Challenges in the Development of Exoskeletons for People with Disabilities
Abstract
1. Introduction
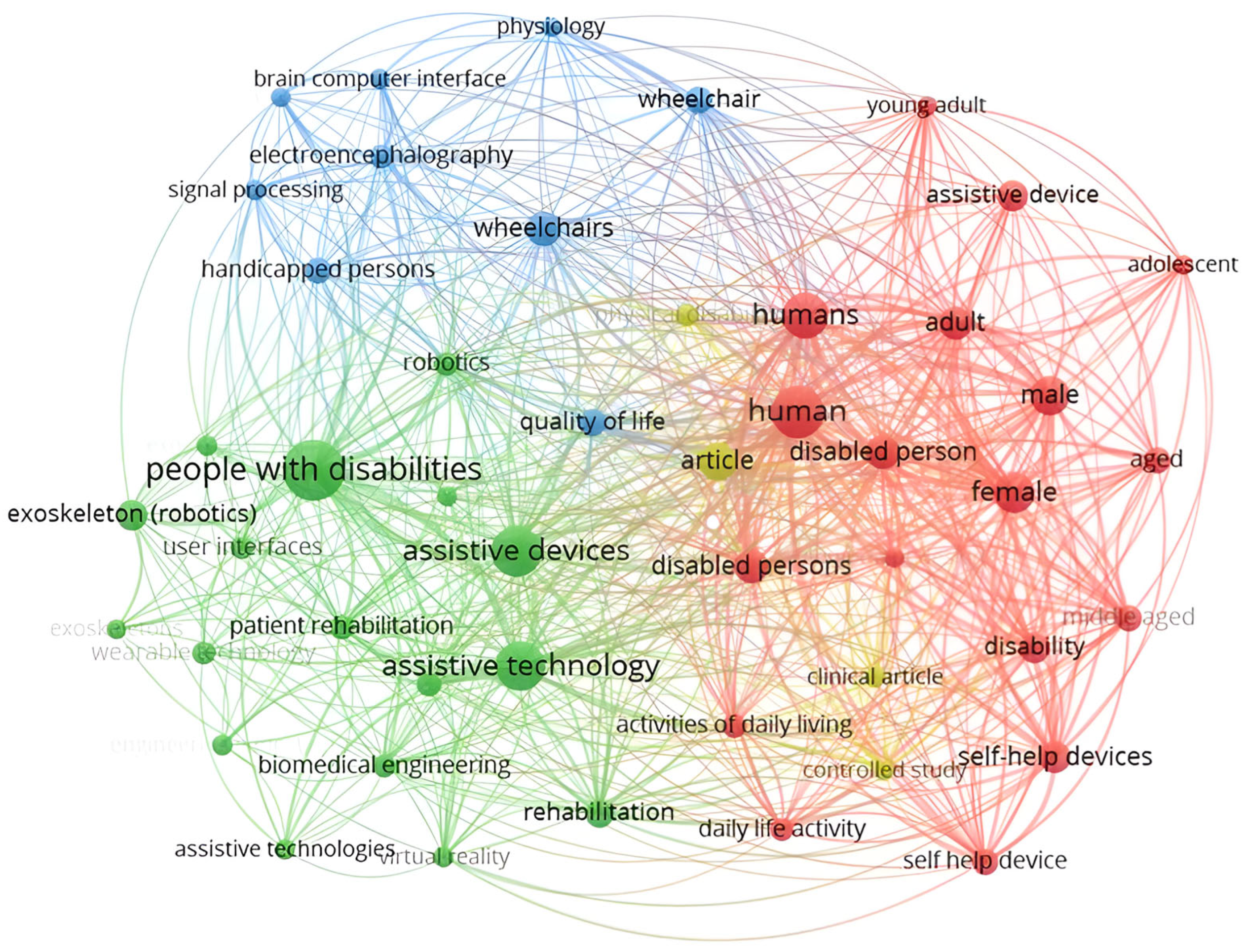
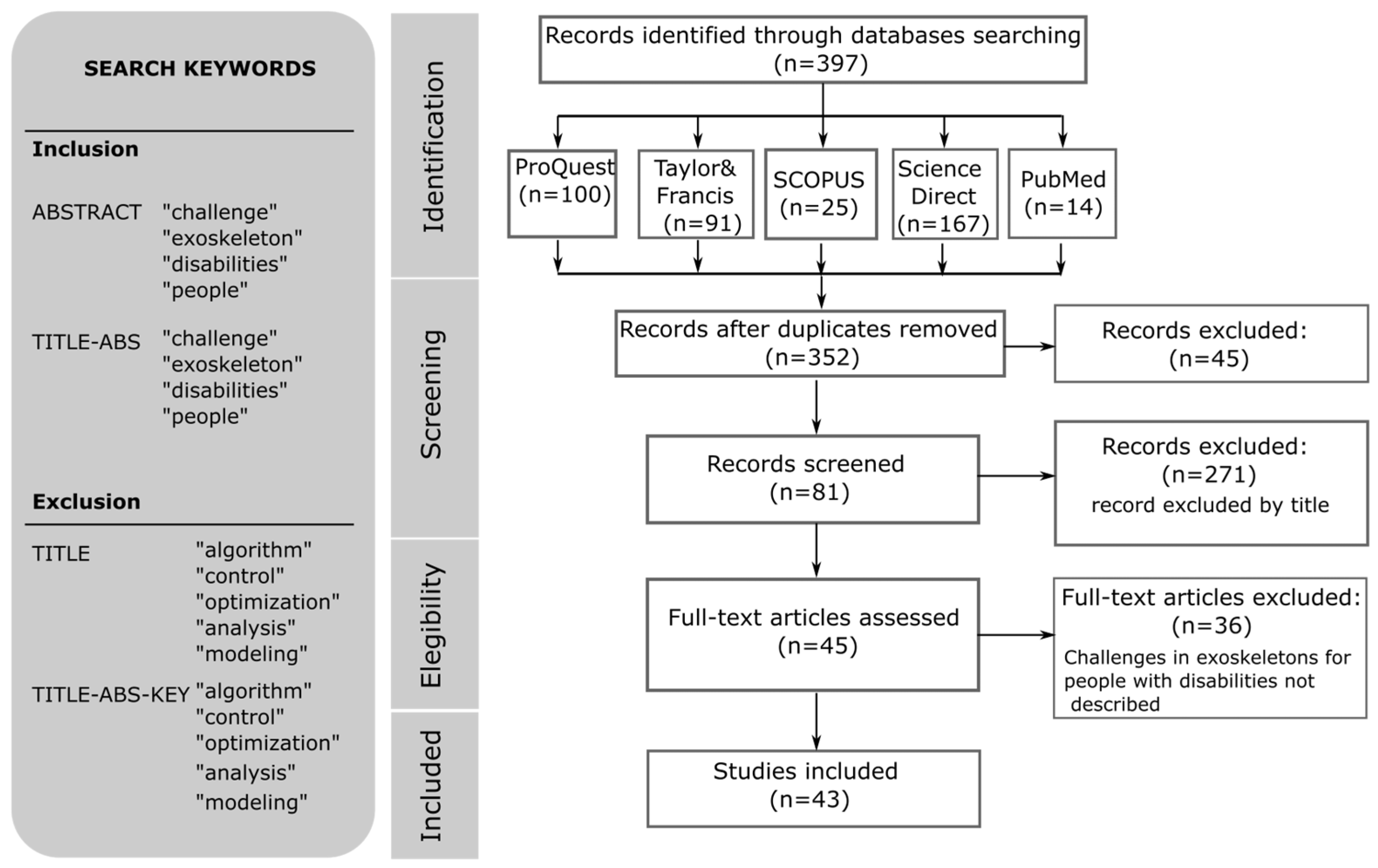
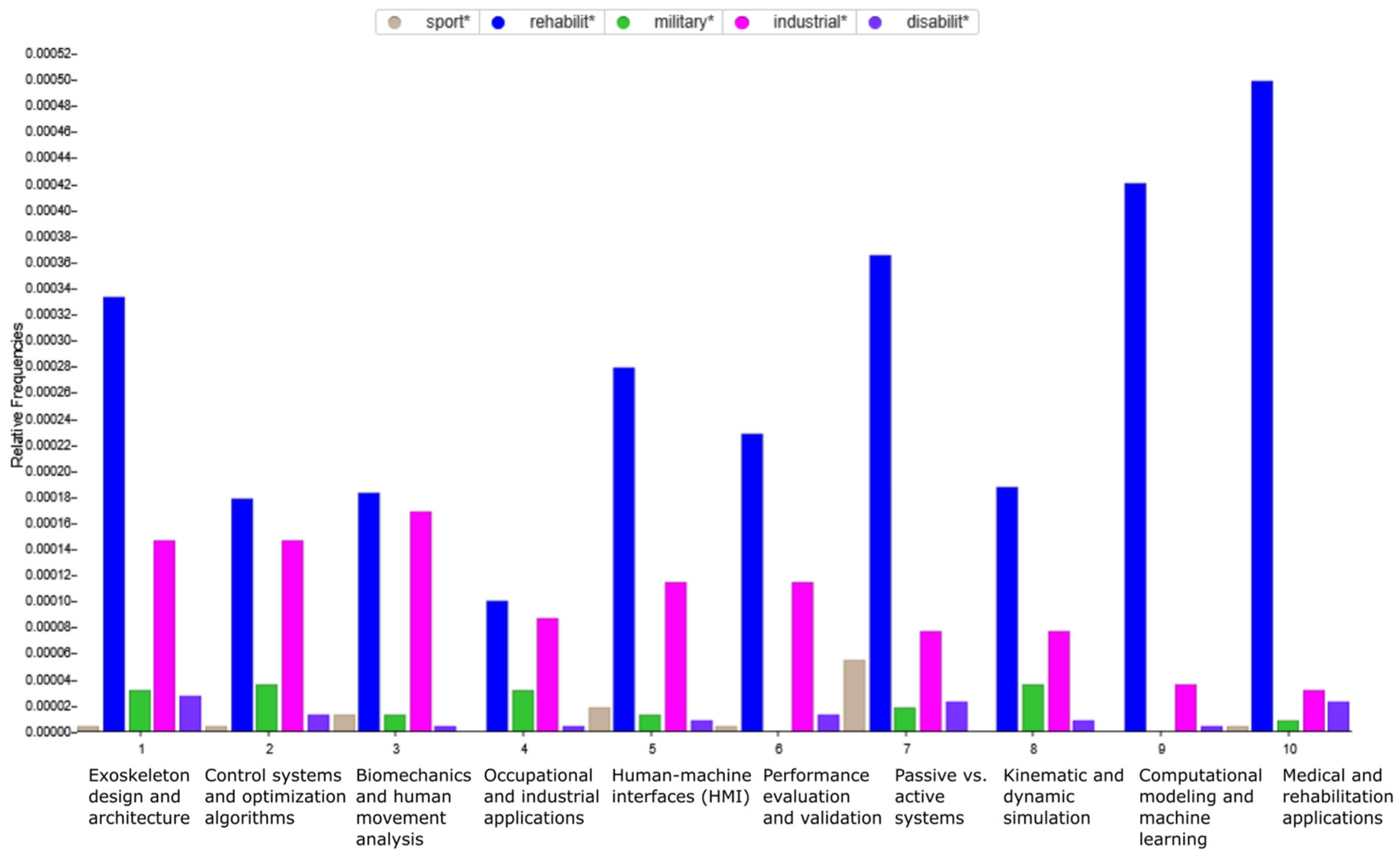
2. Methodology
2.1. Inclusion Criteria
2.2. Exclusion Criteria
3. Results
3.1. Upper Extremity Disability Exoskeletons
3.2. Lower Limb Disability Exoskeletons
3.3. Specific Features of Exoskeletons for People with Disabilities
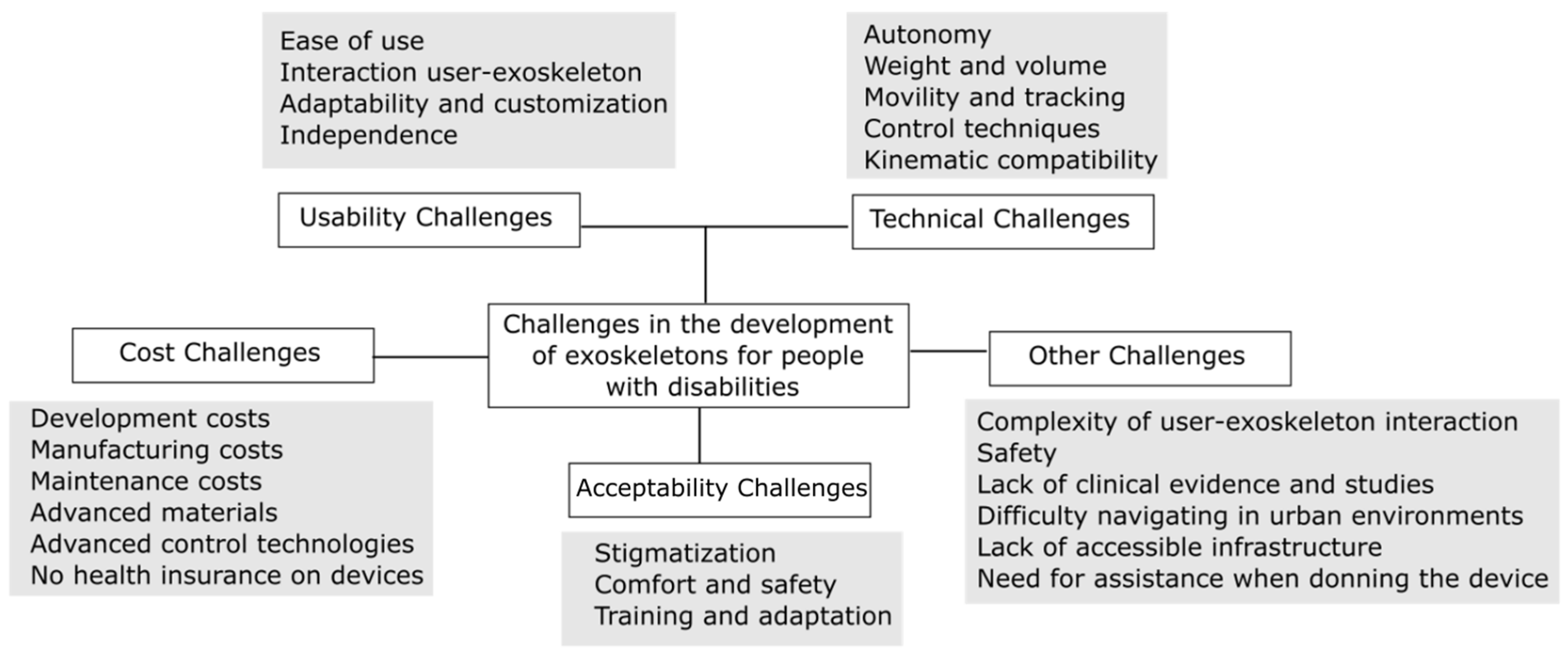
3.4. Developmental Challenges in Exoskeletons for People with Disabilities
3.4.1. Technical Challenges
3.4.2. Usability Challenges
3.4.3. Cost Challenges
3.4.4. User Acceptance Challenges
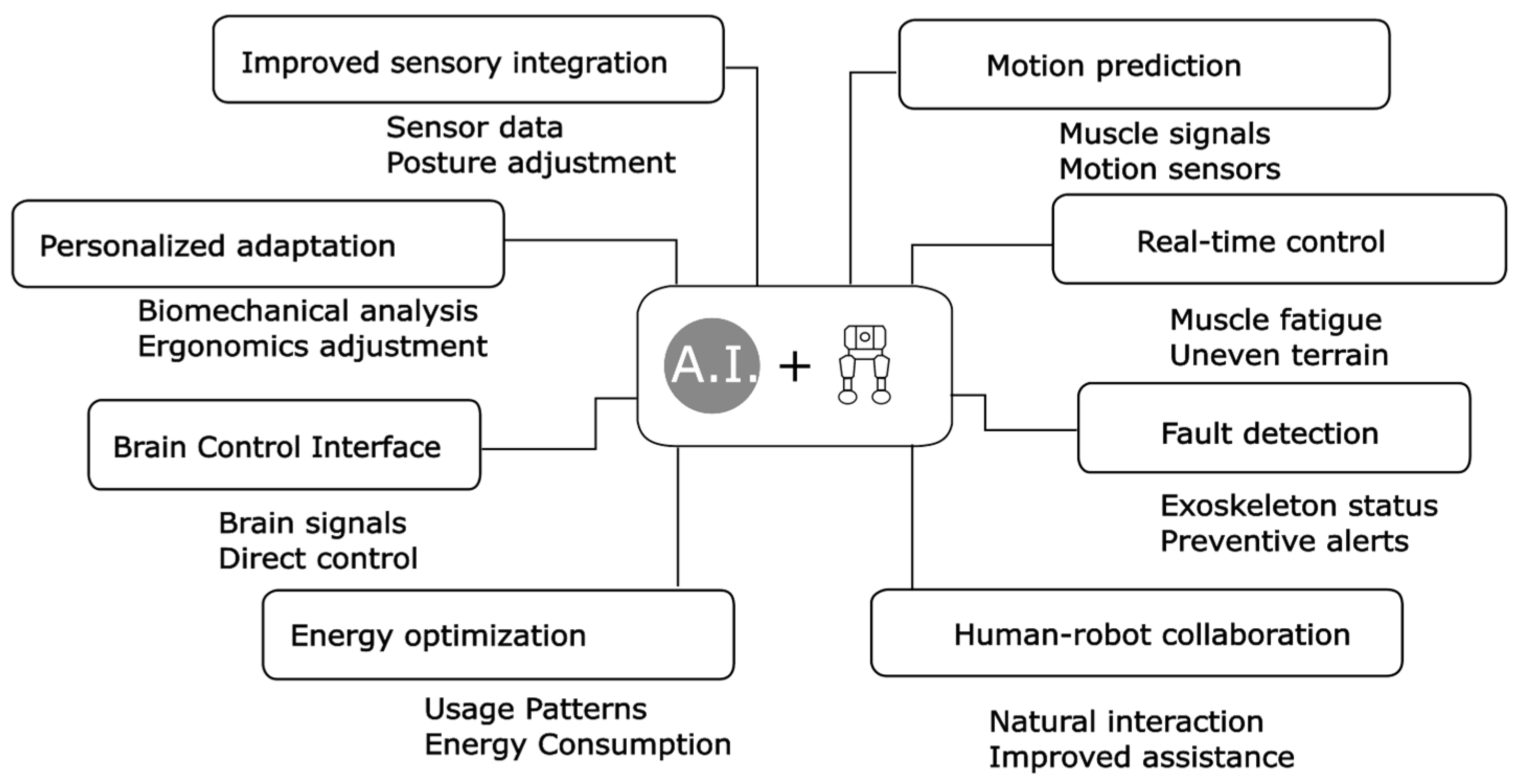
3.5. Perspectives on Future Developments in Exoskeletons for Disabilities
4. Discussion
4.1. Technical Aspects
4.2. Usability and User Acceptance
4.3. Cost and Technological Complexity
4.4. Absence of Clinical and End-User Perspectives
4.5. Other Challenges
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| SDGs | Sustainable development goals |
| RQ | Research questions |
| SJR | Scientific journal rankings |
| EMG | Electromyographic |
| EEG | Electroencephalographic |
| SMAs | Shape-memory alloys |
| AI | Artificial intelligence |
| BCIs | Brain–computer interfaces |
Appendix A
| SECTION | ITEM | PRISMA-ScR CHECKLIST ITEM | REPORTED ON PAGE # |
|---|---|---|---|
| TITLE | |||
| Title | 1 | Identify the report as a scoping review. | 1 |
| ABSTRACT | |||
| Structured summary | 2 | Provide a structured summary that includes (as applicable): background, objectives, eligibility criteria, sources of evidence, charting methods, results, and conclusions that relate to the review questions and objectives. | 1 |
| INTRODUCTION | |||
| Rationale | 3 | Describe the rationale for the review in the context of what is already known. Explain why the review questions/objectives lend themselves to a scoping review approach. | 1, 2, 3, 4 |
| Objectives | 4 | Provide an explicit statement of the questions and objectives being addressed with reference to their key elements (e.g., population or participants, concepts, and context) or other relevant key elements used to conceptualize the review questions and/or objectives. | 2 |
| METHODS | |||
| Protocol and registration | 5 | Indicate whether a review protocol exists; state if and where it can be accessed (e.g., a Web address); and if available, provide registration information, including the registration number. | 4, 5 |
| Eligibility criteria | 6 | Specify characteristics of the sources of evidence used as eligibility criteria (e.g., years considered, language, and publication status), and provide a rationale. | 5 |
| Information sources * | 7 | Describe all information sources in the search (e.g., databases with dates of coverage and contact with authors to identify additional sources), as well as the date the most recent search was executed. | 5 |
| Search | 8 | Present the full electronic search strategy for at least 1 database, including any limits used, such that it could be repeated. | 5 |
| Selection of sources of evidence † | 9 | State the process for selecting sources of evidence (i.e., screening and eligibility) included in the scoping review. | 5 |
| Data charting process ‡ | 10 | Describe the methods of charting data from the included sources of evidence (e.g., calibrated forms or forms that have been tested by the team before their use, and whether data charting was done independently or in duplicate) and any processes for obtaining and confirming data from investigators. | 5 |
| Data items | 11 | List and define all variables for which data were sought and any assumptions and simplifications made. | 5 |
