google Scholar] [CrossRef] [PubMed]
- Villa-Silva, P.Y.; Iliná, A.; Ascacio-Valdés, J.A.; Esparza-González, S.C.; Cobos-Puc, L.E.; Rodríguez-Herrera, R.; Silva-Belmares, S.Y. Phenolic compounds of Tagetes lucida Cav. with antibacterial effect due to membrane damage. Bol. Latinoam. Caribe Plantas Med. Aromat. 2020, 19, 580–590. [Google Scholar] [CrossRef]
- Lepe, J.A.; Martínez-Martínez, L. Mecanismos de resistencia en bacterias gramnegativas. Med. Intensiv. 2022, 46, 392–402. [Google Scholar] [CrossRef]
- Adzitey, F.; Agbolosu, A.A.; Udoka, U.J. Antibacterial effect of Aloe vera gel extract on Escherichia coli and Salmonella enterica isolated from the gastrointestinal tract of Guinea Fowls. World’s Vet. J. 2019, 9, 166–173. [Google Scholar] [CrossRef]
- Breijyeh, Z.; Jubeh, B.; Karaman, R. Resistance of Gram-Negative Bacteria to Current Antibacterial Agents and Approaches to Resolve It. Molecules 2020, 25, 1340. [Google Scholar] [CrossRef] [PubMed]
- Arbab, S.; Buriro, R.; Bhugio, S.U.; Shah, A.H.; Soomro, J.; Kalwar, Q.; Fazilani, S.A.; Vistro, W.A. Antimicrobial Properties of Aloe vera Gel Extracts against Bacterial Isolates from Wound of Donkey. Pak. J. Zool. 2020, 52, 2333–2339. [Google Scholar] [CrossRef]
- Solanke, S.B.; Bhujbal, S.S.; Tawar, M.G. Development and Evaluation of Surgical Sutures from Agave americana Linn. Var. Americana. Am. J. PharmTech Res. 2018, 8, 114–125. [Google Scholar] [CrossRef]
- Chatterjee, S.P. Comparative efficacy of Tagetes erecta and Centella asiatica extracts on wound healing in albino rats. Chin. Med. 2011, 2, 138–142. [Google Scholar] [CrossRef]
- Singh, N.; Mrinal; Thakur, R. Review on Pharmacological aspects of Tagetes erecta Linn. PharmaTutor 2019, 7, 16–24. [Google Scholar]
- Selvam, S.I.; Joicesky, S.M.B.; Dashli, A.A.; Vinothini, A.; Premkumar, K. Assessment of anti-bacterial, anti-inflammation and wound healing activity in Wistar albino rats using green silver nanoparticles synthesized from Tagetes erecta leaves. J. Appl. Nat. Sci. 2021, 13, 343–351. [Google Scholar] [CrossRef]
- Sultana, A.; Hasan, M.; Rahman, M.; Alam, M.M. Healing potentials of Marigold flower (Tagetes erecta) on full thickness dermal wound in caprine model. Eur. Respir. J. 2021, 7, 332–339. [Google Scholar] [CrossRef]
- Manisha, U.K.; Ghosh, T.; Apoorva, V.P.; Divya, B.; Swathy, S.P.; Paul, A.; Basavraj, B.V. Isolation, phytochemical elucidation, and wound healing potential of chitosan-based film loaded with Tagetes erecta. In Materials Today: Proceedings; Elsevier: Amsterdam, The Netherlands, 2022. [Google Scholar] [CrossRef]
- Tan, B.L.; Norhaizan, M.E.; Liew, W.P.P.; Sulaiman, R.H. Antioxidant and Oxidative Stress: A Mutual Interplay in Age-Related Diseases. Front. Pharmacol. 2018, 9, 1162. [Google Scholar] [CrossRef] [PubMed]
