Spatial Patterns of the Spread of COVID-19 in Singapore and the Influencing Factors
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Area and Data Collection
2.2. Methods
2.2.1. Spatial Autocorrelation Analysis
2.2.2. Variable Selection and Modeling
3. Results
3.1. The Six-Phase Division of the Studied Time Duration
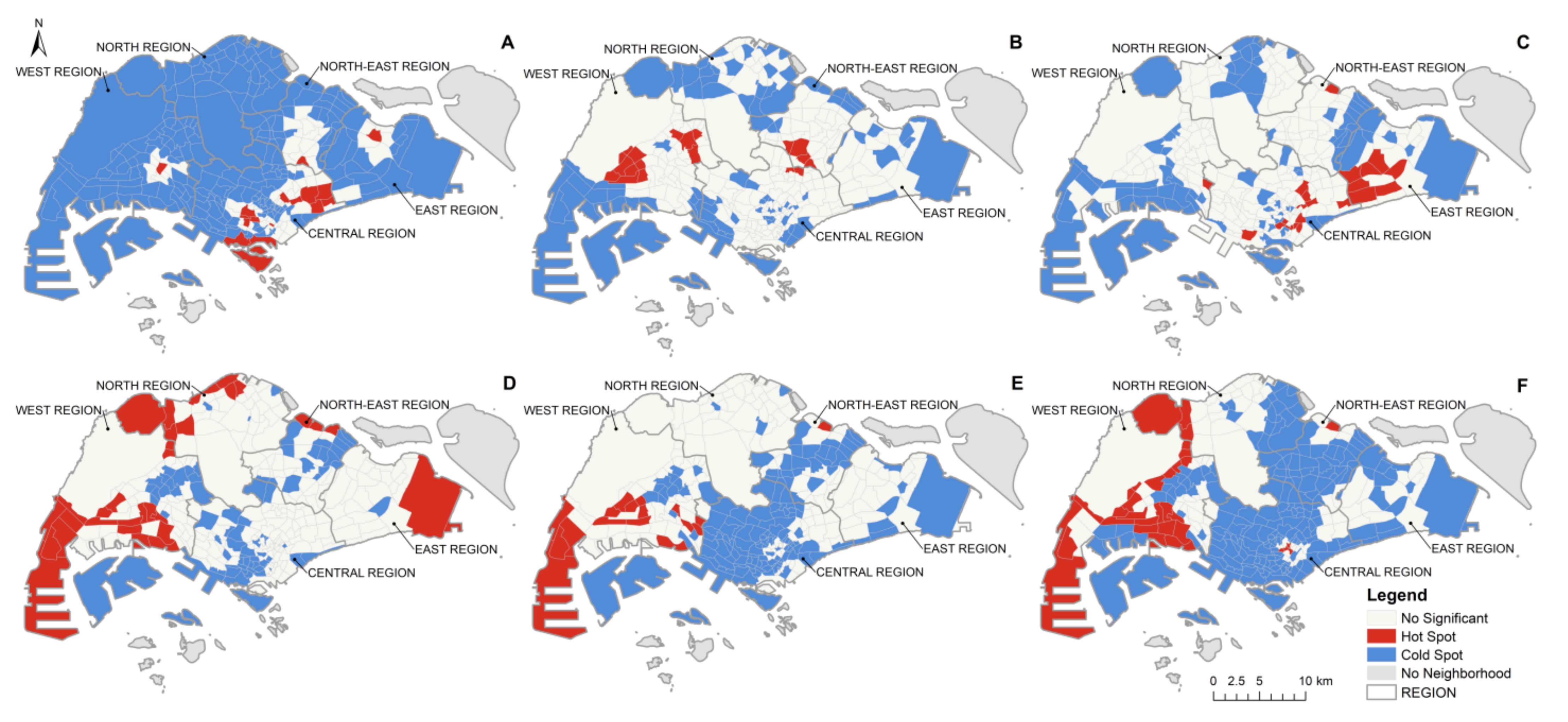
3.2. Spatial Distribution Patterns of the COVID-19 Pandemic in Singapore
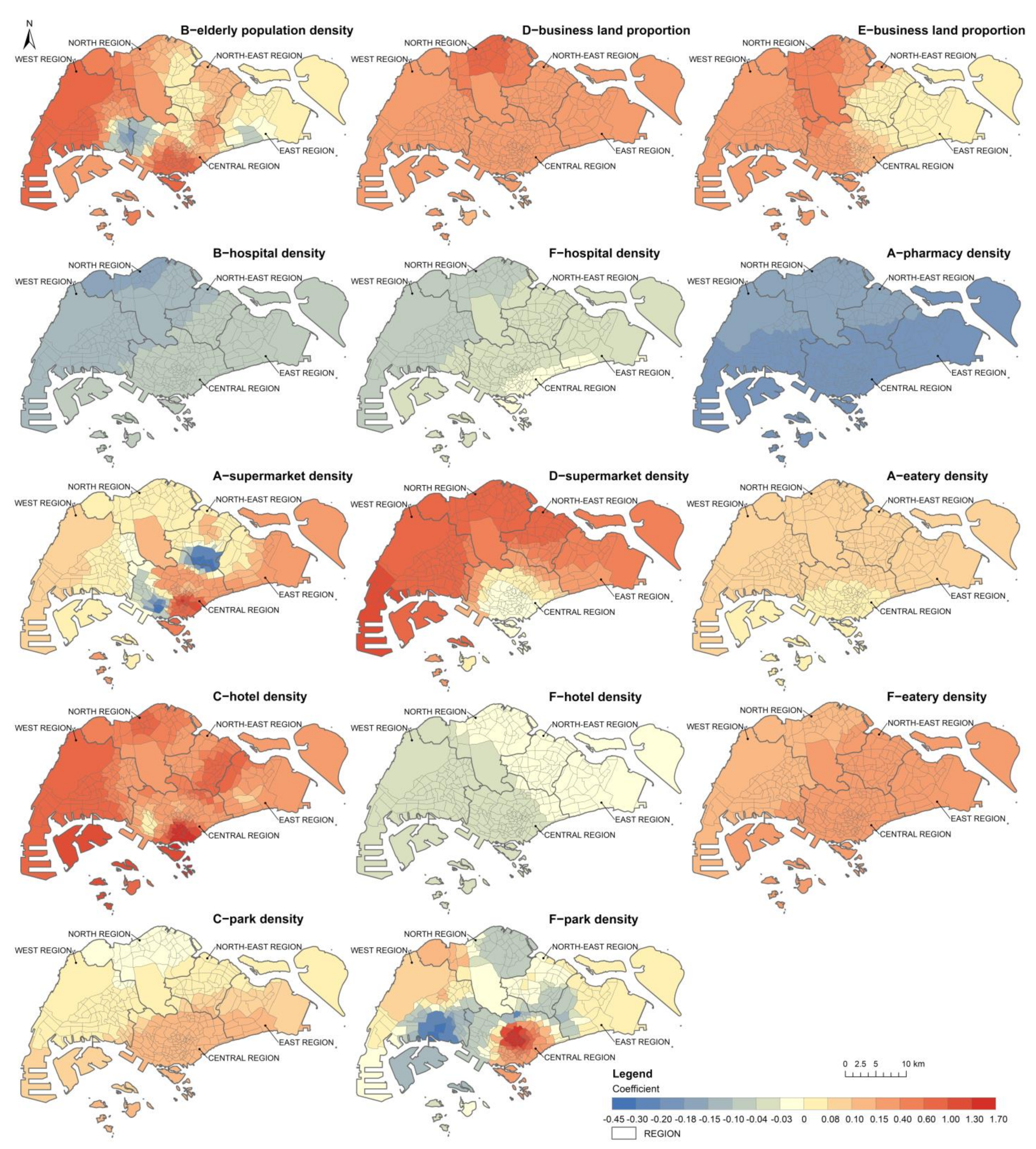
3.3. The Associations between Demographic and Built-Environment Factors with the COVID-19 Incidence Density
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 31 December 2020).
- World Health Organization. Coronavirus Disease 2019 (COVID-19): Situation Report. Weekly Epidemiological Update on COVID-19—28 September 2021. Available online: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19—28-september-2021 (accessed on 15 October 2021).
