Using Higher-Order Constructs to Estimate Health-Disease Status: The Effect of Health System Performance and Sustainability
Abstract
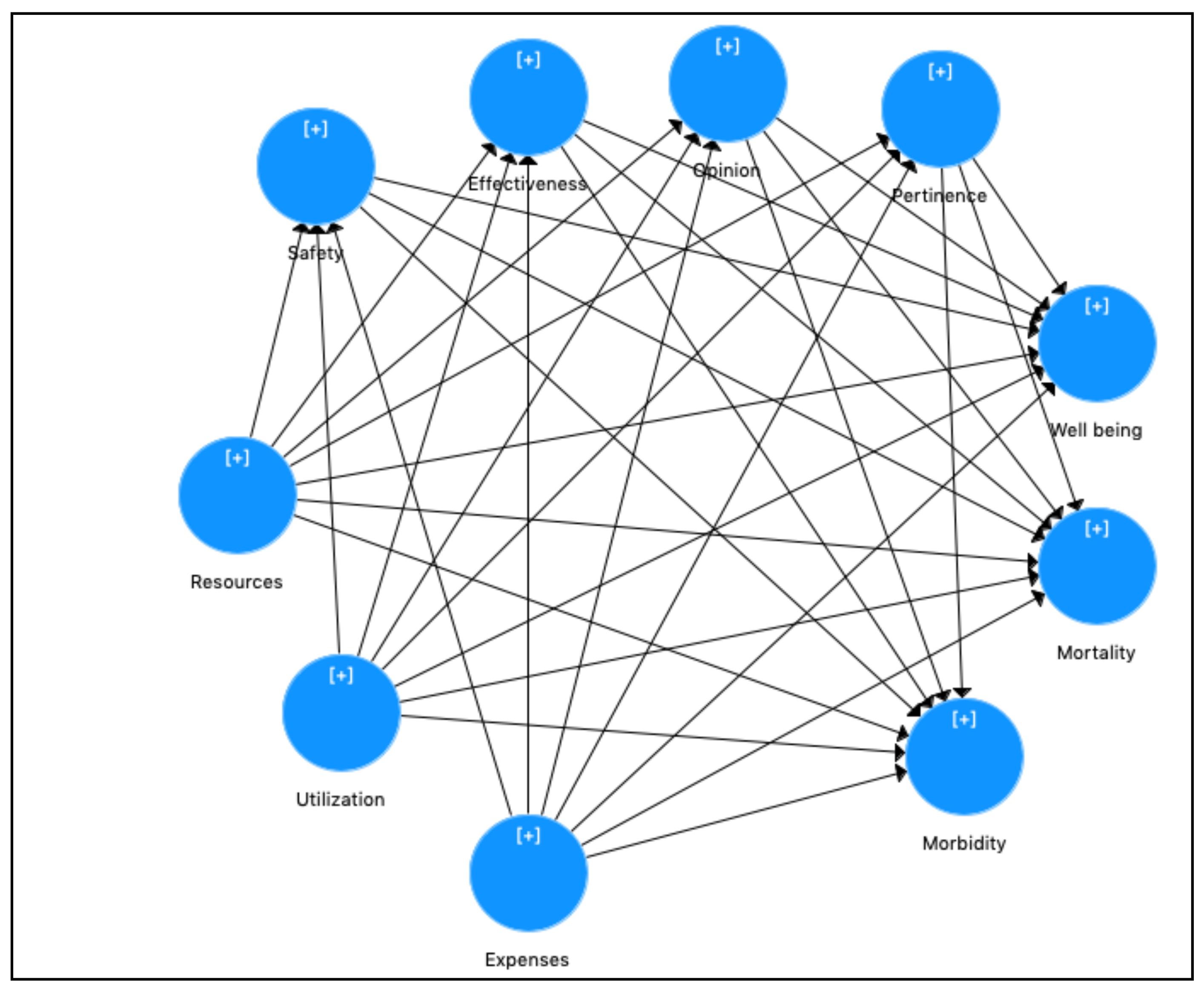
:1. Introduction
Literature Background and Hypotheses
- Health system sustainability
- Health system performance
- Health–disease status
2. Research Methodology
2.1. PLS-SEM Analysis
2.2. Specification of PLS-SEM Model
2.3. Data and Sample
3. Assessing PLS-SEM Results
3.1. Evaluation of LOC Measurement Model
3.1.1. Reflective Measurement Model
- Individual item reliability LOC
- Construct Reliability LOC
- Convergent validity LOC
- Discriminant validity LOC
3.1.2. Formative Measurement Model
- Collinearity of mode B indicators’ LOC
- Compute the LOC scores
3.2. Evaluation of HOC Measurement Model
3.2.1. Reflective Measurement Model
- Individual item reliability HOC
- Construct Reliability HOC
- Convergent validity HOC
- Discriminant validity HOC
3.2.2. Formative Measurement Model
3.3. Evaluation of HOC Structural Model
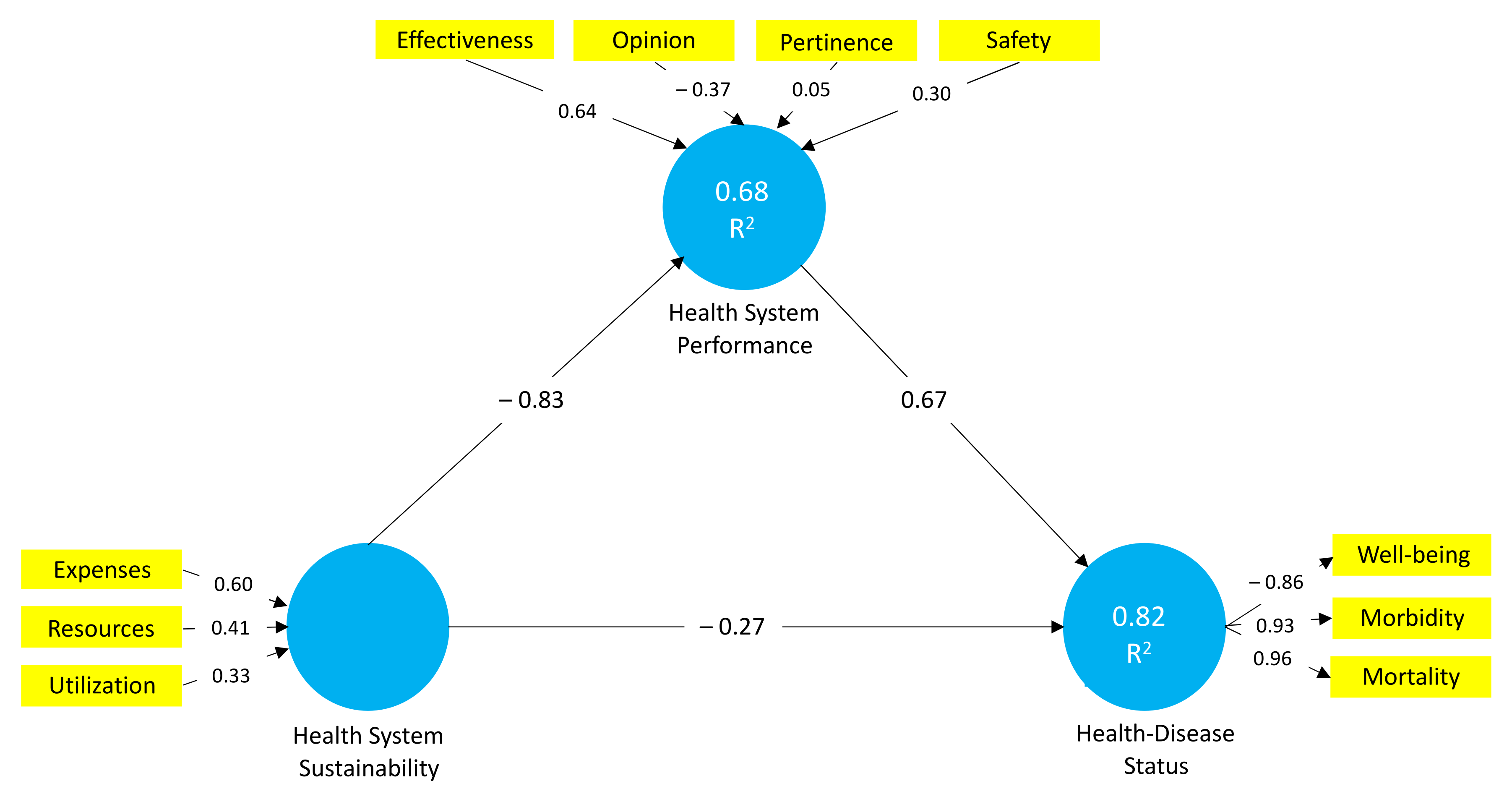
3.3.1. Evaluation of Path Coefficients
3.3.2. Assessment of the Coefficient of Determination (R2)
3.3.3. Review of Effect Sizes (f2)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Blouin, G.G. Data Performativity and Health: The Politics of Health Data Practices in Europe. Sci. Technol. Hum. Values 2020, 45, 317–341. [Google Scholar] [CrossRef]
