3.2.1. Performance of OLS, SLM, SEM, and MGWR
Table 5 shows the coefficients of the health, socioeconomic, demographic, and environmental factors derived from the OLS, SLM, SEM, and MGWR models, respectively.
Table 6 shows their performances. Note, the adjusted
R-squared value and AICc were not reported by
GeoDa for both SLM and SEM, and
ArcGIS Pro did not report the Breusch–Pagan test and AIC for MGWR.
The adjusted
R-squared value is highest for 2020 MAM (0.68), indicating our selected independent variables could explain 68% of the variation in the COVID-19 incidence rate in the OLS model, whereas the OLS model performed the worst for 2021 MAM, and the selected variables only could explain 17% of the variation in the COVID-19 incidence rate. This is confirmed by the AICc values, ranging from 148.21 for 2020 MAM to 205.36 for 2021 MAM (
Table 6). Nevertheless, all OLS models are statistically significant at the 5% level, indicating the reliability of the models.
The Moran’s
I values of the OLS residuals for 2020 SON, 2020 DJF, 2021 JJA, and 2021 SON are statistically significant (
Table 6) at the 10% level, indicating that there is spatial autocorrelation in the residuals. This highlights that the OLS approach is not the best approach for modeling the COVID-19 incidence rate in these seasons. Spatial autocorrelation regression modeling (i.e., SLM and SEM) is necessary to improve the performance. Compared to the OLS models, the
R-squared values for 2020 SON, 2020 DJF, 2021 JJA, and 2021 SON increase from 0.37 to 0.50 (0.49), 0.40 to 0.43 (0.43), 0.45 to 0.52 (0.53), and 0.62 to 0.67 (0.64) for SLM (SEM), respectively. Correspondingly, the AIC values of the OLS models for 2020 SON, 2020 DJF, 2021 JJA, and 2021 SON reduce from 188.06 to 177.44 (178.17), 184.59 to 183.99 (181.93), 186.19 to 181.28 (178.58), 159.10 to 152.43 (156.61) for SLM (SEM), respectively. Moreover, the Moran’s
I values derived from SLM and SEM for those seasons are statistically insignificant (
Table 6). All this indicates the effectiveness of SLM and SEM. For 2020 SON and 2021 SON, SLM performs a little better compared to SEM (
Table 6). This is consistent with the results of the LM-lag and LM-error tests, which denot that the LM-lag and robust LM-lag tests are statistically significant for 2020 SON and 2021 SON, while the LM-error test and robust LM-error test are insignificant for 2020 SON and 2021 SON, respectively (
Table A3). This implies that the SLM is more appropriate for these two seasons, although their differences are minor (
Table 5 and
Table 6).
For the residuals without spatial autocorrelation (i.e., 2020 MAM, 2020 JJA, 2021 MAM, and 2021 DJF), we also built the SLM and SEM for comparison purposes. As expected, the performances of the SLM and SEM and OLS are similar (
Table 6). Consistently, the coefficients for different factors also show similar values (
Table 5).
The Breusch–Panga tests indicate that there is spatial heterogeneity in the residuals of the OLS models for 2020 MAM, 2020 JJA, and 2020 SON (
Table 6). It is necessary to develop MGWR for these seasons. We also still built the models for 2020 DJF, 2021 MAM, 2021 JJA, 2021 SON, and 2021 DJF for comparison purposes and being consistent with the other seasons. The highest local condition number of all the models is 13.5, much smaller than 30, indicating the absence of multicollinearity in the local models. As expected, the adjusted
R-squared values of the MGWR models for 2020 MAM (0.77), 2020 JJA (0.57), and 2020 SON (0.52) are higher than that of the OLS models (adjusted
R-squared = 0.68, 0.52, and 0.34, respectively). Consistently, the AICc values of the MGWR models (128.01, 167.50, and 172.64) are lower than that of the OLS models (148.21, 169.62, and 191.29) over the three seasons (
Table 6). Although the residuals of the OLS models for the seasons of 2020 DJF, 2021 JJA, 2021 SON, and 2021 DJF do not have spatial heterogeneity, there are varying bandwidths for the independent variables (
Table A4), which may improve the performance of MGWR. However, the adjusted
R-squared value (0.16) and AICc (206.05) for 2021 MAM of the MGWR model are found to be similar to the OLS model in the same season (adjusted
R-squared = 0.17 and AICc = 205.36) (
Table 6). This is within our expectations, as the residuals of the OLS model for the season are randomly distributed, and the bandwidths are all global values for all independent variables (
Table A4).
