A Smart Healthcare Knowledge Service Framework for Hierarchical Medical Treatment System
Abstract
1. Introduction
2. Research Status of Medical CBR
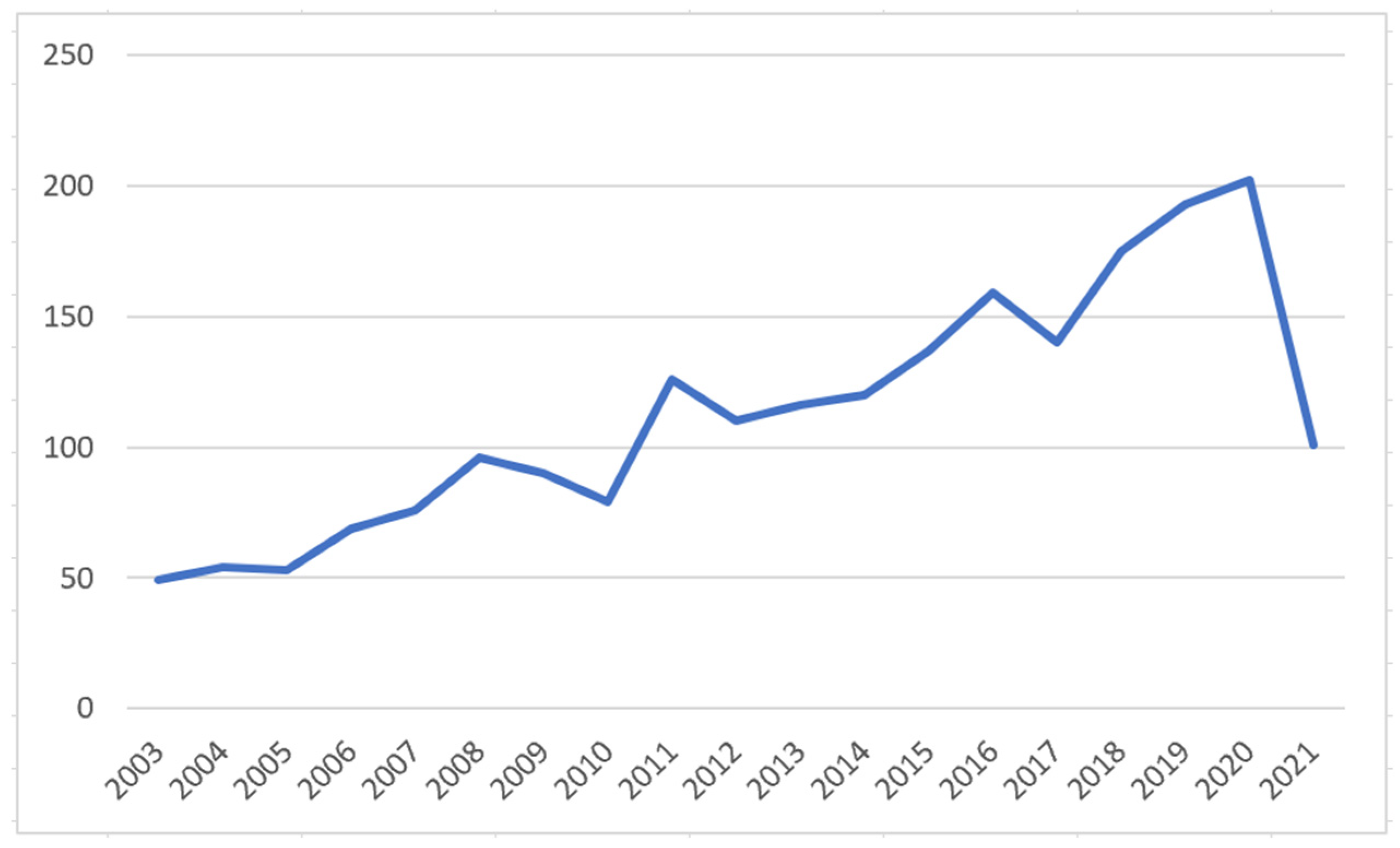
2.1. Time Series Analysis of Volume of Articles
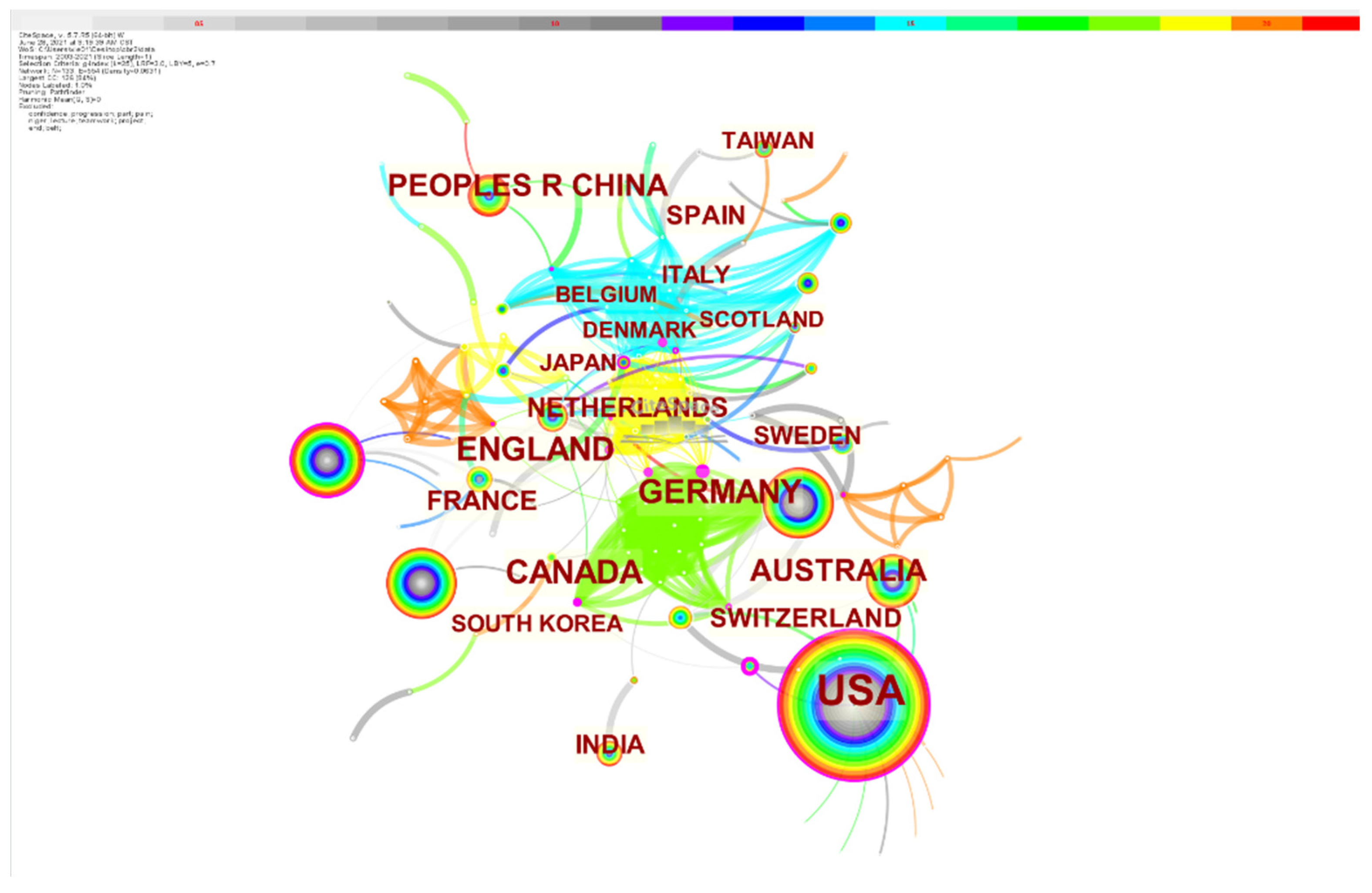
2.2. Country and Region Distribution Analysis
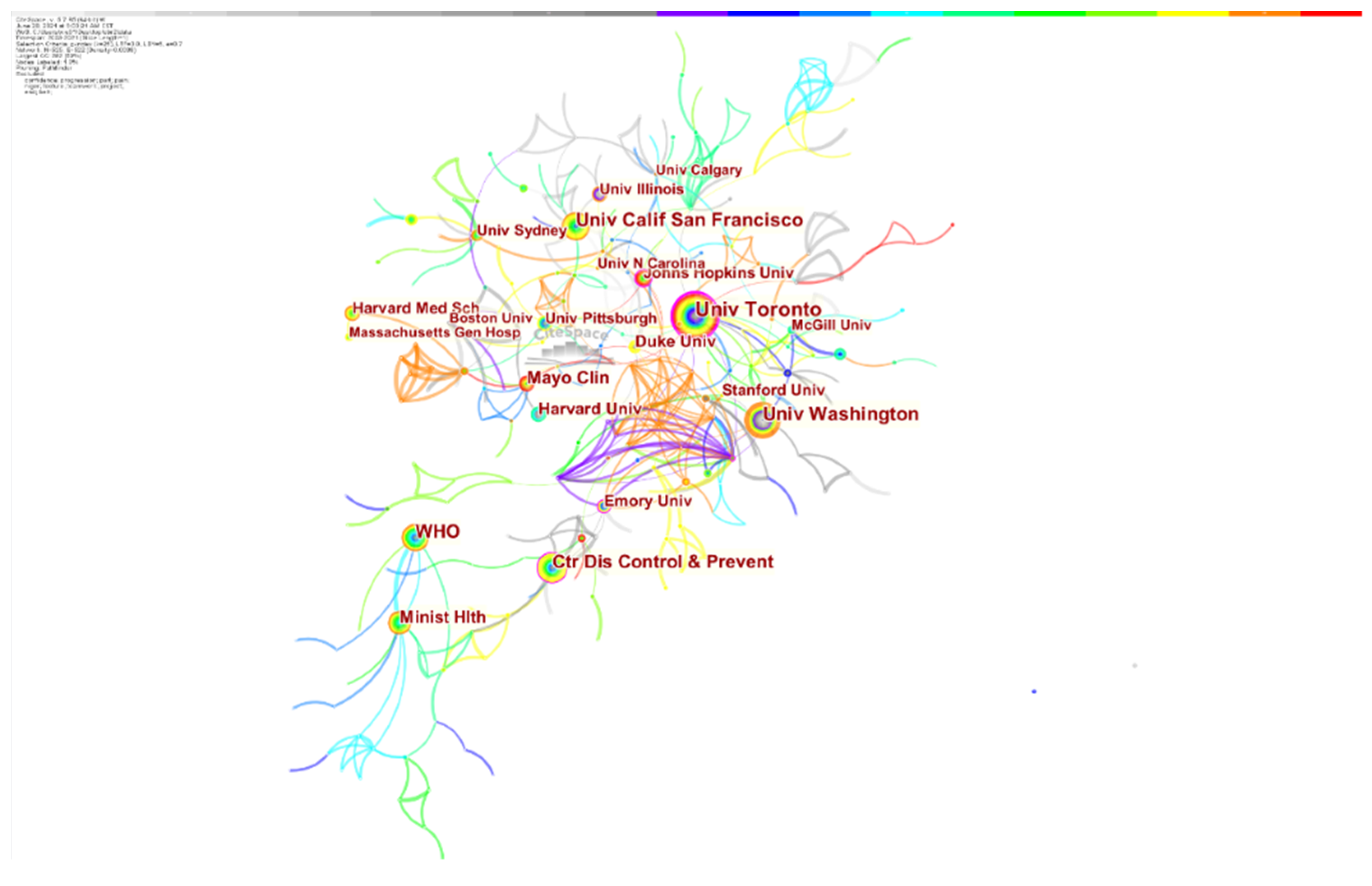
2.3. Institutional Distribution Analysis
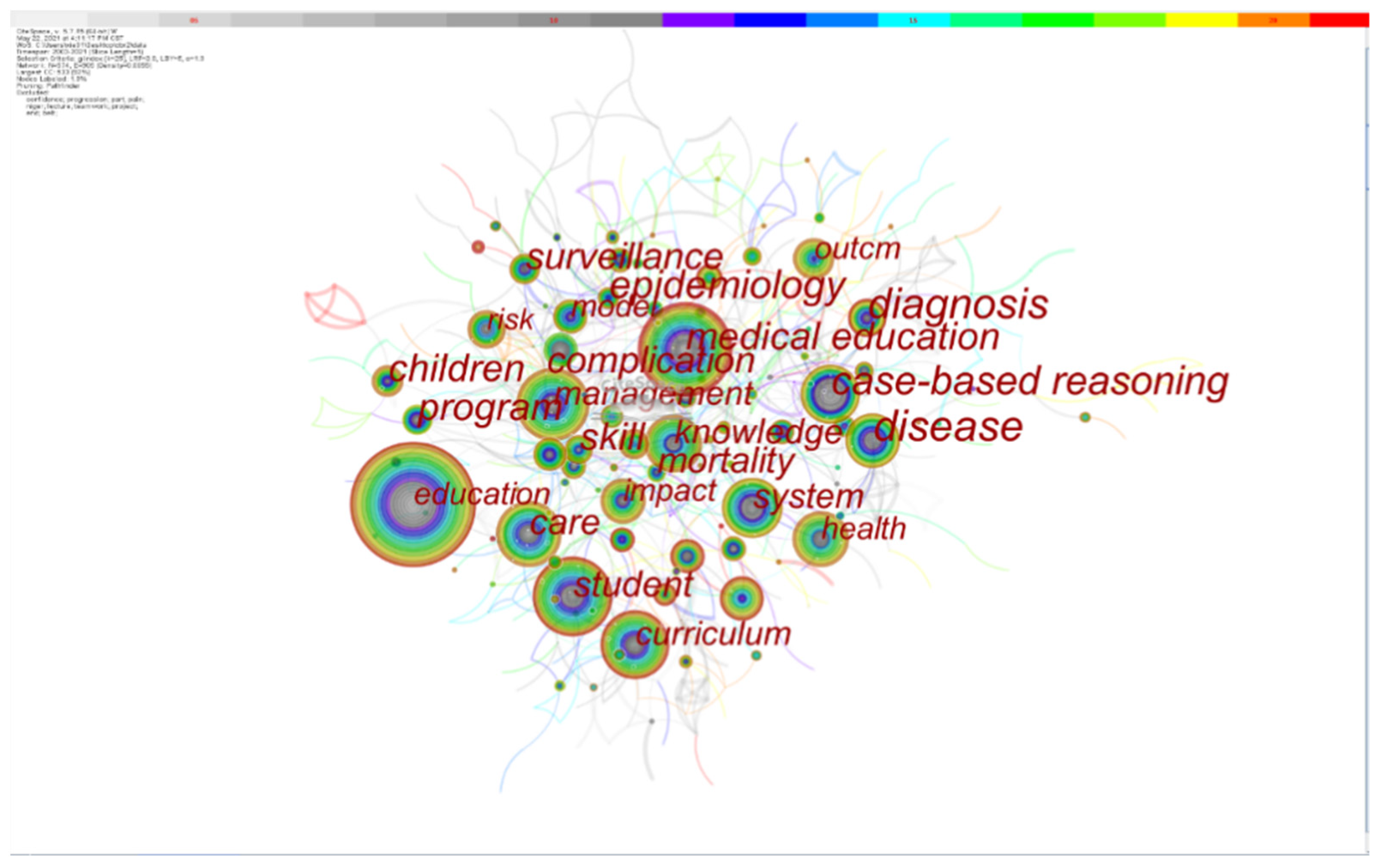
2.4. Analysis of Keyword Co-Occurrence
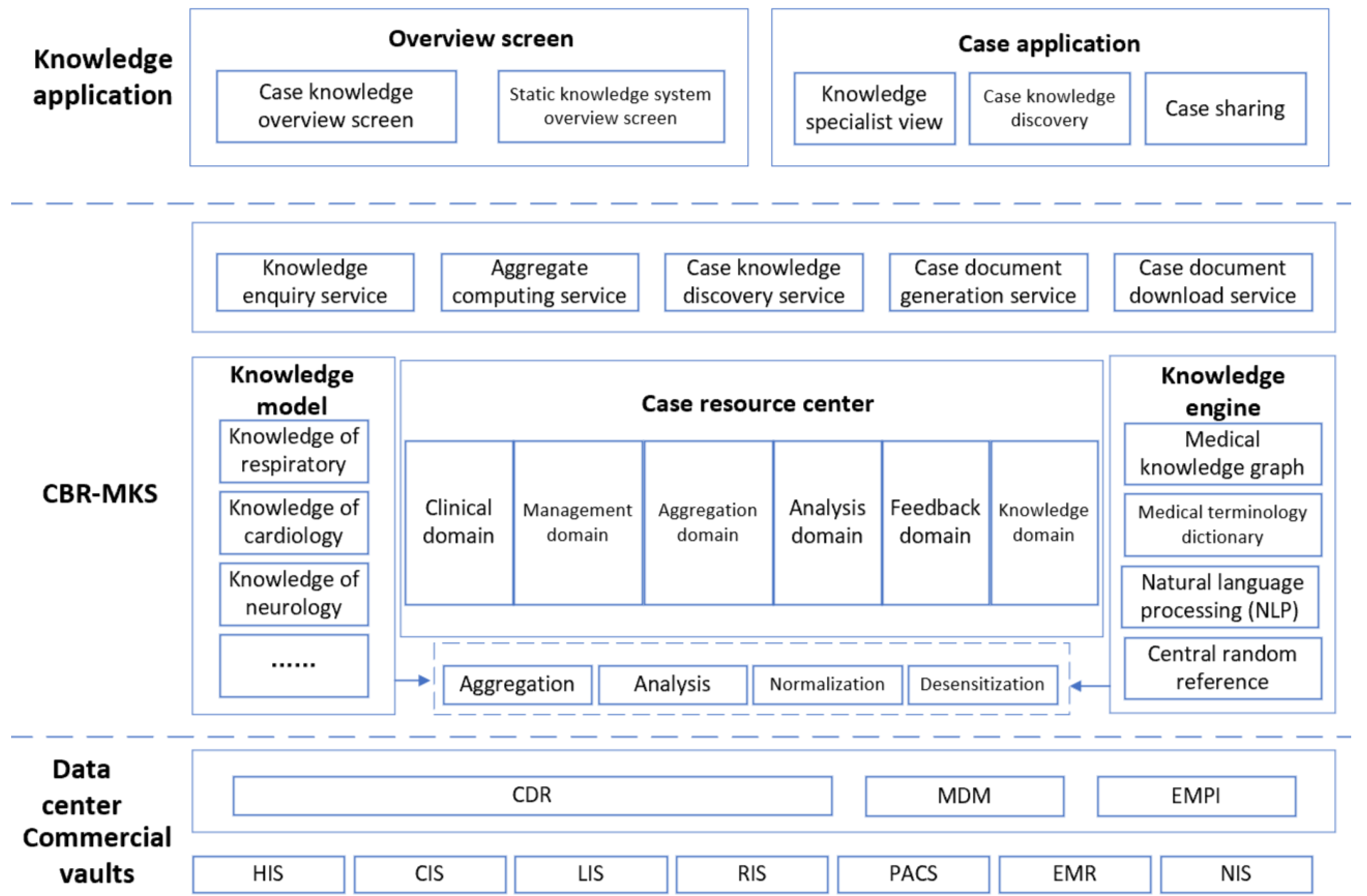
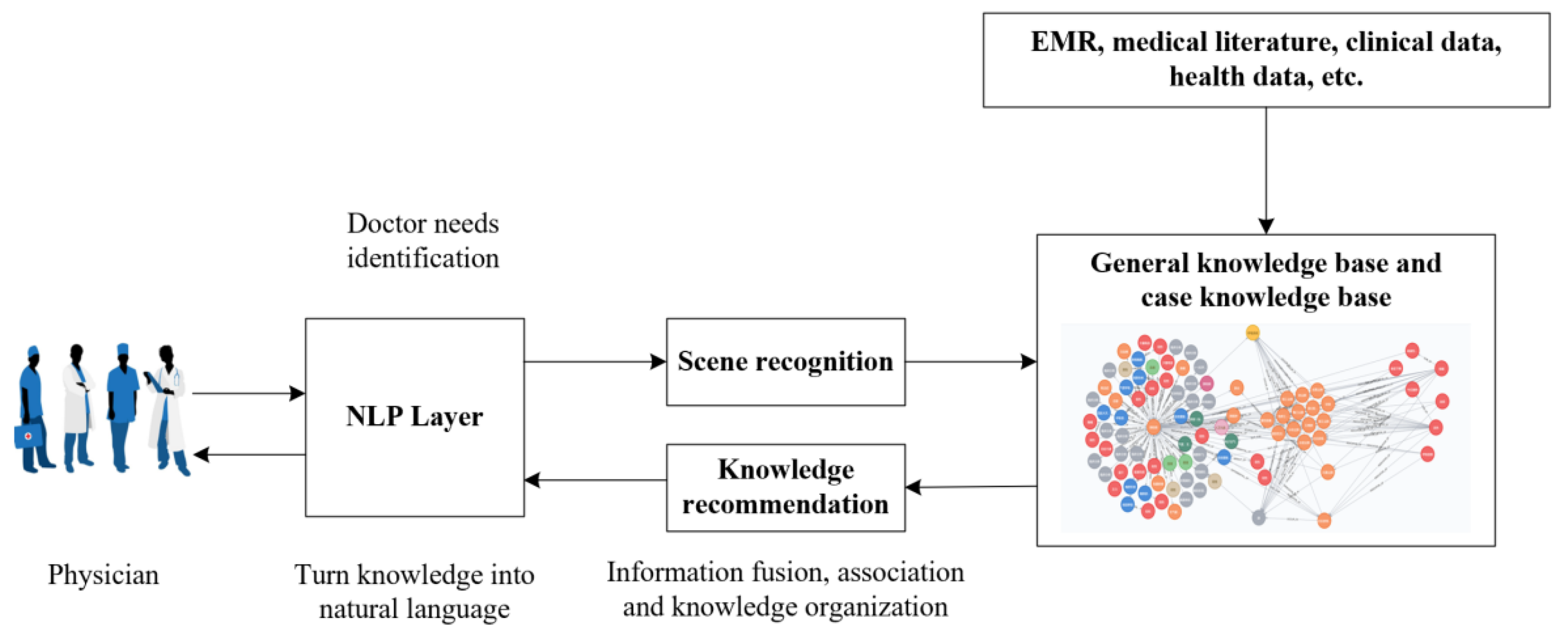
3. CBR-MKS System Framework Design
