Abstract
In developing countries, aging is rapid and new towns in suburban and rural districts are emerging. However, the spatial accessibility and equity of healthcare services for older adults in new towns is rarely examined. This study is among the earliest attempts to evaluate the spatial accessibility and equity of public hospitals for older adults, using data from Songjiang District, Shanghai, China. A modified Gaussian Huff-based three-step floating catchment area (GH3SFCA) method was adopted based on the real-time travel costs of public transit, driving, cycling, and walking. The Gini coefficient and Bivariate Moran’s Index were integrated to estimate spatial equity. The results showed that the spatial accessibility of high-tier hospitals decreases from the central areas to the outskirts for older adults in Songjiang. Meanwhile, the accessibility of low-tier hospitals varies substantially across areas. Although the low-tier hospitals are distributed evenly, their Gini coefficient showed less equitable spatial accessibility than the high-tier hospitals. Furthermore, driving and cycling lead to more equitable spatial accessibility than public transit or walking. Finally, communities with a low-supply–high-demand mismatch for public hospitals were suggested to be improved preferentially. These findings will facilitate planning strategies for public hospitals for older adults in developing new towns.
1. Introduction
As aging is becoming more rapid globally, around 20% of people are expected to be 60 years or older by 2050 [1]. In China, the population has aged significantly in recent decades, and it is expected to boom in the future [2,3,4]. By the end of 2023, the aging population in China reached 296 million, covering 21.1% of the general population. This percentage is expected to rise to 35.1% in 2050 [5]. By the end of 2021, older adults over 60 took up 36.3% of the total population in Shanghai, and the proportions were 25.9% for over age 65, 16.6% for over age 70, and 5.6% for over age 80. There is a constant and growing need for healthcare services in rural, suburban, and urban areas, particularly during population growth and aging [6,7]. Age-related chronic diseases, such as cancer, arthritis, heart disease, and stroke, are more likely to occur as people get older [8]. Accessibility to healthcare is recognized as essential to the general health and quality of life of older adults. Examining spatial variations in older adults’ access to public hospitals can help identify inequity and suggest resource allocation [9,10]. Spatial barriers for older adults to reach public hospitals result in their reduced satisfaction with disease-prevention services and lower utilization of public hospitals [11,12]. More significantly, compared to their younger counterparts, older adults experience worsening inequities in healthcare access. They are more likely to have worse health conditions and fewer options for mobility, such as difficulty walking and reduced or stopped driving [13]. Equity in spatial accessibility has received growing attention among researchers, who are using spatial accessibility to evaluate inequity [14,15,16]. A study in India found that the utilization of public health facilities increased with age among older adults, but health-seeking behavior decreased with age among them [17]. In addition to enhancing spatial accessibility, planning and investments in public healthcare services should prioritize the needs of the dependent and vulnerable, such as older people and those with disabilities.
New towns in western industrialized countries were gradually brought under local government supervision in the mid–late 1980s, slowing planning and construction [18]. Conversely, with the acceleration of economic globalization, new towns are emerging in suburban and rural areas of developing countries. New town development became an important concept in Chinese urban planning at the beginning of the 21st century. Shanghai launched its new town project as early as 2000, and this project has since been replicated by other Chinese cities. In 2017, Shanghai planned to cultivate five new towns, including Songjiang, Jiading, Qingpu, Fengxian, and Nanhui, into comprehensive node towns with a radiation-driving role in the Yangtze River Delta urban agglomeration [19]. The new generation of new towns are more comprehensively planned in terms of land use profile and urban functions, focusing on not only economic development but also livability [20]. Today, more than 3800 new towns in China occupy nearly 30,000 km2 of land and provide shelters for about 150 million residents [21]. Before the media used the term “ghost cities” to describe new town developments with few residents, neither the public nor researchers paid much attention to the insufficient planning of new towns [22]. An important part of making these new towns more livable is to understand and improve the accessibility and equity of healthcare for their residents.
The concept of accessibility has evolved in many ways since it was brought up in 1959 [23]. Accessibility can, in short, be defined as the relative ease by which certain locations can be reached from other locations [24]. The accessibility of health services can be measured using the space between the population demand for and the available healthcare supply, which is influenced by the travel impedance in between [25,26]. According to earlier research, access and proximity are highly correlated with the use of healthcare services [27,28,29,30,31]. Therefore, policy making and urban planning are necessary to enable people access these services easily [32]. To that end, it is necessary to be able to assess the current state of the healthcare accessibly. An essential advantage of the accessibility approach is the analysis of spatial and social inequalities [33,34]. The value of the methods for spatial health research is becoming more and more recognized, with the ultimate goal to uncover social disparities in spatial access to healthcare [35,36]. Spatial accessibility to healthcare services is generally measured with GIS-based tools. It focuses on the role of spatial distances in the interactions between populations’ medical demands and healthcare supply [37,38]. Several methods have been applied to measure the spatial accessibility of healthcare services, with common methods including the two-step floating catchment area (2SFCA) method, potential model, and gravity model. The 2SFCA method is the most widely used in the evaluation of the spatial accessibility of public hospitals. It incorporates the interaction between supply, demand, and minimum cost into the measure of accessibility. This method has advantages in the equity measurement of medical resources [39].
The traditional 2SFCA accessibility measurement was improved from different aspects. In order to solve the defects of the dichotomous method of the 2SFCA method to deal with distance, many studies introduced the distance decay function in the original model, mainly in the form of exponential function [35], Gaussian function [40], and kernel density function [41]. As an extension of demand or supply competition, the enhanced 2SFCA method aims to include the distance decay effect into the original 2SFCA method by incorporating different weights for different time zones [42]. Considering the competition effect between facilities when multiple facilities exist within the search radius of a demand point, 3SFCA is proposed by adding a third step to the search including all demand points and facilities [43]. The Enhanced 3SFCA (E3SFCA) method proposed by Luo aims to overcome the problem of overestimation in the 2SFCA and E2SFCA methods [44,45]. As an extension of travel modes, Tao and Wang (2022) aimed to measure transportation-induced healthcare inequity by comparing the accessibility of hospitals under different transportation situations [46]. Xing and Ng (2022) adopted the modal accessibility gap (MAG) Index to reveal the spatial disparities in accessibility between the public transport and private car modes [47]. As for demand data in FCA methods, some researchers used detailed information on individual household addresses as medical demand points [48]. In other studies, due to statistical reasons, populations were aggregated to larger spatial units. The choice of data aggregation method is crucial in accessibility analyses, as different approaches can introduce spatial biases. Kowalski (2022) demonstrated the influence of population data aggregation methods on walking accessibility results, and suggested that reducing aggregated data to more precise levels can reduce aggregation errors [49].
Spatial accessibility is vital for older adults in seeking healthcare services in primary hospitals and specialty care [50,51]. Uneven spatial distribution of populations, healthcare facilities, and the transport system connecting them can cause many healthcare disparities [52]. Transportation policies are established to reduce spatial barriers for the aging population, such as public transit services, pedestrian environments, car or van rides, and social support [53,54,55,56,57]. For example, Zainab described the importance of public transit for older adults in Sydney to the greater usage of dental care [50]. Loo and Lam highlighted the importance of a walkable pedestrian environment around healthcare facilities in order to promote active aging [55].
An increasing number of studies have focused on the spatial equity of older adults’ access to healthcare services. Health policies need to include the supply of more accessible health services, especially for the aging population, who use healthcare facilities more frequently and intensively than other age groups [58,59]. Researchers found that there is an negative correlation between patients’ physical location (usually residential) and their use of healthcare services [60]. Tao and Cheng showed the uneven distribution of spatial accessibility to hospitals for older adults in Beijing, where the level of accessibility decreases significantly from the central area outwards. Their findings indicated that older adults were disadvantaged in the competition with their younger counterparts for healthcare services [61]. Spatial accessibility and inequity indices were used to evaluate disparities in senior community care services. The results suggested that policymakers should not only measure overall accessibility but also aim for a more equitable distribution [62]. Moreover, spatial accessibility can help to identify healthcare service shortage areas and inform the equitable allocation of resources [63].
Various approaches have been explored to measure equity in healthcare accessibility, with simple economic indicators and complicated spatial models. The Gini coefficient has been used in recent research to assess transport equity from a social justice perspective [15,48,64,65]. For instance, the spatial disparity between the population and physicians in Japan was analyzed using Lorenz curves and Gini coefficients [66]. The disparity in the geographical distribution of clinics in the metropolitan city of Daejeon, South Korea, was measured by hot-spot analysis [67]. The spatiotemporal disparity in public healthcare resources across China in the period of 2003–2015 was analyzed using Moran’s Index model and the dynamic spatial Durbin panel model [68].
However, there are still research gaps in the existing literature. Firstly, few studies have focused on new towns in developing countries. Compared with urban areas, the policies for new towns will boost population size in the future, causing low accessibility and equity with regard to healthcare facilities, especially for older adults [69]. Secondly, although accessibility-related equity studies are emerging, there is a lack of consideration of the hierarchical characteristics of hospitals. Hospitals of higher tiers could provide basic medical services like primary or specialty hospitals. Considering all medical facilities to be the same may result in a biased understanding of accessibility [48]. Thirdly, many previous accessibility studies estimated the actual travel time based on the grade and average speed of road sections, neglecting the impact of actual traffic conditions on the time cost. In morning peak hours, the travel time to publics hospitals would be longer, and it is natural for older adults to go to hospitals early to receive medical services sooner.
In view of the above research gaps, this study evaluates the spatial accessibility and equity of public hospitals for older adults in Songjiang District, Shanghai, China. The research objectives are as follows: (1) to adopt a modified Gaussian Huff-based three-step floating catchment area (GH3SFCA) method that focuses on measuring the spatial accessibility associated with public hospitals; (2) to explore the spatial inequity of public hospitals in Songjiang and identify the spatial disparity patterns for older adults; and (3) to identify the priority of the locations where older adult public hospital accessibility improvements are most needed in Songjiang.
The contributions of this study are three-fold. First, the modified GH3SFCA method adopted in this study incorporated the Gaussian distance decay function and Huff probability model, which are more linked to travel behaviors during public hospital trips and enhance the accuracy in calculating spatial accessibility and equity. Second, real-time travel time costs were obtained to reflect the actual situation at peak hour for four prevailing travel modes, making the results better suited for the circumstances compared to traditional road network analysis. Third, instead of choosing large administrative units (e.g., subdistricts or districts), this study employed small administrative units (i.e., communities and villages). This helps to discover fine-grained variability in the spatial accessibility and equity of public hospitals and derive targeted planning strategies in different communities.
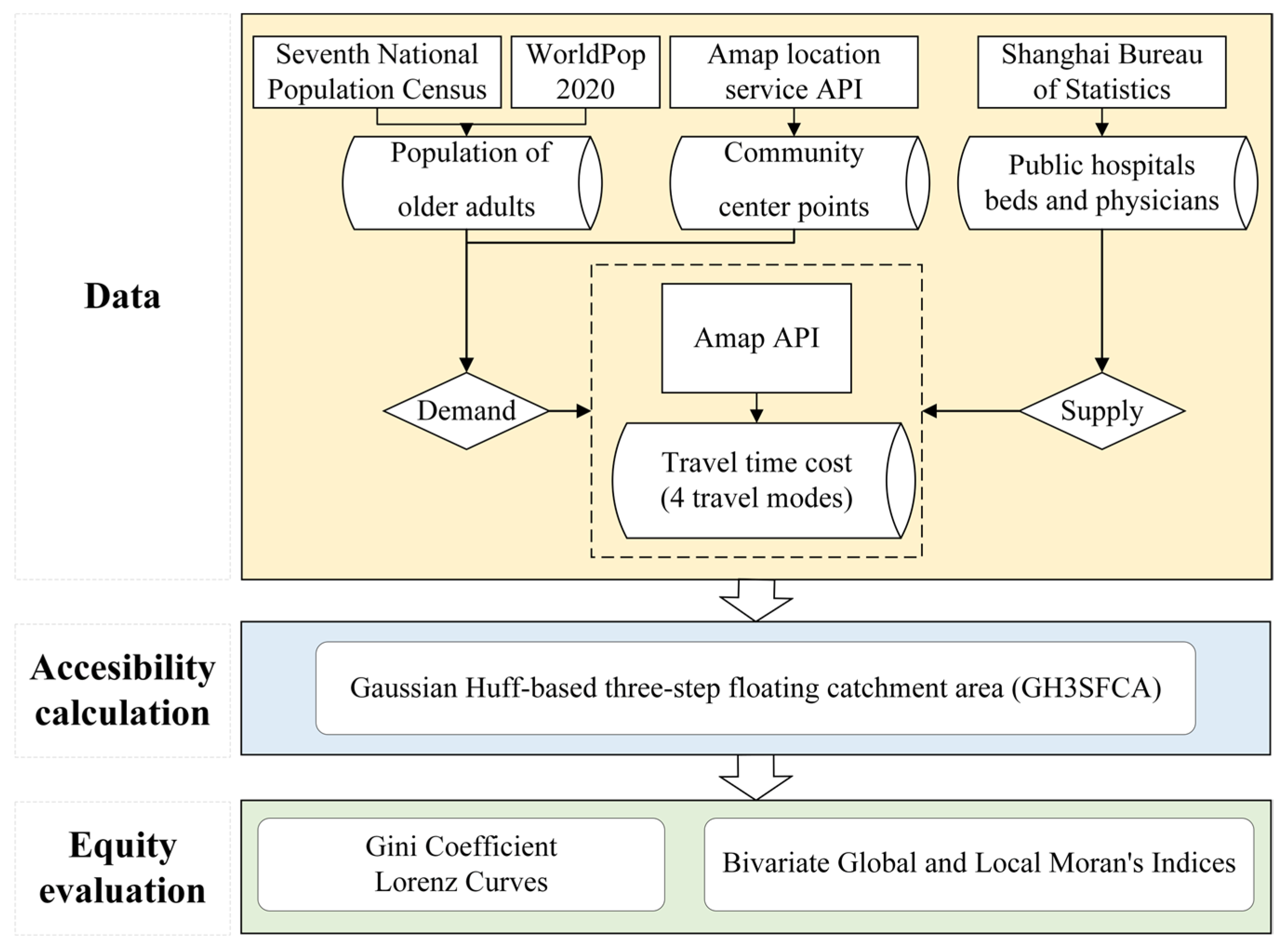
The research framework of this paper includes three parts (Figure 1). Firstly, we collect and preprocess data on the older population, public hospitals and travel time cost. Secondly, we adopted a modified GH3SFCA method and calculate accessibility with the supply (public hospitals) and demand (older population) data and travel time cost data. Finally, the spatial equity of the public hospitals is analyzed using a Lorenz curve, the Gini coefficient, and Bivariate global and local Moran’s Indices.