Collectively, the MGWR models outperform OLS, SLM, and SLM (
Table 6). The coefficients for each independent variable for each season have consistent signs for all models (
Table 5), and the magnitudes of the coefficients for most of the OLS, SLM, and SEM models are within the range of the MGWR models (
Table 5). Thus, in the following discussion, we focus on the MGWR results.
Figure 4 shows the local
R-squared values of the MGWR models for each county in each season. Some counties in some seasons have low
R-squared values (e.g.,
R-squared value <0.2 in Benton County in 2020 SON) (
Figure 4c). Interestingly, the relatively poor performances of the MGWR models dominate in 2021 MAM (
Figure 4e). This may denote that other explanatory variables (e.g., running water [
21]) need to be considered in those regions during 2021 MAM. Nevertheless, in most counties and seasons, the local
R-squared values of the MGWR models are larger than 0.5 (
Figure 4), indicating that our models could capture more than 50% of the variability in the standardized COVID-19 case rate. This implies the relative reliability of MGWR in modeling the COVID-19 rate.
3.2.2. Associations of COVID-19 with Health Factors
Figure 5,
Figure 6,
Figure 7 and
Figure 8 present the spatiotemporal impacts of different health, socioeconomic, demographic, and environmental variables on COVID-19 at the Arkansas county level during all seasons from 2020 to 2021. In general, the associations of the variables from the four categories with COVID-19 vary across space and time.
The associations of poor health with COVID-19 are insignificant at the 5% level in most of the counties in Arkansas in the summer of 2021, excepting a few counties in Northern Arkansas, with coefficients ranging from −0.72 to −0.36 (
Figure 5a). The significant negative impacts of poor health on COVID-19 may be attributed to people’s preferences to stay at home given the fear of COVID-19 [
66], thus reducing the risk of exposure. This may also be the potential reason for the significantly negative associations (coefficients ranging from −0.54 to −0.18) of mental distress with COVID-19 during spring 2020 (
Figure 5f).
Adult obesity has significantly positive associations with COVID-19 in all counties during spring 2020, with the highest coefficients (0.36–0.54) in Chicot County (
Figure 5b), indicating that people with obesity are vulnerable to COVID-19. Such positive associations persist during fall 2020; however, the effects are not statistically significant at the 5% level (
Figure 5c). This finding is consistent with previous studies [
67]. Mohammad et al. [
68] stated that obesity could weaken the immune system and, therefore, make the host vulnerable to infectious diseases such as COVID-19. Further, Sawadogo et al. [
69] demonstrated that people with obesity were at increased risk of both COVID-19-related hospitalizations and death.
The access to exercise shows both significantly negative (coefficients from −0.54 to −0.18) and positive (coefficients from 0.0 to 0.36) associations with COVID-19 during spring 2020 (
Figure 5d) and summer 2021 (
Figure 5e), respectively. Regular exercise has been shown to improve human immune regulation [
70], which may reduce the risk of COVID-19 infection. Yet, exercising may increase the risk of exposure to the virus, especially without social distancing [
71]. Arkansas has reopened gyms and fitness centers since 4 May 2020 [
72]. As such, people may resume their exercise routines in gyms or fitness centers, which may increase exposure to COVID-19 in a confined environment. However, during the summer, people prefer to exercise outdoors, increasing their contact distance and thus reducing the possibility of COVID-19 infection.
Diabetes shows positive associations with COVID-19 in all counties for winter 2020 (
Figure 5i), summer 2021 (
Figure 5j), and fall 2021 (
Figure 5k), with coefficients ranging from 0 to 0.54, although some counties in Southern Arkansas have insignificant associations (
Figure 5i,k)). This is in line with Leon-Abarca et al. [
73], who claimed that people with diabetes had a higher probability of being infected after analyzing the cases of more than 1 million Mexican patients. In addition, the positive impacts of diabetes on COVID-19 show spatial variations, with the strongest impacts in Northeastern Arkansas during the winter of 2020 (
Figure 5i), while the reason is not clear. Complicating this finding is that diabetes significantly negatively associates with COVID-19 in the eastern part of Arkansas during the summer in 2020 (
Figure 5h), with the effects decreasing from the southeastern part (coefficients ranging from −0.72 to −0.54) to northwestern part (coefficients ranging from −0.36 to −0.18). The reasons for the significantly negative associations remain unclear. It may be related to the drugs used by some Type 2 diabetics, as Nyland et al. [
74] identified that glucagon-like peptide-1 receptor (GLP-1R) agonists, which have anti-inflammatory effects, were associated with reductions in COVID-19 complications. The stronger negative effects in the southeastern part are probably related to the relatively higher number of people receiving diabetes treatment in this region [
75].
