Assessing the Value of a Human Life in Heat-Related Mortality: Lessons from COVID-19 in Belgium
Abstract
:1. Introduction
2. Data and Methods
2.1. COVID-19 Mortality as a Proxy for Heat-Related Mortality
- Elderly individuals, especially those with multiple chronic conditions and those living in nursing homes;
- People with underlying medical conditions such as cardiovascular and cerebrovascular disease, hypertension, chronic pulmonary disease, kidney disease, diabetes, obesity, Alzheimer’s disease, and dementia;
- Socially isolated persons (homeless people, migrants, older people living alone).
2.2. Gross Domestic Product (GDP)
2.3. COVID-19 Mortality
2.4. Epidemiological Modelling
3. Results
3.1. Net Loss of Gross Domestic Product (GDP)
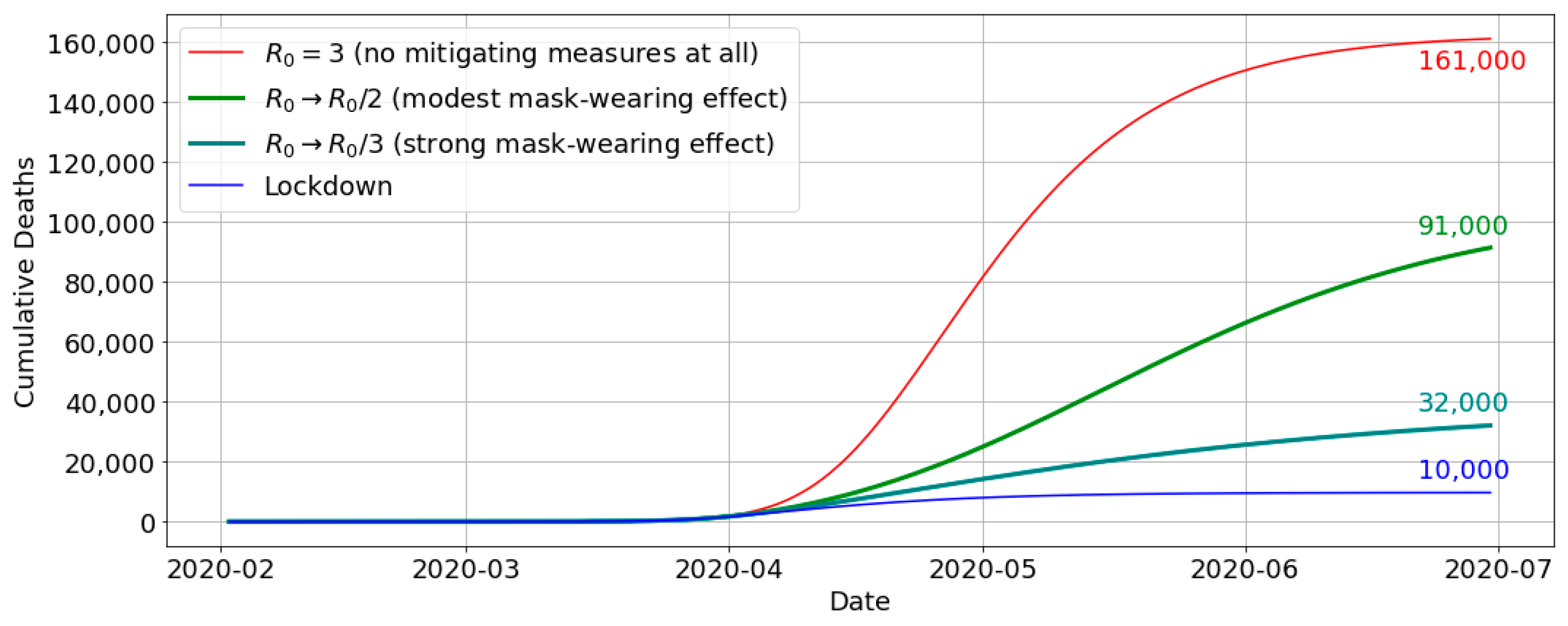
3.2. Number of Lives Saved Due to the Lockdown
3.3. Cost per Avoided Death
- The net GDP loss caused by the lockdown amounts to EUR 19.4 billion ± EUR 2.7 billion;
- The number of avoided deaths due to the lockdown is estimated at 52,000 ± 29,000.
