Abstract
Recent developments in sensors, wireless communications, and data processing technologies are the main drivers for adopting the Internet of Things (IoT) in healthcare systems. IoT-based healthcare systems can enhance the quality of life significantly and help prevent the occurrence of health problems and epidemics. Deploying IoT-based healthcare on a massive scale raises several issues and challenges. One of the main challenges is the management of the end-to-end network connections of the IoT-based healthcare system. This paper presents a comprehensive survey of smart network management protocols that improve IoT-based healthcare efficiency, ensuring real-time monitoring, secure data transmission, and effective device management. Moreover, a reference architecture has been proposed for the network management of IoT-based smart healthcare systems to ensure the sustainability of service delivery to patients and caregivers. The architecture avoids health-related risks and anomalies by incorporating proper network management techniques and operational requirements pertaining to smart healthcare systems. This paper also discusses architectural implementation insights supported by new technologies such as software-defined networking (SDN) and deep learning (DL). Finally, this paper explores emerging paradigms to advance next-generation network management protocols for future smart healthcare systems.
Keywords:
wireless body area network; Internet of Things; patient monitoring; smart healthcare; location contexts; network management; wearable devices MSC:
68-02
1. Introduction
The widespread development of Internet of Things (IoT)-based smart systems and the integration of different infrastructure technologies has inspired several academic and industrial institutions to adopt IoT-based research and development and consider it in their strategic plans. Professionals estimate that the number of connected IoT objects will reach 500 billion by 2030 [1]. The development of IoT technologies stimulated the massive deployment of a wide range of intelligent small-form-factor sensing devices in various vertical applications. Sensing devices are characterized by constrained energy resources, limited processing capability, and limited Radiofrequency (RF) communication capabilities [2]. Sensing devices and sensor networks are being implemented and deployed in several domains, like homes, hospitals, factories, mobile phones, shopping malls, roadsides, and vehicles. Despite their benefits, some barriers still limit their social acceptance. Yang et al. [3] discussed these barriers and their solutions. The core concept of IoT is to enable smart sensors to interact autonomously, eliminating the need for human intervention and facilitating a new range of applications. IoT is anticipated to integrate various technologies, allowing physical objects to connect and support intelligent decision-making [4].
One of the key application domains of IoT is healthcare, where medical sensors track vital health indicators such as body temperature, blood glucose levels, and blood pressure [5]. By 2030, the healthcare sector is projected to have the most substantial global economic influence among IoT applications, with an estimated market value between USD 1.4 and 3.3 trillion annually [4]. This contribution is particularly notable given that the overall economic impact of IoT is expected to range from USD 5.5 to 12.6 trillion per year [6]. Advances in sensor technology, wireless communication, and data processing play a crucial role in enabling IoT-driven healthcare solutions. These sensors facilitate patient monitoring, daily activity tracking, and elderly care. The adoption of IoT in healthcare is expected to significantly improve the quality of life and aid in the prevention of health complications.
Smart systems are predictive and operate autonomously, interacting with the environment to make critical decisions based on the collected data. These systems are a cornerstone of Healthcare 4.0 [7], an evolution driven by the convergence of advanced technologies to enhance healthcare services and patient outcomes. Healthcare 4.0 leverages cutting-edge concepts like the Internet of Things (IoT), artificial intelligence (AI), big data analytics, cloud computing, edge computing, and cyber–physical systems to revolutionize healthcare delivery. Incorporating sensors and actuators into medical and environmental products provides healthcare professionals with precise tools to monitor and treat patients at the hospital and home. These smart systems improve patient care and integrate seamlessly with telemetric and tele-diagnostic infrastructure to significantly reduce decision response time. This integration is particularly valuable in containing epidemic diseases and optimizing healthcare expenditures.
Managing devices and networks in IoT-enabled smart healthcare systems differs significantly from traditional networks. Unlike general-purpose systems, healthcare systems must manage patient-related and environmental data with high precision and reliability. Fault management is critical to these systems, as failures can lead to severe consequences for patient health. Unlike traditional wireless sensor networks that rely on reactive fault-tolerant techniques such as redundancy, proactive network management leverages predictive analytics, machine learning, and real-time monitoring to prevent failures before they occur. By continuously analyzing sensor data, AI-driven fault detection systems can identify early indicators of potential device malfunctions and trigger preemptive maintenance or load balancing. This proactive approach ensures continuous system operation, minimizes downtime, and enhances the reliability of healthcare services [8]. Additionally, self-healing network architectures that dynamically adjust routing paths or reallocate computational resources improve resilience against unexpected failures, particularly in environments with life-critical applications.
Healthcare 4.0 brings about a paradigm shift in how healthcare systems operate. It emphasizes interoperability, scalability, and intelligence across all healthcare processes. Integrating cloud and edge computing enables distributed processing and real-time decision-making, reducing latency and improving efficiency. Additionally, advanced analytics and machine learning algorithms enhance the predictive capabilities of healthcare systems, enabling early intervention and personalized care. This holistic approach redefines healthcare into a smart, connected, and adaptive ecosystem [9].
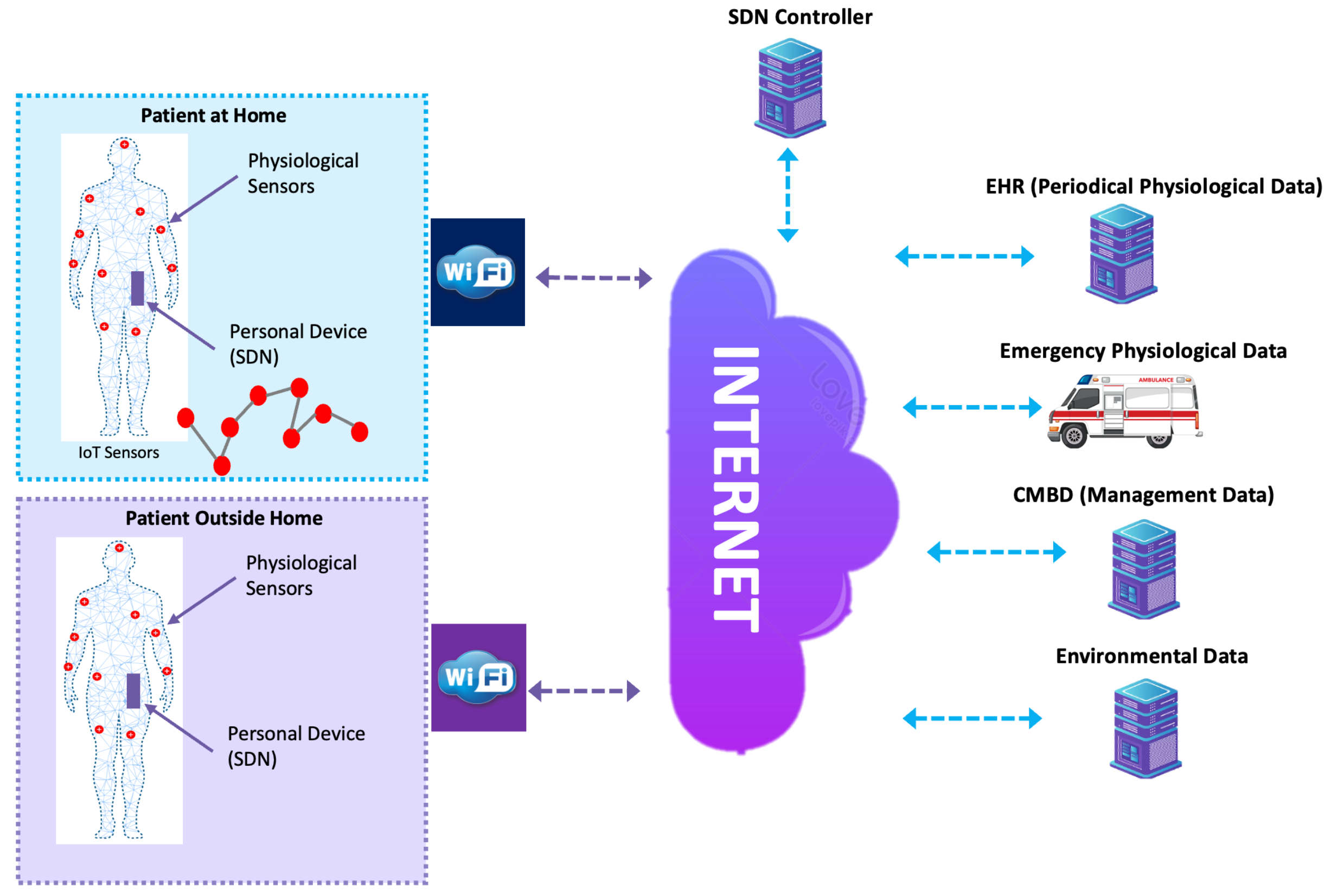
Despite numerous research studies that have addressed IoT-based network management, there are several open issues, especially in the healthcare field. Smart healthcare systems’ device and network management needs a well-defined design strategy before considering their technical problems. The strategy should consider all organizations involved in providing end-to-end services to end-users. For instance, if a healthcare provider remotely monitors a patient at home, the end-to-end connection includes different segments of network authorities. The first segment is located on the patient’s premises, which usually consists of sensors, actuators, gateways, and Wi-Fi networks. The connection between the patient’s premises and the healthcare provider may go through several Internet Service Providers (ISPs). Finally, the healthcare provider segment may include network elements, wireless and wired connections, and backend servers. Therefore, the entities involved should cooperate and support the end-to-end solution to guarantee a reliable and secure service. The design strategy should articulate all technical and medical requirements that should be handled in the implementation to cope with the constraints of IoT objects and the sensitivity of smart healthcare applications. In addition, deploying IoT-based smart healthcare systems on a massive scale would raise other issues. Patients and elderly individuals will rely on the service to monitor their health and daily wellness, while caregivers should provide reliable, secure, effective, and well-performed services. If an IoT-based smart healthcare system is not effective, reliable, and secure, patients’ and elderly individuals’ health becomes prone to risk. In addition, if it does not provide a reasonable return on investment, the caregiver’s business model will be unsatisfactory. This research includes a literature review of IoT-based smart healthcare systems and management solutions referenced in [10]. We comprehensively reviewed network management protocols that suit IoT-based smart healthcare systems based on telecommunications management standards. Moreover, we propose a reference architecture to support network management protocols in smart healthcare network management. The main contributions of the paper are as follows:
- 1.
- This paper explores the integration of various smart network management protocols to enhance the efficiency and reliability of IoT-based healthcare systems. It evaluates protocols that facilitate real-time monitoring, secure data transmission, and efficient device management in resource-constrained environments.
- 2.
- This paper introduces a reference architecture designed to manage the end-to-end network of smart healthcare systems. It ensures sustainable service delivery for both patients and caregivers while addressing challenges such as fault management, security, and scalability. The architecture integrates emerging technologies like software-defined networking (SDN) and deep learning (DL) to enhance network adaptability and predictive management.
- 3.
- Finally, this paper explores emerging paradigms to advance next-generation network management protocols for future smart healthcare systems.
This paper is organized as follows: Section 2 presents the literature review, while Section 3 explores smart healthcare remote monitoring contexts. Section 4 discusses network management protocols, and Section 5 introduces the reference architecture for smart healthcare systems. Section 6 outlines the architecture implementation plan, detailing deployment strategies. Section 7 delves into Advanced Futuristic Network Management Protocols, addressing emerging techniques for enhancing network efficiency and reliability. The paper concludes with key findings and future research directions.
2. Literature Review
The vast deployment of the Internet of Things, Wireless Body Area Networks (WBANs), and the associated standards (e.g., IEEE 802.15.4 [11] and IEEE 802.15.6 [12]) have boosted the emergence of smart healthcare systems. Despite their acceptance in the healthcare sector, smart healthcare systems still face challenges that hinder their large-scale deployment. This section surveys scholarly research studies that tackle the large-scale deployment of smart healthcare systems. This section starts with a literature review of IoT and its architectures, applications, and protocols. Then, it reviews topics related to Wireless Body Area Networks, as these networks play an essential role in the context of smart healthcare systems. Finally, a discussion of the network management of IoT systems is presented.
2.1. Internet of Things
Interest in IoT has increased among industrial and academic institutions, which has necessitated the development of testbeds and platforms to evaluate IoT solutions. Gluhak et al. identified some requirements for IoT experimental facilities [13]. They surveyed currently available research testbeds and suggested new directions. The development of IoT-based systems is an incremental process starting from existing technologies and applications. IoT-based systems should comply at a minimum with these non-functional requirements: heterogeneity, scalability, ubiquitous data exchange through proximity wireless technologies, energy-optimized solutions, localization and tracking capabilities, self-organization capabilities, semantic interoperability as well as data management, and embedded security and privacy-preserving mechanisms [14].
Even though IoT is envisioned to augment the global Internet and make a unified mega-network that connects the physical and digital worlds, current Internet protocols may not apply to IoT due to its resource-constrained devices. Therefore, the IETF is developing new protocol suites tailored to the IoT paradigm [2]. Al-Fuqaha et al. [4] summarized the most relevant protocols and discussed some application issues related to IoT. They also discussed relations between IoT and emerging technologies like big data and cloud computing. Whitmore et al. [15] presented the current state of research on IoT through an intensive literature review. They identified current trends and described challenges that threaten IoT diffusion. Interested researchers in this area may consult the same paper for open research questions, future directions, and a comprehensive reference list.
As of today, IoT consists of heterogeneous devices, technologies, and protocols, making it difficult for hardware and software developers to develop applications that seamlessly integrate. This heterogeneity necessitates the involvement of middleware that supports standard functional and non-functional IoT requirements [16]. In addition, middleware provides hardware and software abstractions that facilitate developers’ work so that they focus more on their applications. IoT-based applications generate considerable data (i.e., big data) that require storage, analysis, and ease of access. These requirements pose challenges for systems deployed within enterprises. Therefore, there is a need to integrate cloud computing and IoT [17]. This work provided a literature survey on integrating the cloud, IoT, and applications. They also discussed the available platforms for cloud and IoT integration.
Mobility management is an inevitable requirement for the IoT paradigm. Objects attached to people, vehicles, animals, etc., move with their hosts’ bodies. Mobility represents a significant challenge for IoT, which requires extensive research to develop suitable algorithms and protocols to handle it. Ghaleb et al. [18] reviewed and discussed algorithms to address IP integration challenges with resource-constrained IoT devices. They also provided a comprehensive review encompassing the mechanisms, advantages, and disadvantages of related works on IPv6 mobility management. For areas with poor social infrastructures and information communication infrastructures, IoT can be deployed to provide an IoT-based mobility information network [19]. An IoT-based mobility management information network consists of fixed wireless nodes deployed on many roads (semi-electrostatic field sensor, acceleration sensor, gyro sensor, temperature sensor, humidity sensor, infrared sensor, and sensor server) and mobile nodes. Mobile nodes collect data captured by road sensors while moving along the roads and transmit them via the Internet to residents. Such transmitted data are intended to help in disaster prevention, sightseeing information, and shopping.
Fifth-generation (5G) mobile networks have become the preferred choice for connecting IoT devices to backend systems, offering capabilities far beyond those of fourth-generation (4G) networks [20]. While 4G supported the initial wave of IoT adoption, the rapid growth in IoT devices and applications soon exceeded its performance limits, particularly in bandwidth, latency, and overall network efficiency. The transition to 5G has significantly expanded the scope of IoT, offering remarkable speed and ultra-low latency. It provides tailored solutions to meet the diverse demands of IoT applications, particularly in healthcare, where real-time data transmission, remote monitoring, and telemedicine services are critical for improving patient outcomes and operational efficiency. Mahdi et al. [21] reviewed ongoing advancements in IoT, highlighting the transformative impact of 5G while exploring the potential of sixth-generation (6G) networks to meet future demands for ubiquitous IoT connectivity and enhanced service capabilities.
Stankovic [22] identified eight key research areas that tackle existing challenges and encourage further investigation. These areas include large-scale system expansion, architectural design, interdependencies in knowledge generation and big data, system resilience, openness, security, privacy, and human-in-the-loop considerations. Despite these advancements, numerous unresolved research challenges remain, primarily due to the complex nature of system deployment and the strict requirements imposed by various services utilizing these complex frameworks. Therefore, it is essential to examine existing standardization efforts, explore ways to enhance them, and identify research opportunities that will contribute to the advancement of the IoT field.
IoT influenced enterprises’ and governments’ digital strategies with disruptive business models and fast-changing markets. Many vertical industrial sectors, like transportation, healthcare, and logistics, have incorporated IoT into their digital strategy. IoT still experiences heterogeneity issues in devices, technologies, and protocols. These heterogeneity issues impose challenges on new IT strategies. Zimmermann et al. [23] described a new meta-model-based approach for integrating IoT architectural objects semi-automatically federated into a holistic digital enterprise architectural environment. The large-scale deployment of IoT in various vertical applications is still a challenge. The most important is the diversity of protocols developed for IoT and WSNs [24]. For a recent survey of IoT architectures, protocols, and challenges, the reader may refer to [25].