As expected, the % of persons with at least one dose shows significantly negative associations with COVID-19 in Eastern Arkansas during fall 2021 (
Figure 5m), with coefficients ranging from −0.18 to 0. Moghadas et al. [
76] found that vaccination reduced the overall COVID-19 attack rate from 9.0% (without vaccination) to 4.5%. However, vaccination does not always perform as an effective prevention for COVID-19, as stated in Brüssow and Zuber [
77]. The % of persons with at least one dose, % of 18+ persons with at least one dose, and % of 65+ persons with at least one dose have significantly positive relationships with COVID-19 during the winter 2020 and 2021 and summer 2021 (
Figure 5n–p). This may be due to the fact that people with vaccinations are more likely to break social distances and reduce their willingness to stay at home [
78]. Such a reason may also explain the significantly positive associations of masks with COVID-19 during summer 2021 in most Arkansas counties (
Figure 5l). The contrasting effects of the % of persons with at least one dose on COVID-19 during fall 2021 (
Figure 5m) and winter 2021 (
Figure 5n) may be because of changes in people’s perceptions. COVID-19 in fall 2021 was at a low level in Arkansas, which may have led people to change their perception of COVID-19 from severe to weak. Therefore, people may lose their COVID-19 practices (e.g., keeping social distance), resulting in increased infections. There is a spatial variation of the impacts of the % of 18+ persons with at least one dose on COVID-19, with the largest magnitudes in Southern Arkansas, followed by Central Arkansas, in the winter 2020 (
Figure 5o). Such variations may be related to the requirement of wearing masks in several universities in Central Arkansas.
Figure 5.
Spatial impacts of health variables on the COVID-19 rate derived from a multiscale geographically weighted regression model in each county in Arkansas, US from 2020 to 2021. The unhatched regions indicate a 5% significance level. (MAM: March–April–May; JJA: June–July–August; SON: September–October–November; DJF: December–January–February).
Figure 5.
Spatial impacts of health variables on the COVID-19 rate derived from a multiscale geographically weighted regression model in each county in Arkansas, US from 2020 to 2021. The unhatched regions indicate a 5% significance level. (MAM: March–April–May; JJA: June–July–August; SON: September–October–November; DJF: December–January–February).
3.2.3. Associations of COVID-19 with Socioeconomic Factors
The coefficients of children in poverty with COVID-19 range from 0 to 0.40 in the summer 2020 (
Figure 6b) and from 0.40 to 0.80 in the fall 2021 (
Figure 6c). Children living in poverty are more likely to experience poor nutrition and live in overcrowded and damp housing and are less likely to have access to green spaces for exercise and less likely to be vaccinated [
79]. Thus, they are more vulnerable to catching infectious diseases such as COVID-19.
Consistent with previous studies, income inequality has divergent influences on COVID-19. It has significantly negative effects on the COVID-19 levels in all counties during the spring 2020 (
Figure 6d), with the magnitudes ranging from -0.40 to 0, but significantly positive effects (coefficients ranging from 0 to 0.80) on the COVID-19 levels in Eastern Arkansas during the summer 2020 (
Figure 6e). Gong and Zhao [
80] found that richer people were more mobile and more easily exposed to infection, bringing the virus into their neighborhoods. Oppositely, Demenech et al. [
81] found that COVID-19 incidence and mortality increased more pronouncedly among those with greater economic inequality in Brazilian Federative Units. The different signs of impacts of income inequality on COVID-19 may be due to the fact that richer people are more able to work remotely after recognizing the severity of COVID-19, while poorer people, such as the farmers in Eastern Arkansas, have to go outside to make money [
1]. This leads to increased COVID-19 infections.
Unlike Ahmad et al. (2020), who found that poor housing conditions induced higher COVID-19 incidence [
82], our results show that inadequate facilities significantly negatively affects the COVID-19 levels in most of the counties in Arkansas during the fall 2021 (
Figure 6f). This is probably related to the behavior change that households without a kitchen may directly order ready-to-eat food without visiting the grocery stores because of the fear of COVID-19 [
83], thus reducing the infection risk.