4. Discussion
5. Conclusions
- The net loss in the gross domestic product (GDP) occurring in the first half of the year 2020 (i.e., the period encompassing the first COVID-19 wave) due to the measures taken by the government, which was estimated to represent a loss of 19.4 billion ± EUR 2.7 billion;
- The number of avoided deaths due to the lockdown, estimated using evidence from the literature and through epidemiological modelling, considering the hypothetical number of people that were saved due to the measures taken by the government, their number amounting to 52,000 ± 29,000.
Funding
Data Availability Statement
Conflicts of Interest
References
- van Daalen, K.R.; Tonne, C.; Semenza, J.C.; Rocklöv, J.; Markandya, A.; Dasandi, N.; Jankin, S.; Achebak, H.; Ballester, J.; Bechara, H.; et al. The 2024 Europe report of the Lancet Countdown on health and climate change: Unprecedented warming demands unprecedented action. Lancet Public Health 2024, 9, e495–e522. [Google Scholar] [CrossRef] [PubMed]
- Matthews, T.K.R.; Wilby, R.L.; Murphy, C. Communicating the deadly consequences of global warming for human heat stress. Proc. Natl. Acad. Sci. USA 2017, 114, 3861–3866. [Google Scholar] [CrossRef]
- Borden, K.A.; Cutter, S.L. Spatial patterns of natural hazards mortality in the United States. Int. J. Health Geograph. 2008, 7, 64. [Google Scholar] [CrossRef] [PubMed]
- Beven, J.L., II; Avila, L.A.; Blake, E.S.; Brown, D.P.; Franklin, J.L.; Knabb, R.D.; Pasch, R.J.; Rhome, J.R.; Stewart, S.R. Atlantic Hurricane Season of 2005. Mon. Weather Rev. 2008, 136, 1109–1173. [Google Scholar] [CrossRef]
- Robine, J.-M.; Cheung, S.L.K.; le Roy, S.; van Oyen, H.; Griffiths, C.; Michel, J.-P.; Herrmann, F.R. Death toll exceeded 70,000 in Europe during the summer of 2003. Comptes. Rendus. Biol. 2008, 331, 171–178. [Google Scholar] [CrossRef]
- Golnaraghi, M.; Etienne, C.; Guha-Sapir, D.; Below, R. Atlas of Mortality and Economic Losses from Weather, Climate and Water Extremes (1970–2012); World Meteorological Organization: Geneva, Switzerland, 2014; ISBN 978-92-63-11123-4. Available online: https://library.wmo.int/idurl/4/57564 (accessed on 22 August 2024).
- Ballester, J.; Quijal-Zamorano, M.; Méndez Turrubiates, R.F.; Pegenaute, F.; Herrmann, F.R.; Robine, J.M.; Basagaña, X.; Tonne, C.; Antó, J.M.; Achebak, H. Heat-related mortality in Europe during the summer of 2022. Nat. Med. 2023, 29, 1857–1866. [Google Scholar] [CrossRef] [PubMed]
- United Nations Secretary-General’s Call to Action on Extreme Heat. 25 July 2024. Available online: https://www.un.org/sites/un2.un.org/files/unsg_call_to_action_on_extreme_heat_for_release.pdf (accessed on 2 August 2024).