- Hejduková, P.; Kureková, L. National Health Systems’ Performance: Evaluation WHO Indicators. Procedia Soc. Behav. Sci. 2016, 230, 240–248. [Google Scholar] [CrossRef] [Green Version]
- Hanson, K. La Medición Del Estado de la Salud: Género, Carga de Morbilidad Y Establecimiento de Prioridades en el Sector Salud. OPS Publ. Occas. 2000, 5. [Google Scholar]
- Kramers, P.G.N. The ECHI project. Eur. J. Public Health 2003, 13, 101–106. [Google Scholar] [CrossRef]
- Verschuuren, M.; Gissler, M.; Kilpeläinen, K.; Tuomi-Nikula, A.; Sihvonen, A.-P.; Thelen, J.; Gaidelyte, R.; Ghirini, S.; Kirsch, N.; Prochorskas, R.; et al. Public health indicators for the EU: The joint action for ECHIM (European Community Health Indicators & Monitoring). Arch. Public Health 2013, 71, 12. [Google Scholar] [CrossRef] [Green Version]
- Kruk, M.E.; Freedman, L.P. Assessing health system performance in developing countries: A review of the literature. Health Policy 2008, 85, 263–276. [Google Scholar] [CrossRef]
- Cuggia, M.; Toubiana, L. Health Information Systems. Yearb Med. Inform. 2013, 22, 114–116. [Google Scholar] [CrossRef] [Green Version]
- World Health Oragnization. 2020. Available online: https://www.who.int/es/about/who-we-are/constitution (accessed on 1 May 2021).