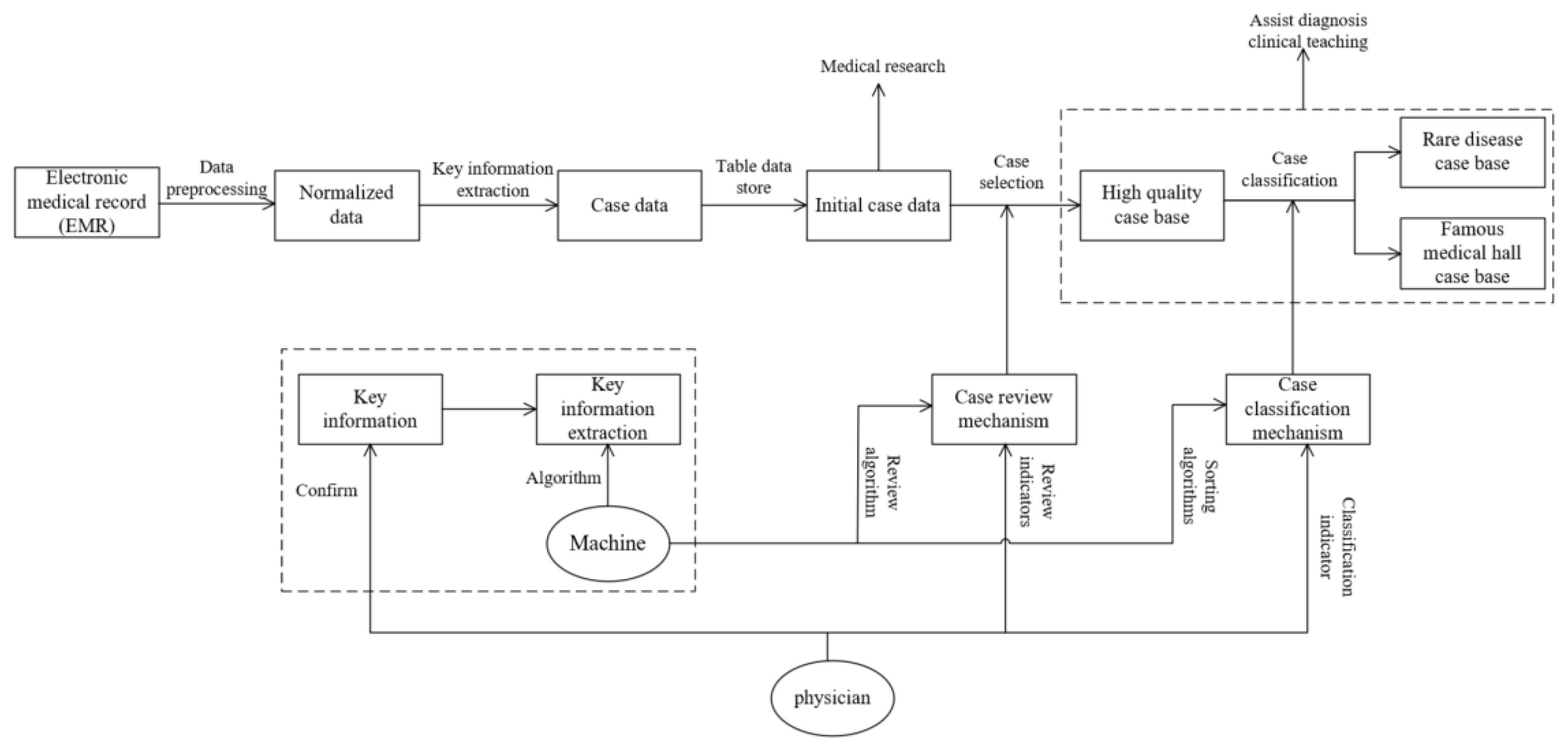
4. Case Base Construction Method
- According to the pre-trained medical word vector dictionary, the word vector matrix of the unstructured text data is obtained.
- The word vector matrix is input into a plurality of pre-constructed classifiers to obtain the sentence sequence after word segmentation.
- The sentence sequence after word segmentation is input into multiple pre-constructed part-of-speech markers to obtain the result of the part-of-speech markers.
CL5:“examination test,” CL6:“treatment plan,” CL7:“other”}
- According to the part-of-speech tagging results, the key text information is obtained.
