Clean Air Benefits and Climate Penalty: A Health Impact Analysis of Mortality Trends in the Mid-South Region, USA
Abstract
1. Introduction
2. Methods
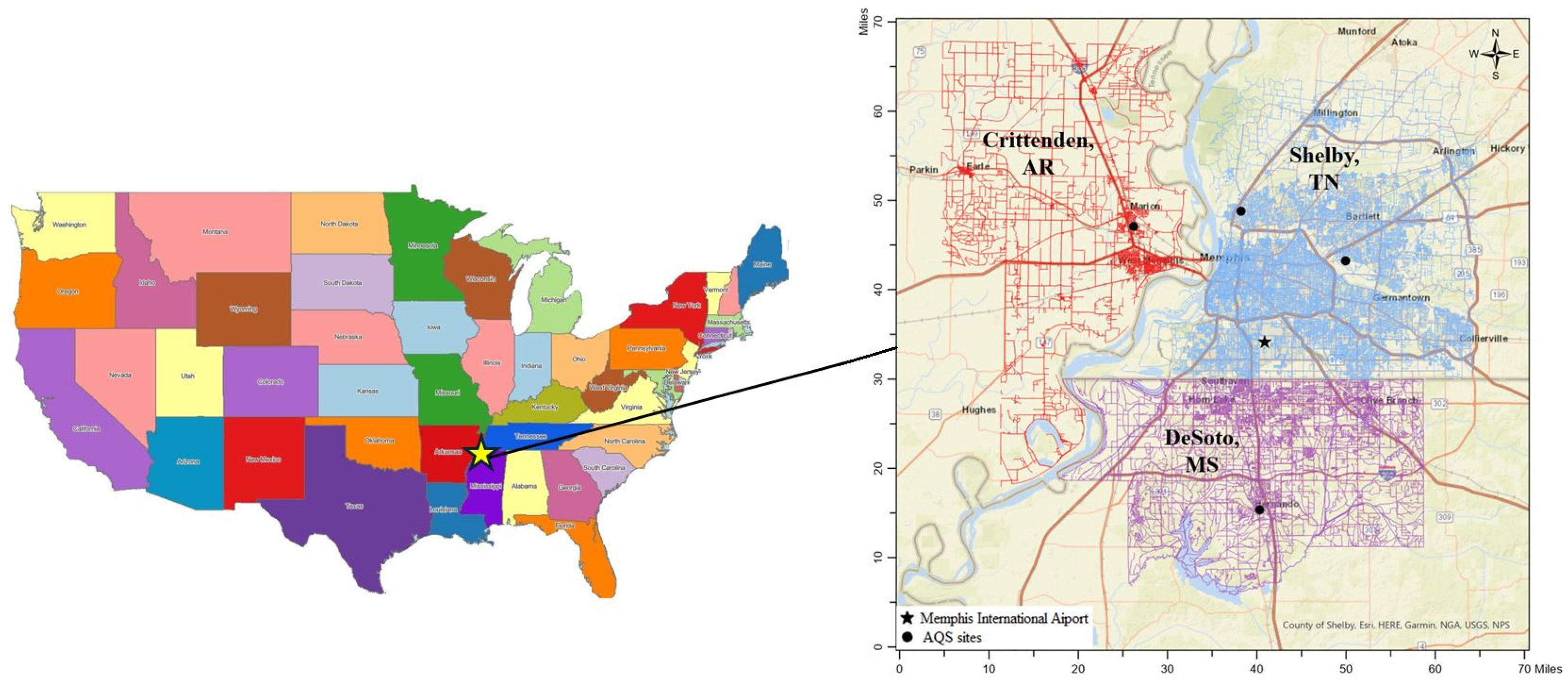
2.1. Study Area
2.2. Vital and Environmental Data
2.3. Trend Analysis
2.4. Impacts of Environmental Factors on Mortality
3. Results
3.1. Trends in Air Pollution and Temperature
3.2. All-Cause and Environment-Related Mortality Rates
3.3. Contributions of Environmental Factors to MR Changes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Manisalidis, I.; Stavropoulou, E.; Stavropoulos, A.; Bezirtzoglou, E. Environmental and Health Impacts of Air Pollution: A Review. Front. Public Health 2020, 8, 14. [Google Scholar] [CrossRef] [PubMed]
- USEPA. Our Nation’s Air: Trends Through 2022; U.S. Environmental Protection Agency: Washington, DC, USA, 2023.