| Critical appraisal of individual sources of evidence § | 12 | If performed, provide a rationale for conducting a critical appraisal of included sources of evidence; describe the methods used and how this information was used in any data synthesis (if appropriate). | 5 |
| Synthesis of results | 13 | Describe the methods of handling and summarizing the data that were charted. | 5, 6 |
| RESULTS | |||
| Selection of sources of evidence | 14 | Give numbers of sources of evidence screened, assessed for eligibility, and included in the review, with reasons for exclusions at each stage, ideally using a flow diagram. | 5–17 |
| Characteristics of sources of evidence | 15 | For each source of evidence, present characteristics for which data were charted and provide the citations. | - |
| Critical appraisal within sources of evidence | 16 | If performed, present data on critical appraisal of included sources of evidence (see Item 12). | - |
| Results of individual sources of evidence | 17 | For each included source of evidence, present the relevant data that were charted that relate to the review questions and objectives. | - |
| Synthesis of results | 18 | Summarize and/or present the charting results as they relate to the review questions and objectives. | 1, 7, 10 |
| DISCUSSION | |||
| Summary of evidence | 19 | Summarize the main results (including an overview of concepts, themes, and types of evidence available), link to the review questions and objectives, and consider the relevance to key groups. | 17, 18 |
| Limitations | 20 | Discuss the limitations of the scoping review process. | 2, 16 |
| Conclusions | 21 | Provide a general interpretation of the results with respect to the review questions and objectives, as well as potential implications and/or next steps. | 18 |
| FUNDING | |||
| Funding | 22 | Describe sources of funding for the included sources of evidence, as well as sources of funding for the scoping review. Describe the role of the funders of the scoping review. | 18 |
References
- Gull, M.A.; Thoegersen, M.; Bengtson, S.H.; Mohammadi, M.; Struijk, L.N.S.A.; Moeslund, T.B.; Bak, T.; Bai, S. A 4-DOF Upper Limb Exoskeleton for Physical Assistance: Design, Modeling, Control and Performance Evaluation. Appl. Sci. 2021, 11, 5865. [Google Scholar] [CrossRef]
- Catalan, J.M.; Blanco, A.; Bertomeu-Motos, A.; Garcia-Perez, J.V.; Almonacid, M.; Puerto, R.; Garcia-Aracil, N. A Modular Mobile Robotic Platform to Assist People with Different Degrees of Disability. Appl. Sci. 2021, 11, 7130. [Google Scholar] [CrossRef]
- Plessis, T.D.; Djouani, K.; Oosthuizen, C. A Review of Active Hand Exoskeletons for Rehabilitation and Assistance. Robotics 2021, 10, 40. [Google Scholar] [CrossRef]
- Panesar, S.; Wolbring, G. Analysis of North American Newspaper Coverage of Bionics Using the Disability Studies Framework. Technologies 2014, 2, 1–30. [Google Scholar] [CrossRef]
- Silva-Acosta, V.D.C.; Román-Godínez, I.; Torres-Ramos, S.; Salido-Ruiz, R.A. Automatic estimation of continuous elbow flexion–extension movement based on electromyographic and electroencephalographic signals. Biomed. Signal Process. Control. 2021, 70, 102950. [Google Scholar] [CrossRef]
- Wang, T.; Zhang, B.; Liu, C.; Liu, T.; Han, Y.; Wang, S.; Ferreira, J.P.; Dong, W.; Zhang, X. A Review on the Rehabilitation Exoskeletons for the Lower Limbs of the Elderly and the Disabled. Electronics 2022, 11, 388. [Google Scholar] [CrossRef]
- Schabron, B.; Desai, J.; Yihun, Y. Wheelchair-Mounted Upper Limb Robotic Exoskeleton with Adaptive Controller for Activities of Daily Living. Sensors 2021, 21, 5738. [Google Scholar] [CrossRef]
