Abstract
(1) Background: This scoping review aims to explore the literature on feedback for pharmacy students during experiential learning, with a focus on identifying the modes of delivery of feedback and the perceived impact of feedback on student learning outcomes. (2) Methods: The scoping review was conducted in accordance with the Joanna Briggs Institute (JBI) methodology and reported following the Preferred Reporting Items for Systematic Reviews Extension for Scoping Reviews (PRISMA-ScR) guidelines. PubMed, Web of Science, Embase, EBSCO, ERIC, and ProQuest Central were searched electronically from their inception until the end of February 2023 using a combination of keywords and MeSH terms related to feedback, pharmacy education, and student learning outcomes. Data were synthesized narratively. (3) Results: This review included 13 studies published between 2008 and 2022. Almost half of the included studies were conducted in the USA (n = 6, 46%) and reported the perspective of undergraduate pharmacy students (n = 6, 46%). Verbal feedback was the most common mode of feedback delivery (n = 6, 46%). The enablers of effective feedback included timely feedback (n = 6, 46%), feedback provided in a goal-oriented and objective manner (n = 5, 40%), and student-specific feedback (n = 4, 30%). On the other hand, the most common impediments to feedback efficacy were providing extremely positive feedback and lack of constructive criticism. (4) Conclusions: Our findings highlight the importance of feedback model implementation in pharmacy education and preceptor training programs to ensure effective and quality feedback to pharmacy students.
1. Introduction
A skilled and competent pharmacy workforce is a crucial aspect of a thriving healthcare system, as it plays a vital role in ensuring the safe and cost-effective use of medication [1]. Experiential learning is a significant component of health professionals’ education [2]. In pharmacy education, experiential learning courses offer real-life experiences within the pharmacy curriculum [3]. Experiential learning courses include specific learning objectives and outcomes with assigned tasks that focus on student application of knowledge and skills in a real-world pharmacy practice setting supervised by a licensed and practicing pharmacist (preceptors) for a defined period [4]. However, in certain situations, other healthcare professionals may serve as mentors, depending on the specific context and learning objectives of the experiential learning program. Effectively providing feedback is considered one of the core functions of a clinical preceptor and a critical step in experiential learning as it facilitates learning and development among pharmacy students [5]. In 2008, Van de Ridder et al. defined feedback as “specific information about a comparison between a trainee’s observed performance and a standard” [6]. Feedback can help students identify their strengths and weaknesses, guide how to improve their skills, and motivate them to engage in the learning process [7]. In recent years, there has been a growing body of literature on feedback in medical education [8]. However, much of this literature has focused on medical learners and specific types of feedback, such as formative assessment or peer feedback. Feedback is a vital component of the learning journey; it helps to minimize the gap between current and target performance levels [9]. Feedback functions as a great tool to support the learner’s development and learning process, thereby contributing significantly to their educational improvements [10]. There is a lack of consensus on the most effective forms of feedback for pharmacy students, especially for experiential learning. There are substantial published studies in the healthcare literature about the evaluation process as a form of assessment, but fairly little is published and known about the feedback process [8]. Evaluation is an essential part of the learning and assessment process; however, it is different from feedback, as outlined by Ende et al., who differentiated between delivering information for improvement (feedback) and involving a judgment of performance (evaluation) [11].
A scoping review by Bing-You et al. conducted on feedback for medical education learners found that feedback is an important component of medical education and that there is a need for more research on how to provide effective feedback to learners [1]. The authors identified several key factors that can affect the effectiveness of feedback, including the timing, frequency, and content of feedback, as well as the relationship between the feedback provider and recipient. They also noted that feedback should be tailored to the individual needs of the learner and that learners should be encouraged to use feedback to reflect on their performance and set goals for improvement. This study focused mainly on medical students and residents (83%).
A preliminary search of the Cochrane Database of Systematic Reviews was conducted, and no current or ongoing systematic reviews of the topic were identified. However, after searching PubMed, several relevant articles were found, including a recent scoping review by Nelson NR (2021), which stated that the literature on pharmacy education feedback lacks depth beyond student perceptions. Furthermore, it stated that the effectiveness and quality of feedback are areas for future research, in addition to post-graduate and interprofessional education, and was limited to articles in English [12]. Moreover, this review explores feedback based on feedback metatheories and an integrative feedback model, including five components: message, implementation, student, context, and agents (MISCA) [13]. The MISCA model facilitates a comprehensive exploration of all aspects of feedback. Each component plays an important role in understanding the dynamics of feedback processes. Considering the interrelated components, the integrative MISCA model offers a comprehensive approach to exploring the feedback process and its impact on student learning and performance.
