A Sociotechnical Approach to Analyze Pharmaceutical Policy and Services Management in Primary Health Care in a Brazilian Municipality
Abstract
:1. Introduction
2. Materials and Methods
2.1. The Place of Study
2.2. Data Collection
2.2.1. Sources, Search Strategies, and Data Characterization
| Database | Link | Description of the Data |
|---|---|---|
| IBGE 1 | https://cidades.ibge.gov.br/ | Year of Installation, territorial area, distance from the capital, estimated population, human development index, predominant economic activity, GDP per capita, percentage of urban households [22]. |
| SIDEMS 2 | https://indicadores.fecam.org.br/index/index/ano/2020 | Municipal sustainable development index (IDMS), health situation analysis [23]. |
| Municipal Transparency Portal | https://brusque.atende.net/?pg=transparencia#!/ | Expenses with pharmaceutical policy and services [24]. |
- Municipal health system: Infrastructure, organizational structure, Family Health Strategy coverage, workforce description of the Family Health Support Center, health funding, and financial circumstances;
- PPS: Goals, organizational structure, available workforce and infrastructure, processes, and organizational culture.
2.2.2. Assessment Matrix of the Management Capacity of Municipal PPS
2.3. Data Analysis
2.4. Ethical Aspects
3. Results
3.1. Organization of Environment
| Date | Headline | Narrative | Source |
|---|---|---|---|
| 1/26/16 | Lack of medication | “The article on the cover of the newspaper Município Dia a Dia, last Thursday (21), speaks of the lack of medicines inpublic pharmacies. According to the report, there are 53 drugs missing from the downtown basic pharmacy, and the list contains drugs prescribed very frequently, as is the case of the omeprazol, amoxicillin and buscopan”. | [37] |
| 5/27/16 | City Hall clarifies about lack of medicines in the Municipal Health Network | “The Health Secretariat informs that some medications are missing in the Primary Health Centers and in the Basic Pharmacy, located in the Center. The items have already been requested and the situation can be regularized at any time. According to the folder, the situation occurs due to several situations, such as lack of raw material for production, discontinuation of imports and lack of supplier. However, some of the remedies await only the supply of the bidding company”. | [38] |
| 9/19/17 | Patients suffer from lack of medication to relieve back pain | “Patients who have a back problem, suffer from severe pain and need Tramadol to relieve symptoms since the last week, face the shortage of medication. | [39] |
| Goal | Indicator | Action | Budget (R$) | Budget Origin |
|---|---|---|---|---|
| Implement actions to dispense medication and inventory maintenance regularly | Number of actions implemented | Take actions to ensure adequate dispensing of medication; Promote regular stock maintenance; Ensure adequate distribution in the municipal health network. | 5000.00 | Municipal resource. |
| Maintain the supply of medicines regularly. | Number of pharmacies in operation | Ensure the distribution of selected drugs on a regular basis; Regular stock maintenance; Adequate distribution in the municipal health network | 2,034,534.40 | Federal resource. Municipal resource. |
- (a)
- Complementary Law No. 224/2014: Institutes the Municipal Health Code, which defines pharmacy as a health service and medicines as products subject to sanitary control [41].
- (b)
- Normative No. 005/2015: It defined the organization and assignments of the tasks, the prescription, dispensing and supply of medicines, and the parameters for the functioning and structure of the services [42].
- (c)
- Decree No. 7826, 8 July 2016: Disciplines procedures to be adopted by doctors and dentists, municipal civil servants, and service providers for the Unified Health System at the municipal level in the prescription of medications [43].