- Tian, H.; Liu, Y.; Li, Y.; Wu, C.-H.; Chen, B.; Kraemer, M.U.G.; Li, B.; Cai, J.; Xu, B.; Yang, Q.; et al. An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China. Science 2020, 368, 638–642. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carballada, A.M.; Balsa-Barreiro, J. Geospatial Analysis and Mapping Strategies for Fine-Grained and Detailed COVID-19 Data with GIS. ISPRS Int. J. Geo-Inf. 2021, 10, 602. [Google Scholar] [CrossRef]
- Franch-Pardo, I.; Napoletano, B.M.; Rosete-Verges, F.; Billa, L. Spatial analysis and GIS in the study of COVID-19. A review. Sci. Total Environ. 2020, 739, 140033. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Du, D.; Wei, Y.; Yang, H. The development of COVID-19 in China: Spatial diffusion and geographical pattern. Geogr. Res. 2020, 39, 1450–1462. [Google Scholar]
- Huang, Z. Spatiotemporal Evolution Patterns of the COVID-19 Pandemic Using Space-Time Aggregation and Spatial Statistics: A Global Perspective. ISPRS Int. J. Geo-Inf. 2021, 10, 519. [Google Scholar] [CrossRef]
- Caprarelli, G.; Fletcher, S. A brief review of spatial analysis concepts and tools used for mapping, containment and risk modelling of infectious diseases and other illnesses. Parasitology 2014, 141, 581–601. [Google Scholar] [CrossRef]
- Scarpone, C.; Brinkmann, S.T.; Grosse, T.; Sonnenwald, D.; Fuchs, M.; Walker, B.B. A multimethod approach for county-scale geospatial analysis of emerging infectious diseases: A cross-sectional case study of COVID-19 incidence in Germany. Int. J. Health Geogr. 2020, 19, 32. [Google Scholar] [CrossRef]
- Kwok, K.O.; Lai, F.Y.L.; Wei, V.W.I.; Tsoi, M.T.F.; Wong, S.Y.S.; Tang, J.W.T. Comparing the impact of various interventions to control the spread of COVID-19 in twelve countries. J. Hosp. Infect. 2020, 106, 214–216. [Google Scholar] [CrossRef]
- Giuliani, D.; Dickson, M.M.; Espa, G.; Santi, F. Modelling and predicting the spatio-temporal spread of COVID-19 in Italy. BMC Infect. Dis. 2020, 20, 700. [Google Scholar] [CrossRef]
- Yang, W.; Deng, M.; Li, C.; Huang, J. Spatio-Temporal Patterns of the 2019-nCoV Epidemic at the County Level in Hubei Province, China. Int. J. Environ. Res. Public Health 2020, 17, 2563. [Google Scholar] [CrossRef] [Green Version]
- Chen, X.; Huang, Y.; Li, J.; Wang, S.; Pei, T. Clustering characteristics of COVID-19 cases and influencing factors in Chongqing Municipality. Prog. Geogr. 2020, 39, 11. [Google Scholar] [CrossRef]
- Sannigrahi, S.; Pilla, F.; Basu, B.; Basu, A.S.; Molter, A. Examining the association between socio-demographic composition and COVID-19 fatalities in the European region using spatial regression approach. Sust. Cities Soc. 2020, 62, 102418. [Google Scholar] [CrossRef]
- Zheng, A.; Wang, T.; Li, X. Spatiotemporal Characteristics and Risk Factors of the COVID-19 Pandemic in New York State: Implication of Future Policies. ISPRS Int. J. Geo-Inf. 2021, 10, 627. [Google Scholar] [CrossRef]
- Zhang, C.H.; Schwartz, G.G. Spatial Disparities in Coronavirus Incidence and Mortality in the United States: An Ecological Analysis as of May 2020. J. Rural Health 2020, 36, 433–445. [Google Scholar] [CrossRef]
- Mansour, S.; Al Kindi, A.; Al-Said, A.; Al-Said, A.; Atkinson, P. Sociodemographic determinants of COVID-19 incidence rates in Oman: Geospatial modelling using multiscale geographically weighted regression (MGWR). Sust. Cities Soc. 2021, 65, 102627. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Hao, J.; Sun, Y.; Shi, Z. Network analysis of population flow among major cities and its influence on COVID-19 transmission in China. Cities 2021, 112, 103138. [Google Scholar] [CrossRef]