- Gabriel, K.M.A.; Endlicher, W.R. Urban and rural mortality rates during heatwaves in Berlin and Brandenburg, Germany. Environ. Poll. 2011, 159, 2044–2050. [Google Scholar] [CrossRef] [PubMed]
- Dousset, B.; Gourmelon, F.; Laaidi, K.; Zeghnoun, A.; Giraudet, E.; Bretin, P.; Maurid, E.; Vandentorren, S. Satellite monitoring of summer heatwaves in the Paris metropolitan area. Int. J. Climatol. 2011, 31, 313–323. [Google Scholar] [CrossRef]
- Huang, W.T.K.; Masselot, P.; Bou-Zeid, E.; Fatichi, S.; Paschalis, A.; Sun, T.; Gasparrini, A.; Manoli, G. Economic valuation of temperature-related mortality attributed to urban heat islands in European cities. Nat. Commun. 2023, 14, 7438. [Google Scholar] [CrossRef]
- Wouters, H.; De Ridder, K.; Poelmans, L.; Willems, P.; Brouwers, J.; Hosseinzadehtalaei, P.; Tabari, H.; Vanden Broucke, S.; van Lipzig, N.P.M.; Demuzere, M. Heat stress increase under climate change twice as large in cities as in rural areas: A study for a densely populated midlatitude maritime region. Geophys. Res. Lett. 2017, 44, 8997–9007. [Google Scholar] [CrossRef]
- De Ridder, K.; Maiheu, B.; Lauwaet, D.; Daglis, I.A.; Keramitsoglou, I.; Kourtidis, K.; Manunta, P.; Paganini, M. Urban Heat Island Intensification during Hot Spells—The Case of Paris during the Summer of 2003. Urban Sci. 2017, 1, 3. [Google Scholar] [CrossRef]
- Keller, R.C. Fatal Isolation: The Devastating Paris Heatwave of 2003; University of Chicago Press: Chicago, IL, USA, 2015; 240p. [Google Scholar]
- Toulemon, L.; Barbieri, M. The mortality impact of the August 2003 heatwave in France: Investigating the ‘harvesting’ effect and other long-term consequences. Popul. Stud. 2008, 62, 39–53. [Google Scholar] [CrossRef]
- Bosello, F.; Schechter, M. Integrated socio-economic assessment. In Regional Assessment of Climate Change in the Medi-Terranean. Vol. 2: Agriculture, Forests, Ecosystem Services and People; Navarra, A., Tubiana, L., Eds.; Springer: Berlin/Heidelberg, Germany, 2013; 402p. [Google Scholar]
- Sánchez-Martínez, G.; Williams, E.; Yu, S.S. The economics of health damage and adaptation to climate change in Europe: A review of the conventional and grey literature. Climate 2015, 3, 522–541. [Google Scholar] [CrossRef]
- OECD. Mortality Risk Valuation in Environment, Health and Transport Policies; OECD Publishing: Paris, France, 2012. [Google Scholar] [CrossRef]
- Ciscar, J.C.; Rising, J.; Kopp, R.E.; Feyen, L. Assessing future climate change impacts in the EU and the USA: Insights and lessons from two continental-scale projects. Environ. Res. Lett. 2019, 14, 084010. [Google Scholar] [CrossRef]
- Ščasný, M.; Alberini, A. Valuation of Mortality Risk Attributable to Climate Change: Investigating the Effect of Survey Administration Modes on a VSL. Int. J. Environ. Res. Public Health 2012, 9, 4760–4781. [Google Scholar] [CrossRef] [PubMed]
- Adélaïde, L.; Chanel, O.; Pascal, M. Health effects from heat waves in France: An economic evaluation. Eur. J. Health Econ. 2022, 23, 119–131. [Google Scholar] [CrossRef] [PubMed]
- Szewczyk, W.; Feyen, L.; Matei, A.; Ciscar, J.C.; Mulholland, E.; Soria, A. Economic Analysis of Selected Climate Impacts; EUR 30199 EN; Publications Office of the European Union: Luxembourg, 2020; Available online: https://data.europa.eu/doi/10.2760/845605 (accessed on 22 August 2024).