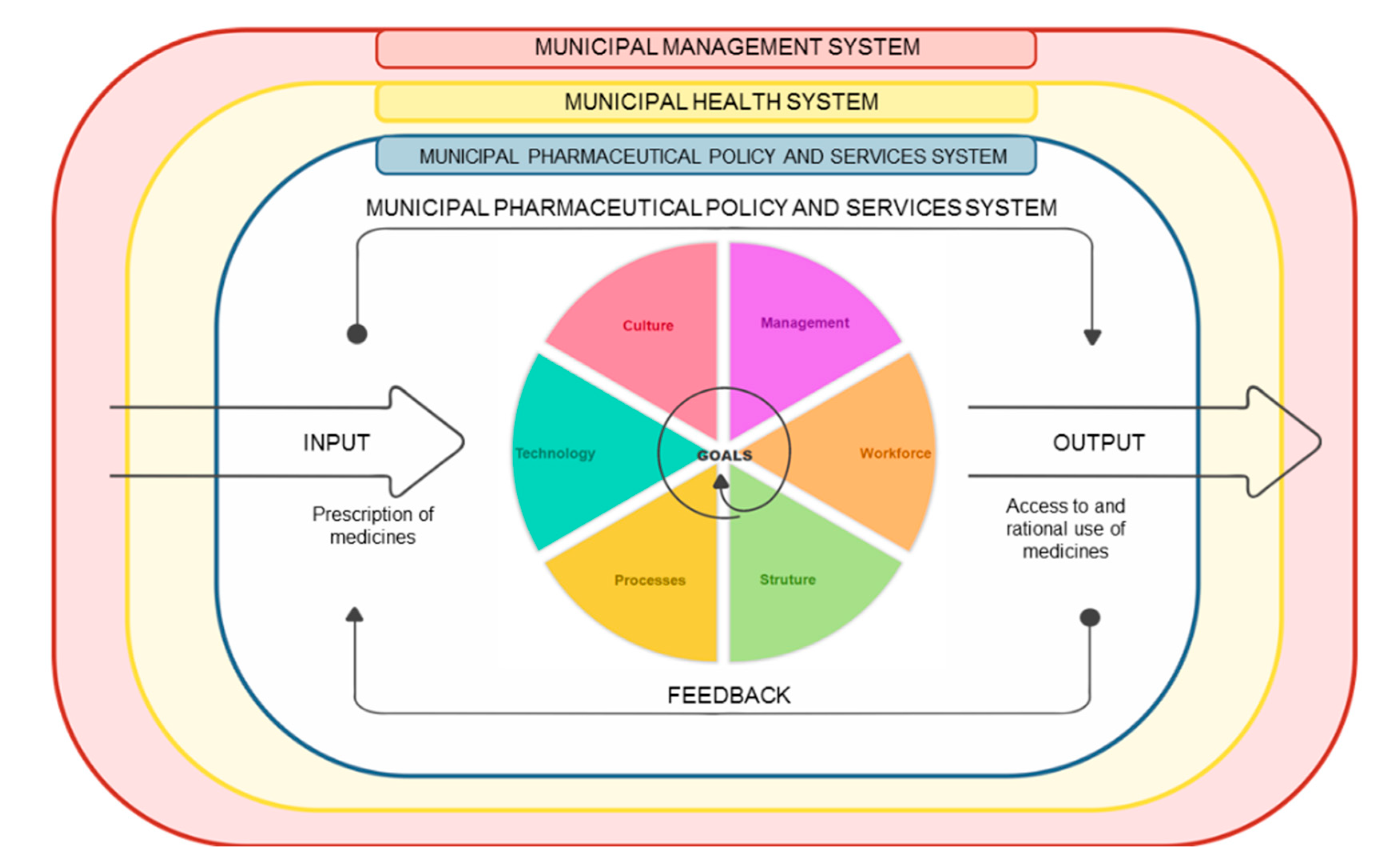
3.2. Socio-Technical Characterization of the Municipal PPS
3.2.1. Goal of the Sociotechnical System of PPS in PHC
3.2.2. PPS Management in PHC
3.2.3. Workforce of Municipal PPS in PHC
3.2.4. PPS Infrastructure and Processes in PHC
“When I started at the warehouse, our purchases were based on the transfers that we made to the healthcare centers and then these values, these amounts that we had, they were not very reliable, because they were not based on the real demand that we had in the units at that time”.
“I worked in the health store, in the medication sector and in the period 2014–2016, we did not have stock control, we did not have the management of stock control in health units, nor which distributions in the stockroom. The distribution was made to health units once a month and that was the supply that the units have”.