- Liu, Y.; He, Z.; Zhou, X. Space-Time Variation and Spatial Differentiation of COVID-19 Confirmed Cases in Hubei Province Based on Extended GWR. ISPRS Int. J. Geo-Inf. 2020, 9, 536. [Google Scholar] [CrossRef]
- Mollalo, A.; Vahedi, B.; Rivera, K.M. GIS-based spatial modeling of COVID-19 incidence rate in the continental United States. Sci. Total Environ. 2020, 728, 138884. [Google Scholar] [CrossRef] [PubMed]
- Kan, Z.; Kwan, M.-P.; Wong, M.S.; Huang, J.; Liu, D. Identifying the space-time patterns of COVID-19 risk and their associations with different built environment features in Hong Kong. Sci. Total Environ. 2021, 772, 145379. [Google Scholar] [CrossRef]
- You, H.; Wu, X.; Guo, X. Distribution of COVID-19 Morbidity Rate in Association with Social and Economic Factors in Wuhan, China: Implications for Urban Development. Int. J. Environ. Res. Public Health 2020, 17, 3417. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Zhou, L.; Jia, T.; Peng, R.; Fu, X.; Zou, Y. Associating COVID-19 Severity with Urban Factors: A Case Study of Wuhan. Int. J. Environ. Res. Public Health 2020, 17, 6712. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Kwan, M.-P.; Kan, Z.; Wong, M.S.; Kwok, C.Y.T.; Yu, X. Investigating the Relationship between the Built Environment and Relative Risk of COVID-19 in Hong Kong. ISPRS Int. J. Geo-Inf. 2020, 9, 624. [Google Scholar] [CrossRef]
- Lu, Y.; Zhao, J.; Wu, X.; Lo, S.M. Escaping to nature during a pandemic: A natural experiment in Asian cities during the COVID-19 pandemic with big social media data. Sci. Total Environ. 2021, 777, 146092. [Google Scholar] [CrossRef]
- Pan, J.; Bardhan, R.; Jin, Y. Spatial distributive effects of public green space and COVID-19 infection in London. Urban For. Urban Green. 2021, 62, 127182. [Google Scholar] [CrossRef] [PubMed]
- Chang, S.; Pierson, E.; Koh, P.W.; Gerardin, J.; Redbird, B.; Grusky, D.; Leskovec, J. Mobility network models of COVID-19 explain inequities and inform reopening. Nature 2021, 589, 82–87. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Kwan, M.-P.; Kan, Z. The superspreading places of COVID-19 and the associated built-environment and socio-demographic features: A study using a spatial network framework and individual-level activity data. Health Place 2021, 72, 102694. [Google Scholar] [CrossRef]
- Wang, L.; Zhang, S.; Yang, Z.; Zhao, Z.; Moudon, A.V.; Feng, H.; Liang, J.; Sun, W.; Cao, B. What county-level factors influence COVID-19 incidence in the United States? Findings from the first wave of the pandemic. Cities 2021, 118, 103396. [Google Scholar] [CrossRef]
- Wu, X.; Yin, J.; Li, C.; Xiang, H.; Lv, M.; Guo, Z. Natural and human environment interactively drive spread pattern of COVID-19: A city-level modeling study in China. Sci. Total Environ. 2021, 756, 143343. [Google Scholar] [CrossRef]
- Niehus, R.; De Salazar, P.M.; Taylor, A.R.; Lipsitch, M. Using observational data to quantify bias of traveller-derived COVID-19 prevalence estimates in Wuhan, China. Lancet Infect. Dis. 2020, 20, 803–808. [Google Scholar] [CrossRef]
- Anderson, R.M.; Heesterbeek, H.; Klinkenberg, D.; Hollingsworth, T.D. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet 2020, 395, 931–934. [Google Scholar] [CrossRef]
- Capano, G.; Howlett, M.; Jarvis, D.S.L.; Ramesh, M.; Goyal, N. Mobilizing Policy (In)Capacity to Fight COVID-19: Understanding Variations in State Responses. Policy Soc. 2020, 39, 285–308. [Google Scholar] [CrossRef]
- Koo, J.R.; Cook, A.R.; Park, M.; Sun, Y.; Sun, H.; Lim, J.T.; Tam, C.; Dickens, B.L. Interventions to mitigate early spread of SARS-CoV-2 in Singapore: A modelling study. Lancet Infect. Dis. 2020, 20, 678–688. [Google Scholar] [CrossRef] [Green Version]