- Pope, C.A.; Ezzati, M.; Dockery, D.W. Fine-Particulate Air Pollution and Life Expectancy in the United States. N. Engl. J. Med. 2009, 360, 376–386. [Google Scholar] [CrossRef]
- Correia, A.W.; Pope, C.A., 3rd; Dockery, D.W.; Wang, Y.; Ezzati, M.; Dominici, F. Effect of air pollution control on life expectancy in the United States: An analysis of 545 U.S. counties for the period from 2000 to 2007. Epidemiology 2013, 24, 23–31. [Google Scholar] [CrossRef] [PubMed]
- Cromar, K.R.; Gladson, L.A.; Ewart, G. Trends in Excess Morbidity and Mortality Associated with Air Pollution above American Thoracic Society-Recommended Standards, 2008–2017. Ann. Am. Thorac. Soc. 2019, 16, 836–845. [Google Scholar] [CrossRef] [PubMed]
- Wong, E.Y.; Gohlke, J.; Griffith, W.C.; Farrow, S.; Faustman, E.M. Assessing the health benefits of air pollution reduction for children. Environ. Health Perspect. 2004, 112, 226–232. [Google Scholar] [CrossRef] [PubMed]
- Gauderman, W.J.; Urman, R.; Avol, E.; Berhane, K.; McConnell, R.; Rappaport, E.; Chang, R.; Lurmann, F.; Gilliland, F. Association of improved air quality with lung development in children. N. Engl. J. Med. 2015, 372, 905–913. [Google Scholar] [CrossRef]
- Garcia, E.; Berhane, K.T.; Islam, T.; McConnell, R.; Urman, R.; Chen, Z.; Gilliland, F.D. Association of Changes in Air Quality with Incident Asthma in Children in California, 1993–2014. JAMA J. Am. Med. Assoc. 2019, 321, 1906–1915. [Google Scholar] [CrossRef]
- Schraufnagel, D.E.; Balmes, J.R.; de Matteis, S.; Hoffman, B.; Kim, W.J.; Perez-Padilla, R.; Rice, M.; Sood, A.; Vanker, A.; Wuebbles, D.J. Health benefits of air pollution reduction. Ann. Am. Thorac. Soc. 2019, 16, 1478–1487. [Google Scholar] [CrossRef] [PubMed]
- Ye, T.; Guo, S.; Xie, Y.; Chen, Z.; Abramson, M.J.; Heyworth, J.; Hales, S.; Woodward, A.; Bell, M.; Guo, Y.; et al. Health and related economic benefits associated with reduction in air pollution during COVID-19 outbreak in 367 cities in China. Ecotoxicol. Environ. Saf. 2021, 222, 112481. [Google Scholar] [CrossRef]
- USEPA. Climate Change Indicators: Heat Waves; U.S. Environmental Protection Agency: Washington, DC, USA, 2023.