“When I was at the healthcare center, we didn’t have this process in place yet, I can’t say it was a mess because it was part of the process, but we have two or three technicians in each healthcare center and each one who had a little time went into the pharmacy and dispensed medication. With that, we had a lot of puncture in the stock, and there were several complications like that. Even for the nurse, it was difficult to charge someone who was a continuous process and walked smoothly”.
3.2.5. Technology in PHC
- (a)
- Municipality’s Medicines List: Edition not reviewed for five years, not approved by the Municipal Health Council, and not published in an official bulletin. There were no defined procedures for disclosing the list.
- (b)
- Computerized PPS management system: Outsourced service, restricted to inventory management in PHC.
- (c)
- Electronic medical record: Pharmacists had access to patient data in all PPS facilities.
- (d)
- Standard operating procedures: Outdated and used only by Central Pharmacy staff.
3.2.6. Organizational Culture in PHC
“When I arrived and took over the portfolio of the health department, PPS was quite confused, there was no line or better a municipal policy for PPS, and this is what we need today,. We are not only ensuring insuring costs or expenses, but working with the public money in a responsible way. So, we had a very messy house, a lot of expired medicines and put in stock, something that today we prioritize the right purchase, good purchase, right and something that each health center worked on dispensing medication in the way that best suits them”.
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AHP: | Annual Health Program |
| MHP: | Municipal health plans |
| REMUME: | Municipal List of Medicines |
| AMMC: | Assessment Matrix of the Management Capacity |
| IBGE: | Brazilian Institute of Geography and Statistics |
| SIDEMS: | System of Sustainable Municipal Development Indicators |
| UDI: | Human Development Index |
| MHS: | Municipal Health Secretariat |
| PHC: | Primary health care |
| SUS: | Brazilian Unified Health System |
| PPS: | Pharmaceutical policy and services |
References
- Kruk, M.E.; Gage, A.D.; Arsenault, C.; Jordan, K.; Leslie, H.H.; Roder-DeWan, S.; Adeyi, O.; Barker, P.; Daelmans, B.; Doubova, S.V.; et al. High-quality health systems in the Sustainable Development Goals era: Time for a Revolution. Lancet Glob. Health Comm. 2018, 6. [Google Scholar] [CrossRef] [Green Version]
- WHO. Urgent Health Challenges for the Next Decade. 2020. Available online: https://www.who.int/news-room/photo-story/photo-story-detail/urgent-health-challenges-for-the-next-decade (accessed on 6 May 2020).
- Holloway, K.A.; Ivanovska, V.; Wagner, A.K.; Vialle-Valentin, C.; Ross-Degnan, D. Have we improved use of medicines in developing and transitional countries and do we know how to? Two decades of evidence. Trop. Med. Int. Health 2013, 18, 656–664. [Google Scholar] [CrossRef] [PubMed]
- Brasil. Ministério da Saúde. Conselho Nacional de Saúde. Resolução n. 338, de 6 de Maio de 2004. Aprova a Política Nacional de Assistência Farmacêutica. Available online: https://bvsms.saude.gov.br/bvs/saudelegis/cns/2004/res0338_06_05_2004.html (accessed on 27 October 2019).
