Impact of Illegible Prescriptions on Dispensing Practice: A Pilot Study of South African Pharmacy Personnel
Abstract
1. Introduction
2. Study Aims and Objectives
3. Materials and Methods
3.1. Ethics Approval
3.2. Study Design
3.3. Study Population and Sample Size
3.4. Data collection Tool
3.4.1. The Survey
- Part 1: Demographic Information
- Part 2: Accuracy of reading an illegible prescription. The online survey comprised five prescriptions with illegible handwriting, and from the responses obtained, it was determined how accurately participants were able to decipher the prescribers’ handwriting. The illegible prescriptions were obtained from a local community pharmacy, and the prescription instructions were verified with the respective prescribers. The survey entailed the interpretation of the prescription (Phase I of the dispensing process) by listing the medication(s) prescribed, date, abbreviations, quantity prescribed, dosage and dosage form, as these are mandatory and regulated by the Medicines and Related Substances Control Act (1965). Participants were allowed to select ‘unsure’ if they could not determine what was written.
- Part 3: Open-ended questions explored the challenges in dispensing an illegible prescription and concerns/views on its consequences.
Scoring System
3.4.2. Survey Dissemination and Study Procedure
3.5. Data Analysis
4. Results
4.1. Demographic Data
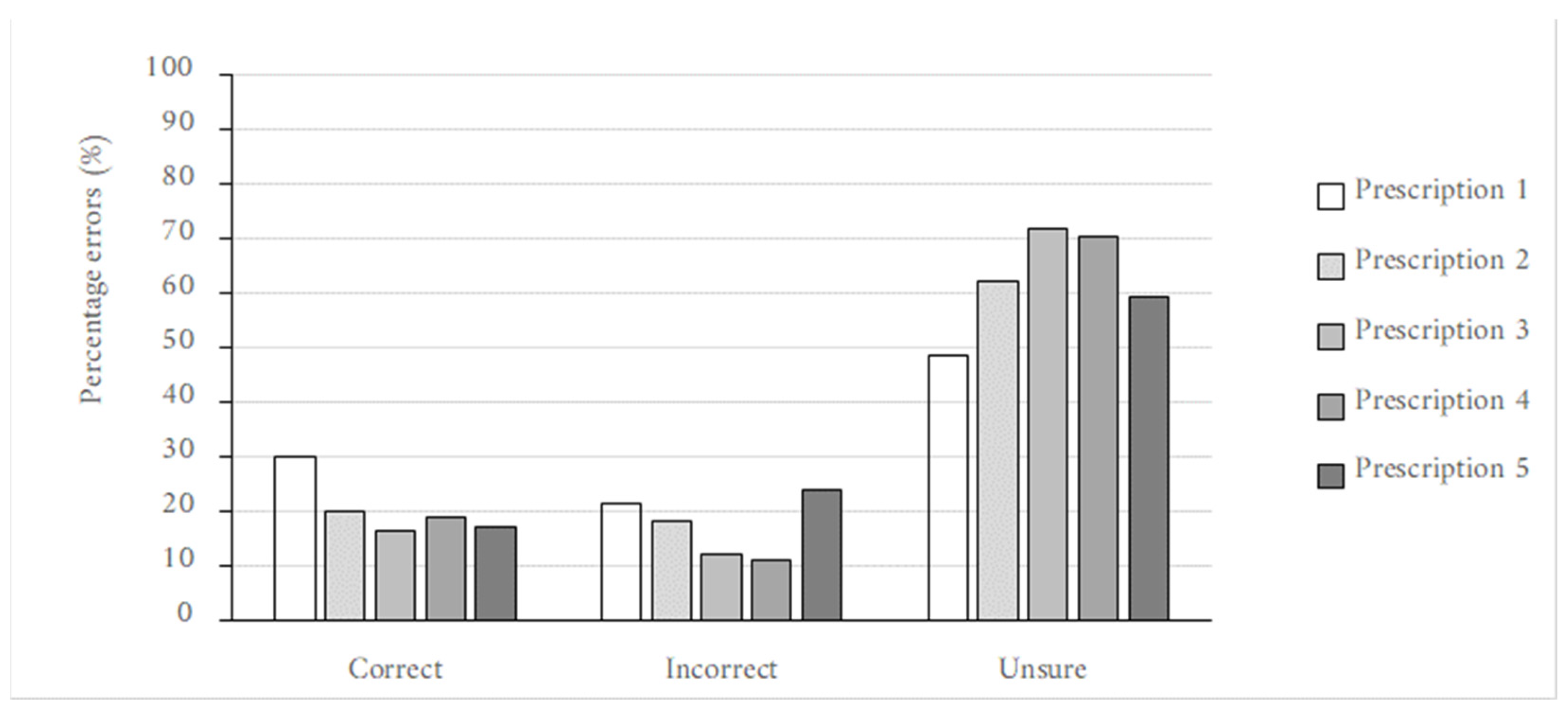
4.2. Prescription Reading Errors
4.3. Perceived Concerns and Challenges Encountered
4.3.1. How Pharmacy Personnel Deal with Illegible Prescriptions: Experiences
4.3.2. Patient Frustration Due to Illegible Prescriptions
4.4. Preferences of Pharmacy Personnel and Proposed Considerations
5. Discussion
A pharmacist assistant post-basic commented: “Identify other items to see if there is a pattern, i.e.,) pain script, antibiotic script. With an antibiotic script, you would expect to find a probiotic, cough mixture, antihistamine combination, nose spray and so on. Doctors also follow a prescribing style, so you get to know the doctors in the area and the combination of scripts they produce. So, they will always prescribe Augmentin with reuterina and flomist. So, you begin to recognize the patterns. That’s why unfamiliar doctor scripts are difficult to decipher.”
A pharmacist commented: “Yes. Patients start getting impatient that it’s taking ‘too long’. Also, patients lose faith in pharmacist abilities because it looks like we don’t know what we’re doing. Also, pharmacists get frustrated as well as often prescribers are not available to confirm, and patients must be sent back.”
