Spatiotemporal Patterns of Human Mobility and Its Association with Land Use Types during COVID-19 in New York City
Abstract
:1. Introduction
- What are the spatiotemporal human mobility patterns revealed by Twitter data at the tax lot level?
- How do human mobility patterns change by different land use types?
- How are the change patterns detected by Twitter different or similar to the change patterns detected by Google Community Mobility Report?
2. Background
2.1. Social Media for Human Mobility in Epidemiological Studies
2.2. Big Data for Human Mobility in Response to COVID-19
3. Study Area and Data
3.1. New York City
3.2. Google Community Mobility Report
3.3. Twitter Data
4. Methodology
4.1. Twitter Data Processing
4.2. Spatial Patterns of Human Mobility Changes
4.3. Daily Mobility Pattern Change by Land Use Type
5. Results
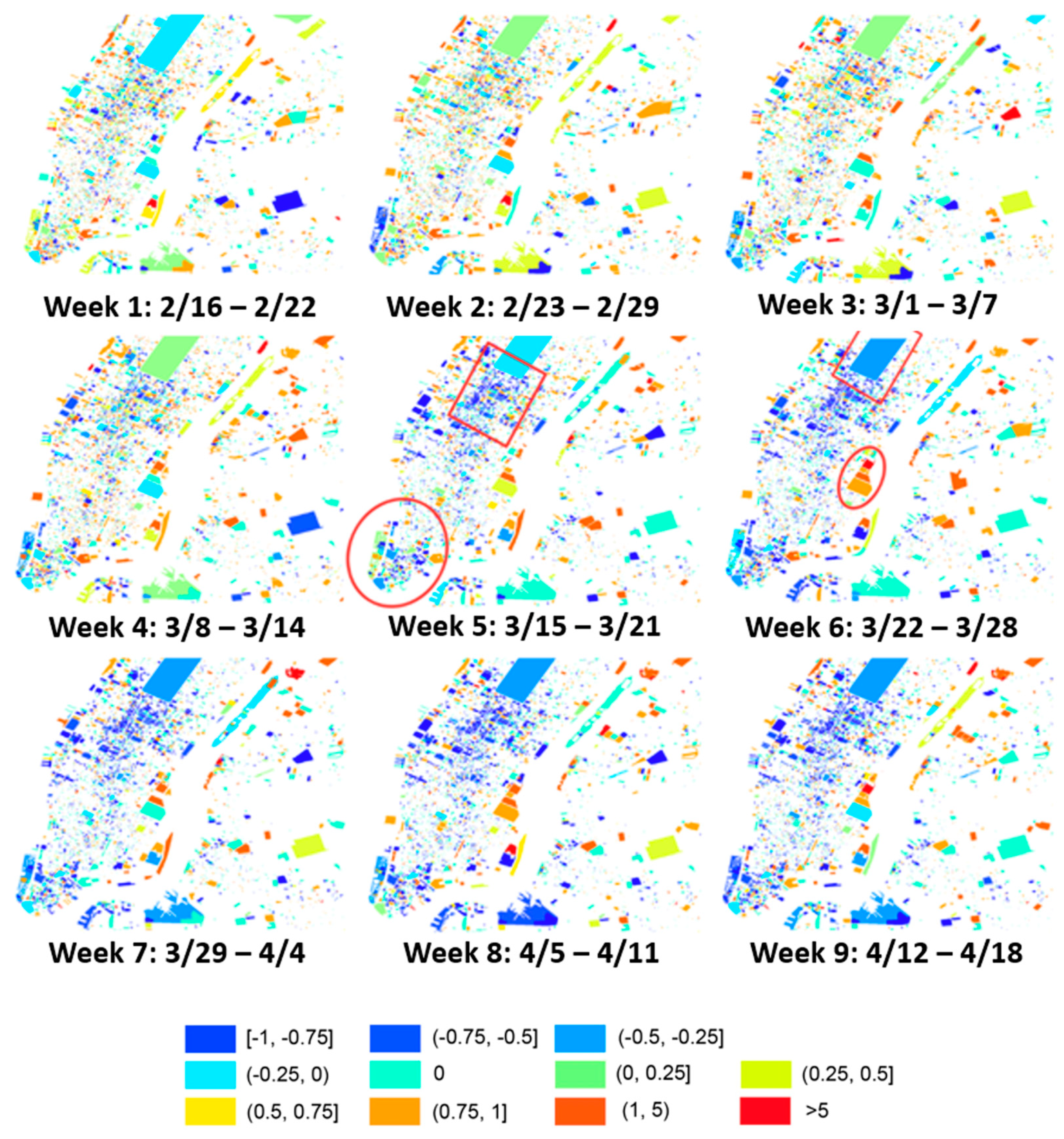
5.1. Spatial Human Mobility Patterns Based on Twitter Data
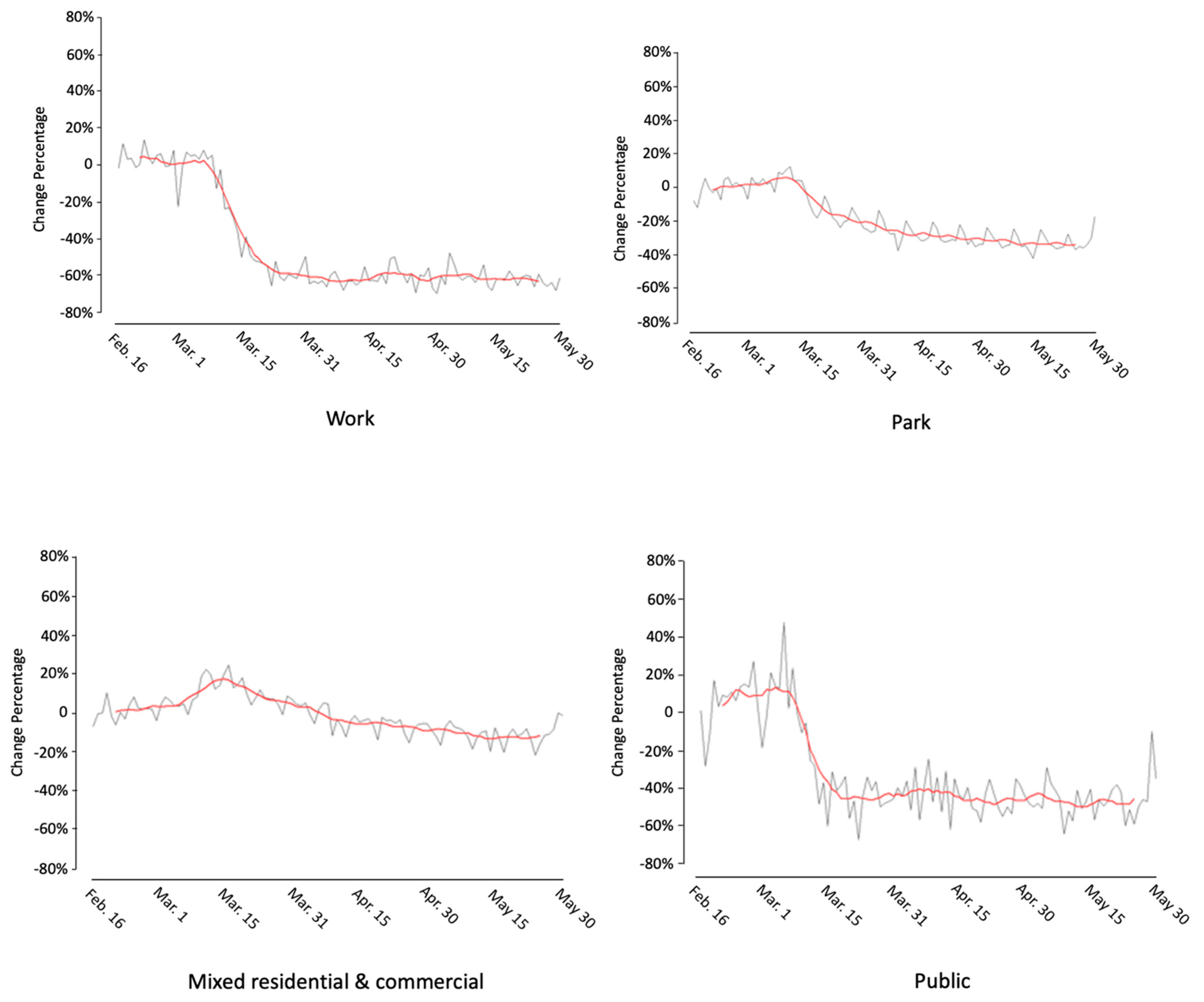
5.2. Temporal Changes by Land Use Type
5.2.1. Bronx County
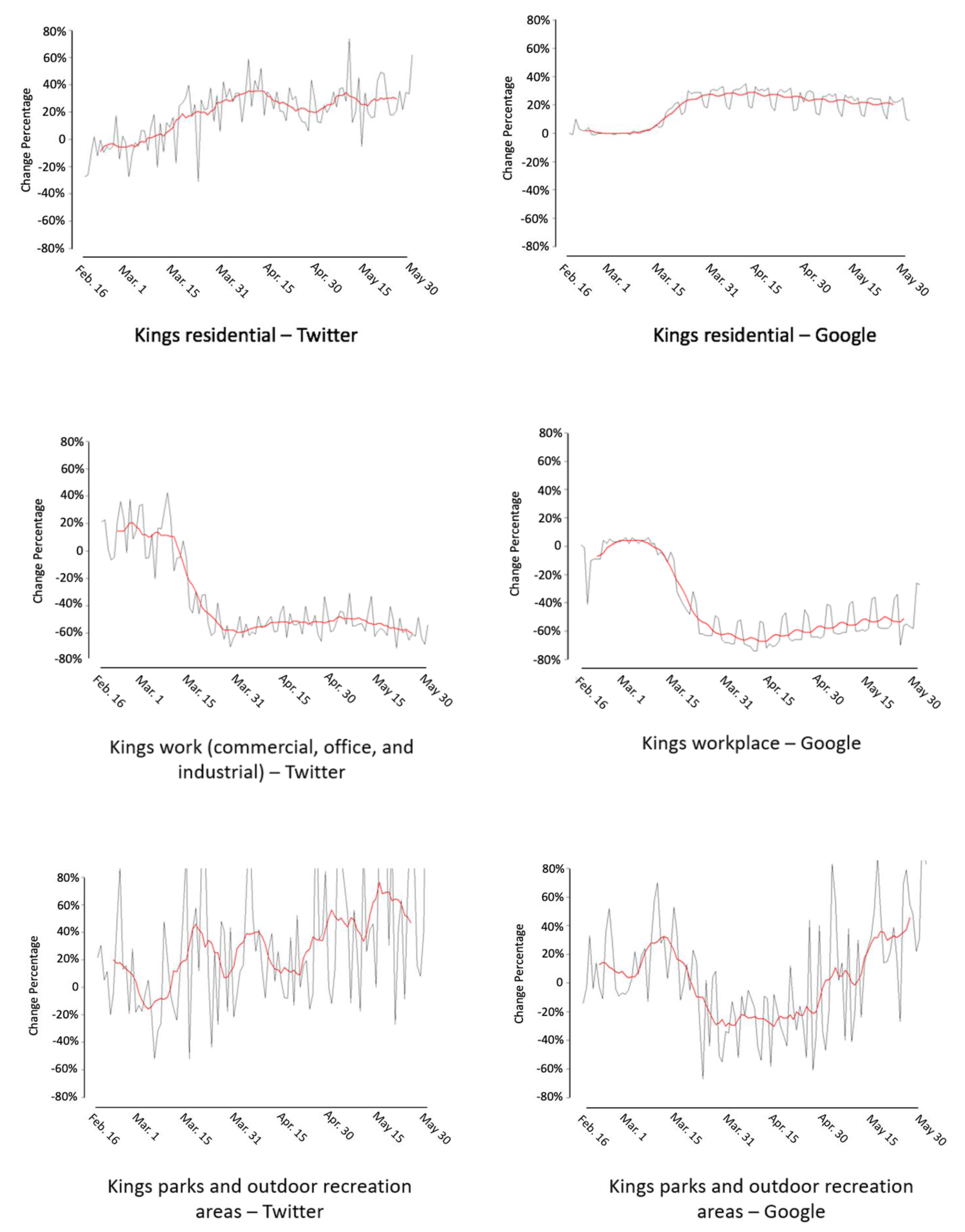
5.2.2. Kings County (Brooklyn Borough)
5.2.3. New York County (Manhattan Borough)
5.2.4. Queens County
6. Discussion
6.1. Comparison of Mobility Patterns Derived from Google and Twitter
6.2. Limitations
6.3. Future Research
7. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO Coronavirus Disease (COVID-19) Dashboard | WHO Coronavirus Disease (COVID-19) Dashboard. Available online: https://covid19.who.int/table (accessed on 28 September 2020).
- Calgary, O. United States COVID-19 Cases and Deaths by State over Time | Data | Centers for Disease Control and Prevention. Available online: https://data.cdc.gov/Case-Surveillance/United-States-COVID-19-Cases-and-Deaths-by-State-o/9mfq-cb36 (accessed on 27 September 2020).
- Proclamation on Declaring a National Emergency Concerning the Novel Coronavirus Disease (COVID-19) Outbreak. Available online: https://www.whitehouse.gov/presidential-actions/proclamation-declaring-national-emergency-concerning-novel-coronavirus-disease-covid-19-outbreak/ (accessed on 28 September 2020).
- CDC Coronavirus Disease 2019 (COVID-19). Available online: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/social-distancing.html (accessed on 28 September 2020).