- Wu, S.; Mickley, L.J.; Leibensperger, E.M.; Jacob, D.J.; Rind, D.; Streets, D.G. Effects of 2000–2050 global change on ozone air quality in the United States. J. Geophys. Res. Atmos. 2008, 113, 112481. [Google Scholar] [CrossRef]
- Jacob, D.J.; Winner, D.A. Effect of climate change on air quality. Atmos. Environ. 2009, 43, 51–63. [Google Scholar] [CrossRef]
- Hedegaard, G.B.; Christensen, J.H.; Brandt, J. The relative importance of impacts from climate change vs. emissions change on air pollution levels in the 21st century. Atmos. Chem. Phys. 2013, 13, 3569–3585. [Google Scholar] [CrossRef]
- Fu, T.-M.; Tian, H. Climate Change Penalty to Ozone Air Quality: Review of Current Understandings and Knowledge Gaps. Curr. Pollut. Rep. 2019, 5, 159–171. [Google Scholar] [CrossRef]
- Shen, L.; Mickley, L.J.; Murray, L.T. Influence of 2000–2050 climate change on particulate matter in the United States: Results from a new statistical model. Atmos. Chem. Phys. 2017, 17, 4355–4367. [Google Scholar] [CrossRef]
- Shi, L.; Liu, P.; Zanobetti, A.; Schwartz, J. Climate Penalty: Climate-driven increases in ozone and PM2.5 levels and mortality. Environ. Epidemiol. 2019, 3, 365. [Google Scholar] [CrossRef]
- Chen, K.; Vicedo-Cabrera, A.M.; Dubrow, R. Projections of Ambient Temperature- and Air Pollution-Related Mortality Burden Under Combined Climate Change and Population Aging Scenarios: A Review. Curr. Environ. Health Rep. 2020, 7, 243–255. [Google Scholar] [CrossRef] [PubMed]
- Limaye, V.S.; Vargo, J.; Harkey, M.; Holloway, T.; Patz, J.A. Climate change and heat-related excess mortality in the eastern USA. EcoHealth 2018, 15, 485–496. [Google Scholar] [CrossRef] [PubMed]
- Neumann, J.E.; Amend, M.; Anenberg, S.; Kinney, P.L.; Sarofim, M.; Martinich, J.; Lukens, J.; Xu, J.W.; Roman, H. Estimating PM2.5-related premature mortality and morbidity associated with future wildfire emissions in the western US. Environ. Res. Lett. 2021, 16, 035019. [Google Scholar] [CrossRef]
- Wilson, A.; Reich, B.J.; Nolte, C.G.; Spero, T.L.; Hubbell, B.; Rappold, A.G. Climate change impacts on projections of excess mortality at 2030 using spatially varying ozone-temperature risk surfaces. J. Expo. Sci. Environ. Epidemiol. 2017, 27, 118–124. [Google Scholar] [CrossRef]
- Zhang, Y.; Smith, S.J.; Bowden, J.H.; Adelman, Z.; West, J.J. Co-benefits of global, domestic, and sectoral greenhouse gas mitigation for US air quality and human health in 2050. Environ. Res. Lett. 2017, 12, 114033. [Google Scholar] [CrossRef]
- Sacks, J.D.; Fann, N.; Gumy, S.; Kim, I.; Ruggeri, G.; Mudu, P. Quantifying the public health benefits of reducing air pollution: Critically assessing the features and capabilities of WHO’s AirQ+ and U.S. EPA’s environmental benefits mapping and analysis program-community edition (BenMAP-CE). Atmosphere 2020, 11, 516. [Google Scholar] [CrossRef]
- Curtin, S.; Spencer, M.R. Trends in Death Rates in Urban and Rural Areas: United States, 1999–2019; National Center for Health Statistics: Hyattsville, MD, USA, 2021.
- Commane, R.; Schiferl, L.D. Climate mitigation policies for cities must consider air quality impacts. Chem 2022, 8, 910–923. [Google Scholar] [CrossRef]
- Castillo, M.D.; Anenberg, S.C.; Chafe, Z.A.; Huxley, R.; Johnson, L.S.; Kheirbek, I.; Malik, M.; Marshall, J.D.; Naidoo, S.; Nelson, M.L.; et al. Quantifying the Health Benefits of Urban Climate Mitigation Actions: Current State of the Epidemiological Evidence and Application in Health Impact Assessments. Front. Sustain. Cities 2021, 3, 768227. [Google Scholar] [CrossRef]
- CDC. CDC WONDER Online Databases; U.S. Centers for Disease Control and Prevention: Atlanta, GA, USA. Available online: https://wonder.cdc.gov/ (accessed on 23 May 2023).