- Tariq, A.; Lee, Y.; Roosa, K.; Blumberg, S.; Yan, P.; Ma, S.; Chowell, G. Real-time monitoring the transmission potential of COVID-19 in Singapore, March 2020. BMC Med. 2020, 18, 166. [Google Scholar] [CrossRef]
- Pung, R.; Chiew, C.J.; Young, B.E.; Chin, S.; Chen, M.I.C.; Clapham, H.E.; Cook, A.R.; Maurer-Stroh, S.; Toh, M.P.H.S.; Poh, C.; et al. Investigation of three clusters of COVID-19 in Singapore: Implications for surveillance and response measures. Lancet 2020, 395, 1039–1046. [Google Scholar] [CrossRef]
- Yi, H.; Ng, S.T.; Farwin, A.; Low, P.T.A.; Chang, C.M.; Lim, J. Health equity considerations in COVID-19: Geospatial network analysis of the COVID-19 outbreak in the migrant population in Singapore. J. Travel Med. 2020, 28, taaa159. [Google Scholar] [CrossRef]
- Jiang, P.; Fu, X.; Fan, Y.V.; Klemes, J.J.; Chen, P.; Ma, S.; Zhang, W. Spatial-temporal potential exposure risk analytics and urban sustainability impacts related to COVID-19 mitigation: A perspective from car mobility behaviour. J. Clean Prod. 2021, 279, 123673. [Google Scholar] [CrossRef] [PubMed]
- Woo, J.J. Policy capacity and Singapore’s response to the COVID-19 pandemic. Policy Soc. 2020, 39, 345–362. [Google Scholar] [CrossRef]
- Government Technology Agency of Singapore. Master Plan 2019 Region Boundary (No Sea). Available online: https://geo.data.gov.sg/ura-mp19-region-no-sea-pl/2019/12/23/kml/ura-mp19-region-no-sea-pl.kml (accessed on 1 December 2020).
- Government Technology Agency of Singapore. Master Plan 2019 Subzone Boundary (No Sea). Available online: https://geo.data.gov.sg/ura-mp19-subzone-no-sea-pl/2019/12/23/kml/ura-mp19-subzone-no-sea-pl.kml (accessed on 1 December 2020).
- Ministry of Health, Singapore. Updates on COVID-19 (Coronavirus Disease 2019) Local Situation. Available online: https://www.moh.gov.sg/covid-19 (accessed on 15 November 2020).
- Getis, A.; Ord, J.K. The Analysis of Spatial Association by Use of Distance Statistics. Geogr. Anal. 1992, 24, 189–206. [Google Scholar] [CrossRef]
- Moran, P.A.P. The Interpretation of Statistical Maps. J. R. Stat. Soc. Ser. B Methodol. 1948, 10, 243–251. [Google Scholar] [CrossRef]
- Fotheringham, A.S.; Yang, W.; Kang, W. Multiscale Geographically Weighted Regression (MGWR). Ann. Am. Assoc. Geogr. 2017, 107, 1247–1265. [Google Scholar] [CrossRef]
- Oshan, T.M.; Smith, J.P.; Fotheringham, A.S. Targeting the spatial context of obesity determinants via multiscale geographically weighted regression. Int. J. Health Geogr. 2020, 19, 11. [Google Scholar] [CrossRef]
- Iyanda, A.E.; Adeleke, R.; Lu, Y.; Osayomi, T.; Adaralegbe, A.; Lasode, M.; Chima-Adaralegbe, N.J.; Osundina, A.M. A retrospective cross-national examination of COVID-19 outbreak in 175 countries: A multiscale geographically weighted regression analysis (January 11-June 28, 2020). J. Infect. Public Health 2020, 13, 1438–1445. [Google Scholar] [CrossRef] [PubMed]
- Tonidandel, S.; LeBreton, J.M. Relative Importance Analysis: A Useful Supplement to Regression Analysis. J. Bus. Psychol. 2011, 26, 1–9. [Google Scholar] [CrossRef]
- Oshan, T.M.; Li, Z.; Kang, W.; Wolf, L.J.; Fotheringham, A.S. mgwr: A Python Implementation of Multiscale Geographically Weighted Regression for Investigating Process Spatial Heterogeneity and Scale. ISPRS Int. J. Geo-Inf. 2019, 8, 269. [Google Scholar] [CrossRef] [Green Version]
- Ministry of Health, Singapore. End of Circuit Breaker, Phased Approach to Resuming Activities Safely. Available online: https://www.moh.gov.sg/news-highlights/details/end-of-circuit-breaker-phased-approach-to-resuming-activities-safely (accessed on 20 May 2020).