- Marin, N.; Luiza, V.L.; Osorio-de-Castro, C.; Machado-dos-Santos, S.C. Assistência Farmacêutica Para Gerentes Municipais. Rio de Janeiro; OPAS/OMS: Washington, DC, USA, 2003. [Google Scholar]
- Rover, M.; Leite, S.N. Gestão em saúde e gestão da assistência farmacêutica. In Gestão da Assistência Farmacêutica: Proposta Para Avaliação no Contexto Municipal: A Experiência em Santa Catarina; Leite, S.N., Farias, M.R., Manzini, F., Mendes, S.M., Rover, M.R.M., Eds.; Editora da UFSC: Florianópolis, Brazil, 2015; pp. 39–58. [Google Scholar]
- Oliveira, M.A.; Luiza, V.L.; Tavares, N.U.L.; Mengue, S.S.; Arrais, P.S.D.; Farias, M.R.; da Silva Dal Pizzol, T.; Ramos, L.R.; Bertoldi, A.D. Acesso a medicamentos para doenças crônicas no Brasil: Uma abordagem multidimensional. Rev. Saúde Pública 2016, 50, 6s. [Google Scholar] [PubMed] [Green Version]
- Barreto, J.L.; Guimarães, M.C.L. Avaliação da gestão descentralizada da assistência farmacêutica básica em municípios, Brasil. Cad. Saúde Pública 2010, 26, 1207–1220. [Google Scholar] [CrossRef] [PubMed]
- Leite, S.N.; Farias, M.R.; Manzini, F.; Mendes, S.M.; Rover, M.R.M. Gestão da Assistência Farmacêutica: Proposta Para Avaliação no Contexto Municipal: A Experiência em Santa Catarina; Editora da UFSC: Florianópolis, Brazil, 2015. [Google Scholar]
- Gerlack, L.F.; Karnikowski, M.G.O.; Areda, C.A.; Galato, D.; de Oliveira, A.G.; Álvares, J.; Leite, S.N.; Costa, E.A.; Guibu, I.A.; Soeiro, O.M.; et al. Gestão da Assistência Farmacêutica na Atenção Primária no Brasil. Rev. Saude Publica 2017, 51, 15s. [Google Scholar]
- Leite, S.N.; Manzini, F.; da Veiga, A.; Lima, M.E.O.; Pereira, M.A.; de Araujo, S.Q.; Santos, R.F.D.; Bermudez, J.A.Z. Science, Technology and Pharmaceutical Policy on the agenda: Contributions from the society to the 16th National Conference on Health. Cienc. Saude Colet. 2018, 23, 4259–4268. [Google Scholar] [CrossRef] [Green Version]
- Akerman, M.; Freitas, O. Pesquisa Nacional sobre Acesso, Utilização e Promoção do Uso Racional de Medicamentos (PNAUM): Avaliação dos serviços de atenção farmacêutica primária. Saúde Pública 2017, 51, 1s–5s. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barros, R.D.; Costa, E.A.; Santos, D.B.; Souza, G.S.; Álvares, J.; Guerra, A.A., Jr.; de Assis Acurcio, F.; Guibu, I.A.; Costa, K.S.; de Oliveira Karnikowski, M.G.; et al. Acesso a medicamentos: Relações com a institucionalização da assistência farmacêutica. Rev. Saude Publica 2017, 51, 8s. [Google Scholar]
- Brasil. Ministério da Saúde. Secretaria de Ciência, Tecnologia e Insumos Estratégicos. Departamento de Assistência Farmacêutica e Insumos Estratégicos. Assistência Farmacêutica no SUS: 20 Anos de Políticas e Propostas Para Desenvolvimento e Qualificação: Relatório Com Análise e Recomendações de Gestores, Especialistas e Representantes da Sociedade Civil Organizada [recurso eletrônico]. Ministério da Saúde: Brasília, Brazil. 2018. Available online: http://www.as.saude.ms.gov.br/wp-content/uploads/2019/11/AF-no-SUS-20-Anos-de-Pol%C3%ADticas-e-Propostas-para-Desenvolvimento-e-Qualifica%C3%A7%C3%A3o.pdf (accessed on 6 May 2020).
- Botla, L.; Kondur, H. Socio Technical Systems of a Company: The Dimensionality of Socio Technical Systems. Purshartha J. Manag. Ethics Spiritual. 2018, 11. [Google Scholar] [CrossRef]
- Emery, F.E.; Trist, E.L. The causal texture of organization environments. Hum. Relat. 1965. [Google Scholar] [CrossRef] [Green Version]
- Meeks, D.W.; Takian, A.; Sittig, D.F.; Singh, H.; Barber, N. Exploring the sociotechnical intersection of patient safety and electronic health record implementation. J. Am. Med. Inform. Assoc. 2014, 21, e28–e34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Novak, L.L.; Holden, R.J.; Anders, S.H.; Hong, J.Y.; Karsh, B.-T. Using a sociotechnical framework to understand adaptations in health IT implementation. Int. J. Med. Inform. 2013, 82, e331–e344. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sittig, D.F.; Ash, J. On the importance of using a multidimensional sociotechnical model to study health information technology. Ann. Fam. Med. 2011, 9, 390–391. [Google Scholar] [CrossRef] [Green Version]
- Harvey, J.; Avery, A.J.; Ashcroft, D.; Boyd, M.; Phipps, D.L.; Barber, N. Exploring safety systems for dispensing in community pharmacies: Focusing on how staff relate to organizational components. Res. Soc. Adm. Pharm. 2015, 11, 216–227. [Google Scholar] [CrossRef] [PubMed]
- Szeinbach, S.; Seoane-Vazquez, E.; Parekh, A.; Herderick, M. Dispensing errors in community pharmacy: Perceived influence of sociotechnical factors. Int. J. Qual. Health Care 2007, 19, 203–209. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- IBGE. Brusque. Censo. 2010. Available online: https://cidades.ibge.gov.br/brasil/sc/brusque. (accessed on 6 May 2020).