The objective of this scoping review is to explore the literature on feedback for pharmacy students during experiential learning, with a focus on identifying the modes of feedback delivery, the challenges faced by pharmacy students in incorporating feedback during experiential learning, and the perceived impact of feedback on student learning outcomes.
Review Question
What are the various modes and models of feedback delivery in experiential learning for pharmacy students and how do they impact the attainment of learning outcomes?
The key objectives are as follows:
- To explore sources (preceptors, peers, patients, and self-assessment) and modalities (verbal, written, electronic, or simulation-based feedback) of feedback in experiential learning and analyze their effectiveness from the perspective of pharmacy learners.
- To identify enablers of effective feedback and impediments to feedback efficacy in incorporating feedback during experiential learning.
- To examine the perceived impact of feedback on attainment of learning outcomes, including knowledge acquisition, skill development, and attitudes, to understand the educational value of feedback in the context of pharmacy education.
- To map the literature on feedback metatheory, MISCA, across its five components: message, implementation, student, context, and agents.
2. Materials and Methods
The proposed scoping review was conducted in accordance with the Joanna Briggs Institute (JBI) methodology and reported following the Preferred Reporting Items for Systematic Reviews Extension for Scoping Reviews (PRISMA-ScR) guidelines [14,15].
2.1. Search Strategy
A comprehensive search strategy was developed to identify relevant literature from a variety of databases, including PubMed, Web of Science, Embase, EBSCO, ERIC, and ProQuest Central. A combination of keywords and MeSH terms related to feedback, pharmacy education, and student learning outcomes were used to identify relevant studies (Supplementary Materials). Studies were searched from database inception until the end of February 2023. Studies published in the English language without any study design (qualitative, quantitative, mixed-methods) limitations were included. Review articles, letters, opinion papers, and editorials were also excluded. Two reviewers screened the articles for eligibility using the inclusion criteria detailed below using the PCC model. The PCC model, standing for Population/Participant, Concept, and Context, is a framework commonly used in scoping reviews to guide the formulation of research questions and search strategies [15].
2.1.1. Participants
Studies focusing on the perspectives of pharmacy students and residents regarding feedback received during experiential learning.
Exclusion: Studies primarily focused on feedback in non-experiential learning settings or perspectives from other stakeholders (e.g., educators, preceptors) without direct input from students and residents.
2.1.2. Concept
This review focused on the feedback provided to pharmacy students during experiential learning.
Experiential learning in pharmacy education refers to structured placements integrated into the pharmacy curriculum, offering real-life experiential courses with designated learning outcomes and assigned tasks to enable pharmacy students to practice skills and apply acquired knowledge [4].
Feedback: A formative continuing process of non-judgemental information that guides and helps students or learners to build on their skills, attitudes, and future goals [11].
Exclusion: Studies that focused on other aspects of pharmacy education, such as curriculum design or assessment, as well as studies that focused on feedback from other healthcare professions and limited only to peer feedback were excluded.
2.1.3. Context
Studies were conducted in various settings where pharmacy students and residents undergo experiential learning, including but not limited to community pharmacies, hospitals, clinics, and academic institutions.
Exclusion: Studies involving feedback provided in a non-experiential learning setting were excluded.
2.2. Study Selection
All identified citations were collated and uploaded to the EndNote desktop, and duplicates were removed. Titles and abstracts were screened by two independent reviewers for assessment against the inclusion criteria. Potentially relevant and eligible sources were retrieved in full and assessed in detail against the inclusion criteria by two independent reviewers. Reference lists of the included articles were searched for relevant papers to ensure a comprehensive search of the literature. A flowchart of the results was updated throughout the review process to detail the search results, duplicates, and screening results. Reasons for the exclusion of sources that did not meet the inclusion criteria were reported in the scoping review. Any disagreements that arose between the reviewers at each stage of the selection process were resolved through discussion and with an additional reviewer.
2.3. Data Extraction
Two reviewers independently extracted data from the included studies using a standardized data extraction tool developed by the reviewers. The extracted data included specific details, including the year of publication, participants, study objective, setting, study design, sample size, feedback model, and perceived student learning outcomes. The draft data extraction tool was piloted, modified, and revised as necessary prior to data extraction.