IoT provides several services that can be utilized to create many vertical applications. IoT services can be divided into four categories: identity-related services, information aggregation services, collaborative-aware services, and ubiquitous services [26]. IoT applications may use the services of one or more of these categories. Moreover, IoT services are essential to application developers to help them focus on their tasks, while the services are provided through some middleware technologies.
Cook et al. [27] presented a full-fledged smart home application based on the ZigBee WSN. This is a product in a box that can be easily installed in homes to monitor specific parameters. The product utilizes recent application protocols developed initially for WSNs and later adopted for IoT. Smart homes can be connected through their gateways and form a smart community [28]. An innovative community could provide useful services to its residents, specifically the elderly and residents with disabilities, by incorporating smart healthcare and connecting it to a community call center. Another exciting possible application of IoT is smart cities that allow municipalities to incorporate IoT into their cities [29].
2.2. Smart Healthcare
Smart IoT objects fulfill the requirements of ubiquitous communication, pervasive computing, and ambient intelligence [30]. These characteristics have encouraged scientific and industrial developers to propose services and applications for the healthcare industry. A direct and useful application of IoT in healthcare is the Ambient Assisted Living (AAL) application, which aims to help older people and people with disabilities and chronic diseases live their everyday lives without being restricted by conventional monitoring and assistive tools. Also, people can stay in their homes and receive treatment similar to that which they would receive if admitted to a hospital [31]. Bui et al. [32] inferred the non-functional requirements for smart healthcare applications through the storyline of a person with diabetes. They highlighted the requirements for interoperability, bounded latency, reliability, and security as the main ones for successful monitoring and supervision. IoT can be used to manage the administration of diabetic therapy by developing a personal device to assist and manage the insulin therapy dosage calculation [33]. The authors provided an overall architecture based on new communications protocols developed by the IETF that enable the connectivity of personal devices with the global Internet. A new concept called ‘Health Internet of Things (HIoT)’ was proposed to exploit sensor technologies and wireless networks for monitoring medical conditions [34]. This work presents an interconnection framework for mobile Health (mHealth) based on IoT.
Jung [35] explored how wearable and motion sensors, in the context of a smart home, can be used to monitor the movement of senior citizens by continuously logging and reporting their vital signs and the surrounding environmental conditions. It is worth mentioning that pervasive computing, as part of the IoT paradigm, is becoming an essential part of consumers’ electronics and can be integrated with a smart home environment to adopt a smart-home-based healthcare model [36]. Collected data from various sensors deployed throughout the home can generate a smart home visualization system that provides different analyses to help detect and understand abnormal behaviors of targeted household residents [37]. Integrating mobile health as part of smart cities is becoming inevitable [38]. The authors provided an overview of how smart health can complement mobile health as part of a smart city initiative. They discussed the various aspects needed to achieve a comprehensive strategy for providing smart healthcare applications as part of a smart city environment. Ghose et al. [39] proposed a mobile software platform for ubiquitous healthcare support in homes and small clinic areas. The IoT platform replaces the PC gateway used in traditional telemedicine with a mobile device to ensure mobility support. Santos et al. [40] proposed an IoT-based mobile health and patient monitoring application. The proposed application is a set of health monitoring services deployed in a mobile gateway device. It collects real-time information about the user’s heart rate, location, and environmental conditions and forwards them to an intelligent personal assistant platform called AMBRO. Pereira et al. [41] studied the performance of IoT-based mobile e-health applications and services.
Khattak et al. [42] conducted a comprehensive survey on the technologies and methodologies used for connecting and monitoring medical sensors. They introduced a testbed architecture specifically designed for healthcare applications. Similarly, Rahmani et al. [43] proposed the Smart e-Health Gateway, a system that facilitates the connection between sensor networks and the Internet. This gateway effectively addresses several challenges in ubiquitous healthcare systems, including energy efficiency, scalability, and reliability. Implementing Smart e-Health Gateways on a large scale can significantly enhance ubiquitous health monitoring, particularly in clinical settings. Additionally, they introduced a framework designed for various healthcare environments, including hospitals, specialized clinical settings, patient homes, senior citizen residences, gyms, and mobile healthcare services such as ambulances, mobile clinics, and travel health services.
Islam et al. [44] conducted a review of research on advancements in IoT-driven healthcare technologies. They analyzed cutting-edge network architectures, platforms, applications, and industry developments within IoT-based healthcare solutions. Furthermore, they proposed an intelligent collaborative security framework aimed at mitigating security threats. Their study also explored how emerging technologies such as big data, ambient intelligence, and wearable devices can enhance healthcare applications. Additionally, they examined global IoT and eHealth policies and regulations, assessing their economic and societal impact on sustainable development.
Farahani et al. [45] presented an architecture for applying IoT in healthcare and medicine. The architecture is patient-centric, where all constituents, such as the hospital, patients, and services, are seamlessly connected. The architecture consists of three layers, the device, fog computing, and the cloud, to empower handling complex data in terms of variety, speed, and latency. They also addressed the challenges of IoT eHealth, such as data management, scalability, regulations, interoperability, device–network–human interfaces, security, and privacy. Smart healthcare systems may proactively manage the patient’s health—prevent disease, detect disease early, and improve healthcare outcomes [46]. Adame et al. [47] developed a platform for monitoring healthcare environments that integrates RFID and WSN technologies, providing the location, status, and tracking of patients and assets.
2.3. WBAN
The IEEE 802.15.4 standard, published in 2006, specifies the PHY and the MAC layers for short-range, low-power, low-cost, and low-bit-rate networks. These capabilities make it suitable for general WSN applications and IoT applications. However, IEEE 802.15.4 was not intended to support wireless communications in the vicinity of or inside the human body [12]. Therefore, IEEE 802.15 Task Group 6 initiated WBAN standardization activities in November 2007. The group recognized that existing standards did not fully meet the medical (i.e., proximity to human tissues) and relevant communication regulations for some application environments. The first draft was released in May 2010, and the final version was published in February 2012. IEEE 802.15.6 is targeted to serve a range of medical and non-medical applications.
Since its initial release, the IEEE 802.15.6 standard has undergone revisions to accommodate emerging use cases. The IEEE 802.15.6ma project is updating the standard to improve dependability for Human Body Area Networks (HBANs) and expand its applicability to Vehicle Body Area Networks (VBANs) [48]. Additionally, an amendment has been introduced to enhance the Ultra-Wideband (UWB) physical layer (PHY) and medium access control (MAC) to support more reliable communication in HBANs [49]. These advancements reflect ongoing efforts to refine WBAN standards to address modern medical and non-medical requirements better.
Cavallari et al. [50] surveyed the main WBAN applications, technologies, and standards, as well as issues related to WBAN design and evolution. They also presented a comparative study of the WBAN standards with simulation and experimental results. In another work [51], the authors surveyed the current state-of-the-art WBANs based on the latest standards and publications. They also discussed some open issues and challenges with WBANs. Healthcare systems in residential environments use WBANs for remote monitoring and health management. Ghamari et al. [52] provided an architecture for residential environment healthcare systems and stated the technologies and networks needed in such an environment.
2.4. IoT Network Management Protocols
The Simple Network Management Protocol (SNMP) is the standard management protocol for traditional TCP/IP networks. However, several issues make SNMP ineffective for IoT. Firstly, the communication overhead associated with SNMP is significant for low-bandwidth and low-power wireless IoT links. Secondly, SNMP follows a centralized management approach where the management station pulls the managed nodes at specified intervals. Thirdly, Management Agent and Management Information Base (MIB) object variables should be configured at each sensor node, which often has limited storage. Finally, SNMP may not adequately handle sensor-specific failures, which is common in IoT [53].
Sheng et al. [54] conducted a review of IoT network management and highlighted that, despite extensive research on various aspects of sensor networks, the management of sensor devices remains largely unexplored. To bridge this gap, a lightweight web service grounded in REST (Representational State Transfer) principles was introduced to streamline wireless sensor device management. Leveraging IPv6-based open standards, the service enables access to resource-restricted wireless networks. Specifically, it incorporates essential IETF protocols intended for such environments, including IPv6 over Low-Power Wireless Personal Area Networks (6LoWPANs), the Routing Protocol for Low-Power and Lossy Networks (RPL), and the Constrained Application Protocol (CoAP). A CoAP-driven device management method further simplifies the administration and accessibility of IPv6-capable sensor devices.
Given that end-to-end connectivity in IoT environments involves multiple networks with varying performance and connectivity requirements, sectional monitoring is suggested as a more effective management strategy [55]. Furthermore, a layered fault management scheme is recommended for end-to-end transmission to accommodate the heterogeneous nature of IoT networks.
Lindholm et al. [56] examined the feasibility of deploying SNMP (Simple Network Management Protocol) in IoT environments and found it to be highly challenging, despite its established usefulness as an Internet management protocol. By leveraging the CoAP protocol, they explored techniques that enable SNMP-based tools and applications to coexist and interact with CoAP-enabled endpoints. While SNMP has the potential to manage sensors in IoT networks [57], its implementation is impractical due to excessive memory and power consumption, as well as increased communication overhead.
Fault tolerance is a critical yet challenging non-functional requirement in IoT systems, particularly in healthcare applications. While fault tolerance mechanisms can be effectively applied to IoT applications such as smart homes [58], they may not be suitable for certain smart healthcare scenarios, such as implanted sensors. A study in [59] explores the opportunities and challenges of healthcare monitoring and management within the IoT framework, incorporating cloud-based processing. The same study also reviews the current state and future directions for integrating remote health monitoring technologies into clinical medical practice.
Gia et al. [60] propose an IoT-based architecture that supports scalability and fault tolerance in healthcare applications. However, their approach primarily addresses faults in a reactive manner, meaning it lacks proactive mechanisms to assess the condition of sensor nodes and prevent failures in advance.
The widespread adoption of smart applications and services is expected to generate vast amounts of data, including text, audio, and video, necessitating batch, interactive, or real-time processing. One of the key challenges is the integration of heterogeneous data from multiple sources [61]. To address this, researchers have developed a flexible and cost-effective infrastructure that incorporates cloud and fog computing, blockchain technology, and message brokers to enable secure and private IoT deployment for smart healthcare applications and services. Another major challenge is efficiently managing this large volume of data throughout its lifecycle.
Gharaibeh et al. [62] take a data-centric approach, outlining key data management techniques designed to ensure the consistency, interoperability, granularity, and reusability of IoT-generated data in smart cities. Additionally, they identify security and privacy strategies while discussing the networking and computing technologies that support smart city implementations [63].
The Open Mobile Alliance (OMA) SpecWorks [64] developed a device management protocol called LightweightM2M (LwM2M). The protocol is designed for sensor networks and supports a machine-to-machine (M2M) environment. It has also been developed to manage lightweight and low-power devices on various networks, which is necessary to realize the potential of IoT. The LwM2M protocol features an architectural design based on REST. It defines an extensible resource and data model and builds on the CoAP standard, making it suitable for the remote management of M2M devices and related service enablement.
The Message Queuing Telemetry Transport (MQTT) protocol, widely used in IoT systems, is vulnerable to various cyberattacks, including replay and Man-in-the-Middle (MITM) attacks. A novel cyber range system was proposed in [65] to analyze vulnerabilities and implement countermeasures. This system provides an experimental environment for real-world attack scenarios, supporting new research to enhance MQTT protocol security and ensure robust communication in IoHT systems.
To address network congestion and reliability issues in IoHT, an adaptive data communication model was introduced in [66]. The model ensures efficient and reliable data transmission in high-traffic scenarios by dynamically switching between MQTT-SN and CoAP protocols based on network conditions.
A hybrid network management system combining the NETCONF protocol and decision tree algorithms was designed to improve configuration efficiency and fault diagnosis in IoHT networks [67]. This system achieves a fault diagnosis accuracy of 96%, outperforming traditional methods and demonstrating the potential of AI in enhancing network management scalability and adaptability.
A comparative analysis of the Lightweight Machine to Machine (LwM2M) and Extensible Messaging and Presence Protocol (XMPP) highlights their suitability for IoHT applications in [68]. While LwM2M offers efficient device management and low power consumption, XMPP supports robust messaging in constrained systems. The study recommends protocol selection based on specific IoHT application needs.
3. Smart Healthcare Remote Monitoring Contexts
The Internet of Things (IoT) extends Internet connectivity beyond conventional devices such as desktops, laptops, tablets, and smartphones, enabling a broader range of computing and communication-enabled objects. These objects, equipped with sensing, computing, and communication capabilities, can be integrated with both living and non-living entities. In the context of smart healthcare, such devices facilitate the collection of vital signs and physiological parameters, enabling continuous patient monitoring and timely medical interventions.
Smart healthcare is poised to transform the healthcare industry by offering personalized and adaptive healthcare environments. However, for the effective deployment and management of a robust smart healthcare system, it is crucial to understand the various contexts in which a patient may exist. This section categorizes the different contextual scenarios that a patient might encounter.
Most smart healthcare solutions advocate the use of a gateway between sensors and the backend server. This gateway can be either a dedicated device or a smartphone equipped with IoT and Wireless Sensor Network (WSN) protocols. By performing preliminary data processing and filtering, these gateways help minimize the volume of data transmitted to the backend. Rahmani et al. [43] proposed a framework designed for various healthcare settings, including hospitals, specialized clinical facilities, home care, senior citizen residences, gyms, and mobile healthcare environments such as ambulances, mobile clinics, and travel health services.