- According to the key feature information, the initial case knowledge base is obtained.
- According to the audit index proposed by physicians for disease knowledge, high-quality cases are selected from the initial case knowledge base, and the high-quality case knowledge base is obtained.
- According to the classification indices proposed by physicians for ease of understanding and rare cases, the high-quality case knowledge base is classified, and the case knowledge bases of cases by expert physicians and rare diseases are obtained.
5. Case Knowledge Matching Model
6. Pilot Application Evaluation
7. Limitations and Future Works
- Although the accuracy of the system’s recommendation algorithm is already high, it is still not 100%, and the system still has the possibility of recommending error cases. Under this circumstance, if the physician could not conduct comprehensive research and judgment on the basis of the actual condition of the patient combined with his or her own experience and apply the results recommended by the system rigidly, it may bring more serious consequences. Before using the system, physicians need to be trained on the operating specifications, risks, and ethics to help them use the system correctly and clarify the potential risks that may exist in the system.
- A large number of historical cases contain private information, such as the patient’s name, disease, and contact information. A risk of patient privacy disclosure is present in the process of opening and sharing case data from one medical institution to another. Although some patient privacy information (including name, contact information, ID card number, and other sensitive privacy information) has been masked or removed to ensure patients’ privacy during CBR-MKS use, and different users are set different access and browsing permissions for information, a stricter patient privacy protection mechanism needs to be constructed in the system to further reduce the risk of disclosure of patient privacy information due to high sensitivity of medical data.
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Probability of Dying between Exact Ages 30 and 70 from Any of Cardiovascular Disease, Cancer, Diabetes, or Chronic Respiratory (%). Available online: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/probability-of-dying-between-exact-ages-30-and-70-from-any-of-cardiovascular-disease-cancer-diabetes-or-chronic-respiratory-(-) (accessed on 18 July 2021).