- Forzieri, G.; Cescatti, A.; Batista e Silva, F.; Feyen, L. Increasing risk over time of weather-related hazards to the European population: A data-driven prognostic study. Lancet Planet. Health 2017, 1, e200–e208. [Google Scholar] [CrossRef]
- World Health Organization. Care for Vulnerable Population Groups: Updated Evidence on Risk Factors and Vulnerability in Heat and Health in the WHO European Region: Updated Evidence for Effective Prevention; Sánchez-Martínez, G., de’Donato, F., Kendrovski, V., Eds.; World Health Organization: Copenhagen, Denmark, 2021; pp. 97–120. Available online: https://iris.who.int/bitstream/handle/10665/339462/9789289055406-eng.pdf (accessed on 22 August 2024).
- Vandresse, M. Belgium—Excess Mortality in 2020: 124,000 Years of Life Lost (Federal Planning Bureau Fact Sheet No. 5). 2021. Available online: https://www.plan.be/uploaded/documents/202105100808300.FACTSHEET_005_DEMO_12407_E.pdf (accessed on 27 June 2024).
- Shapiro, D.; MacDonald, D.; Greenlaw, S.A. Principles of Economics, 3rd ed.; OpenStax Rice University, 2022; Available online: https://openstax.org/details/books/principles-economics-3e (accessed on 22 August 2024).
- National Bank of Belgium. National Accounts—Quarterly and Annual Aggregates. 2023. Available online: https://stat.nbb.be/ (accessed on 27 June 2024).
- European Union. European System of Accounts (ESA 2010). Eurostat, Manual and Guidelines. 2013. Available online: https://doi.org/10.2785/16644 (accessed on 30 July 2024).
- Renard, F.; Scohy, A.; Van der Heyden, J.; Peeters, I.; Dequeker, S.; Vandael, E.; Van Goethem, N.; Dubourg, D.; De Viron, L.; Kongs, A.; et al. Establishing an ad hoc COVID-19 mortality surveillance during the first epidemic wave in Belgium, 1 March to 21 June 2020. Eurosurveillance 2021, 26, 2001402. [Google Scholar] [CrossRef]
- Bustos Sierra, N.; Bossuyt, N.; Braeye, T.; Leroy, M.; Moyersoen, I.; Peeters, I.; Scohy, A.; Van der Heyden, J.; Van Oyen, H. All-cause mortality supports the COVID-19 mortality in Belgium and comparison with major fatal events of the last century. Arch. Public Health 2020, 78, 117. [Google Scholar] [CrossRef]
- Luyten, J.; Schokkaert, E. Belgium’s response to the COVID-19 pandemic. Health Econ. Policy Law 2021, 17, 37–47. [Google Scholar] [CrossRef]
- Molenberghs, G.; Faes, C.; Verbeeck, J.; Deboosere, P.; Abrams, S.; Willem, L.; Aerts, J.; Theeten, H.; Devleesschauwer, B.; Bustos Sierra, N.; et al. COVID-19 mortality, excess mortality, deaths per million and infection fatality ratio, Belgium, 9 March 2020 to 28 June 2020. Eurosurveillance 2022, 27, 2002060. [Google Scholar] [CrossRef] [PubMed]
- COVID-19 Excess Mortality Collaborators. Estimating excess mortality due to the COVID-19 pandemic: A systematic analysis of COVID-19-related mortality, 2020–2021. Lancet 2022, 399, 1513–1536. [Google Scholar] [CrossRef]
- Belgium COVID-19 Epidemiological Situation—Deaths. Belgium COVID-19 Dashboard, Sciensano. (Right-Click on the Graph ‘Daily New Deaths’ and Select ‘Export’ to Download a Csv File Containing the Data). Available online: https://lookerstudio.google.com/embed/reporting/c14a5cfc-cab7-4812-848c-0369173148ab/page/QTSKB (accessed on 1 August 2024).