- Chen, J.; Hoek, G. Long-term exposure to PM and all-cause and cause-specific mortality: A systematic review and meta-analysis. Environ. Int. 2020, 143, 105974. [Google Scholar] [CrossRef]
- Turner, M.C.; Jerrett, M.; Pope III, C.A.; Krewski, D.; Gapstur, S.M.; Diver, W.R.; Beckerman, B.S.; Marshall, J.D.; Su, J.; Crouse, D.L. Long-term ozone exposure and mortality in a large prospective study. Am. J. Respir. Crit. Care Med. 2016, 193, 1134–1142. [Google Scholar] [CrossRef] [PubMed]
- Zanobetti, A.; Schwartz, J. Temperature and mortality in nine US cities. Epidemiology 2008, 19, 563. [Google Scholar] [CrossRef]
- Voorhees, A.S.; Fann, N.; Fulcher, C.; Dolwick, P.; Hubbell, B.; Bierwagen, B.; Morefield, P. Climate change-related temperature impacts on warm season heat mortality: A proof-of-concept methodology using BenMAP. Environ. Sci. Technol. 2011, 45, 1450–1457. [Google Scholar] [CrossRef] [PubMed]
- CDC. Age Adjustment. Available online: https://www.cdc.gov/nchs/hus/sources-definitions/age-adjustment.htm (accessed on 22 January, 2025).
- CDC. Compressed Mortality File. Available online: https://wonder.cdc.gov/wonder/help/cmf.html#Age-Adjusted%20Rates (accessed on 10 February, 2025).
- Wyatt, L.H.; Peterson, G.C.L.; Wade, T.J.; Neas, L.M.; Rappold, A.G. The contribution of improved air quality to reduced cardiovascular mortality: Declines in socioeconomic differences over time. Environ. Int. 2020, 136, 105430. [Google Scholar] [CrossRef] [PubMed]
- USEPA. Air Quality System; U.S. Environmental Protection Agency: Washington, DC, USA. Available online: https://aqs.epa.gov/aqsweb/airdata/download_files.html (accessed on 22 May 2023).
- Jia, C.; Fu, X.; Bartelli, D.; Smith, L. Insignificant Impact of the “Stay-At-Home” Order on Ambient Air Quality in the Memphis Metropolitan Area, U.S.A. Atmosphere 2020, 11, 630. [Google Scholar] [CrossRef]
- NOAA. Data Tools: Local Climatological Data (LCD); National Oceanic and Atmospheric Administration: Washington, DC, USA. Available online: https://www.ncdc.noaa.gov/cdo-web/datatools/lcd (accessed on 22 May 2023).
- Madrigano, J.; Jack, D.; Anderson, G.B.; Bell, M.L.; Kinney, P.L. Temperature, ozone, and mortality in urban and non-urban counties in the northeastern United States. Environ. Health 2015, 14. [Google Scholar] [CrossRef]
- Nordio, F.; Zanobetti, A.; Colicino, E.; Kloog, I.; Schwartz, J. Changing patterns of the temperature-mortality association by time and location in the US, and implications for climate change. Environ. Int. 2015, 81, 80–86. [Google Scholar] [CrossRef] [PubMed]
- USEPA. Estimating PM2.5- and Ozone-Attributable Health Benefits; U.S. Environmental Protection Agency: Research Triangle Park, NC, USA, 2023.
