Abstract
This article presents a comprehensive review of assistive devices for synovial joints, addressing their definitions, classifications, and technological advancements. The historical evolution of artificial exoskeletons, orthoses, prostheses, and splints is analyzed, emphasizing their impact on rehabilitation and the enhancement of human mobility. Through a systematic compilation of scientific literature, patents, and medical regulations, the study clarifies terminology and classifications that have often been imprecisely used in scientific discourse. The review examines the biomechanical principles of the musculoskeletal system and the kinematics of synovial joints, providing a reference framework for the optimization and design of these devices. Furthermore, it explores the various types of artificial exoskeletons, and their classification based on structure, mobility, power source, and control system, as well as their applications in medical, industrial, and military domains. Finally, this study highlights the necessity of a systematic approach in the design and categorization of these technologies to facilitate their development, comparison, and effective implementation, ultimately improving users’ quality of life.
Keywords:
exoskeleton; orthosis; prosthesis; splint; synovial joint; movements; trajectories; origins; records; appearances; definitions; uses; differences; biomechanics 1. Introduction
Low back pain is the leading contributor to the overall burden of musculoskeletal diseases. An analysis of the Global Burden of Disease (GBD) reports 570 million prevalent cases worldwide, responsible for 7.4% of global activities of daily living (ADLs). Other contributors to the overall musculoskeletal disease burden include fractures, which affect 440 million people globally (26 million ADLs), and osteoarthritis, impacting 528 million people (19 million ADLs), neck pain (222 million people; 22 million ADLs), amputations (180 million people; 5.5 million ADLs), rheumatoid arthritis (18 million people; 2.4 million ADLs), gout (54 million people; 1.7 million ADLs), and other musculoskeletal conditions (453 million people; 38 million ADLs) [1]. As a solution, musculoskeletal assistive devices are used, which mimic the behavior of synovial joints to prevent, correct, and predict injuries.
It is incredible that technologies exist that are adapted to human physiology, providing superior characteristics to those we possess. Technologies can enhance and amplify movements and forces, acting as a sort of external bones and muscles. For decades, technologies that resemble animal behavior have been developed [2,3,4], such as devices that mimic biological nature, including their physiological functions and chemical characteristics [5,6,7]. Based on this, mechanical and mechatronic adaptations have been made to suit the physiology of the human body, primarily to artificially exploit these characteristics.
This article will address devices that align with joint movement behavior, that is, assisting the movement of one or more synovial joints. Devices such as splints, prostheses, orthoses, and exoskeletons that have been under development for years. Prostheses have existed since the time of the ancient Egyptians [8], splints were crucial in events such as wars, where devices were needed to immobilize areas of the body to transport the wounded [9], or in more recent times, where artificial exoskeletons are of great help for a soldier or a worker in the industry, being especially effective in rehabilitation, just like orthoses. Additionally, the benefits these devices offer are extremely useful, and although still costly, the initiative to focus on technologies designed to assist a person’s movement has gained increasing importance. The intricacy of such technology, the complexity of locomotion, and understanding of the movement trajectories in space are key, as this would lead to a better understanding of them and allow for artificial replication.
An artificial exoskeleton, in addition to fulfilling its specific design applications, can perform functions like those of a splint, orthosis, or prosthesis. Although it shares some similar characteristics with an orthosis, its functions and applications vary depending on the type of use. Like a prosthesis, which helps reinforce or replace an affected area, an exoskeleton can also serve as an assistance device, adapting to the user’s needs over time, with differences in its use depending on the phase of support required. This creates a competitive environment for innovation, encouraging more and more researchers to take an interest in the topic. Research relies on concepts, definitions, and classifications, which, although not misused, have not been applied correctly based on their definition and intended use. This commonly occurs in article titles, newspapers, brochures, and general publications, causing difficulty for researchers to find information in a relevant way, and leading to a lack of uniformity in public information.
This article is structured into several sections to facilitate understanding. Section 2 presents the materials and methods used in the review. Also, in Section 2 the biomechanical characteristics of synovial joints are presented. Section 3 details the classifications and definitions of assistive devices. Section 4 examines current technological trends and their future implications. Finally, Section 5 presents the conclusions and recommendations for the future development of these devices.
2. Materials and Methods
2.1. Splints, Prostheses, Orthoses, and Artificial Exoskeletons
For a person to perform movements, it must be clarified that these consist of the displacement of limbs at a point in space. To carry out bodily movements, it is important to consider that they are performed with the force generated by the muscles, under the supervision of sensory and mechanical fields, and with the freedoms and restrictions that the joints impose. A study by the World Health Organization from 1990 to 2019 determined that, globally, there were a total of 178 million bone fractures [10]. This represents a 33.4% increase since the 1990s, compared to the analyses provided by the Global Burden of Disease (GBD), which showed that around 1.71 million people worldwide suffer from musculoskeletal conditions, including bone fractures, sprains, osteoarthritis, and amputations, among others [1]. For this reason, devices that correct and prevent injuries are essential for rehabilitation and/or treatment follow-up, to improve reversible injuries or provide temporary or permanent replacements, with the goal of allowing a person to have a dignified life routine.
Devices such as splints, prostheses, orthoses, and artificial exoskeletons were, and continue to be, developed to improve rehabilitation capabilities, ergonomics, and assistance with injuries or limitations of the human body. Lighter devices with greater and better characteristics, and above all, economical accessibility, are necessary. Devices are constantly being evaluated or are being improved with new materials or new sophisticated technologies.
Technologies such as assistive devices provide artificial characteristics for different areas of the body, with some focused on containing, replacing, enhancing, and smoothing movements and loads. The National Library of Medicine of the United States defines a splint as a device used to stabilize a part of the body to reduce pain and prevent further injury [11]. A prosthesis is a device designed to replace a missing body part or to improve the function of an existing body part. Injured or missing eyes, arms, hands, legs, or joints are commonly replaced with prosthetic devices [12]. The University of Michigan Health describes an orthosis as a device designed to improve biomechanical function, encourage proper joint alignment, or protect an existing limb [13]. Garcia, M.A. et al. describe an exoskeleton as a type of assistance/rehabilitation robot that can be worn by a human [14]. According to Urrea, C. et al., an exoskeleton is a structure intended to be worn on the human body as a piece of clothing, i.e., a wearable robot (WR), either to complement the function of a limb or to completely replace it [15]. In summary, the four types of human body movement assistance devices can be defined as:
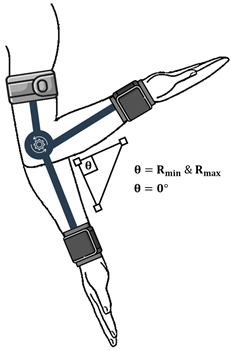
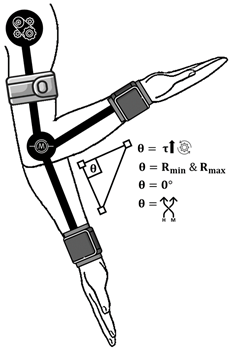
- Splint: It is based on the immobilization of the joint(s).
- Prosthesis: It has two characteristics: to replace the function of amputated areas or to reinforce damaged areas.
- Orthosis: It is based on limiting the range of motion of a single joint.
- Artificial exoskeleton: It is based on increasing physical resistance and the smoothness of movements in the joint(s).
The idea of creating an information database is supported, covering everything from the biological and biomechanical aspects of a person’s movements to their mechanical adaptation in artificial assistive devices, creating classifications based on their etymology and application. To achieve this, the biomechanical study of the musculoskeletal system and the classifications of the different joints in the human body were addressed.
2.2. Musculoskeletal System
The musculoskeletal system, according to Poon, L. et al. (2017), is an organ system that provides the framework, support, stability, and movement to the human body, playing a pivotal role in our daily function [16]. Cathy, S. et al. (2014) describes the composition of the musculoskeletal system with ligaments, bones, tendons, cartilage, and connective tissues [17].
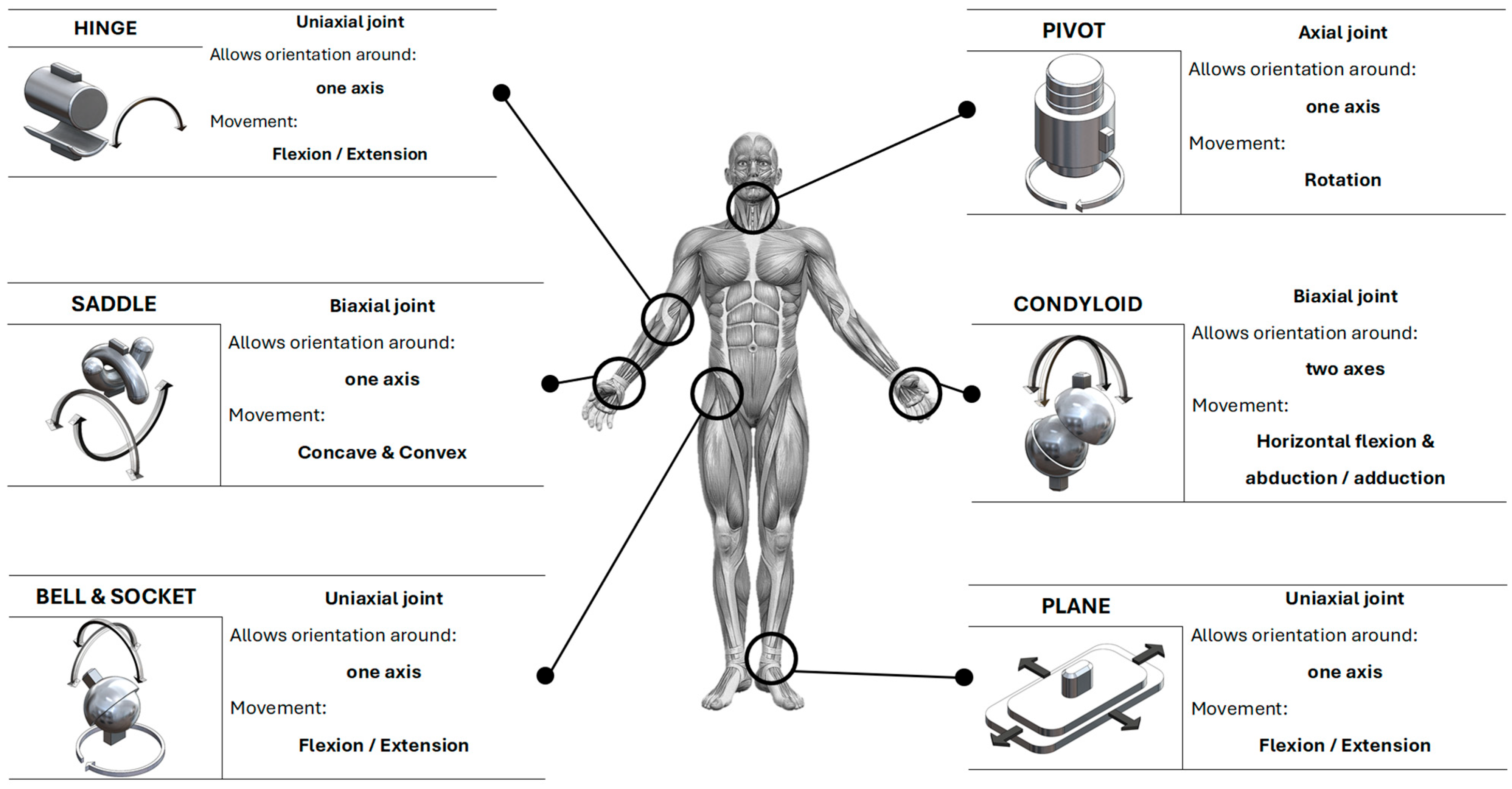
The coordinated work of these systems allows a person to perform movements, but this is merely the force-generating work; however, the nervous system and the joints control muscular movements and determine the range and manner of motion, respectively. The unification of the force generated by the musculoskeletal system, the control of the nervous system, and the freedoms of movement characteristic of the joints allow for actions such as standing, sitting, running, walking, among others. Gordon, J. et al. (2013) describe the movement of the musculoskeletal system as a series of 6 characteristic types of movements [18]. Hinge, Pivot, Saddle, Condyloid, Bell and Socket, Plane.
In Figure 1, an example of each of the six characteristic movements is provided, indicating the type of movement in the joint. Although this would not be the only movement, as a joint can be uniaxial, biaxial, or multiaxial, this depends on the axis and plane of the specific type of movement of the joints.
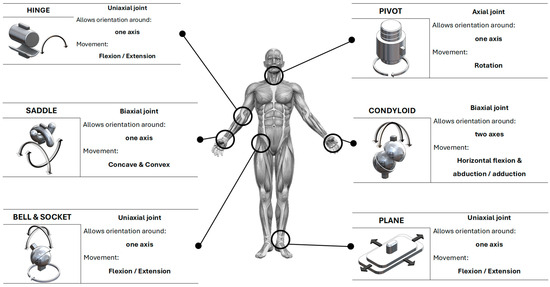
Figure 1.
Mechanical movements associated with synovial joints in a person.
The characteristic movements of the joints are essential for understanding movement trajectories and, with this, characterize devices that are more faithful to the movement of the musculoskeletal system. Below, the different types of joints are analyzed, from their biological characteristics to their biomechanical ones.
2.3. Joints
A joint is a point where two skeletal elements come into contact [19], allowing movement between them. Joints are essential for mobility and the function of the musculoskeletal system in the human body. There are different types of joints, classified based on their structure and the amount of movement they allow. The main categories of joints are fibrous, cartilaginous, and synovial [19]. Fibrous and cartilaginous joints allow very limited movements, such as those of the skull or the vertebrae in the spine, as they are connected by fibrous connective tissue and cartilage, respectively, while synovial joints are formed by a joint capsule, synovial fluid, and articular surfaces covered with cartilage, such as the knee [19]. Considering that fibrous and cartilaginous joints have very limited movements, they can be considered as fixed or low-mobility joints, while synovial joints allow a wide variety of movements.
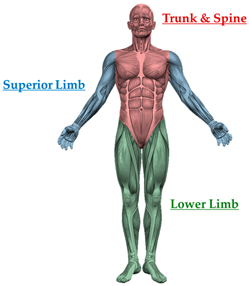
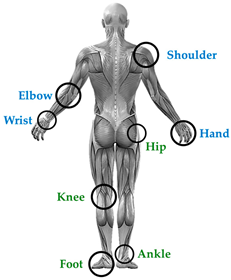
Once the structural composition of fibrous, cartilaginous, and synovial joints is understood, it becomes viable to analyze synovial joints, as they possess the mobility required for the behavior of movement trajectories and the range of movements of different body segments. According to the volumes of A. I. Kapandji [20,21,22], joint physiology is highlighted in three sections: upper limb [20], lower limb [21], and trunk and spine [22]. Due to the limited information available on the trunk and spine in assistive devices, only the joints located in the upper and lower limbs will be addressed.
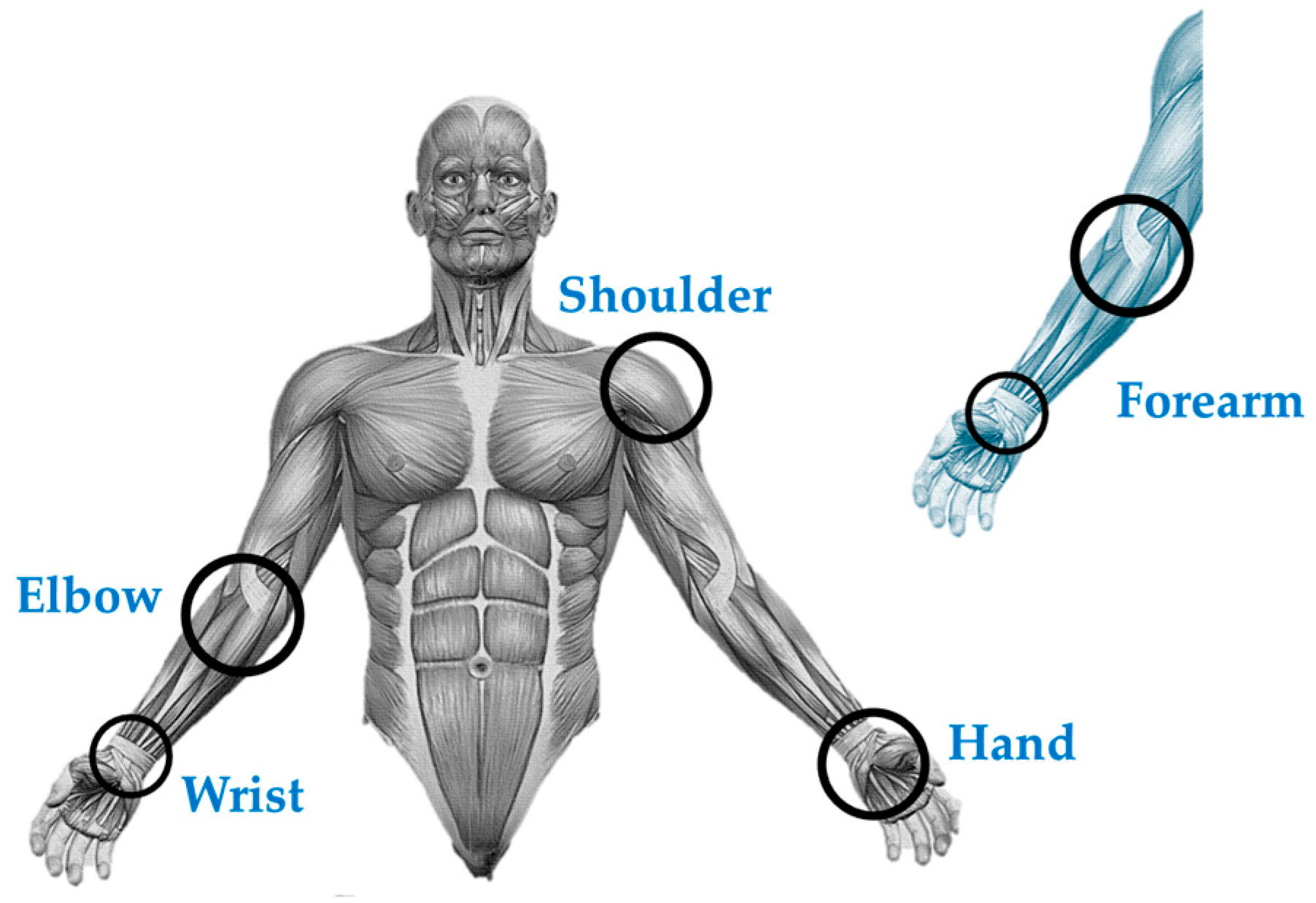
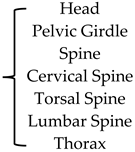
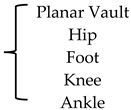
In Table 1, the joints belonging to each section of the body are broken down. As mentioned earlier, this article will only focus on analyzing the joints belonging to the upper limbs (Elbow, Shoulder, Hand, and Wrist) and lower limbs (Pelvic Girdle, Hip, Gait, Foot, Knee, Ankle).