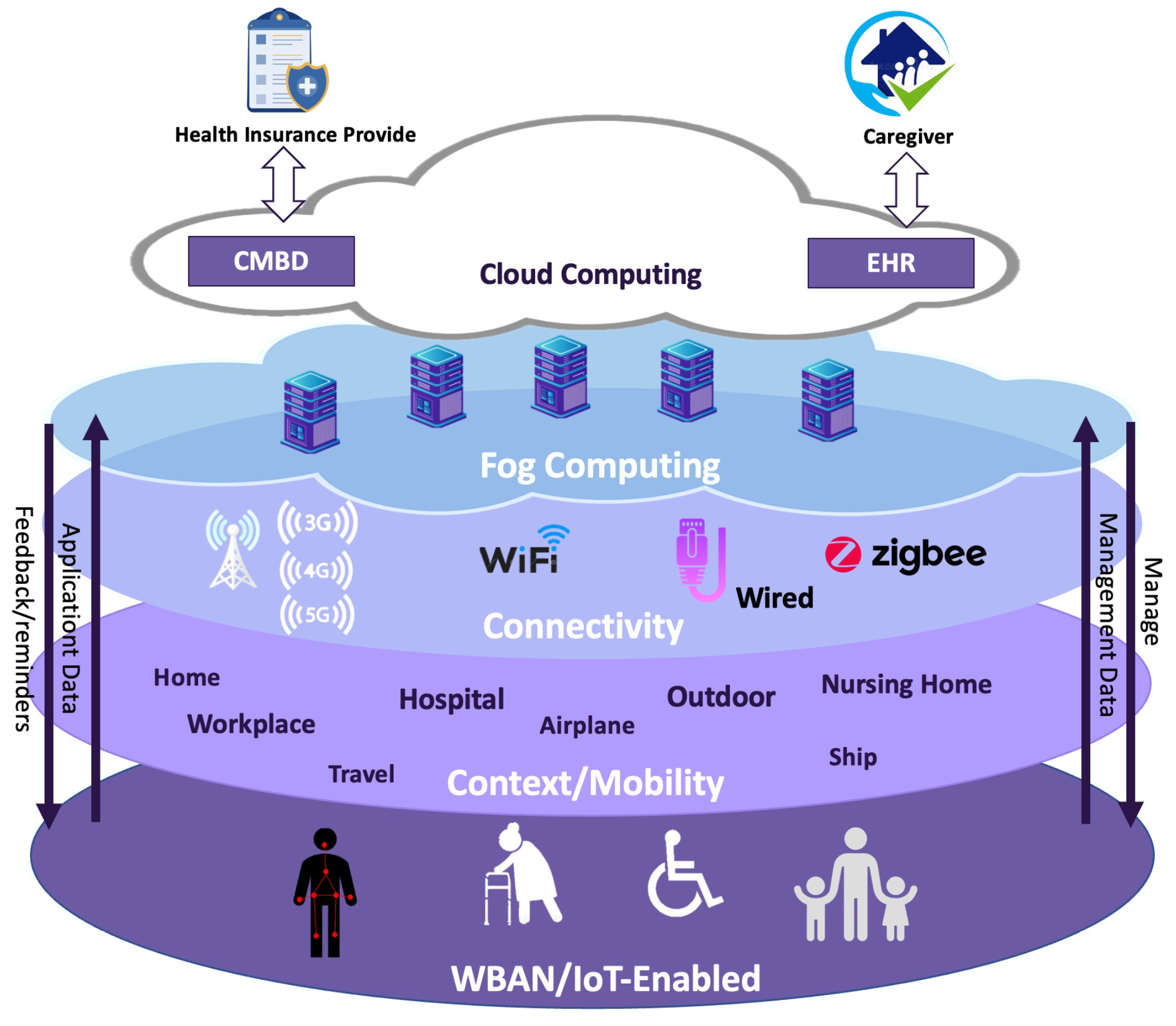
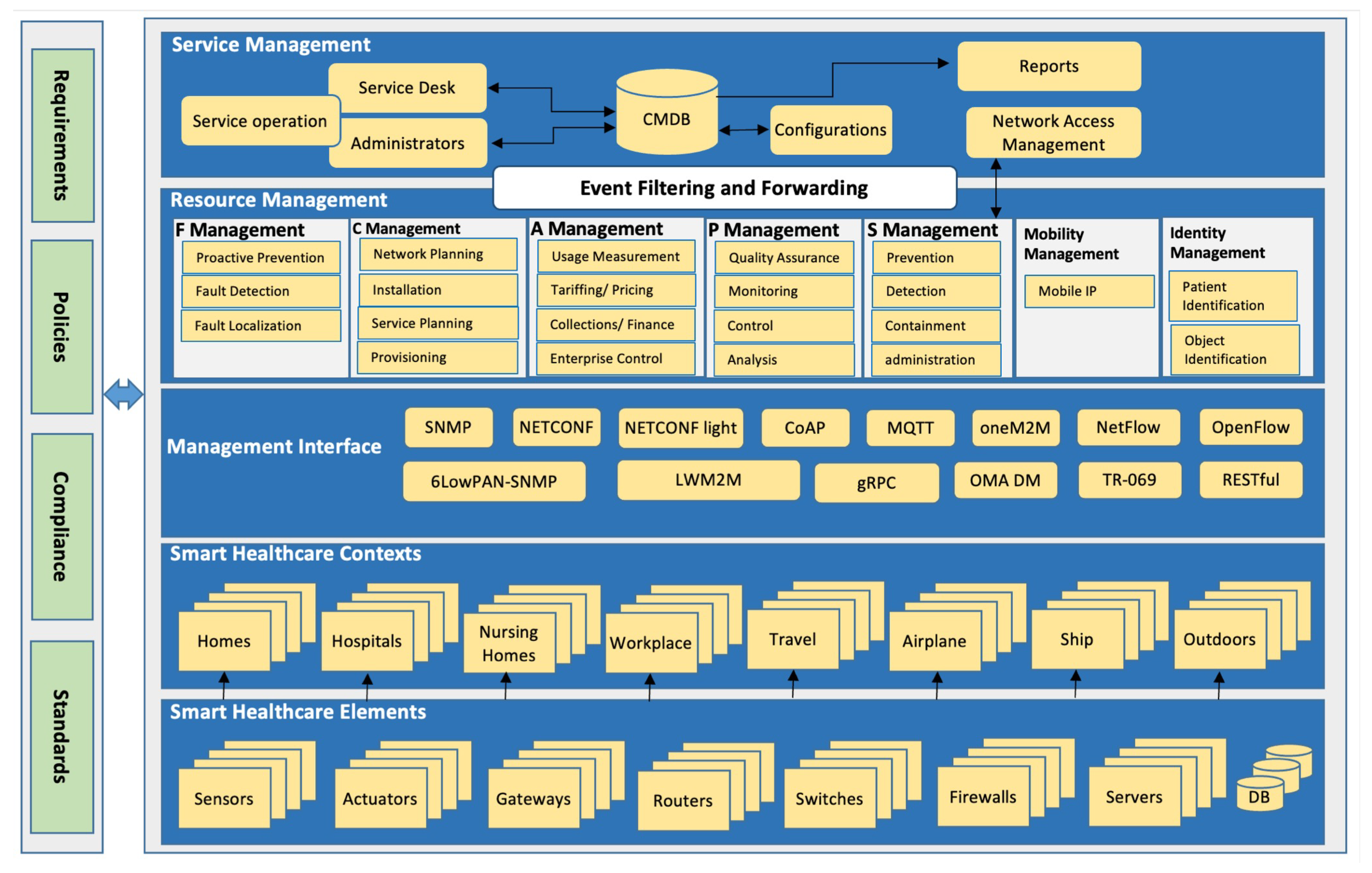
While the primary settings for smart healthcare systems are typically homes, nursing homes, and hospitals, additional contexts can be considered to provide patients with greater mobility and enable them to fully benefit from the IoT framework. Figure 1 presents both conventional and unconventional contexts where smart healthcare systems can be utilized. These contexts are categorized into three main groups, as outlined below.
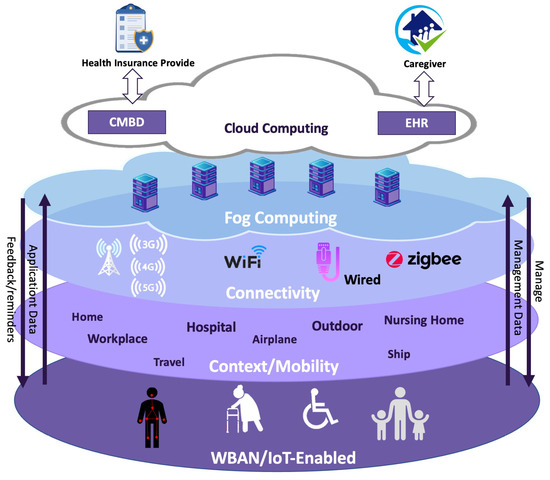
Figure 1.
Typical and atypical location contexts.
3.1. Dominant Contexts (Typical)
These contexts refer to locations where patients spend the majority of their time, including homes, hospitals, and nursing homes. Such environments are characterized by a fixed IoT infrastructure. According to Khattak et al. [42], a sensor network deployed in a hospital—where the infrastructure is stable and continuously powered—differs significantly from a network designed for home-based patient monitoring, where the patient is in a remote setting. Home-based monitoring requires a more pervasive and unobtrusive approach to effectively manage patient care.
Various studies have explored patient monitoring systems in hospital settings [69] and personal monitoring at home [70]. In most IoT-driven patient monitoring solutions, a gateway serves as an intermediary between the sensor network and the Internet. This gateway typically handles essential tasks such as protocol translation between Internet-based systems and sensor networks.
3.2. Considered Contexts (Typical)
These contexts encompass, but are not limited to, the workplace and outdoor environments. Patients can continue their daily activities, including going to work, while being monitored for specific health conditions. Workplace monitoring can be facilitated through a dedicated gateway or by utilizing the patient’s smartphone. When patients travel outside their homes but remain within the same country, connectivity to the backend system can be maintained through their mobile device or a specialized device provided by the service provider.
3.3. Possible Contexts (Atypical)
These contexts should be determined based on the patient’s preferences and health condition. They may include travel-related locations such as airplanes, ships, or international destinations. When a patient travels outside their home country, maintaining connectivity to the healthcare system becomes essential. To address this, the service broker should facilitate seamless integration by connecting the patient to a local service provider in the visiting country. This connection can be established using the patient’s mobile phone or a dedicated device that links them to the home network via the local provider.
4. Smart Healthcare Network Management Protocols
Network management protocols play a crucial role in healthcare systems, enabling the efficient monitoring, configuration, and maintenance of vast device networks. These protocols form the backbone of healthcare system management, ensuring reliable operation and seamless communication between devices and management systems. This section examines the primary protocols that facilitate IoT network management and their specific applications.
4.1. Simple Network Management Protocol (SNMP) in IoT for Healthcare
SNMP operates in a manager–agent architecture, where the manager queries or modifies the state of agents. In healthcare IoT, SNMP monitors devices like wearables and medical equipment, ensuring real-time tracking of device health, usage, and alerts. SNMP enables timely responses to device failures, improving patient safety. The protocol flow is described in Algorithm 1.
| Algorithm 1 SNMP protocol flow |
|
Let M represent the manager, the agents (IoT devices), and the monitored data for agent at time t. Here, f is a function representing the SNMP GET request operation, through which the manager M obtains monitored data from an agent at time t. The SNMP operations are defined as follows:
where explicitly represents the updated monitored data after applying the new parameters . Here, represents the set of parameters or configuration values provided by the manager M at time t. These parameters are used in the SNMP SET operation to update or modify the settings or monitored data of the agent device .
The Simple Network Management Protocol (SNMP) is widely used for network device monitoring and management in centralized healthcare settings, such as hospitals and medical data centers. It facilitates the remote tracking of IoT-enabled medical equipment like ventilators and infusion pumps, allowing healthcare providers to monitor their status and performance in wired, high-bandwidth hospital networks. Moreover, SNMP enhances hospital safety by generating automated alerts for critical device failures, enabling timely maintenance and reducing the risk of equipment malfunctions. This proactive management approach improves healthcare efficiency and ensures reliable medical device operation.
However, SNMP is not well suited for resource-constrained IoT healthcare environments, such as wearable health devices, Wireless Body Area Networks (WBANs), and home-based patient monitoring systems. Its centralized architecture and polling-based communication mechanism result in high bandwidth consumption, increased latency, and excessive energy overhead, making it inefficient for real-time monitoring in power-constrained medical IoT networks. Furthermore, frequent polling mechanisms introduce latency and unnecessary energy consumption in battery-powered medical sensors, limiting SNMP’s applicability in ultra-low-power healthcare scenarios [71].
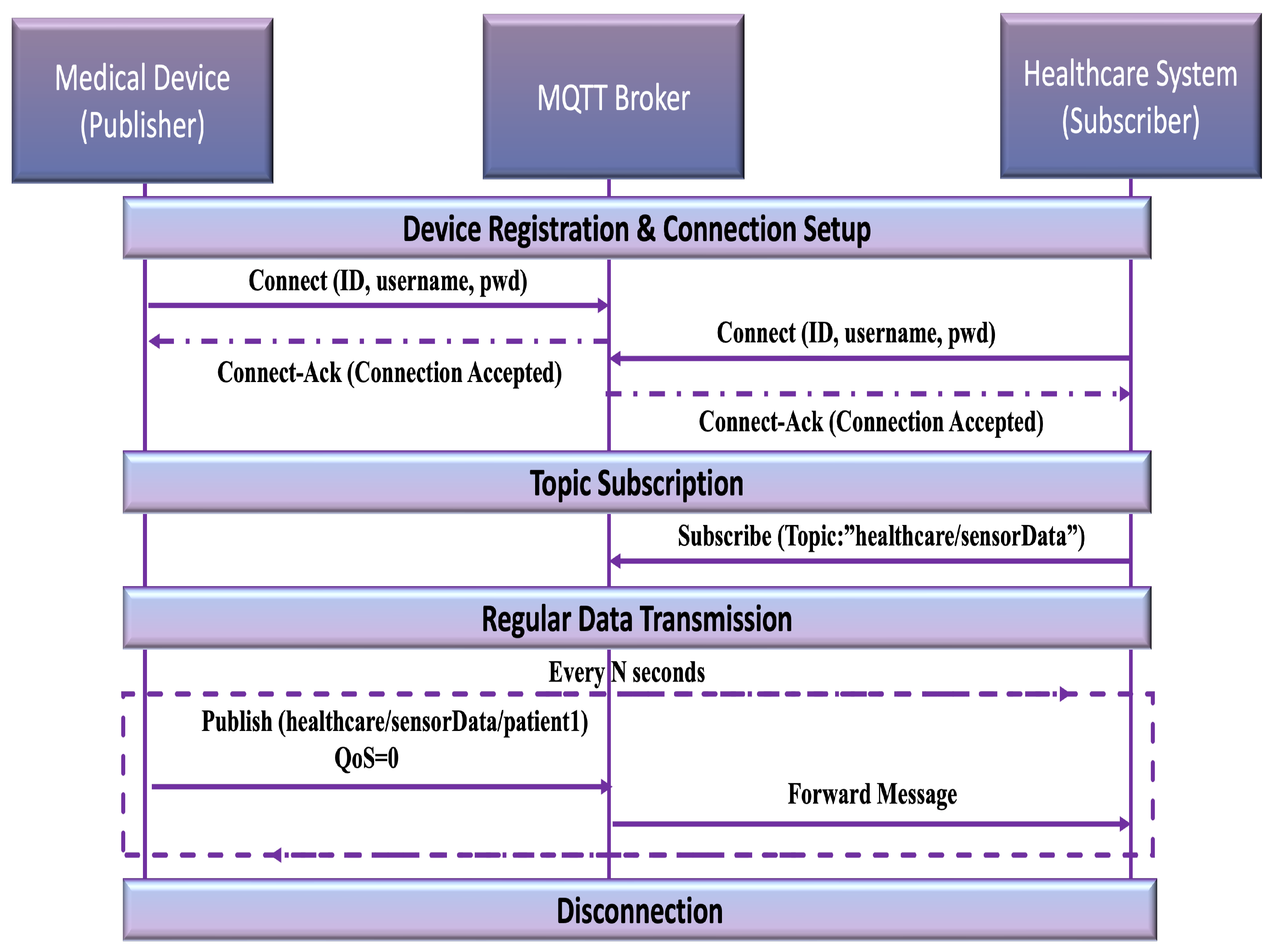
4.2. Message Queuing Telemetry Transport (MQTT)
MQTT [72] is a lightweight messaging protocol designed for low-bandwidth and resource-constrained environments. It operates on a publish/subscribe messaging model, where a central broker manages communication between publishers (data producers) and subscribers (data consumers), as shown in Figure 2. Initially developed for satellite communication, MQTT has become a cornerstone of IoT communications, offering efficiency and scalability. It offers several key features that make it highly suitable for IoT-based healthcare network management [73]. One of its most significant advantages is minimal packet overhead, with packet sizes as small as 2 bytes, ensuring efficient data transmission over low-bandwidth networks. Another crucial feature is its support for different quality of service (QoS) levels, allowing for flexible message delivery reliability. QoS 0 (at most once) sends messages without requiring acknowledgment, making it ideal for non-critical data. QoS 1 (at least once) ensures message delivery with acknowledgment, preventing data loss while avoiding duplicates. QoS 2 (exactly once) guarantees that messages are received and processed only once, ensuring the highest level of reliability for critical applications. Additionally, MQTT includes a Last Will and Testament mechanism, which notifies the broker in case of an unexpected device disconnection. This feature enhances fault detection and allows for timely interventions. Another essential capability is persistent sessions and queuing, which ensures that messages are stored and delivered even when devices experience intermittent connectivity. These features collectively enhance MQTT’s reliability, making it a robust and efficient protocol for managing healthcare IoT networks.
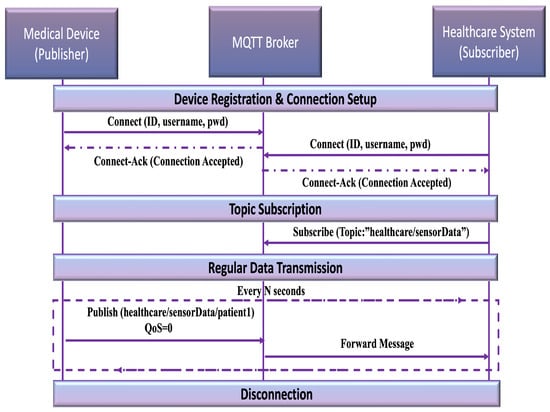
Figure 2.
MQTT protocol.
In network management, MQTT facilitates real-time monitoring by allowing devices to publish telemetry data, enabling network managers to track device status, health, and performance continuously. The protocol also ensures reliable command execution, as messages sent by network managers to devices are delivered based on QoS levels, providing appropriate reliability for various applications. Furthermore, MQTT’s Last Will and Testament feature allows the network to detect disconnected devices and alert administrators for prompt remedial action. Its scalability is another major advantage, efficiently handling communication in large-scale IoT networks with thousands of connected devices while maintaining minimal overhead. These features make MQTT an essential protocol for managing healthcare networks, ensuring reliable and efficient communication across medical devices and systems. However, it lacks robust security features, making it vulnerable to cyber threats [72].
4.3. NETCONF/RESTCONF in IoT for Healthcare
NETCONF [74] and RESTCONF protocols offer effective mechanisms for configuring and monitoring healthcare IoT networks. Utilizing structured data formats such as XML and JSON, they automate network updates, thus ensuring interoperability among diverse healthcare devices.
Configuration updates across devices in the network can be represented by a set:
The manager performs updates to a device by employing a remote procedure call (RPC) as follows:
where is a function describing the update process, M denotes the managing entity, and specifies the current configuration parameters of device . Typically, is implemented as an integral operation defined over time or update steps, represented as
where describes the instantaneous rate or mechanism of configuration change, and and are the initial and final limits indicating the duration of the update process.
The NETCONF and RESTCONF protocols streamline remote configurations, enhancing the seamless integration and interoperability of IoT diagnostic devices in healthcare settings. Additionally, they facilitate secure firmware updates, thus bolstering both security and operational performance. These protocols also provide flexibility in dynamically adjusting configurations during emergencies, ensuring continuous connectivity and efficient operation within healthcare facilities. However, these protocols are relatively complex and may not be ideal for low-power healthcare IoT devices, as they require higher computational resources and introduce parsing overhead due to their reliance on structured data formats like XML and JSON [75].