In general, the % of persons in group quarters has a significantly positive relationship with the COVID-19 levels (
Figure 6g–i), with coefficients ranging from 1.20 to 1.60 in Northern-Central Arkansas during the fall 2020 (
Figure 6i) to 0 to 0.40 in all of Arkansas during the summer 2020 (
Figure 6h). People living in group quarters (e.g., nursing homes, homeless shelters, dormitories, and prisons) usually share space and facilities (e.g., bathrooms). Thus, such positive relationships are anticipated, as the COVID-19 virus spreads mainly between people who are in close contact with each other [
84]. The impacts of the % of persons in group quarters on COVID-19 are strongest in Southern Arkansas, followed by the northern and western parts in the spring 2020 (
Figure 6g), while the strongest impacts show in Northern-Central Arkansas, followed by the central and southern parts in the fall 2020 (
Figure 6i). These variations may be related to interactions with other factors (
Table 5), which needs to be further examined.
Surprisingly, we found negative associations of being unemployment (
Figure 6a) with COVID-19 levels. One possible reason is that unemployment people are unlikely to test for COVID-19 given their financial burdens [
85], leading to many unreported cases among these groups.
Figure 6.
Spatial impacts of the socioeconomic variables on the COVID-19 rate derived from the multiscale geographically weighted regression model on COVID-19 in each county in Arkansas, US from 2020 to 2021. The unhatched regions indicate a 5% significance level. (MAM: March–April–May; JJA: June–July–August; SON: September–October–November; DJF: December–January–February).
Figure 6.
Spatial impacts of the socioeconomic variables on the COVID-19 rate derived from the multiscale geographically weighted regression model on COVID-19 in each county in Arkansas, US from 2020 to 2021. The unhatched regions indicate a 5% significance level. (MAM: March–April–May; JJA: June–July–August; SON: September–October–November; DJF: December–January–February).
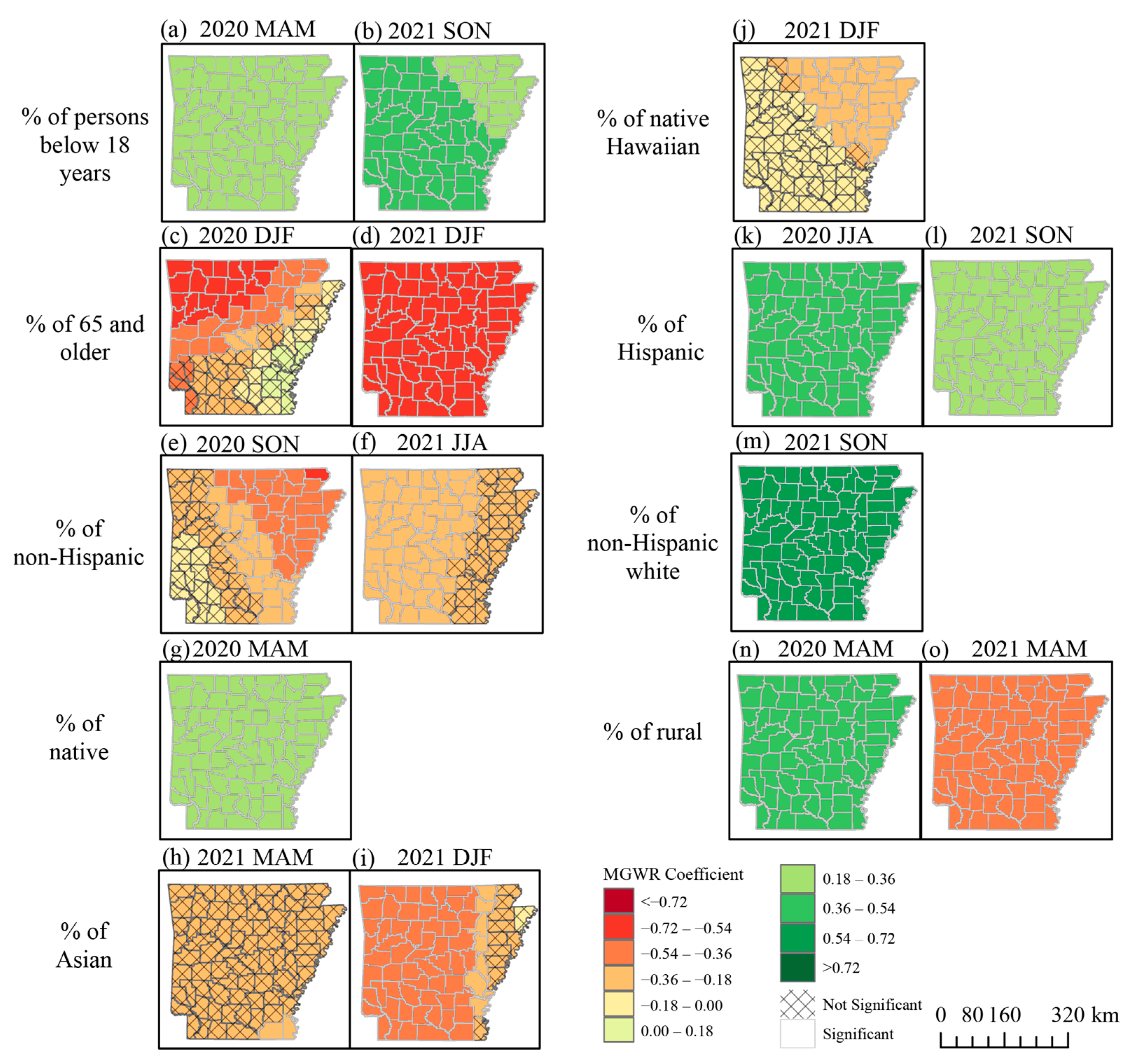
3.2.4. Associations of COVID-19 with Demographic Factors
For demographic impacts, there are significantly positive relationships of the % of persons below 18 years (
Figure 7a,b), % of native (
Figure 7g), % of Hispanic (
Figure 7k,l), and % of non-Hispanic White (
Figure 7m) with COVID-19 in all counties in Arkansas during different seasons, with coefficients ranging from 0.18 to 0.72. These findings are consistent with previous research. According to the CDC [
86], older teens, ages 16 and 17, face the highest rate of weekly cases. This is reinforced by Rumain et al. [
87], who concluded that the prevalence of COVID-19 for adolescents (10–19) was significantly greater than that for older adults. McLernon [