2.4. Data Analysis and Presentation
A descriptive analytical approach was employed to collect, summarize and categorize the literature, including a numerical count of study characteristics (quantitative) and thematic analysis (qualitative). The framework synthesis approach was used to identify key themes and patterns in the data. This review explored the literature on feedback based on feedback metatheories (MISCA) [13]. The MISCA model facilitates a comprehensive exploration of all aspects of feedback. Each component plays a crucial role in understanding the dynamics of feedback processes. By considering these interrelated components, the integrative MISCA model offers a comprehensive approach to exploring the feedback process and its impact on student learning and performance.
A systematic approach was used to extract and analyze the data from these studies. Key information from each study, including the study design, sample size, type and model of feedback, and its impact on student learning outcomes, was extracted using a structured data collection tool. Thematic analysis was also used to identify key themes and patterns in the data, such as the enablers of effective feedback delivery and impediments to feedback efficacy in pharmacy education.
3. Results
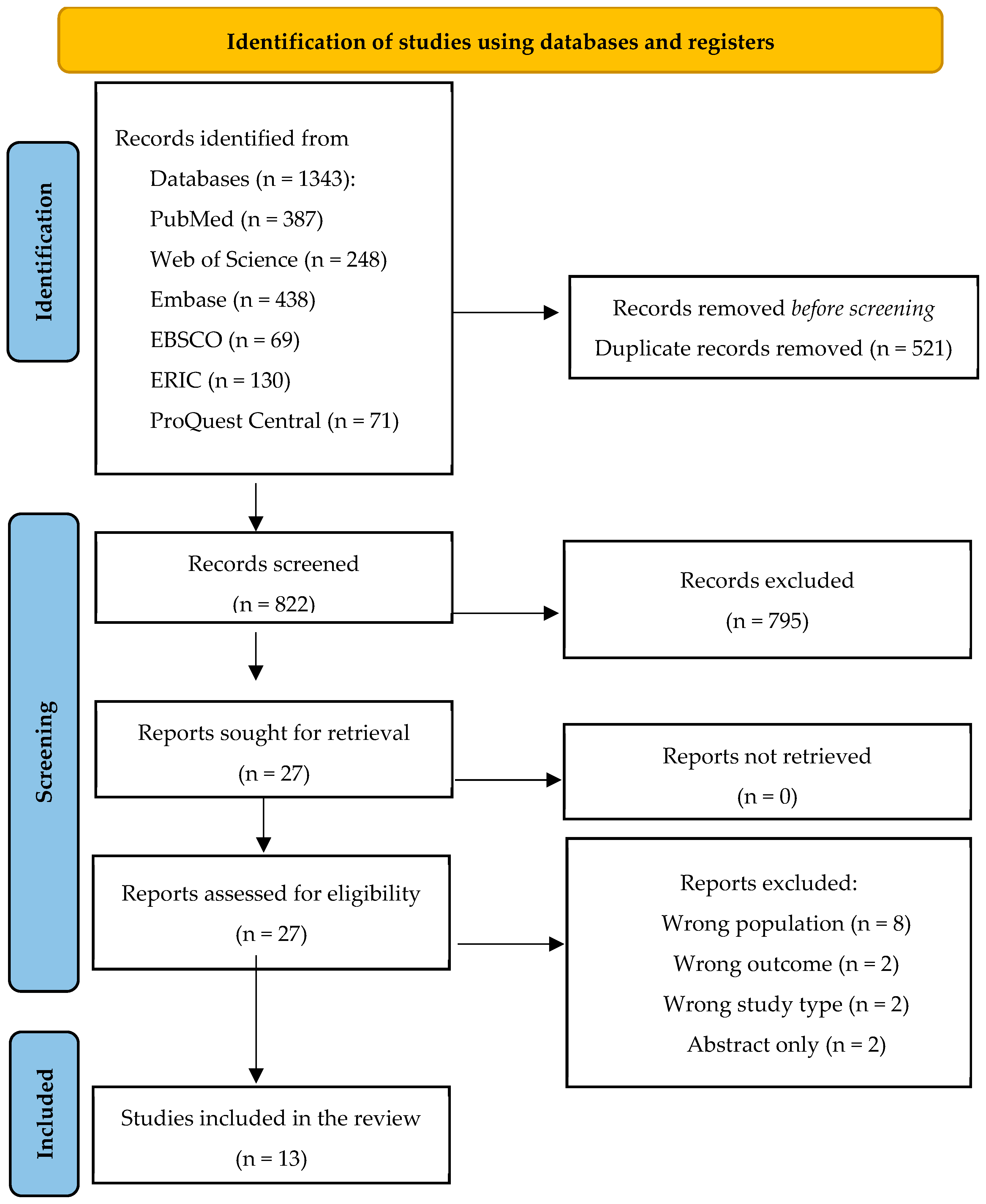
The results of the search and the study inclusion process are presented in the PRISMA-ScR flow diagram (Figure 1). As shown in the PRISMA-ScR flow diagram, the search retrieved 1343 publications. After removing duplicates (n = 521), titles and abstracts of 822 articles were screened, resulting in 27 full-text articles being retrieved and reviewed for eligibility against inclusion and exclusion criteria. This yielded 13 articles [16,17,18,19,20,21,22,23,24,25,26,27,28] that were subsequently included in this review.