4.4. gRPC in IoT for Healthcare
gRPC [76] is a communication framework built on top of HTTP/2 that enables high-throughput, bidirectional data exchange between healthcare IoT devices and backend systems. This approach supports both request–response interactions and continuous data streaming, ensuring minimal transmission delays for critical patient information. The Request–Response Model gRPC is defined as follows:
where captures a discrete request at time t and its corresponding response. In a healthcare context, each may represent a specific query for clinical data, while holds the information returned by the device. The Streaming Model is defined below:
where denotes a time-varying function of health-related data (e.g., heart rate or ECG signals). The integration from to aggregates these continuous measurements, which are then delivered in near real time via gRPC streams. Because healthcare applications often require immediate insights, we focus on end-to-end latency. Let be the sending time for a data chunk i and its receiving time. Then, the latency for chunk i can be defined as
Minimizing the average latency is crucial to ensure fast feedback and timely clinical decision-making.
| Algorithm 2 NETCONF-Light |
|
4.5. NETCONF-Light: A Lightweight Protocol for Resource-Constrained Devices
NETCONF-Light [77] is a lightweight version of the NETCONF protocol specifically designed for resource-constrained devices. It provides a streamlined subset of NETCONF operations to facilitate configuration management, including the ability to install, manipulate, and delete network configurations as described in Algorithm 2. The key operations of NETCONF-Light (O) can be expressed as
These operations are applied to device configurations (D), and their effect is to transition the device to a desired configuration state:
where
- D: the set of device configurations.
- State: the target state after applying the operations.
4.6. 6LowPAN-SNMP: Lightweight Management for Resource-Constrained Networks
6LowPAN-SNMP [78] adapts the Simple Network Management Protocol (SNMP) for IPv6 Low-Power Wireless Personal Area Networks (6LowPANs). It introduces mechanisms such as SNMP header compression, as described in Algorithm 3, to reduce message overhead, making it suitable for resource-constrained networks. Compatibility with standard SNMP is maintained through a proxy forwarder that translates between SNMP and 6LowPAN-SNMP messages. The header compression in 6LowPAN-SNMP can be mathematically modeled as
where
- : compression ratio of the SNMP header.
- : original header size.
- : reduced header size after compression.
Applications of 6LoWPAN-SNMP include enabling the lightweight monitoring and management of sensor nodes, facilitating efficient data collection, and detecting sensor failures, transmission errors, and battery levels to ensure reliable operation.
| Algorithm 3 6LowPAN-SNMP |
|
4.7. CoAP Management Interface (CoMI)
The CoAP Management Interface (CoMI) [79] is a specialized protocol for managing IoT devices and networks with constrained resources. It uses CoAP (Constrained Application Protocol) as a transport layer to perform operations on device resources defined in YANG or converted from SMIv2 to YANG. CoMI focuses on lightweight device management and supports actions such as configuring, monitoring, and updating devices.
In CoMI, resource management can be represented using a mapping between YANG-modeled resources and their CoAP representations:
where each resource is identified by a URI. Operations such as GET, POST, PUT, and DELETE are performed over CoAP to manage resources.
CoMI is widely used in smart home systems, environmental monitoring, and wearable device configurations, where lightweight communication is vital. However, despite its efficiency, CoMI faces scalability challenges in complex healthcare IoT networks, where diverse medical devices require high levels of security, fault tolerance, and real-time interoperability [80].
4.8. Lightweight Machine to Machine (LWM2M)
LWM2M (Lightweight Machine to Machine) [81] is a client-server protocol specifically designed for managing IoT (Internet of Things) devices with low power and constrained resources. Developed by the Open Mobile Alliance (OMA), it builds upon protocol and security standards from the Internet Engineering Task Force (IETF). The protocol supports functionalities such as connectivity monitoring, resource monitoring, and firmware upgrades, which are essential for managing IoT ecosystems efficiently.
The LWM2M architecture follows a hierarchical structure. The LWM2M server resides on the network manager device, while LWM2M clients operate on managed IoT devices. These devices organize their resources into objects. For instance, a location object encompasses resources that provide geolocation information. This modular structure facilitates the efficient management of resources.
A mathematical representation of LWM2M operations can be modeled as resource mappings:
where R represents the set of IoT resources organized into objects. The protocol supports operations like read (), write (), and execute ():
Here, V denotes the value space of a resource.
Applications of LWM2M in healthcare include the remote management of medical devices, ensuring timely software updates, continuous performance monitoring, and secure communication. While LwM2M is designed to manage constrained IoT devices and provide efficient remote device management, it may face performance limitations in large-scale deployments [82].
4.9. Technical Report 069 (TR-069)
TR-069 [83], also known as CPE WAN Management Protocol (CWMP), is a protocol designed for the remote management of customer premises equipment (CPE), including IoT devices. It provides a comprehensive framework for device provisioning, diagnostics, and maintenance in IoT networks. The protocol features auto-configuration capabilities, allowing IoT devices to be remotely configured and updated without manual intervention. Its diagnostic features enable administrators to monitor device health and troubleshoot issues efficiently. TR-069’s secure communication framework ensures data integrity and confidentiality during remote management. It uses a hierarchical management model where a centralized Auto-Configuration Server (ACS) communicates with devices to perform operations such as firmware updates, configuration changes, and performance monitoring. The protocol is particularly suitable for large-scale IoT deployments due to its scalable architecture, enabling the efficient management of thousands of connected devices.
TR-069 plays a crucial role in network management by enabling remote device configuration and provisioning, ensuring consistency and scalability across large IoT deployments. With its auto-configuration capabilities, administrators can remotely set up devices without requiring manual intervention, streamlining operations in dynamic network environments. One of its key advantages is support for over-the-air firmware updates, which help maintain device security and functionality by ensuring that all connected devices run the latest software versions. Additionally, TR-069 provides real-time device health monitoring and remote diagnostics, allowing network administrators to quickly identify and troubleshoot issues, minimizing downtime and enhancing overall network efficiency. Its scalable architecture makes it particularly well suited for managing large IoT deployments in geographically distributed networks, ensuring seamless and centralized control over numerous connected devices.
In healthcare, TR-069 is widely used to manage the connectivity and firmware updates of medical devices, ensuring they remain functional and secure. Automated device updates play a crucial role in maintaining compliance with the latest security protocols, safeguarding sensitive patient data and protecting against cyber threats. Furthermore, TR-069 facilitates the real-time monitoring of device health and usage patterns in hospital environments, helping healthcare providers optimize device performance and proactively address potential failures. By ensuring the reliable and efficient management of medical IoT devices, TR-069 contributes to improved patient care and operational efficiency in healthcare networks.
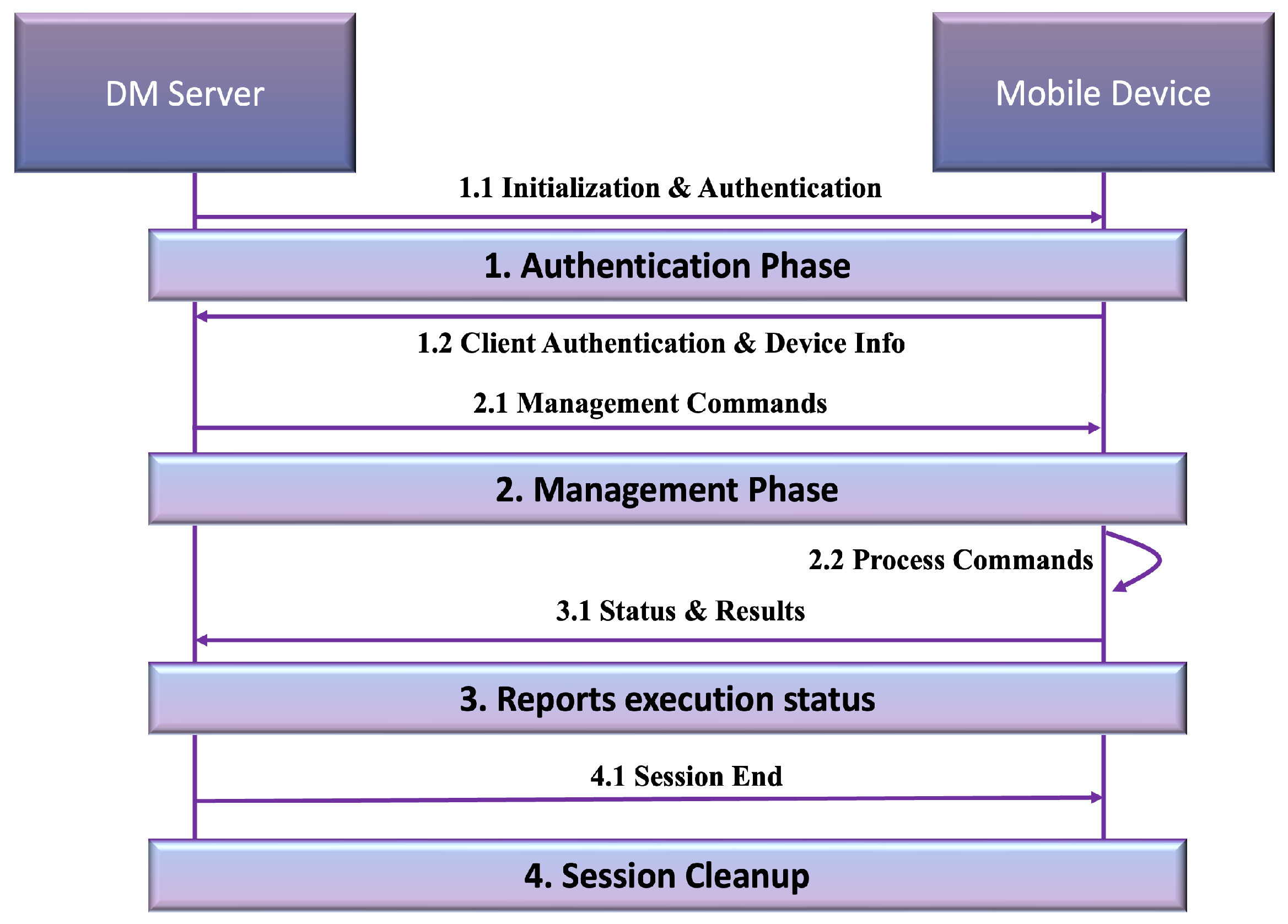
4.10. Open Mobile Alliance Device Management (OMA DM)
OMA DM [84] has evolved from its mobile device management roots to address IoT device management needs. The protocol’s standardized management objects and session-based communication provide a robust framework for remote device administration. OMA DM’s strong security features and extensible framework enable comprehensive device configuration management, software updates, and security policy enforcement in IoT environments. The protocol flow, as shown in Figure 3, begins with mutual authentication between the server and the mobile device, ensuring a secure connection is established. After authentication, the device transmits its capabilities and authentication details to the server, allowing the server to determine the appropriate management operations required for the device. The server then issues management commands, which the device processes and executes. These commands may include updates to network configurations, the implementation of security policy changes, or software and firmware updates. Following the execution of these tasks, the device reports the results back to the server. Finally, the session concludes with the proper cleanup of resources to maintain operational efficiency.
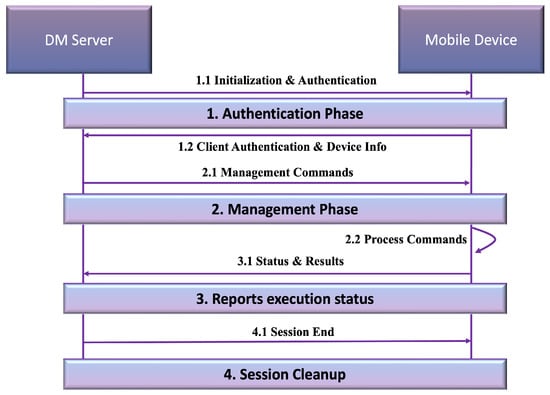
Figure 3.
OMA DM protocol.
OMA DM plays a vital role in IoT network management by enabling centralized remote administration, significantly reducing the need for on-site interventions. Through its efficient device configuration capabilities, the protocol ensures consistent network operations by remotely pushing updates and enforcing security policies. One of its key features is the ability to deliver firmware updates over the air, keeping connected devices secure and ensuring they operate with the latest software. Additionally, OMA DM facilitates task monitoring, where devices report execution results back to the server, allowing network administrators to track performance, identify potential issues, and streamline troubleshooting. This remote management capability enhances operational efficiency while ensuring the security and reliability of IoT networks.
In the healthcare sector, OMA DM is widely used for the remote management of wearable healthcare devices, such as glucose monitors and heart rate sensors, ensuring they function optimally and securely. The protocol also enables the secure configuration and monitoring of critical medical equipment, including infusion pumps and patient monitors, which require continuous oversight to maintain accuracy and reliability. Furthermore, OMA DM supports remote diagnostics for advanced medical equipment, such as MRI machines and ventilators, allowing healthcare providers to detect and resolve potential issues before they impact patient care. By ensuring seamless device management and security enforcement, OMA DM enhances the efficiency and reliability of healthcare IoT networks.
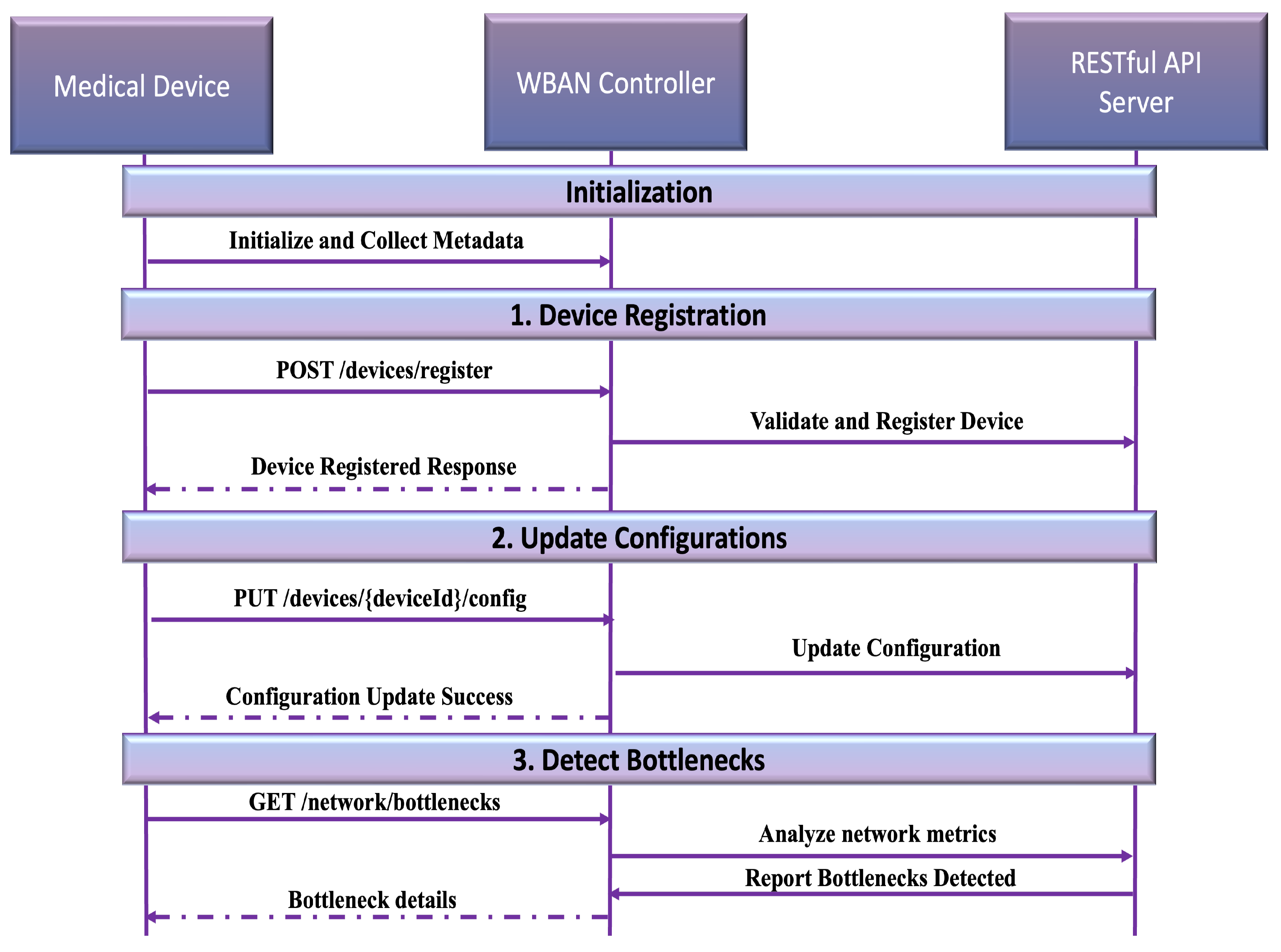
4.11. Representational State Transfer (RESTful)
RESTful (Representational State Transfer) [85] is an architectural style widely adopted for IoT network management and device communication. Built on top of the HTTP protocol, RESTful APIs offer a lightweight, stateless, cacheable, and uniform interface for interacting with IoT devices. The protocol’s resource-oriented design uses standard HTTP methods—GET (retrieve resources), POST (create resources), PUT (update resources), and DELETE (remove resources)—to enable seamless device management, configuration, and monitoring.