Table 1.
Distribution of joints across the sections of the human body.
There is a movement called “pronation–supination” [20] (pp. 102–145), located between the elbow and wrist joints, known as the “forearm”. This movement is used to position the hand when grasping objects. The forearm has one degree of freedom, and its movement occurs along the axis between the elbow and wrist, as these two joints share an axis, the transverse axis, which can be considered the axis for pronation and supination movement [20] (pp. 102–145). In the lower limb, the knee and foot can exhibit a similar movement to pronation–supination; however, this movement originates from the hip, making it an additional movement to that of the hip.
In Table 1 and Figure 2, the distribution of joints throughout the body and their additions, such as the forearm, can be seen. This refers to the movement of the musculoskeletal system, which is essential for the development of technological devices for joint assistance, in this case, synovial joints. By locating the joints, biomechanical analyses can be made, which are useful for calculating ideal trajectories for improvements in assistive devices. Table 2 describes the joints of the upper limb, considering their axes as degrees of mobility and their biomechanical description.
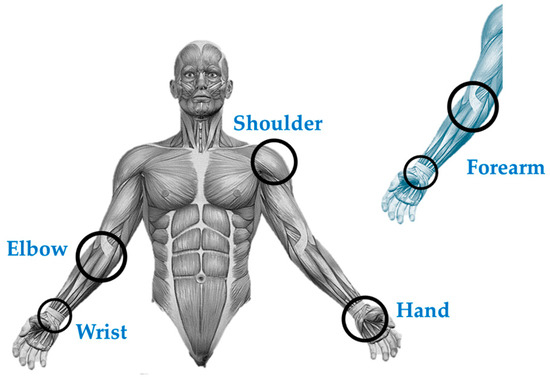
Figure 2.
Location of the forearm between the elbow and wrist joints in the upper limb; pronation and supination movement, also known as pronosupination.