- De Visscher, A. The COVID-19 pandemic: Model-based evaluation of non-pharmaceutical interventions and prognoses. Nonlinear Dyn. 2020, 101, 1871–1887. [Google Scholar] [CrossRef]
- Abrams, S.; Wambua, J.; Santermans, E.; Willem, L.; Kuylen, E.; Coletti, P.; Libin, P.; Faes, C.; Petrof, O.; Herzog, S.A.; et al. Modelling the early phase of the Belgian COVID-19 epidemic using a stochastic compartmental model and studying its implied future trajectories. Epidemics 2021, 35, 100449. [Google Scholar] [CrossRef]
- COVID-19 Forecasting Team. Variation in the COVID-19 infection-fatality ratio by age, time, and geography during the pre-vaccine era: A systematic analysis. Lancet 2022, 399, 1469–1488. [Google Scholar] [CrossRef] [PubMed]
- Flaxman, S.; Mishra, S.; Gandy, A.; Unwin, H.J.T.; Mellan, T.A.; Coupland, H.; Whittaker, C.; Zhu, H.; Berah, T.; Eaton, J.W.; et al. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature 2020, 584, 257–261. [Google Scholar] [CrossRef]
- Jamison, J.C.; Bundy, D.; Jamison, D.T.; Spitz, J.; Verguet, S. Comparing the impact on COVID-19 mortality of self-imposed behavior change and of government regulations across 13 countries. Health Serv. Res. 2021, 56, 874–884. [Google Scholar] [CrossRef]
- Lison, A.; Banholzer, N.; Sharma, M.; Mindermann, S.; Unwin, H.J.T.; Mishra, S.; Stadler, T.; Bhatt, S.; Ferguson, N.M.; Brauner, J.; et al. Effectiveness assessment of non-pharmaceutical interventions: Lessons learned from the COVID-19 pandemic. Lancet Public Health 2023, 8, e311–e317. [Google Scholar] [CrossRef]
- Agyapon-Ntra, K.; McSharry, P.E. A global analysis of the effectiveness of policy re-sponses to COVID-19. Sci. Rep. 2023, 13, 5629. [Google Scholar] [CrossRef] [PubMed]
- Fisman, D.N.; Greer, A.L.; Tuite, A.R. Bidirectional impact of imperfect mask use on reproduction number of COVID-19: A next generation matrix approach. Infect. Dis. Model. 2020, 5, 405–408. [Google Scholar] [CrossRef]
- Molenberghs, G.; Buyse, M.; Abrams, S.; Hens, N.; Beutels, P.; Faes, C.; Verbeke, G.; Van Damme, P.; Goossens, H.; Neyens, T.; et al. Infectious diseases epidemiology, quantitative methodology, and clinical research in the midst of the COVID-19 pandemic: Perspective from a European country. Contemp. Clin. Trials 2020, 99, 106189. [Google Scholar] [CrossRef]
- Desaigues, B.; Ami, D.; Bartczak, A.; Braun-Kohlová, M.; Chilton, S.; Czajkowski, M.; Farreras, V.; Hunt, A.; Hutchison, M.; Jeanrenaud, C.; et al. Economic valuation of air pollution mortality: A 9-country contingent valuation survey of value of a life year (VOLY). Ecol. Indic. 2011, 11, 902–910. [Google Scholar] [CrossRef]
- Botzen, W.J.W.; Martinius, M.L.; Bröde, P.; Folkerts, M.A.; Ignjacevic, P.; Estrada, F.; Harmsen, C.N.; Daanen, H.A.M. Economic valuation of climate change–induced mortality: Age dependent cold and heat mortality in the Netherlands. Clim. Chang. 2020, 162, 545–562. [Google Scholar] [CrossRef]
- Chiabai, A.; Spadaro, J.V.; Neumann, M.B. Valuing deaths or years of life lost? Economic benefits of avoided mortality from early heat warning systems. Mitig. Adapt. Strateg. Glob. Chang. 2018, 23, 1159–1176. [Google Scholar] [CrossRef]
- Ignjačević, P.; Botzen, W.; Estrada, F.; Daanen, H.; Lupi, V. Climate-induced mortality projections in Europe: Estimation and valuation of heat-related deaths. Int. J. Disaster Risk Reduct. 2024, 111, 104692. [Google Scholar] [CrossRef]
- WHO. 2021 WHO Health and Climate Change Global Survey Report; World Health Organization: Geneva, Switzerland, 2021; 92p, Available online: https://www.who.int/publications/i/item/9789240038509 (accessed on 22 August 2024).