Figure 4 illustrates how RESTful APIs enable efficient communication between a medical device and a WBAN (Wireless Body Area Network) controller. Initially, the medical device undergoes initialization, where it gathers its metadata (e.g., ID, type, and network details). The device then registers with the WBAN controller through a POST request, which is validated and forwarded to the API server. Configuration updates, such as network adjustments, are handled via PUT requests, while GET requests retrieve performance metrics for bottleneck detection and troubleshooting. This flow highlights the stateless and resource-oriented nature of RESTful APIs, which are particularly suited for lightweight, scalable IoT environments like healthcare networks. Their simplicity and widespread adoption make RESTful APIs an ideal choice for cloud-based IoT management systems.
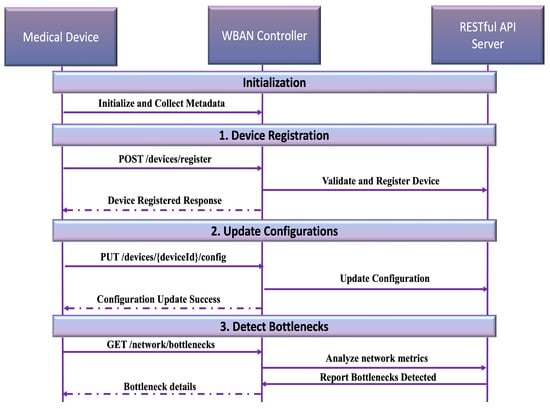
Figure 4.
RESTful protocol.
RESTful APIs have become a fundamental component of modern network management, providing a flexible and efficient approach to device communication. One of their key applications is device monitoring, where GET requests enable real-time retrieval of critical information. Additionally, RESTful APIs support configuration management by allowing administrators to remotely update device settings using PUT or POST requests, ensuring seamless adjustments without manual intervention. They also facilitate data collection, enabling scalable telemetry data retrieval from IoT devices for performance analysis and optimization. Moreover, RESTful APIs enhance cloud integration by simplifying communication between IoT devices and cloud platforms, allowing centralized control and analytics. Their stateless operation ensures lightweight and efficient communication, making them particularly suitable for resource-constrained devices by eliminating the need for maintaining session states. These capabilities contribute to a more scalable, responsive, and efficient approach to managing IoT networks.
They are widely utilized in healthcare network management to enhance performance monitoring, device connectivity, and fault detection. One key application is the ability to monitor healthcare network performance, allowing administrators to identify bottlenecks and troubleshoot issues in real time. By continuously retrieving network metrics and analyzing device data, RESTful APIs help maintain optimal system functionality. Additionally, they play a crucial role in managing the connectivity of medical devices in Wireless Body Area Networks (WBANs) by enabling the registration of new medical devices and updating their network configurations remotely. This ensures seamless integration and reliable communication within healthcare environments. Furthermore, RESTful APIs contribute to fault detection by identifying connectivity failures and triggering automated recovery mechanisms, ensuring continuous operation and minimizing disruptions in healthcare networks.
4.12. OpenFlow in IoT for Healthcare
OpenFlow [86] is a foundational SDN protocol that dynamically updates flow tables in switches, allowing fine-grained traffic management. In healthcare IoT, it ensures optimal routing and prioritization of critical health data traffic, reducing latency and ensuring reliability. The flow table F is defined as
The controller dynamically programs flows:
One of the critical applications of OpenFlow in healthcare IoT networks is prioritizing emergency health data from IoT devices, ensuring that vital patient information, such as alerts from heart rate monitors or emergency notifications, is transmitted with minimal latency. This prioritization helps healthcare providers respond promptly to critical situations. Additionally, OpenFlow plays a crucial role in managing traffic in hospital IoT networks, enabling dynamic resource allocation and optimizing network performance to prevent congestion. By intelligently routing data flows, it ensures efficient communication between connected medical devices, hospital systems, and cloud platforms. Furthermore, OpenFlow facilitates the dynamic control of video streaming for remote patient monitoring, ensuring that bandwidth is allocated efficiently to support high-quality video feeds for telemedicine applications. This capability is essential for continuous patient observation and remote consultations, improving accessibility to healthcare services.
4.13. NetFlow/IPFIX in IoT for Healthcare
NetFlow/IPFIX [87] collects and analyzes traffic flows in healthcare IoT networks. It monitors patterns, detects anomalies, and ensures the uninterrupted flow of critical health data, such as those from wearable devices or connected medical equipment. In NetFlow/IPFIX, the flow record R is
Traffic utilization is calculated as
NetFlow/IPFIX supports key healthcare IoT applications by monitoring data flows from wearable devices, ensuring seamless transmission for real-time health assessments. It enhances cybersecurity by detecting and mitigating abnormal traffic, preventing threats such as unauthorized access and data breaches. Additionally, it ensures uninterrupted data transfer for remote surgery devices, maintaining stable connectivity for latency-sensitive procedures. These capabilities make NetFlow/IPFIX essential for secure, efficient, and reliable healthcare network management. A detailed comparison of different IoT network management protocols is provided in Table 1. Moreover, Table 2 offers a wide-ranging synthesis of heterogeneous IoT devices, core technologies, protocols, and essential requirements, establishing a robust foundation for analyzing and developing cutting-edge solutions across diverse application scenarios.

Table 1.
Comparison of different network management protocols in IoT.

Table 2.
Comparative review of heterogeneous devices, technologies, and specified protocols in IoT topic areas.
5. Reference Architecture for Smart Healthcare System Network Management
In this work, architecture is defined as the structure of components that are involved in the network management practice of smart healthcare systems, the relationships between them, and the policies, requirements, compliance, and standards that govern the operations, administration, maintenance, and provisioning of networked systems. Network management architecture consists of three primary functions: (1) the transport of management information across the system, (2) the management of network elements, networks, services, and business, and (3) the storage of configuration management data. Even though the reference architecture deals with end-to-end network management, the focus of this work is on the segment that constitutes the patient’s context (i.e., the sensors, actuators, gateways, and Internet interfaces). The rest of the network consists of traditional networks and elements managed by existing protocols. The requirements for smart healthcare system network management architecture are outlined in Table 3, detailing the key design considerations necessary for ensuring efficient, secure, and scalable network management in smart healthcare environments [88].

Table 3.
Smart healthcare system network management architecture requirements.
Smart healthcare systems integrate sensing, actuation, and control functions to assess and analyze situations, enabling predictive or adaptive decision-making that leads to intelligent actions. The “smart” nature of these systems is primarily attributed to their autonomous operation, which relies on closed-loop control and networking capabilities.
Managing large-scale smart healthcare systems is a complex task that demands meticulous coordination and systematic oversight. A structured management approach emphasizes the management process itself rather than just the outcomes. To enhance efficiency, we propose a management system reference architecture, which aims to define the key components of smart healthcare system network management, their interrelationships, and their roles. This framework ensures that operational processes remain cost-effective, precise, and well organized while maintaining an optimal inventory.
The architecture must accommodate the diverse restoration requirements of biomedical sensors, as determined by healthcare professionals. The key architectural requirements include the following:
- Provide reactive and proactive fault management.
- Enable objects to cooperate in providing the desired service.
- Provide a reliable end-to-end connection and service.
- Implement high-level asset management.
- Provide scalability to accommodate new patients and services.
- Support patient mobility.
- Enforce security measures at all levels.
- Identify network management protocols.
Figure 5 shows a network management reference architecture for a smart healthcare system. The architecture consists of five layers, and each layer consists of different components. The architecture considers the stakeholders’ requirements and policies. It consolidates existing industry frameworks and standards to maximize systems’ interoperability. The system architecture should also consider requirements from external regulators for compliance.
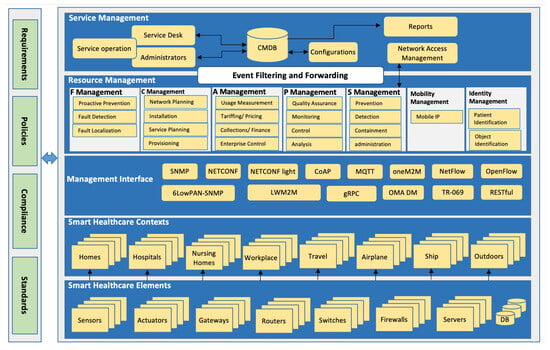
Figure 5.
Smart healthcare system management reference architecture.
5.1. Smart Healthcare Element Layer
Network devices such as wearables, implants, IoT devices, gateways, routers, switches, and backend devices are individual components of the network that run across one or more of the network protocol layers [89]. Network device performance can be evaluated using multiple categories: end-to-end, per-link, per-network, and per-element, each corresponding to a different scope. End-to-end measurements look at the collective behavior across multiple network devices or the entire network path for one or more traffic flows. They may include metrics such as availability, capacity, delay, jitter, throughput, error rates, and utilization. In contrast, per-link, per-network, and per-element assessments concentrate on particular types of hardware or individual segments of the network. Per-link metrics often highlight factors such as propagation delay and link utilization, while per-element metrics (for example, for an IP router) might include IP forwarding rates (like packets per second), buffer usage, and authentication failure logs. Furthermore, these lower-level characteristics can be combined to provide an aggregated end-to-end performance profile.
Wearables, implants, and IoT devices are the main elements of the smart healthcare system as they connect directly to the patient [90]. Once installed, the broker should configure, manage, and keep them operational and updated. The network management system can poll individual components for status updates, and these components can either respond with the requested information or send automatic alerts in the event of abnormal behavior. Monitoring needs depend on the type of physiological data being measured. Some devices, such as spirometers and glucometers, only require attention when a reading is captured (discrete monitoring). Others require continuous data sampling and transmission, as is the case with electrocardiogram (ECG) devices, which constantly track cardiac signals [91].
5.2. Smart Healthcare Context Layer
Smart healthcare contexts are configured using the components in the first layer. The broker configures and maintains the contexts of the patient, for example, home, hospital, or workplace. A smart healthcare network must support patient mobility and switch between different location contexts [59]. Details of this layer are explained in Section 4.
5.3. Management Interface Layer
This layer defines the network management interfaces, usually referred to as the southbound interface, needed to connect the management station with the management agents (i.e., managed devices). In the traditional Internet, several protocols can be used for this purpose, such as SNMP. For the WBAN and IoT segments, there is no specific interface protocol defined for network management. Existing management protocols are not appropriate for resource-constrained WBAN/IoT devices. In the literature, there are several attempts to define these interfaces. Some of these attempts suggested using SNMP to manage sensor nodes [57], while other work suggested using SNMP over traditional IP networks and using other protocols over WBAN/IoT network segments and then linking the two segments through a proxy [56]. Sheng et al. [54] proposed a lightweight RESTful web service approach to enable device management of wireless sensor devices, motivated by the recent development of 6LoWPAN and CoAP protocols for resource-constrained devices. They developed a prototype and demonstrated that the proposed solution was efficient and effective for managing wireless sensor devices. Another work [92] investigated how existing IP-based network management protocols, SNMP and NETCONF, can be implemented on resource-constrained devices. They conducted a resource requirement analysis of SNMP and NETCONF on an 8-bit AVR-based device. They implemented light versions of the SNMP and NETCONF protocols and identified some challenges in message processing, session establishment and maintenance, and security. In their implementation, the authors did not mention how they implemented MIBs and how they could be used in resource-constrained devices.
Other widely used lightweight machine-to-machine IoT protocols are MQTT (Message Queuing Telemetry Transport) [93] and oneM2M [94]. MQTT is a publish/subscribe messaging protocol that is extremely simple and lightweight. It is designed for constrained devices and low-bandwidth, high-latency, or unreliable networks. It can be used in sensor networks and bridged to SNMP-enabled IP networks [95]. The oneM2M protocol is a global initiative to standardize a common M2M service layer platform for globally applicable and access-independent M2M services. The current M2M solutions are proprietary systems, which make them difficult to extend to support new services, integrate new data, and interoperate with other M2M systems [96]. Woo et al. [97] proposed a oneM2M-based IoT system for Personal Healthcare Devices (PHDs). They implemented a protocol to convert between ISO/IEEE 11073 [98] and oneM2M protocol messages. The conversion protocols are deployed in gateways located between the PHD and the management server. Bedside monitoring systems in hospitals use the ISO/IEEE 11073 standards. With minor modifications, the ISO/IEEE 11073 standards can be successfully applied to wearable, wireless, point-of-care systems in home healthcare [99].
5.4. Resource Management Layer
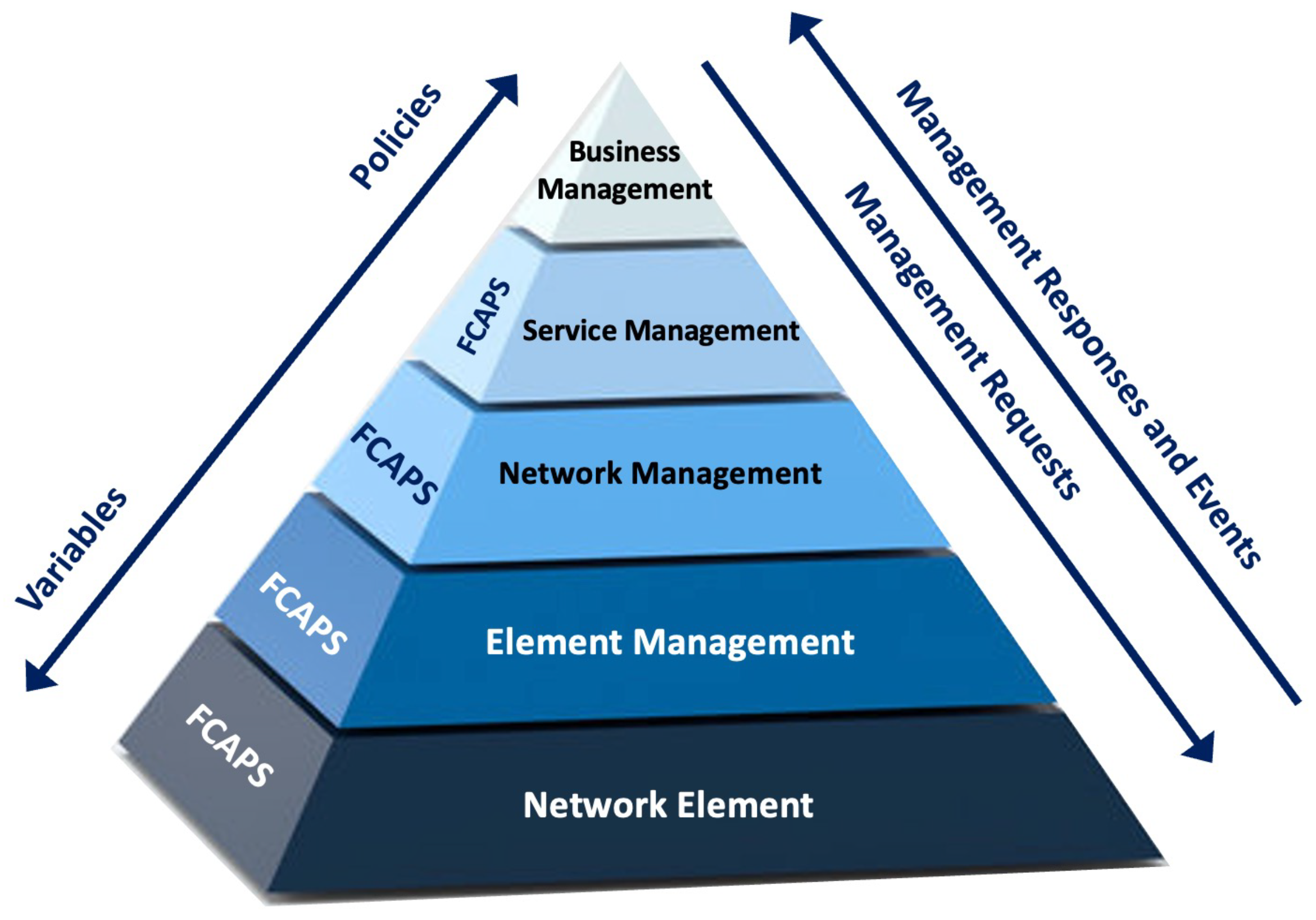
The resource management layer abstracts all smart healthcare elements as reachable resources that can be managed remotely by the network management system. This layer consists of the network management functional areas, including Fault, Configuration, Accounting, Performance, and Security (FCAPS), mobility, and identity management [100]. The structure of this layer aligns with the Telecommunications Management Network (TMN) reference model, which provides a hierarchical framework for managing open systems. As illustrated in Figure 6, the TMN’s layered approach enables efficient resource monitoring and control, ensuring the seamless operation of smart healthcare networks.