88] reported that COVID-19 cases, mortality, and case fatality incidences were 2.2, 3.8, and 1.7 times higher for Native Americans compared with White people in Montana. Further, Weeks [
89] stated that the American Indian and Alaska Native communities have been experiencing some of the highest rates of COVID-19 in the United States based on the maps generated by The John’s Hopkins Coronavirus Resource Center. As Hispanics or Latinos are heavily represented in the service industry, they were 1.5 times more likely to contact COVID-19 than their non-Hispanic White counterparts, as well as 1.9 times more likely to be hospitalized from COVID-19 and 1.8 times more likely to die from COVID-19 [
90]. The White population has a relatively low vaccination rate (only 50% of the population are fully vaccinated), leading to a high risk of COVID-19 [
91].
The % of 65 and older has a significantly negative impact on the COVID-19 levels during the winter 2020 and 2021 (
Figure 7c,d), with coefficients ranging from −0.72 to −0.18. Due to the severe illness of COVID-19 in older people, the CDC has suggested giving the top priority to more senior people to get the vaccine [
92]. As such, more than 95% of 65 to 74 years old people in the U.S. received at least one dose of the vaccine [
91], which thereby may reduce the total COVID-19 burden. In addition, the % of 65 and older shows the strongest negative impacts in Northwestern Arkansas, followed by a belt stretching from the northeastern to southwestern parts in the winter 2020 (
Figure 7c). Such variations need to be further explored.
Unlike Native Americans and Hispanics, the % of Asians and % of Native Hawaiians show significantly negative relationships with the COVID-19 levels in Southeastern Arkansas in the spring 2021 (
Figure 7h) and Western and Northeastern Arkansas in the winter 2021 (
Figure 7i,j). The magnitudes of the relationships range from −0.54 to −0.18. Asians and Native Hawaiian/Pacific Islanders has high vaccination rates. The vaccination may provide some protection for them from COVID-19 [
91].
The % of rural parts has both significantly positive (coefficients ranging from 0.36 to 0.54) and negative (coefficients ranging from −0.54 to −0.36) associations with COVID-19 during the spring 2020 (
Figure 7n) and spring 2021 (
Figure 7o), respectively. The rural area populations tend to be older, sicker, heavier, poorer, and less vaccinated and have experienced higher COVID-19 incidence and mortality rates [
93]. Meanwhile, the population density in rural areas is lower compared to metropolitan areas [
94], leading to a reduction in COVID-19 transmission. The different signs of impacts are presumably due to the fact that after getting vaccination and a better education, people in rural areas with a lower population density and more open space are less likely to be infected by COVID-19.