- Castro-Vázquez, Á.; Espinosa-Gutiérrez, I.; Rodríguez-Contreras, P.; Santos-Iglesias, P. Relación entre el estado de salud percibido e indicadores de salud en la población española. Int. J. Clin. Health Psychol. 2007, 7, 883–898. [Google Scholar]
- Cinaroglu, S.; Baser, O. Understanding the relationship between effectiveness and outcome indicators to improve quality in healthcare. Total. Qual. Manag. Bus. Excel. 2018, 29, 1294–1311. [Google Scholar] [CrossRef]
- Murray, C.J.L.; Frenk, J. A framework for assessing the performance of health systems. Bull. World Health Organ. 2000, 78, 717–731. [Google Scholar]
- Anderson, G.; Hussey, P.S. Comparing Health System Performance in OECD Countries. Health Aff. 2001, 20, 219–232. [Google Scholar] [CrossRef]
- Faezipour, M.; Ferreira, S. A System Dynamics Perspective of Patient Satisfaction in Healthcare. Procedia Comput. Sci. 2013, 16, 148–156. [Google Scholar] [CrossRef] [Green Version]
- Puertas, R.; Marti, L.; Guaita-Martinez, J.M. Innovation, lifestyle, policy and socioeconomic factors: An analysis of European quality of life. Technol. Forecast. Soc. Chang. 2020, 160, 120209. [Google Scholar] [CrossRef]
- García-Alfranca, F.; Puig, A.; Galup, C.; Aguado, H.; Cerdá, I.; Guilabert, M.; Pérez-Jover, V.; Carrillo, I.; Mira, J.J. Patient Satisfaction with Pre-Hospital Emergency Services. A Qualitative Study Comparing Professionals’ and Patients’ Views. Int. J. Environ. Res. Public Health 2018, 15, 233. [Google Scholar] [CrossRef] [Green Version]
- Rosenbusch, J.; Ismail, I.R.; Ringle, C.M. The agony of choice for medical tourists: A patient satisfaction index model. J. Hosp. Tour. Technol. 2018, 9, 267–279. [Google Scholar] [CrossRef]
- Vogus, T.J.; McClelland, L.E. When the customer is the patient: Lessons from healthcare research on patient satisfaction and service quality ratings. Hum. Resour. Manag. Rev. 2016, 26, 37–49. [Google Scholar] [CrossRef]
- Varabyova, Y.; Müller, J.-M. The efficiency of health care production in OECD countries: A systematic review and meta-analysis of cross-country comparisons. Health Policy 2016, 120, 252–263. [Google Scholar] [CrossRef]
- Garcia-Lacalle, J.; Martin, E. Rural vs urban hospital performance in a ‘competitive’ public health service. Soc. Sci. Med. 2010, 71, 1131–1140. [Google Scholar] [CrossRef]
- Chang, C.-W.; Tseng, T.-H.; Woodside, A.G. Configural algorithms of patient satisfaction, participation in diagnostics, and treatment decisions ’ influences on hospital loyalty. J. Serv. Mark. 2013, 27, 91–103. [Google Scholar] [CrossRef] [Green Version]
- Ferreira, P.L.; Raposo, V.; Tavares, A.I. Primary health care patient satisfaction: Explanatory factors and geographic characteristics. Int. J. Qual. Health Care 2020, 32, 93–98. [Google Scholar] [CrossRef]
- Manzoor, F.; Wei, L.; Hussain, A.; Asif, M.; Shah, S.I.A. Patient Satisfaction with Health Care Services; An Application of Physician’s Behavior as a Moderator. Int. J. Environ. Res. Public Health 2019, 16, 3318. [Google Scholar] [CrossRef] [Green Version]
- Aiken, L.H.; Sloane, D.M.; Ball, J.; Bruyneel, L.; Rafferty, A.M.; Griffiths, P. Patient satisfaction with hospital care and nurses in England: An observational study. BMJ Open 2021, 8, e019189. [Google Scholar] [CrossRef]
- Pérez-Romero, S.; Gascón-Cánovas, J.J.; Salmerón-Martínez, D.; Parra-Hidalgo, P.; Monteagudo-Piqueras, O. Relevancia del contexto socioeconómico y sanitario en la satisfacción del paciente. Gac. Sanit. 2017, 31, 416–422. [Google Scholar] [CrossRef]
- Draper, M.; Cohen, P.; Buchan, H. Seeking consumer views: What use are results of hospital patient satisfaction surveys? Int. J. Qual. Health Care 2001, 13, 463–468. [Google Scholar] [CrossRef]
- Kamra, V.; Singh, H.; De, K.K. Factors affecting patient satisfaction: An exploratory study for quality management in the health-care sector. Total. Qual. Manag. Bus. Excel. 2016, 27, 1013–1027. [Google Scholar] [CrossRef]
- Evangelinos, K.; Fotiadis, S.; Skouloudis, A.; Khan, N.; Konstandakopoulou, F.; Nikolaou, I.; Lundy, S. Occupational health and safety disclosures in sustainability reports: An overview of trends among corporate leaders. Corp. Soc. Responsib. Environ. Manag. 2018, 25, 961–970. [Google Scholar] [CrossRef]
- Molero, A.; Calabrò, M.; Vignes, M.; Gouget, B.; Gruson, A.D. Sustainability in Healthcare: Perspectives and Reflections Regarding Laboratory Medicine. Ann. Lab. Med. 2021, 41, 139–144. [Google Scholar] [CrossRef]
- Handayani, P.W.; Hidayanto, A.N.; Sandhyaduhita, P.I.; Kasiyah; Ayuningtyas, D. Strategic hospital services quality analysis in Indonesia. Expert Syst. Appl. 2015, 42, 3067–3078. [Google Scholar] [CrossRef]
- lo Storto, C.; Goncharuk, A.G. Efficiency vs effectiveness: A benchmarking study on European healthcare systems. Econ. Sociol. 2017, 10, 102–115. [Google Scholar] [CrossRef] [Green Version]
- Ruo, B.; Rumsfeld, J.S.; Hlatky, M.A.; Liu, H.; Browner, W.S.; Whooley, M.A. Depressive Symptoms and Health-Related Quality of Life. JAMA 2003, 290, 215–221. [Google Scholar] [CrossRef]
- Hussain, A.; Asif, M.; Jameel, A.; Hwang, J.; Sahito, N.; Kanwel, S. Promoting OPD Patient Satisfaction through Different Healthcare Determinants: A Study of Public Sector Hospitals. Int. J. Environ. Res. Public Health 2019, 16, 3719. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- European Observatory on Health Systems and Policies. State of Health in the EU-Spain: Country Health Profile 2019. Available online: https://ec.europa.eu/health/sites/health/files/state/docs/2019_chp_es_english.pdf (accessed on 12 March 2021).