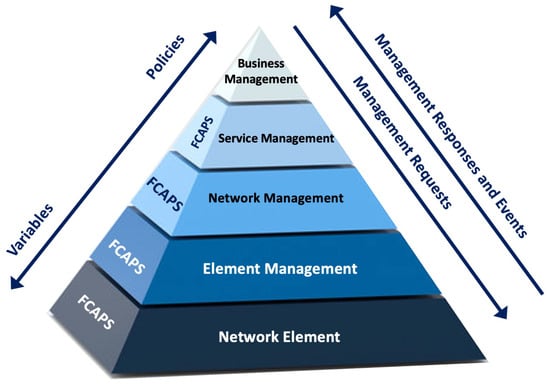
Figure 6.
TMN model for managing open systems.
5.4.1. Fault Management
Fault Management is a set of functions, which enables the detection, localization, isolation, and correction of abnormal operations of the telecommunication network and its environment. Various types of faults can arise in IoT-based healthcare networks, affecting data integrity, system performance, and network reliability. These faults can be categorized into data-centric, system-centric, and network-centric issues, each with distinct causes, durations, and impacts. A detailed classification and analysis of these fault types are provided in Table 4, highlighting their characteristics and potential consequences for system operations [101].

Table 4.
Fault type analysis.
5.4.2. Configuration Management
It encompasses the functions needed to control network elements, identify and gather their data, and provide them with required information. It also facilitates network planning, engineering, installation, service planning and negotiation, provisioning, status checks, and control.
5.4.3. Accounting Management
This measures how network services are used and determines the associated costs for providers, as well as charges for customers. It also assists in calculating appropriate pricing for these services.
5.4.4. Performance Management
It evaluates and reports on the behavior of telecommunications devices and the overall network, measuring their effectiveness. It additionally gathers and examines statistical data to both monitor and optimize the performance of the network and its individual components.
5.4.5. Security Management
It enables the management of security, which is required for all management functional areas and TMN transactions.
5.4.6. Mobility Management
It provides the necessary functions that allow the patient to switch between different contexts on different IP networks.
5.4.7. Identity Management
It provides the necessary functions to identify patients and objects and the relationship between them.
5.5. Service Management Layer
The uppermost layer in the architecture is the service management layer. This layer manages the end-to-end services provided to end-users. It receives filtered events from the resource management layer. Within this layer lies the architecture repository, the Configuration Management Database (CMDB), that saves all inventory, configurations, and filtered events related to all devices. Service delivery and management represent the organizational strategic objectives that require effective and efficient support. Therefore, the services should be planned in a systematic and standard way to guarantee service continuity and interoperability. In this architecture, we recommend using the ITILv3 framework. ITILv3 best practices define five core processes, namely, service strategy, service design, service transition, service operation, and continual service improvement. Service operation management further defines five service operation processes, namely, incident management, problem management, event management, service request fulfillment, and access management. The ITILv3 framework can be adapted for smart healthcare systems’ service management by incorporating smart healthcare’s technical and medical requirements. Defining a service management layer requires comprehensive strategy development and implementation. ITILv3 defines a priority framework to prioritize incidents based on impact and urgency. It also defines the IT support roles and levels that handle different incident complexities and time constraints.
6. Architecture Implementation Plan
This section discusses the implementation approach of the management entities that are under the administrative domain of a third party accountable for managing the smart healthcare system.
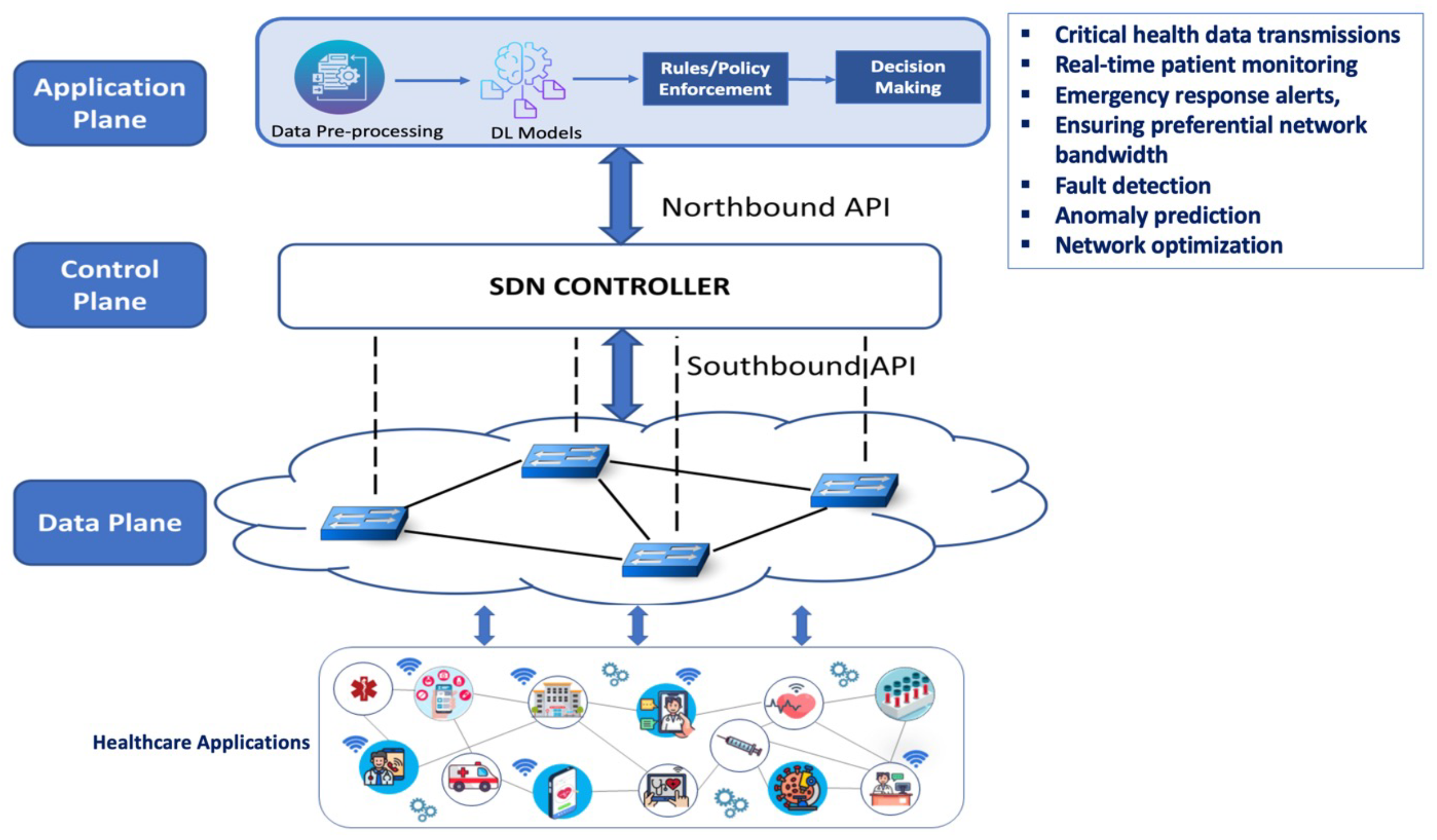
6.1. Supporting the Architecture with Software-Defined Networking and Deep Learning
Providing reliable, timely, secure, cost-effective, and pervasive smart healthcare is an essential requirement of the healthcare industry nowadays. These requirements are driven by the increasing number of patients with chronic diseases, the increasing average life expectancy, and associated healthcare spending. Considerable research is being conducted to tackle these issues and provide practical solutions based on the current Internet architecture and the deployed technologies. However, common challenges related to network and device heterogeneity, complexity, and the lack of full control of the underlying network infrastructure hinder the achievement of desirable end-to-end healthcare-specific requirements. In addition, the massive amount of data generated from the various sensors will make it extremely difficult to use traditional management techniques and tools for fault management, performance analysis, traffic management, and real-time response to any possible malfunction of the software or hardware components. Therefore, we mention two promising technologies that will add value to the architecture and help address the above challenges, namely, software-defined networking (SDN) and deep learning. SDN is an emerging networking paradigm that helps in facilitating network configuration and management [102]. Unlike traditional network configurations used in the current Internet architecture, where network devices implement a control plane and a data-forwarding plane, SDN has two distinct features: SDN separates the control plane from the data plane while enabling programmatic control for network application development. Through this design, SDN aims to achieve more efficient configuration, enhanced performance, and flexible adaptation to emerging network innovations [103].
Four main principles define this SDN architecture:
- Flow-based forwarding rather than traditional destination-based forwarding.
- Externalized control logic, handled by an SDN controller located outside the forwarding devices.
- Programmable network elements, managed by software applications running on the controller.
- Decoupled control and data planes, allowing independent yet coordinated operation.
SDN plays a crucial role in predictively allocating network resources and preventing performance bottlenecks in healthcare applications. The SDN controller dynamically prioritizes critical health data transmissions, such as real-time patient monitoring and emergency response alerts, ensuring preferential network bandwidth for life-saving applications over non-urgent traffic. This proactive approach improves network reliability, reduces congestion, and enhances the overall efficiency of healthcare services [103].
Deep learning (DL) has emerged recently as a powerful tool for machine learning capable of solving complex optimization and predictive analytics problems. It is contributing to solving significant problems that previous attempts by the artificial intelligence community failed to solve for many years. It enables multi-layered computational models to learn abstract representations of healthcare data, providing enhanced fault detection, anomaly prediction, and network optimization. Artificial intelligence techniques have already been explored for fault management in computer networks, where neural networks have been applied for alarm filtering and correlation [104]. DL is also widely used in healthcare analytics and bioinformatics [48,49], demonstrating its potential in predictive network management. DL-based predictive models continuously analyze network performance metrics to anticipate failures, allowing for preemptive intervention. We also envisage the use of deep learning by SDN controller applications. For example, deep learning-based applications can be used to control the switching, intelligent routing, and firewalling behavior of the overall healthcare infrastructure. A DL-enabled SDN architecture for healthcare is presented in Figure 7. Beyond SDN, Network Function Virtualization (NFV) and Management and Orchestration (MANO) play critical roles in modernizing healthcare network infrastructures. NFV virtualizes network functions, decoupling them from dedicated hardware and running them as software instances, thereby reducing dependency on specialized networking equipment, improving scalability, and lowering operational costs [48]. This shift is particularly beneficial in smart healthcare systems, where the rapid deployment and adaptation of network services are essential for real-time patient monitoring and emergency response scenarios.
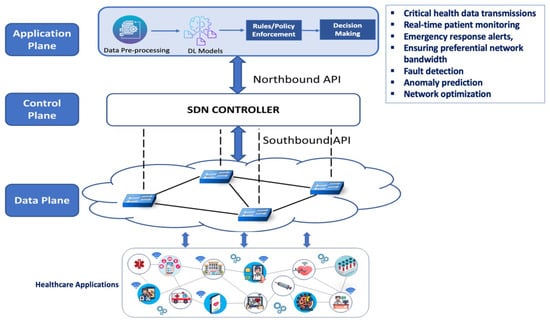
Figure 7.
Smart health system architecture implementation plan supported by software-defined networking and deep learning.
The MANO framework further enhances NFV by automating the deployment, configuration, and lifecycle management of virtualized network functions (VNFs). This automation reduces manual intervention, minimizes errors, and ensures efficient resource allocation, leading to higher flexibility and reliability in healthcare networks. Moreover, chaining VNFs through MANO enables dynamic service adaptation, allowing healthcare applications to seamlessly scale based on demand, thus enhancing quality of service (QoS) and patient care outcomes [49].
6.2. Low-Power Low-Range Wireless Networks
WBAN elements are best configured with IEEE 802.15.6, while other IoT devices can be configured with IEEE 801.15.4. IEEE 801.15.4 provides a more extended range compared with IEEE 802.15.6. Implanted sensors can only be configured as relayed devices that should not relay any packets from other sensors [12]. Wearable sensors might be configured as relayed or relaying devices. The PDA (or hub, as defined by IEEE 802.15.6) should be positioned in a place that supports star topology.
Given the anticipated large number of monitored and managed smart healthcare users, the Personal Digital Assistant (PDA) is optimally configured as a software-defined networking (SDN) device, which is programmed by an SDN controller hosted by a third-party provider. Traffic flows within smart healthcare systems can be categorized into three main types: physiological data, environmental data, and sensor health data.
Physiological or vital sign data can be further divided into periodic physiological data and emergency physiological data [105]. Environmental data, on the other hand, may be collected from indoor or outdoor settings. The PDA is responsible for classifying and directing the traffic flows generated by various sensors to their designated destinations. Figure 8 illustrates the traffic flow from sensors to the PDA and onward to the respective end systems.
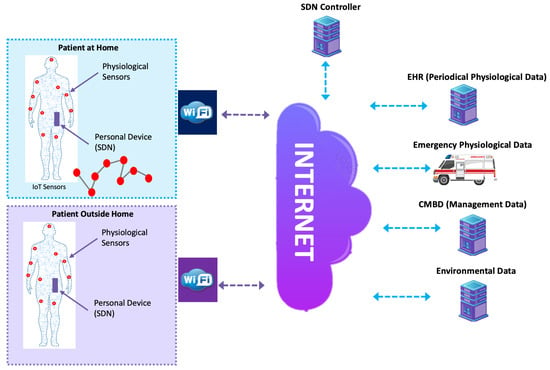
Figure 8.
SDN-based traffic classification and management.
6.3. Smart Healthcare Context Management
SDN may also provide substantial help in configuring smart healthcare contexts and switching between contexts by exploiting the capability of running software applications on top of the controller [106]. All elements of the context can be configured and managed directly or indirectly by the controller as long as they are under the administrative authority of the managing entity. The configuration and management of the context elements can be realized by providing a management plane over the control plane. Context management may also include mobility and handover between different network architectures as well as the same network architecture. Mobility is best handled by a mobile IP in the case of all-IP networks.
6.4. Smart Healthcare Service Management
Service management is the focus of the management system to ensure service continuity. Due to the sensitivity of the smart healthcare system, healthcare services should be provisioned without anomalies. Service malfunctions can happen because of hardware or software faults, which cause network elements to produce incorrect outputs. When the smart healthcare system is deployed on a massive scale, it becomes hard to monitor and manage such services, especially with the reception of a considerable number of alarms and sensor-related management data. To provide efficient alarm filtering and real-time decisions, we propose using deep learning techniques for this purpose. To further elaborate on the use of deep learning in fault management, the workflow of the fault management process is outlined as follows:
- Collect monitoring and performance alarms.
- Provide feedback to users to ensure service continuity.
- Filter, eliminate, and correlate the alarms.
- Diagnose faults through analysis and testing to eliminate the cause of the fault.
- Determine a plan for correction, display correction options to patients, and implement the plan.
- Verify the fault is eliminated.
- Record data and determine the effectiveness of the current fault management process.
Deep learning can help in filtering, classifying, and correlating alarms and recognizing basic fault patterns. However, to identify the exact fault location, a further process is necessary. This procedure involves human intervention to make some decisions that might be deemed impossible by deep learning alone. Some work suggests using case-based reasoning to analyze the data further and run tests to identify the exact location of the fault [104]. However, one recent work suggests an architecture for deep learning that explains its reasoning process and learns by observation [107].
7. Advanced Futuristic Network Management Protocols
As networks continue to evolve into self-healing, AI-driven, and hyper-connected ecosystems, traditional network management protocols struggle to meet the demands of real-time automation, security, and predictive analytics. Future networks will be defined by protocols that leverage AI, quantum cryptography, blockchain, and intent-based networking to enable seamless, autonomous operations. These next-generation protocols will be designed to support critical infrastructures such as 6G, healthcare cyber–physical systems [108], smart cities, and autonomous vehicles, ensuring ultra-reliable and intelligent network management. One of the most promising advancements in network management is Intent-Based Networking Protocols (IBNPs). Unlike traditional protocols that require manual configurations, IBNPs allow network administrators to define high-level business objectives, and the network autonomously configures itself to meet these goals. These protocols will rely on AI-driven automation, machine learning, federated learning [109,110], and real-time data analytics to dynamically optimize traffic, predict failures, and enforce security policies. Future versions of IBNPs will also incorporate blockchain for decentralized trust and zero-trust architectures to enhance cybersecurity in highly distributed environments.