- Fouillet, A.; Rey, G.; Wagner, V.; Laaidi, K.; Empereur-Bissonnet, P.; Le Tertre, A.; Frayssinet, P.; Bessemoulin, P.; Laurent, F.; De Crouy-Chanel, P.; et al. Has the impact of heat waves on mortality changed in France since the European heat wave of summer 2003? A study of the 2006 heat wave. Int. J. Epidemiol. 2008, 37, 309–317. [Google Scholar] [CrossRef] [PubMed]
- Gallo, E.; Quijal-Zamorano, M.; Méndez Turrubiates, R.F.; Tonne, C.; Basagaña, X.; Achebak, H.; Ballester, J. Heat-related mortality in Europe during 2023 and the role of adaptation in protecting health. Nat. Med. 2024. [Google Scholar] [CrossRef]
- Vargo, J.; Stone, B.; Habeeb, D.; Liu, P.; Russell, A. The social and spatial distribution of temperature-related health impacts from urban heat island reduction policies. Environ. Sci. Policy 2016, 66, 366–374. [Google Scholar] [CrossRef]
- Johnson, D.; See, L.; Oswald, S.M.; Prokop, G.; Krisztin, T. A cost–benefit analysis of implementing urban heat island adaptation measures in small- and medium-sized cities in Austria. Environ. Plan. B Urban Anal. City Sci. 2021, 48, 2326–2345. [Google Scholar] [CrossRef]
- Iungman, T.; Cirach, M.; Marando, F.; Barboza, E.P.; Khomenko, S.; Masselot, P.; Quijal-Zamorano, M.; Mueller, N.; Gasparrini, A.; Urquiza, J.; et al. Cooling cities through urban green infrastructure: A health impact assessment of European cities. Lancet 2023, 401, 577–589. [Google Scholar] [CrossRef]