- Ferreira, D.C.; Nunes, A.M.; Marques, R.C. Operational efficiency vs clinical safety, care appropriateness, timeliness, and access to health care. J. Prod. Anal. 2020, 53, 355–375. [Google Scholar] [CrossRef]
- Rabar, D.; Fabić, M.G.; Petrlić, A. Financial performance–efficiency nexus in public health services: A nonparametric evidence-based approach. Econ. Res. Ekonomska Istraživanja 2020, 33, 3334–3355. [Google Scholar] [CrossRef]
- Gutierrez-Robredo, L. Morbilidad en la poblacion mayor. El proceso de la transición epidemiológica. Demos 2001, 14, 8–9. [Google Scholar]
- Díaz, R. Satisfacción del paciente: Principal motor y centro de los servicios sanitarios. Rev. Calid. Asist. 2002, 17, 22–29. [Google Scholar] [CrossRef]
- Pederson, J.L.; Warkentin, L.M.; Majumdar, S.R.; McAlister, F.A. Depressive symptoms are associated with higher rates of readmission or mortality after medical hospitalization: A systematic review and meta-analysis. J. Hosp. Med. 2016, 11, 373–380. [Google Scholar] [CrossRef] [Green Version]
- Purcărea, V.L.; Gheorghe, I.R.; Petrescu, C.M. The Assessment of Perceived Service Quality of Public Health Care Services in Romania Using the SERVQUAL Scale. Procedia Econ. Financ. 2013, 6, 573–585. [Google Scholar] [CrossRef] [Green Version]
- Yang, H.; Guo, X.; Wu, T. Exploring the influence of the online physician service delivery process on patient satisfaction. Decis. Support Syst. 2015, 78, 113–121. [Google Scholar] [CrossRef]
- Vieco-Gómez, G.F.; Abello Llanos, R. Psychosocial factors at work, stress and morbidity around the world. Psicol. Desde Caribe 2014, 31, 354–385. [Google Scholar] [CrossRef]
- Llobet, C.V.; Banqué, M.; Fuentes, M.; Ojuel, J. Morbilidad diferencial entre mujeres y hombres. Anuario Psicol. 2008, 39, 9–22. [Google Scholar]
- Carreras, M.; Puig, G.; Sánchez-Pérez, I.; Inoriza, J.M.; Coderch, J.; Gispert, R. Morbidity and self-perception of health, two different approaches to health status. Gac. Sanit. 2020, 34, 601–607. [Google Scholar] [CrossRef]
- Berta, P.; Ingrassia, S.; Punzo, A.; Vittadini, G. Multilevel cluster-weighted models for the evaluation of hospitals. Metron 2016, 74, 275–292. [Google Scholar] [CrossRef]
- Mendoza, L.A.; Arias, M.; Mendoza, L.I. Hijo de madre adolescente: Riesgos, morbilidad y mortalidad neonatal. Rev. Chil. Obstet. Ginecol. 2012, 77, 375–382. [Google Scholar] [CrossRef] [Green Version]
- Kashian, R.; Lovett, N.; Xue, Y. Has the affordable care act affected health care efficiency? J. Regul. Econ. 2020, 58, 193–233. [Google Scholar] [CrossRef]
- Martínez, M.D.C.V.; Ramírez-Orellana, A. Patient Satisfaction in the Spanish National Health Service: Partial Least Squares Structural Equation Modeling. Int. J. Environ. Res. Public Health 2019, 16, 4886. [Google Scholar] [CrossRef] [Green Version]
- Horvat, A.; Filipovic, J. Healthcare system quality indicators: The complexity perspective. Total. Qual. Manag. Bus. Excel. 2020, 31, 161–177. [Google Scholar] [CrossRef]
- Amin, M.; Nasharuddin, S.Z. Hospital service quality and its effects on patient satisfaction and behavioural intention. Clin. Gov. Int. J. 2013, 18, 238–254. [Google Scholar] [CrossRef] [Green Version]
- Huynh, H.P.; Sweeny, K.; Miller, T. Transformational leadership in primary care: Clinicians’ patterned approaches to care predict patient satisfaction and health expectations. J. Health Psychol. 2018, 23, 743–753. [Google Scholar] [CrossRef] [Green Version]
- Ricci-Cabello, I.; Stevens, S.; Dalton, A.R.H.; Griffiths, R.I.; Campbell, J.L.; Valderas, J.M. Identifying Primary Care Pathways from Quality of Care to Outcomes and Satisfaction Using Structural Equation Modeling. Health Serv. Res. 2018, 53, 430–449. [Google Scholar] [CrossRef] [Green Version]
- DiMatteo, M. Variations in patients’ adherence to medical recommendations: A quantitative review of 50 years of research. Med. Care 2004, 42, 200–209. [Google Scholar] [CrossRef]
- Hunter-Jones, P.; Line, N.; Zhang, J.J.; Malthouse, E.C.; Witell, L.; Hollis, B. Visioning a hospitality-oriented patient experience (HOPE) framework in health care. J. Serv. Manag. 2020, 31, 869–888. [Google Scholar] [CrossRef]
- Macrae, H. “It’s my body, my future”: Older women’s views of their interactions with physicians. J. Women Aging 2016, 28, 211–224. [Google Scholar] [CrossRef] [PubMed]