- Borisoff, J. Increasing the Safety and Effectiveness of Lower Limb Exoskeletons for Community Use. In Proceedings of the International Conference of Control, Dynamic Systems, and Robotics, Ottawa, ON, Canada, 9–10 May 2016. [Google Scholar] [CrossRef]
- Gandolla, M.; Antonietti, A.; Longatelli, V.; Gasperina, S.D.; Ambrosini, E.; Pedrocchi, A. Research Technologies for Assistance During Daily Life Activities. In XV Mediterranean Conference on Medical and Biological Engineering and Computing—MEDICON 2019; Henriques, J., Neves, N., De Carvalho, P., Eds.; IFMBE Proceedings; Springer International Publishing: Cham, Switzerland, 2020; Volume 76, pp. 1709–1713. [Google Scholar] [CrossRef]
- Benson, I.; Hart, K.; Tussler, D.; Van Middendorp, J.J. Lower-limb exoskeletons for individuals with chronic spinal cord injury: Findings from a feasibility study. Clin. Rehabil. 2015, 30, 73–84. [Google Scholar] [CrossRef]
- Johnson, M.J.; Keyvanian, S.; Mendonca, R.J. Toward inclusive rehabilitation robots. In Rehabilitation Robots for Neurorehabilitation in High-, Low-, and Middle-Income Countries; Elsevier: Amsterdam, The Netherlands, 2024; pp. 471–498. [Google Scholar] [CrossRef]
- Flor-Unda, O.; Casa, B.; Fuentes, M.; Solorzano, S.; Narvaez-Espinoza, F.; Acosta-Vargas, P. Exoskeletons: Contribution to Occupational Health and Safety. Bioengineering 2023, 10, 1039. [Google Scholar] [CrossRef]
- Fox, S.; Aranko, O.; Heilala, J.; Vahala, P. Exoskeletons: Comprehensive, comparative and critical analyses of their potential to improve manufacturing performance. JMTM 2019, 31, 1261–1280. [Google Scholar] [CrossRef]
- Bonello, A.; Francalanza, E.; Refalo, P. Smart and Sustainable Human-Centred Workstations for Operators with Disability in the Age of Industry 5.0: A Systematic Review. Sustainability 2023, 16, 281. [Google Scholar] [CrossRef]
- Näf, M.B.; Junius, K.; Rossini, M.; Rodriguez-Guerrero, C.; Vanderborght, B.; Lefeber, D. Misalignment Compensation for Full Human-Exoskeleton Kinematic Compatibility: State of the Art and Evaluation. Appl. Mech. Rev. 2018, 70, 050802. [Google Scholar] [CrossRef]
- Gonçalves, R.S.; Soares, G.; Carvalho, J.C. Conceptual design of a rehabilitation device based on cam-follower and crank-rocker mechanisms hand actioned. J. Braz. Soc. Mech. Sci. Eng. 2019, 41, 277. [Google Scholar] [CrossRef]
- Jayaraman, A.; Marinov, B.; Singh, Y.; Burt, S.; Rymer, W.Z. Current Evidence for Use of Robotic Exoskeletons in Rehabilitation. In Wearable Robotics; Elsevier: Amsterdam, The Netherlands, 2020; pp. 301–310. [Google Scholar] [CrossRef]
- Drużbicki, M.; Guzik, A.; Przysada, G.; Perenc, L.; Brzozowska-Magoń, A.; Cygoń, K.; Boczula, G.; Bartosik-Psujek, H. Effects of Robotic Exoskeleton-Aided Gait Training in the Strength, Body Balance, and Walking Speed in Individuals With Multiple Sclerosis: A Single-Group Preliminary Study. Arch. Phys. Med. Rehabil. 2021, 102, 175–184. [Google Scholar] [CrossRef]
- Flor, O.; Bustos-Estrella, A.; Palacios-Cabrera, H. Challenges in Disabilities People’s Exoskeletons. Mendeley Data, 2 April 2025. Available online: https://data.mendeley.com/datasets/6rd4h8b44m/1 (accessed on 5 May 2025).
- Corrigan, M.C.; Mathie, B.; Foulds, R.A. Translation of an upper extremity exoskeleton to home and community use for individuals with duchenne muscular dystrophy. In 2017 International Symposium on Wearable Robotics and Rehabilitation (WeRob); IEEE: Houston, TX, USA, 2017; pp. 1–2. [Google Scholar] [CrossRef]
- Li, B.; Cunha, A.B.; Kriner, S.M.; Lobo, M.A. Playskin AirTM: A Pediatric Pneumatic Exoskeleton for Children with Upper Extremity Disabilities. In Proceedings of the 2022 ACM International Symposium on Wearable Computers, Cambridge, UK, 11–15 September 2022; ACM: New York, NY, USA, 2022; pp. 123–126. [Google Scholar] [CrossRef]