Table 2.
Description of the upper limb joints.
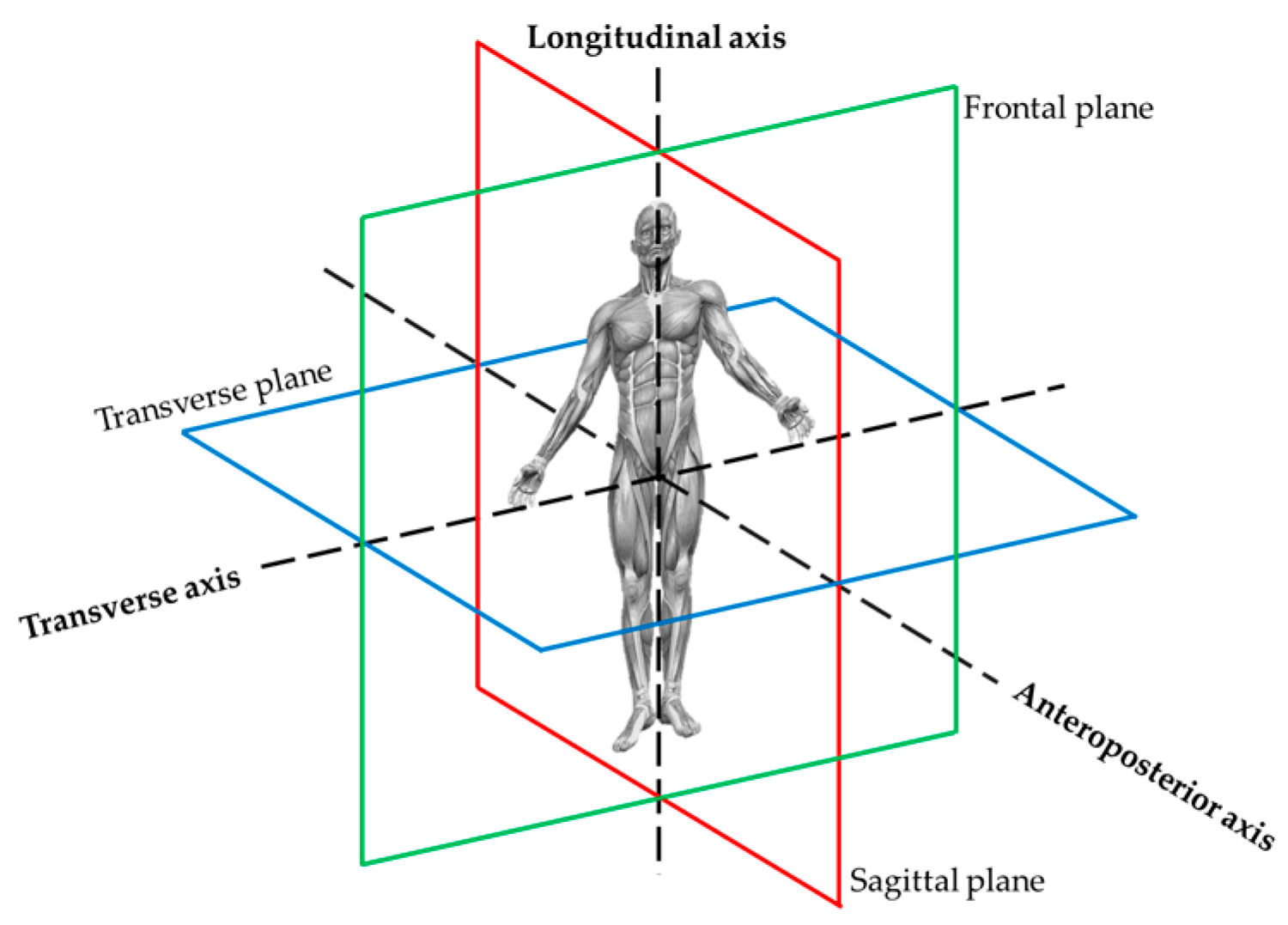
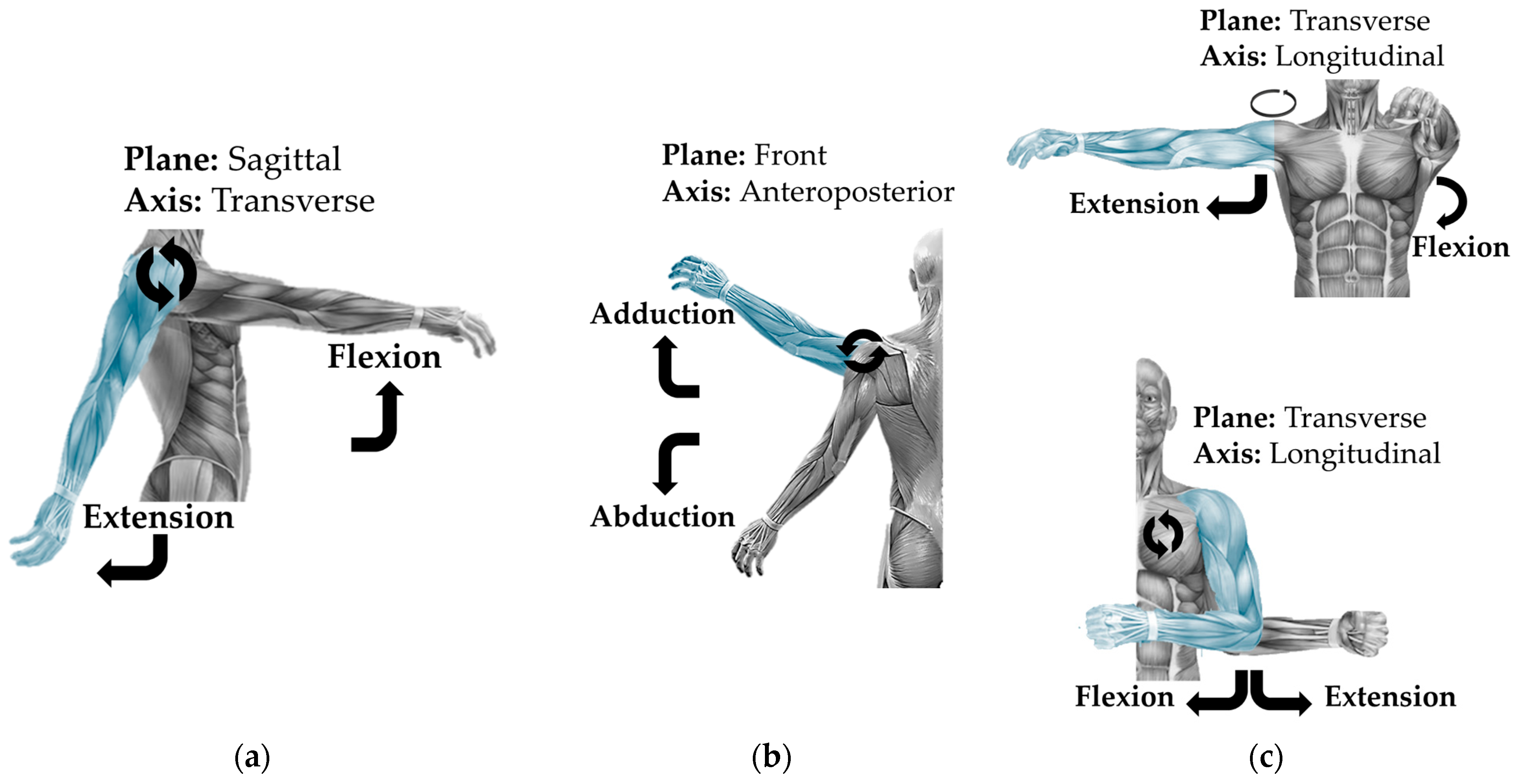
Body movements are represented in axes and planes [20,21,22,23] that describe the characteristic movements of the joints. See Figure 3. The sagittal plane divides the body into right and left halves and allows flexion and extension movements. The frontal plane divides the body into anterior and posterior parts, allowng abduction and adduction movements, and the transverse plane crosses the upper and lower body, allowing rotations [20,23]. In Figure 3, a graphical representation is made for oriental with respect to Table 3 and Figure 4 and Figure 5.
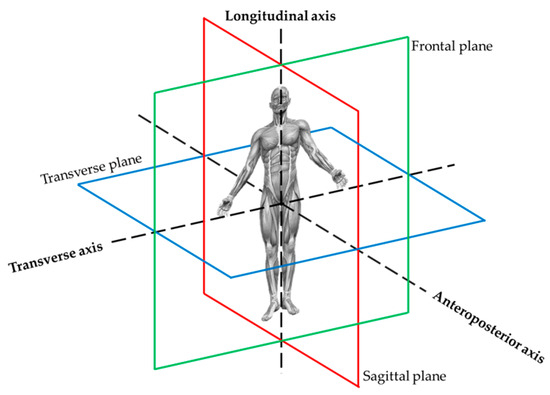
Figure 3.
Planes and axes belonging to the spatial references in a person.

Table 3.
Characteristic movements in each joint of the upper limb.
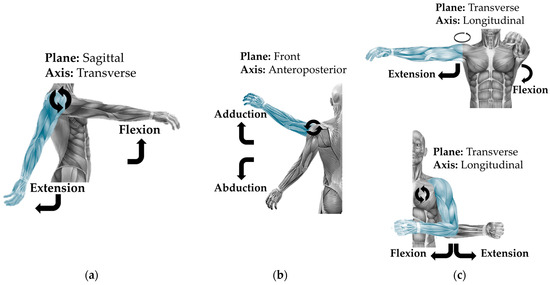
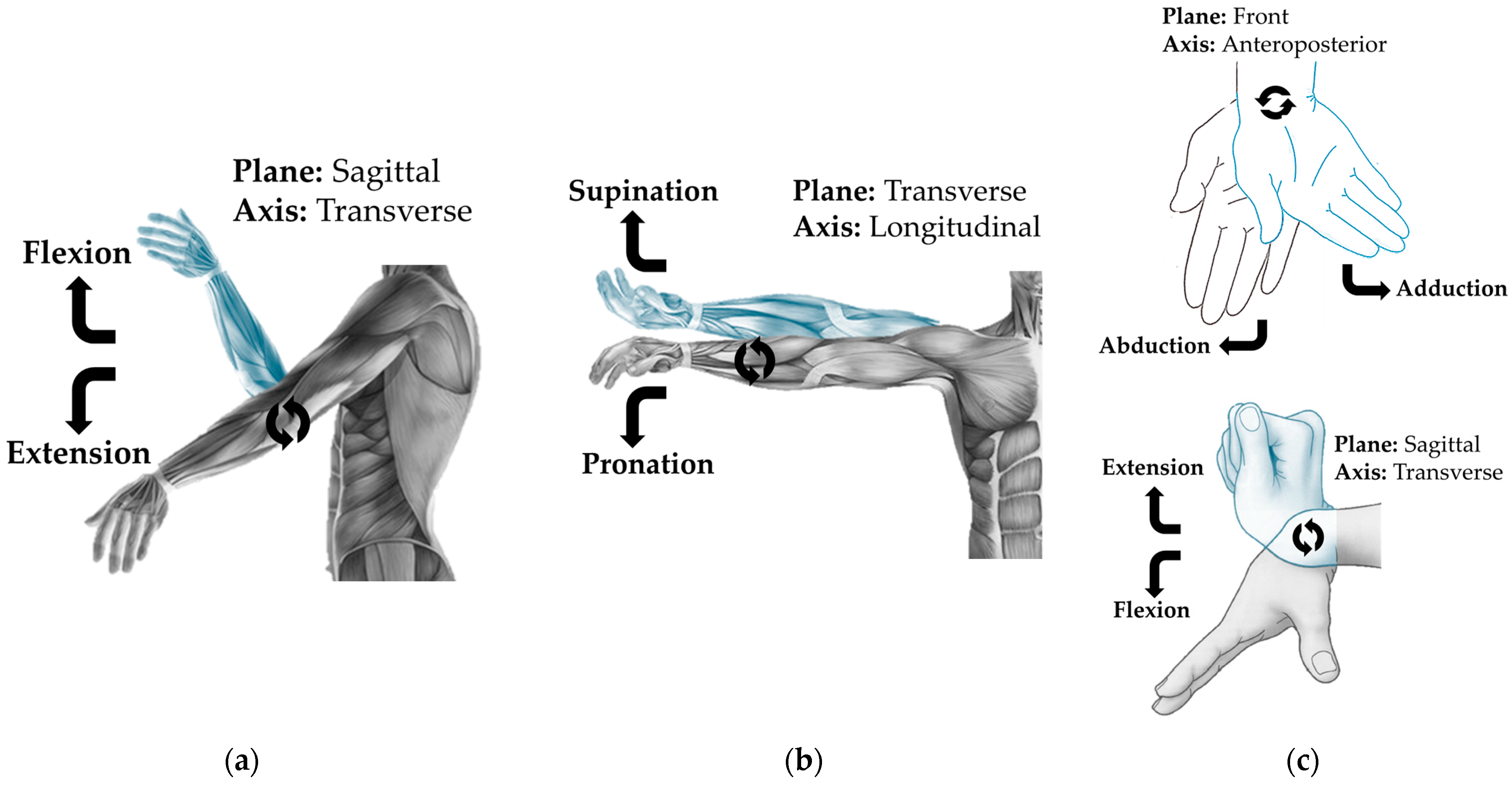
Figure 4.
Shoulder movements: (a) movement in the transverse axis; (b) movement in the anteroposterior axis; (c) movement in the longitudinal axis.
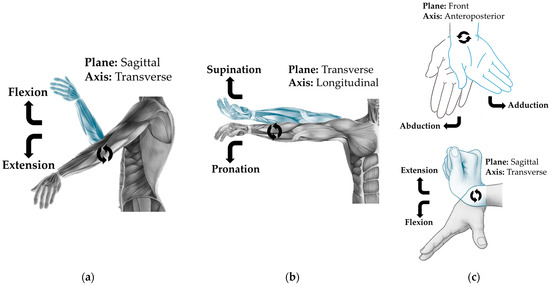
Figure 5.
Movements of the elbow, forearm, and wrist: (a) movement on the transversal axis; (b) movement on the longitudinal axis; (c) movement on the anteroposterior and transversal axes.
Given that the information collected for joint movements is extensive, the joints, degrees of freedom, axes, planes, characteristic movements, and illustrative references will be described in independent figures (Figure 4 and Figure 5), as their descriptions cannot be clearly distinguished within the space provided in Table 3.
From Table 1, the joints of the upper limb and their pronosupination were taken as the basis, and in the same table, the joints of the lower limb are described. Like the previous joints, these are analyzed to calculate ideal trajectories for improving assistive devices. In Table 4, the joints of the lower limb are described, considering their axes, degrees of mobility, and biomechanical description. Given that the information collected for joint movements is extensive, the joints, degrees of freedom, axes, planes, characteristic movements, and illustrative references will be described in independent figures (Figure 6 and Figure 7), as their descriptions cannot be clearly distinguished within the space provided in the table.