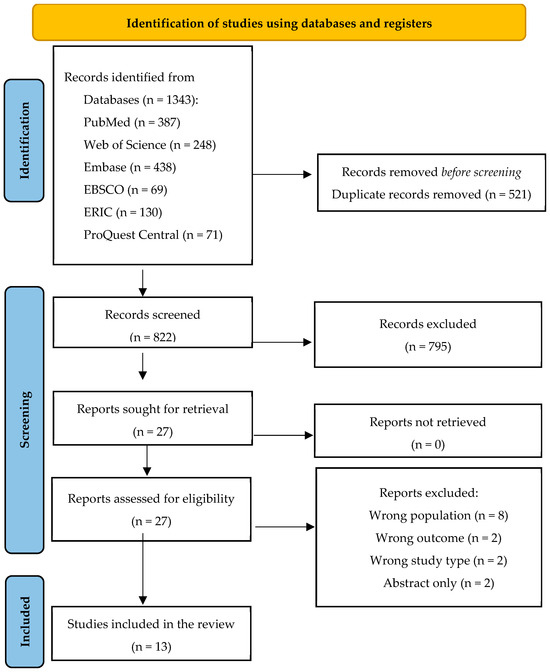
Figure 1.
PRISMA flow diagram indicating the study selection process. From Page, “The PRISMA 2020 statement is an updated guideline for reporting systematic reviews” [29].
3.1. Characteristics of the Included Studies
This review included 13 studies (Figure 1). Studies were published between 2008 and 2022. Almost half of the included studies were conducted in the United States (n = 6, 46%). Community care settings (42%), hospital care settings (31%), and ambulatory care settings (21%) were the most common settings in which studies were conducted. Most studies reported the perspective of undergraduate pharmacy students (46%). The sample size varied considerably among the included studies. Settings ranged from as few as 16 participants to community settings with a sample size of 136 participants.
A summary of the characteristics of the included studies is presented in Table 1. Of the 13 studies, most (62%) used cross-sectional surveys and two used mixed methods. Only one of the 13 studies provided a clear definition of feedback [22], whereas none of the studies discussed the model of feedback in their manuscript. The theoretical framework used was only mentioned in two of the 13 studies [22,25]. The study by Wilbur (2019) employed the cultural dimension models of Hofstede and Hall to understand the feedback encounters and behaviors described by the students. The other study by Jacob (Part 1, 2020) adopted the grounded theory method. Verbal feedback was the most common mode of feedback delivery (n = 6, 46%). Moreover, most studies reported the perceived impact of feedback on student learning outcomes (n = 10, 77%). The perceived impact of feedback reported was improved knowledge, communication skills, and development of clinical and self-management skills.

Table 1.
Summary of the characteristics of the included studies (n = 13).
3.2. Enablers of Effective Feedback Delivery, Impediments to Feedback Efficacy, and Proposed Interventions to Improve Feedback Delivery (Table 2)

Table 2.
Enablers of effective feedback delivery, impediments to feedback efficacy, and proposed interventions (n = 13).
The majority of the studies reported enablers of effective feedback delivery (n = 12, 92%) and barriers (n = 10, 77%). Enablers of effective feedback delivery included regular and timely feedback (n = 6, 46%), feedback provided in a goal-oriented and objective manner (n = 5, 40%), and student-specific feedback/tailored (n = 4, 30%). Other enablers of effective feedback delivery identified in the review were use of structured rubrics to provide feedback, and the interpersonal characteristics of preceptors including training and interest in providing feedback. The scoping review identified several barriers to receiving feedback. One barrier was providing extremely positive feedback and lacked constructive criticism. Other barriers included lack of feedback, providing short and quick feedback, and lack of recognition of individual performance. Moreover, the proposed intervention to enhance feedback mechanisms involved providing training for preceptors in providing feedback and communication skills and using a structured checklist to assess students’ performance.