- SIDEMS.Índice de Desenvolvimento Sustentável dos Municípios Catarinenses. 2017. Available online: https://indicadores.fecam.org.br/indice/estadual/ano/2017 (accessed on 6 May 2020).
- Brusque. Annual Management Report. 2017. Available online: https://brusque.atende.net/#!/tipo/acesso-informacao/valor/especifico/item/5 (accessed on 6 May 2020).
- Reorientação da Assistência Farmacêutica Na Atenção Primária do Município de Brusque. Available online: https://www.youtube. com / watch? v = MqtG8mI8Srw (accessed on 19 January 2021).
- Phipps, D.L.; Noyce, P.R.; Parker, D.; Ashcroft, D.M. Medication safety in community pharmacy: A qualitative study of the sociotechnical context. BMC Health Serv. Res. 2009, 9, 158. [Google Scholar] [CrossRef]
- Sittig, D.F.; Singh, H. A new sociotechnical model for studying health information technology in complex adaptive healthcare systems. Qual. Saf. Health Care 2010, 19, 68–74. [Google Scholar] [CrossRef] [PubMed]
- Harvey, J.; Avery, A.J.; Waring, J.; Barber, N. The socio-technical organisation of community pharmacies as a factor in the Electronic Prescription Service Release Two implementation: A qualitative study. BMC Health Serv. Res. 2012, 12, 471. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leavitt, H.J. Applied organizational change in industry: Structural, technological, andhumanistic approaches. In Handbook of Organizations; March, J.G., Ed.; RandMcNally& Co.: Chicago, IL, USA, 1965; pp. 1144–1170. [Google Scholar]
- Appelbaum, S. Socio-technical systems theory: An intervention strategy for organizational development. Manag. Decis. 1997, 35, 452–463. [Google Scholar] [CrossRef]
- Trist, E.L. The Evolution of Socio-Technical System; Ministry of Labor/Ontario Quality of Working Life Center: Toronto, ON, Canada, 1981.
- Davis, M.C.; Challenger, R.; Jayewardene, D.N.; Clegg, C.W. Advancing socio-technical systems thinking: A call for bravery. Appl. Ergon. 2014, 45, 171–180. [Google Scholar] [CrossRef]
- Clegg, C.W. Sociotechnical principles for system design. Appl. Ergon. 2000, 31, 463–477. [Google Scholar] [CrossRef]
- Challenger, R.; Clegg, C.W. Crowd disasters: A socio-technical systems perspective. Contemp. Soc. Sci. 2011, 6, 343–360. [Google Scholar] [CrossRef]
- Guimarães, M.C.L.; Santos, S.M.C.; Melo, C.; Sanches Filho, A. Avaliação da capacidade de gestão de organizações sociais: Uma proposta metodológica em desenvolvimento. Cad. Saúde Pública 2004, 20, 1642–1650. [Google Scholar] [CrossRef]
- Lima, M.G.; Álvares, J.; Guerra, A.A., Jr.; Costa, E.A.; Guibu, I.A.; Soeiro, O.M.; Leite, S.N.; de Oliveira Karnikowski, M.G.; Costa, K.S.; de Assis Acurcio, F. Indicadores relacionados ao uso racional de medicamentos e seus fatores associados. Rev. Saude Publica 2017, 51, 23s. [Google Scholar]
- Rádio Araguaia 970AM. Available online: https://araguaiabrusque.com.br/index.php/home (accessed on 6 April 2020).