Table 4.
Description of the joints of the lower limb.
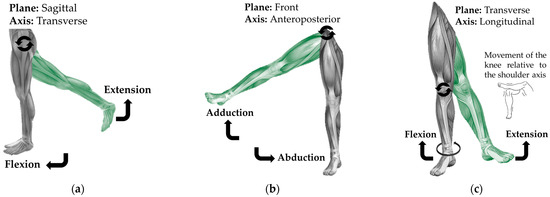
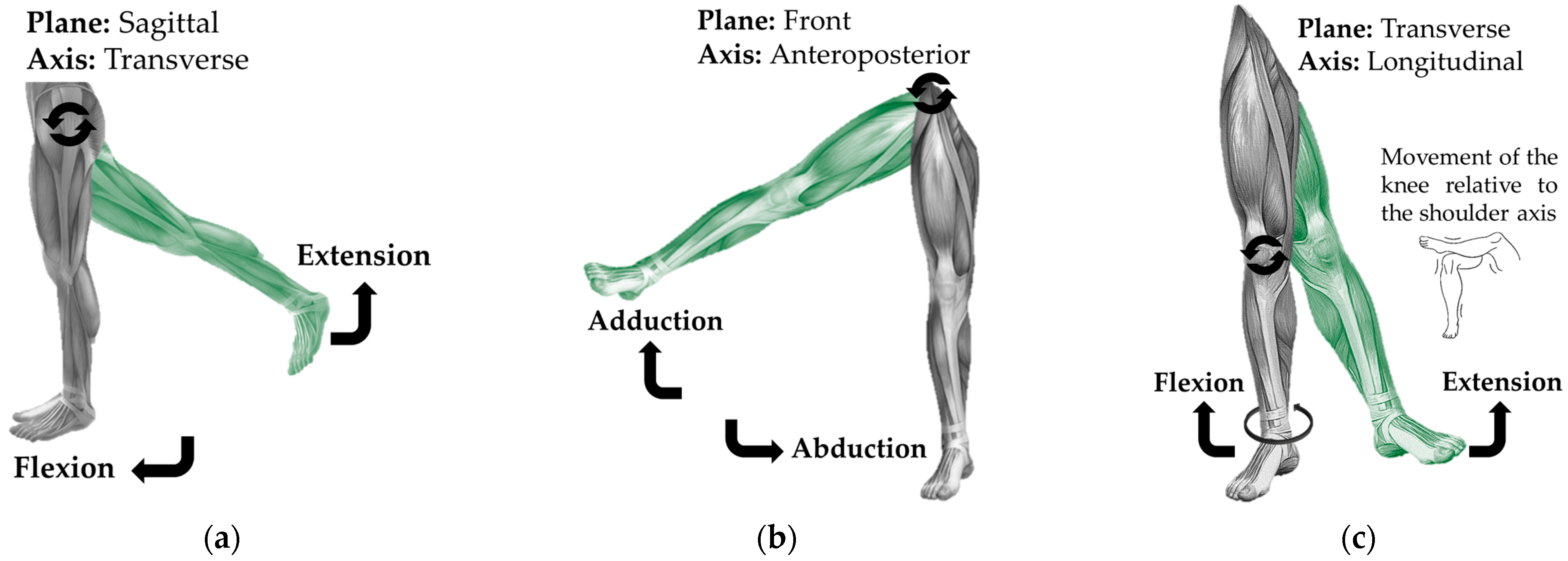
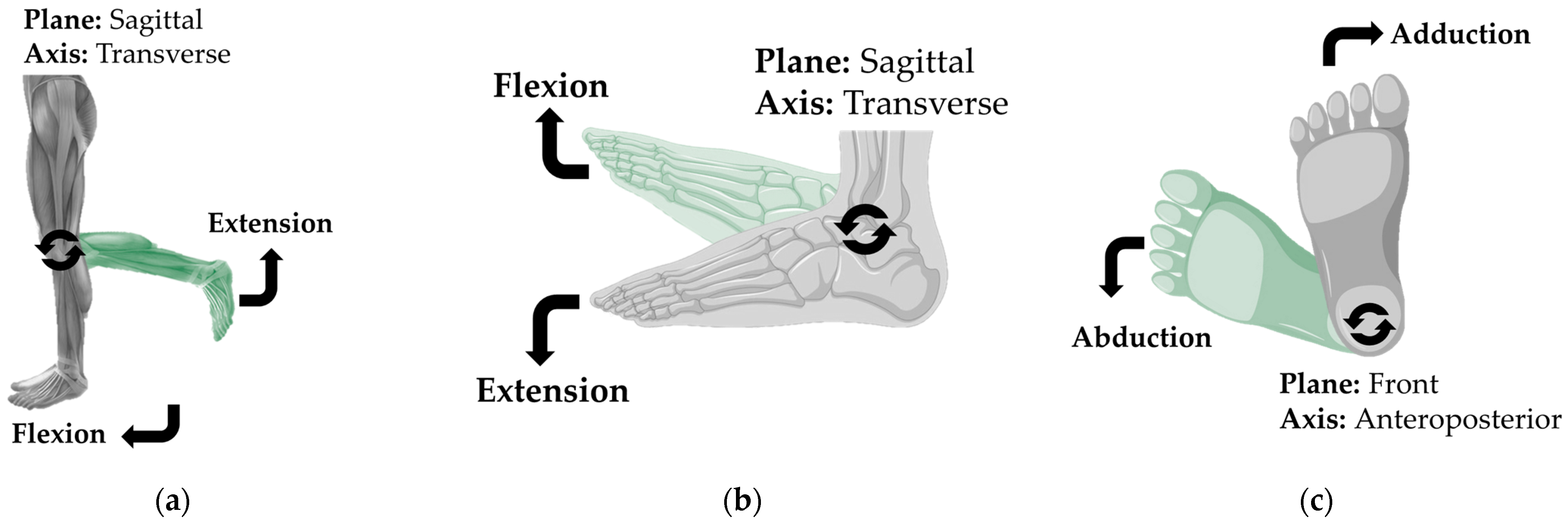
Figure 6.
Hip movements: (a) movement around the transverse axis; (b) movement around the anteroposterior axis; (c) movement around the longitudinal axis.
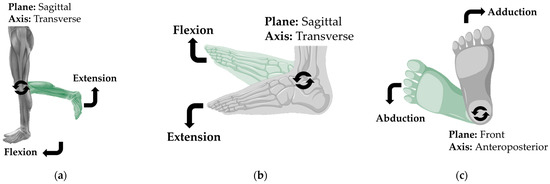
Figure 7.
(a) Knee movements around the transverse axis; (b) ankle movement; (b) movement around the transverse axis; (c) movement around the anteroposterior axis.
Given that the information collected for joint movements is extensive, the joints, degrees of freedom, axes, planes, characteristic movements, and illustrative references will be described in independent figures (Figure 6 and Figure 7), as their descriptions cannot be clearly distinguished within the space provided in Table 5.

Table 5.
Characteristic movements in each joint.
The movements of the upper and lower limbs are crucial for the design and analysis of robotic devices due to their complexity and variety. These movements are directly related to human biomechanics, involving precise interactions between bones, muscles, tendons, and joints, enabling a wide range of actions and adaptability in various daily tasks. For a robotic device to effectively mimic these movements, it is essential to thoroughly understand how they are performed, both kinematically and dynamically. By studying natural human movements, the kinematics of the exoskeleton or robot can be optimized, improving its ability to replicate human gestures with precision. This not only enhances the device’s efficiency and comfort but also allows for better integration into the user’s daily activities, ensuring smoother usage and reducing the risk of injury or fatigue. A robot’s ability to accurately emulate human movements is also crucial for ensuring that the assistance provided is effective and natural, thus optimizing the device’s performance and interaction with the environment.
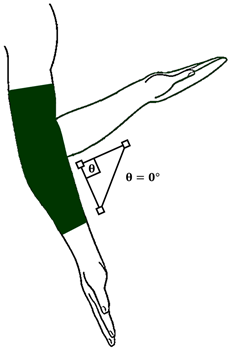
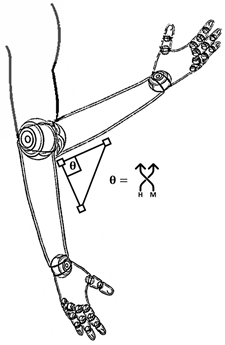
In the synovial joints of an average person, understanding movement and its behavior is useful, as the trajectories generated by these joints help develop devices that behave more appropriately according to the movement axes of each joint. In Table 6, the function and application area where each device is most used are described, as each device has its own characteristic application. The four devices are illustrated from the elbow joint, located in the upper limb of a person, as this joint has only one degree of freedom and can be described more simply.

Table 6.
Description of the functioning of each device.
Example: In the case of the elbow representation in Table 6, in the event of an injury where movement needs to be immobilized, it would be feasible to place a common cast. If this had to be both immobile and mobile at different hours of the day, it would be correct to place an orthosis. This would provide immobility for the defined time and could be adjusted to allow movement within a safe range. If the joint is entirely damaged and the only way for the patient to heal is through amputation or internal segment wear such as the bone, the correct option would be to implement a prosthesis to replace the damaged section. Lastly, if the joint presents scenarios where injury could occur, or to prevent one, an artificial exoskeleton with mechanical or robotic quality could be used.
If there was an injury in the joint, this device would have the capability to place it in positions, speeds, and accelerations suitable for optimal recovery. Just like the function of the splint or orthosis, where it can be immobile or mobile, the artificial exoskeleton can immobilize it, limit it, or extend it to reach its natural mobility through actuation. In another case, when substituting the function of the joint due to loss of functionality, with a prosthesis, the normal procedure would be to amputate. However, with this device, since there is a structure surrounding the damaged joint, amputation is unnecessary, as the structure would act to replace the joint’s function. Lastly, if the goal is to prevent injury or improve movement and strength characteristics of the joint, the correct option would be to use an artificial exoskeleton with actuation capabilities and a structure that, when surrounding the joint, would replace the muscle’s function with mechanical work.
The typology of assistance devices for synovial joints represents the characteristics, functions, and applications of each of the developments and scientific contributions regarding the care of these joints. The dissemination through articles, academia, and private products has a significant influence on the classification of each device. Although there is diversity in these technologies, this article focuses on the analysis of the four most important, as they have been in constant evolution throughout history and continue to be applied today. Table 7, Table 8, Table 9, Table 10 and Table 11 describe the origins, appearances, registrations, definitions, and uses of these technologies. This classification is important because these technologies are often misused in scientific dissemination. While not entirely the case, this causes confusion due to the lack of standardization, leading to new developers having scattered foundations.

Table 7.
Description of the origins of the names of the different devices.

Table 8.
Description of the first record of the different devices.

Table 9.
Description of the first appearance of the different devices.

Table 10.
Description of the definitions of the different devices.