- Kraemer, M.U.; Yang, C.-H.; Gutierrez, B.; Wu, C.-H.; Klein, B.; Pigott, D.M.; Du Plessis, L.; Faria, N.R.; Li, R.; Hanage, W.P. The Effect of Human Mobility and Control Measures on the COVID-19 Epidemic in China. Science 2020, 368, 493–497. [Google Scholar] [CrossRef] [Green Version]
- Maier, B.F.; Brockmann, D. Effective Containment Explains Subexponential Growth in Recent Confirmed COVID-19 Cases in China. Science 2020, 368, 742–746. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shim, E.; Tariq, A.; Choi, W.; Lee, Y.; Chowell, G. Transmission Potential and Severity of COVID-19 in South Korea. Int. J. Infect. Dis. 2020, 93, 339–344. [Google Scholar] [CrossRef]
- Gatto, M.; Bertuzzo, E.; Mari, L.; Miccoli, S.; Carraro, L.; Casagrandi, R.; Rinaldo, A. Spread and Dynamics of the COVID-19 Epidemic in Italy: Effects of Emergency Containment Measures. Proc. Natl. Acad. Sci. USA 2020, 117, 10484–10491. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Courtemanche, C.; Garuccio, J.; Le, A.; Pinkston, J.; Yelowitz, A. Strong Social Distancing Measures in The United States Reduced The COVID-19 Growth Rate: Study Evaluates the Impact of Social Distancing Measures on the Growth Rate of Confirmed COVID-19 Cases across the United States. Health Aff. 2020, 39, 1237–1246. [Google Scholar] [CrossRef] [PubMed]
- Pan, B.; Zheng, Y.; Wilkie, D.; Shahabi, C. Crowd Sensing of Traffic Anomalies Based on Human Mobility and Social Media. In Proceedings of the 21st ACM International Conference on Advances in Geographical Information Systems, Orlando, FL, USA, November 2013; Association for Computing Machinery: New York, NY, USA, 2013; pp. 344–353. [Google Scholar]
- Nawaz, M.S.; Bilal, M.; Lali, M.I.; Ul Mustafa, R.; Aslam, W.; Jajja, S. Effectiveness of Social Media Data in Healthcare Communication. J. Med. Imaging Health Inform. 2017, 7, 1365–1371. [Google Scholar] [CrossRef]
- Charles-Smith, L.E.; Reynolds, T.L.; Cameron, M.A.; Conway, M.; Lau, E.H.; Olsen, J.M.; Pavlin, J.A.; Shigematsu, M.; Streichert, L.C.; Suda, K.J. Using Social Media for Actionable Disease Surveillance and Outbreak Management: A Systematic Literature Review. PLoS ONE 2015, 10, e0139701. [Google Scholar] [CrossRef] [Green Version]
- Tang, L.; Bie, B.; Park, S.-E.; Zhi, D. Social Media and Outbreaks of Emerging Infectious Diseases: A Systematic Review of Literature. Am. J. Infect. Control 2018, 46, 962–972. [Google Scholar] [CrossRef] [PubMed]
- Lwin, M.O.; Lu, J.; Sheldenkar, A.; Schulz, P.J.; Shin, W.; Gupta, R.; Yang, Y. Global Sentiments Surrounding the COVID-19 Pandemic on Twitter: Analysis of Twitter Trends. JMIR Public Health Surveill. 2020, 6, e19447. [Google Scholar] [CrossRef]
- Zhu, B.; Zheng, X.; Liu, H.; Li, J.; Wang, P. Analysis of Spatiotemporal Characteristics of Big Data on Social Media Sentiment with COVID-19 Epidemic Topics. Chaos Solitons Fractals 2020, 140, 110123. [Google Scholar] [CrossRef]
- Liao, C.-M.; You, S.-H. Assessing Risk Perception and Behavioral Responses to Influenza Epidemics: Linking Information Theory to Probabilistic Risk Modeling. Stoch. Environ. Res. Risk Assess. 2014, 28, 189–200. [Google Scholar] [CrossRef]
- Bansal, S.; Chowell, G.; Simonsen, L.; Vespignani, A.; Viboud, C. Big Data for Infectious Disease Surveillance and Modeling. J. Infect. Dis. 2016, 214, S375–S379. [Google Scholar] [CrossRef] [PubMed]
- Ye, X.; Li, S.; Yang, X.; Qin, C. Use of Social Media for the Detection and Analysis of Infectious Diseases in China. ISPRS Int. J. Geo-Inf. 2016, 5, 156. [Google Scholar] [CrossRef] [Green Version]
- Lazard, A.J.; Scheinfeld, E.; Bernhardt, J.M.; Wilcox, G.B.; Suran, M. Detecting Themes of Public Concern: A Text Mining Analysis of the Centers for Disease Control and Prevention’s Ebola Live Twitter Chat. Am. J. Infect. Control 2015, 43, 1109–1111. [Google Scholar] [CrossRef]
- Fung, I.C.-H.; Duke, C.H.; Finch, K.C.; Snook, K.R.; Tseng, P.-L.; Hernandez, A.C.; Gambhir, M.; Fu, K.-W.; Tse, Z.T.H. Ebola Virus Disease and Social Media: A Systematic Review. Am. J. Infect. Control 2016, 44, 1660–1671. [Google Scholar] [CrossRef]
- Fu, K.-W.; Liang, H.; Saroha, N.; Tse, Z.T.H.; Ip, P.; Fung, I.C.-H. How People React to Zika Virus Outbreaks on Twitter? A Computational Content Analysis. Am. J. Infect. Control 2016, 44, 1700–1702. [Google Scholar] [CrossRef] [PubMed]
- Stefanidis, A.; Vraga, E.; Lamprianidis, G.; Radzikowski, J.; Delamater, P.L.; Jacobsen, K.H.; Pfoser, D.; Croitoru, A.; Crooks, A. Zika in Twitter: Temporal Variations of Locations, Actors, and Concepts. JMIR Public Health Surveill. 2017, 3, e22. [Google Scholar] [CrossRef] [PubMed]
