Mapping the Accessibility of Medical Facilities of Wuhan during the COVID-19 Pandemic
Abstract
1. Introduction
2. Methodology
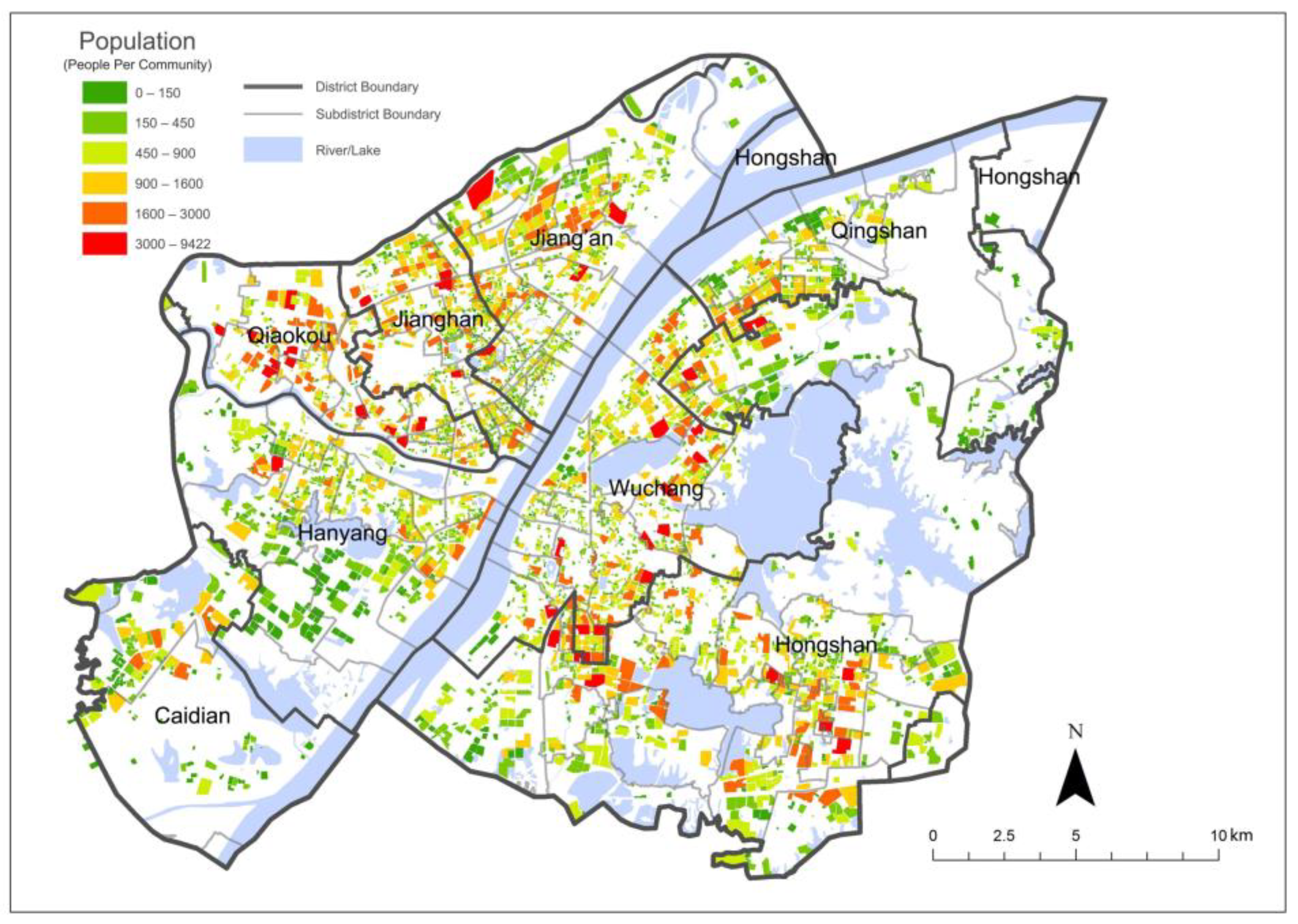
2.1. Study Area and Objects
2.2. Method and Indices
- Combine the official information and online map data, mapping the geographical locations and beds information of the medical facilities relevant to COVID-19;
- Compile boundaries of all the communities (4076) in the study area of Wuhan;
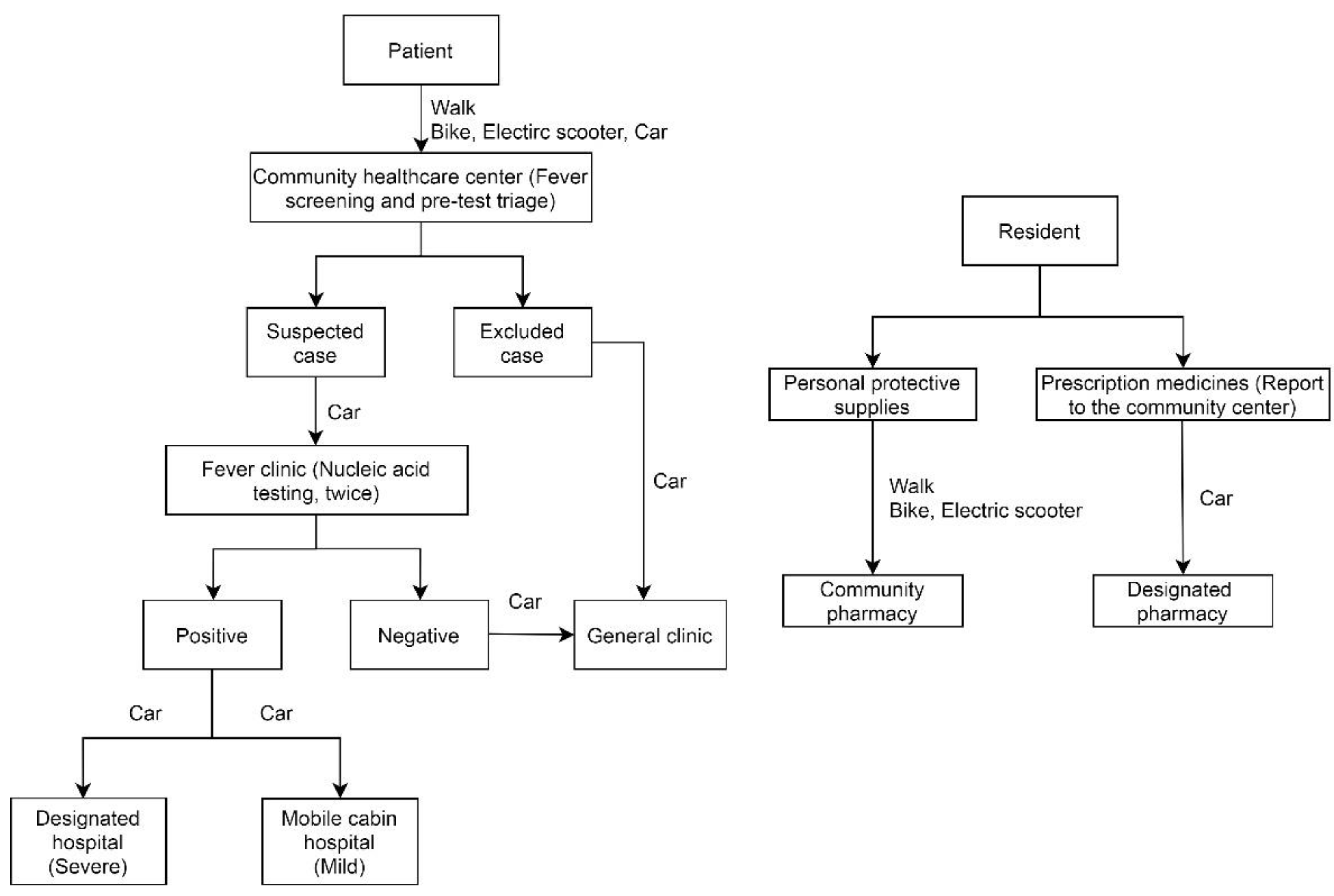
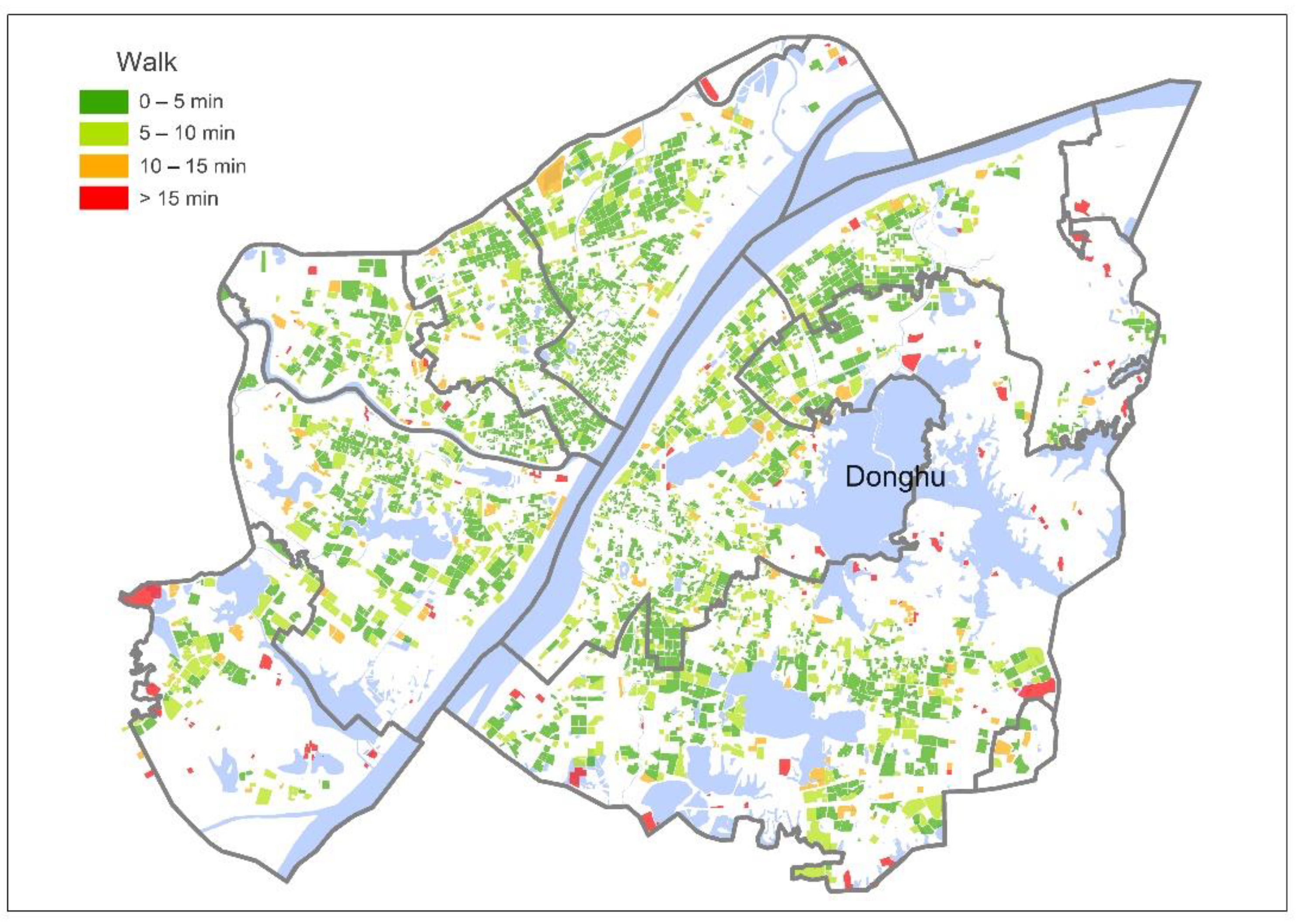
- Scrape travel distance and time of various travel modes from communities to community healthcare centers, from community healthcare centers to fever clinics, from fever clinics to design hospitals and mobile cabin hospitals, from communities to community pharmacies and designated pharmacies (Figure 3); then, select the shortest-time travel as the presumed one. From communities to community healthcare centers and community pharmacies, the selections are based on walking mode, while for the others, the selections are based on driving mode (with the Baidu Map API from February to March, 2020) [41];
- Following the treatment procedure shown in Figure 3, identify the amount of communities and service areas each pandemic-related medical facility can serve; then, overlay the medical facilities’ service areas on the community population layer to estimate the potential capacities of those medical facilities. Table 1 shows the relevant indices, which are PPR-related. Due to ‘the lockdown and no cross-district medical treatment policy’, these indices can ignore their disadvantages of neglecting the cross-border healthcare-seeking behavior and take advantage of their merits of easy understanding and simple calculation [21,27,28].