Table 11.
Description of the uses of the different devices.
Knowing the first records and early appearances of a technological device is essential for understanding its evolution and historical context. These records allow us to trace the origin of the innovation, identify key advancements that have contributed to its development, and recognize the needs or problems that motivated its creation. Additionally, by reviewing the early versions of a device, it is possible to evaluate how they have improved over time in terms of efficiency, functionality, and accessibility, impacting their role in society and industry regarding the design and development of future technologies, helping to avoid past mistakes and optimize innovation processes.
The etymology of words and their first official appearance are essential for understanding the evolution of concepts and preventing misunderstandings. In the context of robotic devices such as splints, prosthetics, orthoses, and exoskeletons, knowing their origin helps to better understand their function and purpose. Terms like “prosthesis” (replacement) and “exoskeleton” (external support) reflect their specific use and how they have been adapted to medical and technological needs. Thus, etymological knowledge ensures precise and proper use of these terms in the development of technologies.
3. Results
3.1. Artificial Exoskeletons
Diseases, accidents, or the lack of certain attributes in the human body have led us to develop technologies that, while they may not fully facilitate recovery, are valuable for coping with the process, particularly in medical terms. Technologies that enhance, smooth, and/or protect the movements of their users are important not only for safeguarding their physiological integrity but also for implementing artificial characteristics that a regular person does not possess. These characteristics provide security and, most importantly, improve quality of life. Devices such as splints, prostheses, and orthoses are typically limited to one or two tasks. Artificial exoskeletons, on the other hand, serve multiple functions, with applications and features in sectors like medicine, military, industry, and education, among others. They offer added value, as they provide more options for different situations, and this article tracks the records and classifications of this technology.
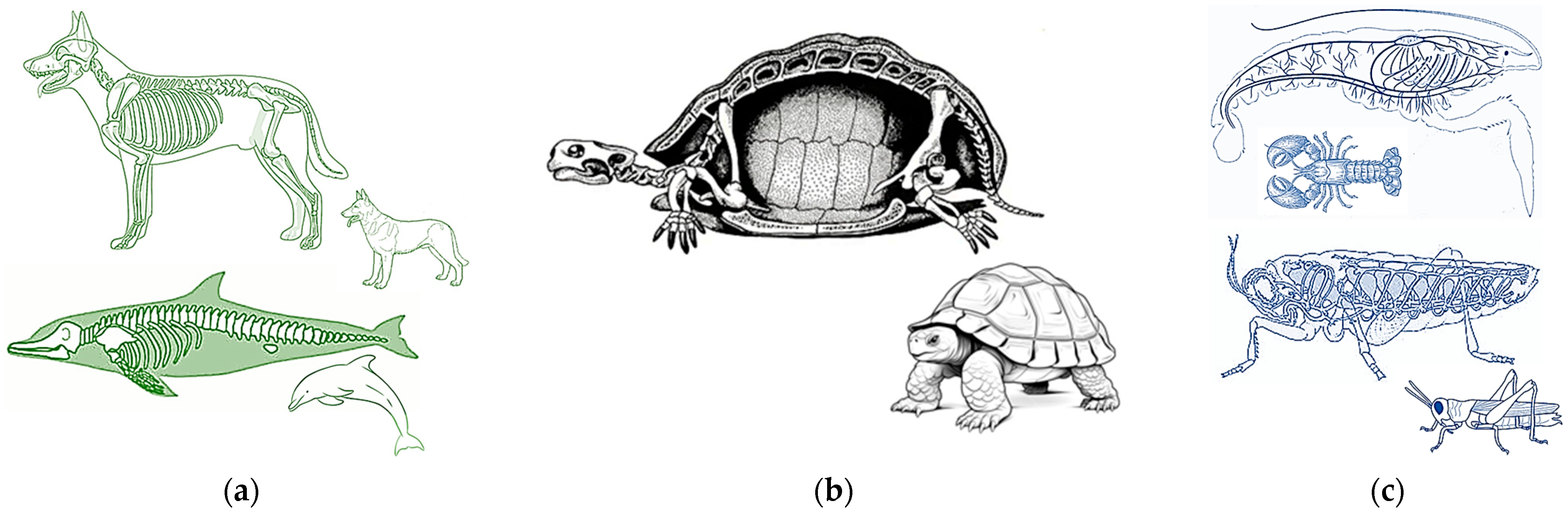
3.2. From Biological to Artificial
Based on Table 10, the origin of the word “exoskeleton” comes from zoology, describing a hardened structure, mostly of bone nature [27]. In Table 7, it is defined as a hard layer that covers, supports, and protects an invertebrate biological being, which uses the external skeletal structure to support, move, and protect itself [37]. Therefore, an exoskeleton is used for invertebrates, in contrast to vertebrates, which possess an internal skeletal structure called an endoskeleton (Figure 8a). Humans, as well as terrestrial, aerial, or marine animals, have both endo and exoskeletons, and the variety is finite and can be distinguished by their visible characteristics. However, there are animals where the difference is not so clear, such as the terrestrial tortoises, which have both an external and internal skeletal structure (Figure 8b). Their shell and limbs do not share the same line, even though their limbs have an internal bone structure, the containment of their organs is under an external bone structure, making them a hybrid in terms of skeletal composition. This composition is artificially represented when a mechanical structure is placed around a vertebrate.
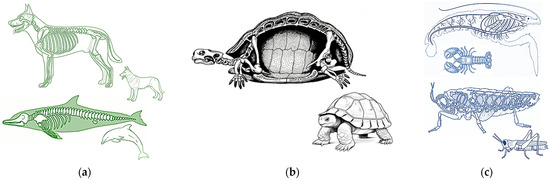
Figure 8.
(a) Species with internal bone structures; (b) species with both internal and external bone structures; (c) species with external bone structures.
An animal like an ant or beetle is known for being able to lift several times its body weight, thanks to having an exoskeleton [43]. The exoskeleton provides greater resistance because its external bone structure absorbs most of the load, in contrast to a vertebrate animal, where the load is absorbed by muscles, joints, and only then reaches the internal skeletal structure. The application of an artificial exoskeleton to a human or animal follows the same principle as species that possess them (Figure 8c); they serve to contain and protect the integrity of the user inside. Based on Table 11, according to standards NTP 1162 and 1163, an artificial exoskeleton is a portable external device that is placed on the user’s body, used to increase ergonomic intervention capabilities and improve working conditions, especially regarding physical load [42].
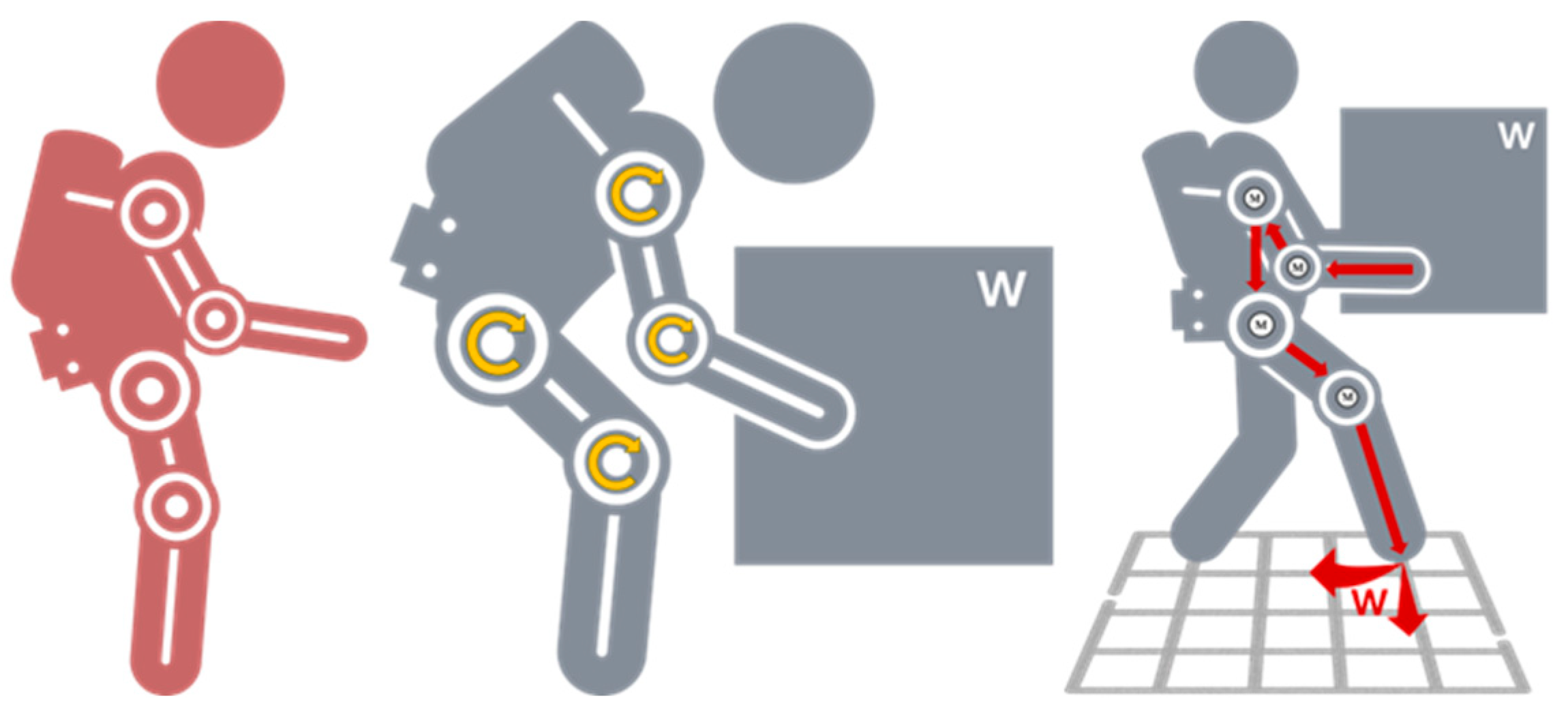
In Figure 9, the concept of the suit’s use and the general use of the device is divided into two parts. Here, it is shown that when a user is wearing it, they are covered and protected by it, although this is not always the case. Most artificial exoskeletons are partial, focusing mostly on the upper and lower limbs, but total protection is the primary goal for human exoskeletons.
Figure 9.
User—Device: artificial exoskeleton on a user.
Based on Figure 9 and Figure 10, and the content from the previous tables, it can be concluded that an exoskeleton is an organic term, in this case, referring to external bone structures. In the case of structural devices developed from non-organic materials such as metals or polymers, it can be referred to as an artificial structure, as it mimics the naturalness of an organic exoskeleton. Therefore, referring to an artificial structure usable by a vertebrate as simply “an exoskeleton” would be incorrect without an adjective to complement it. For example, if it is a mechanical structure made from metal links and assisted by elastic actuators (springs), it can be defined as a Mechanical Exoskeleton. If the structure includes electric motors and its assistance is actuated, controlled, and communicated through instrumental circuits, it can be referred to as a Robotic Exoskeleton. In more recent technologies, like the metaverse, devices that can read movements and translate them into coordinates in cyberspace could be defined as a Haptic Exoskeleton, among others.
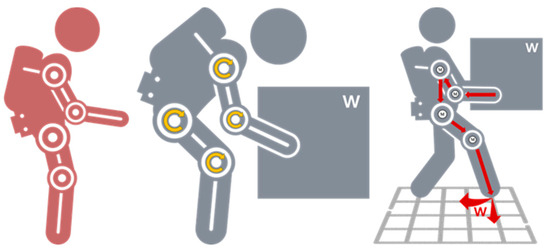
Figure 10.
Application: the user does not interact with surrounding loads.
3.3. Classification of Artificial Exoskeletons
Earlier, behaviors related to muscles and joints were analyzed to understand the freedom of movement a typical person possesses, aiming to comprehend the application and behavior of the different devices discussed throughout the article, such as splints, prostheses, orthoses, and artificial exoskeletons. The latter has a wide range of applications and configurations. Therefore, an extensive classification of artificial exoskeletons is proposed, addressing their global and partial configurations. Additionally, the analysis is based on Table 7, Table 8, Table 9, Table 10 and Table 11, which outline the origins, definitions, records, uses, and appearances of this device. According to the tables on etymology, uses, and applications, three basic points should be considered for something to be considered an artificial exoskeleton.
For a satisfactory classificatory analysis of the types of artificial exoskeletons, the de-vice must meet three essential criteria:
- It must be an external structure to the body.
- It must be parallel to the musculoskeletal system.
- It must assist or enhance the forces and movements of the joints.
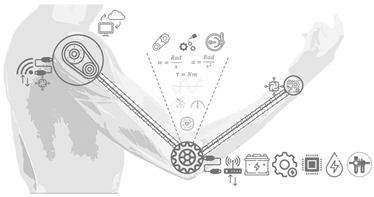
The analysis of artificial exoskeletons for classification purposes should focus on two main qualities: assistance and enhancement. Based on these two principles, considerations are made regarding the type of structures that resemble the user, the materials that can be used to mold the device, the type of mobility it is designed to employ (which aligns with its application in the medical, military, industrial sectors, among others), the type of energy supply (which is crucial, as it defines the exoskeleton’s designation), the type of control used to manage the movement of the structure, the systems that will determine its functionality within its applications, and the types of construction, which can be performed by private sector companies or public sector organizations such as universities or research institutions.
Given that the device may opt for different types of structures, mobilities, power sources, control systems, functional systems, and construction, a global classification of parameters is provided, detailing the characteristics for the different types of developments this device may present [44,45].
Regarding structure, mobility, control, and construction, the most prominent characteristics come from power sources and functional systems. The power supply defines whether the exoskeleton will be mechanical, robotic, pneumatic, or hydraulic. A mechanical exoskeleton, while using elastic actuators as springs, does not provide external energy other than that of the user, making it a passive system. In contrast, an active system involves external energy, with peaks of power input along specific parts of the structure, especially at the actuators. While the structure may not necessarily contain them, the power supply, such as electricity, not only fuels the actuation but also powers the exoskeleton’s instrumentation. Pneumatic and hydraulic power supplies, when compared to electrical or non-powered systems, do not provide any other function except actuation of the joints, and are therefore considered pneumatic exoskeletons or hydraulic exoskeletons, as their primary function is to supply movement.
There are four different systems available. Although the literature includes additional variations, two main categories are considered: active and passive systems. Passive systems use gravity compensation and elastic/spring members to store and release energy during movements, assisting users in physical movements. Active systems, on the other hand, rely on one or more actuators to increase the power of the limbs. Once the global characteristics that an artificial exoskeleton may possess have been outlined, an analysis of their behaviors in different configurations is made. Based on this description, in Table 12 each of the various types of behaviors will be described in terms of power supply, structure, and functioning within different applications [46].