- Gulías, E.; Díez, N.; Pereira, M. Los componentes de la satisfacción de los pacientes y su utilidad para la gestión hospitalaria. Rev. Española Cienc. Política 2013, 32, 161–181. [Google Scholar]
- Fernández-Pérez, Á.; Sánchez, Á. Improving People’s Self-Reported Experience with the Health Services: The Role of Non-Clinical Factors. Int. J. Environ. Res. Public Health 2020, 17, 178. [Google Scholar] [CrossRef] [Green Version]
- Bible, J.E.; Shau, D.N.; Kay, H.F.; Cheng, J.S.; Aaronson, O.S.; Devin, C.J. Are Low Patient Satisfaction Scores Always Due to the Provider? Spine 2018, 43, 58–64. [Google Scholar] [CrossRef]
- Vámosi, M.; Lauberg, A.; Borregaard, B.; Christensen, A.V.; Thrysoee, L.; Rasmussen, T.B.; Ekholm, O.; Juel, K.; Berg, S.K. Patient-reported outcomes predict high readmission rates among patients with cardiac diagnoses. Findings from the DenHeart study. Int. J. Cardiol. 2020, 300, 268–275. [Google Scholar] [CrossRef]
- Ferreira, D.; Marques, R.C. Do quality and access to hospital services impact on their technical efficiency? Omega 2019, 86, 218–236. [Google Scholar] [CrossRef]
- Martini, G.; Berta, P.; Mullahy, J.; Vittadini, G. The effectiveness–efficiency trade-off in health care: The case of hospitals in Lombardy, Italy. Reg. Sci. Urban Econ. 2014, 49, 217–231. [Google Scholar] [CrossRef]
- Kilpeläinen, K.; Tuomi-Nikula, A.; Thelen, J.; Gissler, M.; Sihvonen, A.-P.; Kramers, P.; Aromaa, A. Health indicators in Europe: Availability and data needs. Eur. J. Public Health 2012, 22, 716–721. [Google Scholar] [CrossRef] [Green Version]
- Williams, L.J.; Vandenberg, R.J.; Edwards, J.R. 12 Structural Equation Modeling in Management Research: A Guide for Improved Analysis. Acad. Manag. Ann. 2009, 3, 543–604. [Google Scholar] [CrossRef]
- Wold, H. Soft modelling: Intermediate between traditional model building and data analysis. Banach Cent. Publ. 1980, 6, 333–346. [Google Scholar] [CrossRef] [Green Version]
- Chin, W.W. The partial least squares approach to structural equation modeling. In Modern Methods for Business Research; Marcoulides, G., Ed.; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 1998; pp. 295–336. [Google Scholar]
- Roldán, J.; Sánchez-Franco, M. Variance-based structural equation modeling: Guidelines for using partial least squares in information systems research. In Research Methodologies, Innovations and Philosophies in Software Systems Engineering and Information Systems; Mora, M., Steenkamp, A., Johnston, L., Gamon, J., Eds.; IGI Global: Hershey, PA, USA, 2012; pp. 193–221. [Google Scholar]
- Henseler, J.; Ringle, C.M.; Sarstedt, M. Testing measurement invariance of composites using partial least squares. Int. Mark. Rev. 2016, 33, 405–431. [Google Scholar] [CrossRef]
- Hair, J.F.; Risher, J.J.; Sarstedt, M.; Ringle, C.M. When to use and how to report the results of PLS-SEM. Eur. Bus. Rev. 2019, 31, 2–24. [Google Scholar] [CrossRef]
- Wetzels, M.; Odekerken-Schröder, G.; Van Oppen, C. Using PLS Path Modeling for Assessing Hierarchical Construct Models: Guidelines and Empirical Illustration. MIS Q. 2009, 33, 177–195. [Google Scholar] [CrossRef]
- Chin, W.W. How to Write Up and Report PLS Analyses. In Handbook of Partial Least Squares; Esposito, V.V., Chin, W.W., Henseler, J., Wang, H., Eds.; Springer: Berlin/Heidelberg, Germany, 2009; pp. 655–690. [Google Scholar]
- Richter, N.F.; Cepeda, G.; Roldán, J.L.; Ringle, C.M. European management research using partial least squares structural equation modeling (PLS-SEM). Eur. Manag. J. 2016, 34, 589–597. [Google Scholar] [CrossRef]
- Bollen, K.A.; Bauldry, S. Three Cs in measurement models: Causal indicators, composite indicators, and covariates. Psychol. Methods 2011, 16, 265–284. [Google Scholar] [CrossRef] [Green Version]
- Müller, T.; Schuberth, F.; Henseler, J. PLS path modeling—A confirmatory approach to study tourism technology and tourist behavior. J. Hosp. Tour. Technol. 2018, 9, 249–266. [Google Scholar] [CrossRef] [Green Version]
- Ringle, C.M.; Sarstedt, M.; Mitchell, R.; Gudergan, S.P. Partial least squares structural equation modeling in HRM research. Int. J. Hum. Resour. Manag. 2020, 31, 1617–1643. [Google Scholar] [CrossRef]