A community service pharmacist commented: “Yes, because in the public sector doctors see a large number of patients so calling isn’t that efficient because he or she might have forgotten the patient and sending them is frustrating and time-consuming for the patient.”
A pharmacist intern commented: “In my opinion, it depends. If you get a bad prescription and you care about the patient’s health and well-being, you’ll call the prescriber to confirm. By doing this you’re offering a valuable service. Everything you do you should do it with quality, accuracy, and integrity. But then if you look at it from a time-consuming perspective, it does for sure affect the service delivery. That time you used to get hold of the doctor could’ve been time spent counselling the patient. You are probably wondering, “okay but you can counsel the patient afterwards”, yes well the queue in pharmacies gets pretty hectic and patients complain. But then again, those patients waiting in line doesn’t know the true value of this profession, which is not their fault. It’s 100% our fault. (I could go on and on and on about this one, but let me stop here)”.
A pharmacist intern commented: “it should start by the starting line: the doctor. So basically, have a mandatory typewritten prescription in place. I’m not an IT guru, but surely someone can develop some system in place to make things easier for both the doctor, nurses, and pharmacists. I am aware of the amount of patients doctors and nurses see a day, but surely there should be something out there”.
Limitations, Strengths and Interpretations of the Study
6. Conclusion and Study Recommendations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- South African Pharmacy Council. Pharmacists_Overview n.d. Available online: https://pharmcouncil.co.za/Pharmacists_Overview (accessed on 21 October 2021).
- South African Pharmacy Council. Pharmacy Act 53 of 1974 n.d. Available online: https://www.mm3admin.co.za/documents/docmanager/0C43CA52-121E-4F58-B8F6-81F656F2FD17/00010723.pdf (accessed on 21 October 2021).
- South African Pharmacy Council. GNR.1158 of 20 November 2000: Regulation relating to the practice of pharmacy n.d. Available online: https://www.mm3admin.co.za/documents/docmanager/0C43CA52-121E-4F58-B8F6-81F656F2FD17/00010804.pdf (accessed on 21 October 2021).
- Juta’s Regulations of South Africa (as at 30 May 2008. Good Pharmacy Practice Manual and Associated SAPC Rules.pdf 2008. Available online: https://www.pharmcouncil.co.za/Media/Default/Documents/Rules%20published%20in%20terms%20of%20section%2035A%20of%20the%20Pharmacy%20Act%2053%20of%201974.pdf (accessed on 8 October 2022).