- French, J.A.; Rose, C.G.; O’Malley, M.K. System Characterization of MAHI Exo-II: A Robotic Exoskeleton for Upper Extremity Rehabilitation. In Industrial Applications; Modeling for Oil and Gas, Control and Validation, Estimation, and Control of Automotive Systems; Multi-Agent and Networked Systems; Control System Design; Physical Human-Robot Interaction; Rehabilitation Robotics; Sensing and Actuation for Control; Biomedical Systems; Time Delay Systems and Stability; Unmanned Ground and Surface Robotics; Vehicle Motion Controls; Vibration Analysis and Isolation; Vibration and Control for Energy Harvesting; Wind Energy; American Society of Mechanical Engineers: San Antonio, TX, USA, 2014; Volume 3, p. V003T43A006. [Google Scholar] [CrossRef]
- Rahman, M.H.; Rahman, M.J.; Cristobal, O.L.; Saad, M.; Kenné, J.P.; Archambault, P.S. Development of a whole arm wearable robotic exoskeleton for rehabilitation and to assist upper limb movements. Robotica 2015, 33, 19–39. [Google Scholar] [CrossRef]
- Rahman, T.; Galloway, C.; Kokkoni, E.; Lobo, M. Development and Testing of a Modular Upper Extremity Exoskeleton for Infants. In Proceedings of the International Conference on Biomedical Electronics and Devices, ESEO, Angers, Loire Valley, France, 3–6 March 2014; SCITEPRESS—Science and Technology Publications: Setubal, Portugal, 2014; pp. 316–319. [Google Scholar] [CrossRef]
- Kozlowski, A.J.; Fabian, M.; Lad, D.; Delgado, A.D. Feasibility and Safety of a Powered Exoskeleton for Assisted Walking for Persons with Multiple Sclerosis: A Single-Group Preliminary Study. Arch. Phys. Med. Rehabil. 2017, 98, 1300–1307. [Google Scholar] [CrossRef]
- Rodríguez-Fernández, A.; Lobo-Prat, J.; Font-Llagunes, J.M. Systematic review on wearable lower-limb exoskeletons for gait training in neuromuscular impairments. J. Neuroeng. Rehabil. 2021, 18, 22. [Google Scholar] [CrossRef]
- Koljonen, P.A.; Virk, A.S.; Jeong, Y.; McKinley, M.; Latorre, J.; Caballero, A.; Hu, Y.; Wong, Y.W.; Cheung, K.; Kazerooni, H. Outcomes of a Multicenter Safety and Efficacy Study of the SuitX Phoenix Powered Exoskeleton for Ambulation by Patients with Spinal Cord Injury. Front. Neurol. 2021, 12, 689751. [Google Scholar] [CrossRef]
- Jyräkoski, T.; Merilampi, S.; Puustinen, J.; Kärki, A. Over-ground robotic lower limb exoskeleton in neurological gait rehabilitation: User experiences and effects on walking ability. Technol. Disabil. 2021, 33, 53–63. [Google Scholar] [CrossRef]
- Ju, Y. Lower limb rehabilitation exoskeleton robots: A review of development directions. In Proceedings of the Third International Conference on Intelligent Mechanical and Human-Computer Interaction Technology (IHCIT 2024), Hangzhou, China, 5–7 July 2024; Kong, X., Wang, X., Eds.; SPIE: Bellingham, WA, USA, 2024; p. 78. [Google Scholar] [CrossRef]
- Aach, M.; Schildhauer, T.A.; Zieriacks, A.; Jansen, O.; Weßling, M.; Brinkemper, A.; Grasmücke, D. Feasibility, safety, and functional outcomes using the neurological controlled Hybrid Assistive Limb exoskeleton (HAL®) following acute incomplete and complete spinal cord injury—Results of 50 patients. J. Spinal Cord Med. 2023, 46, 574–581. [Google Scholar] [CrossRef]
- Plaza, A.; Hernandez, M.; Puyuelo, G.; Garces, E.; Garcia, E. Wearable rehabilitation exoskeletons of the lower limb: Analysis of versatility and adaptability. Disabil. Rehabil. Assist. Technol. 2023, 18, 392–406. [Google Scholar] [CrossRef]