- Chew, C.; Eysenbach, G. Pandemics in the Age of Twitter: Content Analysis of Tweets during the 2009 H1N1 Outbreak. PLoS ONE 2010, 5, e14118. [Google Scholar] [CrossRef] [PubMed]
- Signorini, A.; Segre, A.M.; Polgreen, P.M. The Use of Twitter to Track Levels of Disease Activity and Public Concern in the US during the Influenza A H1N1 Pandemic. PLoS ONE 2011, 6, e19467. [Google Scholar] [CrossRef] [Green Version]
- Albinati, J.; Meira, W., Jr.; Pappa, G.L.; Teixeira, M.; Marques-Toledo, C. Enhancement of Epidemiological Models for Dengue Fever Based on Twitter Data; Association for Computing Machinery: New York, NY, USA, 2017; pp. 109–118. [Google Scholar]
- Ramadona, A.L.; Tozan, Y.; Lazuardi, L.; Rocklöv, J. A Combination of Incidence Data and Mobility Proxies from Social Media Predicts the Intra-Urban Spread of Dengue in Yogyakarta, Indonesia. PLoS Negl. Trop. Dis. 2019, 13, e0007298. [Google Scholar] [CrossRef] [PubMed]
- Kraemer, M.U.; Bisanzio, D.; Reiner, R.; Zakar, R.; Hawkins, J.B.; Freifeld, C.C.; Smith, D.L.; Hay, S.I.; Brownstein, J.S.; Perkins, T.A. Inferences about Spatiotemporal Variation in Dengue Virus Transmission Are Sensitive to Assumptions about Human Mobility: A Case Study Using Geolocated Tweets from Lahore, Pakistan. EPJ Data Sci. 2018, 7, 16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Broniatowski, D.A.; Paul, M.J.; Dredze, M. National and Local Influenza Surveillance through Twitter: An Analysis of the 2012-2013 Influenza Epidemic. PLoS ONE 2013, 8, e83672. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Allen, C.; Tsou, M.-H.; Aslam, A.; Nagel, A.; Gawron, J.-M. Applying GIS and Machine Learning Methods to Twitter Data for Multiscale Surveillance of Influenza. PLoS ONE 2016, 11, e0157734. [Google Scholar] [CrossRef] [PubMed]
- Lai, S.; Ruktanonchai, N.W.; Zhou, L.; Prosper, O.; Luo, W.; Floyd, J.R.; Wesolowski, A.; Santillana, M.; Zhang, C.; Du, X. Effect of Non-Pharmaceutical Interventions for Containing the COVID-19 Outbreak in China. medRxiv 2020. [Google Scholar] [CrossRef] [Green Version]
- Barlacchi, G.; Perentis, C.; Mehrotra, A.; Musolesi, M.; Lepri, B. Are You Getting Sick? Predicting Influenza-like Symptoms Using Human Mobility Behaviors. EPJ Data Sci. 2017, 6, 27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Souza, R.C.; Assunção, R.M.; Neill, D.B.; Meira, W., Jr. Detecting Spatial Clusters of Disease Infection Risk Using Sparsely Sampled Social Media Mobility Patterns. In Proceedings of the 27th ACM SIGSPATIAL International Conference on Advances in Geographic Information Systems, Chicago, IL, USA, 5–8 November 2019; pp. 359–368. [Google Scholar]
- Franch-Pardo, I.; Napoletano, B.M.; Rosete-Verges, F.; Billa, L. Spatial Analysis and GIS in the Study of COVID-19. A Review. Sci. Total Environ. 2020, 739, 140033. [Google Scholar] [CrossRef]
- Yang, C.; Sha, D.; Liu, Q.; Li, Y.; Lan, H.; Guan, W.W.; Hu, T.; Li, Z.; Zhang, Z.; Thompson, J.H. Taking the Pulse of COVID-19: A Spatiotemporal Perspective. Int. J. Digit. Earth 2020, 1–26. [Google Scholar] [CrossRef]
- Zhou, C.; Su, F.; Pei, T.; Zhang, A.; Du, Y.; Luo, B.; Cao, Z.; Wang, J.; Yuan, W.; Zhu, Y. COVID-19: Challenges to GIS with Big Data. Geogr. Sustain. 2020, 1, 77–87. [Google Scholar] [CrossRef]
- Bragazzi, N.L.; Dai, H.; Damiani, G.; Behzadifar, M.; Martini, M.; Wu, J. How Big Data and Artificial Intelligence Can Help Better Manage the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 17, 3176. [Google Scholar] [CrossRef]
- Gasser, U.; Ienca, M.; Scheibner, J.; Sleigh, J.; Vayena, E. Digital Tools against COVID-19: Framing the Ethical Challenges and How to Address Them. arXiv 2020, arXiv:2004.10236. [Google Scholar]
- Li, Z.; Huang, X.; Hu, T.; Ning, H.; Ye, X.; Li, X. ODT FLOW: A Scalable Platform for Extracting, Analyzing, and Sharing Multi-Source Multi-Scale Human Mobility. arXiv 2021, arXiv:2104.05040. [Google Scholar]
- Guan, W.; Ni, Z.; Hu, Y.; Liang, W.; Ou, C.; He, J.; Liu, L.; Shan, H.; Lei, C.; Hui, D.S. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef]
- Huang, J.; Wang, H.; Fan, M.; Zhuo, A.; Sun, Y.; Li, Y. Understanding the Impact of the COVID-19 Pandemic on Transportation-Related Behaviors with Human Mobility Data. In Proceedings of the 26th ACM SIGKDD International Conference on Knowledge Discovery & Data Mining, CA, USA, July 2020; pp. 3443–3450. Available online: https://dl.acm.org/doi/10.1145/3394486.3412856 (accessed on 28 September 2020).