- Grace, J.B.; Bollen, K.A. Representing general theoretical concepts in structural equation models: The role of composite variables. Environ. Ecol. Stat. 2008, 15, 191–213. [Google Scholar] [CrossRef]
- Alfalla-Luque, R.; Machuca, J.A.; Marin-Garcia, J.A. Triple-A and competitive advantage in supply chains: Empirical research in developed countries. Int. J. Prod. Econ. 2018, 203, 48–61. [Google Scholar] [CrossRef]
- Polites, G.L.; Roberts, N.; Thatcher, J. Conceptualizing models using multidimensional constructs: A review and guidelines for their use. Eur. J. Inf. Syst. 2012, 21, 22–48. [Google Scholar] [CrossRef]
- Hair, J.F.; Hult, G.; Ringle, C.; Sarstedt, M. A Primer on Partial Least Squares Structural Equation Modeling (Pls-SeM), 2nd ed.; Sage Publications: Thousand Oaks, CA, USA, 2017. [Google Scholar]
- Sarstedt, M.; Hair, J.F.; Cheah, J.-H.; Becker, J.-M.; Ringle, C.M. How to Specify, Estimate, and Validate Higher-Order Constructs in PLS-SEM. Australas. Mark. J. 2019, 27, 197–211. [Google Scholar] [CrossRef]
- Law, K.S.; Wong, C.-S.; Mobley, W.H. Toward a Taxonomy of Multidimensional Constructs. Acad. Manag. Rev. 1998, 23, 741. [Google Scholar] [CrossRef]
- Edwards, J.R. Multidimensional Constructs in Organizational Behavior Research: An Integrative Analytical Framework. Organ. Res. Methods 2001, 4, 144–192. [Google Scholar] [CrossRef]
- Roemer, E. A tutorial on the use of PLS path modeling in longitudinal studies. Ind. Manag. Data Syst. 2016, 116, 1901–1921. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.-G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carmines, E.; Zeller, R. Reliability and Validity Assessment; SAGE Publications Inc.: London, UK, 1979. [Google Scholar]
- Garson, G. Partial Least Squares: Regression & Structural Equation Models; Statistical Publishing Associates: Asheboro, NC, USA, 2016; pp. 1–262. [Google Scholar]
- Dijkstra, T.K.; Henseler, J. Consistent partial least squares path modeling. MIS Q. 2015, 39, 297–316. [Google Scholar] [CrossRef]
- Henseler, J.; Ringle, C.M.; Sarstedt, M. A new criterion for assessing discriminant validity in variance-based structural equation modeling. J. Acad. Mark. Sci. 2015, 43, 115–135. [Google Scholar] [CrossRef] [Green Version]
- Franke, G.; Sarstedt, M. Heuristics versus statistics in discriminant validity testing: A comparison of four procedures. Internet Res. 2019, 29, 430–447. [Google Scholar] [CrossRef]
- Fornell, C.; Larcker, D.F. Evaluating Structural Equation Models with Unobservable Variables and Measurement Error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- Barclay, D.; Higgins, C.; Thomson, R. The partial least squares approach to causal modeling personal computer adoption and use as an illustration. Technol. Stud. 1995, 2, 285–309. [Google Scholar]
- Henseler, J.; Ringle, C.M.; Sinkovics, R.R. The use of partial least squares path modeling in international marketing. In New Advances in International Marketing; Emerald Publishing Limited: Bingley, UK, 2009; Volume 20, pp. 277–319. [Google Scholar]
- Hair, J.F.; Ringle, C.M.; Sarstedt, M. PLS-SEM: Indeed a Silver Bullet. J. Mark. Theory Pract. 2011, 19, 139–152. [Google Scholar] [CrossRef]
- Hayes, A.F. Beyond Baron and Kenny: Statistical Mediation Analysis in the New Millennium. Commun. Monogr. 2009, 76, 408–420. [Google Scholar] [CrossRef]
- Cepeda, G.; Nitzl, C.; Roldán, J. Mediation analyses in partial least squares structural equation modeling: Guidelines and empirical examples. In Partial Least Squares Path Modeling: Basic Concepts, Methodological Issues and Applications; Latan, H., Noonan, R., Eds.; Springer: Cham, Switzerland, 2017; pp. 173–195. [Google Scholar]
- Falk, R.; Miller, N. A Primer for Soft Modeling; University of Akron Press: Akron, OH, USA, 1992. [Google Scholar]
- Cohen, J. Set Correlation and Contingency Tables. Appl. Psychol. Meas. 1988, 12, 425–434. [Google Scholar] [CrossRef]
- Cameron, C.M.; Purdie, D.M.; Kliewer, E.V.; McClure, R.J. Differences in prevalence of pre-existing morbidity between injured and non-injured populations. Bull. World Health Organ. 2005, 83, 345–352. [Google Scholar]
- Leino-Kilpi, H.; Vuorenheimo, J. Patient satisfaction as an indicator of the quality of nursing care. Nord. J. Nurs. Res. 1992, 12, 22–28. [Google Scholar] [CrossRef]