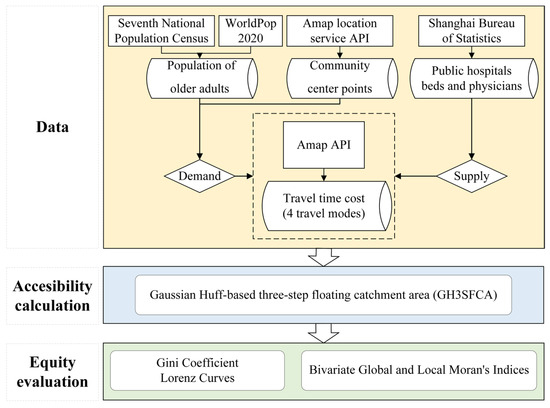
Figure 1.
Research framework.
2. Research Data
2.1. Study Area
In this research, we chose Songjiang District as the study area. In the 2001 Shanghai One City Nine Towns Planning, Songjiang became the one of the first new towns in Shanghai. As the experimental site for Shanghai’s new town project, Songjiang pioneered a new mode of outer suburban development and became the role model for other towns [69]. In 2000, the population of Songjiang was 0.64 million, and there were 18 hospitals with 2846 hospital beds and 3018 physicians. As the most populated new town in Shanghai, the population in Songjiang tripled to 1.9 million in 2021. Nevertheless, the number of hospitals only increased to 22 (+22%), with 3991 hospital beds (+40%) and 6318 physicians (+109%). Therefore, Songjiang would be a good case for studying the spatial accessibility and equity of healthcare services in developing countries’ new towns during rapid urbanization.
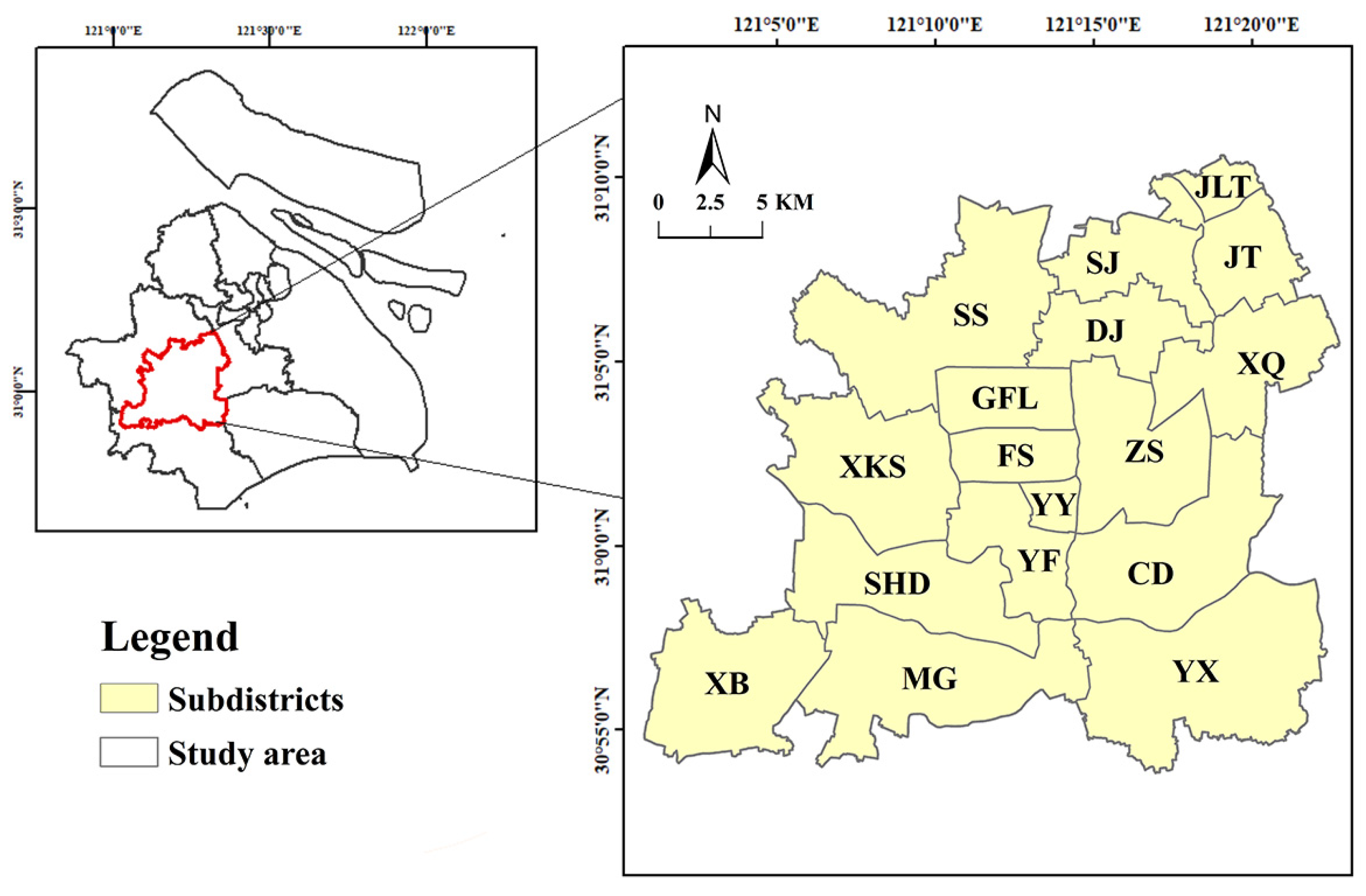
Songjiang is in the southwest of Shanghai, with a total area of 604.64 km2. The administrative division of Chinese cities has four levels: city–district (county, new towns)–subdistrict–community (village). There are 17 subdistricts in Songjiang, and a total of 356 communities (villages) under these subdistricts. The locations of the study area is shown in Figure 2.
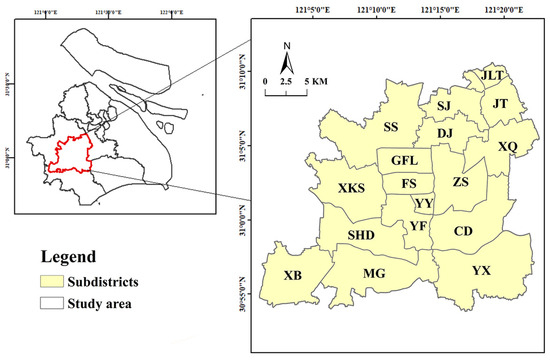
Figure 2.
Study area and spatial distribution of community centers.
2.2. Data
2.2.1. Public Hospitals
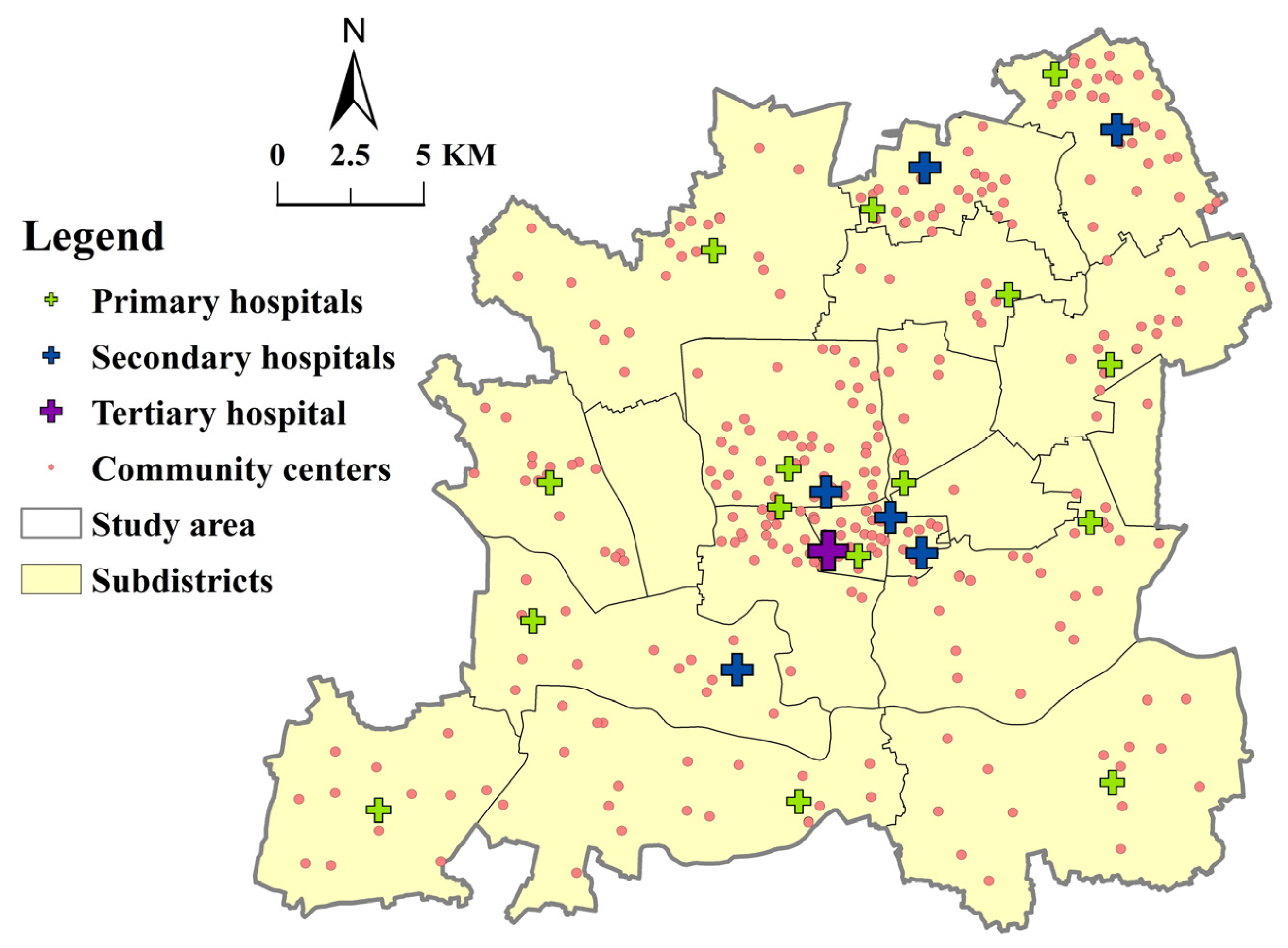
In China, hospitals are categorized into three tiers–primary, secondary, and tertiary–providing different qualities and types of services [70,71]. Primary hospitals in China provide diagnoses and treatments for common diseases and serve the basic public health needs of residents in adjacent communities. Secondary hospitals offer more services than primary ones and provide outpatient, emergency, and surgery services. Tertiary hospitals have the largest scale and are equipped with sufficient medical facilities and highly skilled staff to diagnose and treat difficult diseases. However, hospital services are not delivered through this multi-tier system in line with a gatekeeping and two-directional referral network [71,72]. High-tier (secondary and tertiary) hospitals also provide primary care, and residents have the freedom to access high-tier hospitals to receive first diagnosis and treatment services. They serve nearby residents and also attract those from a further distance. There are a total of 22 public hospitals in Songjiang: primary (15), secondary (6), and tertiary (1) (Table 1). The locations of public hospitals were obtained through the Amap location service API. The distribution of public hospitals and community centers is shown in Figure 3. Secondary and tertiary hospitals are more spatially aggregated in the center of Songjiang than primary hospitals.

Table 1.
Service capacity of different public hospitals in Songjiang (2021).
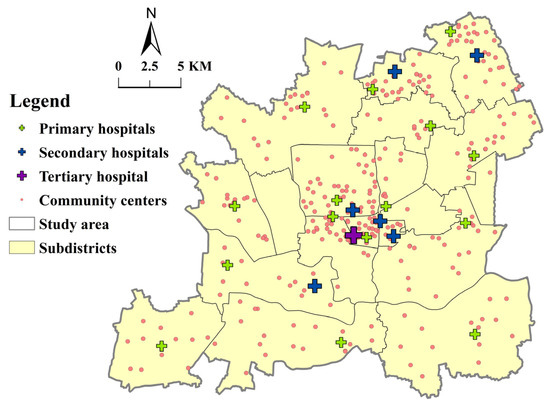
Figure 3.
The distribution of public hospitals and community centers.
In this study, we combined secondary and tertiary hospitals into one category, and primary hospitals formed another. There are two reasons for this: (1) primary hospitals are called community healthcare centers or clinics, while secondary and tertiary hospitals are general or specialized hospitals and overlap in their functions [73]; (2) there is only one tertiary hospital in the study area, which could not be analyzed because it lacked attraction competition in the FCA methods.
2.2.2. Older Population Distribution
In the Law of the PRC on the Protection of the Rights and Interests of Older Adults, citizens over 60 years of age are called older adults. According to the Seventh National Population Census in 2021, the aging population (60 and above) in Songjiang accounts for 302,000 people, 16% of the general population. In China, city administrative division has four levels: city–district (county, new towns)–subdistrict–community (village). Many current studies on the accessibility of medical facilities were conducted at the subdistrict level, taking the mass center of the subdistrict as the population demand point [74]. In this study, we set the 356 community administration centers (hereafter referred to as community centers) as the demand point for health services. We obtained the coordinates of all community centers through the Amap API service. Then, the entirety of Songjiang was divided into 306 community areas by the ArcGIS 10.7 Thiessen Polygons tool, based on the current 356 community centers. Some community centers were automatically merged by the ArcGIS Thiessen Polygons tool due to geographical proximity.