3. Results
3.1. Service Areas and Potential Capacities of the COVID-19 Medical Facilities
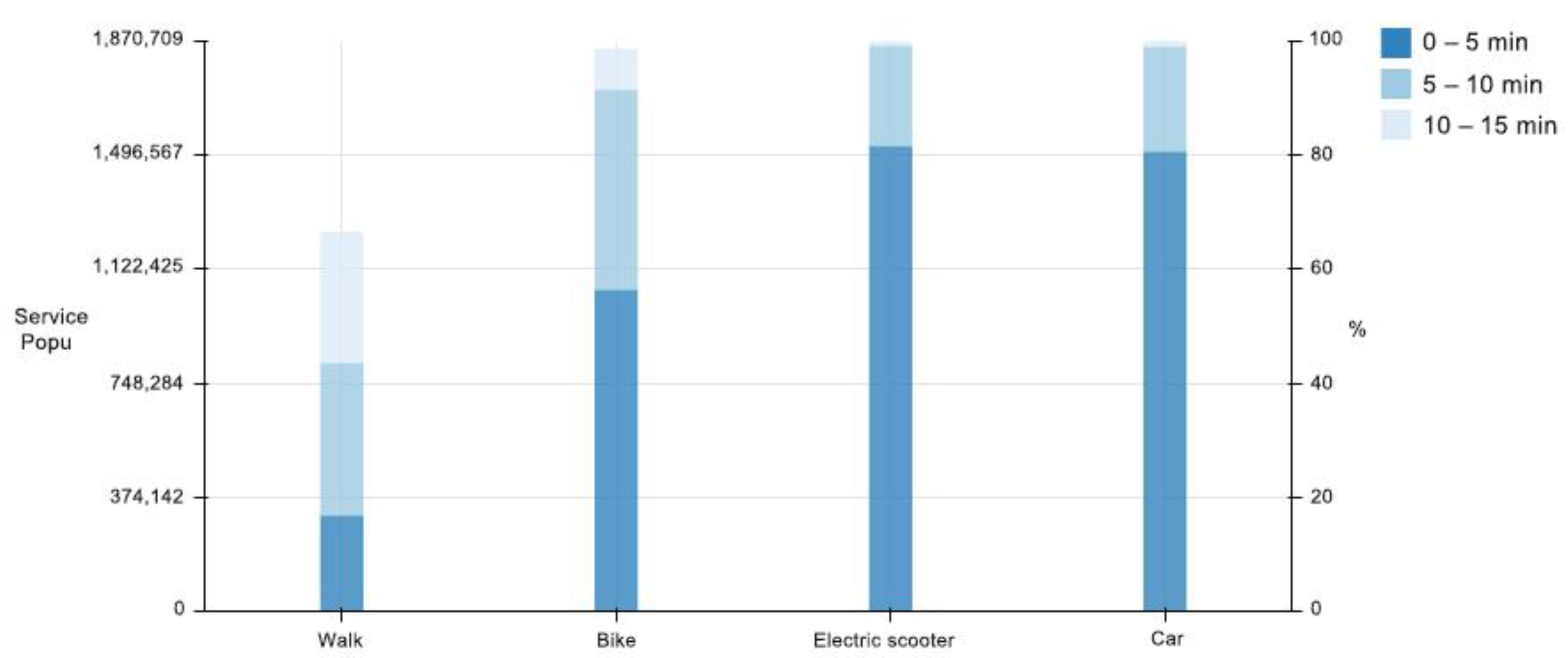
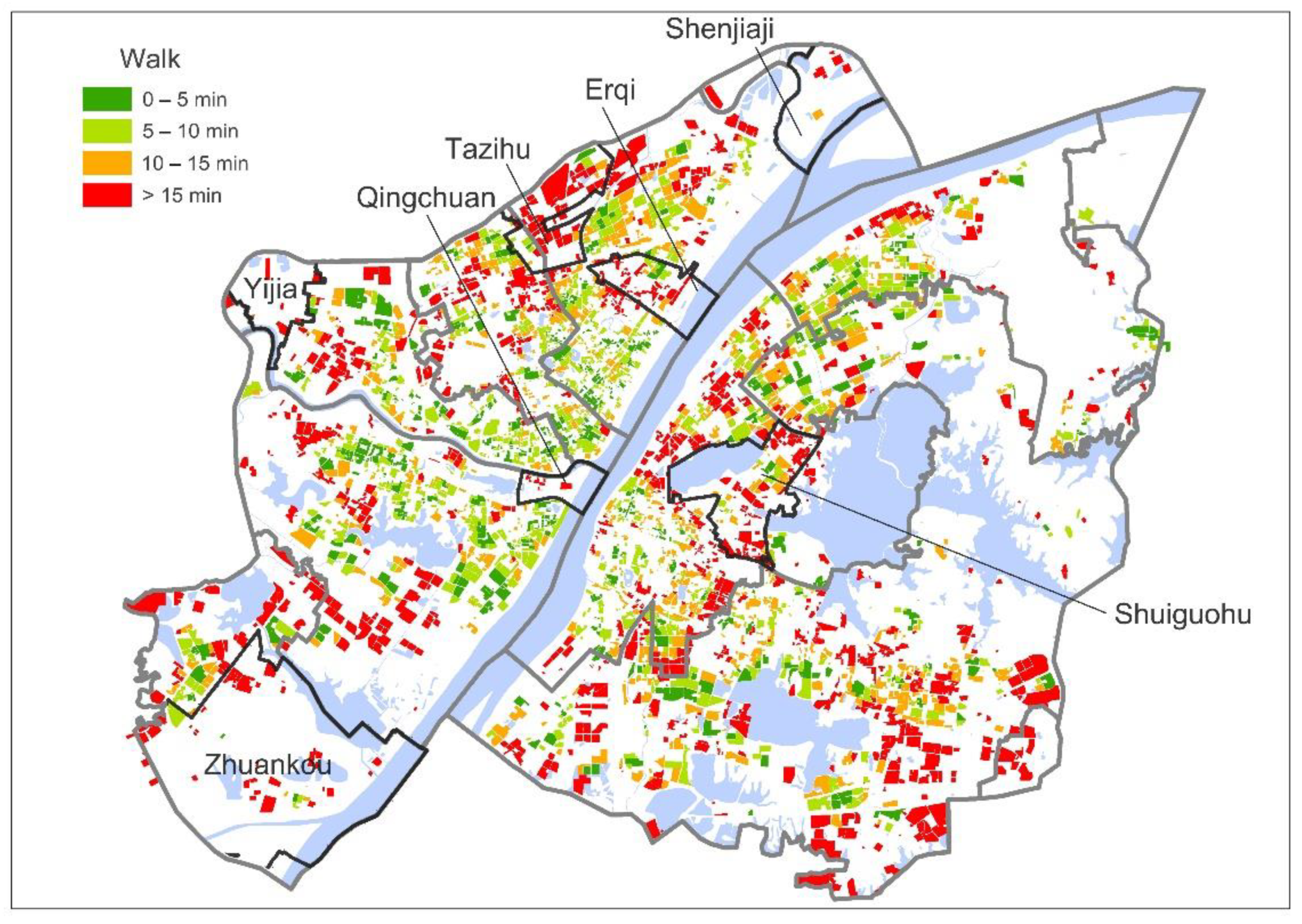
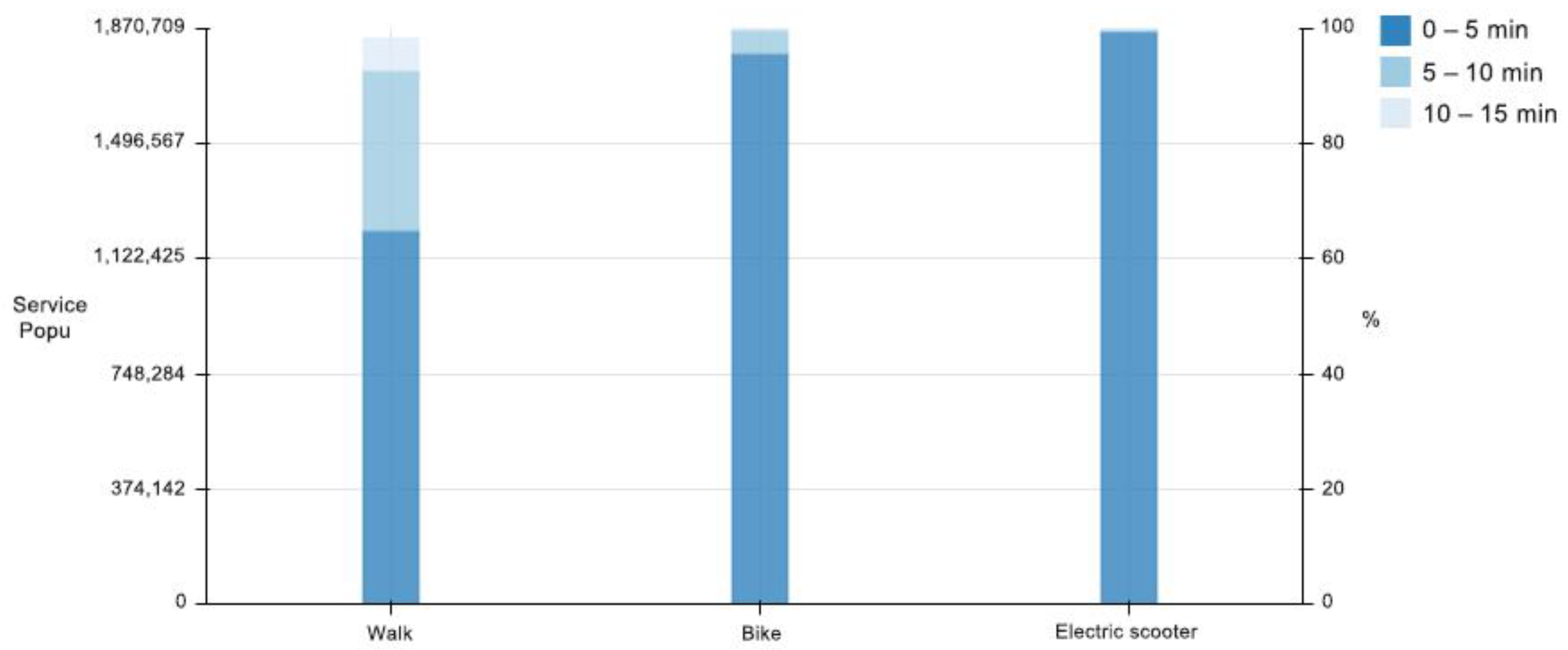
3.1.1. Service Areas and Population of the Community Healthcare Centers
3.1.2. Service Areas and Population of the Fever Clinics
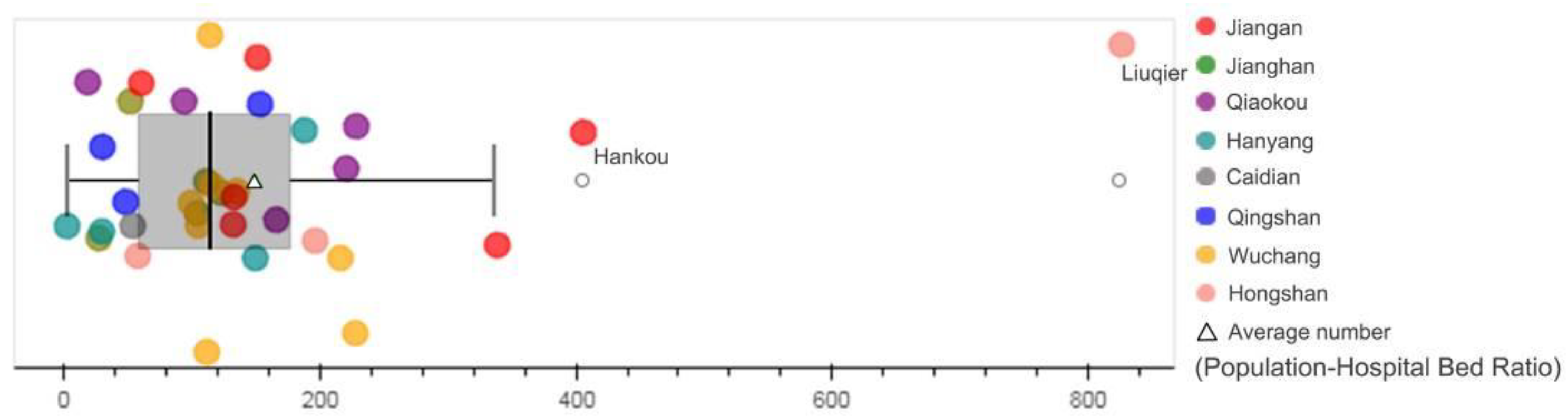
3.1.3. Service Areas and Population–Hospital Bed Ratios of the Designated Hospitals
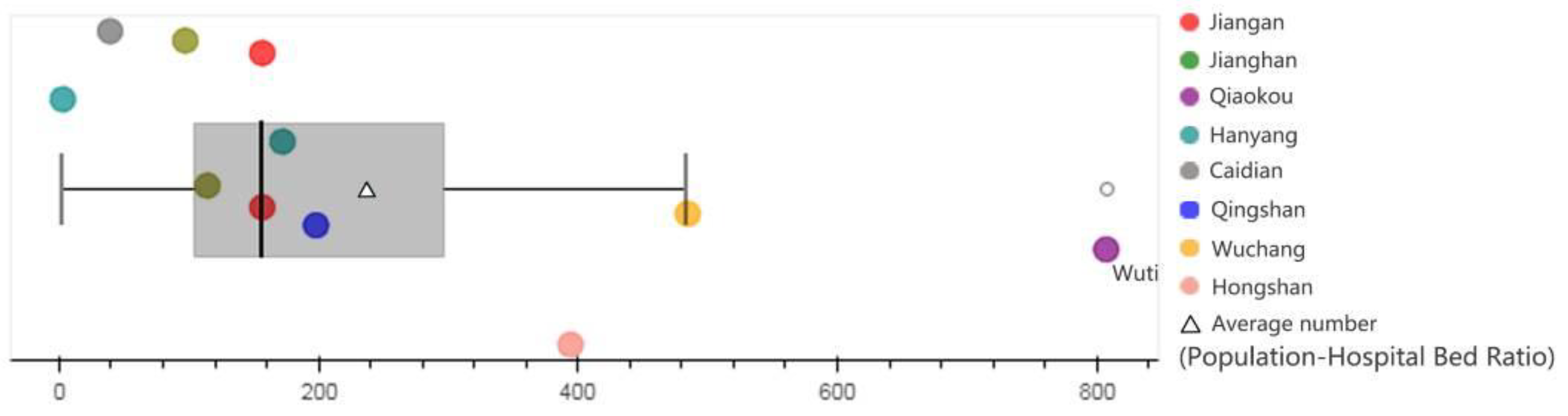
3.1.4. Service Areas and Population–Hospital Bed Ratios of the Mobile Cabin Hospitals
3.2. Service Areas and Potential Capacities of the Pharmacies Related to Residents
3.2.1. Service Areas and Population of the Community Pharmacies
3.2.2. Service Areas and Population of the Designated Pharmacies
4. Discussion
5. Conclusions
6. Patents
- Computer Software Copyright: Walking simulation trip generator software (5161030), Copyright Protection Center of China.
- Computer Software Copyright: Peripheral walking routes extractor software (4353770), Copyright Protection Center of China.
- Computer Software Copyright: Cycling simulation trip generator software (5161237), Copyright Protection Center of China.
- Computer Software Copyright: Car simulation trip generator software (5054443), Copyright Protection Center of China.
- Computer Software Copyright: POI extractor software (5054449), Copyright Protection Center of China.
- Computer Software Copyright: AOI extractor software (5220045), Copyright Protection Center of China.
- Computer Software Copyright: Coordinate converter software (5607408), Copyright Protection Center of China.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Weekly, C.C.; The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team. Vital surveillances: The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19)—China, 2020. China CDC Wkly. 2020, 2, 113–122. [Google Scholar] [CrossRef]
- Wuhan Government. Notification of Wuhan COVID-19 Prevention and Control Headquarters (No.1). 2020. Available online: http://www.wuhan.gov.cn/zwgk/tzgg/202003/t20200316_972434.shtml (accessed on 23 January 2020).