- Arab-Mazar, Z.; Sah, R.; Rabaan, A.A.; Dhama, K.; Rodriguez-Morales, A.J. Mapping the Incidence of the COVID-19 Hotspot in Iran–Implications for Travellers. Travel Med. Infect. Dis. 2020, 34, 101630. [Google Scholar] [CrossRef] [PubMed]
- Ahmadi, M.; Sharifi, A.; Dorosti, S.; Ghoushchi, S.J.; Ghanbari, N. Investigation of Effective Climatology Parameters on COVID-19 Outbreak in Iran. Sci. Total Environ. 2020, 729, 138705. [Google Scholar] [CrossRef] [PubMed]
- Giuliani, D.; Dickson, M.M.; Espa, G.; Santi, F. Modelling and Predicting the Spatio-Temporal Spread of Coronavirus Disease 2019 (COVID-19) in Italy. BMC Infect. Dis. 2020, 20, 700. [Google Scholar] [CrossRef] [Green Version]
- Grantz, K.H.; Meredith, H.R.; Cummings, D.A.; Metcalf, C.J.E.; Grenfell, B.T.; Giles, J.R.; Mehta, S.; Solomon, S.; Labrique, A.; Kishore, N. The Use of Mobile Phone Data to Inform Analysis of COVID-19 Pandemic Epidemiology. Nat. Commun. 2020, 11, 4961. [Google Scholar] [CrossRef] [PubMed]
- Keeling, M.J.; Hollingsworth, T.D.; Read, J.M. The Efficacy of Contact Tracing for the Containment of the 2019 Novel Coronavirus (COVID-19). medRxiv 2020. [Google Scholar] [CrossRef] [PubMed]
- Cho, H.; Ippolito, D.; Yu, Y.W. Contact Tracing Mobile Apps for COVID-19: Privacy Considerations and Related Trade-Offs. arXiv 2020, arXiv:2003.11511. [Google Scholar]
- Zhou, Y.; Xu, R.; Hu, D.; Yue, Y.; Li, Q.; Xia, J. Effects of Human Mobility Restrictions on the Spread of COVID-19 in Shenzhen, China: A Modelling Study Using Mobile Phone Data. Lancet Digit. Health 2020, 2, e417–e424. [Google Scholar] [CrossRef]
- Cecilia, J.M.; Cano, J.-C.; Hernández-Orallo, E.; Calafate, C.T.; Manzoni, P. Mobile Crowdsensing Approaches to Address the COVID-19 Pandemic in Spain. IET Smart Cities 2020, 2, 58–63. [Google Scholar] [CrossRef]
- Lee, D.; Lee, J. Testing on the Move South Korea’s Rapid Response to the COVID-19 Pandemic. Transp. Res. Interdiscip. Perspect. 2020, 5, 100111. [Google Scholar] [CrossRef]
- Gao, S.; Rao, J.; Kang, Y.; Liang, Y.; Kruse, J.; Doepfer, D.; Sethi, A.K.; Reyes, J.F.M.; Patz, J.; Yandell, B.S. Mobile Phone Location Data Reveal the Effect and Geographic Variation of Social Distancing on the Spread of the COVID-19 Epidemic. arXiv 2020, arXiv:2004.11430. [Google Scholar]
- Gao, S.; Rao, J.; Kang, Y.; Liang, Y.; Kruse, J. Mapping County-Level Mobility Pattern Changes in the United States in Response to COVID-19. SIGSPATIAL Spec. 2020, 12, 16–26. [Google Scholar] [CrossRef]
- Jeffrey, B.; Walters, C.E.; Ainslie, K.E.; Eales, O.; Ciavarella, C.; Bhatia, S.; Hayes, S.; Baguelin, M.; Boonyasiri, A.; Brazeau, N.F. Anonymised and Aggregated Crowd Level Mobility Data from Mobile Phones Suggests That Initial Compliance with COVID-19 Social Distancing Interventions Was High and Geographically Consistent across the UK. Wellcome Open Res. 2020, 5, 170. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.; Lu, J.; Gao, S.; Wang, S.; Liu, Z.; Wei, H. Staying at Home Is a Privilege: Evidence from Fine-Grained Mobile Phone Location Data in the U.S. during the COVID-19 Pandemic. Ann. Am. Assoc. Geogr. 2021. [Google Scholar] [CrossRef]
- Huang, X.; Li, Z.; Lu, J.; Wang, S.; Wei, H.; Chen, B. Time-Series Clustering for Home Dwell Time during COVID-19: What Can We Learn from It? ISPRS Int. J. Geo-Inf. 2020, 9, 675. [Google Scholar] [CrossRef]
- Kang, Y.; Gao, S.; Liang, Y.; Li, M.; Rao, J.; Kruse, J. Multiscale Dynamic Human Mobility Flow Dataset in the US during the COVID-19 Epidemic. Sci. Data 2020, 7, 390. [Google Scholar] [CrossRef]