- Duggirala, M.; Rajendran, C.; Anantharaman, R. Patient-perceived dimensions of total quality service in healthcare. Benchmarking Int. J. 2008, 15, 560–583. [Google Scholar] [CrossRef]
- Urrego, C.; Romero, M.; Murcia, Z.; Medina, C.; Marulanda, J.; Zerón, H. Evaluación de factores de riesgo asociados a enfermedad cardiovascular en jóvenes universitarios de la Localidad Santafé en Bogotá, Colombia. Nova 2016, 14, 35–45. [Google Scholar] [CrossRef] [Green Version]

| Composites | Indicators | Description |
|---|---|---|
| Effectiveness (Mode B) | EF1 | Birth of children from women less than 20 years old for each 100 births |
| EF2 | Incidence of tetanus per 100,000 inhab. | |
| EF3 | Incidence of hepatitis B per 100,000 inhab. | |
| EF4 | Incidence of mumps per 100,000 inhab. | |
| Safety (Mode B) | SA1 | Rate of suspected severe adverse effects rate to medication notified per 1,000,000 inhab. |
| SA2 | Intrahospital mortality of post-heart attack for every 100 discharges per a heart attack | |
| SA3 | Amputation rate of the lower limb in diabetes patients | |
| Opinion (Mode A) | O1 | Level of satisfaction of citizens with the public health system |
| O2 * | Level of satisfaction of citizens with their historical knowledge and the tracking of their health condition by their family doctor and pediatrician | |
| O3 | Level of satisfaction of citizens with the information provided by their doctor about their health condition | |
| Pertinence (Mode B) | PE1 | Percentage of laparoscopic cholecystectomy |
| PE2 | Percentage of conservative breast cancer surgery | |
| PE3 | Percentage of hip fracture patients with surgery in the first 48 h | |
| Expenses (Mode B) | EX1 | Percentage of health expenditure in primary care |
| EX2 | Percentage of health expenditure in pharmacy | |
| EX3 | Public health expenditure per covered population | |
| EX4 * | Percentage of health expenditure in specialized care | |
| EX5 | Percentage of health expenditure on salaries | |
| EX6 | Percentage of health expenditure on intermediate consumption | |
| EX7 * | Percentage of health expenditure on public–private contract | |
| EX8 | Percentage of health expenditure on internship training | |
| Utilization (Mode B) | U1 | Consultations with specialist doctors (% NHS) |
| U2 * | Hospitalizations (% NHS) | |
| U3 | Surgical interventions (% NHS) | |
| U4 * | CT utilization (% NHS) | |
| U5 * | Use rate of nuclear magnetic resonance (% NHS) | |
| U6 | Hemodialysis usage (% NHS) | |
| U7 | Hemodynamic usage (%NHS) | |
| Resources (Mode B) | RE1 | Specialist doctors (% NHS) |
| RE2 * | Specialized nursing (% NHS) | |
| RE3 | Beds in operation (% NHS) | |
| RE4 | Day hospital places (% NHS) | |
| RE5 * | Operating rooms (% NHS) | |
| RE6 | CT equipment (% NHS) | |
| RE7 * | Nuclear magnetic resonance equipment (% NHS) | |
| RE8 | Hemodialysis equipment (% NHS) | |
| RE9 | Hemodynamic equipment (% NHS) | |
| Well-being (Mode A) | WB1 | Life expectancy at birth |
| WB2 | Life expectancy at 65 years | |
| WB3 | Healthy life years at birth | |
| WB4 | Healthy life years at the age of 65 years | |
| Mortality (Mode B) | MT1 * | Ischemic heart disease mortality rate per 100,000 inhab. |
| MT2 | Cerebrovascular disease mortality rate per 100,000 inhab. | |
| MT3 | Cancer mortality rate per 100,000 inhab. | |
| MT4 | Chronic obstructive pulmonary disease mortality rate per 100,000 inhab. | |
| MT5 | Pneumonia and influenza mortality rate per 100,000 inhab. | |
| MT6 * | Chronic liver disease mortality rate per 100,000 inhab. | |
| MT7 | Diabetes mellitus mortality rate per 100,000 inhab. | |
| MT8 | Unintentional accidents mortality rate per 100,000 inhab. | |
| MT9 | Suicide mortality rate per 100,000 inhab. | |
| MT10 | Alzheimer’s mortality rate per 100,000 inhab. | |
| Morbidity (Mode B) | MB1 | Tuberculosis incidence |
| MB2 | New HIV diagnosis | |
| MB3 | Diabetes in adult population | |
| MB4 | Acute myocardial infarction hospitalization per 10,000 inhab. (NHS only) | |
| MB5 | Cerebrovascular disease hospitalization per 10,000 inhab. (NHS only) | |
| MB6 | Chronic obstructive pulmonary disease hospitalization per 10,000 inhab. (NHS only) | |
| MB7 | Diabetes mellitus hospitalization per 10,000 inhab. (NHS only) | |