3.3. Mapping the Reported Findings Using the MISCA Model
The data extracted from the included studies were mapped with the MISCA model to present a comprehensive exploration of all aspects of feedback (Table 3). All included studies provided a clear description of the feedback message (content of feedback), implementation (purpose of feedback), and agent (person who provided the feedback). The agent or the source of feedback was mainly from students (n = 10, 76%), including Advanced Pharmacy Practice Experience (APPE) students, Master (MPharm) students, and residents. In one study, source of feedback was peer feedback. However, some studies did not mention whether the feedback was tailored to the student characteristics and context (timing of feedback). The context (time) of feedback varied among the studies: at the end of the rotation (n = 2, 15%), during the rotation (n = 4, 30%), and after the rotation (n = 3, 23%). The other studies did not provide details on the context of the feedback (n = 4, 30%).

Table 3.
Mapping the reported findings with the MISCA model (n = 13).
4. Discussion
This review has contributed valuable insights into the perceptions of undergraduate and post-graduate pharmacy students regarding feedback during experiential learning with a focus on identifying the modes of delivery of feedback, the challenges faced by pharmacy students during experiential learning, and the perceived impact of feedback on student learning outcomes. Verbal feedback was the most common mode of feedback delivery (n = 6, 46%), yet there was no comparison between different modes of feedback on student learning outcomes. Compared to written feedback, verbal feedback empowers students by prompting self-directed questions, fostering critical thinking, and enabling them to take ownership of their work [30]. Verbal feedback is more feasible in experiential settings because each preceptor has a smaller number of students compared to other teaching settings [12]. Effective feedback strategies include several key components that contribute to supporting students’ learning and growth [31,32,33]. Firstly, understanding the importance of feedback with clear and specific objectives sets the foundation for its value. Timeliness plays a pivotal role, emphasizing the need for feedback to be delivered after a task to maximize its impact. Constructive and actionable feedback is another essential component, as it guides individuals towards improvement by highlighting specific areas for improvement and providing a plan to overcome weaknesses [33]. Emphasizing a commitment to follow-up ensures that the feedback is not a one-time event but an ongoing cycle that supports students’ progress.
The included articles in this review described the enablers of effective feedback delivery and impediments to feedback efficacy. The most frequently reported enabler was providing timely feedback, which was supported by other literature [34] and accreditation standards, for example, the American Society of Health-System Pharmacists Standard 3.4 mandates providing verbal formative feedback [35]. The impediments to feedback efficacy were the lack of constructive criticism and providing extremely positive feedback. In a systematic review focusing on feedback in nursing education, it was emphasized that the feedback should be timely and include both positive and constructive comments [2]. Moreover, the limited time is one of the barriers for the preceptors to provide comprehensive, consistent, and constructive feedback [36]. The proposed intervention to enhance feedback involved providing training for preceptors and the use of a structured checklist to assess students’ performance. An Australian study by Lucas et al. highlighted that standardization of preceptor training was important, particularly in feedback [37].
Despite the rich data obtained, certain gaps persist in the existing literature that warrant further investigation. The feedback provided to pharmacy students is mostly written in summative evaluation, and the quality of feedback is rarely assessed [38]. There is limited understanding of how feedback is used in pharmacy education, particularly during experiential learning [13]. First, the literature lacks a clear, comprehensive, and standardized definition of feedback in pharmacy practice during experiential learning. The definition of feedback in pharmacy education is crucial for establishing consistency, ensuring a standardized understanding and application of this fundamental element across pharmacy educational settings [39]. Feedback in healthcare education differs from general feedback due to the critical nature of the medical environment, complexity of medical knowledge, and professional competence involved. The aim is not to create a new definition but rather to establish a consensus on its application within the healthcare education context. This consensus tailors feedback to specific skills, interdisciplinary collaboration, and patient-centered care. By fostering agreement on these unique aspects, healthcare organizations can promote continuous learning among the learners and professionals and improve patient outcomes [8]. Second, studies exploring the process and impact of feedback in pharmacy education are needed to consider the integrative models such as the MISCA model. A robust feedback model serves as a guiding framework that facilitates effective communication between educators and students [38]. The MISCA model is a comprehensive framework for understanding feedback dynamics and facilitates a thorough investigation of factors influencing feedback effectiveness, including message content, delivery methods, student characteristics, contextual factors, and agent attributes. By identifying enablers of effective feedback delivery and impediments to feedback efficacy, the feedback delivery and utilization can be optimized to advance educational practice and enhance student learning outcomes. Moreover, the MISCA model can serve as a framework for future research and practical ideas, guiding the development of evidence-based strategies to improve feedback practices in educational settings [13]. A well-structured feedback model provides a systematic approach for preceptors to communicate constructive insights, enabling students to understand their strengths and identify areas for improvement with a clear action plan. Models of feedback are crucial in the field of medical and pharmacy education as they provide structured frameworks that enhance precision, ensuring effective communication and improvement strategies for students. Moreover, this model contributes to the overall quality of pharmacy education by promoting consistency and transparency in the feedback process. There is also a need for the use of a theoretical framework in pharmacy education research to assist researchers in better understanding the feedback process and guiding the implementation of the proposed intervention. This can result in an effective and sustained feedback process during experiential learning [28]. Implementation of a theoretical framework and feedback models helps in measuring the impact of feedback on student outcomes and understanding the strategies that can enhance student performance and learning [28]. The lack of consistent, constructive, timely, and individualized feedback, as reported by most of the included studies in this review, highlights the need for feedback model implementation in pharmacy education.