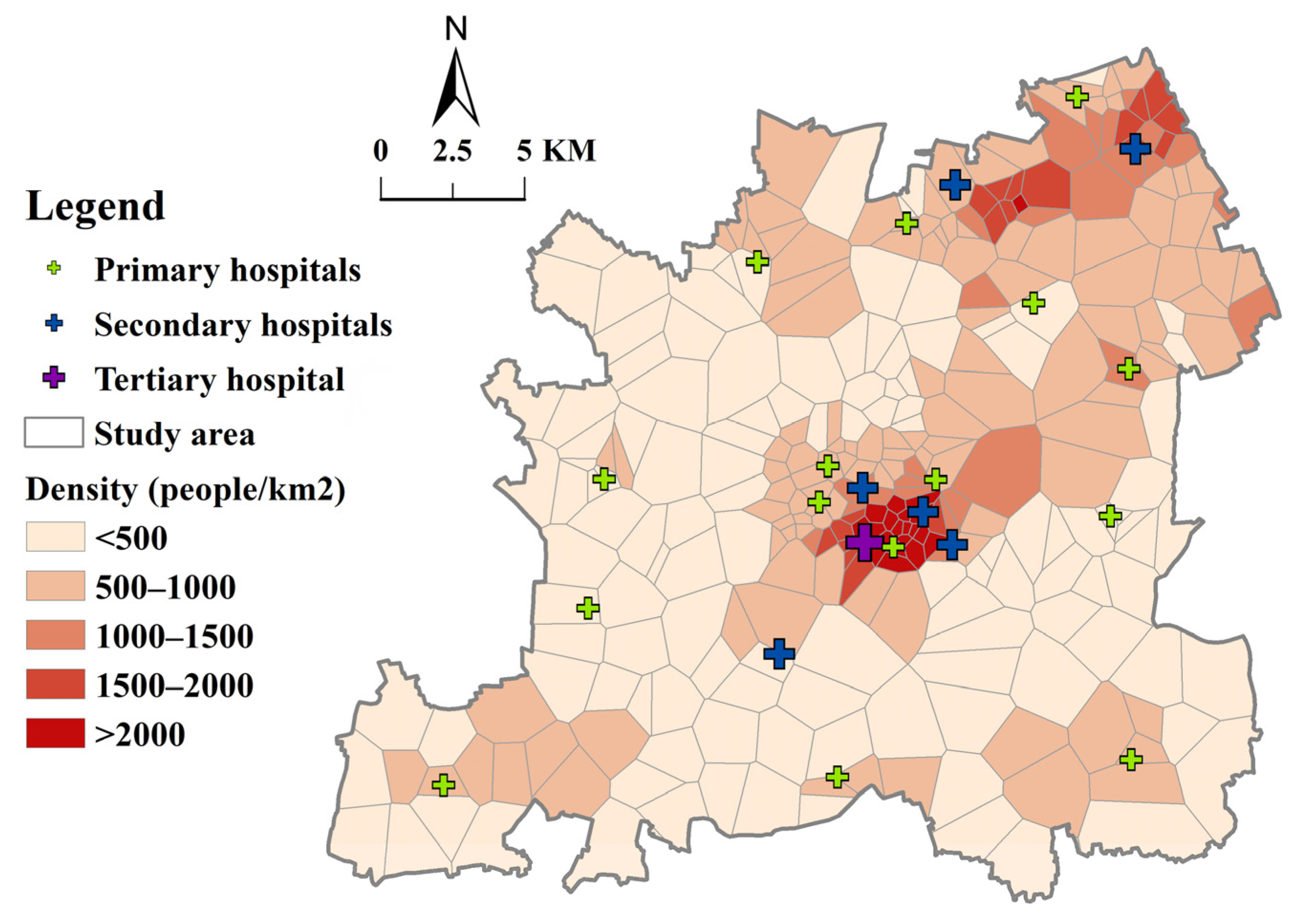
Firstly, we obtained a 100 m × 100 m resolution population raster dataset of China from the WorldPop website for the year 2020, and clipped the Songjiang raster data from it. Secondly, the WorldPop population raster data were divided into the community areas outlined above. We modified the population of each community under each subdistrict by proportion according to the population of the 17 subdistricts in the 2020 Seventh National Population Census in Songjiang District. The total population of Songjiang District in the raster data was adjusted from 1.4 m in WorldPop to 1.9 m in the Seventh National Census. Lastly, the proportion of the older population in each subdistrict in the Census was used to calculate the average of the older population raster data in each community. The population density of older people in Songjiang is shown in Figure 4. In terms of spatial distribution, the older population in Songjiang is densely represented in central and northeastern subdistricts (>1000 persons/km2). On the contrary, the population density of older people in most other subdistricts is lower than 500 persons/km2. The significant variation in the population density of older people (S.D. = 756 persons/km2) requires a sensible allocation of public hospitals.
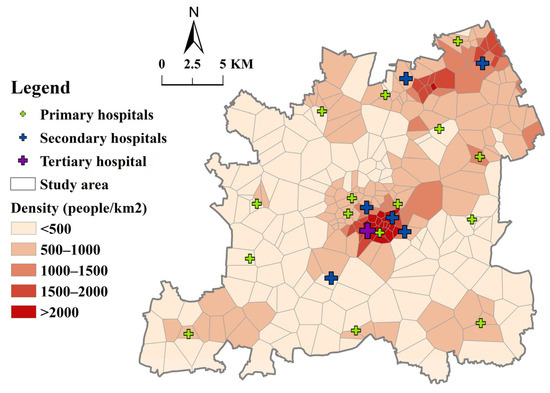
Figure 4.
Population density of older people of Songjiang District.
2.2.3. Travel Time Cost
Determining the threshold is an important part of floating catchment area analysis. A small threshold can polarize the distributional pattern, while a large one would flatten the geographical pattern and mask local clusters with high values [75]. Generally, different tiers of hospitals have different searching thresholds due to the varied service capacity and attraction to residents. Shanghai commenced 15 min life circle planning in 2014. One of the aims is to ensure access to community (or primary) hospitals within a 15 min walking or cycling distance [76]. Therefore, we set a 15 min time threshold for primary hospitals for walking or cycling. For driving, we set it at 15 min, and for public transit, to 30 min considering time loss due to waiting and transferring. Since secondary and tertiary hospitals have higher service capacities, the time threshold for walking was set at 30 min, which is the maximum walking endurance time [77]. Similarly, cycling, driving, and public transit for secondary and tertiary hospitals were set at 30, 30, and 45 min.
The peak hour is another key factor in understanding accessibility to public hospitals, and it was provided by hospitals in Songjiang. Our study focused on regular medical services and general departments in hospital medical services, and emergency services and emergency rooms were not taken into consideration. The service hour begins at 8 A.M. according to the public hospital appointment schedule for general medical departments. Public hospitals offer a number of appointments for one time period, and every patient appointed in a certain time period (say 8:00–9:00 A.M.) waits in line in order of arrival. The hospitals, especially secondary and tertiary, are often crowded in China, and patients tend to arrive early to reduce their waiting time [78]. The peak hour is around 8–9 A.M. for primary hospitals, and is between 7:30 and 8:30 A.M. for secondary and tertiary hospitals as residents arrive early to line up. Peak hour travel time data were obtained and averaged for weekdays during a week (4–8 December 2023) through the Amap API. Using 306 community centers as the origin and 22 public hospitals as the destination, we collected the actual travel time cost for four travel modes: public transit, driving, cycling, and walking.
According to our field research at Songjiang Central Hospital on 27 November 2023, patients would prefer electric bikes to bicycles to go to hospitals. This aligns with the finding that the preferred transportation mode of Chinese nonmotor vehicle users is shifting from bicycles to electric bikes [79]. Private electric bikes are commonly-used in China [80]. They can be accessed in the majority of cities and almost all suburban and rural areas. Field research in rural and suburban areas in China shows that, unless they have a critical illness, residents are willing to go to medical facilities by themselves or with their family members by electric bike. This is consistent with the travel options in rural and suburban areas of China, where the terrain is flat and travel distances are moderate [81]. There are also some studies about older riders of electric bikes [82]. Therefore, we considered travel time by electric bike to represent cycling.
The peak hour travel time was recorded as the passage of time from the community to the public hospital for a specific travel mode. The travel times in this study were provided directly by Amap and captured by us through an API. The estimated travel times were returned based on actual conditions, including traffic jams in driving and public transportation, as well as pedestrian crossings, overpasses, and the speed of travel modes. The time is based on a huge amount of actual travel data from users, of all age groups. However, the cycling (electric bikes) time of older adults, even with a family member driving, would be longer than that of younger adults [79]. Walking speed can also be expected to be reduced in adults of older age [83]. Therefore, we multiplied the cycling and walking times of older adults by factors of 1.15 and 1.3, respectively. A total of 306 × 22 × 4 travel time cost datapoints were obtained from Amap, and example data for walking mode are shown in Table 2.

Table 2.
Example of obtained travel time data from community to public hospital by walking (in seconds).
These results show that for all tiers of hospitals, driving and cycling have a lower mean travel time, followed by public transit. Notably, walking has an average travel time that is more than six times longer than that of driving (see Table 3).

Table 3.
Statistical characteristics of travel time cost (in minutes).
3. Methods
3.1. Evaluation of Spatial Accessibility
Since Luo and Wang developed the two-step floating catchment area (2SFCA) method to measure spatial access, it has been widely used [26,31,84]. It defines the service area of a healthcare provider by a threshold while accounting for the capability of the provider to satisfy its nearby demands. The calculation takes two steps, and is formulated as Equations (1) and (2).
where is the supply-to-demand ratio of facility ; is the capacity of facility ; is the population at location ; is the distance between and ; and is the threshold travel distance.
3.2. Gaussian Huff-Based Three-Step Floating Catchment Area Method (GH3SFCA)
In this study, a modified Gaussian Huff-based 3SFCA was adopted to evaluate the spatial accessibility of public hospitals for the older adults in each community area inside the study area with different travel modes. It consisted of the following three steps.
Step 1: The demand probability of each community was calculated with regard to every service provider, taking into account the supply competition. The Huff probability model can overcome the problems of both over- and under-estimating population demand and adopts a more comprehensive service competition scheme which includes both travel cost and service capacity [44]. The calculation made according to the Huff model [44] was as follows:
The demand probability for community seeking healthcare at hospital increases with the service capacity of hospital and decreases with distance according to the decay function applied. In this study, we use hospital beds as the service capacity indicator [74,85,86]. In the model, refers to the actual peak hour travel time from community to hospital , and is the travel time threshold. Furthermore, the demand probability depends on alternative health service providers and therefore is calculated in relation to the capacities and distances to all locations within the maximal relevant catchment expressed by the sum in the dominator. The maximal relevant catchment size is assessed individually with reference to each hospital’s type and travel modes.
In FCA methods, a distance weight is attributed to every subzone according to a distance decay function:
Various functions have been used so far: the Gaussian function, gravity function, exponential function, inverse power function, or logistic-based function [87].We adopted the widely used Gaussian Function as the decay function, as it tends to choose the nearest destination points [88]. In case studies of healthcare accessibility, especially by low-speed travel modes, the Gaussian decay function would be more appropriate in choosing the closest services [49]. The Gaussian decay function is as follows:
Step 2: The Huff probability was calculated in step 1, and a supply ratio was determined for each hospital as follows:
The supply ratio is given by the service capacity of hospital divided by the sum of population of all communities within the maximum catchment size multiplied by their probability of seeking service from hospital .
The second step of the GH3SFCA incorporates the strengths by accounting for the absolute differences in distances. Unlike the previous method, this is accomplished by eliminating a distance weight from the denominator rather than adding one more distance weight to the numerator. This can be carried out because the impact of distance is taken into account in both the first and last steps, having already been taken into account within the Huff probability.
Step 3: The accessibility value is calculated for each community as the sum of the supply ratios of all hospitals reachable for community within the maximum catchment size , multiplied by the corresponding Huff probabilities and the distance decay function :
3.3. Lorenz Curve and Gini Coefficient
In this study, the Gini Index was used to evaluate the inequality associated with accessibility value when different travel modes are used. It was also used to measure the medical demand of older adults at the community level. A higher Gini coefficient indicates a more uneven accessibility distribution for older adults. The Gini coefficient was calculated as follows:
where is the Gini coefficient, is the cumulative percentage of the older population in the community area, and is the cumulative ratio of resources in the community area. The Lorenz curve, plotted to obtain the Gini coefficient, denotes the rank-ordered cumulative distribution of accessibility for residents in different communities across Songjiang.
3.4. Spatial Inequity Analysis
Geospatial analysis was performed by calculating the global Moran’s Index, an inferential statistic which estimates spatial autocorrelation and falls between −1 and +1. More positive or negative values correspond to greater spatial clustering or competitive dispersion, respectively. To test the null hypothesis of random spatial distribution, empiric significance is computed through permutation to yield a pseudo-p-value. A pseudo-p-value is a summary of the results of the reference distribution and is dependent on the number of permutations used [89].
To visualize spatial clustering, local indicators of spatial autocorrelation (LISA) maps were created using local Moran’s Index calculations. This statistic identifies significant locations as high–high or low–low spatial clusters and high–low or low–high spatial outliers relative to neighboring regions [90]. Furthermore, the bivariate global Moran’s Index measures the spatial autocorrelation between a variable in one geographic area and another variable in a neighboring area, and in this study, the local Moran’s Index was mapped with bivariate LISA (BiLISA) maps.
GeoDa version 1.22 was used for geospatial analyses. All global and local bivariate Moran’s indices and BiLISA maps were permuted 999 times. The default significance level was set at 0.05.
4. Results
4.1. Accessibility to Public Hospitals
The statistical results of accessibility to public hospitals by different travel modes for the GH3SFCA and 2SFCA methods are shown in Table 4. In the GH3SFCA results, primary hospitals have lower average accessibility than secondary and tertiary hospitals across all four travel modes, while they have the highest maximum accessibility values. Among the four travel modes, cycling has the highest average accessibility value for all tiers of hospitals, followed by driving, public transit, and walking. A possible reason for this is that cycling is less influenced by peak hour traffic congestion, and public transit takes longer due to waiting and transfers. Noticeably, the standard deviations of driving accessibility are the lowest, followed by public transit, cycling, and walking, which is the highest. This indicates that high-speed travel modes lead to less of a distribution discrepancy in accessibility, regardless of the tier of the hospital. In the 2SFCA model, the accessibility values are significantly larger. It is noticeable that the standard deviations of the GH3SFCA accessibility results are lower than those of the 2SFCA results, indicating less of a distribution discrepancy in accessibility using the adopted modified GH3SFCA method.

Table 4.
Statistical characteristics of accessibility value.