- Rossiter, D. University of Cape Town. Division of Clinical Pharmacology. South African Medicines Formulary, 12th ed.; Health and Medical Publising Group of the South African Medical Association: Cape Town, South Africa, 2016. [Google Scholar]
- Nkera-Gutabara, J.G.; Ragaven, L.B. Adherence to prescription-writing guidelines for outpatients in Southern Gauteng district hospitals. Afr. J. Prim. Health Care Fam. Med. 2020, 12, 11. [Google Scholar] [CrossRef] [PubMed]
- Medicines and Related Substances Act 101 of 1965 n.d. Available online: https://www.hpcsa.co.za/Uploads/Legal/legislation/medicines_and_related_sub_act_101_of_1965.pdf (accessed on 21 October 2021).
- De Vries, T.P.G.M.; Henning, R.H.; Hogerzeil, H.V.; Fresle, D.A. Drugs WAP on E, Policy WHOED and M. Guide to Good Prescribing: A Practical Manual; World Health Organization, Action Programme on Essential Drugs, 199; World Health Organization: Geneva, Switzerland, 1994. Available online: https://apps.who.int/iris/handle/10665/59001 (accessed on 21 October 2021).
- Brits, H.; Botha, A.; Niksch, L.; Terblanché, R.; Venter, K.; Joubert, G. Illegible handwriting and other prescription errors on prescriptions at National District Hospital, Bloemfontein. South Afr. Fam. Pract. 2017, 59, 52–55. [Google Scholar] [CrossRef]
- Illegible Prescriptions—The Pharmacist’s Dilemma—Pharmaciae—SAPC n.d. Available online: https://online.pharmaciae.org.za/illegible-prescriptions-the-pharmacists-dilemma/ (accessed on 21 October 2021).
- Rodríguez-Vera, F.J.; Marín, Y.; Sánchez, A.; Borrachero, C.; Pujol, E. Illegible handwriting in medical records. J. R. Soc. Med. 2002, 95, 545–546. [Google Scholar] [CrossRef]
- Rosa, M.B.; Perini, E.; Anacleto, T.A.; Neiva, H.M.; Bogutchi, T. Errors in hospital prescriptions of high-alert medications. Rev. Saude Publica 2009, 43, 490–498. [Google Scholar] [CrossRef] [PubMed]
- World Medical Association. Declaration of Helsinki- Medical Research Involving Human Subjects n.d. Available online: https://www.wma.net/what-we-do/medical-ethics/declaration-of-helsinki/ (accessed on 22 October 2021).
- Vally, M. Prescribing Errors at an Academic Teaching Hospital in Johannesburg; University of the Witwatersrand: Johannesburg, South Africa, 2017. [Google Scholar]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Department of Health (South Africa). General Regulations Made in Terms of the Medicines and Related Substances Act 101 of 1965, as Amended-Government Notice No. 859 in Government Gazette No. 41064, dated 25 August 2017 (Regulation 33). 2017. Available online: https://www.sahpra.org.za/wp-content/uploads/2021/11/Medicines-Act-General-Regulations-2017.pdf (accessed on 9 September 2021).
- Mohan, P.; Sharma, A.K.; Panwar, S.S. Identification and quantification of prescription errors. Med. J. Armed Forces India 2014, 70, 149–153. [Google Scholar] [CrossRef]
- Fadare, J.O.; Agboola, S.M.; Alabi, R.A. Quality of Prescriptions in a Tertiary Care Hospital in South-West Nigeria. J. Appl. Pharm. Sci. 2013, 3, 81–84. [Google Scholar] [CrossRef]
- Calligaris, L.; Panzera, A.; Arnoldo, L.; Londero, C.; Quattrin, R.; Troncon, M.G.; Brusaferro, S. Errors and omissions in hospital prescriptions: A survey of prescription writing in a hospital. BMC Clin. Pharmacol. 2009, 9, 9. [Google Scholar] [CrossRef] [PubMed]
- Lauren, C.; Doctors Bad Handwriting Can Be Costly|Scott Harris Law. Law off Scott Harris APLC n.d. Available online: https://www.scottsharrislaw.com/resources/articles/bad-handwriting-doctor/ (accessed on 23 October 2021).