- Otálora, S.; Sergio, D.; Sierra, M.; Ballén-Moreno, F.; Múnera, M.; Cifuentes, C.A. Exploring Multimodal Gait Rehabilitation and Assistance through an Adaptable Robotic Platform. In Proceedings of the 2023 IEEE International Conference on Robotics and Automation (ICRA), London, UK, 29 May–2 June 2023; IEEE: New York, NY, USA, 2023; pp. 10449–10456. [Google Scholar] [CrossRef]
- Kerdraon, J.; Previnaire, J.G.; Tucker, M.; Coignard, P.; Allegre, W.; Knappen, E.; Ames, A. Evaluation of safety and performance of the self balancing walking system Atalante in patients with complete motor spinal cord injury. Spinal Cord Ser. Cases 2021, 7, 71. [Google Scholar] [CrossRef]
- González-España, J.J.; Sánchez-Rodríguez, L.; Pacheco-Ramírez, M.A.; Feng, J.; Nedley, K.; Chang, S.-H.; Francisco, G.E.; Contreras-Vidal, J.L. At-Home Stroke Neurorehabilitation: Early Findings with the NeuroExo BCI System. Sensors 2025, 25, 1322. [Google Scholar] [CrossRef]
- Kotov, S.V.; Romanov, A.I.; Silina, E.V.; Stupin, V.A.; Isakova, E.V.; Lijdvoy, V.Y.; Petrushanskaya, K.A.; Kotov, A.S.; Kodzokova, L.K.; Filatov, N.A.; et al. Efficiency of Leg Exoskeleton Use in Rehabilitation of Cerebral Stroke Patients. Serbian J. Exp. Clin. Res. 2021, 22, 257–264. [Google Scholar] [CrossRef]
- Woods, C.; Callagher, L.; Jaffray, T. Walk tall: The story of Rex Bionics. J. Manag. Organ. 2021, 27, 239–252. [Google Scholar] [CrossRef]
- Bioulac, B.; Jarry, B.; Ardaillou, R. Rapport 20-06—Interfaces cerveau-machine: Essais d’applications médicales, technologie et questions éthiques. Bull. L’académie Natl. Médecine 2021, 205, 118–129. [Google Scholar] [CrossRef]
- Martinez, A.; Tovar, L.; Amparan, C.I.; Gonzalez, K.; Edayath, P.; Pennathur, P.; Pennathur, A. Heuristic Evaluations of Back-Support, Shoulder-Support, Handgrip-Strength Support, and Sit-Stand-Support Exoskeletons Using Universal Design Principles. IISE Trans. Occup. Ergon. Hum. Factors 2025, 13, 18–31. [Google Scholar] [CrossRef]
- Infante, Y.Y.; Blanco, A.E.; Jonguitud, A.E. The exoskeleton: Operation with electrostimulators for rehabilitation. In Proceedings of the 2019 IEEE International Conference on Engineering Veracruz (ICEV), Boca del Rio, Veracruz, Mexico, 14–17 October 2019; IEEE: New York, NY, USA, 2019; pp. 1–4. [Google Scholar] [CrossRef]
- Nolan, K.J.; Karunakaran, K.K.; Roberts, P.; Tefertiller, C.; Walter, A.M.; Zhang, J.; Leslie, D.; Jayaraman, A.; Francisco, G.E. Utilization of Robotic Exoskeleton for Overground Walking in Acute and Chronic Stroke. Front. Neurorobot. 2021, 15, 689363. [Google Scholar] [CrossRef]
- Pilla, A.; Trigili, E.; McKinney, Z.; Fanciullacci, C.; Malasoma, C.; Posteraro, F.; Crea, S.; Vitiello, N. Robotic Rehabilitation and Multimodal Instrumented Assessment of Post-stroke Elbow Motor Functions—A Randomized Controlled Trial Protocol. Front. Neurol. 2020, 11, 587293. [Google Scholar] [CrossRef]
- Lee, H.; Ferguson, P.W.; Rosen, J. Lower Limb Exoskeleton Systems—Overview. In Wearable Robotics; Elsevier: Amsterdam, The Netherlands, 2020; pp. 207–229. [Google Scholar] [CrossRef]
- Blanchet, L.; Achiche, S.; Docquier, Q.; Fisette, P.; Raison, M. A procedure to optimize the geometric and dynamic designs of assistive upper limb exoskeletons. Multibody Syst. Dyn. 2020, 51, 221–245. [Google Scholar] [CrossRef]
- Alhamad, R.; Seth, N.; Abdullah, H.A. Initial testing of robotic exoskeleton hand device for stroke rehabilitation. Sensors 2023, 23, 6339. [Google Scholar] [CrossRef]
- Batkuldinova, K.; Abilgaziyev, A.; Shehab, E.; Ali, M.H. The recent development of 3D printing in developing lower-leg exoskeleton: A review. Mater. Today Proc. 2021, 42, 1822–1828. [Google Scholar] [CrossRef]
- Nie “Miraze Zdrowia. A Naukowo Uzasadnione Zabezpieczenie Zdrowia i Szcześ. Available online: https://journals.indexcopernicus.com/search/article?articleId=338816 (accessed on 4 June 2025).