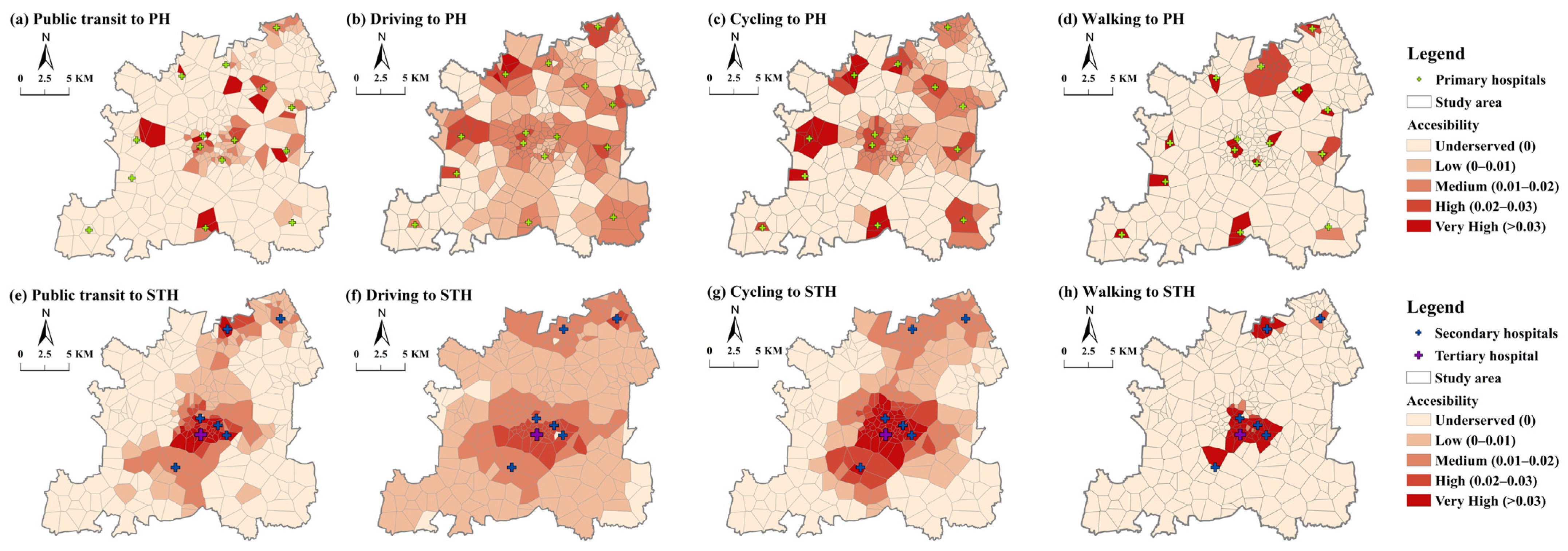
The distribution of spatial accessibility to primary hospitals for older adults is presented in Figure 5. The results show that primary hospitals are more accessible in the outskirts, while tertiary hospitals have better accessibility in areas surrounding the new town center. The level of accessibility to secondary and tertiary hospitals is unevenly distributed, decreasing significantly from the new town center outwards. This result is due to the concentration of tertiary and secondary hospitals in central areas of Songjiang, reflecting the unfavorable inter-area disparities. On the contrary, the high accessibility levels for primary hospitals are not so pronounced in the new town center. Primary hospitals are more accessible in wider areas and several highly accessible clusters on the outskirts. This overall picture of accessibility is consistent with a pattern of concentrated secondary and tertiary hospitals and more dispersed locations of primary hospitals in new towns. The central area has a high accessibility value due to its developed economy, convenient transportation service, and rich medical facilities. However, there are some communities in the central area that have low accessibility to primary hospitals, caused by the high population density of older people compared to the outskirts. The areas underserved by public transit and walking are significantly larger in number than those underserved by driving and cycling. This indicates that it is hard for residents to access public hospitals by public transit or walking within an acceptable time threshold. The number of areas underserved is the least for driving mode. Even in traffic jams, the speed of cars helps them to access hospitals more quickly than any other travel mode.
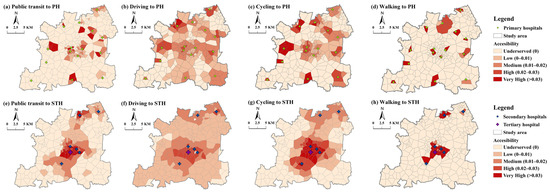
Figure 5.
Accessibility distribution with GH3SFCA (PH = primary hospitals; STH = secondary and tertiary hospitals).
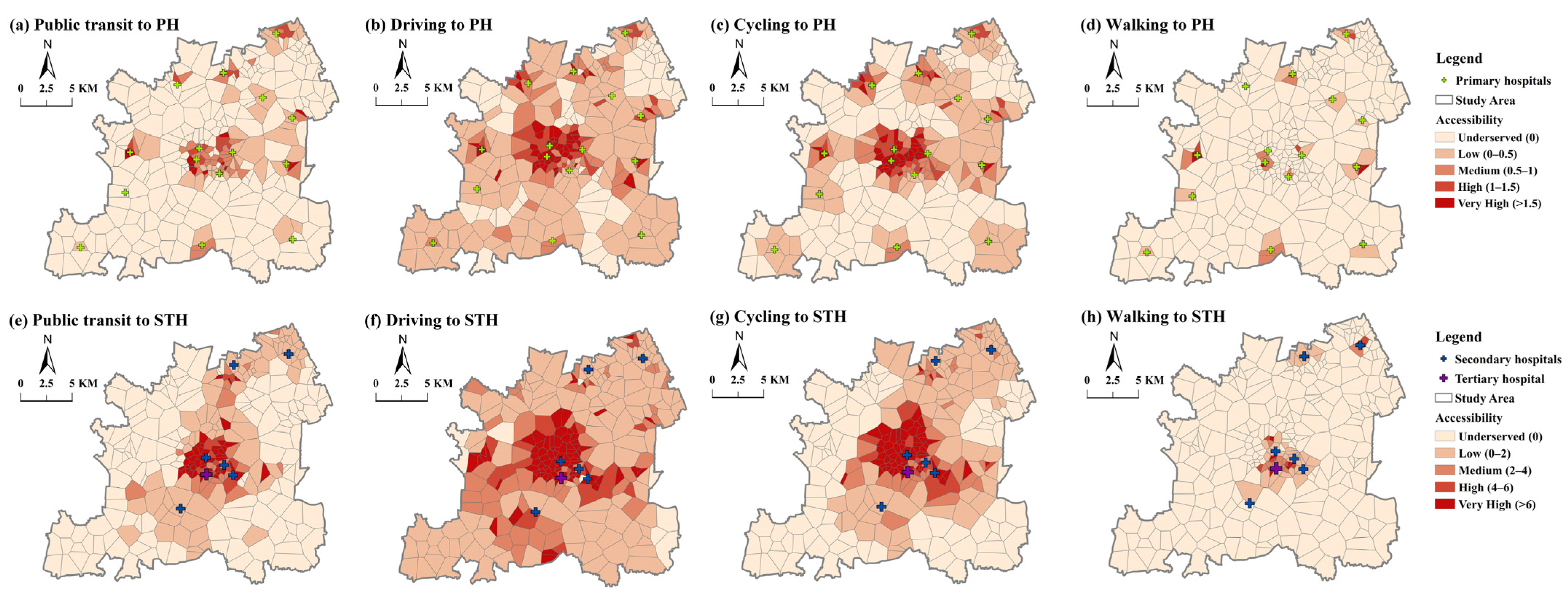
The accessibility distribution patterns to public hospitals with the 2SFCA method are shown in Figure 6. The distribution pattern and number of underserved areas are close to the results of the GH3SFCA method. However, the areas of high and very high accessibility are more numerous with the 2SFCA method, especially in the central area of Songjiang. In addition, the quantiles we use for 2SFCA have a higher value, to show a clear distribution level. This means 2SFCA overestimates the accessibility values in high-value area.
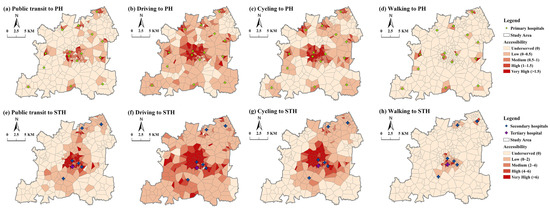
Figure 6.
Accessibility distribution with 2SFCA (PH = primary hospitals; STH = secondary and tertiary hospitals).
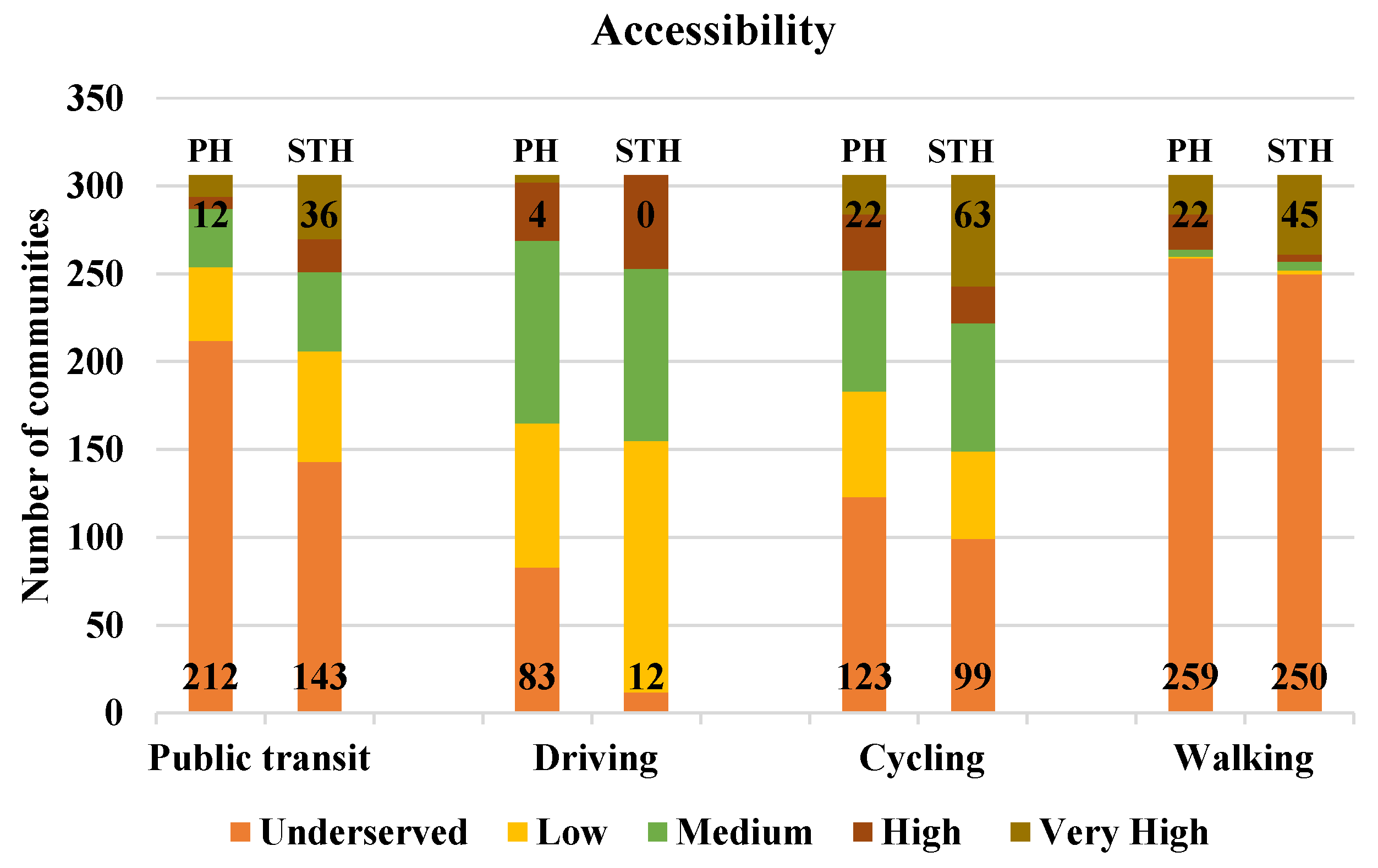
To further explore the differences in the accessibility distribution for public hospitals across travel modes, we compared the number of communities with accessibility at various levels (see Figure 7). Combining all four travel modes, the number of communities with high and very high levels of accessibility for secondary and tertiary hospitals is 239, higher than that for primary hospitals (152). Considering specific travel modes, the accessibility to different tiers of public hospitals shows varied characteristics. For cycling, the number of communities with high and very high accessibility to hospitals at all levels is the highest out of the four travel modes. For public transit, primary hospitals have larger underserved areas than secondary and tertiary hospitals. On the contrary, the number of communities with more than medium accessibility to all tiers of hospitals by driving is close, while the number of areas with very high accessibility is very low for all tiers. Walking trips have a much better distribution of accessibility, with the highest number of very-high-accessibility neighborhoods, but also the highest percentage of underserved communities.
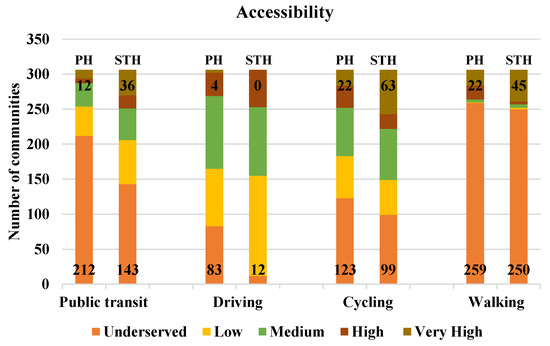
Figure 7.
Number of communities with different levels of accessibility to public hospitals, with very high on top and underserved on bottom (PH = primary hospitals; STH = secondary and tertiary hospitals).