4.1. Strengths and Limitations
To the best of our knowledge, this scoping review is the first to map studies using the MISCA model to present a comprehensive exploration of all aspects of feedback in the literature. It is important to highlight that most studies were conducted in the USA and Europe, in addition to including studies from Africa and one study from the Middle East, as experiential learning experiences are different in each country. One limitation is that the review was restricted to primary research articles published only in English, which may have limited our findings.
4.2. Further Research and Recommendations
Future research in pharmacy education should focus on investigating the implementation and impact of effective feedback models in experiential learning. In addition, research focuses on the successful implementation of the proposed interventions to improve feedback. Equally important is exploring preceptors’ training programs to ensure that they are well-equipped to provide constructive feedback and action plans for improvement and follow-up during experiential learning. These areas require continuous exploration to enhance the feedback process and improve the quality of pharmacy education that promotes students’ development and satisfaction.
5. Conclusions
This review provided a wide breadth of literature on the perceptions provided by pharmacy students regarding their experiences of receiving feedback during experiential learning that was mapped with the MISCA model. Our findings highlight the importance of feedback model implementation in pharmacy education and preceptor training programs to ensure effective and quality feedback to pharmacy students. Future research should focus on investigating the implementation and impact of effective feedback models in experiential learning.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/pharmacy12030074/s1, Table S1: Search Strategy for PubMed; Table S2: Search strategy for Web of Science; Table S3: Search strategy for Embase; Table S4: Search strategy for Academic Search Ultimate (EBSCO); Table S5: Search strategy for EBSCO (ERIC); Table S6: Search strategy for ProQuest Central.
Author Contributions
Conceptualization, D.A.; methodology, M.A.H.; validation, M.A.H.; formal analysis, D.A. and S.A.S.; investigation, D.A. and S.A.S.; data curation, M.A.H. and A.S.; writing—original draft preparation, D.A.; writing—review and editing, M.A.H., S.A.S. and A.S.; visualization M.A.H., supervision, M.A.H. and A.S.; project administration, D.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent statement
Not applicable.
Data Availability Statement
The data presented in this study are presented in the tables.
Conflicts of Interest
The authors declare no conflicts of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Dalton, K.; Byrne, S. Role of the pharmacist in reducing healthcare costs: Current insights. Integr. Pharm. Res. Pract. 2017, 6, 37–46. [Google Scholar] [CrossRef]
- Yardley, S.; Teunissen, P.W.; Dornan, T. Experiential learning: AMEE Guide No. 63. Med. Teach. 2012, 34, e102–e115. [Google Scholar] [CrossRef]
- Wilbur, K.; Wilby, K.J.; Pawluk, S. Pharmacy preceptor judgments of student performance and behavior during experiential training. Am. J. Pharm. Educ. 2018, 82, 6451. [Google Scholar] [CrossRef]
- Hope, D.L.; Rogers, G.D.; Grant, G.D.; King, M.A. Experiential Learning in a Gamified Pharmacy Simulation: A Qualitative Exploration Guided by Semantic Analysis. Pharmacy 2021, 9, 81. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, S.T.; Couldry, R.; Phillips, H.; Buck, B. Preceptor development: Providing effective feedback. Hosp. Pharm. 2013, 48, 26–32. [Google Scholar] [CrossRef]