- Dharmik, A.L.; Atre, S.K.; Sharma, S.J. Design of an Exoskeleton for Hand Rehabilitation. In Proceedings of the 2022 IEEE Conference on Interdisciplinary Approaches in Technology and Management for Social Innovation (IATMSI), Gwalior, India, 21–23 December 2022; IEEE: New York, NY, USA, 2022; pp. 1–4. [Google Scholar] [CrossRef]
- Alqahtani, M.S.; Cooper, G.; Diver, C.; Bártolo, P.J. Exoskeletons for Lower Limb Applications: A Review. In Bio-Materials and Prototyping Applications in Medicine; Bártolo, P.J., Bidanda, B., Eds.; Springer International Publishing: Cham, Switzerland, 2021; pp. 139–164. [Google Scholar] [CrossRef]
- Sharma, C.A.A.; Kumar, A.S.K.S.V.; Prasad, A.; Begum, R.; Sharvani, G.S.; Manjunath, A.E. Multifaceted bio-medical applications of exoskeleton: A review. In Proceedings of the 2018 2nd International Conference on Inventive Systems and Control (ICISC), Coimbatore, India, 19–20 January 2018; IEEE: New York, NY, USA, 2018; pp. 11–15. [Google Scholar] [CrossRef]
- Tanveer, M.H.; Koduru, C.; Voicu, R.C.; Ham, C. Exoskeleton-Wheelchair Synergy for Rehabilitation & User Assistance. In Proceedings of the 2022 7th International Conference on Automation, Control and Robotics Engineering (CACRE), Xi’an, China, 15–16 July 2022; IEEE: New York, NY, USA, 2022; pp. 313–317. [Google Scholar] [CrossRef]
- Pillai, B.M.; Owatchaiyapong, P.; Treratanakulchai, S.; Sivaraman, D.; Ongwattanakul, S.; Suthakorn, J. Lower Limb Exoskeleton With Energy-Storing Mechanism for Spinal Cord Injury Rehabilitation. IEEE Access 2023, 11, 133850–133866. [Google Scholar] [CrossRef]
- Mittapally, S.R.; Srinivasan, S.; Rakshit, S. Design Optimization of Series Elastic Actuator (SEA) for Lower Limb Rehabilitation Exoskeleton. In Recent Advances in Machines, Mechanisms, Materials and Design; Kumar, R.S., Sanyal, S., Pathak, P.M., Eds.; Lecture Notes in Mechanical Engineering; Springer Nature: Singapore, 2024; pp. 755–766. [Google Scholar] [CrossRef]
- Lacuata, N.; O’dell, B.; John, A.; Pelletier, C.; Jefferson, D.; Lineberger, R.; Sharifi, M. Design and Fabrication of a Modular, Lightweight, and Portable Upper Limb Exoskeleton for Shoulder and Elbow. In Biomedical and Biotechnology; American Society of Mechanical Engineers: New Orleans, LA, USA, 2023; Volume 5, p. V005T06A063. [Google Scholar] [CrossRef]
- Terrazas-Rodas, D.; Rocca-Huaman, L.; Ramirez-Amaya, C.; Requejo-Rosales, J.; Gutierrez-Atacusi, J.; Estacio-Cayetano, F. Control Systems in Lower-limb Exoskeletons for Rehabilitation and/or Assistance: A Brief Review. In Proceedings of the 2022 International Conference on Smart Systems and Power Management (IC2SPM), Beirut, Lebanon, 10–12 November 2022; IEEE: New York, NY, USA, 2022; pp. 117–123. [Google Scholar] [CrossRef]
- Androwis, G.J.; Karunakaran, K.; Nunez, E.; Michael, P.; Yue, G.; Foulds, R.A. Research and development of new generation robotic exoskeleton for over ground walking in individuals with mobility disorders (Novel design and control). In Proceedings of the 2017 International Symposium on Wearable Robotics and Rehabilitation (WeRob), Houston, TX, USA, 5–8 November 2017; IEEE: New York, NY, USA, 2017; pp. 1–2. [Google Scholar] [CrossRef]
- Eguren, D.; Cestari, M.; Luu, T.P.; Kilicarslan, A.; Steele, A.; Contreras-Vidal, J.L. Design of a customizable, modular pediatric exoskeleton for rehabilitation and mobility. In Proceedings of the 2019 IEEE International Conference on Systems, Man and Cybernetics (SMC), Bari, Italy, 6–9 October 2019; IEEE: New York, NY, USA, 2019; pp. 2411–2416. [Google Scholar] [CrossRef]
- Lim, Y.X.; Sharifi, M. A Chain-Based Cable-Driven Upper-Limb Exoskeleton: Design, Mechanical Analysis and Development. In Proceedings of the 2024 International Symposium on Medical Robotics (ISMR), Atlanta, GA, USA, 3–5 June 2024; IEEE: New York, NY, USA, 2024; pp. 1–7. [Google Scholar] [CrossRef]
- Dhatrak, P.; Durge, J.; Dwivedi, R.K.; Pradhan, H.K.; Kolke, S. Interactive design and challenges on exoskeleton performance for upper-limb rehabilitation: A comprehensive review. Int. J. Interact. Des. Manuf. 2024, 19, 4565–4587. [Google Scholar] [CrossRef]
- McGibbon, C.; Sexton, A.; Gryfe, P.; Dutta, T.; Jayaraman, A.; Deems-Dluhy, S.; Novak, A.; Fabara, E.; Adans-Dester, C.; Bonato, P. Effect of using of a lower-extremity exoskeleton on disability of people with multiple sclerosis. Disabil. Rehabil. Assist. Technol. 2023, 18, 475–482. [Google Scholar] [CrossRef]
- Bhatnagar, T.; Mortensen, W.B.; Mattie, J.; Wolff, J.; Parker, C.; Borisoff, J. A survey of stakeholder perspectives on a proposed combined exoskeleton-wheelchair technology. In Proceedings of the 2017 International Conference on Rehabilitation Robotics (ICORR), London, UK, 17–20 July 2017; IEEE: New York, NY, USA, 2017; pp. 1574–1579. [Google Scholar] [CrossRef]
- De Luca, R.; Maresca, G.; Balletta, T.; Cannavò, A.; Leonardi, S.; Latella, D.; Maggio, M.G.; Portaro, S.; Naro, A.; Calabrò, R.S. Does overground robotic gait training improve non-motor outcomes in patients with chronic stroke? Findings from a pilot study. J. Clin. Neurosci. 2020, 81, 240–245. [Google Scholar] [CrossRef]
- Planelles, D.; Hortal, E.; Costa, Á.; Úbeda, A.; Iáez, E.; Azorín, J. Evaluating Classifiers to Detect Arm Movement Intention from EEG Signals. Sensors 2014, 14, 18172–18186. [Google Scholar] [CrossRef]
- Fu, J.; Choudhury, R.; Hosseini, S.M.; Simpson, R.; Park, J.-H. Myoelectric Control Systems for Upper Limb Wearable Robotic Exoskeletons and Exosuits—A Systematic Review. Sensors 2022, 22, 8134. [Google Scholar] [CrossRef]
- Lee, H.; Kim, S.H.; Park, H.-S. A Fully Soft and Passive Assistive Device to Lower the Metabolic Cost of Sit-to-Stand. Front. Bioeng. Biotechnol. 2020, 8, 966. [Google Scholar] [CrossRef]
- Brahmi, B.; Dahani, H.; Bououden, S.; Farah, R.; Rahman, M.H. Adaptive-Robust Controller for Smart Exoskeleton Robot. Sensors 2024, 24, 489. [Google Scholar] [CrossRef]
- Andrade, R.M.; Sapienza, S.; Mohebbi, A.; Fabara, E.E.; Bonato, P. Overground Walking with a Transparent Exoskeleton Shows Changes in Spatiotemporal Gait Parameters. IEEE J. Transl. Eng. Health Med. 2024, 12, 182–193. [Google Scholar] [CrossRef]
- Qi, W.; Xu, X.; Qian, K.; Schuller, B.W.; Fortino, G.; Aliverti, A. A Review of AIoT-Based Human Activity Recognition: From Application to Technique. IEEE J. Biomed. Health Inform. 2025, 29, 2425–2438. [Google Scholar] [CrossRef]
- Delgado, P.; Jaradat, L.; Yihun, Y. Assessment of Task and Joint-Based Exoskeleton Designs for Elbow Joint Rehabilitation. In Proceedings of the 2022 Design of Medical Devices Conference, Minneapolis, MN, USA, 11–14 April 2022; American Society of Mechanical Engineers: New York, NY, USA, 2022; p. V001T07A002. [Google Scholar] [CrossRef]