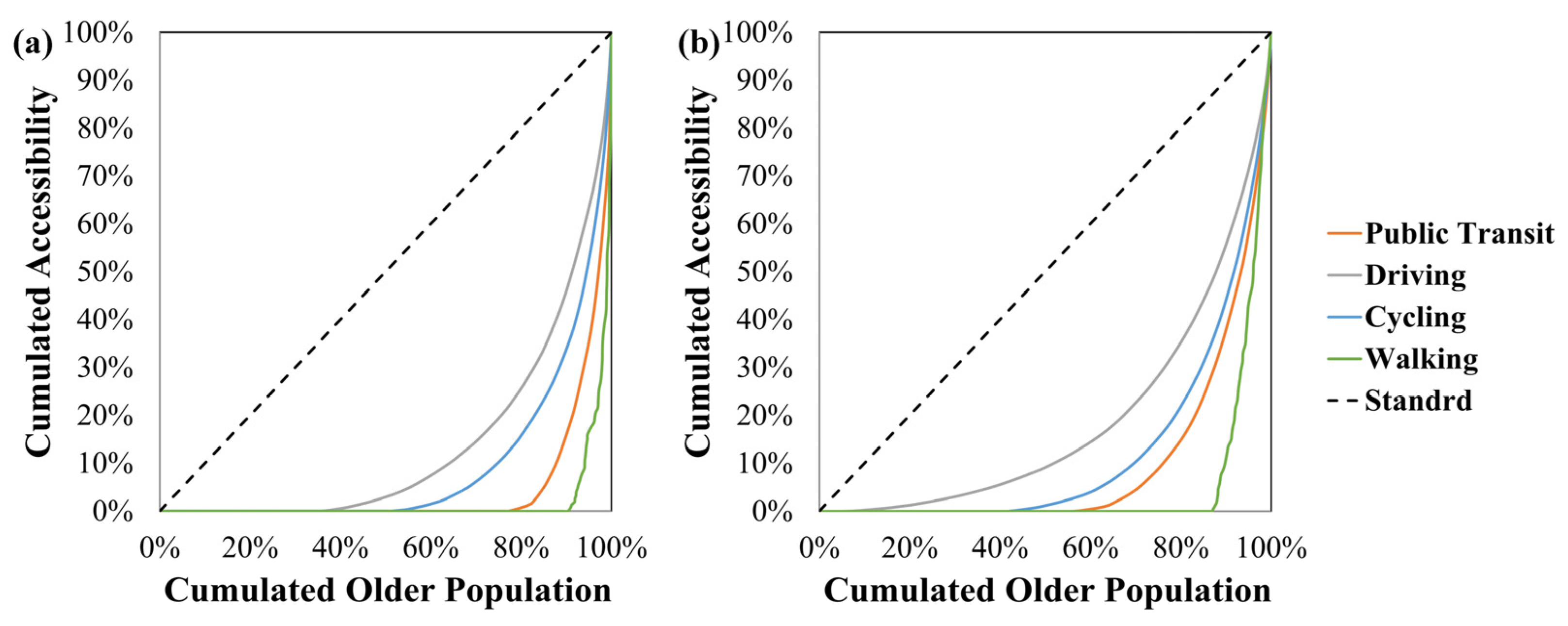
4.2. Gini Coefficient Analysis
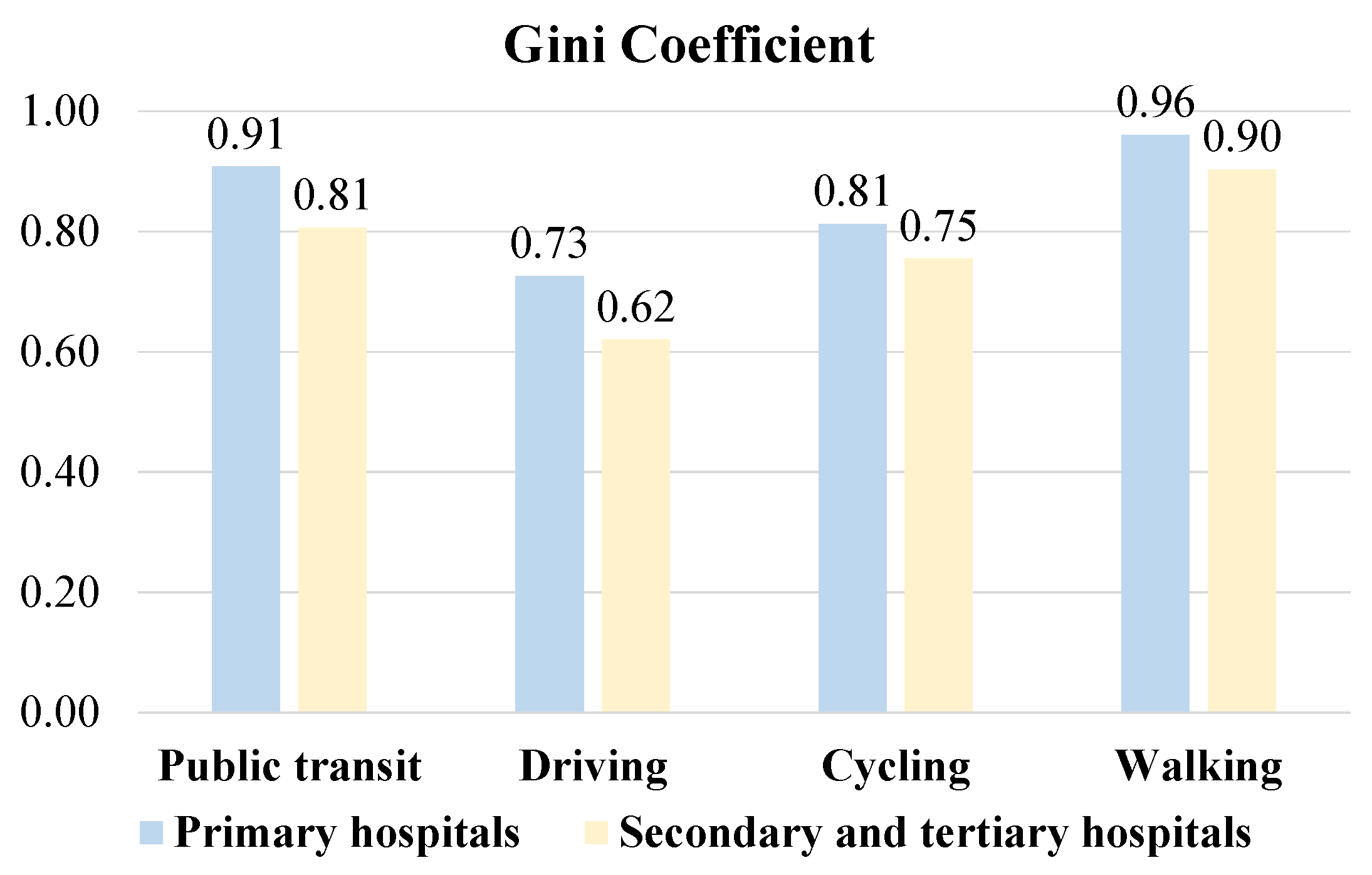
The accessibility inequity across public hospitals and different travel modes is shown by the Lorenz curve in Figure 8 and the Gini coefficient in Figure 9. The value of the Gini coefficient ranges from 0 to 1. A lower Gini coefficient indicates more equal access to public hospitals by older adults, with 1 being completely unequal.
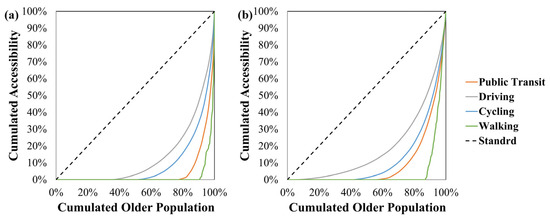
Figure 8.
Lorenz curve of public hospitals in different travel modes. (a) Primary hospitals. (b) Secondary and tertiary hospitals.
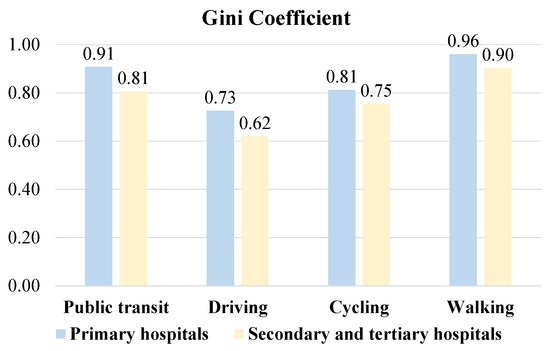
Figure 9.
Gini coefficient of accessibility to public hospitals by four travel modes.
Most communities in Songjiang showed more unequal accessibility by public transit and walking than by driving and cycling (Figure 8). At all tiers of public hospitals, accessibility by driving had the lowest Gini coefficient (0.73 for primary hospitals and 0.62 for secondary and tertiary hospitals) (Figure 9). This suggested that older adults driving to public hospitals obtained more spatially equal medical services than those traveling by other travel modes in Songjiang. In contrast, walking (0.96 and 0.90) and public transit (0.91 and 0.81) resulted in the highest Gini coefficients. These results indicated that older adults who walk or use public transit to access public hospitals had the largest spatial disparity between different communities. With Gini coefficients of 0.81 and 0.75, accessibility by cycling was slightly more equal across communities than by public transit or walking. Moreover, the Gini coefficients for all travel modes in primary hospitals were higher than those in secondary and tertiary hospitals. These findings demonstrated that older adults visiting primary hospitals experienced more unequal accessibility than those visiting secondary and tertiary hospitals, regardless of travel mode.
4.3. Spatial Relationships Between Population Density of Older People and Accessibility Distribution
Accessibility measures the overall availability of public hospitals within a certain time threshold, but the service efficiency of public hospitals is also highly related to the population density of older people. Therefore, we used Bivariate Global and Local Moran’s Indices to conduct a spatial correlation analysis between the population density of older people and accessibility distribution.
As shown in Table 5, the bivariate global Moran’s Index values are close to zero for primary hospitals among all four modes (first row). This result shows no significant global spatial correlation between accessibility and the population density of older people for primary hospitals. However, for secondary and tertiary hospitals, the bivariate global Moran’s Index values for the four modes are 0.672, 0.608, 0.584, and 0.496, respectively. They all pass the 5% significance level test, suggesting a positive spatial correlation between accessibility and the population density of older people across different travel modes.

Table 5.
Bivariate Moran’s Index values for public hospitals using different travel modes.
By using the bivariate local Moran’s Index, the spatial relationships between the population density of older people (medical service demand) and public hospital accessibility (medical service supply) are divided into five types, namely, high–high (HH) cluster, high–low (HL) outlier, low–high (LH) outlier, low–low (LL) cluster, and non-significant. The first ‘High (or Low)’ stands for the demand for medical services by older adults. The second ‘High (or Low)’ represents the supply of medical services by public hospitals across four travel modes. Both the HH and LL clusters mean spatial match. The HH cluster indicates a positive spatial match (high demand and supply) and the LL cluster means a negative spatial match (low demand and supply). Both the HL outlier and LH outlier indicate a spatial mismatch between public hospital accessibility and the population density of older people. The LH outlier means a positive spatial mismatch in which supply outweighs demand, while the HL outlier means a negative spatial mismatch in which demand outweighs supply. Notably, communities belonging to the HL outliers need special attention as they lack the medical services of public hospitals when traveling by at least one of the four travel modes. The non-significant type means the spatial relationships between population densities and public hospitals are not significant in the area.
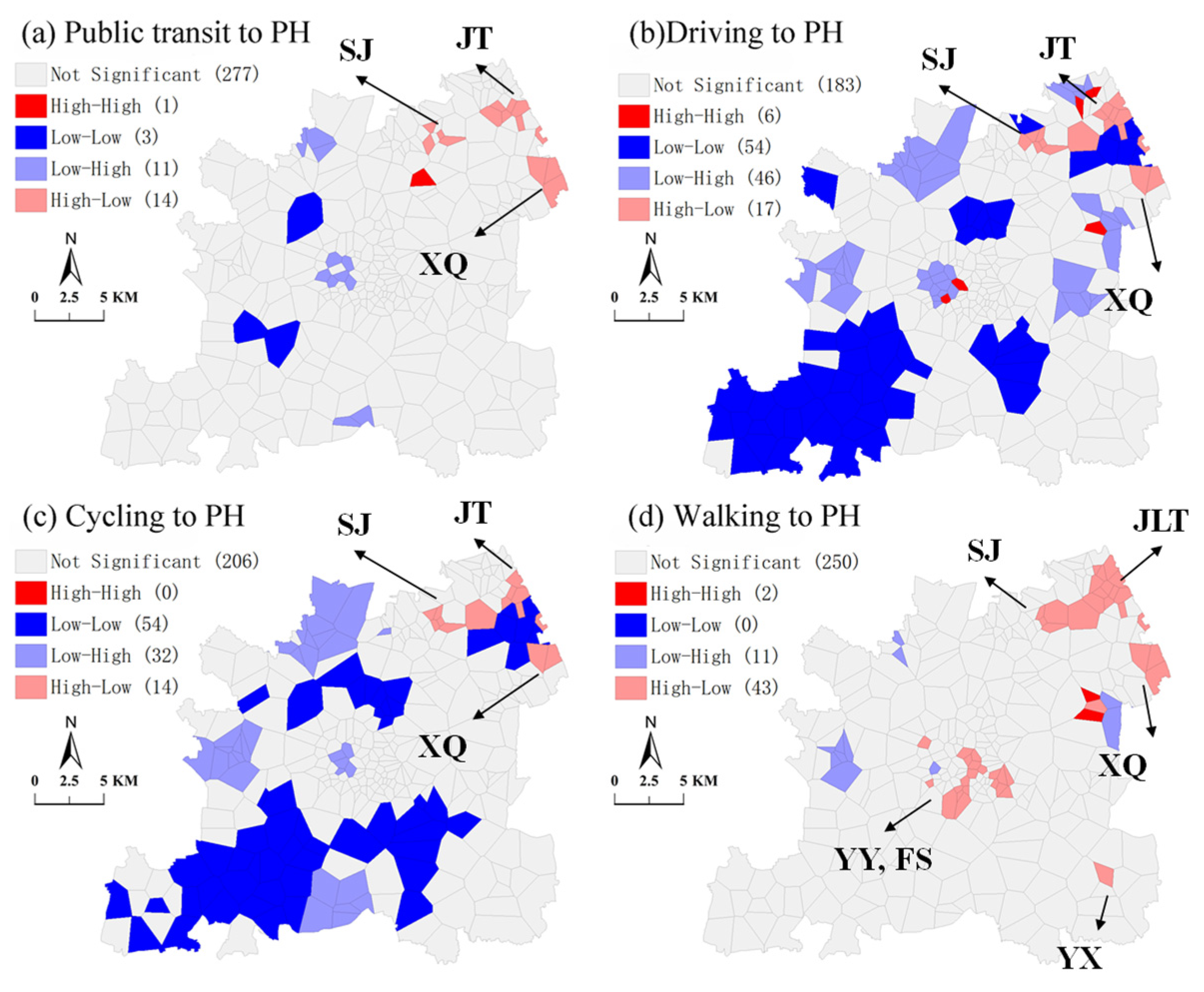
The clusters and outliers for primary hospitals are shown in the BiLISA maps in Figure 10. The distribution patterns are differentiable across the four travel modes, and most communities have non-significant spatial relationships for public transit and walking. The number of communities in HH clusters (deep red areas in Figure 10) is small among all four travel modes (1, 6, 0, and 2, respectively). Most of the communities in the LL clusters (deep blue areas) and LH clusters (light blue areas) are related to driving (54 LL and 46 LH) and cycling (54 LL and 32 LH). The LL communities are generally distributed in the southwestern part of Songjiang, whereas the LH communities are scattered inside the entire district. Regarding the HL outliers (light red areas), communities travel significantly more by walking (43) than by the other three modes. These communities, which are experiencing a shortfall of medical services from primary hospitals, are densely located in northeast Songjiang, including subdistricts of JT, JLT, SJ, and XQ. It is noticeable that northeast Songjiang has all five types of spatial relationships, demonstrating the complexity of the correlations between the population density of older people and primary hospital accessibility in these areas.