As for the impacts of unemployment impacts on COVID-19, the negative influences of the % of non-Hispanic Blacks on COVID-19 (
Figure 7e,f) are presumably because of the hidden COVID-19 cases caused by the inability to test for it, which need to be further explored.
Figure 7.
Spatial impacts of demographic variables on the COVID-19 rate derived from a multiscale geographically weighted regression model on COVID-19 in each county in Arkansas, US from 2020 to 2021. The unhatched regions indicate a 5% significance level. (MAM: March–April–May; JJA: June–July–August; SON: September–October–November; DJF: December–January–February).
Figure 7.
Spatial impacts of demographic variables on the COVID-19 rate derived from a multiscale geographically weighted regression model on COVID-19 in each county in Arkansas, US from 2020 to 2021. The unhatched regions indicate a 5% significance level. (MAM: March–April–May; JJA: June–July–August; SON: September–October–November; DJF: December–January–February).
3.2.5. Associations of COVID-19 with Climate Factors
Air pollution has significantly negative effects on COVID-19 in all of Arkansas during the spring 2020 (
Figure 8a). This supports the previous study that COVID-19 cases were reduced when the amount of PM
2.5 was above the threshold level, as a higher concentration of PM
2.5 may restrict human mobility [
95].
The humidity consistently shows significantly negative effects on the COVID-19 levels in Arkansas during the spring 2020 (
Figure 8b), summer 2021 (
Figure 8d), fall 2021 (
Figure 8e), and winter 2021 (
Figure 8f). The effects are the strongest in Northeastern Arkansas during the fall 2021, with coefficients ranging from −0.54 to −0.36. These negative effects have been documented by existing studies. For instance, Ward et al. [
96] found that a reduction in the relative humidity of 1% was predicted to be associated with an increase of COVID-19 cases by ~6% in New South Wales, Australia. By reviewing 517 articles, Mecenas et al. [
97] concluded that a wet climate appeared to reduce the spread of COVID-19. The impacts of humidity on COVID-19 in the fall 2021 show spatial variations, with the largest magnitudes in Northeastern Arkansas, followed by a belt stretching from the northwestern to southeastern parts (
Figure 8e).
The temperature significantly positively influenced the COVID-19 levels (
Figure 8g) in Arkansas during the spring of 2020. Menebo et al. [
16] stated that people were more prone to outdoor activities when the sun was shining outside and so eventually became exposed to the virus.
The wind also shows significantly positive impacts on COVID-19 during the fall 2020 (
Figure 8h). A high wind speed likely circulated any suspended respiratory droplets in the air and thereby increased the possibility of inhalation by people. The impacts of wind on COVID-19 gradually decrease from Northeastern Arkansas to Southwestern Arkansas (
Figure 8h), which is possibly because of the mountainous terrain in Western Arkansas (
Figure 1) that blocks the wind to circulate the droplets.
Figure 8.
Spatial impacts of climate variables on the COVID-19 rate derived from a geographically weighted regression model on COVID-19 in each county in Arkansas, US from 2020 to 2021. The unhatched regions indicate a 5% significance level. (MAM: March–April–May; JJA: June–July–August; SON: September–October–November; DJF: December–January–February).
Figure 8.
Spatial impacts of climate variables on the COVID-19 rate derived from a geographically weighted regression model on COVID-19 in each county in Arkansas, US from 2020 to 2021. The unhatched regions indicate a 5% significance level. (MAM: March–April–May; JJA: June–July–August; SON: September–October–November; DJF: December–January–February).
In summary, different factors contribute to COVID-19 transmission across time. This may be because different variables were involved in the MGWR models in different seasons. For instance, during the spring season in 2020, there were 11 factors from four categories contributing to the COVID-19 rate variation, while, in spring 2021, only two factors from two categories explained the COVID-19 rate variation. Along with different COVID-19 variants (i.e., early variants in winter 2020, Delta in summer 2021, and Omicron in winter 2021), the contributions of driving factors are different. Only diabetes shows consistently positive roles in the spread of both early COVID-19 variants and Delta, while humidity plays consistently negative roles in the spread of both Delta and Omicron.