- Lai, S.; Ruktanonchai, N.W.; Zhou, L.; Prosper, O.; Luo, W.; Floyd, J.R.; Wesolowski, A.; Santillana, M.; Zhang, C.; Du, X.; et al. Effect of non-pharmaceutical interventions to contain COVID-19 in China. Nature 2020, 585, 410–413. [Google Scholar] [CrossRef] [PubMed]
- Wuhan Government. Notification of Wuhan COVID-19 Prevention and Control Headquarters (No.12). 2020. Available online: http://www.wuhan.gov.cn/zwgk/tzgg/202003/t20200316_972539.shtml (accessed on 11 February 2020).
- Wuhan Government. Notification of Wuhan COVID-19 Prevention and Control Headquarters (No.9). 2020. Available online: http://www.wuhan.gov.cn/zwgk/tzgg/202003/t20200316_972460.shtml (accessed on 25 January 2020).
- Wuhan Government. Notification of Wuhan COVID-19 Prevention and Control Headquarters (No.7). 2020. Available online: http://www.wuhan.gov.cn/zwgk/tzgg/202003/t20200316_972456.shtml (accessed on 24 January 2020).
- Chen, S.; Zhang, Z.; Yang, J.; Wang, J.; Zhai, X.; Bärnighausen, T.; Wang, C. Fangcang shelter hospitals: A novel concept for responding to public health emergencies. Lancet 2020, 395, 1305–1314. [Google Scholar] [CrossRef]
- Wuhan Government. Notification of Wuhan COVID-19 Prevention and Control Headquarters (No.11). 2020. Available online: http://www.wuhan.gov.cn/zwgk/tzgg/202003/t20200316_972538.shtml (accessed on 11 February 2020).
- Donabedian, A. Aspects of Medical Care Administration: Specifying Requirements for Health Care, 1st ed.; Harvard University Press: Cambridge, MA, USA, 1973. [Google Scholar]
- Penchansky, R.; Thomas, J.W. The concept of access: Definition and relationship to consumer satisfaction. Med. Care 1981, 19, 127–140. [Google Scholar] [CrossRef]
- Wang, F. Measurement, optimization, and impact of health care accessibility: A methodological review. Ann. Assoc. Am. Geogr. 2012, 102, 1104–1112. [Google Scholar] [CrossRef]
- Gu, W.; Wang, X.; McGregor, S.E. Optimization of preventive health care facility locations. Int. J. Health Geogr. 2010, 9, 17. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Berman, O.; Verter, V. The impact of client choice on preventive healthcare facility network design. OR Spectrum 2012, 34, 349–370. [Google Scholar] [CrossRef]
- Gage, A.J.; Calixte, M.G. Effects of the physical accessibility of maternal health services on their use in rural Haiti. Pop. Stud. J. Demog. 2006, 60, 271–288. [Google Scholar] [CrossRef] [PubMed]
- Kyei, N.N.A.; Campbell, O.M.R.; Gabrysch, S. The influence of distance and level of service provision on antenatal care use in rural Zambia. PLoS ONE 2012, 7, e46475. [Google Scholar] [CrossRef]
- Grimes, C.E.; Bowman, K.G.; Dodgion, C.M.; Lavy, C.B.D. Systematic review of barriers to surgical care in low-income and middle-income countries. World J. Surg. 2011, 35, 941–950. [Google Scholar] [CrossRef] [PubMed]
- Tansley, G.; Stewart, B.; Zakariah, A.; Boateng, E.; Achena, C.; Lewis, D.; Mock, C. Population-level spatial access to prehospital care by the national ambulance service in Ghana. Prehosp. Emerg. Care 2016, 20, 768–775. [Google Scholar] [CrossRef]
- Avdic, D. Improving efficiency or impairing access? Health care consolidation and quality of care: Evidence from emergency hospital closures in Sweden. J. Health Econ. 2016, 48, 44–60. [Google Scholar] [CrossRef]
- Aday, L.A.; Andersen, R. A framework for the study of access to medical care. Health Serv. Res. 1974, 9, 208–220. [Google Scholar] [PubMed]
- Jones, S.G.; Ashby, A.J.; Momin, S.R.; Naidoo, A. Spatial implications associated with using Euclidean distance measurements and geographic centroid imputation in health care research. Health Serv. Res. 2010, 45, 316–327. [Google Scholar] [CrossRef] [PubMed]
- Neutens, T. Accessibility, equity and health care: Review and research directions for transport geographers. J. Transp. Geogr. 2015, 43, 14–27. [Google Scholar] [CrossRef]
- Reshadat, S.; Zangeneh, A.; Saeidi, S.; Teimouri, R.; Yigitcanlar, T. Measures of spatial accessibility to health centers: Investigating urban and rural disparities in Kermanshah, Iran. J. Public. Health 2019, 27, 519–529. [Google Scholar] [CrossRef]
- Wang, F.; Xu, Y. Estimating O-D travel time matrix by Google Maps API: Implementation, advantages, and implications. Ann. GIS 2011, 17, 199–209. [Google Scholar] [CrossRef]
- Jia, T.; Tao, H.; Qin, K.; Wang, Y.; Liu, C.; Gao, Q. Selecting the optimal healthcare centers with a modified P-median model: A visual analytic perspective. Int. J. Health Geogr. 2014, 13, 42. [Google Scholar] [CrossRef]
- Ni, J.; Wang, J.; Rui, Y.; Qian, T.; Wang, J. An enhanced variable two-step floating catchment area method for measuring spatial accessibility to residential care facilities in Nanjing. Int. J. Environ. Res. Public Health 2015, 12, 14490–14504. [Google Scholar] [CrossRef]