- WHO. WHO Global Air Quality Guidelines: Particulate Matter (PM2.5 and PM10), Ozone, Nitrogen Dioxide, Sulfur Dioxide and Carbon Monoxide; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Anderson, B.G.; Bell, M.L. Weather-Related Mortality: How Heat, Cold, and Heat Waves Affect Mortality in the United States. Epidemiology 2009, 20, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Ren, T.; Kinney, P.L.; Joyner, A.; Zhang, W. Projecting future climate change impacts on heat-related mortality in large urban areas in China. Environ. Res. 2018, 163, 171–185. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Akkus, C.; Yu, X.; Joyner, A.; Kmet, J.; Sweat, D.; Jia, C. Heatwave events and mortality outcomes in Memphis, Tennessee: Testing effect modification by socioeconomic status and urbanicity. Int. J. Environ. Res. Public Health 2019, 16, 4568. [Google Scholar] [CrossRef]
- GBD 2017 Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1923–1994. [Google Scholar] [CrossRef]
- Mokdad, A.H.; Marks, J.S.; Stroup, D.F.; Gerberding, J.L. Actual causes of death in the United States, 2000. JAMA 2004, 291, 1238–1245. [Google Scholar] [CrossRef]
- The US Burden of Disease Collaborators. The State of US Health, 1990-2016: Burden of Diseases, Injuries, and Risk Factors Among US States. JAMA 2018, 319, 1444–1472. [Google Scholar] [CrossRef]
- Thun, M.J.; Jemal, A. How much of the decrease in cancer death rates in the United States is attributable to reductions in tobacco smoking? Tob. Control 2006, 15, 345–347. [Google Scholar] [CrossRef] [PubMed]
- Bowe, B.; Xie, Y.; Yan, Y.; Al-Aly, Z. Burden of Cause-Specific Mortality Associated With PM2.5 Air Pollution in the United States. JAMA Netw. Open 2019, 2, e1915834. [Google Scholar] [CrossRef]
- Wang, J.; Xing, J.; Mathur, R.; Pleim, J.E.; Wang, S.; Hogrefe, C.; Gan, C.-M.; Wong, D.C.; Hao, J. Historical Trends in PM2.5-Related Premature Mortality during 1990-2010 across the Northern Hemisphere. Environ. Health Perspect. 2017, 125, 400–408. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Jason West, J.; Mathur, R.; Xing, J.; Hogrefe, C.; Roselle, S.J.; Bash, J.O.; Pleim, J.E.; Gan, C.M.; Wong, D.C. Long-term trends in the ambient PM2.5- and O3-related mortality burdens in the United States under emission reductions from 1990 to 2010. Atmos. Chem. Phys. 2018, 18, 15003–15016. [Google Scholar] [CrossRef] [PubMed]
- Castillo, M.D.; Kinney, P.L.; Southerland, V.; Arno, C.A.; Crawford, K.; van Donkelaar, A.; Hammer, M.; Martin, R.V.; Anenberg, S.C. Estimating Intra-Urban Inequities in PM2.5-Attributable Health Impacts: A Case Study for Washington, DC. GeoHealth 2021, 5, e2021GH000431. [Google Scholar] [CrossRef] [PubMed]
- Chalbot, M.C.G.; Jones, T.A.; Kavouras, I.G. Trends of non-accidental, cardiovascular, stroke and lung cancer mortality in Arkansas are associated with ambient PM2.5 reductions. Int. J. Environ. Res. Public Health 2014, 11, 7442–7455. [Google Scholar] [CrossRef] [PubMed]
- Vodonos, A.; Schwartz, J. Estimation of excess mortality due to long-term exposure to PM2.5 in continental United States using a high-spatiotemporal resolution model. Environ. Res. 2021, 196, 110904. [Google Scholar] [CrossRef] [PubMed]
- Bobb, J.F.; Peng, R.D.; Bell, M.L.; Dominici, F. Heat-related mortality and adaptation to heat in the United States. Environ. Health Perspect. 2014, 122, 811–816. [Google Scholar] [CrossRef]
- Requia, W.J.; Coull, B.A.; Koutrakis, P. Where air quality has been impacted by weather changes in the United States over the last 30 years? Atmos. Environ. 2020, 224, 117360. [Google Scholar] [CrossRef]