- Gao, S.; Rao, J.; Kang, Y.; Liang, Y.; Kruse, J.; Dopfer, D.; Sethi, A.K.; Reyes, J.F.M.; Yandell, B.S.; Patz, J.A. Association of Mobile Phone Location Data Indications of Travel and Stay-at-Home Mandates with Covid-19 Infection Rates in the Us. JAMA Netw. Open 2020, 3, e2020485. [Google Scholar] [CrossRef]
- Kogan, N.E.; Clemente, L.; Liautaud, P.; Kaashoek, J.; Link, N.B.; Nguyen, A.T.; Lu, F.S.; Huybers, P.; Resch, B.; Havas, C. An Early Warning Approach to Monitor COVID-19 Activity with Multiple Digital Traces in near Real Time. Sci. Adv. 2021, 7, eabd6989. [Google Scholar] [CrossRef] [PubMed]
- Queiroz, L.; Ferraz, A.; Melo, J.L.; Barboza, G.; Urbanski, A.H.; Nicolau, A.; Oliva, S.; Nakaya, H. Large-Scale Assessment of Human Mobility during COVID-19 Outbreak. 2020. Available online: https://osf.io/nqxrd/ (accessed on 28 September 2020).
- Huang, X.; Li, Z.; Jiang, Y.; Li, X.; Porter, D. Twitter, Human Mobility, and COVID-19. arXiv 2020, arXiv:2007.01100. [Google Scholar]
- Cotti, C.D.; Engelhardt, B.; Foster, J.; Nesson, E.T.; Niekamp, P.S. The Relationship between In-Person Voting, Consolidated Polling Locations, and Absentee Voting on Covid-19: Evidence from the Wisconsin Primary; National Bureau of Economic Research: Cambridge, MA, USA, 2020. [Google Scholar]
- Ghader, S.; Zhao, J.; Lee, M.; Zhou, W.; Zhao, G.; Zhang, L. Observed Mobility Behavior Data Reveal Social Distancing Inertia. arXiv 2020, arXiv:2004.14748. [Google Scholar]
- Zhao, J.; Lee, M.; Ghader, S.; Younes, H.; Darzi, A.; Xiong, C.; Zhang, L. Quarantine Fatigue: First-Ever Decrease in Social Distancing Measures after the COVID-19 Pandemic Outbreak before Reopening United States. arXiv 2020, arXiv:2006.03716. [Google Scholar]
- Bisanzio, D.; Kraemer, M.U.; Bogoch, I.I.; Brewer, T.; Brownstein, J.S.; Reithinger, R. Use of Twitter Social Media Activity as a Proxy for Human Mobility to Predict the Spatiotemporal Spread of COVID-19 at Global Scale. Geospat. Health 2020, 15. [Google Scholar] [CrossRef]
- Porcher, S.; Renault, T. Social Distancing Beliefs and Human Mobility: Evidence from Twitter. arXiv 2020, arXiv:2008.04826. [Google Scholar]
- Huang, X.; Li, Z.; Jiang, Y.; Ye, X.; Deng, C.; Zhang, J.; Li, X. The Characteristics of Multi-Source Mobility Datasets and How They Reveal the Luxury Nature of Social Distancing in the US during the COVID-19 Pandemic. medRxiv 2020. [Google Scholar] [CrossRef]
- Li, L.; Zhang, Q.; Wang, X.; Zhang, J.; Wang, T.; Gao, T.-L.; Duan, W.; Tsoi, K.K.; Wang, F.-Y. Characterizing the Propagation of Situational Information in Social Media during Covid-19 Epidemic: A Case Study on Weibo. IEEE Trans. Comput. Soc. Syst. 2020, 7, 556–562. [Google Scholar] [CrossRef]
- Cinelli, M.; Quattrociocchi, W.; Galeazzi, A.; Valensise, C.M.; Brugnoli, E.; Schmidt, A.L.; Zola, P.; Zollo, F.; Scala, A. The Covid-19 Social Media Infodemic. Sci. Rep. 2020, 10, 16598. [Google Scholar] [CrossRef]
- Depoux, A.; Martin, S.; Karafillakis, E.; Preet, R.; Wilder-Smith, A.; Larson, H. The Pandemic of Social Media Panic Travels Faster than the COVID-19 Outbreak. J. Travel Med. 2020, 27, taaa031. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bridgman, A.; Merkley, E.; Loewen, P.J.; Owen, T.; Ruths, D.; Teichmann, L.; Zhilin, O. The Causes and Consequences of COVID-19 Misperceptions: Understanding the Role of News and Social Media. Harv. Kennedy Sch. Misinform. Rev. 2020, 1. [Google Scholar] [CrossRef]