- Olszowy, M. What is responsible for antioxidant properties of polyphenolic compounds from plants? Plant Physiol. Biochem. 2019, 144, 135–143. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.H.; Yoon, K.D.; Chin, Y.W.; Park, J.H.; Kim, J. Phenolic compounds with radical scavenging and cyclooxygenase-2 (COX-2) inhibitory activities from Dioscorea opposita. Bioorg. Med. Chem. 2009, 17, 2689–2694. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, D.; Freitas, M.; Tomé, S.M.; Silva, A.M.; Laufer, S.; Lima, J.L.; Fernandes, E. Flavonoids inhibit COX-1 and COX-2 enzymes and cytokine/chemokine production in human whole blood. Inflammation 2015, 38, 858–870. [Google Scholar] [CrossRef]
- Chummun, I.; Bekah, D.; Goonoo, N.; Bhaw-Luximon, A. Assessing the mechanisms of action of natural molecules/extracts for phase-directed wound healing in hydrogel scaffolds. RSC Med. Chem. 2021, 12, 1476–1490. [Google Scholar] [CrossRef]
- Davis, R.H.; Donato, J.J.; Hartman, G.M.; Haas, R.C. Anti-inflammatory and wound healing activity of a growth substance in Aloe vera. J. Am. Podiatr. Med. Assoc. 1994, 84, 77–81. [Google Scholar] [CrossRef] [PubMed]
- Radha, M.H.; Laxmipriya, N.P. Evaluation of biological properties and clinical effectiveness of Aloe vera: A systematic review. J. Tradit. Complement. Med. 2014, 5, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Sierra-García, G.D.; Castro-Ríos, R.; González-Horta, A.; Lara-Arias, J.; Chávez-Montes, A. Acemannan, an Extracted Polysaccharide from Aloe vera: A Literature Review. Nat. Prod. Commun. 2014, 9, 1217–1221. [Google Scholar] [PubMed]
- Silva, S.S.; Fernandes, E.M.; Pina, S.; Silva-Correia, J.; Vieira, S.; Oliveira, J.M.; Reis, R.L. Polymers of Biological Origin. Compr. Biomater. II 2017, 2, 228–252. [Google Scholar] [CrossRef]
- Fouché, M.; Willers, C.; Hamman, S.; Malherbe, C.; Steenekamp, J. Wound Healing Effects of Aloe muth-muth: In vitro Investigations Using Immortalized Human Keratinocytes (HaCaT). Biology 2020, 9, 350. [Google Scholar] [CrossRef]
- Mukherjee, P.K.; Nema, N.K.; Maity, N.; Mukherjee, K.; Harwansh, R.K. Phytochemical and therapeutic profile of Aloe vera. J. Nat. Remedies 2014, 14, 1–26. [Google Scholar] [CrossRef]


| Secondary Metabolites | T. nelsonii | A. americana | A. vera |
|---|---|---|---|
| Sterols | +++ | + | + |
| Terpenes | +++ | + | + |
| Anthraquinones | + | + | + |
| Carbohydrates | − | + | +++ |
| Saponins | + | ++ | ++ |
| Flavonoids | +++ | + | + |
| Tanins | + | ++ | + |
| Coumarins | + | + | + |
| Secondary Metabolites | T. nelsonii | A. americana | A. vera |
|---|---|---|---|
| Total phenols | 2.220 ± 0.014 | 0.102 ± 0.005 | 0.138 ± 0.007 |
| Flavonoids | 1.313 ± 0.006 | 0.026 ± 0.002 | 0.019 ± 0.001 |
| Saponins | 0.406 ± 0.018 | 1.009 ± 0.002 | 0.188 ± 0.014 |
| Tannins | 0.871 ± 0.011 | 0.518 ± 0.003 | 0.014 ± 0.002 |
| Coumarins | 0.103 ± 0.007 | 0.030 ± 0.001 | 0.020 ± 0.001 |
| Concentration | 100 mg mL−1 | 400 mg mL−1 | 800 mg mL−1 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Inhibition Zone (mm) | |||||||||
| Microorganism | P.a | E.c | S.a | P.a | E.c | S.a | P.a | E.c | S.a |
| T. nelsonii | 17.00 Aa | 10.67 Aa | 17.33 Aa | 18.33 Aa | 13.67 Aa | 18.66 Aa | 18.00 Aa | 10.67 Aa | 19.93 Aa |
| A. vera | WA | WA | WA | WA | WA | WA | WA | WA | WA |