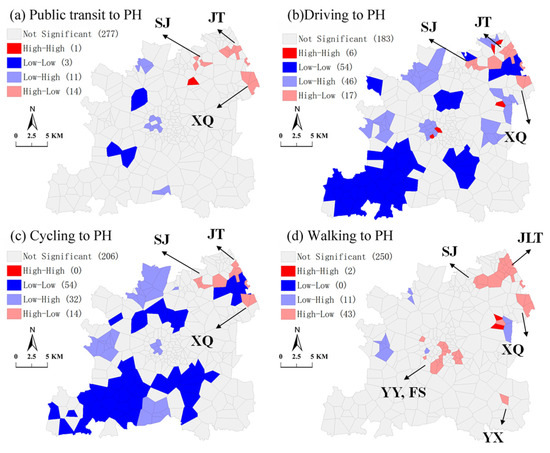
Figure 10.
BiLISA map between population density of older people and accessibility to primary hospitals (PH = primary hospitals).
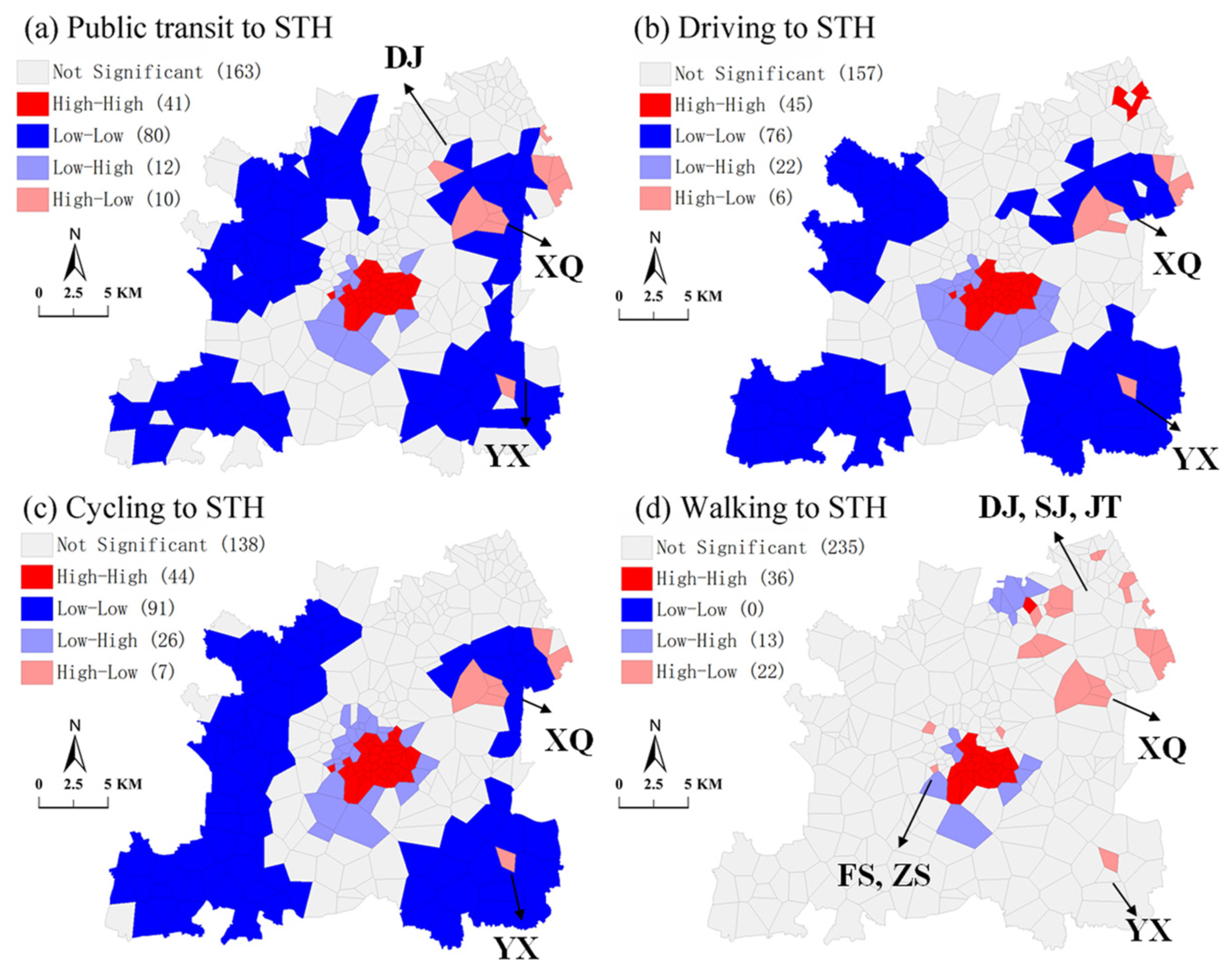
For secondary and tertiary hospitals (Figure 11), the spatial clusters and outlier patterns are similar across four travel modes, except for walking. The numbers of LL communities are high for public transit (80), driving (76), and cycling (91), while there are none for walking. The LL communities are mostly distributed around the outskirts of Songjiang. On the contrary, the HH communities are located in the central areas of Songjiang and surrounded by the LH communities. These two types of communities possess most of the secondary and tertiary hospitals, which provide sufficient medical services for older adults. As for the HL outliers, there are 22 communities related to walking and 10, 6, and 7 to public transit, driving, and cycling, respectively. The HL communities are mainly located in the XQ and JLT subdistricts in northeast Songjiang, where secondary and tertiary hospitals are scarce, but population densities high.
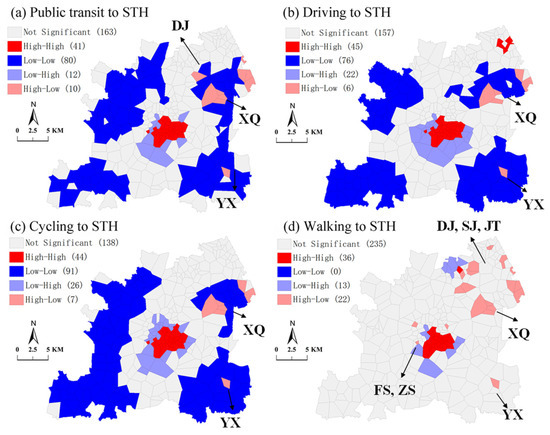
Figure 11.
BiLISA map between population density of older people and accessibility to primary hospitals (STH = secondary and tertiary hospitals).
5. Discussion
5.1. Spatial Accessibility to Public Hospitals
The differences in GH3SFCA and 2SFCA occur for a few reasons. One major limitation of 2SFCA is that it defines a supply facility as being accessible or inaccessible by a threshold distance, while the generalized 2SFCA incorporates distance decay in the supply–demand interaction [91]. A stronger distance decay function like Gaussian, which we used in our study, is more likely to result in a decentralized polycentric structure of accessibility. Our results align with some studies which state that while it has a minor impact on most accessible areas, it tends to identify more areas with the poorest accessibility [92]. On the other hand, the major advantage of introducing Huff probability is that it adopts a more comprehensive service competition scheme which includes both travel time and service capacity, but without overestimating distance effects [44].
These results suggest an insufficient healthcare service supply from public hospitals in Songjiang. For primary hospitals, the spatial accessibility decreases with the distance between surrounding communities and hospitals. This result makes sense, as each subdistrict in Songjiang is equipped with one primary hospital, except for JT. In geographically large or densely populated subdistricts, low spatial accessibility to primary hospitals is found among older adults, especially when traveling by public transit or walking. Regarding geographically large subdistricts, this study identified the SS and XKS subdistricts in northwest Songjiang, and the MG and XB subdistricts in southwest Songjiang. The subdistricts with a dense population of older people include the YY, FS, and ZS subdistricts in central Songjiang and the SJ and JT subdistricts in the northeast. Another study showed great disparity in accessibility to primary healthcare services in rural and suburban areas [73]. Therefore, the number of hospital beds and doctors should be increased in order to improve the provision of primary hospital services. It is also possible to set up another primary hospital in a subdistrict according to special circumstances.
The spatial accessibility to secondary and tertiary hospitals, however, declines from the central areas to outskirts of the entirety of Songjiang, regardless of travel mode. Some studies have found that the accessibility to secondary and tertiary hospitals in urban areas in developing countries is generally higher than that to primary hospitals [93], which is consistent with the average data in the new town area in our study. This may also be related to the higher threshold set for secondary and tertiary hospitals.
The seven secondary and tertiary hospitals in Songjiang are situated in the densely populated areas, with five in the central areas and the remaining two in the northeast. Consequently, these hospitals are not fully accessible to older adults from communities in other areas, albeit to varying degrees. Regarding different travel modes, driving is the most accessible, followed by electric bikes. Consistent with previous literature, this finding is due to the speed and mobility of these two modes. Additionally, the majority of communities are underserved in terms of hospitals service with the public transit and walking modes, particularly in the outskirts of Songjiang. Thus, new branches of tertiary hospitals should be built in areas with low accessibility, or some secondary hospitals of appropriate size should be established.
Moreover, the development of public transit should be accelerated in underserved areas. Public transportation is considered to be more environmentally friendly and more sustainable than private vehicles. Driving is still a choice for some residents, but quite a lot of families do not own private cars in Shanghai [94]. It has become a consensus to prioritize the development of public transit in China. Public transport interchanges can be optimized, and additional routes and frequencies can be established. The accessibility of healthcare facilities can be significantly improved by eliminating underserved areas of healthcare facilities through public transport.
In addition, the efficiency of the referral system should be improved in order to achieve an overall balance between the supply and demand of public hospital services. Different tiers of hospitals have different service capacities, and their attractiveness to older adults varies. Patients usually have a higher preference for higher-tier hospitals. An efficient referral system can guide patients’ hospital preferences and increase the equity of public hospitals [95].
5.2. Equity Analysis and Planning Suggestion
Considering the medical service supply (i.e., number of hospital beds) and demand (population density of older people), this study further examined the spatial equity of public hospitals by four travel modes. No global spatial correlation was found between the population density of older people and the spatial equity of primary hospitals. Nevertheless, a significant global spatial correlation was detected for secondary and tertiary hospitals. These results indicate more unequitable accessibility of primary hospitals than secondary and tertiary hospitals, especially by public transit and walking. A possible reason for this surprising finding is that the medical service supply of a primary hospitals is, on average, around 60% lower than that of a secondary or tertiary hospital. Meanwhile, some studies have found that the accessibility of secondary and tertiary hospitals in the central urban area of Shanghai is generally higher than that of primary hospitals, which is consistent with the average data in the suburbs of Shanghai in our study. As primary hospitals provide basic diagnoses and treatments to older adults in adjacent communities, they are more frequently visited than secondary and tertiary hospitals. Presumably, communities with a dense population of older people are more often underserved by primary hospitals than by secondary or tertiary hospitals. The BiLISA map further visualized the community-level distributions of spatial matches and mismatches between the population density of older people and medical service from public hospitals for the four travel modes. The typical ‘high-demand–low-supply’ communities are located in northeast Songjiang, including the JT, JLT, SJ, and XQ subdistricts. The YX subdistrict also has communities with ‘high-demand–low-supply’.
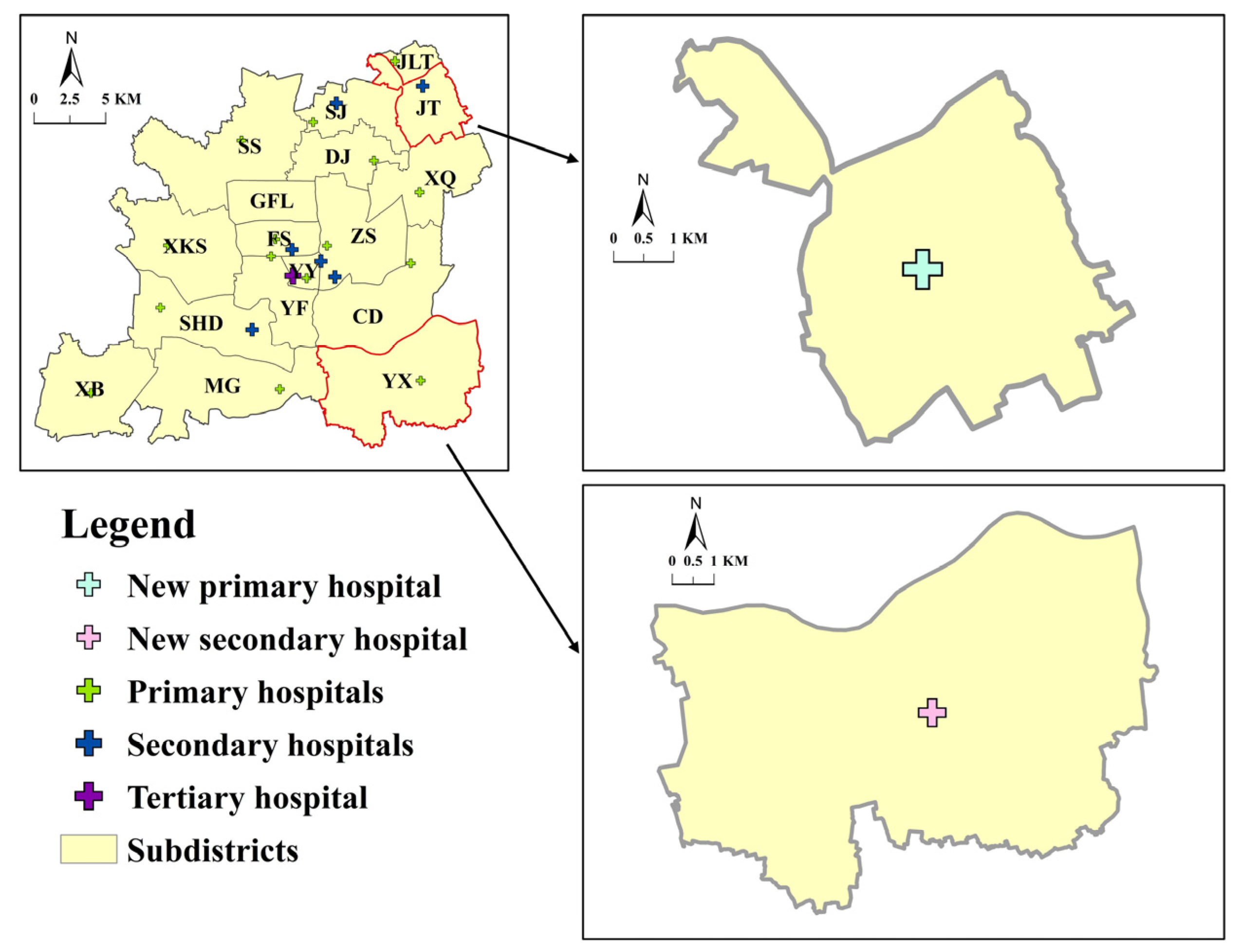
In future planning, these communities with ‘high-demand–low-supply’ should be prioritized in order to increase their capacity to supply healthcare services. Figure 12 depicts this study’s suggested sites for newly established primary and secondary hospitals. The JT subdistrict lacks primary hospitals due to previous planning reasons. At the same time, there are many communities with high populations of older people and a scarcity of primary hospitals located both within and around JT. Therefore, a primary hospital should be established in the JT subdistrict with 170 beds, higher than the average number of beds in primary hospitals. For high-tier hospitals, there are communities with ‘high-demand–low-supply’ in the YX subdistrict, along with communities with ‘low-demand–low-supply’ in the surrounding area. Therefore, only one secondary hospital is suggested, with the average number of beds of a secondary hospital (252).