- van de Ridder, J.M.; Stokking, K.M.; McGaghie, W.C.; ten Cate, O.T. What is feedback in clinical education? Med. Educ. 2008, 42, 189–197. [Google Scholar] [CrossRef]
- Steven, K.; Wenger, E.; Boshuizen, H.; Scherpbier, A.; Dornan, T. How clerkship students learn from real patients in practice settings. Acad. Med. 2014, 89, 469–476. [Google Scholar] [CrossRef]
- Burgess, A.; van Diggele, C.; Roberts, C.; Mellis, C. Feedback in the clinical setting. BMC Med. Educ. 2020, 20 (Suppl. S2), 460. [Google Scholar] [CrossRef] [PubMed]
- Burgess, A.; Mellis, C. Feedback and assessment during clinical placements: Achieving the right balance. Adv. Med. Educ. Pract. 2015, 6, 373–381. [Google Scholar] [CrossRef]
- Shepard, L.A. The role of assessment in a learning culture. Educ. Res. 2000, 29, 4–14. [Google Scholar] [CrossRef]
- Ende, J. Feedback in clinical medical education. J. Am. Med. Assoc. 1983, 250, 777–781. [Google Scholar] [CrossRef]
- Nelson, N.R.; Carlson, R.B.; Corbett, A.H.; Williams, D.M.; Rhoney, D.H. Feedback for Learning in Pharmacy Education: A Scoping Review. Pharmacy 2021, 9, 91. [Google Scholar] [CrossRef] [PubMed]
- Panadero, E.; Lipnevich, A.A. A review of feedback models and typologies: Towards an integrative model of feedback elements. Educ. Res. Rev. 2022, 35, 100416. [Google Scholar] [CrossRef]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; the PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis proto-cols (PRISMA-P) 2015: Elaboration and explanation. BMJ 2015, 349, g7647. [Google Scholar] [CrossRef] [PubMed]
- Peters, M.D.J.; Marnie, C.; Tricco, A.C.; Pollock, D.; Munn, Z.; Alexander, L.; McInerney, P.; Godfrey, C.M.; Khalil, H. Updated methodological guidance for the conduct of scoping reviews. JBI Evid. Synth. 2020, 18, 2119–2126. [Google Scholar] [CrossRef] [PubMed]
- Hyvarinen, M.L.; Tanskanen, P.; Katajavuori, N.; Isotalus, P. Feedback in patient counselling training—Pharmacy students’ opinions. Patient Educ. Couns. 2008, 70, 363–369. [Google Scholar] [CrossRef] [PubMed]
- Boland, C.; Koval, P.G.; Parker, M.H. Determining the utility of a student survey to provide valuable feedback on precepting skills of pharmacy residents. Curr. Pharm. Teach. Learn. 2014, 6, 406–411. [Google Scholar] [CrossRef]
- Bates, J.S.; Buie, L.W.; Lyons, K.; Rao, K.; Pinelli, N.R.; McLaughlin, J.E.; Roth, M.T. A Study of Layered Learning in Oncology. Am. J. Pharm. Educ. 2016, 80, 68. [Google Scholar] [CrossRef] [PubMed]
- Belachew, S.A.; Abegaz, T.M.; Bhagavathula, A.S.; Getachew, H.; Tefera, Y.G. Evaluation of preceptors and skills achievement by clinical pharmacy clerkship students during their clinical rotations at University of Gondar, Ethiopia. Adv. Med. Educ. Pract. 2016, 7, 187–196. [Google Scholar]
- Melaku, T.; Bhagavathula, A.S.; Getaye, Y.; Admasu, S.; Alkalmi, R. Perceptions of pharmacy clerkship students and clinical preceptors regarding preceptors’ teaching behaviors at Gondar University in Ethiopia. J. Educ. Eval. Health Prof. 2016, 13, 9. [Google Scholar] [CrossRef]
- Linedecker, S.J.; Barner, J.; Ridings-Myhra, J.; Garza, A.; Lopez, D.; McIntyre, W. Development of a direct observation of procedural skills rubric for fourth-year pharmacy students in ambulatory care rotations. Am. J. Health-Syst. Pharm. AJHP Off. J. Am. Soc. Health-Syst. Pharm. 2017, 74, S17–S23. [Google Scholar] [CrossRef] [PubMed]
- Wilbur, K.; BenSmail, N.; Ahkter, S. Student feedback experiences in a cross-border medical education curriculum. Int. J. Med. Educ. 2019, 10, 98–105. [Google Scholar] [CrossRef]
- Schweiss, S.; Pavelka, A.; Garza, O.W.; Moon, J.Y. Using a multisite and multi-health system pharmacy resident program model for care documentation quality improvement. J. Am. Pharm. Assoc. JAPhA 2019, 59, 862–866.e1. [Google Scholar] [CrossRef] [PubMed]