| MB8 | Hypertensive disease hospitalization per 10,000 inhab. (NHS only) | |
| MB9 * | Congestive heart failure hospitalization per 10,000 inhab. (NHS only) | |
| MB10 | Victims of traffic accidents | |
| MB11 | Work accidents | |
| MB12 | Frequency of work accidents |
| Lower Order Composites | Higher-Order Composites |
|---|---|
| Effectiveness | Health system performance |
| Safety | |
| Opinion | |
| Pertinence | |
| Expenses | Health system sustainability |
| Utilization | |
| Resources | |
| Well-being | Health–disease status |
| Mortality | |
| Morbidity |
| Constructs | Cronbach Alpha | ρA | Composite Reliability |
| Opinion | 0.774 | 1.210 | 0.884 |
| Well-being | 0.841 | 0.878 | 0.890 |
| Constructs | EF | EX | MB | MT | O | PE | RE | SA | U | W−B |
|---|---|---|---|---|---|---|---|---|---|---|
| EF | n/a | |||||||||
| EX | −0.537 | n/a | ||||||||
| MB | 0.854 | −0.71 | n/a | |||||||
| MT | 0.846 | −0.635 | 0.873 | n/a | ||||||
| O | −0.271 | 0.364 | −0.452 | −0.369 | 0.891 | |||||
| PE | −0.186 | 0.342 | −0.136 | −0.033 | 0.167 | n/a | ||||
| RE | −0.548 | 0.421 | −0.627 | −0.555 | 0.614 | 0.141 | n/a | |||
| SA | 0.578 | −0.622 | 0.673 | 0.599 | −0.188 | −0.199 | −0.422 | n/a | ||
| U | −0.405 | 0.112 | −0.382 | −0.465 | 0.341 | −0.104 | 0.403 | −0.252 | n/a | |
| W−B | −0.657 | 0.543 | −0.665 | −0.761 | 0.367 | 0.110 | 0.519 | −0.405 | 0.431 | 0.820 |
| Constructs | Morbidity | Mortality | Well-Being |
|---|---|---|---|
| Health–disease Status | 0.934 | 0.960 | −0.860 |
| Construct | Cronbach Alpha | ρA | Composite Reliability |
|---|---|---|---|
| Health–disease Status | −0.876 | 0.926 | 0.696 |
| Constructs | Health–Disease Status | HS Performance | HS Sustainability |
|---|---|---|---|
| Health–disease St. | 0.919 | ||
| HS Performance | 0.890 | n/a | |
| HS Sustainability | −0.821 | −0.826 | n/a |
| Constructs | Original Sample | t | Loadings | Lo95 | Hi95 |
|---|---|---|---|---|---|
| Health System Sustainability | |||||
| Expenses | 0. 600 *** | 9.974 | 0.810 | [0.479; | 0.714] |
| Resources | 0. 413 *** | 7.978 | 0.798 | [0.314; | 0.517] |
| Utilization | 0. 328 *** | 6.194 | 0.562 | [0.220; | 0.427] |
| Health System Performance | |||||
| Effectiveness | 0. 639 *** | 14.307 | 0.902 | [0.547; | 0.723] |
| Opinion | −0. 367 *** | 7.616 | −0.588 | [−0.459; | −0.270] |
| Pertinence | 0. 051 ns | 1.410 | −0.189 | [−0.018; | 0.122] |
| Safety | 0. 298 *** | 6.267 | 0.727 | [0.205; | 0.392] |
| Constructs | Path | t | p | Lo95 | Hi95 | f2 | VIF |
|---|---|---|---|---|---|---|---|
| Direct effects | |||||||
| HSP→HS | 0.667 *** | 14.413 | 0.000 | 0.577; | 0.760 | 0.766 | 3.152 |
| HSS→HS | −0.821 *** | 36.448 | 0.000 | −0.864; | −0.775 | 0.125 | 3.152 |
| R2: 0.816; Q2: 0.672 | |||||||
| HSS→HSP | −0.826 *** | 35.197 | 0.000 | −0.873; | −0.781 | 2.152 | 1.000 |
| R2: 0.683 | |||||||
| Indirect effect | VAF | ||||||
| HSS→HSP→HS | −0.551 *** | 13.219 | 0.000 | −0.640 | −0.475 | 67.31% | n/a |
| HS Performance → Health–Disease Status | 0.766 | 0.000 |
| HS Sustainability → Health–Disease Status | 0.125 | 0.010 |
| HS Sustainability → HS Performance | 2.152 | 0.000 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ramírez-Orellana, A.; del Carmen Valls Martínez, M.; Grasso, M.S. Using Higher-Order Constructs to Estimate Health-Disease Status: The Effect of Health System Performance and Sustainability. Mathematics 2021, 9, 1228. https://doi.org/10.3390/math9111228
Ramírez-Orellana A, del Carmen Valls Martínez M, Grasso MS. Using Higher-Order Constructs to Estimate Health-Disease Status: The Effect of Health System Performance and Sustainability. Mathematics. 2021; 9(11):1228. https://doi.org/10.3390/math9111228
Chicago/Turabian StyleRamírez-Orellana, Alicia, María del Carmen Valls Martínez, and Mayra Soledad Grasso. 2021. "Using Higher-Order Constructs to Estimate Health-Disease Status: The Effect of Health System Performance and Sustainability" Mathematics 9, no. 11: 1228. https://doi.org/10.3390/math9111228
APA StyleRamírez-Orellana, A., del Carmen Valls Martínez, M., & Grasso, M. S. (2021). Using Higher-Order Constructs to Estimate Health-Disease Status: The Effect of Health System Performance and Sustainability. Mathematics, 9(11), 1228. https://doi.org/10.3390/math9111228