- The Top 10 Causes of Death. Available online: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death (accessed on 13 July 2021).
- The Head of the Office of the Leading Group of the Seventh National Census under the State Council Interviewed with China News Agency. Available online: http://www.stats.gov.cn/tjsj/sjjd/202105/t20210513_1817436.html (accessed on 29 June 2021).
- Transcript of the State Council Information Office’s Press Conference on December 23, 2020. Available online: http://www.nhc.gov.cn/xcs/s3574/202012/bc4379ddf4324e7f86f05d31cc1c4982.shtml (accessed on 29 June 2021).
- Lee, T.; Liu, C.; Kuo, Y.; Mills, M.E.; Fong, J.; Hung, C. Application of Data Mining to the Identification of Critical Factors in Patient Falls Using a Web-Based Reporting System. Int. J. Med. Inform. 2011, 80, 141–150. [Google Scholar] [CrossRef] [PubMed]
- Islam, M.S.; Hasan, M.M.; Wang, X.; Germack, H.D.; Noor, E.A.M. A Systematic Review on Healthcare Analytics: Application and Theoretical Perspective of Data Mining. Healthcare 2018, 6, 54. [Google Scholar] [CrossRef] [PubMed]
- Thompson, S.; Whitaker, J.; Kohli, R.; Jones, C. Chronic Disease Management: How It and Analytics Create Healthcare Value through the Temporal Displacement of Care. MIS Q. 2020, 44, 227–256. [Google Scholar] [CrossRef]
- Shilo, S.; Rossman, H.; Segal, E. Axes of a Revolution: Challenges and Promises of Big Data in Healthcare. Nat. Med. 2020, 26, 29–38. [Google Scholar] [CrossRef] [PubMed]
- Pramanik, I.; Lau, R.Y.K.; Azad, A.K.; Hossain, S.; Hossain, K.; Karmaker, B.K. Healthcare Informatics and Analytics in Big Data. Expert Syst. Appl. 2020, 152, 113388. [Google Scholar] [CrossRef]
- Son, J.; Brennan, P.F.; Zhou, S. A Data Analytics Framework for Smart Asthma Management Based on Remote Health Information Systems with Bluetoothenabled Personal Inhalers. MIS Q. 2020, 44, 285–303. [Google Scholar] [CrossRef]
- Liang, H.; Tsui, B.Y.; Ni, H.; Valentim, C.C.; Baxter, S.L.; Liu, G.; Cai, W.; Kermany, D.S.; Sun, X.; Chen, J.; et al. Evaluation and Accurate Diagnoses of Pediatric Diseases Using Artificial Intelligence. Nat. Med. 2019, 25, 433–438. [Google Scholar] [CrossRef] [PubMed]
- Aamodt, A.; Plaza, E. Case-Based Reasoning: Foundational Issues, Methodological Variations, and System Approaches. AI Commun. 1994, 7, 39–59. [Google Scholar] [CrossRef]
- Montani, S.; Portinale, L.; Leonardi, G.; Bellazzi, R.; Bellazzi, R. Case-Based Retrieval to Support the Treatment of End Stage Renal Failure Patients. Artif. Intell. Med. 2006, 37, 31–42. [Google Scholar] [CrossRef] [PubMed]
- Eshach, H.; Bitterman, H. From Case-Based Reasoning to Problem-Based Learning. Acad. Med. 2003, 78, 491–496. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Soubhi, H.; Bayliss, E.A.; Fortin, M.; Hudon, C.; van den Akker, M.; Thivierge, R.; Posel, N.; Fleiszer, D. Learning and Caring in Communities of Practice: Using Relationships and Collective Learning to Improve Primary Care for Patients with Multimorbidity. Ann. Fam. Med. 2010, 8, 170–177. [Google Scholar] [CrossRef] [PubMed]
- Arora, S.; Kalishman, S.; Thornton, K.; Dion, D.; Murata, G.; Deming, P.; Parish, B.; Brown, J.; Komaromy, M.; Colleran, K.; et al. Expanding Access to Hepatitis C Virus Treatment-Extension for Community Healthcare Outcomes (Echo) Project: Disruptive Innovation in Specialty Care. J. Hepatol. 2010, 52, 1124–1133. [Google Scholar] [CrossRef] [PubMed]
- Montani, S. Exploring New Roles for Case-Based Reasoning in Heterogeneous AI Systems for Medical Decision Support. Appl. Intell. 2008, 28, 275–285. [Google Scholar] [CrossRef]
- Gu, D.; Liang, C.; Zhao, H. A Case-Based Reasoning System Based on Weighted Heterogeneous Value Distance Metric for Breast Cancer Diagnosis. Artif. Intell. Med. 2017, 77, 31–47. [Google Scholar] [CrossRef] [PubMed]
- Nasiri, S.; Zahedi, G.; Kuntz, S.; Fathi, M. Knowledge Representation and Management Based on an Ontological CBR System for Dementia Caregiving. Neurocomputing 2019, 350, 181–194. [Google Scholar] [CrossRef]