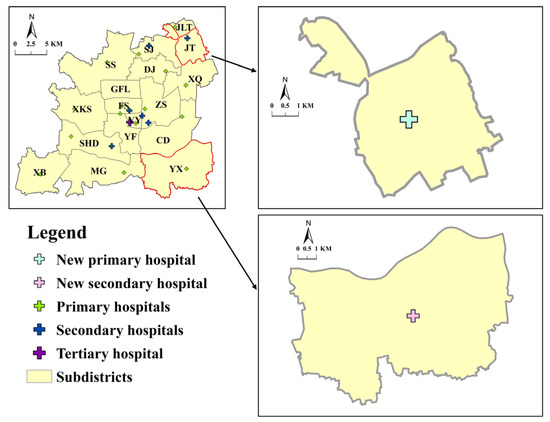
Figure 12.
Suggested sites for newly planned hospitals in Songjiang.
6. Conclusions
Developing countries are experiencing a tremendous increase in their aging populations, and are also witnessing the emergence of new towns. Nevertheless, the spatial accessibility and equity of healthcare services for older adults in new towns is rarely studied. This study is one of the early attempts to assess the spatial accessibility and equity of public hospitals for older adults, with data from Songjiang District, Shanghai, China. A Gaussian Huff-based three-step floating catchment area (GH3SFCA) method was adopted based on the real-time travel costs of public transit, driving, cycling, and walking. The results demonstrated the uneven spatial distribution patterns of public hospital services for different travel modes. Our findings will facilitate planning strategies and policies for public hospitals for older adults in new towns.
The advantages in this paper are as follows: (1) the real-time peak hour travel time of four travel modes, obtained by Amap API, echoes older adults’ travel conditions during actual public hospital visits; (2) the community-level analysis yields more accurate results than a subdistrict-level analysis, alleviates unnecessary deviation in travel time estimation, and discovers fine-grained variability in spatial accessibility and equity; and (3) by examining older adults’ accessibility and equity for different tiers of public hospital services, areas where improvement should be prioritized were found and plans suggested for them.
This study focused on the overall accessibility of different tiers of hospitals, as in some previous studies [48,96]. However, due to data limitations, different medical services in different departments were not discussed, such as emergencies and specialized diagnoses. On the demand side, because of the lack of detailed demographic data for older adults, we could not examine spatial accessibility related to specified medical needs and travel behaviors. Older adults in different age groups may have different medical needs, like chronic diseases, and travel mode options, like car ownership or mobility; these factors could affect healthcare accessibility. Also, our results did not consider medical demand and supply around the borders of the study area. The majority of the studies on this subject did not consider population and hospital services outside of the study area. A few studies considered a buffer zone outside of the study area, but still used the data and discussed the results inside the study area [97].
Based on our findings, we suggest some future research directions. As we focus on older adults, factors such as gender, income, and social status, which may have important influences on older adults’ access to hospitals, are not considered. Furthermore, the different choices of travel mode are a complicated problem with many factors that need to be considered. These require a large number of detailed studies and could be investigated in the future.
Author Contributions
Conceptualization, Mirkamiljan Mahmut, Pei Yin and Yi Zhang; Methodology, Mirkamiljan Mahmut and Pei Yin; Software, Mirkamiljan Mahmut and Pei Yin; Validation, Mirkamiljan Mahmut, Bozhezi Peng and Tao Wang; Formal Analysis, Mirkamiljan Mahmut, Bozhezi Peng and Yi Zhang; Investigation, Mirkamiljan Mahmut; Resources, Shengqiang Yuan; Data Curation, Mirkamiljan Mahmut, Pei Yin and Bozhezi Peng; Writing—Original Draft Preparation, Mirkamiljan Mahmut and Pei Yin; Writing—Review and Editing, Pei Yin, Tao Wang and Yi Zhang; Visualization, Mirkamiljan Mahmut and Jiani Wu; Supervision, Yi Zhang; Funding Acquisition, Shengqiang Yuan, Tao Wang and Yi Zhang. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by the National Social Science Foundation (No. 22AZD082), Shanghai Social Science Foundation (Nos. 2023BSH003, 22Z350204369, and 2022BSH005), Shanghai Scientific Research Foundation (Nos. 23DZ1202900, 23DZ1203200, 23DZ1202400, 22DZ1203200, 21Z510203259, and 21DZ1200800), Special Project of Healthy Shanghai Action (No. JKS-HZX_2022-13), and Scientific Research Fund (No. K2015K017).
Data Availability Statement
Some data used in this study are confidential and can only be provided with restrictions.
Conflicts of Interest
Author Shengqiang Yuan is a Shanghai Municipal Engineering Design Institute (Group) Co., Ltd., Shanghai 200092, China employee. The remaining authors declare that the research was carried out in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest, by providing the disclosure form of potential conflict of interest.
References
- Fatima, K.; Moridpour, S.; De Gruyter, C.; Saghapour, T. Elderly Sustainable Mobility: Scientific Paper Review. Sustainability 2020, 12, 7319. [Google Scholar] [CrossRef]
- Peng, B.; Wang, L.; Wu, J.; Li, C.; Wang, T.; Yuan, S.; Zhang, Y. Association between Built Environment and Bus Usage among Older Adults: Urban–Rural Differences in the Nonlinearities. ISPRS Int. J. Geo-Inf. 2024, 13, 316. [Google Scholar] [CrossRef]
- Cheng, L.; Chen, X.; Yang, S.; Cao, Z.; De Vos, J.; Witlox, F. Active travel for active ageing in China: The role of built environment. J. Transp. Geogr. 2019, 76, 142–152. [Google Scholar] [CrossRef]
- World Health Organization. China Country Assessment Report on Ageing and Health; WHO: Geneva, Switzerland, 2015. [Google Scholar]
- United Nations. World Population Ageing; Department of Economic and Social Affairs: New York City, NY, USA, 2017. [Google Scholar]
- Murray, A.T.; Grubesic, T.H. Locational planning of health care facilities. In Spatial Analysis in Health Geography; Routledge: London, UK, 2016; pp. 243–260. [Google Scholar]
- Xiaohelaiti, X.; Liu, X.; Li, C.; Wang, T.; Wu, J.; Peng, B.; Zhang, Y. Neighborhood environment and body mass index in community-dwelling older adults in China: The mediating role of transport-related physical activity. Geriatr. Nurs. 2024, 55, 304–310. [Google Scholar] [CrossRef]
- Prince, M.J.; Wu, F.; Guo, Y.; Gutierrez Robledo, L.M.; O’Donnell, M.; Sullivan, R.; Yusuf, S. The burden of disease in older people and implications for health policy and practice. Lancet 2015, 385, 549–562. [Google Scholar] [CrossRef]
- Dewulf, B.; Neutens, T.; De Weerdt, Y.; Van de Weghe, N. Accessibility to primary health care in Belgium: An evaluation of policies awarding financial assistance in shortage areas. BMC Fam. Pract. 2013, 14, 122. [Google Scholar] [CrossRef]
- Widener, M.J.; Hatzopoulou, M. Contextualizing research on transportation and health: A systems perspective. J. Transp. Health 2016, 3, 232–239. [Google Scholar] [CrossRef]
- Cvitkovich, Y.; Wister, A. The importance of transportation and prioritization of environmental needs to sustain well-being among older adults. Environ. Behav. 2001, 33, 809–829. [Google Scholar] [CrossRef]
- Hiscock, R.; Pearce, J.; Blakely, T.; Witten, K. Is neighborhood access to health care provision associated with individual-level utilization and satisfaction? Health Serv. Res. 2008, 43, 2183–2200. [Google Scholar] [CrossRef]
- Satariano, W.A.; Guralnik, J.M.; Jackson, R.J.; Marottoli, R.A.; Phelan, E.A.; Prohaska, T.R. Mobility and aging: New directions for public health action. Am. J. Public Health 2012, 102, 1508–1515. [Google Scholar] [CrossRef]
- Cheng, L.; Caset, F.; De Vos, J.; Derudder, B.; Witlox, F. Investigating walking accessibility to recreational amenities for elderly people in Nanjing, China. Transp. Res. Part D Transp. Environ. 2019, 76, 85–99. [Google Scholar] [CrossRef]
- Lucas, K.; Van Wee, B.; Maat, K. A method to evaluate equitable accessibility: Combining ethical theories and accessibility-based approaches. Transportation 2016, 43, 473–490. [Google Scholar] [CrossRef]
- Ricciardi, A.M.; Xia, J.C.; Currie, G. Exploring public transport equity between separate disadvantaged cohorts: A case study in Perth, Australia. J. Transp. Geogr. 2015, 43, 111–122. [Google Scholar] [CrossRef]
- Roopani; Dumka, N.; Ahmad, T.; Hannah, E.; Kotwal, A. Health facility utilization and Healthcare-seeking behaviour of the elderly population in India. J. Fam. Med. Prim. Care 2023, 12, 902–916. [Google Scholar] [CrossRef] [PubMed]
- Charney, I. Re-planning an edge city: Tysons in the post-suburban era. Cities 2020, 106, 102919. [Google Scholar] [CrossRef]
- Gu, X.; Zhou, H.; Zhang, L. Spatial Accessibility Assessment of Healthcare Services and Governance Optimization in New Urban Areas of Megacity: The Case of Five New Towns in Shanghai. Urban Stud. 2022, 29, 20–26. [Google Scholar]
- Wang, L.; Kundu, R.; Chen, X. Building for what and whom? New town development as planned suburbanization in China and India. In Suburbanization in Global Society; Emerald Group Publishing Limited: Bradford, UK, 2010; Volume 10, pp. 319–345. [Google Scholar]
- Wang, K.L.J.; Wang, H. China’s New Town and New District 40 Years: Process, Evaluation, and Prospect; China Architecture & Building Press: Beijing, China, 2021. [Google Scholar]
- Powell, B. Inside China’s runaway building boom. Time Magazine, 5 April 2010. [Google Scholar]
- Hansen, W.G. How accessibility shapes land use. J. Am. Inst. Plan. 1959, 25, 73–76. [Google Scholar] [CrossRef]
- Morris, J.M.; Dumble, P.L.; Wigan, M.R. Accessibility indicators for transport planning. Transp. Res. Part A Gen. 1979, 13, 91–109. [Google Scholar] [CrossRef]
- Penchansky, R.; Thomas, J.W. The concept of access: Definition and relationship to consumer satisfaction. Med. Care 1981, 19, 127–140. [Google Scholar] [CrossRef]
- Luo, W.; Wang, F. Measures of spatial accessibility to health care in a GIS environment: Synthesis and a case study in the Chicago region. Environ. Plan. B Plan. Des. 2003, 30, 865–884. [Google Scholar] [CrossRef]
- Abernathy, W.J.; Hershey, J.C. A spatial-allocation model for regional health-services planning. Oper. Res. 1972, 20, 629–642. [Google Scholar] [CrossRef]
- Alegana, V.A.; Wright, J.A.; Pentrina, U.; Noor, A.M.; Snow, R.W.; Atkinson, P.M. Spatial modelling of healthcare utilisation for treatment of fever in Namibia. Int. J. Health Geogr. 2012, 11, 6. [Google Scholar] [CrossRef] [PubMed]
- Mayhew, L.D.; Leonardi, G. Equity, efficiency, and accessibility in urban and regional health-care systems. Environ. Plan. A 1982, 14, 1479–1507. [Google Scholar] [CrossRef]
- Tanser, F.; Gething, P.; Atkinson, P. Location-allocation Planning. In A Companion to Health and Medical Geography; Wiley: Hoboken, NJ, USA, 2009; pp. 540–566. [Google Scholar]
- Wang, F. Measurement, optimization, and impact of health care accessibility: A methodological review. Ann. Assoc. Am. Geogr. 2012, 102, 1104–1112. [Google Scholar] [CrossRef]
- Wang, F. Quantitative Methods and Socio-Economic Applications in GIS; CRC Press: Boca Raton, FL, USA, 2014. [Google Scholar]
- Kwan, M.P.; Weber, J. Individual accessibility revisited: Implications for geographical analysis in the twenty-first century. Geogr. Anal. 2003, 35, 341–353. [Google Scholar]
- Neutens, T.; Schwanen, T.; Witlox, F.; De Maeyer, P. Equity of urban service delivery: A comparison of different accessibility measures. Environ. Plan. A 2010, 42, 1613–1635. [Google Scholar] [CrossRef]
- Guagliardo, M.F. Spatial accessibility of primary care: Concepts, methods and challenges. Int. J. Health Geogr. 2004, 3, 3. [Google Scholar] [CrossRef]
- Neutens, T. Accessibility, equity and health care: Review and research directions for transport geographers. J. Transp. Geogr. 2015, 43, 14–27. [Google Scholar] [CrossRef]
- Langford, M.; Higgs, G. Measuring potential access to primary healthcare services: The influence of alternative spatial representations of population. Prof. Geogr. 2006, 58, 294–306. [Google Scholar] [CrossRef]
- Mao, L.; Nekorchuk, D. Measuring spatial accessibility to healthcare for populations with multiple transportation modes. Health Place 2013, 24, 115–122. [Google Scholar] [CrossRef]
- Rauch, S.; Stangl, S.; Haas, T.; Rauh, J.; Heuschmann, P.U. Spatial inequalities in preventive breast cancer care: A comparison of different accessibility approaches for prevention facilities in Bavaria, Germany. J. Transp. Health 2023, 29, 101567. [Google Scholar] [CrossRef]
- Dai, D. Black residential segregation, disparities in spatial access to health care facilities, and late-stage breast cancer diagnosis in metropolitan Detroit. Health Place 2010, 16, 1038–1052. [Google Scholar] [CrossRef] [PubMed]