- Bell, M.L.; Goldberg, R.; Hogrefe, C.; Kinney, P.L.; Knowlton, K.; Lynn, B.; Rosenthal, J.; Rosenzweig, C.; Patz, J.A. Climate change, ambient ozone, and health in 50 US cities. Clim. Change 2007, 82, 61–76. [Google Scholar] [CrossRef]
- Yin, L.; Bai, B.; Zhang, B.; Zhu, Q.; Di, Q.; Requia, W.J.; Schwartz, J.D.; Shi, L.; Liu, P. Climate Penalty on Air Pollution Abated by Anthropogenic Emission Reductions in the United States. Res. Sq. 2023, preprint. [Google Scholar] [CrossRef]
- Sheridan, S.C.; Kalkstein, A.J. Seasonal variability in heat-related mortality across the United States. Nat. Hazards 2010, 55, 291–305. [Google Scholar] [CrossRef]
- Wang, H.; Naghavi, M.; Allen, C.; Barber, R.M.; Bhutta, Z.A.; Carter, A.; Casey, D.C.; Charlson, F.J.; Chen, A.Z.; Coates, M.M.; et al. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1459–1544. [Google Scholar] [CrossRef] [PubMed]
- Barreca, A.; Clay, K.; Deschenes, O.; Greenstone, M.; Shapiro, J.S. Adapting to climate change: The remarkable decline in the US temperature-mortality relationship over the Twentieth Century. J. Political Econ. 2016, 124, 105–159. [Google Scholar] [CrossRef]
- Stafoggia, M.; Michelozzi, P.; Schneider, A.; Armstrong, B.; Scortichini, M.; Rai, M.; Achilleos, S.; Alahmad, B.; Analitis, A.; Åström, C.; et al. Joint effect of heat and air pollution on mortality in 620 cities of 36 countries. Environ. Int. 2023, 181, 108258. [Google Scholar] [CrossRef]
- Ma, Y.; Zang, E.; Opara, I.; Lu, Y.; Krumholz, H.M.; Chen, K. Racial/ethnic disparities in PM2.5-attributable cardiovascular mortality burden in the United States. Nat. Hum. Behav. 2023, 7, 2074–2083. [Google Scholar] [CrossRef] [PubMed]
- Garcia, M.C.; Faul, M.; Massetti, G.; Thomas, C.C.; Hong, Y.; Bauer, U.E.; Iademarco, M.F. Reducing potentially excess deaths from the five leading causes of death in the rural United States. MMWR Surveill. Summ. 2017, 66, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Odame, E.A.; Silver, K.; Zheng, S. Comparing Urban and Rural Vulnerability to Heat-Related Mortality: A Systematic Review and Meta-analysis. J. Glob. Epidemiol. Environ. Health 2017, 1, 9–15. [Google Scholar] [CrossRef]



| Environmental Parameter | Mortality | Relative Risk (95% Confidence Interval) | β (95% CI) | Source |
|---|---|---|---|---|
| PM2.5 1 | Natural-cause mortality, excluding accidents, suicides, and homicides | 1.08 (1.06, 1.09) per 10 µg/m3 | 0.0077 (0.0058, 0.0086) per 1 µg/m3 | [28] |
| Ozone 2 | All-cause mortality | 1.02 (1.01, 1.03) per 10 ppb | 0.00198 (0.0010, 0.0030) per 1 ppb | [29] |
| Temperature in the warm season 3 | All-cause mortality, excluding accidental deaths | 1.0009 (1.0000, 1.0018) per 1 °C 4 | 0.0009 (0.0000, 0.0018) per 1 °C | [42] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jia, C.; Zhang, H.; Batbaatar, N.; Naser, A.M.; Li, Y.; Kavouras, I. Clean Air Benefits and Climate Penalty: A Health Impact Analysis of Mortality Trends in the Mid-South Region, USA. Climate 2025, 13, 45. https://doi.org/10.3390/cli13030045
Jia C, Zhang H, Batbaatar N, Naser AM, Li Y, Kavouras I. Clean Air Benefits and Climate Penalty: A Health Impact Analysis of Mortality Trends in the Mid-South Region, USA. Climate. 2025; 13(3):45. https://doi.org/10.3390/cli13030045
Chicago/Turabian StyleJia, Chunrong, Hongmei Zhang, Namuun Batbaatar, Abu Mohd Naser, Ying Li, and Ilias Kavouras. 2025. "Clean Air Benefits and Climate Penalty: A Health Impact Analysis of Mortality Trends in the Mid-South Region, USA" Climate 13, no. 3: 45. https://doi.org/10.3390/cli13030045
APA StyleJia, C., Zhang, H., Batbaatar, N., Naser, A. M., Li, Y., & Kavouras, I. (2025). Clean Air Benefits and Climate Penalty: A Health Impact Analysis of Mortality Trends in the Mid-South Region, USA. Climate, 13(3), 45. https://doi.org/10.3390/cli13030045