Table 12.
Components characterize an artificial exoskeleton.
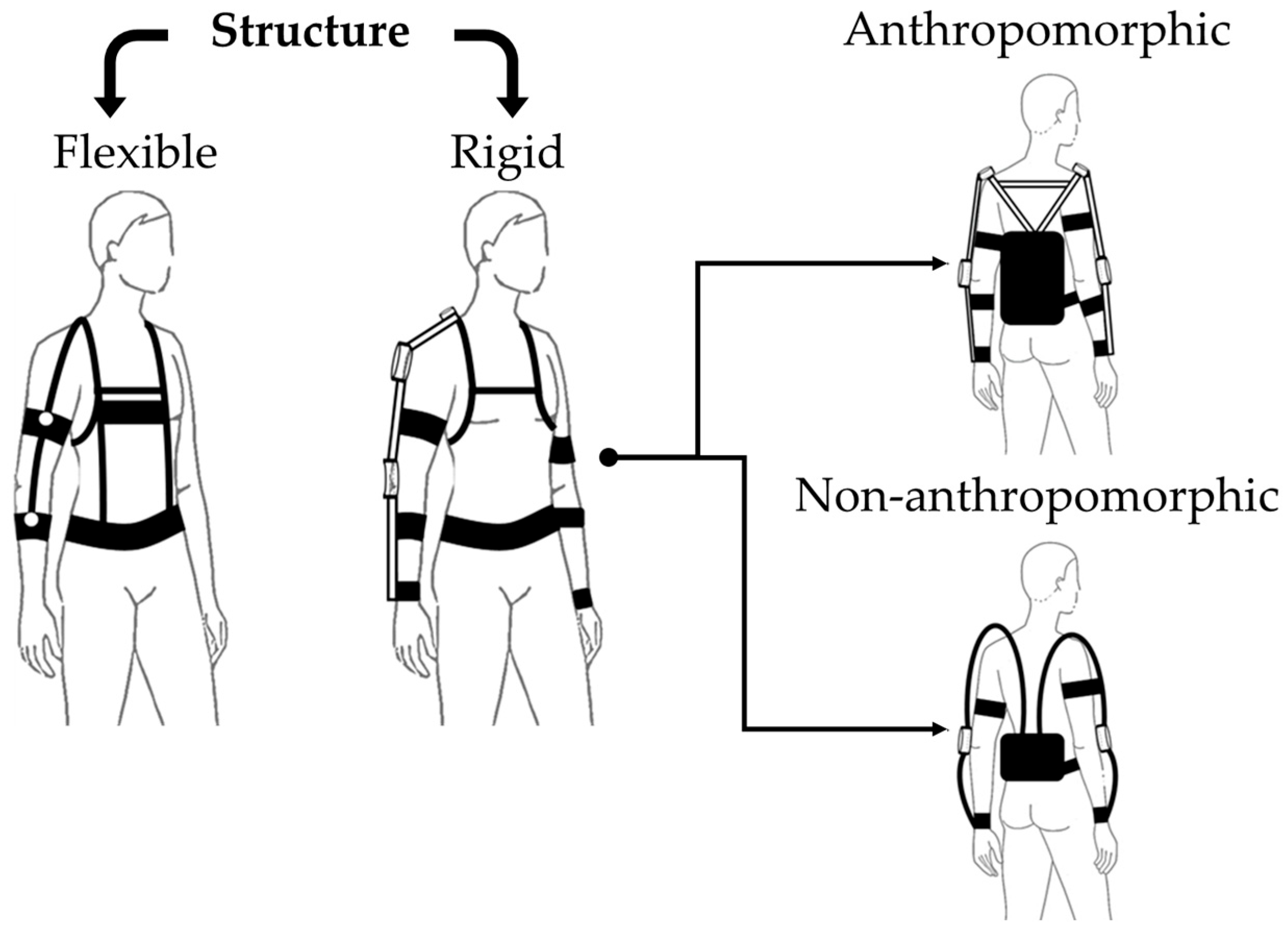
3.4. Types of Structure for an Artificial Exoskeleton
Figure 11 presents a classification of artificial exoskeletons by type of kinematic structure. Table 13 presents a description of these exoskeletons.
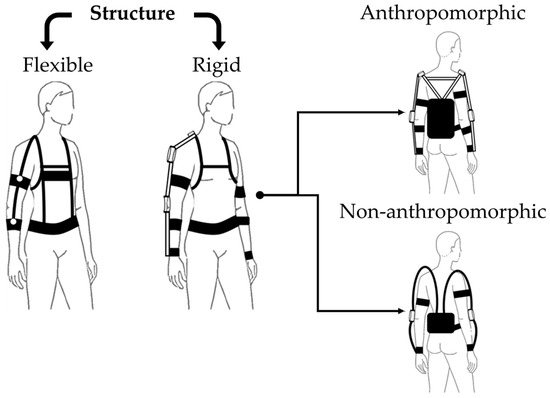
Figure 11.
Classification of artificial exoskeletons by kinematic structure type.

Table 13.
Description of artificial exoskeletons by kinematic structure type.
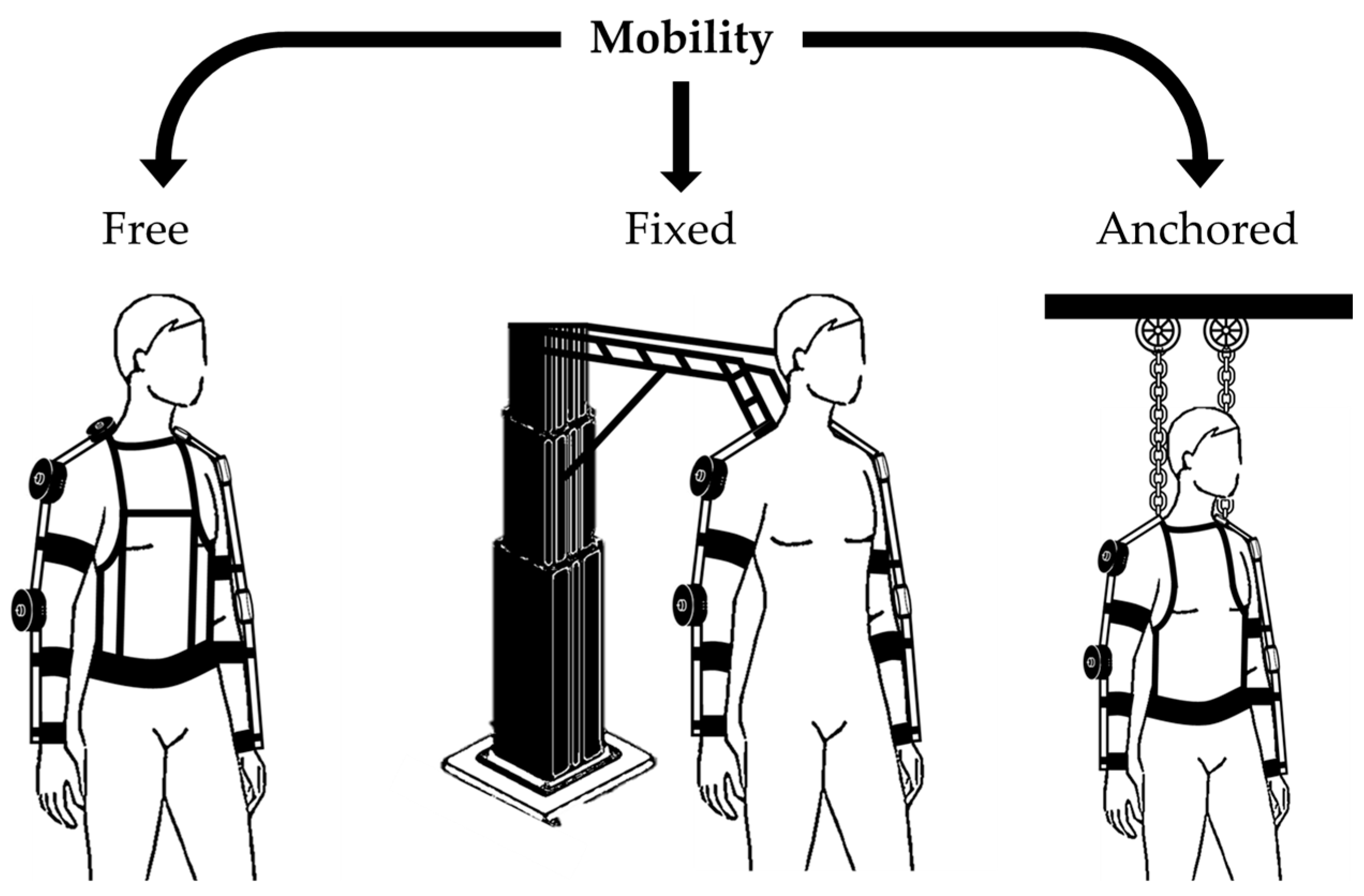
3.5. Types of Mobility of an Artificial Exoskeleton
Figure 12 presents a classification of artificial exoskeletons according to their workspace and grounding: mobile, fixed, and anchored. Table 14 presents a description of each of these exoskeleton types.
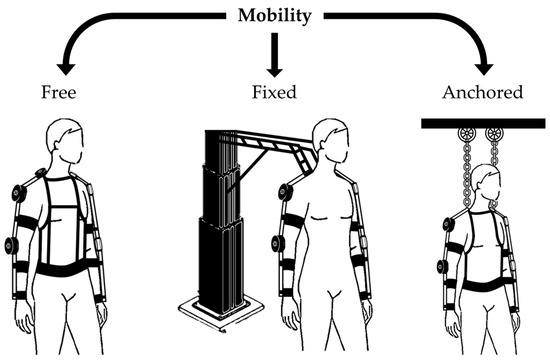
Figure 12.
Classification of mobility between a mobile, fixed, and anchored artificial exoskeleton.

Table 14.
Description of mobility between a mobile, fixed, and anchored artificial exoskeleton.
3.6. Type of Power Supply for an Artificial Exoskeleton
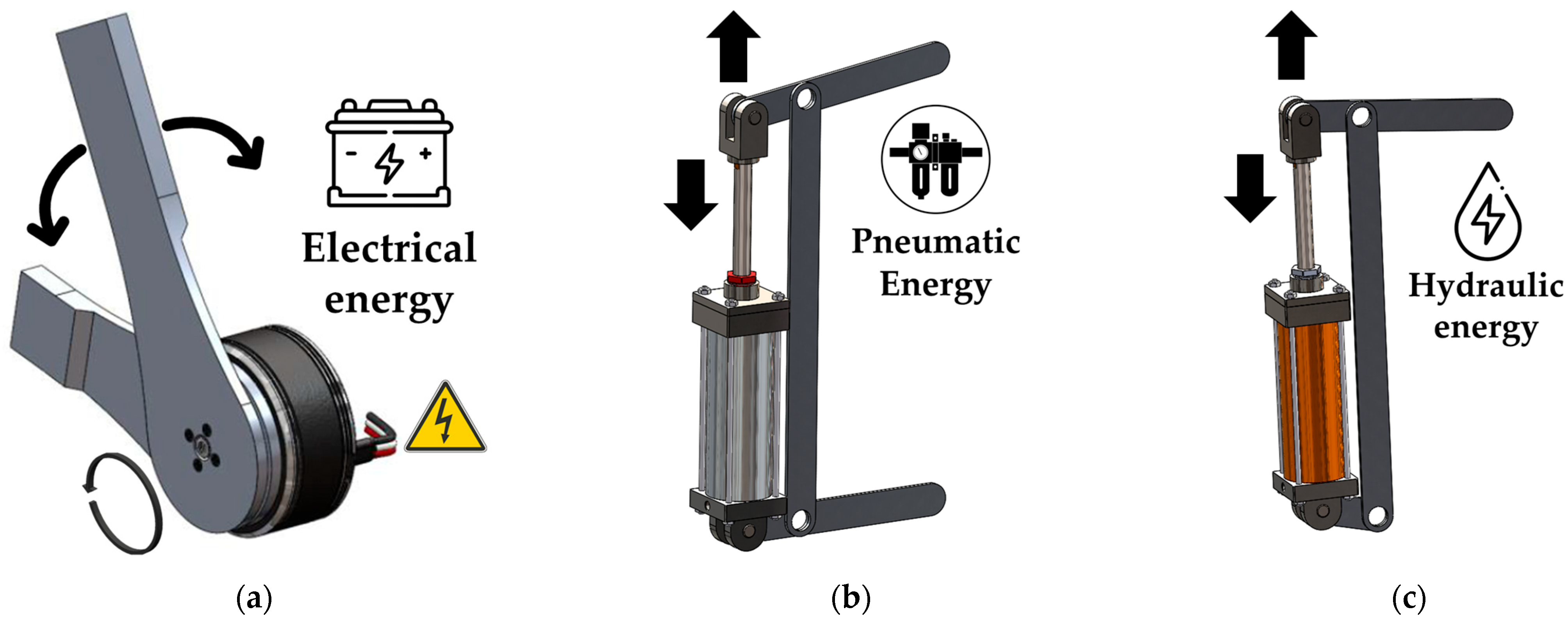
Figure 13 presents a classification of energies according to their performance as electric, pneumatic, or hydraulic motor work. Table 15 describes each energy use for use in an artificial exoskeleton.
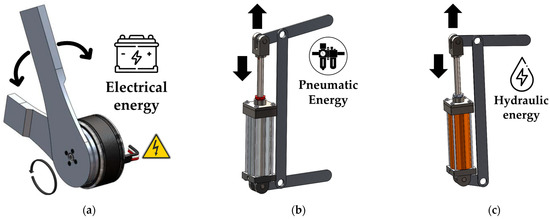
Figure 13.
Classification of artificial exoskeletons according to the type of actuation. (a) electric actuator; (b) pneumatic actuator; (c) hydraulic actuator.

Table 15.
Classification of external energies used in an artificial exoskeleton.
3.7. Type of Artificial Exoskeleton System
There are four different systems available. Although the literature includes additional variations, the two main categories are considered: active and passive systems. Passive systems use gravity compensation and elastic/spring members to store and release energy during movements, assisting users in physical movements. Active systems, on the other hand, rely on one or more actuators to increase the power of the limbs. Once the global characteristics that an artificial exoskeleton may possess have been outlined, an analysis of their behaviors in different configurations is made. Based on this description, each of the various types of behaviors will be described in terms of power supply, structure, and functioning within different applications [46]. See Table 16.