Another significant innovation is Predictive Telemetry Protocols (PTPs), which will replace conventional polling-based network monitoring systems with AI-powered proactive anomaly detection. Instead of relying on reactive alerts, PTPs will analyze vast amounts of real-time network data using deep learning models to predict failures before they happen. These protocols will enable self-healing networks by autonomously rerouting traffic, reconfiguring devices, and mitigating security threats before they impact operations. This will be particularly crucial for critical applications such as autonomous transportation, smart factories, and real-time healthcare monitoring. With the rise of quantum computing, current encryption mechanisms will become obsolete, necessitating Quantum-Secure Network Management Protocols [111,112]. These protocols will integrate post-quantum cryptographic algorithms and quantum key distribution (QKD) to protect sensitive network communications. Future networks, especially in financial institutions, government infrastructures, and military communications, will require these quantum-resistant protocols to prevent potential cyber threats posed by quantum decryption capabilities.
In addition, Bio-Inspired Autonomous Network Protocols (BANPs) will revolutionize network resilience by mimicking biological self-organizing systems [113]. Inspired by swarm intelligence and neural networks, BANPs will enable self-adaptive, decentralized, and fault-tolerant network management. These protocols will be vital for managing massive IoT ecosystems, where devices must seamlessly communicate, self-optimize, and self-heal in unpredictable environments. The future of network management will be AI-driven, quantum-secure, predictive, and intent-based, ensuring autonomous, self-optimizing, and ultra-resilient network infrastructures that can support the demands of next-generation technologies.
8. Conclusions
This paper provides a comprehensive review of smart network management protocols for Internet of Things (IoT)-based healthcare systems, addressing critical challenges in ensuring seamless connectivity, secure data exchange, and efficient device management. A reference architecture is proposed to enhance network reliability and service continuity by integrating standards and frameworks into a comprehensive management system that mitigates health risks through robust strategies while proactively predicting and preventing healthcare faults via the collection of data from multiple protocols, which are then forwarded to a central entity for machine learning-based analysis. Additionally, this study explores the integration of advanced technologies, including software-defined networking (SDN) and deep learning (DL), to optimize network performance. Furthermore, it highlights emerging paradigms shaping next-generation network management solutions for future smart healthcare ecosystems.
Author Contributions
Conceptualization, F.M.S.; methodology, F.M.S., A.T. and H.M.K.; writing, F.M.S., A.T. and H.M.K.; review, M.H., K.S., F.M.S., A.T. and E.S.B.; editing, F.M.S., H.M.K. and A.T.; visualization, F.M.S., H.M.K. and A.T.; supervision, F.M.S.; project administration, M.H. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Informed Consent Statement
Not applicable.
Data Availability Statement
No data were used or produced in this study.
Acknowledgments
This work was supported by UAEU.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Chen, Y.; Zhong, W.; Da, H.; Ruosen, L. 6G is coming: Discussion on key candidate technologies and application scenarios. In Proceedings of the 2020 International Conference on Computer Communication and Network Security (CCNS), Xi’an, China, 21–23 August 2020; IEEE: Piscataway, NJ, USA, 2020; pp. 59–62. [Google Scholar]
- Pereira, F.; Correia, R.; Pinho, P.; Lopes, S.I.; Carvalho, N.B. Challenges in resource-constrained IoT devices: Energy and communication as critical success factors for future IoT deployment. Sensors 2020, 20, 6420. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Liu, Z.; Tang, K.; Yin, X.; Zhuo, C.; Wei, Q.; Qiao, F. Breaking the energy-efficiency barriers for smart sensing applications with “Sensing with Computing” architectures. Sci. China Inf. Sci. 2023, 66, 200409. [Google Scholar] [CrossRef]
- Lin, J.; Yu, W.; Zhang, N.; Yang, X.; Zhang, H.; Zhao, W. A survey on internet of things: Architecture, enabling technologies, security and privacy, and applications. IEEE Internet Things J. 2017, 4, 1125–1142. [Google Scholar] [CrossRef]
- Tariq, M.U. Advanced wearable medical devices and their role in transformative remote health monitoring. In Transformative Approaches to Patient Literacy and Healthcare Innovation; IGI Global: Hershey, PA, USA, 2024; pp. 308–326. [Google Scholar]
- Chui, M.; Collins, M.; Patel, M. The Internet of Things: Catching Up to an Accelerating Opportunity; McKinsey & Company: New York, NY, USA, 2021. [Google Scholar]
- Wehde, M. Healthcare 4.0. IEEE Eng. Manag. Rev. 2019, 47, 24–28. [Google Scholar] [CrossRef]
- Khater, H.M.; Sallabi, F.; Serhani, M.A.; Turaev, S.; Barka, E. Efficient hybrid fault-management clustering algorithm (hfmca) in wbans based on weighted bipartite graph. IEEE Access 2023, 11, 57977–57990. [Google Scholar] [CrossRef]
- Saha, E.; Rathore, P. The impact of healthcare 4.0 technologies on healthcare supply chain performance: Extending the organizational information processing theory. Technol. Forecast. Soc. Change 2024, 201, 123256. [Google Scholar] [CrossRef]
- Sallabi, F.; Shuaib, K. Internet of Things Network Management System Architecture for Smart Healthcare. In Proceedings of the 2016 Sixth International Conference on Digital Information and Communication Technology and its Applications (DICTAP), Konya, Turkey, 21–23 July 2016; pp. 165–170. [Google Scholar]
- IEEE. IEEE Std 802.15.4-2020; IEEE Standard for Low-Rate Wireless Networks. IEEE: New York, NY, USA, 2020; pp. 1–800.
- IEEE. IEEE Std 802.15.6-2012; IEEE Standard for Local and Metropolitan Area Networks—Part 15.6: Wireless Body Area Networks. IEEE: New York, NY, USA, 2012.
- Detwal, P.K.; Agrawal, R.; Samadhiya, A.; Kumar, A.; Garza-Reyes, J.A. Revolutionizing healthcare organizations with Operational Excellence and Healthcare 4.0: A systematic review of the state-of-the-art literature. Int. J. Lean Six Sigma 2024, 15, 80–102. [Google Scholar] [CrossRef]
- Gopich, G.; Sarath, T.; Dumka, A.; Goyal, H.R.; Singh, R.; Gehlot, A.; Gupta, L.R.; Thakur, A.K.; Priyadarshi, N.; Twala, B. Use of IoT sensor devices for efficient management of healthcare systems: A review. Discov. Internet Things 2024, 4, 8. [Google Scholar] [CrossRef]
- Whitmore, A.; Agarwal, A.; Da Xu, L. The Internet of Things A survey of topics and trends. Inf. Syst. Front. 2015, 17, 261–274. [Google Scholar] [CrossRef]
- Razzaque, M.A.; Milojevic-Jevric, M.; Palade, A.; Cla, S. Middleware for internet of things: A survey. IEEE Internet Things J. 2016, 3, 70–95. [Google Scholar] [CrossRef]
- Botta, A.; De Donato, W.; Persico, V.; Pescapé, A. Integration of Cloud computing and Internet of Things: A survey. Future Gener. Comput. Syst. 2016, 56, 684–700. [Google Scholar] [CrossRef]
- Ghaleb, S.M.; Subramaniam, S.; Zukarnain, Z.A.; Muhammed, A. Mobility management for IoT: A survey. EURASIP J. Wirel. Commun. Netw. 2016, 2016, 165. [Google Scholar] [CrossRef]
- Shibata, Y.; Sato, G. IoT based mobility information infrastructure in challenged network environment toward aging society. In Proceedings of the 31st IEEE International Conference on Advanced Information Networking and Applications Workshops, WAINA 2017, Taipei, Taiwan, 27–29 March 2017; pp. 645–648. [Google Scholar]
- Ulrich. T. 5G: An Introduction to the 5th Generation Mobile Networks; Walter de Gruyter GmbH & Co KG: Berlin, Germany, 2021. [Google Scholar]
- Li, S.; Zhao, S.; Zhao, S. 5G Internet of Things: A Survey. J. Ind. Inf. Integr. 2018, 10, 1–9. [Google Scholar] [CrossRef]
- Stankovic, J.A. Research Directions for the Internet of Things. IEEE Internet Things J. 2014, 1, 3–9. [Google Scholar] [CrossRef]
- Zimmermann, A.; Schmidt, R.; Sandkuhl, K.; Wißotzki, M.; Jugel, D.; Möhring, M. Digital enterprise architecture-transformation for the internet of things. In Proceedings of the 2015 IEEE 19th International Enterprise Distributed Object Computing Workshop EDOCW 2015, Adelaide, SA, Australia, 21–25 September 2015; pp. 130–138. [Google Scholar]
- Al-Fuqaha, A.; Khreishah, A.; Guizani, M.; Rayes, A.; Mohammadi, M. Toward better horizontal integration among IoT services. IEEE Commun. Mag. 2015, 53, 72–79. [Google Scholar] [CrossRef]
- Aswale, P.; Shukla, A.; Bharati, P.; Bharambe, S.; Palve, S. An Overview of Internet of Things: Architecture, Protocols and Challenges. In Information and Communication Technology for Intelligent Systems; Springer: Singapore, 2019; pp. 299–308. [Google Scholar]
- Gigli, M. Internet of Things: Services and Applications Categorization. Adv. Internet Things 2011, 1, 27–31. [Google Scholar] [CrossRef]
- Cook, D.J.; Crandall, A.S.; Thomas, B.L.; Krishnan, N.C. CASAS: A Smart Home in a Box. Computer 2013, 46, 62–69. [Google Scholar] [CrossRef]
- Li, X.; Lu, R.; Liang, X.; Shen, X.; Chen, J.; Lin, X. Smart community: An internet of things application. IEEE Commun. Mag. 2011, 49, 68–75. [Google Scholar] [CrossRef]
- Zanella, A.; Bui, N.; Castellani, A.; Vangelista, L.; Zorzi, M. Internet of things for smart cities. IEEE Internet Things J. 2014, 1, 22–32. [Google Scholar] [CrossRef]
- Dohr, A.; Modre-Opsrian, R.; Drobics, M.; Hayn, D.; Schreier, G. The Internet of Things for Ambient Assisted Living. In Proceedings of the 2010 Seventh International Conference on Information Technology: New Generations, Las Vegas, NV, USA, 12–14 April 2010; pp. 804–809. [Google Scholar]
- Marques, G. Ambient Assisted Living and Internet of Things. In Harnessing the Internet of Everything (IoE) for Accelerated Innovation Opportunities; IGI Global: Hershey, PA, USA, 2019; pp. 100–115. [Google Scholar]
- Bui, N.; Zorzi, M. Health care applications: A solution based on the internet of things. In Proceedings of the 4th International Symposium on Applied Sciences in Biomedical and Communication Technologies, Barcelona, Spain, 26–29 October 2011; pp. 1–5. [Google Scholar]
- Jara, A.J.; Zamora, M.A.; Skarmeta, A.F.G. An Internet of things-based personal device for diabetes therapy management in ambient assisted living (AAL). Pers. Ubiquitous Comput. 2011, 15, 431–440. [Google Scholar] [CrossRef]
- Jara, A.J.; Zamora-Izquierdo, M.A.; Skarmeta, A.F. Interconnection Framework for mHealth and Remote Monitoring Based on the Internet of Things. IEEE J. Sel. Areas Commun. 2013, 31, 47–65. [Google Scholar] [CrossRef]
- Jung, Y. Hybrid-aware model for senior wellness service in smart home. Sensors 2017, 17, 1182. [Google Scholar] [CrossRef] [PubMed]
- Bennett, J.; Rokas, O.; Chen, L. Healthcare in the Smart Home: A Study of Past, Present and Future. Sustainability 2017, 9, 840. [Google Scholar] [CrossRef]
- Liao, Z.; Kong, L.; Wang, X.; Zhao, Y.; Zhou, F.; Liao, Z.; Fan, X. A Visual Analytics Approach for Detecting and Understanding Anomalous Resident Behaviors in Smart Healthcare. Appl. Sci. 2017, 7, 254. [Google Scholar] [CrossRef]
- Solanas, A.; Patsakis, C.; Conti, M.; Vlachos, I.S.; Ramos, V.; Falcone, F.; Postolache, O.; Pérez-Martínez, P.A.; Di Pietro, R.; Perrea, D.N.; et al. Smart health: A context-aware health paradigm within smart cities. IEEE Commun. Mag. 2014, 52, 74–81. [Google Scholar] [CrossRef]
- Ghose, A.; Bhaumik, C.; Das, D.; Agrawal, A.K. Mobile healthcare infrastructure for home and small clinic. In Proceedings of the 2nd ACM international Workshop on Pervasive Wireless Healthcare—MobileHealth ’12, Hilton Head, SC, USA, 11–14 June 2012; p. 15. [Google Scholar]
- Santos, J.; Rodrigues, J.J.P.C.; Silva, B.M.C.; Casal, J.; Saleem, K.; Denisov, V. An IoT-based mobile gateway for intelligent personal assistants on mobile health environments. J. Netw. Comput. Appl. 2016, 71, 194–204. [Google Scholar] [CrossRef]
- Pereira, C.; Pinto, A.; Ferreira, D.; Aguiar, A. Experimental Characterization of Mobile IoT Application Latency. IEEE Internet Things J. 2017, 4, 1082–1094. [Google Scholar] [CrossRef]
- Khattak, H.A.; Ruta, M.; Eugenio, E.; Sciascio, D. CoAP-based healthcare sensor networks: A survey. In Proceedings of the 2014 11th International Bhurban Conference on Applied Sciences & Technology (IBCAST), 2014, Islamabad, Pakistan, 14–18 January 2014; pp. 499–503. [Google Scholar]
- Rahmani, A.-M.; Thanigaivelan, N.K.; Gia, T.N.; Granados, J.; Negash, B.; Liljeberg, P.; Tenhunen, H. Smart e-Health Gateway: Bringing intelligence to Internet-of-Things based ubiquitous healthcare systems. In Proceedings of the 2015 12th Annual IEEE Consumer Communications and Networking Conference CCNC 2015, Las Vegas, NV, USA, 9–12 January 2015; pp. 826–834. [Google Scholar]
- Islam, S.M.R.; Kwak, D.; Kabir, H.; Hossain, M.; Kwak, K.-S. The Internet of Things for Health Care: A Comprehensive Survey. IEEE Access 2015, 3, 678–708. [Google Scholar] [CrossRef]
- Farahani, B.; Firouzi, F.; Chang, V.; Badaroglu, M.; Constant, N.; Mankodiya, K. Towards fog-driven IoT eHealth: Promises and challenges of IoT in medicine and healthcare. Future Gener. Comput. Syst. 2018, 78, 659–676. [Google Scholar] [CrossRef]
- Pagán, J.; Zapater, M.; Ayala, J.L. Power transmission and workload balancing policies in eHealth mobile cloud computing scenarios. Future Gener. Comput. Syst. 2018, 78, 587–601. [Google Scholar] [CrossRef]
- Adame, T.; Bel, A.; Carreras, A.; Melià-Seguí, J.; Oliver, M.; Pous, R. CUIDATS: An RFID–WSN hybrid monitoring system for smart health care environments. Future Gener. Comput. Syst. 2018, 78, 602–615. [Google Scholar] [CrossRef]
- Miotto, R.; Wang, F.; Wang, S.; Jiang, X.; Dudley, J.T. Deep learning for healthcare: Review, opportunities and challenges. Briefings Bioinform. 2017, 19, 1236–1246. [Google Scholar] [CrossRef] [PubMed]
- Ravì, D.; Wong, C.; Deligianni, F.; Berthelot, M.; Andreu-Perez, J.; Lo, B.; Yang, G.Z. Deep Learning for Health Informatics. IEEE J. Biomed. Health Inform. 2017, 21, 4–21. [Google Scholar] [CrossRef] [PubMed]
- Cavallari, R.; Martelli, F.; Rosini, R.; Buratti, C.; Verdone, R. A Survey on Wireless Body Area Networks: Technologies and Design Challenges. IEEE Commun. Surv. Tutor. 2014, 16, 1635–1657. [Google Scholar] [CrossRef]
- Movassaghi, S.; Member, S.; Abolhasan, M.; Member, S. Wireless Body Area Networks: A Survey. IEEE Commun. Surv. Tutor. 2013, 16, 1658–1686. [Google Scholar] [CrossRef]
- Ghamari, M.; Janko, B.; Sherratt, R.S.; Harwin, W.; Piechockic, R.; Soltanpur, C. A survey on wireless body area networks for ehealthcare systems in residential environments. Sensors 2016, 16, 831. [Google Scholar] [CrossRef]
- Sinche, S.; Silva, J.S.; Raposo, D.; Rodrigues, A.; Pereira, V.; Boavida, F. Towards Effective IoT Management. In Proceedings of the 2018 IEEE SENSORS, New Delhi, India, 28–31 October 2018; pp. 18–21. [Google Scholar]
- Sheng, Z.; Wang, H.; Yin, C.; Hu, X.; Yang, S.; Leung, V. Lightweight Management of Resource Constrained Sensor Devices in Internet-of-Things. IEEE Internet Things J. 2015, 2, 402–411. [Google Scholar] [CrossRef]
- Li, X.; Ji, H.; Li, Y. Layered fault management scheme for end-to-end transmission in internet of things. Mob. Netw. Appl. 2013, 18, 195–205. [Google Scholar] [CrossRef]
- Lindholm-Ventola, H.; Bilhanan, S. CoAP-SNMP Interworking IoT Scenarios; Report No. 3; Department of Pervasive Computing, Tampere University of Technology: Tampere, Finland, 2014. [Google Scholar]
- Huang, H.-P.; Xiao, S.-D.; Meng, X.-Y. Applying SNMP Technology to Manage the Sensors in Internet of Things. Open Cybern. Syst. J. 2015, 15, 1019–1024. [Google Scholar]
- Zhou, S.; Lin, K.J.; Na, J.; Chuang, C.C.; Shih, C.S. Supporting Service Adaptation in Fault Tolerant Internet of Things. In Proceedings of the 2015 IEEE 8th International Conference on Service-Oriented Computing and Applications (SOCA), Rome, Italy, 19–21 October 2015; pp. 65–72. [Google Scholar]
- Hassanalieragh, M.; Page, A.; Soyata, T.; Sharma, G.; Aktas, M.; Mateos, G.; Kantarci, B.; Andreescu, S. Health Monitoring and Management Using Internet-of-Things (IoT) Sensing with Cloud-Based Processing: Opportunities and Challenges. In Proceedings of the 2015 IEEE International Conference on Services Computing SCC, New York, NY, USA, 27 June–2 July 2015; pp. 285–292. [Google Scholar]
- Gia, T.N.; Rahmani, A.-M.; Westerlund, T.; Liljeberg, P.; Tenhunen, H. Fault tolerant and scalable IoT-based architecture for health monitoring. In Proceedings of the 2015 IEEE Sensors Applications Symposium (SAS), Zadar, Croatia, 13–15 April 2015; pp. 1–6. [Google Scholar]
- Salahuddin, M.A.M.A.; Al-Fuqaha, A.; Guizani, M.; Shuaib, K.; Sallabi, F. Softwarization of internet of things infrastructure for secure and smart healthcare. Computer 2017, 50, 74–79. [Google Scholar] [CrossRef]
- Gharaibeh, A.; Salahuddin, M.A.; Hussini, S.J.; Khreishah, A.; Khalil, I.; Guizani, M.; Al-Fuqaha, A. Smart Cities: A Survey on Data Management, Security and Enabling Technologies. IEEE Commun. Surv. Tutor. 2017, 19, 2456–2501. [Google Scholar] [CrossRef]
- Tariq, A.; Lakas, A.; Sallabi, F.; Qayyum, T.; Serhani, M.A.; Barka, E. Empowering Trustworthy Client Selection in Edge Federated Learning Leveraging Reinforcement Learning. In Proceedings of the Eighth ACM/IEEE Symposium on Edge Computing, Wilmington, DE, USA, 7–9 December 2023; pp. 372–377. [Google Scholar]
- Lightweight M2M (LWM2M)—OMA SpecWorks. [Online]. Available online: https://www.omaspecworks.org/what-is-oma-specworks/iot/lightweight-m2m-lwm2m/ (accessed on 20 October 2018).