- Tao, Z.; Cheng, Y. Modelling the spatial accessibility of the elderly to healthcare services in Beijing, China. Environ. Plan B Urban. 2019, 46, 1132. [Google Scholar] [CrossRef]
- McGrail, M.R.; Humphreys, J.S. Measuring spatial accessibility to primary care in rural areas: Improving the effectiveness of the two-step floating catchment area method. Appl. Geogr. 2009, 29, 533–541. [Google Scholar] [CrossRef]
- Donohoe, J.; Marshall, V.; Tan, X.; Camacho, F.T.; Anderson, R.; Balkrishnan, R. Evaluating and comparing methods for measuring spatial access to mammography centers in Appalachia. Health Serv. Outcomes Res. Method. 2016, 16, 22–40. [Google Scholar] [CrossRef]
- Joseph, A.E.; Phillips, D.R. Accessibility and utilization: Geographical perspectives on health care delivery. Geography 1984, 69, 375. [Google Scholar]
- Yang, D.H.; Goerge, R.; Mullner, R. Comparing GIS-based methods of measuring spatial accessibility to health services. J. Med. Syst. 2006, 30, 23–32. [Google Scholar] [CrossRef] [PubMed]
- Wang, F. Quantitative Methods and Socio-Economic Applications in GIS, 2nd ed.; CRC Press: Boca Raton, FL, USA, 2014. [Google Scholar]
- Yun, S.B.; Kim, S.; Ju, S.; Noh, J.; Kim, C.; Wong, M.S.; Heo, J. Analysis of accessibility to emergency rooms by dynamic population from mobile phone data: Geography of social inequity in South Korea. PLoS ONE 2020, 15, e0231079. [Google Scholar] [CrossRef] [PubMed]
- Tao, R.; Downs, J.; Beckie, T.M.; Chen, Y.; McNelley, W. Examining spatial accessibility to COVID-19 testing sites in Florida. Ann. GIS 2020, 26, 319–327. [Google Scholar] [CrossRef]
- Kang, J.Y.; Michels, A.; Lyu, F.; Wang, S.; Agbodo, N.; Freeman, V.L.; Wang, S. Rapidly measuring spatial accessibility of COVID-19 healthcare resources: A case study of Illinois, USA. Int. J. Health Geogr. 2020, 19, 36. [Google Scholar] [CrossRef] [PubMed]
- Ghorbanzadeh, M.; Kim, K.; Ozguven, E.E.; Horner, M.W. Spatial accessibility assessment of COVID-19 patients to healthcare facilities: A case study of Florida. Travel Behav. Soc. 2021, 24, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Chokshi, D.A.; Katz, M.H. Emerging lessons from COVID-19 response in New York City. J. Am. Med. Assoc. 2020, 323, 1996–1997. [Google Scholar] [CrossRef]
- Shadmi, E.; Chen, Y.; Dourado, I.; Faran-Perach, I.; Furler, J.; Hangoma, P.; Hanvoravongchai, P.; Obando, C.; Petrosyan, V.; Rao, K.D.; et al. Health equity and COVID-19: Global perspectives. Int. J. Equity Health 2020, 19, 104. [Google Scholar] [CrossRef]
- Ji, Y.; Ma, Z.; Peppelenbosch, M.P.; Pan, Q. Potential association between COVID-19 mortality and healthcare resource availability. Lancet Glob. Health 2020, 8, e480. [Google Scholar] [CrossRef]
- Ma, X.; Ren, F.; Du, Q.; Liu, P.; Li, L.; Xi, Y.; Jia, P. Incorporating multiple travel modes into a floating catchment area framework to analyse patterns of accessibility to hierarchical healthcare facilities. J. Transp. Health 2019, 15, 100675. [Google Scholar] [CrossRef]
- Ye, T.; Zhao, N.; Yang, X.; Ouyang, Z.; Liu, X.; Chen, Q.; Hu, K.; Yue, W.; Qi, J.; Li, Z.; et al. Improved population mapping for China using remotely sensed and points-of-interest data within a random forests model. Sci. Total Environ. 2018, 658, 936–946. [Google Scholar] [CrossRef] [PubMed]
- Baidu Map Application Programming Interface. Baidu Map. 2020. Available online: http://lbsyun.baidu.com/index.php?title=%E9%A6%96%E9%A1%B5 (accessed on 25 November 2020).
- Utilization of Hospital Beds in Designated Hospitals in Wuhan. Wuhan Health Commission; 2020. Available online: http://wjw.wh.gov.cn/front/web/showDetail/2020022609813 (accessed on 25 February 2020).
- Mobile Cabin Hospital: Should Be Treated as Best as Possible. Wuhan Health Commission; 2020. Available online: http://wjw.wh.gov.cn/front/web/showDetail/2020022409772 (accessed on 6 February 2020).
- Zhang, J. To jointly create and restart the community self-organization function-Pen talks on coping with the COVID-19. City Plan. Rev. 2020, 44, 10. [Google Scholar]
- The Chinese State Council. 2016; Opinions of the CPC Central Committee and the State Council on Further Strengthening the Administration of Urban Planning and Construction. Available online: http://www.gov.cn/zhengce/2016-02/21/content_5044367.htm (accessed on 21 February 2016).
- Wu, T.; Hu, E.; Zeng, W.; Zhang, H.; Xue, X.; Ma, J. Unprecedented action has been taken to contain the epidemic of coronavirus disease 2019 in China. J. Cent. S. Univ. 2020, 45, 334–337. [Google Scholar] [CrossRef]
- The Chinese State Council. 2015; Guidelines of the General Office of the State Council on Promoting the Construction of the Hierarchical Diagnosis and Treatment System. Available online: http://www.gov.cn/zhengce/content/2015-09/11/content_10158.htm (accessed on 11 September 2015).