- Kouzy, R.; Abi Jaoude, J.; Kraitem, A.; El Alam, M.B.; Karam, B.; Adib, E.; Zarka, J.; Traboulsi, C.; Akl, E.W.; Baddour, K. Coronavirus Goes Viral: Quantifying the COVID-19 Misinformation Epidemic on Twitter. Cureus 2020, 12, e7255. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gao, J.; Zheng, P.; Jia, Y.; Chen, H.; Mao, Y.; Chen, S.; Wang, Y.; Fu, H.; Dai, J. Mental Health Problems and Social Media Exposure during COVID-19 Outbreak. PLoS ONE 2020, 15, e0231924. [Google Scholar] [CrossRef]
- Wahbeh, A.; Nasralah, T.; Al-Ramahi, M.; El-Gayar, O. Mining Physicians’ Opinions on Social Media to Obtain Insights into COVID-19: Mixed Methods Analysis. JMIR Public Health Surveill. 2020, 6, e19276. [Google Scholar] [CrossRef]
- Li, D.; Chaudhary, H.; Zhang, Z. Modeling Spatiotemporal Pattern of Depressive Symptoms Caused by COVID-19 Using Social Media Data Mining. Int. J. Environ. Res. Public Health 2020, 17, 4988. [Google Scholar] [CrossRef] [PubMed]
- Koh, J.X.; Liew, T.M. How Loneliness Is Talked about in Social Media during COVID-19 Pandemic: Text Mining of 4,492 Twitter Feeds. J. Psychiatr. Res. 2020. [Google Scholar] [CrossRef] [PubMed]
- New York City Department of City Planning PLUTO DATA DICTIONARY September 2020 (20v6). Available online: http://www.nyc.gov/html/dcp/html/bytes/applbyte.shtml (accessed on 28 September 2020).
- Google LLC. COVID-19 Community Mobility Report. Available online: https://www.google.com/covid19/mobility?hl=en. (accessed on 2 December 2020).
- Pfeffer, J.; Mayer, K.; Morstatter, F. Tampering with Twitter’s Sample API. EPJ Data Sci. 2018, 7, 50. [Google Scholar] [CrossRef] [Green Version]
- Jiang, Y.; Li, Z.; Ye, X. Understanding Demographic and Socioeconomic Biases of Geotagged Twitter Users at the County Level. Cartogr. Geogr. Inf. Sci. 2019, 46, 228–242. [Google Scholar] [CrossRef]
- Malik, M.M.; Lamba, H.; Nakos, C.; Pfeffer, J. Population Bias in Geotagged Tweets. People 2015, 1, 3–759. [Google Scholar]
- Hecht, B.J.; Stephens, M. A Tale of Cities: Urban Biases in Volunteered Geographic Information. ICWSM 2014, 14, 197–205. [Google Scholar]
- Zhao, Z.; Shaw, S.-L.; Xu, Y.; Lu, F.; Chen, J.; Yin, L. Understanding the Bias of Call Detail Records in Human Mobility Research. Int. J. Geogr. Inf. Sci. 2016, 30, 1738–1762. [Google Scholar] [CrossRef]
- Wesolowski, A.; Eagle, N.; Noor, A.M.; Snow, R.W.; Buckee, C.O. The Impact of Biases in Mobile Phone Ownership on Estimates of Human Mobility. J. R. Soc. Interface 2013, 10, 20120986. [Google Scholar] [CrossRef]
- Hooper, M.W.; Nápoles, A.M.; Pérez-Stable, E.J. COVID-19 and Racial/Ethnic Disparities. JAMA 2020, 323, 2466–2467. [Google Scholar] [CrossRef] [PubMed]






Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jiang, Y.; Huang, X.; Li, Z. Spatiotemporal Patterns of Human Mobility and Its Association with Land Use Types during COVID-19 in New York City. ISPRS Int. J. Geo-Inf. 2021, 10, 344. https://doi.org/10.3390/ijgi10050344
Jiang Y, Huang X, Li Z. Spatiotemporal Patterns of Human Mobility and Its Association with Land Use Types during COVID-19 in New York City. ISPRS International Journal of Geo-Information. 2021; 10(5):344. https://doi.org/10.3390/ijgi10050344
Chicago/Turabian StyleJiang, Yuqin, Xiao Huang, and Zhenlong Li. 2021. "Spatiotemporal Patterns of Human Mobility and Its Association with Land Use Types during COVID-19 in New York City" ISPRS International Journal of Geo-Information 10, no. 5: 344. https://doi.org/10.3390/ijgi10050344
APA StyleJiang, Y., Huang, X., & Li, Z. (2021). Spatiotemporal Patterns of Human Mobility and Its Association with Land Use Types during COVID-19 in New York City. ISPRS International Journal of Geo-Information, 10(5), 344. https://doi.org/10.3390/ijgi10050344