- Thomas, H.; Angrist, N.; Cameron-Blake, E.; Hallas, L.; Kira, B.; Majumdar, S.; Petherick, A.; Phillips, T.; Tatlow, H.; Webster, S. Oxford COVID-19 Government Response Tracker. Available online: https://www.bsg.ox.ac.uk/research/research-projects/coronavirus-government-response-tracker (accessed on 25 December 2020).
- Aral, N.; Bakir, H. Spatiotemporal Analysis of COVID-19 in Turkey. Sustain. Cities Soc. 2022, 76, 103421. [Google Scholar] [CrossRef]
- Li, S.; Ma, S.; Zhang, J. Association of built environment attributes with the spread of COVID-19 at its initial stage in China. Sustain. Cities Soc. 2021, 67, 102752. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health, Singapore. Additional precautionary measures to protect our seniors. Available online: https://www.moh.gov.sg/news-highlights/details/additional-precautionary-measures-to-protect-our-seniors (accessed on 20 May 2020).
- Li, Y.; Qian, H.; Hang, J.; Chen, X.; Hong, L.; Liang, P.; Li, J.; Xiao, S.; Wei, J.; Liu, L.; et al. Evidence for probable aerosol transmission of SARS-CoV-2 in a poorly ventilated restaurant. medRxiv 2020. [Google Scholar] [CrossRef] [Green Version]
- Mamode Khan, N.; Bakouch, H.S.; Soobhug, A.D.; Scotto, M.G. Insights on the trend of the Novel Coronavirus 2019 series in some Small Island Developing States: A Thinning-based Modelling Approach. Alex. Eng. J. 2021, 60, 2535–2550. [Google Scholar] [CrossRef]
- Roques, L.; Bonnefon, O.; Baudrot, V.; Soubeyrand, S.; Berestycki, H. A parsimonious approach for spatial transmission and heterogeneity in the COVID-19 propagation. R. Soc. Open Sci. 2020, 7, 201382. [Google Scholar] [CrossRef]
- Yeoh, E.K.; Chong, K.C.; Chiew, C.J.; Lee, V.J.; Ng, C.W.; Hashimoto, H.; Kwon, S.; Wang, W.; Chau, N.N.S.; Yam, C.H.K.; et al. Assessing the impact of non-pharmaceutical interventions on the transmissibility and severity of COVID-19 during the first five months in the Western Pacific Region. One Health 2021, 12, 100213. [Google Scholar] [CrossRef]
- Fu, X.; Zhai, W. Examining the spatial and temporal relationship between social vulnerability and stay-at-home behaviors in New York City during the COVID-19 pandemic. Sustain. Cities Soc. 2021, 67, 102757. [Google Scholar] [CrossRef] [PubMed]

| Index | Phase A | Phase B | Phase C | Phase D | Phase E | Phase F |
|---|---|---|---|---|---|---|
| Moran’s I | −0.008 | 0.077 | −0.012 | 0.202 | 0.075 | −0.007 |
| p value | 0.454 | 0.018 | 0.430 | 0.001 | 0.026 | 0.359 |
| Z score | −0.109 | 2.924 | −0.335 | 6.470 | 2.586 | −0.157 |
| Patterns | Random | Clustered | Random | Clustered | Clustered | Random |
| Index | Phase A | Phase B | Phase C | ||
|---|---|---|---|---|---|
| Imported | Local | Imported | Local | Imported | |
| Moran’s I | −0.008 | 0.089 | −0.001 | −0.015 | −0.037 |
| p value | 0.413 | 0.004 | 0.363 | 0.347 | 0.128 |
| Z score | −0.124 | 3.667 | 0.067 | −0.533 | −1.075 |
| Patterns | Random | Clustered | Random | Random | Random |
| Variables | Phase A | Phase B | Phase C | Phase D | Phase E | Phase F |
|---|---|---|---|---|---|---|
| Elderly population (65+) density | 0.002 | 0.290 *** | −0.018 | −0.094 | −0.061 | 0.041 |