- Lauwaet, D.; Berckmans, J.; Hooyberghs, H.; Wouters, H.; Driesen, G.; Lefebre, F.; De Ridder, K. High resolution modelling of the urban heat island of 100 European cities. Urban Clim. 2024, 54, 101850. [Google Scholar] [CrossRef]
- Robinson, L.A.; Hammitt, J.K.; Chang, A.Y.; Resch, S. Understanding and improving the one-and-three- times GDP per capita cost-effectiveness thresholds. Health Policy Plan 2017, 32, 141–145. [Google Scholar] [CrossRef] [PubMed]



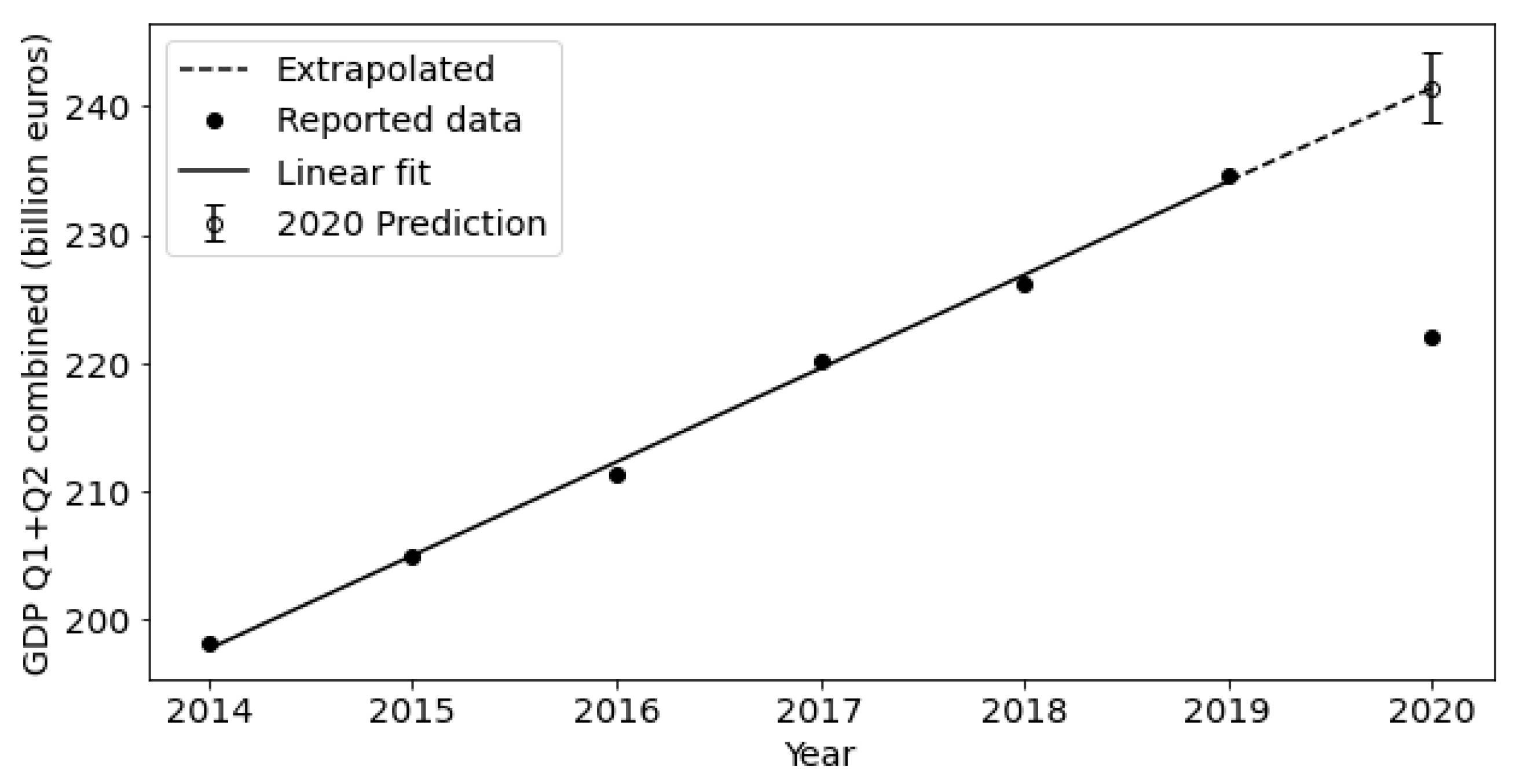
| 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | |
|---|---|---|---|---|---|---|---|
| Q1 | 97.1 | 100.1 | 102.4 | 107.7 | 110.3 | 114.7 | 116.3 |
| Q2 | 101.0 | 104.9 | 108.9 | 112.5 | 116.0 | 119.9 | 105.7 |
| Q1 + Q2 | 198.2 | 205.0 | 211.3 | 220.2 | 226.3 | 234.6 | 222.0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Ridder, K. Assessing the Value of a Human Life in Heat-Related Mortality: Lessons from COVID-19 in Belgium. Climate 2024, 12, 129. https://doi.org/10.3390/cli12090129
De Ridder K. Assessing the Value of a Human Life in Heat-Related Mortality: Lessons from COVID-19 in Belgium. Climate. 2024; 12(9):129. https://doi.org/10.3390/cli12090129
Chicago/Turabian StyleDe Ridder, Koen. 2024. "Assessing the Value of a Human Life in Heat-Related Mortality: Lessons from COVID-19 in Belgium" Climate 12, no. 9: 129. https://doi.org/10.3390/cli12090129
APA StyleDe Ridder, K. (2024). Assessing the Value of a Human Life in Heat-Related Mortality: Lessons from COVID-19 in Belgium. Climate, 12(9), 129. https://doi.org/10.3390/cli12090129