- Albarrak, A.I.; Al Rashidi, E.A.; Fatani, R.K.; Al Ageel, S.I.; Mohammed, R. Assessment of legibility and completeness of handwritten and electronic prescriptions. Saudi Pharm. J. 2014, 22, 522–527. [Google Scholar] [CrossRef] [PubMed]
- Mandal, P.; Jana, S.; Ghosh, B.; Ghosh, S.; Dalal, I.; Kundu, K.K. An Assessment of legibility and accuracy of prescriptions through prescription surveys. IOSR J. Nurs. Health Sci. 2013, 1, 1–3. [Google Scholar] [CrossRef]
- The National Academies of Sciences Engineering Medicine. Medication Errors Injure 1.5 Million People and Cost Billions of Dollars Annually—Report Offers Comprehensive Strategies for Reducing Drug-Related Mistakes|National Academies 2006. Available online: https://www.nationalacademies.org/news/2006/07/medication-errors-injure-one-point-five-million-people-and-cost-billions-of-dollars-annually-report-offers-comprehensive-strategies-for-reducing-drug-related-mistakes (accessed on 23 October 2021).
- Borah, N. Doctor’s Illegible Handwriting Creating Confusion, Causing Death—Health Files by Dr. Nomal Chandra Borah|ET HealthWorld. ETHealthworldCom 2015. Available online: http://health.economictimes.indiatimes.com/health-files/doctor-s-illegible-handwriting-creating-confusion-causing-death/591 (accessed on 23 October 2021).
- Ni, K.; Noor, M.; Chua, S. Noncompliance with prescription writing-requirements and prescribing errors in an outpatient department. Malays. J. Pharm. 2002, 1, 45–50. [Google Scholar] [CrossRef]
- Winslow, E.H.; Nestor, V.A.; Davidoff, S.K.; Thompson, P.G.; Borum, J.C. Legibility and completeness of physicians’ handwritten medication orders. Heart Lung 1997, 26, 158–164. [Google Scholar] [CrossRef]
- Bruner, A.; Kasdan, M.L. Handwriting errors: Harmful, wasteful and preventable. J. Ky. Med. Assoc. 2001, 99, 189–192. [Google Scholar] [PubMed]
- Cohen, J.; Bancilhon, J.-M.; Jones, M. South African physicians’ acceptance of e-prescribing technology: An empirical test of a modified UTAUT model. S. Afr. Comput. J. 2013, 50, 43–54. [Google Scholar] [CrossRef]


| Demographic Characteristic | Category | Number of Participants (n = 59) | Frequency (%) |
|---|---|---|---|
| Age | 18–25 | 42 | 71% |
| 26–30 | 12 | 20% | |
| 31–39 | 3 | 5% | |
| >40 | 2 | 3% | |
| Gender | Female | 47 | 80% |
| Male | 12 | 20% | |
| Prefer not to say | - | 0% | |
| Other | - | - | |
| Pharmacy Personnel | Pharmacist | 16 | 27% |
| Pharmacist intern | 8 | 14% | |
| Pharmacist assistant (qualified-post basic) | 1 | 2% | |
| Community service pharmacist | 3 | 5% | |
| Third-year pharmacy student | 9 | 15% | |
| Fourth-year pharmacy student | 22 | 37% | |
| Current sector of practice | Retail/community | 26 | 36% |
| Locum (retail/community) | 8 | 11% | |
| Hospital/Institutional | 23 | 32% | |
| Academia | 11 | 15% | |
| Industry/Manufacturing | 3 | 4% | |
| Other | 2 | 3% | |
| Years of experience | <1 year | 27 | 46% |
| 1–5 years | 26 | 44% | |
| 6–10 years | 3 | 5% | |
| 11–15 years | 0 | 0% | |
| 16–20 years | 1 | 2% | |
| >20 years | 2 | 3% |
| Prescription | Correct Details |
|---|---|
 | Prescription 1: Label 1: Prexum® (Tablets) Label 2: Flomist® Label 3: Allerway® Date: 5 January 2021 Quantity medication 1: 30 Dosage medication 1: 4 mg |
 | Prescription 2: Label 1: Amoksiklav®, (Bio- Amoksiklav) Label 2: Arcoxia® Label 3: Alcophyllex® Label 4: Prednisone Label 5: Combivent® Nebuliser OR Duolin® respules (generic) Date: 2 Ferbrary 2021 Label 4 quantity: 30 Label 2 dosage: 90 mg |