- Jacob, S.A.; Boyter, A.C. Survey of undergraduates’ perceptions of experiential learning in the MPharm programme: The TELL Project. Pharm. Pract. 2020, 18, 1856. [Google Scholar] [CrossRef] [PubMed]
- Jacob, S.A.; Boyter, A.C. “My experiences were highly dependent on the knowledge and enthusiasm of the tutor”: Graduates’ feedback of experiential learning in an MPharm programme Part 1 (TELL Project). Stud. Educ. Eval. 2020, 66, 100891. [Google Scholar] [CrossRef]
- Jacob, S.A.; Boyter, A.C. “It has very good intentions but it’s not quite there yet”: Graduates’ feedback of experiential learning in an MPharm programme Part 2 (TELL Project). Stud. Educ. Eval. 2020, 66, 100889. [Google Scholar] [CrossRef]
- Hatcher, T.M.; Schoen, R.R.; Garmong, G.E.; Stewart-Lynch, A.L. Student Pharmacist Perspectives of a Remote Ambulatory Care and Community Pharmacy Dual-Cohort APPE. J. Pharm. Pract. 2022, 36, 1505–1515. [Google Scholar] [CrossRef] [PubMed]
- Margolis, A.; Shah, S.; Zorek, J.A.; Kieser, M.; Martin, B. Implementation of the Individual Teamwork Observation and Feedback Tool to Evaluate Pharmacy Student Performance. Am. J. Pharm. Educ. 2022, 86, 8578. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; Chou,, R.; et al. The PRISMA 2020 statement is an updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Agricola, B.T.; Prins, F.J.; Sluijsmans, D.M. Impact of feedback request forms and verbal feedback on higher education students’ feedback perception, self-efficacy, and motivation. Assess. Educ. Princ. Policy Pract. 2020, 1, 6–25. [Google Scholar] [CrossRef]
- Shaw, S.C.K. How can we promote and facilitate effective study skills in medical students? MedEdPublish 2017, 6, 36. [Google Scholar] [CrossRef]
- Hardavella, G.; Aamli-Gaagnat, A.; Saad, N.; Rousalova, I.; Sreter, K.B. How to give and receive feedback effectively. Breathe 2017, 13, 327–333. [Google Scholar] [CrossRef] [PubMed]
- Gnepp, J.; Klayman, J.; Williamson, I.O.; Barlas, S. The future of feedback: Motivating performance improvement through future-focused feedback. PLoS ONE 2020, 15, e0234444. [Google Scholar] [CrossRef] [PubMed]
- Henderson, M.; Phillips, M.; Ryan, T.; Boud, D.; Dawson, P.; Molloy, E.; Mahoney, P. Conditions that enable effective feedback. High. Educ. Res. Dev. 2019, 7, 1401–1416. [Google Scholar] [CrossRef]
- ASHP Commission on Credentialing Guidance Document for the ASHP Accreditation Standard for Postgraduate Year One (PGY1) Pharmacy Residency Programs. Available online: https://www.ashp.org/-/media/assets/professional-development/residencies/docs/guidance-document-PGY1-standards.ashx?la=en&hash=20D275DC632B78E92626D7233DF52747279FE820 (accessed on 5 January 2021).
- Paterson, C.; Paterson, N.; Jackson, W.; Work, F. What Are Students’ Needs and Preferences for Academic Feedback in Higher Education? A Systematic Review. Nurse Educ. Today 2020, 85, 104236. [Google Scholar] [CrossRef] [PubMed]
- Lucas, C.; Williams, K.; Tudball, J.; Walpola, R. Community, hospital and industry preceptor perceptions of their role in experiential placements—The need for standardization of preceptor responsibilities and evaluations on students. Curr. Pharm. Teach. Learn. 2018, 10, 1447–1455. [Google Scholar] [CrossRef]
- Bing-You, R.; Hayes, V.; Varaklis, K.; Trowbridge, R.; Kemp, H.; McKelvy, D. Feedback for Learners in Medical Education: What Is Known? A Scoping Review. Acad. Med. 2017, 92, 1346–1354. [Google Scholar] [CrossRef]
- Di Costa, N. Feedback on Feedback: Student and academic perceptions, expectations and practices within an undergraduate Pharmacy course. In Proceedings of the ATN Assessment Conference 2010, University of Technology Sydney, Sydney, Australia, 18–19 November 2010. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).