- El-Sappagh, S.; Elmogy, M.; Riad, A.M. A Fuzzy-Ontology-Oriented Case-Based Reasoning Framework for Semantic Diabetes Diagnosis. Artif. Intell. Med. 2015, 65, 179–208. [Google Scholar] [CrossRef] [PubMed]
- Caruana, R.; Lou, Y.; Gehrke, J.; Koch, P.; Sturm, M.; Elhadad, N.; Assoc Comp, M. Intelligible Models for HealthCare: Predicting Pneumonia Risk and Hospital 30-day Readmission. In 21st ACM SIGKDD Conference on Knowledge Discovery and Data Mining (KDD), University Technol Sydney, 10–13 August 2015; Institute for Advanced Analytics: Sydney, Australia, 2015. [Google Scholar]
- Chen, C.M. Citespace II: Detecting and Visualizing Emerging Trends and Transient Patterns in Scientific Literature. J. Assoc. Inf. Sci. Technol. 2006, 57, 359–377. [Google Scholar] [CrossRef]
- Roy, S.B.; Basak, M. Journal of Documentation: A Bibliometric Study. Available online: https://digitalcommons.unl.edu/libphilprac/945 (accessed on 18 July 2021).
- Stanfill, C.; Waltz, D. Toward Memory-Based Reasoning. Commun. ACM 1986, 29, 1213–1228. [Google Scholar] [CrossRef]
- Gu, D.; Su, K.; Zhao, H. A Case-Based Ensemble Learning System for Explainable Breast Cancer Recurrence Prediction. Artif. Intell. Med. 2020, 107, 101858. [Google Scholar] [CrossRef] [PubMed]
- Gu, D.; Deng, S.; Zheng, Q.; Liang, C.; Wu, J. Impacts of case-based health knowledge system in hospital management: The mediating role of group effectiveness. Inf. Manag. 2019, 56, 103162. [Google Scholar] [CrossRef]
| Assessment Item of CBR-MKS | Degree of Approval (10 Full Points) | Assessment Item of CDSS | Degree of Approval (10 Full Points) |
|---|---|---|---|
| 1. Whether the system promotes knowledge adoption | 9.11 | 1. Whether the system promotes knowledge adoption | 6.89 |
| 2. Whether the system is easy to use | 8.77 | 2. Whether the system is easy to use | 7.55 |
| 3. Whether the system facilitates your participation | 8.73 | 3. Whether the system facilitates your participation | 4.93 |
| 4. Whether the system is useful for improving the quality of care | 8.65 | 4. Whether the system is useful for improving the quality of care | 6.92 |
| 5. Whether the system meets your expectations | 8.85 | 5. Whether the system meets your expectations | 6.07 |
| 6. Whether the system recommended solution can be interpreted | 9.01 | 6. Whether the system recommended solution can be interpreted | 4.48 |
| 7. Whether the system is considered reliable | 9.09 | 7. Whether the system is considered reliable | 8.94 |
| 8. Whether the system helps to improve your capabilities | 9.22 | 8. Whether the system helps to improve your capabilities | 7.72 |
| 9. Are you willing to continue using the system? | 9.34 | 9. Are you willing to continue using the system? | 6.95 |
| 10. Are you willing to recommend the system to peers for use? | 8.89 | 10. Are you willing to recommend the system to peers for use? | 5.43 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xie, Y.; Gu, D.; Wang, X.; Yang, X.; Zhao, W.; Khakimova, A.K.; Liu, H. A Smart Healthcare Knowledge Service Framework for Hierarchical Medical Treatment System. Healthcare 2022, 10, 32. https://doi.org/10.3390/healthcare10010032
Xie Y, Gu D, Wang X, Yang X, Zhao W, Khakimova AK, Liu H. A Smart Healthcare Knowledge Service Framework for Hierarchical Medical Treatment System. Healthcare. 2022; 10(1):32. https://doi.org/10.3390/healthcare10010032
Chicago/Turabian StyleXie, Yi, Dongxiao Gu, Xiaoyu Wang, Xuejie Yang, Wang Zhao, Aida K. Khakimova, and Hu Liu. 2022. "A Smart Healthcare Knowledge Service Framework for Hierarchical Medical Treatment System" Healthcare 10, no. 1: 32. https://doi.org/10.3390/healthcare10010032
APA StyleXie, Y., Gu, D., Wang, X., Yang, X., Zhao, W., Khakimova, A. K., & Liu, H. (2022). A Smart Healthcare Knowledge Service Framework for Hierarchical Medical Treatment System. Healthcare, 10(1), 32. https://doi.org/10.3390/healthcare10010032