 | Prescription 3: Label 1: Clacee® Label 2: Dilinct® syrup Label 3: Allerway® tab Date: 19 March 2021 Label 3 abbreviation: b.d. Label 3 quantity: 10 Label 1 dosage: 500 mg Label 2 dosage form: syrup (oral) |
 | Prescription 4: Label 1: Dormicum® Label 2: Synaleve® Date: 1 Ferbrary 2021 Label 2 abbreviation: TDS, tds, Txd Label 1 quantity: 30 Label 1 dosage: 15 mg |
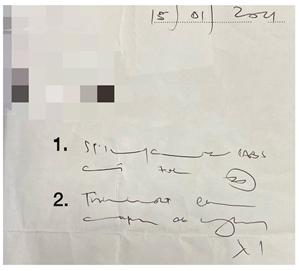 | Prescription 5: Label 1: Stilpane® Label 2: Travocort® cream Date: 15 January 2021 Label 2 abbreviation: od Label 1 quantity: 20 Label 2 dosage form: Cream (skin) (dermal) |
| How Legible Would You Rate the Prescription | Response | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Participants (n = 59) | ||||||||||
| 1 | 2 | 3 | 4 | 5 | ||||||
| n | % | n | % | n | % | n | % | n | % | |
| Prescription 1 | 41 | 69 | 14 | 24 | 3 | 5 | 1 | 2 | 0 | 0 |
| Prescription 2 | 39 | 66 | 16 | 27 | 3 | 5 | 1 | 2 | 0 | 0 |
| Prescription 3 | 47 | 80 | 10 | 17 | 2 | 3 | 0 | 0 | 0 | 0 |
| Prescription 4 | 40 | 68 | 13 | 22 | 6 | 10 | 0 | 0 | 0 | 0 |
| Prescription 5 | 50 | 85 | 8 | 14 | 1 | 2 | 0 | 0 | 0 | 0 |
| Prescription Item | Incorrect | Unsure | Correct |
|---|---|---|---|
| Name | 13% | 62% | 20% |
| Date | 23% | 11% | 66% |
| Quantity | 41% | 29% | 30% |
| Dosage | 23% | 45% | 32% |
| Abbreviation | 5% | 58% | 37% |
| Dosage form | 15% | 68% | 18% |
| Statements | Response | |||||
|---|---|---|---|---|---|---|
| Total Participants (n = 59) | ||||||
| Yes | No | Not Applicable | ||||
| n | % | n | % | n | % | |
| Have you ever faced difficulty reading an illegible prescription? | 59 | 100 | 0 | 0 | 0 | 0 |
| Do you ask a colleague for assistance when you have difficulty reading an illegible prescription? | 58 | 98 | 0 | 0 | 1 | 2 |
| Do you consult WhatsApp/telegram/other social media groups for assistance when you have difficulty reading an illegible prescription? | 16 | 27 | 39 | 66 | 4 | 7 |
| Do you contact the prescriber to confirm the medication/dosage if ambiguity exists? | 47 | 80 | 4 | 7 | 8 | 14 |
| Are you hesitant to call the prescriber when you have difficulty reading a prescription? | 19 | 32 | 34 | 58 | 6 | 10 |
| Have you ever made an error in interpreting or dispensing a prescription due to bad handwriting? | 34 | 58 | 25 | 42 | 0 | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Modi, T.; Khumalo, N.; Shaikh, R.; Booth, Z.; Leigh-de Rapper, S.; Mahumane, G.D. Impact of Illegible Prescriptions on Dispensing Practice: A Pilot Study of South African Pharmacy Personnel. Pharmacy 2022, 10, 132. https://doi.org/10.3390/pharmacy10050132
Modi T, Khumalo N, Shaikh R, Booth Z, Leigh-de Rapper S, Mahumane GD. Impact of Illegible Prescriptions on Dispensing Practice: A Pilot Study of South African Pharmacy Personnel. Pharmacy. 2022; 10(5):132. https://doi.org/10.3390/pharmacy10050132
Chicago/Turabian StyleModi, Tasneem, Ntandoyenkosi Khumalo, Rubina Shaikh, Zelna Booth, Stephanie Leigh-de Rapper, and Gillian Dumsile Mahumane. 2022. "Impact of Illegible Prescriptions on Dispensing Practice: A Pilot Study of South African Pharmacy Personnel" Pharmacy 10, no. 5: 132. https://doi.org/10.3390/pharmacy10050132
APA StyleModi, T., Khumalo, N., Shaikh, R., Booth, Z., Leigh-de Rapper, S., & Mahumane, G. D. (2022). Impact of Illegible Prescriptions on Dispensing Practice: A Pilot Study of South African Pharmacy Personnel. Pharmacy, 10(5), 132. https://doi.org/10.3390/pharmacy10050132