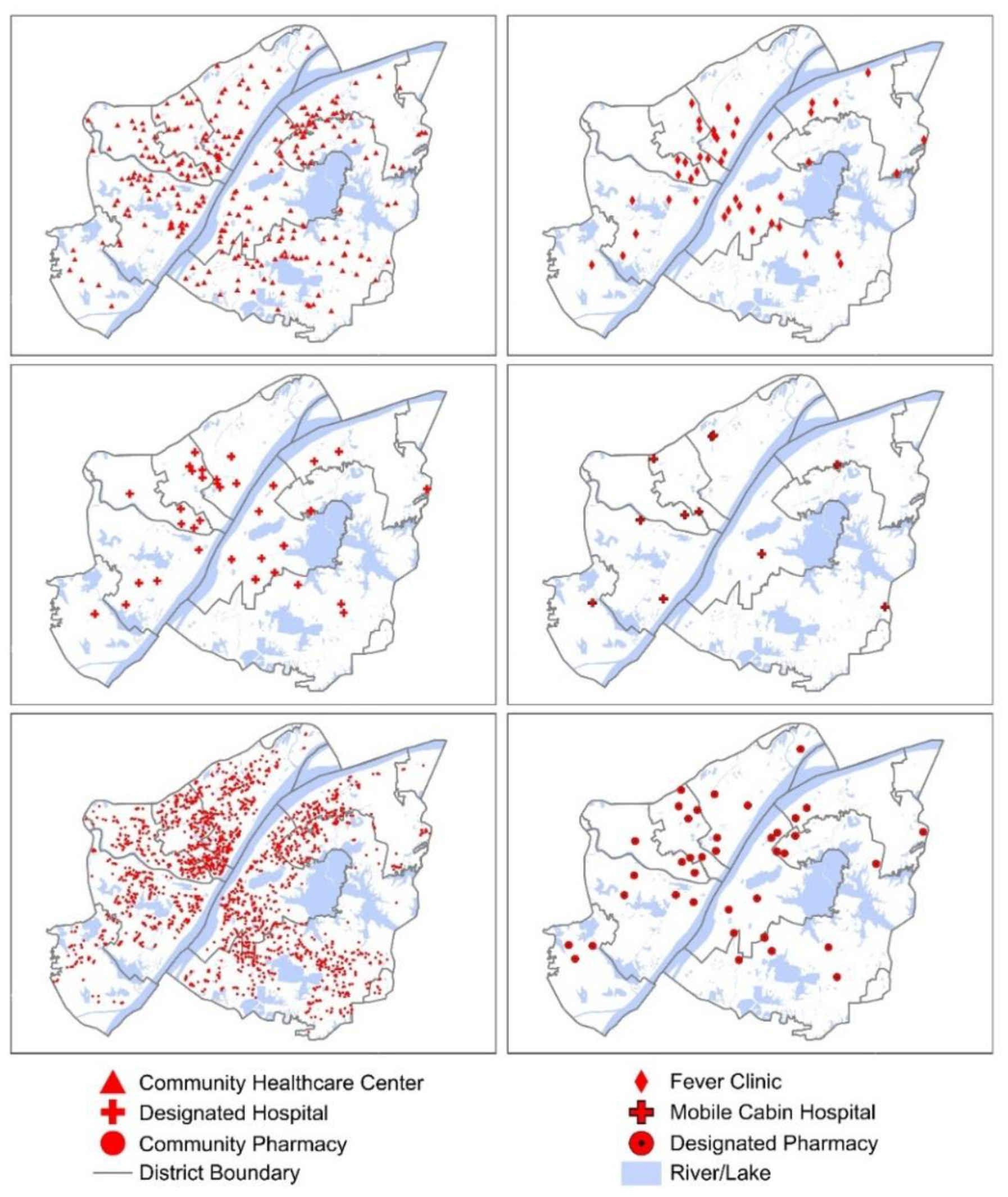






| Medical Facility | Number | Description | Formula |
|---|---|---|---|
| Community healthcare center | 297 | The population that community healthcare centers can serve under the 5, 10, and 15 min thresholds. | Service population * |
| Fever clinic | 44 | The population that each fever clinic can serve within the service area. | Service population * |
| Designated hospital | 35 | Combined with the hospital beds information, the service capacity of each designated hospital within the service area. | Population-hospital bed ratio: Service population */The number of hospital beds |
| Mobile cabin hospital | 11 | Combined with the hospital beds information, the service capacity of each mobile cabin hospital within the service area. | Population-hospital bed ratio: Service population */The number of hospital beds |
| Community pharmacy | 2137 | The population that community pharmacies can serve under the 5, 10, and 15 min thresholds. | Service population * |
| Designated pharmacy | 38 | The population that each designated pharmacy can serve within the service area. | Service population * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhou, Z.; Xu, Z.; Liu, A.; Zhou, S.; Mu, L.; Zhang, X. Mapping the Accessibility of Medical Facilities of Wuhan during the COVID-19 Pandemic. ISPRS Int. J. Geo-Inf. 2021, 10, 318. https://doi.org/10.3390/ijgi10050318
Zhou Z, Xu Z, Liu A, Zhou S, Mu L, Zhang X. Mapping the Accessibility of Medical Facilities of Wuhan during the COVID-19 Pandemic. ISPRS International Journal of Geo-Information. 2021; 10(5):318. https://doi.org/10.3390/ijgi10050318
Chicago/Turabian StyleZhou, Zhenqi, Zhen Xu, Anqi Liu, Shuang Zhou, Lan Mu, and Xuan Zhang. 2021. "Mapping the Accessibility of Medical Facilities of Wuhan during the COVID-19 Pandemic" ISPRS International Journal of Geo-Information 10, no. 5: 318. https://doi.org/10.3390/ijgi10050318
APA StyleZhou, Z., Xu, Z., Liu, A., Zhou, S., Mu, L., & Zhang, X. (2021). Mapping the Accessibility of Medical Facilities of Wuhan during the COVID-19 Pandemic. ISPRS International Journal of Geo-Information, 10(5), 318. https://doi.org/10.3390/ijgi10050318