- Secciani, N.; Bianchi, M.; Ridolfi, A.; Vannetti, F.; Volpe, Y.; Governi, L.; Bianchini, M.; Allotta, B. Tailor-Made Hand Exoskeletons at the University of Florence: From Kinematics to Mechatronic Design. Machines 2019, 7, 22. [Google Scholar] [CrossRef]
- Nasr, A.; Inkol, K.; McPhee, J. Safety in Wearable Robotic Exoskeletons: Design, Control, and Testing Guidelines. J. Mech. Robot. 2025, 17, 050801. [Google Scholar] [CrossRef]
- Kladovasilakis, N.; Kostavelis, I.; Sideridis, P.; Koltzi, E.; Piliounis, K.; Tzetzis, D.; Tzovaras, D. A Novel Soft Robotic Exoskeleton System for Hand Rehabilitation and Assistance Purposes. Appl. Sci. 2023, 13, 553. [Google Scholar] [CrossRef]
- Zhao, Y.; Mao, J.; Todoh, M. Development of a portable assistive exoskeleton for human arm movements. Electron. Lett. 2023, 59, e12785. [Google Scholar] [CrossRef]
- Liu, C.; Wen, J.; Zhu, P. Upper Limb and Back Rehabilitation Exoskeleton. In Proceedings of the 2023 IEEE International Conference on Electrical, Automation and Computer Engineering (ICEACE), Changchun, China, 29–31 December 2023; IEEE: New York, NY, USA, 2023; pp. 206–213. [Google Scholar] [CrossRef]
- Li, J.; Gu, X.; Qiu, S.; Zhou, X.; Cangelosi, A.; Loo, C.K.; Liu, X. A Survey of Wearable Lower Extremity Neurorehabilitation Exoskeleton: Sensing, Gait Dynamics, and Human–Robot Collaboration. IEEE Trans. Syst. Man Cybern. Syst. 2024, 54, 3675–3693. [Google Scholar] [CrossRef]
- Missiroli, F.; Ferrazzi, F.; Tricomi, E.; Casadio, M.; Masia, L. Assistive Force Myography Controlled Exoglove. IEEE Trans. Med. Robot. Bionics 2025, 7, 27–32. [Google Scholar] [CrossRef]
- Rojek, I.; Kaczmarek, M.; Kotlarz, P.; Kempiński, M.; Mikołajewski, D.; Szczepański, Z.; Kopowski, J.; Nowak, J.; Macko, M.; Szczepańczyk, A.; et al. Hand Exoskeleton—Development of Own Concept. Appl. Sci. 2023, 13, 3238. [Google Scholar] [CrossRef]
- Akbas, B.; Yuksel, H.T.; Soylemez, A.; Zyada, M.E.; Sarac, M.; Stroppa, F. The Impact of Evolutionary Computation on Robotic Design: A Case Study with an Underactuated Hand Exoskeleton. In Proceedings of the 2024 IEEE International Conference on Robotics and Automation (ICRA), Yokohama, Japan, 13–17 May 2024; IEEE: New York, NY, USA, 2024; pp. 5519–5525. [Google Scholar] [CrossRef]
- Kumar, N.A.; Patrick, S.; Hur, P. Pilot Study on the Needs of Prospective Exoskeleton Users with Impaired Mobility. In Proceedings of the 2019 IEEE International Conference on Advanced Robotics and its Social Impacts (ARSO), Beijing, China, 31 October–2 November 2019; IEEE: New York, NY, USA, 2019; pp. 106–111. [Google Scholar] [CrossRef]
- Reyes-Cruz, A.; Beltrán-Fernández, J.A.; Hernández-Gómez, L.H.; Cazares-Ramírez, I.O.; González, A.G.-R.Y.; Flores-Campos, J.A.; López-Lievano, A. Design and Methodology to Produce Auxiliary Orthopedic Rehabilitation. In Engineering Design Applications; Öchsner, A., Altenbach, H., Eds.; Advanced Structured Materials; Springer International Publishing: Cham, Switzerland, 2019; Volume 92, pp. 383–391. [Google Scholar] [CrossRef]
- Ableitner, T.; Soekadar, S.; Schilling, A.; Strobbe, C.; Zimmermann, G. User acceptance of augmented reality glasses in comparison to other interaction methods for controlling a hand exoskeleton. In Proceedings of the Mensch und Computer 2019, Hamburg, Germany, 8–11 September 2019. [Google Scholar] [CrossRef]
- Wee, S.K.; Ho, C.Y.; Tan, S.L.; Ong, C.H. Enhancing quality of life in progressive multiple sclerosis with powered robotic exoskeleton. Mult. Scler. J. 2020, 27, 483–487. [Google Scholar] [CrossRef]
- Butnaru, D. Temporarily Abled: How Exoskeleton Experience Reinvents Bodies in Spinal Cord Injury and Cerebrovascular Accidents. Nanoethics 2022, 16, 51–64. [Google Scholar] [CrossRef]
- Afzal, T.; Tseng, S.-C.; Lincoln, J.A.; Kern, M.; Francisco, G.E.; Chang, S.-H. Exoskeleton-assisted Gait Training in Persons with Multiple Sclerosis: A Single-Group Pilot Study. Arch. Phys. Med. Rehabil. 2020, 101, 599–606. [Google Scholar] [CrossRef]
- Ii, T.; Hirano, S.; Tanabe, S.; Saitoh, E.; Yamada, J.; Mukaino, M.; Watanabe, M.; Sonoda, S.; Otaka, Y. Robot-assisted Gait Training Using Welwalk in Hemiparetic Stroke Patients: An Effectiveness Study with Matched Control. J. Stroke Cerebrovasc. Dis. 2020, 29, 105377. [Google Scholar] [CrossRef]
- Pournajaf, S.; Morone, G.; Straudi, S.; Goffredo, M.; Leo, M.R.; Calabrò, R.S.; Felzani, G.; Paolucci, S.; Filoni, S.; Santamato, A.; et al. Neurophysiological and Clinical Effects of Upper Limb Robot-Assisted Rehabilitation on Motor Recovery in Patients with Subacute Stroke: A Multicenter Randomized Controlled Trial Study Protocol. Brain Sci. 2023, 13, 700. [Google Scholar] [CrossRef]
- Berson, J.; Nenert, P.; Choplin, A. La place des exosquelettes d’assistance dans le quotidien des personnes blessées médullaires. Kinésithérapie Rev. 2021, 21, 20–26. [Google Scholar] [CrossRef]
- Sathish, K.; Manickaraj, K.; Krishna, S.A.; Basha, K.M.; Pravin, R. Integrating sustainable materials in exoskeleton development: A review. In Proceedings of the Fifth Scientific Conference for Electrical Engineering Techniques Research (EETR2024), Baghdad, Iraq, 15–16 June 2024; p. 020021. [Google Scholar] [CrossRef]
- Androwis, G.J.; Sandroff, B.M.; Niewrzol, P.; Fakhoury, F.; Wylie, G.R.; Yue, G.; DeLuca, J. A pilot randomized controlled trial of robotic exoskeleton-assisted exercise rehabilitation in multiple sclerosis. Mult. Scler. Relat. Disord. 2021, 51, 102936. [Google Scholar] [CrossRef]
- Lee, S.-M.; Park, J. A soft wearable exoglove for rehabilitation assistance: A novel application of knitted shape-memory alloy as a flexible actuator. Fash Text 2024, 11, 14. [Google Scholar] [CrossRef]
- Wolff, J.; Parker, C.; Borisoff, J.; Mortenson, W.B.; Mattie, J. A survey of stakeholder perspectives on exoskeleton technology. J. Neuroeng. Rehabil. 2014, 11, 169. [Google Scholar] [CrossRef]
- Van Silfhout, L.; Hosman, A.J.F.; Van De Meent, H.; Bartels, R.H.M.A.; Edwards, M.J.R. Design recommendations for exoskeletons: Perspectives of individuals with spinal cord injury. J. Spinal Cord Med. 2023, 46, 256–261. [Google Scholar] [CrossRef]
- Hampshire, L.; Dehghani-Sanij, A.; O’Connor, R.J. Restorative rehabilitation robotics to promote function, independence and dignity: Users’ perspectives on clinical applications. J. Med. Eng. Technol. 2022, 46, 527–535. [Google Scholar] [CrossRef]
- Ferris, D.P.; Schlink, B.R.; Young, A.J. Robotics: Exoskeletons. In Encyclopedia of Biomedical Engineering; Elsevier: Amsterdam, The Netherlands, 2019; pp. 645–651. [Google Scholar] [CrossRef]
- Kapeller, A.; Nagenborg, M.H.; Nizamis, K. Wearable robotic exoskeletons: A socio-philosophical perspective on Duchenne muscular dystrophy research. Paladyn J. Behav. Robot. 2020, 11, 404–413. [Google Scholar] [CrossRef]