- Portal da Cidade Brusque. Available online: https://brusque.portaldacidade.com/noticias/saude/prefeitura-de-brusque-esclarece-sobre-falta-de-medicamentos-na-rede-municipal-de-saude (accessed on 6 April 2020).
- Município. Available online: https://omunicipio.com.br/pacientes-sofrem-com-falta-de-medicamentos-para-aliviar-dores-nas-costas/ (accessed on 6 April 2020).
- Brusque. Annual Health Program in the Municipality. 2015. Available online: https://brusque.atende.net/#!/tipo/acesso-informacao/valor/especifico/item/5 (accessed on 6 May 2020).
- Brusque. Câmara Municipal de Brusque. Complementary Law No. 224/2014: Institutes the Municipal Health Code, Which Defines Pharmacy as a Health Service and Medicines as Products Subject to Sanitary. Available online: http://www.legislador.com.br/LegisladorWEB.ASP?WCI=LeiTexto&ID=11&inEspecieLei=2&nrLei=224&aaLei=2014&dsVerbete=medicamento (accessed on 6 May 2020).
- Brusque. Secretaria Municipal de Saúde. Normative No. 005/2015. Available online: https://portal.brusque.sc.gov.br/secretaria/secretaria-de-saude/ (accessed on 6 May 2020).
- Brusque. Decree No. 7826, July 8, 2016. Available online: https://leismunicipais.com.br/a/sc/b/brusque/decreto/2016/782/7826/decreto-n-7826-2016-disciplina-procedimentos-a-serem-adotados-pelos-medicos-e-odontologos-servidores-publicos-municipais-e-prestadores-de-servico-para-o-sistema-unico-de-saude-em-ambito-municipal-na-prescricao-de-medicamentos-e-na-solicitacao-de-exames-e-procedimentos-de-saude-e-estabelece-outras-providencias (accessed on 6 May 2020).
- WHO. The World Medicines Situation, 2nd ed.; WHO: Geneva, Switzerland, 2004; Available online: https://apps.who.int/iris/handle/10665/68735 (accessed on 6 May 2020).
- WHO. Access and Rational Use of Strategic1 and High-Cost Medicines and Other Health Technologies. 2016. Available online: https://www.paho.org/hq/dmdocuments/2016/CD55-10-e.pdf (accessed on 6 May 2020).
- Frost, L.J.; Reich, M.R. Creating Access to Health Technologies in Poor Countries. Health Aff. 2009, 28, 962–973. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carayon, P.; Bass, E.J.; Bellandi, T.; Gurses, A.P.; Hallbeck, M.S.; Mollo, V. Sociotechnical systems analysis in health care: A research agenda. IIE Trans. Healthc. Syst. Eng. 2011, 1, 145–160. [Google Scholar] [CrossRef] [PubMed]
- Hoepfner, L. Diagnóstico da Assistência Farmacêutica Pública em Santa Catarina: Uma Avaliação; Especialização em Gestão em Saúde; Universidade Federal de Santa Catarina: Florianópolis, Brazil, 2019. [Google Scholar]
- CONASEMS. Entrevista Mauro Junqueira. Revista CONASEMS. 2018, 72, 05–10. Available online: https://www.conasems.org.br/wp-content/uploads/2019/02/Conasems_Revista_72_Web_F01.pdf (accessed on 6 May 2020).