- Kombate, Y.; Houngue, P.; Ouya, S. Securing MQTT: Unveiling Vulnerabilities and Innovating Cyber Range Solutions. Procedia Comput. Sci. 2024, 241, 69–76. [Google Scholar] [CrossRef]
- Weqar, M.; Mehfuz, S.; Gupta, D.; Urooj, S. Adaptive Switching-Based Data-Communication Model for Internet of Healthcare Things Networks. IEEE Access 2024, 12, 11530–11540. [Google Scholar] [CrossRef]
- Qin, W. Construction of Computer Network Management System Based on NETCONF and Artificial Intelligence. In Proceedings of the 2024 International Conference on Intelligent Algorithms for Computational Intelligence Systems (IACIS), Hassan, India, 23–24 August 2024; pp. 1–8. [Google Scholar] [CrossRef]
- Alkwiefi, M.; Khalifeh, A. M2M Protocols: An Overview on LwM2M and XMPP Machine-to-Machine Protocols in IoT Context. In Proceedings of the IEEE International Conference on Computer and Information Science (ICIS), Shanghai, China, 20–22 September 2024; Volume 24, pp. 209–216. [Google Scholar] [CrossRef]
- Varshney, U. Pervasive healthcare and wireless health monitoring. Mob. Netw. Appl. 2007, 12, 113–127. [Google Scholar] [CrossRef]
- Navarro, K.F.; Lawrence, E. WSN applications in personal healthcare monitoring systems: A heterogeneous framework. In Proceedings of the 2010 Second International Conference on eHealth, Telemedicine, and Social Medicine BUSMMed 2010, Saint Maarten, Netherlands Antilles, 10–16 February 2010; pp. 77–83. [Google Scholar]
- Mota, L.D.C.; Moreno, E.D.; Ribeiro, A.L.; Salgueiro, R.J.P.D.B. A Comparative Analysis of Network Management Protocols in IoT Applications. J. Comput. Sci. 2018, 14, 1238–1246. [Google Scholar] [CrossRef]
- Alshammari, H.H. The internet of things healthcare monitoring system based on MQTT protocol. Alex. Eng. J. 2023, 69, 275–287. [Google Scholar] [CrossRef]
- Soni, D.; Makwana, A. A survey on mqtt: A protocol of internet of things (iot). In Proceedings of the International Conference on Telecommunication, Power Analysis and Computing Techniques (ICTPACT-2017), Chennai, India, 6–8 April 2017; Volume 20, pp. 173–177. [Google Scholar]
- Enns, R.; Bjorklund, M.; Schoenwaelder, J.; Bierman, A. RFC 6241; Network Configuration Protocol (NETCONF). Internet Engineering Task Force: Fremont, CA, USA, 2011. [CrossRef]
- Silverajan, B.; Luoma, J.P.; Vajaranta, M.; Itäpuro, R. Collaborative cloud-based management of home networks. In Proceedings of the 2015 IFIP/IEEE International Symposium on Integrated Network Management (IM), Ottawa, ON, Canada, 11–15 May 2015; IEEE: Piscataway, NJ, USA, 2015; pp. 786–789. [Google Scholar]
- Buzhin, I.G.; Derevyankin, A.Y.; Antonova, V.M.; Perevalov, A.P. Comparative Analysis of the REST and gRPC Used in the Monitoring System of Communication Network Virtualized Infrastructure. T-Comm-Телекoммуникации и Транспoрт 2023, 17, 50–55. [Google Scholar] [CrossRef]
- Perelman, V.; Ersue, M.; Schönwälder, J.; Watsen, K. Network Configuration Protocol Light (NETCONF Light); Internet Engineering Task Force (IETF): Fremont, CA, USA, 2012. [Google Scholar]
- Choi, H.; Kim, J.; Choi, S.; Kwon, T. 6LoWPAN-SNMP: Simple Network Management Protocol for 6LoWPAN. In Proceedings of the 2009 11th IEEE International Conference on High Performance Computing and Communications, Seoul, Republic of Korea, 25–27 June 2009; pp. 305–313. Available online: https://ieeexplore.ieee.org/document/5167008/ (accessed on 16 February 2025).
- Veillette, M.; van der Stok, P.; Pelov, A.; Bierman, A.; Bormann, C. CoAP Management Interface (CORECONF); Internet Engineering Task Force, Internet-Draft Draft-Ietf-Core-Comi-19. 2024. Available online: https://datatracker.ietf.org/doc/draft-ietf-core-comi/ (accessed on 29 January 2025).
- Lalhriatpuii, R.; Ruchi; Wasson, V. Comprehensive Exploration of IoT Communication Protocol: CoAP, MQTT, HTTP, LoRaWAN and AMQP. In Proceedings of the ICMLA 2024: Machine Learning Algorithms, Miami, FL, USA, 18–20 December 2024; Springer: Cham, Switzerland, 2025. Communications in Computer and Information Science. Volume 2238, pp. 261–274. [Google Scholar]
- Rao, S.; Chendanda, D.; Deshpande, C.; Lakkundi, V. Implementing LWM2M in Constrained IoT Devices. In Proceedings of the 2015 IEEE Conference on Wireless Sensors (ICWiSe), Malacca, Malaysia, 24–26 August 2015; IEEE: Piscataway, NJ, USA, 2015; pp. 52–57. [Google Scholar]
- Agyemang, J.O.; Kponyo, J.J.; Gadze, J.D.; Nunoo-Mensah, H.; Yu, D. A Lightweight Messaging Protocol for Internet of Things Devices. Technologies 2022, 10, 21. [Google Scholar] [CrossRef]
- Słabicki, M.; Grochla, K. Performance evaluation of snmp, netconf and cwmp management protocols in wireless network. In Electronics, Communications and Networks IV, Proceedings of the 4th International Conference on Electronics, Communications and Networks, Bhopal, India, 7–9 April 2014; CRC Press: Boca Raton, FL, USA, 2014; pp. 12–15. [Google Scholar]
- Kang, J.M.; Ju, H.T.; Choi, M.J.; Hong, J.W.K.; Kim, J.G. OMA DM-based remote software fault management for mobile devices. Int. J. Netw. Manag. 2009, 19, 491–511. [Google Scholar] [CrossRef]
- Khaled, A.E.; Helal, S. Interoperable communication framework for bridging RESTful and topic-based communication in IoT. Future Gener. Comput. Syst. 2019, 92, 628–643. [Google Scholar] [CrossRef]
- McKeown, N.; Anderson, T.; Balakrishnan, H.; Parulkar, G.; Peterson, L.; Rexford, J.; Shenker, S.; Turner, J. OpenFlow: Enabling Innovation in Campus Networks. ACM SIGCOMM Comput. Commun. Rev. 2008, 38, 69–74. [Google Scholar] [CrossRef]
- Claise, B.; Trammell, B.; Aitken, P. RFC 7011; Specification of the IP Flow Information Export (IPFIX) Protocol for the Exchange of Flow Information. Internet Engineering Task Force: Fremont, CA, USA, 2013. [CrossRef]
- Khang, A.; Nazila, A.R.; Vugar, A.H.; Abuzarova, V.A. Advanced technologies and data management in the smart healthcare system. In AI-Centric Smart City Ecosystems; CRC Press: Boca Raton, FL, USA, 2022; pp. 261–270. [Google Scholar]
- Lombardi, M.; Pascale, F.; Santaniello, D. Internet of things: A general overview between architectures, protocols and applications. Information 2021, 12, 87. [Google Scholar] [CrossRef]
- Indrakumari, R.; Poongodi, T.; Sumathi, D.; Suganthi, S.; Suresh, P. IoT-based biomedical sensors for pervasive and personalized healthcare. In Internet of Things, Artificial Intelligence and Blockchain Technology; Springer: Cham, Switzerland, 2021; pp. 111–130. [Google Scholar]
- Navaz, A.N.; Serhani, M.A.; El Kassabi, H.T.; Al-Qirim, N.; Ismail, H. Trends, technologies, and key challenges in smart and connected healthcare. IEEE Access 2021, 9, 74044–74067. [Google Scholar] [CrossRef] [PubMed]
- Sehgal, A.; Perelman, V.; Kuryla, S.; Schönwälder, J. Management of resource constrained devices in the internet of things. IEEE Commun. Mag. 2012, 50, 144–149. [Google Scholar] [CrossRef]
- MQTT Version 3.1.1. [Online]. Available online: http://docs.oasis-open.org/mqtt/mqtt/v3.1.1/mqtt-v3.1.1.html (accessed on 1 March 2025).
- oneM2M. Functional Architecture; Technical Specification TS-0001, Version 3.11.1; oneM2M: Sophia Antipolis, France, 2022; Available online: https://www.onem2m.org/technical (accessed on 13 March 2025).
- Savic, M. Bridging the SNMP gap: Simple network monitoring the internet of things. Facta Univ. Ser. Electron. Energetics 2016, 29, 475–487. [Google Scholar] [CrossRef]
- Swetina, J.; Lu, G.; Jacobs, P.; Ennesser, F.; Song, J. Toward a standardized common M2M service layer platform: Introduction to oneM2M. IEEE Wirel. Commun. 2014, 21, 20–26. [Google Scholar] [CrossRef]
- Woo, M.W.; Lee, J.W.; Park, K.H. A reliable IoT system for Personal Healthcare Devices. Future Gener. Comput. Syst. 2018, 78, 626–640. [Google Scholar] [CrossRef]
- ISO/IEEE. Health Informatics—Medical Device Communication—Part 11073: Service-Oriented Device Connectivity (SDC) Standards Series. ISO/IEEE 11073; International Organization for Standardization (ISO)/IEEE: Geneva, Switzerland; New York, NY, USA, 2021. [Google Scholar]
- Yao, J.; Warren, S. Applying the ISO/IEEE 11073 standards to wearable home health monitoring systems. J. Clin. Monit. Comput. 2005, 19, 427–436. [Google Scholar] [CrossRef]
- Mekrache, A.; Ksentini, A.; Verikoukis, C. Machine Reasoning in FCAPS: Towards Enhanced Beyond 5G Network Management. IEEE Commun. Surv. Tutor. 2024, 26, 2769–2797. [Google Scholar] [CrossRef]
- Amin, A.A.; Hasan, K.M. A review of fault tolerant control systems: Advancements and applications. Measurement 2019, 143, 58–68. [Google Scholar] [CrossRef]
- Tariq, A.; Rehman, R.A.; Kim, B.S. Energy Efficient Priority Aware Forwarding in SDN-Enabled Named Data Internet of Things. In Proceedings of the 2020 International Conference on Electronics, Information, and Communication (ICEIC), Barcelona, Spain,, 19–22 January 2020; IEEE: Piscataway, NJ, USA, 2020; pp. 1–4. [Google Scholar]
- Tariq, A.; Rehman, R.A.; Kim, B.S. An Intelligent Forwarding Strategy in SDN-Enabled Named-Data IoV. Comput. Mater. Contin. 2021, 69, 3. [Google Scholar] [CrossRef]
- Kreutz, D.; Ramos, F.M.V.; Verissimo, P.; Rothenberg, C.E.; Azodolmolky, S.; Uhlig, S. Software-Defined Networking: A Comprehensive Survey. Proc. IEEE 2014, 103, 14–76. [Google Scholar] [CrossRef]
- Deepak, K.S.; Babu, A.V. Improving Reliability of Emergency Data Frame Transmission in IEEE 802.15.6 Wireless Body Area Networks. IEEE Syst. J. 2017, 12, 2082–2093. [Google Scholar] [CrossRef]
- Ahad, A.; Tahir, M.; Yau, K.L.A. 5G-based smart healthcare network: Architecture, taxonomy, challenges and future research directions. IEEE Access 2019, 7, 100747–100762. [Google Scholar] [CrossRef]
- Li, O.; Liu, H.; Chen, C.; Rudin, C. Deep Learning for Case-based Reasoning through Prototypes: A Neural Network that Explains Its Predictions. In Proceedings of the AAAI Conference on Artificial Intelligence, San Francisco, CA, USA, 4–9 February 2017. [Google Scholar]
- Khater, H.M.; Sallabi, F.; Serhani, M.A.; Barka, E.; Shuaib, K.; Tariq, A.; Khayat, M. Empowering Healthcare with Cyber-Physical System–A Systematic Literature Review. IEEE Access 2024, 12, 83952–83993. [Google Scholar] [CrossRef]
- Tariq, A.; Serhani, M.A.; Sallabi, F.M.; Barka, E.S.; Qayyum, T.; Khater, H.M.; Shuaib, K.A. Trustworthy Federated Learning: A Comprehensive Review, Architecture, Key Challenges, and Future Research Prospects. IEEE Open J. Commun. Soc. 2024, 5, 4920–4998. [Google Scholar] [CrossRef]
- Tariq, A.; Sallabi, F.; Serhani, M.A.; Qayyum, T.; Barka, E.S. Leveraging Game Theory and XAI for Data Quality-Driven Sample and Client Selection in Trustworthy Split Federated Learning. IEEE Trans. Consum. Electron. 2025. [Google Scholar] [CrossRef]
- Babu, P.R.; Kumar, S.A.; Reddy, A.G.; Das, A.K. Quantum Secure Authentication and Key Agreement Protocols for IoT-Enabled Applications: A Comprehensive Survey and Open Challenges. Comput. Sci. Rev. 2024, 54, 100676. [Google Scholar] [CrossRef]
- Qayyum, T.; Tariq, A.; Haseeb, M.W.; Lakas, A.; Serhani, M.A.; Trabelsi, Z. Quantum-Enhanced Convolutional Neural Networks for Image Classification. In Proceedings of the 2023 IEEE Future Networks World Forum (FNWF), Baltimore, MD, USA, 13–15 November 2023; IEEE: Piscataway, NJ, USA, 2023; pp. 1–7. [Google Scholar]
- Conti, V.; Militello, C.; Rundo, L.; Vitabile, S. A Novel Bio-Inspired Approach for High-Performance Management in Service-Oriented Networks. IEEE Trans. Emerg. Top. Comput. 2020, 9, 1709–1722. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).