- Cheng, C.Y.M.; Lee, C.C.Y.; Chen, C.K.; Lou, V.W.Q. Multidisciplinary collaboration on exoskeleton development adopting user-centered design: A systematic integrative review. Disabil. Rehabil. Assist. Technol. 2024, 19, 909–937. [Google Scholar] [CrossRef]
- Li, H.; Cheng, L. A Systematic Review on Hand Exoskeletons from the Mechatronics Aspect. IEEE/ASME Trans. Mechatron 2024, 1–19. [Google Scholar] [CrossRef]
- Canela, M.; Del Ama, A.J.; Pons, J.L. Design of a Pediatric Exoskeleton for the Rehabilitation of the Physical Disabilities Caused by Cerebral Palsy. In Converging Clinical and Engineering Research on Neurorehabilitation; Pons, J.L., Torricelli, D., Pajaro, M., Eds.; Biosystems & Biorobotics; Springer: Berlin/Heidelberg, Germany, 2013; Volume 1, pp. 255–258. [Google Scholar] [CrossRef]
- Rupal, B.S.; Rafique, S.; Singla, A.; Singla, E.; Isaksson, M.; Virk, G.S. Lower-limb exoskeletons: Research trends and regulatory guidelines in medical and non-medical applications. Int. J. Adv. Robot. Syst. 2017, 14, 172988141774355. [Google Scholar] [CrossRef]
- Rajasekaran, V.; López-Larraz, E.; Trincado-Alonso, F.; Aranda, J.; Montesano, L.; Del-Ama, A.J.; Pons, J.L. Volition-adaptive control for gait training using wearable exoskeleton: Preliminary tests with incomplete spinal cord injury individuals. J. Neuroeng. Rehabil. 2018, 15, 4. [Google Scholar] [CrossRef]
- Khan, N.A.; Hussain, S.; Spratford, W.; Goecke, R.; Kotecha, K.; Jamwal, P.K. Deep Learning-Driven Analysis of a Six-Bar Mechanism for Personalized Gait Rehabilitation. J. Comput. Inf. Sci. Eng. 2025, 25, 011001. [Google Scholar] [CrossRef]
- Chandrapal, M.; Chen, X.; Wang, W. Intelligent Assistive Knee Exoskeleton. In Mechatronics, 1st ed.; Davim, J.P., Ed.; Wiley: Hoboken, NJ, USA, 2013; pp. 195–237. [Google Scholar] [CrossRef]
- Coser, O.; Tamantini, C.; Soda, P.; Zollo, L. AI-based methodologies for exoskeleton-assisted rehabilitation of the lower limb: A review. Front. Robot. AI 2024, 11, 1341580. [Google Scholar] [CrossRef]
- Kahali, S.; Ngo, T.; Mandahar, T.S.; Martínez-Bueno, E.; Guerrero-Rosado, O.; López-Carral, H.; Freire, I.T.; Mura, A.; Verschure, P.F.M.J. Distributed Adaptive Control for Virtual Cyborgs: A Case Study for Personalized Rehabilitation. In Biomimetic and Biohybrid Systems; Meder, F., Hunt, A., Margheri, L., Mura, A., Mazzolai, B., Eds.; Lecture Notes in Computer Science; Springer Nature: Cham, Switzerland, 2023; Volume 14157, pp. 16–32. [Google Scholar] [CrossRef]


| Quality Assessment Questions | Answer |
|---|---|
| Does the document describe designs or prototypes of exoskeletons specifically developed, or can people with disabilities use them? | (+1) Yes/(+0) No |
| Does the document describe the uses, characteristics, or impacts of exoskeletons on people with disabilities? | (+1) Yes/(+0) No |
| Does the paper highlight the challenges and limitations of developing or implementing exoskeletons for use by people with disabilities? | (+1) Yes/(+0) No |
| Is the journal or conference in which the article was published indexed in the SJR? | (+1) if it is ranked Q1, (+0.75) if it is ranked Q2, (+0.50) if it is ranked Q3, (+0.25) if it is ranked Q4, (+0.0) if it is not ranked |
| Database | String Search | Studies Number |
|---|---|---|
| ProQuest | exoeskeletons (Topic) and disabilities (Topic) | 100 |
| Taylor & Francis | [Abstract: exoeskeletons challenges] AND [Abstract: disabilities] | 91 |
| Scopus | ALL (“exoeskeletons” “disabilities” “challenges”) | 25 |
| Science Direct | “exoeskeletons” “technologies” “disabilities” | 167 |
| PubMed | Search: (exoeskeletons) AND (disabilities) AND (Technologies) | 14 |
| Total number of studies | 397 |
| Feature | General Exoskeletons | Exoskeletons for Specific Disabilities |
|---|---|---|
| Primary Use | Military, industrial, general medical [38] | Rehabilitation, daily assistance [8,39,40,41] |
| Design Focus | Strength, performance, ergonomics [42,43] | Customization, user comfort, adaptive control [8] |
| Control Mechanisms | Electrical motors, impedance control, force control [42] | EMG sensors, electro-stimulators, specialized control strategies [39,41,44] |
| Control Systems | Advanced synchronization with human movements [38,45] | Biosignal-based, adaptive to user needs [41,44] |
| Safety and Usability | General safety features [43,46] | High priority on minimizing fall risk, ease of use, comfort [8] |
| User Benefits | Enhanced capabilities, reduced fatigue [42] | Mobility restoration, improved quality of life [40,47] |
| Category | Identified Challenges | Proposed Category |
|---|---|---|
| Mechanical and Ergonomic | Joint misalignment and poor fit [68,70] | Highly customizable designs [69,76] |
| Control and Sensing | Excess weight and mobility restriction [69,72] | Use of lightweight materials and 3D printing [71,72] |
| Energy and Power | Mechanical failures [70] | Evolutionary computation methods like genetic algorithms [77] |
| Interaction and Safety | Complex control algorithms [70,73] | Force myography (FMG) for reliable control [75] |
| Customization and Accessibility | Sensor failures and unreliable feedback [70,74] | Efficient power systems and regenerative energy solutions [70,74] |
| Challenge | Description | Reference |
|---|---|---|
| Technical | Weight, size, battery life, control systems, kinematic compatibility | [15,16,65,66,72] |
| Usability | Ease of use, interaction forces, mobility, and independency | [8,15,78] |
| Cost | High manufacturing costs, affordability | [72,79] |
| User acceptance | Stigmatization, comfort and safety, training and adaptation | [10,81,82] |
| Others | Complexity in user–exoskeleton interaction, safety, clinical evidence, limitations in everyday use | [7,83,84,85,86] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Flor-Unda, O.; Arcos-Reina, R.; Toapanta, C.; Villao, F.; Bustos-Estrella, A.; Suntaxi, C.; Palacios-Cabrera, H. Challenges in the Development of Exoskeletons for People with Disabilities. Technologies 2025, 13, 291. https://doi.org/10.3390/technologies13070291
Flor-Unda O, Arcos-Reina R, Toapanta C, Villao F, Bustos-Estrella A, Suntaxi C, Palacios-Cabrera H. Challenges in the Development of Exoskeletons for People with Disabilities. Technologies. 2025; 13(7):291. https://doi.org/10.3390/technologies13070291
Chicago/Turabian StyleFlor-Unda, Omar, Rafael Arcos-Reina, Carlos Toapanta, Freddy Villao, Angélica Bustos-Estrella, Carlos Suntaxi, and Héctor Palacios-Cabrera. 2025. "Challenges in the Development of Exoskeletons for People with Disabilities" Technologies 13, no. 7: 291. https://doi.org/10.3390/technologies13070291
APA StyleFlor-Unda, O., Arcos-Reina, R., Toapanta, C., Villao, F., Bustos-Estrella, A., Suntaxi, C., & Palacios-Cabrera, H. (2025). Challenges in the Development of Exoskeletons for People with Disabilities. Technologies, 13(7), 291. https://doi.org/10.3390/technologies13070291