| Components | Literature Description | Adaptation to the Study |
|---|---|---|
| Components | Components of External System: Municipal Management System; Municipal Health System | |
| Environment | Context where the study’s focus system is inserted. | Characterization of the environment where PPS is inserted according to: Objective, guidelines, and society’s goals for PPS. |
| Interested parts | Objective of the system for patients, management, suppliers, and representatives of civil society. | PPS expected outcomes from the perspective of municipal management, the health department, and patients. |
| Financing | Economic situation under which the system is developed and what financial resource the system should operate. | Annual financing of PPS. Budgeted amount and amount paid. |
| Regulations | Rules and laws that regulate the organization. | Rules and municipal laws that regulate the organization and activities of PPS. |
| Components | Components of the Internal System | |
| Goals | Targets of the system, its operation, or that generated the demand for its construction. | Objective of municipal PPS for the different healthcare actors. |
| Management | Organizational structure and its technical operations. | Organizational structure of municipal PPS and its management capacity in PHC. Dimensions: Organizational, operational, and sustainability. |
| Workforce | Number of people able to participate in the social division of labor process. | Group of people with the capacity and ability to carry out PPS activities. Work groups where tasks are performed. |
| Structure | Equipment or the physical structure required for the performance of system activities. | Structures and infrastructure by workgroup of the PPS system. |
| Processes | Main activities that are part of the system, including the main and routine activities. | Main activities by PPS workgroup in PHC. Why does the unit of work exist? How does it communicate with the system and the environment in its technical and relational aspects? |
| Technology | Equipment and methods used to produce products or services. A health technology can be defined as a way, knowledge, and the instruments used to produce health actions. | Description of drug treatments and instruments used for their access, use, and monitoring. Drug treatment: Criteria and places for selection, access, and monitoring of outcomes. Instruments: Municipal List of Medicines, Electronic Health Record, protocol, computerized system. |
| Culture | Organizational culture of the system, the way it thinks and acts, the beliefs and values held in organization and society. | Organizational culture of PPS on three aspects. Symbols: Names, logos, and physical characteristics used to convey the organization’s image. Rituals: Usual and repeated actions within an organization. Ideology: Beliefs, moral principles, and values provide the basis for organizational decision making. |
| Period | Purpose | Goal |
|---|---|---|
| 2010 to 2013 | “The municipal PPS’s main purpose is to provide regular and free supply of selected drugs, in order to contemplate the outpatient drug treatment of the different pathologies that affect the population”. | Ensure the supply of medicines to all SUS patients in accordance with the list of selected medicines. Constantly review the list of selected medicines. Deploy Phytotherapic Handling Pharmacy. |
| 2014 to 2017 | “Guarantee the dispensation medicines of municipal list to the population”. Implement the herbal medicine production laboratory. | Consolidate drug purchase, dispensing and inventory control routines, and the use of the G-MUS management system to improve purchase and dispensing monitoring. Forward a fundraising project at the Ministry of Health to implement the herbal medicine laboratory. |
| Description | MS | SO |
|---|---|---|
| Management component | ||
| Organizational | 96 | 16 |
| Operational | 100 | 49 |
| Sustainability | 96 | 60 |
| Total | ||
| Workforce component | ||
| Condition of existence of the PPS Coordination in the Municipal Health Department (MHD). | 5 | 0 |
| Degree of decision-making autonomy of the PPS Coordination. | 10 | 0 |
| Profession of the PPS coordinator. | 7 | 0 |
| Participation of pharmacists in the preparation of the Municipal Health Plan. | 10 | 0 |
| Participation of PPS coordination in health programs or activities in the municipality (in other MHD sectors). | 10 | 0 |
| Responsibility for defining the programming parameters for distributing medicines to health units. | 7 | 0 |
| Health units with pharmacists working in the team. | 7 | 1 |
| Pharmacists trained in PA, management, public health, or related fields in the past 2 years. | 7 | 2 |
| Type of employment contract of the PPS coordinator. | 7 | 0 |