| Commercial land proportion | −0.127 | 0.088 | −0.172 | −0.034 | −0.026 | 0.139 |
| Business land proportion | −0.031 | 0.000 | 0.003 | 0.257 *** | 0.198 *** | 0.072 |
| Hospital density | −0.058 | −0.184 * | −0.007 | 0.064 | 0.007 | −0.314 *** |
| School density | −0.108 | 0.111 | 0.027 | −0.112 | −0.049 | 0.020 |
| Pharmacy density | −0.311 *** | −0.031 | 0.014 | −0.031 | −0.015 | 0.021 |
| Supermarket density | 0.409 *** | 0.114 | 0.005 | 0.217 ** | 0.134 | 0.058 |
| Hotel density | 0.055 | 0.118 | 0.624 *** | 0.010 | −0.008 | −0.200 ** |
| Eatery density | 0.270 ** | 0.165 | −0.072 | −0.016 | −0.039 | 0.317 *** |
| Park density | 0.008 | −0.016 | 0.127 * | 0.100 | 0.039 | 0.269 *** |
| Phases | OLS | MGWR | ||
|---|---|---|---|---|
| Adjusted R2 | AICc | Adjusted R2 | AICc | |
| A | 0.158 | 899.8 | 0.366 | 828.7 |
| B | 0.149 | 903.4 | 0.289 | 868.6 |
| C | 0.275 | 850.3 | 0.651 | 635.4 |
| D | 0.085 | 927.5 | 0.261 | 871.1 |
| E | 0.030 | 946.9 | 0.076 | 939.5 |
| F | 0.190 | 887.0 | 0.512 | 742.9 |
| Variables | Phase A | Phase B | Phase C | Phase D | Phase E | Phase F |
|---|---|---|---|---|---|---|
| Elderly population (65+) density | 2.34 (7) | 37.45 (1) | 0.47 (7) | 10.55 (4) | 9.3 (2) | 1.28 (8) |
| Commercial land proportion | 2.49 (6) | 5.17 (6) | 12.07 (2) | 0.44 (10) | 1.01 (9) | 6.77 (5) |
| Business land proportion | 0.81 (9) | 2.81 (8) | 0.45 (8) | 55.98 (1) | 64.23 (1) | 1.26 (9) |
| Hospital density | 4.75 (4) | 4.96 (7) | 1.68 (4) | 1.36 (7) | 3.21 (5) | 11.4 (3) |
| School density | 2.5 (5) | 16.29 (2) | 0.33 (9) | 12.04 (3) | 8.38 (4) | 0.63 (10) |
| Pharmacy density | 12.01 (3) | 2.19 (9) | 0.51 (6) | 1.73 (6) | 1.55 (6) | 8.74 (4) |
| Supermarket density | 52.46 (1) | 13.96 (3) | 0.2 (10) | 13.79 (2) | 9.14 (3) | 5.01 (7) |
| Hotel density | 1.37 (8) | 11.06 (4) | 77.86 (1) | 0.53 (9) | 1.03 (8) | 5.91 (6) |
| Eatery density | 20.47 (2) | 5.33 (5) | 1.44 (5) | 1.04 (8) | 1.24 (7) | 19.2 (2) |
| Park density | 0.8 (10) | 0.77 (10) | 4.97 (3) | 2.54 (5) | 0.91 (10) | 39.78 (1) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ma, J.; Zhu, H.; Li, P.; Liu, C.; Li, F.; Luo, Z.; Zhang, M.; Li, L. Spatial Patterns of the Spread of COVID-19 in Singapore and the Influencing Factors. ISPRS Int. J. Geo-Inf. 2022, 11, 152. https://doi.org/10.3390/ijgi11030152
Ma J, Zhu H, Li P, Liu C, Li F, Luo Z, Zhang M, Li L. Spatial Patterns of the Spread of COVID-19 in Singapore and the Influencing Factors. ISPRS International Journal of Geo-Information. 2022; 11(3):152. https://doi.org/10.3390/ijgi11030152
Chicago/Turabian StyleMa, Jianfang, Haihong Zhu, Peng Li, Chengcheng Liu, Feng Li, Zhenwei Luo, Meihui Zhang, and Lin Li. 2022. "Spatial Patterns of the Spread of COVID-19 in Singapore and the Influencing Factors" ISPRS International Journal of Geo-Information 11, no. 3: 152. https://doi.org/10.3390/ijgi11030152
APA StyleMa, J., Zhu, H., Li, P., Liu, C., Li, F., Luo, Z., Zhang, M., & Li, L. (2022). Spatial Patterns of the Spread of COVID-19 in Singapore and the Influencing Factors. ISPRS International Journal of Geo-Information, 11(3), 152. https://doi.org/10.3390/ijgi11030152