- Dai, D.; Wang, F. Geographic disparities in accessibility to food stores in southwest Mississippi. Environ. Plan. B Plan. Des. 2011, 38, 659–677. [Google Scholar] [CrossRef]
- Luo, W.; Qi, Y. An enhanced two-step floating catchment area (E2SFCA) method for measuring spatial accessibility to primary care physicians. Health Place 2009, 15, 1100–1107. [Google Scholar] [CrossRef]
- Wan, N.; Zou, B.; Sternberg, T. A three-step floating catchment area method for analyzing spatial access to health services. Int. J. Geogr. Inf. Sci. 2012, 26, 1073–1089. [Google Scholar] [CrossRef]
- Luo, J. Integrating the huff model and floating catchment area methods to analyze spatial access to healthcare services. Trans. GIS 2014, 18, 436–448. [Google Scholar] [CrossRef]
- Luo, J. Analyzing potential spatial access to primary care services with an enhanced floating catchment area method. Cartogr. Int. J. Geogr. Inf. Geovisualization 2016, 51, 12–24. [Google Scholar] [CrossRef]
- Tao, Z.; Wang, Q. Facility or Transport Inequality? Decomposing Healthcare Accessibility Inequality in Shenzhen, China. Int. J. Environ. Res. Public Health 2022, 19, 6897. [Google Scholar] [CrossRef] [PubMed]
- Xing, J.; Ng, S.T. Analyzing spatiotemporal accessibility patterns to tertiary healthcare services by integrating total travel cost into an improved E3SFCA method in Changsha, China. Cities 2022, 122, 103541. [Google Scholar] [CrossRef]
- Cheng, L.; Yang, M.; De Vos, J.; Witlox, F. Examining geographical accessibility to multi-tier hospital care services for the elderly: A focus on spatial equity. J. Transp. Health 2020, 19, 100926. [Google Scholar] [CrossRef]
- Lechowski, Ł. Effects of choice of data aggregation method to a point on walking accessibility results using the G2SFCA method. Pr. Kom. Geogr. Komun. PTG 2022, 25, 74–93. [Google Scholar] [CrossRef]
- Zainab, U.I.; Kruger, E.; Tennant, M. Major metropolis rail system access to dental care for the retired and elderly: A high-resolution geographic study of Sydney, Australia. Gerodontology 2015, 32, 302–308. [Google Scholar] [CrossRef]
- Evans, R.; Larkins, S.; Cheffins, T.; Fleming, R.; Johnston, K.; Tennant, M. Mapping access to health services as a strategy for planning: Access to primary care for older people in regional Queensland. Aust. J. Prim. Health 2017, 23, 114–122. [Google Scholar] [CrossRef] [PubMed]
- Messinger-Rapport, B. Disparities in long-term healthcare. Nurs. Clin. N. Am. 2009, 44, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Yuan, Y.; Yang, M.; Wu, J.; Rasouli, S.; Lei, D. Assessing bus transit service from the perspective of elderly passengers in Harbin, China. Int. J. Sustain. Transp. 2019, 13, 761–776. [Google Scholar] [CrossRef]
- Cheng, L.; Chen, X.; Yang, S.; Wu, J.; Yang, M. Structural equation models to analyze activity participation, trip generation, and mode choice of low-income commuters. Transp. Lett. 2019, 11, 341–349. [Google Scholar] [CrossRef]
- Loo, B.P.; Lam, W.W.Y. Geographic accessibility around health care facilities for elderly residents in Hong Kong: A microscale walkability assessment. Environ. Plan. B Plan. Des. 2012, 39, 629–646. [Google Scholar]
- Jin, Z.; Northridge, M.E.; Metcalf, S.S. Modeling the influence of social ties and transportation choice on access to oral healthcare for older adults. Appl. Geogr. 2018, 96, 66–76. [Google Scholar] [CrossRef]
- Zhang, Q.; Northridge, M.E.; Jin, Z.; Metcalf, S.S. Modeling accessibility of screening and treatment facilities for older adults using transportation networks. Appl. Geogr. 2018, 93, 64–75. [Google Scholar] [CrossRef]
- Hudson, E.; Nolan, A. Public healthcare eligibility and the utilisation of GP services by older people in Ireland. J. Econ. Ageing 2015, 6, 24–43. [Google Scholar] [CrossRef]
- Wu, J.; Li, C.; Zhu, L.; Liu, X.; Peng, B.; Wang, T.; Yuan, S.; Zhang, Y. Nonlinear and threshold effects of built environment on older adults’ walking duration: Do age and retirement status matter? Front. Public Health 2024, 12, 1418733. [Google Scholar] [CrossRef] [PubMed]
- Kelly, C.; Hulme, C.; Farragher, T.; Clarke, G. Are differences in travel time or distance to healthcare for adults in global north countries associated with an impact on health outcomes? A systematic review. BMJ Open 2016, 6, e013059. [Google Scholar] [CrossRef]
- Tao, Z.; Cheng, Y. Modelling the spatial accessibility of the elderly to healthcare services in Beijing, China. Environ. Plan. B Urban Anal. City Sci. 2019, 46, 1132–1147. [Google Scholar] [CrossRef]
- Wu, H.-C.; Tseng, M.-H. Evaluating disparities in elderly community care resources: Using a geographic accessibility and inequality index. Int. J. Environ. Res. Public Health 2018, 15, 1353. [Google Scholar] [CrossRef]
- Cheng, Y.; Wang, J.; Rosenberg, M.W. Spatial access to residential care resources in Beijing, China. Int. J. Health Geogr. 2012, 11, 32. [Google Scholar] [CrossRef]
- Cao, M.; Zhang, Y.; Zhang, Y.; Li, S.; Hickman, R. Using different approaches to evaluate individual social equity in transport. In A Companion to Transport, Space and Equity; Edward Elgar Publishing: Cheltenham, UK, 2019; pp. 209–228. [Google Scholar]
- Guzman, L.A.; Oviedo, D. Accessibility, affordability and equity: Assessing ‘pro-poor’public transport subsidies in Bogotá. Transp. Policy 2018, 68, 37–51. [Google Scholar] [CrossRef]
- Shinjo, D.; Aramaki, T. Geographic distribution of healthcare resources, healthcare service provision, and patient flow in Japan: A cross sectional study. Soc. Sci. Med. 2012, 75, 1954–1963. [Google Scholar] [CrossRef]
- Lee, K.-S. Disparity in the spatial distribution of clinics within a metropolitan city. Geospat. Health 2013, 7, 199–207. [Google Scholar] [CrossRef] [PubMed]
- Song, X.; Wei, Y.; Deng, W.; Zhang, S.; Zhou, P.; Liu, Y.; Wan, J. Spatio-temporal distribution, spillover effects and influences of China’s two levels of public healthcare resources. Int. J. Environ. Res. Public Health 2019, 16, 582. [Google Scholar] [CrossRef]
- Shen, J.; Wu, F. The suburb as a space of capital accumulation: The development of new towns in Shanghai, China. Antipode 2017, 49, 761–780. [Google Scholar] [CrossRef]
- Pan, J.; Zhao, H.; Wang, X.; Shi, X. Assessing spatial access to public and private hospitals in Sichuan, China: The influence of the private sector on the healthcare geography in China. Soc. Sci. Med. 2016, 170, 35–45. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Song, X.; Wei, Y.; Deng, W. Spatial equity of multilevel healthcare in the metropolis of Chengdu, China: A new assessment approach. Int. J. Environ. Res. Public Health 2019, 16, 493. [Google Scholar] [CrossRef] [PubMed]
- Yu, W.; Li, M.; Ye, F.; Xue, C.; Zhang, L. Patient preference and choice of healthcare providers in Shanghai, China: A cross-sectional study. BMJ Open 2017, 7, e016418. [Google Scholar] [CrossRef] [PubMed]
- Yang, T.; Luo, W.; Tian, L.; Li, J. Integrating Spatial and Non-Spatial Dimensions to Evaluate Access to Rural Primary Healthcare Service: A Case Study of Songzi, China. ISPRS Int. J. Geo-Inf. 2024, 13, 142. [Google Scholar] [CrossRef]
- Liu, L.; Zhao, Y.; Lyu, H.; Chen, S.; Tu, Y.; Huang, S. Spatial Accessibility and Equity Evaluation of Medical Facilities Based on Improved 2SFCA: A Case Study in Xi’an, China. Int. J. Environ. Res. Public Health 2023, 20, 2076. [Google Scholar] [CrossRef]
- Luo, W.; Whippo, T. Variable catchment sizes for the two-step floating catchment area (2SFCA) method. Health Place 2012, 18, 789–795. [Google Scholar] [CrossRef]
- Qian, Z.; Liu, Q.; Huang, D. Three Scales and Planning Trends of 15-Minute Life Circle. Urban Plan. Int. 2022, 37, 63–70. [Google Scholar]
- Wu, W.; Zheng, T. Establishing a “dynamic two-step floating catchment area method” to assess the accessibility of urban green space in Shenyang based on dynamic population data and multiple modes of transportation. Urban For. Urban Green. 2023, 82, 127893. [Google Scholar] [CrossRef]
- Hu, Y.; Zhang, Z. Skilled doctors in tertiary hospitals are already overworked in China. Lancet Glob. Health 2015, 3, e737. [Google Scholar] [CrossRef]
- Weinert, J.X.; Ma, C.; Yang, X. The Transition to Electric Bikes in China and Its Effect on Travel Behavior, Transit Use, and Safety; UC Davis: Institute of Transportation Studies: Davis, CA, USA, 2006. [Google Scholar]
- Peng, B.; Zhang, Y.; Li, C.; Wang, T.; Yuan, S. Nonlinear, threshold and synergistic effects of first/last-mile facilities on metro ridership. Transp. Res. Part D Transp. Environ. 2023, 121, 103856. [Google Scholar] [CrossRef]
- Zhang, J.; Lin, D.; Zhou, X.; Li, F.; Zhou, Y.M.; Cheng, Y.Q.; Wang, P. Spatial accessibility and equality of public medical facilities in rural areas based on the improved 3SFCA: A case of Haikou City. Prog. Geogr. 2022, 41, 636–647. [Google Scholar] [CrossRef]
- Li, Y.; Chen, Q.; Ma, Q.; Yu, H.; Huang, Y.; Zhu, L.; Zhang, H.; Li, C.; Lu, G. Injuries and risk factors associated with bicycle and electric bike use in China: A systematic review and meta-analysis. Saf. Sci. 2022, 152, 105769. [Google Scholar] [CrossRef]
- Bohannon, R.W. Comfortable and maximum walking speed of adults aged 20–79 years: Reference values and determinants. Age Ageing 1997, 26, 15–19. [Google Scholar] [CrossRef]
- Zhang, F.; Li, D.; Ahrentzen, S.; Zhang, J. Assessing spatial disparities of accessibility to community-based service resources for Chinese older adults based on travel behavior: A city-wide study of Nanjing, China. Habitat Int. 2019, 88, 101984. [Google Scholar] [CrossRef]
- Jin, T.; Cheng, L.; Wang, K.; Cao, J.; Huang, H.; Witlox, F. Examining equity in accessibility to multi-tier healthcare services across different income households using estimated travel time. Transp. Policy 2022, 121, 1–13. [Google Scholar] [CrossRef]
- Li, C.; Wang, J. A hierarchical two-step floating catchment area analysis for high-tier hospital accessibility in an urban agglomeration region. J. Transp. Geogr. 2022, 102, 103369. [Google Scholar] [CrossRef]
- Bauer, J.; Groneberg, D.A. Measuring spatial accessibility of health care providers–introduction of a variable distance decay function within the floating catchment area (FCA) method. PLoS ONE 2016, 11, e0159148. [Google Scholar] [CrossRef]
- Del Conte, D.E.; Locascio, A.; Amoruso, J.; McNamara, M.L. Modeling multimodal access to primary care in an urban environment. Transp. Res. Interdiscip. Perspect. 2022, 13, 100550. [Google Scholar] [CrossRef]
- Anselin, L. An Introduction to Spatial Data Science with GeoDaVolume 1: Exploring Spatial Data; CRC Press: Boca Raton, FL, USA, 2024. [Google Scholar]
- Anselin, L. Local indicators of spatial association—LISA. Geogr. Anal. 1995, 27, 93–115. [Google Scholar] [CrossRef]
- Wang, F. Inverted Two-Step Floating Catchment Area Method for Measuring Facility Crowdedness. Prof. Geogr. 2018, 70, 251–260. [Google Scholar] [CrossRef]
- Wang, C.; Leitner, M.; Paulus, G. Multiscale Analysis of Spatial Accessibility to Acute Hospitals in Carinthia, Austria. ISPRS Int. J. Geo-Inf. 2023, 12, 491. [Google Scholar] [CrossRef]
- Cheng, M.; Tao, L.; Lian, Y.; Huang, W. Measuring Spatial Accessibility of Urban Medical Facilities: A Case Study in Changning District of Shanghai in China. Int. J. Environ. Res. Public Health 2021, 18, 9598. [Google Scholar] [CrossRef] [PubMed]
- Gu, X.; Zhang, L.; Tao, S.; Xie, B. Spatial Accessibility to Healthcare Services in Metropolitan Suburbs: The Case of Qingpu, Shanghai. Int. J. Environ. Res. Public Health 2019, 16, 225. [Google Scholar] [CrossRef] [PubMed]
- Siegel, M.; Koller, D.; Vogt, V.; Sundmacher, L. Developing a composite index of spatial accessibility across different health care sectors: A German example. Health Policy 2016, 120, 205–212. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.Y.; Deng, Q.T.; Wang, S.Y.; Wang, G.B. Equity Evaluation of Multilevel Medical Facility Allocation Based on Ga2SFCA. J. Urban Plan. Dev. 2023, 149, 04023041. [Google Scholar] [CrossRef]
- Shao, Y.; Luo, W. Supply-demand adjusted two-steps floating catchment area (SDA-2SFCA) model for measuring spatial access to health care. Soc. Sci. Med. 2022, 296, 114727. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Published by MDPI on behalf of the International Society for Photogrammetry and Remote Sensing. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).