Table 16.
Classification of exoskeletons according to the type of system.
Artificial exoskeletons are classified based on their activation level and energy usage. The four main types are passive, semi-passive, semi-active, and active. The choice of system depends on the specific needs and usage conditions of the exoskeleton. This characteristic is where the adjective artificial can be omitted, and the appropriate adjective for the system type being used can be added. See Table 17.

Table 17.
Description and classification of the internal features of an artificial exoskeleton.
Based on the description in Table 12, the selected system type can define the behavior of the device. This means that an artificial or mechanical exoskeleton may be considered due to the lack of actuation and instrumentation for control and communication; its function is solely to provide support and stability to the user. On the other hand, a robotic system is characterized as a machine programmed to perform tasks autonomously or which is guided by a third party using external components. Although not necessarily robotic, an exoskeleton requires actuation, as in the case of the semi-active system, as described in Table 16, it can also be considered an electronic exoskeleton or a data collection system.
3.8. Type of Communication of an Artificial Exoskeleton
Table 18 describes the standard communication types that the control card has to activate the operation of an artificial exoskeleton.

Table 18.
Classification of communication types in artificial exoskeletons.
3.9. Types of Robotic Exoskeleton Construction
Artificial exoskeletons have experienced significant development in both public and private institutions. To innovate more quickly, engineers and researchers have collaborated to create devices that improve the quality of life for individuals. Institutions and companies are innovating with structures, reduced power supply, and increased efficiency. Additionally, some exoskeletons incorporate artificial intelligence to adapt to the user’s movement patterns, enhancing their effectiveness. In institutions such as companies, innovation is highly sought after. Below are descriptions of the three most important exoskeletons developed by public institutions and the ninety-six most important developers in the private sector.
- XoMotion (Simon Fraser University): Researchers at Simon Fraser University (SFU) created XoMotion, a cutting-edge robotic exoskeleton. This device enables people with mobility disabilities to stand and walk without additional support. It offers a wide range of activities, including walking, climbing stairs, and squatting. XoMotion uses sensors to mimic the human body’s logic and generate balanced movement [49].
- Stanford Ankle Exoskeleton: Researchers at Stanford University developed an ankle exoskeleton that enables people to walk more efficiently. Training and customization are key to its success. This device connects to the shoe and around the leg, mimicking a motorized exoskeleton. It helps users push forward while walking and maintain balance [50].
- Stanford Wireless Exoskeleton: Another achievement by Stanford University, this is a wireless exoskeleton that increases walking speed by applying torque to the ankle. It facilitates movement during walking and is especially useful for individuals with mobility disabilities [51].
In recent years, the search for private companies dedicated to the research and development of robotic devices, particularly exoskeletons, has seen significant growth. These companies, both emerging and established, are at the forefront of technological innovation, working on the design of exoskeletons aimed at improving the quality of life for individuals with reduced mobility and optimizing physical performance for workers in industrial settings. The development of robotic exoskeletons is divided into various categories, depending on their purpose and application. Assistive exoskeletons, focused on rehabilitation, and power exoskeletons, designed to enhance users’ physical abilities, are among the most prominent types. The public sector, universities, research centers, and government agencies collaborate closely on the design of prototypes that aim not only at medical advancements but also at military and rescue applications. In contrast, private companies, driven by the need to commercialize these devices, tend to focus on economic viability and improving technology to meet specific market needs, often allowing them to bring products to practical use more quickly. Collaboration between both sectors is expected to play a crucial role in advancing this technology, combining public resources with the agility and entrepreneurial vision of the private sector.
Below is a selection of the 25 most influential companies in the development of robotic exoskeletons, those that have made a significant impact on the industry thanks to their technological innovations, advances in medical rehabilitation, workplace ergonomics, and general applications. These companies have positioned themselves as leaders in the sector, developing devices that improve human mobility, reduce physical strain in industrial environments, and enhance the recovery of people with motor disabilities. The list includes both established giants and novel startups, all playing a key role in the evolution of this technology that promises to revolutionize human–machine interaction.
- ATOUN Inc.
- (Nara City, Nara Prefecture, Japan) Exoskeletons for physical task assistance.
- Bioness Inc.
- (Santa Clarita City, CA, USA) Neuromuscular stimulation devices and exoskeletons.
- Bionik Laboratories Corp.
- (Toronto City, ON, Canada) Exoskeletons for medical rehabilitation.
- Comau
- (Grugliasco City, Turin, Italy) Exoskeletons for industrial work assistance.
- Cyberdyne Inc.
- (Tsukuba City, Ibaraki Prefecture, Japan) Robotic exoskeletons for rehabilitation and mobility.
- Ekso Bionics
- (San Rafael City, CA, USA) Exoskeletons for medical and industrial rehabilitation.
- Exy—Empowering People
- (Curitiba City, Paraná, Brazil) Exoskeletons for workplace injury reduction.
- Fourier Intelligence
- (Xiu Pu Lu City, Shanghai, China) Robotic exoskeletons for rehabilitation.
- German Bionic
- (Augsburg City, Bavaria, Germany) Smart exoskeletons for industrial assistance.
- Honda Motor Co., Ltd.
- (Minato City, Tokyo, Japan) Mobility and rehabilitation assistive devices.
- Hyundai Motor Company
- (Seocho-gu City, Seoul, Republic of Korea) Exoskeletons for mobility and industrial tasks.
- INDI
- (Monterrey City, Nuevo León, Mexico) Pediatric exoskeletons for walking assistance.
- Lockheed Martin Corporation
- (Bethesda City, MD, USA) Exoskeletons for military and industrial applications.
- Marsi Bionics
- (Rivas Vaciamadrid City, Madrid, Spain) Exoskeletons for children with neuromuscular disorders.
- Myomo Inc.
- (Burlington City, MA, USA) Exoskeletons for neuromuscular injury support.
- Ottobock
- (Duderstadt City, Niedersachsen, Germany) Exoskeletons and prosthetics for mobility enhancement.
- Panasonic Corporation
- (Kadoma City, Osaka Prefecture, Japan) Exoskeletons for mobility and industrial tasks.
- Parker Hannifin
- (Mayfield Heights City, OH, USA) Exoskeletons for rehabilitation and medical assistance.
- Raytheon Company
- (Arlington City, VA, USA) Exoskeletons for military use.
- ReWalk Robotics
- (Yokne‘am Illit City, Northern District, Israel) Exoskeletons for people with spinal cord injuries.
- Rex Bionics
- (Auckland City, Auckland Region (North Island), New Zealand) Autonomous exoskeletons for people with reduced mobility.
- Sarcos Robotics
- (Salt Lake City, UT, USA) Industrial and military exoskeletons.
- SuitX
- (Emeryville City, CA, USA) Modular exoskeletons for rehabilitation and industry.
- Technaid
- (Arganda del Rey City, Madrid, Spain) Exoskeletons for research and rehabilitation.
- Wandercraft SAS
- (Paris City, France) Autonomous exoskeletons for personal mobility.
4. Discussion
The research on assistive devices is based on ergonomic adjustment, energy consumption, and adjustable functionality. The latter is one of the aspects most related to the high development and purchase price. This is because they are designed to fit the user’s physiological needs or are adjustable but limited to a specific task. On the other hand, energy consumption is only feasible through a continuous power supply, which limits technologies to a specific operational radius, or, if independent, their energy consumption is restricted due to the high demand of the system.
The following discussion points are open to the four devices mentioned in this article, although the correct perspective would be related to artificial exoskeletons and possibly orthoses, since prostheses might exchange their characteristics based on the specific needs and circumstances, while splints are based on the application needs and their low material cost.
- Structures: Rigid structures are mostly, if not entirely, made from metal materials due to their high resistance to bending and compression. However, these properties are functional for devices that require excessive physical strength, structural resistance, or conditions that could be dangerous for the user. On the other hand, in the medical field, devices for the rehabilitation of limbs or their segments require lower structural resistance, as the movements are slow and do not usually require prolonged or excessive fatigue. Military devices, while requiring strength, may also require physical resistance for walking or lumbar support, where metallic structures are too heavy for transportation over long distances. Materials with low density and high resistance to bending and compression are ideal to replace the rough and heavy metal structures, which not only are heavy but also have high manufacturing and material costs. Polymers, however, would be ideal for devices that do not require high physical demand. Their use could reduce production costs, given their low manufacturing costs and potential for molding or 3D printing, enabling the creation of complex joints where geometry would help create structures that are both stronger and cheaper with quicker construction timelines.
- Energy Consumption: The type of structure impacts energy consumption. Larger structures tend to have greater weight, which translates into higher torque. Large torques require high energy consumption, adding more weight due to the larger actuators. Lighter structures would result in lower torques, allowing the use of smaller actuators, which reduces weight and, in turn, energy consumption. This would be advantageous for mobile devices, as their autonomy would increase significantly with the same battery bank.
- Energy Efficiency: Developing energy-efficient actuators and control systems would be essential for enhancing the autonomy of mobile devices. By minimizing energy consumption through smart power management and lightweight designs, manufacturers can extend the operational time of devices between charges, making them more practical for users.
- Production Times: Structures would be manufactured with ideal characteristics, since designing in CAD environments allows for complex calculations and geometries that metal structures could not achieve, all at lower cost and time. With polymers, geometries would not be an issue as they can be created using molds or additive manufacturing at low production costs and considerably faster manufacturing times than conventional or CNC metal pieces.
- Design Improvements: Future designs could prioritize lightweight materials with high strength-to-weight ratios, such as advanced polymers or composites, which would significantly reduce the overall weight of devices while maintaining structural integrity. This would allow for greater mobility and usability, particularly in applications where prolonged use is required.
- Cost Reduction Strategies: Implementing additive manufacturing techniques, such as 3D printing, could lower production costs and time. This method enables the creation of complex geometries that are difficult or costly to achieve with traditional metal fabrication. By optimizing designs for manufacturability, manufacturers can streamline production processes, reducing material waste and labor costs.
- Integration of AI and Machine Learning: The incorporation of artificial intelligence and machine learning algorithms could enhance the adaptability and functionality of assistive devices. Smart systems could learn from user interactions, adjusting in real-time to optimize support and improve user experience. This would enable devices to provide personalized assistance based on the user’s specific needs and movements, increasing effectiveness during rehabilitation and daily activities.
5. Conclusions