| A. americana | 6.83 B | 6.33 B | WA | 6.83 B | 6.33 B | WA | 6.83 B | 6.33 B | WA |
| Microorganism | T. nelsonii | Ciprofloxacin | ||
|---|---|---|---|---|
| MIC mg mL−1 | MBC mg mL−1 | MIC mg mL−1 | MBC mg mL−1 | |
| Escherichia coli | 25 | 50 | 0.00016 | 0.00032 |
| Pseudomonas aeruginosa | 25 | 50 | 0.00032 | 0.00064 |
| Staphylococcus aureus | 25 | 50 | 0.00012 | 0.00025 |
| Extract | R.T. (min) | Name | Class |
|---|---|---|---|
| T. nelsonii | 5.839 | Limonene | Terpenoids |
| 10.859 | Eugenol | Terpenoids | |
| 12.542 | Phenol, 2,4-bis-(1,1-dimethylethyl) | Phenols | |
| 15.578 | Myristic acid | Fatty acid | |
| 17.281 | Palmitic acid | Fatty acid | |
| 17.709 | 7-Hydroxy-2H-1-benzopyran-2-one | Coumarin | |
| 19.124 | Phytol | Terpenoids | |
| 19.620 | 11,14,17-Eicosatrienoic acid | Fatty acid | |
| 22.523 | Docosane | Alkane | |
| 24.923 | Squalene | Terpenoids | |
| A americana | 12.540 | Phenol, 2,4-bis-(1,1-dimethylethyl) | Phenols |
| 17.286 | Palmitic acid | Fatty acid | |
| 18.868 | Heneicosane | Alkane | |
| 19.002 | 8,11-Linoleic acid | Fatty acid | |
| 19.043 | Caprilic acid | Fatty acid | |
| 19.081 | Linolenic acid | Fatty acid | |
| 19.124 | Phytol | Terpenoids | |
| 22.426 | Eicosane | Alkane |
| Extract | 3T3 | HaCaT |
|---|---|---|
| LC50 µg mL−1 | LC50 µg mL−1 | |
| T. nelsonii | 346.19 ± 2.47 | 148.40 ± 1.60 |
| A. americana | 40.22 ± 2.43 | 31.19 ± 1.99 |
| A. vera | 64.71 ± 2.99 | 53.38 ± 4.17 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Olán-Jiménez, K.A.; Cruz-Rodríguez, R.I.; Couder-García, B.d.C.; Jacobo-Herrera, N.; Ruiz-Lau, N.; Hernández-Cruz, M.d.C.; Ruíz-Valdiviezo, V.M. Antibacterial and Wound Healing Activity In Vitro of Individual and Combined Extracts of Tagetes nelsonii Greenm, Agave americana and Aloe vera. Sci. Pharm. 2024, 92, 41. https://doi.org/10.3390/scipharm92030041
Olán-Jiménez KA, Cruz-Rodríguez RI, Couder-García BdC, Jacobo-Herrera N, Ruiz-Lau N, Hernández-Cruz MdC, Ruíz-Valdiviezo VM. Antibacterial and Wound Healing Activity In Vitro of Individual and Combined Extracts of Tagetes nelsonii Greenm, Agave americana and Aloe vera. Scientia Pharmaceutica. 2024; 92(3):41. https://doi.org/10.3390/scipharm92030041
Chicago/Turabian StyleOlán-Jiménez, Karen Alejandra, Rosa Isela Cruz-Rodríguez, Beatriz del Carmen Couder-García, Nadia Jacobo-Herrera, Nancy Ruiz-Lau, Maritza del Carmen Hernández-Cruz, and Víctor Manuel Ruíz-Valdiviezo. 2024. "Antibacterial and Wound Healing Activity In Vitro of Individual and Combined Extracts of Tagetes nelsonii Greenm, Agave americana and Aloe vera" Scientia Pharmaceutica 92, no. 3: 41. https://doi.org/10.3390/scipharm92030041
APA StyleOlán-Jiménez, K. A., Cruz-Rodríguez, R. I., Couder-García, B. d. C., Jacobo-Herrera, N., Ruiz-Lau, N., Hernández-Cruz, M. d. C., & Ruíz-Valdiviezo, V. M. (2024). Antibacterial and Wound Healing Activity In Vitro of Individual and Combined Extracts of Tagetes nelsonii Greenm, Agave americana and Aloe vera. Scientia Pharmaceutica, 92(3), 41. https://doi.org/10.3390/scipharm92030041