| Pharmacist position in the list of municipal public service positions. | 7 | 7 |
| Total | 77 | 3 |
| Infrastructure component | ||
| Integration of the PA information system with that used in the health care network. | 6 | 6 |
| Instruments to assess physical and environmental conditions to store medicines (external and internal conditions, lighting, refrigeration, security). | 6 | 3 |
| Investments in infrastructure in the last 4 years in PPS services. | 7 | 7 |
| Total | 19 | 16 |
| Processes component | ||
| Pharmacists and health unit coordinators recognize the existence of PPS coordination. | 8 | 0 |
| Regular functioning of the Pharmacy and Therapeutics Committee in the last year. | 6 | 0 |
| Pharmacists know the Municipal Health Plan. | 8 | 8 |
| PHC drugs purchased based on the schedule. | 6 | 0 |
| Prescribed medicines based on lists of medicines adopted by the municipality. | 6 | 6 |
| Medicines out of date available for dispensing. | 6 | 6 |
| Health services have a waste management plan. | 5 | 0 |
| The pharmacist’s productivity record has a defined procedure. | 7 | 0 |
| Spending on medicines to meet legal demands in relation to the budget to buy medicines, in the last year. | 6 | 6 |
| Schedule for regular distribution of medicines to health units: Monthly, biweekly, or weekly. | 6 | 6 |
| Prescribers receive information about the availability of medicines in pharmacies at health facilities. | 7 | 7 |
| Prescribers know how to find updates to the municipal list of medicines. | 8 | 8 |
| Amount of medications available in health facilities suitable to meet patients’ demands (perceptions of health secretary, PA coordinator, pharmacists, and prescribers). | 4 | 1 |
| Diversity of medications available in health facilities suitable to meet patients’ demands (perceptions of health secretary, PA coordinator, pharmacists, and prescribers). | 4 | 2 |
| Procedures for monitoring the PPS and using data to plan actions. | 6 | 0 |
| Resources diversity introduced in the municipal PPS in partnership with the State PPS. | 7 | 0 |
| Shared definitions about goals, guidelines, and targets PPS in the Municipal Health Plan. | 10 | 0 |
| Official means to receive criticisms and suggestions about medicines from patients (referred by the health unit coordinator). | 7 | 7 |
| Official means to receive criticisms and suggestions about medicines from patients (referred by patients). | 8 | 3 |
| Total | 125 | 70 |
| Technology component | ||
| Pharmacy and Therapeutics Committee has formal institution at the MHD. | 5 | 0 |
| Technical criteria used to prepare the medication schedule. | 6 | 0 |
| Municipal Medicines List Availability. | 6 | 5 |
| Municipal List of Medicines includes drugs are outside National List of Essential Medicines or lists agreed in SUS. | 5 | 5 |
| Instruments to standardize medication dispensing (SOP, manuals). | 6 | 0 |
| Total | 28 | 10 |
| Organizational culture component | ||
| Communication strategies between health units and PPS coordination to resolve medications issues (referred by health unit coordinators and pharmacists). | 7 | 7 |
| Articulation between PPS coordination, the Family Health Strategy coordination, and Community Agents Team. | 7 | 0 |
| Partnership between the municipality’s PPS Coordination and the State PPS Coordination. | 7 | 0 |
| PPS agenda at the meetings of the Municipal Health Council in the last 4 years. | 10 | 3 |
| Total | 31 | 10 |
| Description | Patients | Number of Visits | Number of Items | Quantity of Dispensed Items | Values of Total Dispensed Items (R$) |
|---|---|---|---|---|---|
| Daily average 1 | 928 | 971 | 145 | 71,043 | 8375.00 |
| Monthly Average 2 | 20,406 | 21,355 | 3193 | 1,562,936 | 184,254.00 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
da Bernardo, N.L.M.; Soares, L.; Leite, S.N. A Sociotechnical Approach to Analyze Pharmaceutical Policy and Services Management in Primary Health Care in a Brazilian Municipality. Pharmacy 2021, 9, 39. https://doi.org/10.3390/pharmacy9010039
da Bernardo NLM, Soares L, Leite SN. A Sociotechnical Approach to Analyze Pharmaceutical Policy and Services Management in Primary Health Care in a Brazilian Municipality. Pharmacy. 2021; 9(1):39. https://doi.org/10.3390/pharmacy9010039
Chicago/Turabian Styleda Bernardo, Noemia Liege Maria, Luciano Soares, and Silvana Nair Leite. 2021. "A Sociotechnical Approach to Analyze Pharmaceutical Policy and Services Management in Primary Health Care in a Brazilian Municipality" Pharmacy 9, no. 1: 39. https://doi.org/10.3390/pharmacy9010039
APA Styleda Bernardo, N. L. M., Soares, L., & Leite, S. N. (2021). A Sociotechnical Approach to Analyze Pharmaceutical Policy and Services Management in Primary Health Care in a Brazilian Municipality. Pharmacy, 9(1), 39. https://doi.org/10.3390/pharmacy9010039