The development of assistive devices for synovial joints has advanced significantly, incorporating biomechanical and technological innovations that enhance mobility and improve users’ quality of life. The proper classification and terminology of these devices—splints, prostheses, orthoses, and artificial exoskeletons—are essential for their design, comparison, and effective application across various fields, including medicine, industry, and the military. Artificial exoskeletons stand out as the most versatile technology in this field, providing support for both rehabilitation and performance enhancement. Their classification based on structure, mobility, power source, and control systems is crucial for their development. Future research should focus on improving ergonomics, reducing energy consumption, and optimizing cost-effectiveness to make these devices more accessible. Ultimately, integrating new technologies and materials into the design of these devices will expand their applications and improve their functionality. However, further biomechanical studies and standardized regulations are necessary to ensure the proper implementation of these technologies for the benefit of users.
Author Contributions
Conceptualization, F.C.-F., A.B.O., A.L.S.-B., A.B.S. and A.J.M.M.; methodology, F.C.-F., A.B.O., A.L.S.-B., R.C.A. and H.R.A.R.; investigation, F.C.-F., A.L.S.-B., A.B.O., A.B.S. and A.J.M.M.; writing—original draft preparation, F.C.-F., A.L.S.-B. and A.B.O.; writing—review and editing, F.C.-F., A.L.S.-B., A.B.O., R.C.A., A.B.S. and H.R.A.R.; supervision, A.B.O. and F.C.-F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
The authors thank the Tecnológico Nacional de México and the Centro Nacional de Investigación y Desarrollo Tecnológico for the support provided to carry out this work. Filiberto Cruz Flores thanks CONACYT for the scholarship granted to carry out his postgraduate studies.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- World Health Organization (WHO). Musculoskeletal Health. World Health Organization. 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/musculoskeletal-conditions (accessed on 19 February 2025).
- Tomańska, A.; Stawinoga, M.; Gębarowski, T.; Janeczek, M.; Klećkowska-Nawrot, J.; Goździewska-Harłajczuk, K.; Dobrzyński, M. The musculoskeletal anatomy of the hind limbs of the Komodo dragon (Varanus komodoensis, Varanidae). Animals 2025, 15, 35. [Google Scholar] [CrossRef]
- Li, J.; Sun, Z.; Wei, X.; Tan, Q.; He, X. Effect of structure on osteogenesis of bone scaffold: Simulation analysis based on mechanobiology and animal experiment verification. Bioengineering 2024, 11, 1120. [Google Scholar] [CrossRef]
- Mattucci, S.; Speidel, J.; Liu, J.; Kwon, B.K.; Tetzlaff, W.; Oxland, T.R. Basic biomechanics of spinal cord injury: How injuries happen in people and how animal models have informed our understanding. Clin. Biomech. 2019, 64, 58–68. [Google Scholar] [CrossRef]
- André, A.D.; Martins, P. Exoskeletal support devices: Summary of technical aspects. Bioengineering 2023, 10, 1328. [Google Scholar] [CrossRef]
- Garzón, I.; Muñoz-Hurtado, J.; Pereira-Martínez, J.; Ionescu, A.M.; Cardona, J.D.L.C.; Tejada-Casado, M.; Pérez, M.D.M.; Campos, F.; Chato-Astrain, J.; Alaminos, M. Development of new squid gladius biomaterials for corneal tissue engineering. Mar. Drugs 2024, 22, 535. [Google Scholar] [CrossRef]
- Sutton, G.P. Animal biomechanics: A new silent partner in the control of motion. Curr. Biol. 2013, 23, R651–R652. [Google Scholar] [CrossRef]
- Nerlich, A.G.; Zink, A.; Szeimies, U.; Hagedorn, H.G. Ancient Egyptian prosthesis of the big toe. Lancet 2000, 356, 2176–2179. [Google Scholar] [CrossRef]
- Fess, E.E. A history of splinting: To understand the present, view the past. J. Hand Ther. 2002, 15, 97–132. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Fragility Fractures; World Health Organization: Geneva, Switzerland, 2024; Available online: https://www.who.int/news-room/fact-sheets/detail/fragility-fractures#:~:text=In%202019%2C%20there%20were%20178,by%20population%20growth%20and%20ageing (accessed on 19 February 2025).
- A.D.A.M. Medical Encyclopedia. How to Make a Splint. National Library of Medicine, 2023. [About 3 p.]. Available online: https://medlineplus.gov/ency/article/000040.htm (accessed on 19 February 2025).
- A.D.A.M. Medical Encyclopedia. Prosthesis. National Library of Medicine. 2023. Available online: https://medlineplus.gov/ency/article/002286.htm (accessed on 19 February 2025).
- University of Michigan Health. Orthoses (Braces). Rehabilitation Medicine. 2024. Available online: https://www.uofmhealth.org/conditions-treatments/rehabilitation/orthoses#:~:text=An%20orthosis%20is%20a%20device,Muscular%20Dystrophy (accessed on 19 February 2025).
- Velarde, M.A.G.; Rosado, W.M.A.; Ortega, A.B.; Abúndez, A.; Cortés, C.; Colin, J. Lower limb assistance systems: A state of the art. Lat. Am. Appl. Res. 2022, 52, 89–99. [Google Scholar] [CrossRef]
- Urrea, C.; Agramonte, R. Improving exoskeleton functionality: Design and comparative evaluation of control techniques for pneumatic artificial muscle actuators in lower limb rehabilitation and work tasks. Processes 2023, 11, 3278. [Google Scholar] [CrossRef]
- Lim, P.N.; Wang, Z.; Wang, D.; Konishi, T.; Thian, E.S. Development in additive printing for tissue-engineered bone and tendon regeneration. Curr. Opin. Biomed. Eng. 2017, 2, 99–104. [Google Scholar] [CrossRef]
- Elrod, C.S. Chapter 5—Musculoskeletal system. In Acute Care Handbook for Physical Therapists, 4th ed.; Paz, J.C., West, M.P., Eds.; W.B. Saunders: Philadelphia, PA, USA, 2014; pp. 85–122. [Google Scholar] [CrossRef]
- Betts, J.G.; Young, K.A.; Wise, J.A.; Johnson, E.; Poe, B.; Kruse, D.H.; Korol, O.; Johnson, J.E.; Womble, M.; DeSaix, P. Chapter 9.4 Synovial joints. In Anatomy and Physiology; Ingram: La Vergne, TN, USA, 2013; Available online: https://openstax.org/books/anatomy-and-physiology/pages/9-4-synovial-joints (accessed on 19 February 2025).
- Betts, J.G.; Young, K.A.; Wise, J.A.; Johnson, E.; Poe, B.; Kruse, D.H.; Korol, O.; Johnson, J.E.; Womble, M.; DeSaix, P. 9.1 Classification of joints. In Anatomy and Physiology; Ingram: La Vergne, TN, USA, 2013; Available online: https://openstax.org/books/anatomy-and-physiology/pages/9-1-classification-of-joints (accessed on 19 February 2025).
- Kapandji, A.I. Joint Physiology: Commented Diagrams of Human Mechanics, Upper Limb, 6th ed.; Editorial Medica Panamericana: Madrid, Spain, 2006; Available online: https://www.medicapanamericana.com/es-MX/libros/fisiologia-articular-tomo-1-miembro-superior-tomo-1-miembro-superior-6a-edicion (accessed on 19 February 2025).
- Kapandji, A.I. Joint Physiology: Commented Diagrams of Human Mechanics, Lower Limb, 6th ed.; Editorial Medica Panamericana: Madrid, Spain, 2012; Available online: https://www.medicapanamericana.com/es-MX/libros/fisiologia-articular-tomo-2-miembro-inferior-tomo-2-miembro-inferior (accessed on 19 February 2025).
- Kapandji, A.I. Joint Physiology: Commented Diagrams of Human Mechanics, Trunk and Spine, 6th ed.; Editorial Medica Panamericana: Madrid, Spain, 2012; Available online: https://www.medicapanamericana.com/es-MX/libros/fisiologia-articular-tomo-3-tronco-y-raquis-tomo-3-tronco-y-raquis-6a-edicion (accessed on 19 February 2025).
- Kong, W.; Sessa, S.; Zecca, M.; Takanishi, A. Anatomical calibration through post-processing of standard motion tests data. Sensors 2016, 16, 2011. [Google Scholar] [CrossRef]
- s.v. “splint, n”. In Oxford English Dictionary; Oxford University Press eBooks: Oxford, UK, 2023. [CrossRef]
- s.v. “prosthesis, n”. In Oxford English Dictionary; Oxford University Press eBooks: Oxford, UK, 2023. [CrossRef]
- s.v. “orthosis, n”. In Oxford English Dictionary; Oxford University Press eBooks: Oxford, UK, 2024. [CrossRef]
- s.v. “exoskeleton, n”. In Oxford English Dictionary; Oxford University Press eBooks: Oxford, UK, 2024. [CrossRef]
- Ellis, H. The early days of splints and splinting. J. Perioper. Pract. 2011, 21, 251–252. [Google Scholar] [CrossRef]
- Gray, B.; Santy-Tomlinson, J. The Thomas’ splint: Application and patient care. Int. J. Orthop. Trauma Nurs. 2018, 30, 20–22. [Google Scholar] [CrossRef]
- Forssmann, A. Sophistication in Ancient Egypt: A 3000-year-old prosthesis. In National Geographic History; National Geographic Partners: Washington, DC, USA, 2017; Available online: https://historia.nationalgeographic.com.es/a/sofisticacion-antiguo-egipto-protesis-hace-3000-anos_11639 (accessed on 19 February 2025).
- Genêt, F.; Schnitzler, A.; Mathieu, S.; Autret, K.; Théfenne, L.; Dizien, O.; Maldjian, A. Orthotic devices and gait in polio patients. Ann. Phys. Rehabil. Med. 2010, 53, 51–59. [Google Scholar] [CrossRef]
- Yagn, N. Apparatus for Facilitating Walking, Running, and Jumping. United States Patent Office. United States Patent 420,179, 28 January 1890. Available online: https://patents.google.com/patent/US420179A/en (accessed on 19 February 2025).
- Guan, X.; Ji, L.; Wang, R. Development of exoskeletons and applications in rehabilitation. MATEC Web Conf. 2016, 40, 02004. [Google Scholar] [CrossRef]
- Splint. In Cambridge Dictionary; Cambridge University Press: Cambridge, UK, 2024; Available online: https://dictionary.cambridge.org/us/dictionary/english/splint (accessed on 19 February 2025).
- Prosthesis. In Cambridge Dictionary; Cambridge University Press: Cambridge, UK, 2024; Available online: https://dictionary.cambridge.org/us/dictionary/english/prosthesis?q=Prosthesis (accessed on 19 February 2025).
- Orthosis. In Cambridge Dictionary; Cambridge University Press: Cambridge, UK, 2024; Available online: https://dictionary.cambridge.org/us/dictionary/english/orthosis?q=Orthosis (accessed on 19 February 2025).
- Exoskeleton. In Cambridge Dictionary; Cambridge University Press: Cambridge, UK, 2024; Available online: https://dictionary.cambridge.org/us/dictionary/english/exoskeleton (accessed on 19 February 2025).
- Ferula. Diccionario Médico. (s. f.). Available online: https://www.cun.es/diccionario-medico/terminos/ferula (accessed on 19 February 2025).
- splint. In En Merriam-Webster Dictionary; Merriam-Webster: Springfield, MA, USA, 2025; Available online: https://www.merriam-webster.com/dictionary/splint (accessed on 19 February 2025).
- Vargas Negrín, F. Indications of orthoses in primary care. FMC—Contin. Med. Educ. Prim. Care 2017, 24, 465–478. [Google Scholar] [CrossRef]
- Manuel, C.B.J. Biomechanics in AFOs: Podopediatric AFOs. Span. J. Podiatry 2012, 23, 184–194. [Google Scholar]
- National Institute for Occupational Safety and Health (INSST). NTP 1162: Exoskeletons I: Definition and Classification. INSST Portal. 2021. Available online: https://www.insst.es/documentacion/colecciones-tecnicas/ntp-notas-tecnicas-de-prevencion/34-serie-ntp-numeros-1152-a-1168-ano-2021/ntp-1162-exoesqueletos-i-definicion-y-clasificacion (accessed on 19 February 2025).
- Arroyave-Tobon, S.; Drapin, J.; Moretto, P.; Linares, J.-M. Design features of the kinematic chain of the ant exoskeleton. Procedia CIRP 2023, 119, 855–860. [Google Scholar] [CrossRef]
- Crea, S.; Beckerle, P.; De Looze, M.; De Pauw, K.; Grazi, L.; Kermavnar, T.; Masood, J.; O’Sullivan, L.W.; Pacifico, I.; Rodríguez-Guerrero, C.; et al. Occupational exoskeletons: A roadmap toward large-scale adoption. Methodology and challenges of bringing exoskeletons to workplaces. Wearable Technol. 2021, 2, e11. [Google Scholar] [CrossRef] [PubMed]
- Miao, Q.; Zhang, M.; Cao, J.; Xie, S.Q. Reviewing high-level control techniques on robot-assisted upper-limb rehabilitation. Adv. Robot. 2018, 32, 1253–1268. [Google Scholar] [CrossRef]
- Preethichandra, D.M.G.; Piyathilaka, L.; Sul, J.-H.; Izhar, U.; Samarasinghe, R.; Arachchige, S.D.; de Silva, L.C. Passive and active exoskeleton solutions: Sensors, actuators, applications, and recent trends. Sensors 2024, 24, 7095. [Google Scholar] [CrossRef] [PubMed]
- Denby, C.; Stone, T. Chapter 18—Neurological measurement. In Clinical Engineering, 2nd ed.; Taktak, A., Ganney, P.S., Long, D., Axell, R.G., Eds.; Academic Press: Cambridge, MA, USA, 2020; pp. 309–319. [Google Scholar] [CrossRef]
- Zhao, Y.; He, F.; Guo, Y. EEG signal processing techniques and applications. Sensors 2023, 23, 9056. [Google Scholar] [CrossRef] [PubMed]
- Human In Motion Robotics—Intelligent Innovation in Human Motion. 2014. Available online: https://humaninmotion.com/ (accessed on 19 February 2025).
- Ankle Exoskeleton Enables Faster Walking. Stanford Report, Stanford University. 2021. Available online: https://news.stanford.edu/stories/2021/04/ankle-exoskeleton-enables-faster-walking (accessed on 19 February 2025).
- Exoskeleton Makes Walking Faster, Less Tiring. Stanford Report, Stanford University. 2022. Available online: https://news.stanford.edu/stories/2022/10/exoskeleton-makes-walking-faster-less-tiring (accessed on 19 February 2025).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).